Beruflich Dokumente
Kultur Dokumente
Set Ea505092
Hochgeladen von
davidvpnOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Set Ea505092
Hochgeladen von
davidvpnCopyright:
Verfügbare Formate
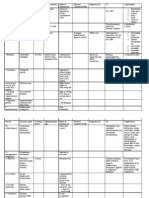
25 Nursing Assessment - Resp (c)
Study online at quizlet.com/_188y3x
1.
accessory muscles
internal intercostals
scalene (lateral neck)
trapezius
abdominals
sternocleidomastoid (ant. neck)
2.
Acute coughs are
most often ____
viral
3.
adventitious breath
sounds
includes crackles, rales, wheezing,
stridor, pleural friction rub
4.
anatomic
deadspace
air in the conducting airway - from mouth
to bronchioles
-not participating in gas exchange
5.
Causes of coughing
inflammation, tension in airways, tumors,
allergies, smoking, post nasal drip,
esophageal reflux, and less commonly
left-sided HF
Chronic Bronchitis
is a classic sign of
? (2)
lung cancer
tuberculosis
7.
clubbing
caused by chronic hypoxia
8.
Correct
auscultation form:
-Breathe normally through open mouth
-start at apices above scapula from left
to right down back
-compare sounds bilaterally
-Breath sounds on Left are heard 1 inch
Lower than right due to higher right
diaphragm/liver
9.
crackles
aka rales; predominately inspiration,
may clear with coughing, due to fluid in
lungs
10.
crepitus
may be used interchangeably with subq
emphysema but also refers to bone or
joint abnormalities
6.
17.
Dehydration and dry skin
is common in ____ pts
COPD (and asthma)
18.
dyspnea
subjective feeling of shortness of
breath/breathlessness
-pts may describe feeling
smothered or pins and needles
sensation
19.
Edema in lower
extremities is usually
related to ____ which is
common in patients with
____
right-sided heart failure, COPD
20.
Expiration
Relaxation: chest size reduces
which increases pressure
gradient
21.
Familial risk of lung
cancer is most likely
related to:
Smoking cigarettes inside the
house
22.
fremitus
vibration transmitted through the
lungs and chest wall and
palpated on the pts thorax during
low frequency vocalization
-increased with density in lungs:
neoplasm, atelectasis,
pneumonia, fibrosis
-decreased when fluid or air in
lung space: COPD, obesity
23.
hemoptysis
coughing up blood
-may indicate infection, pulm
vasculitits pulm emboli, pulm
edema, bronchitits, lung abcess,
TB or cancer
24.
hemothorax
blood in pleural cavity
-usually caused by trauma
-can lead to hemodynamic
compromise and shock
11.
CT angiography are
used to detect
pulm embolism
12.
Cultural
Considerations:
Amulets
Jewelry worn to ward off evil
-ask pt to wear on different part of body
for tests or leave it in view
25.
hyperpnea (Kussmaul
breathing)
Increased rate AND depth
-associated with metabolic
acidosis
13.
Cultural
Considerations:
Coining or Cupping
May leave marks, lesions, burns on skin
- may be mistaken for signs of abuse
26.
hypoxemia
decrease O2 in blood
low pO2 levels
27.
14.
Cultural
Considerations:
Herbal Remedies
and bathing
Some culturals believe that avoid water
and bathing will help resp illness
echinacea (Native American)
opium (Laos) used as analgesic
important info to obtain in
patient history:
culture, nutrition, exercise,
recent travel, social history,
occupational history
28.
Inspiration
15.
Cyanosis is usually
caused by ____,
____, and ____
disorders
cardiac, pulmonary, blood
Contraction: diaphragm drops,
external intercostals expand up
and out
REDUCES pressure inside lungs
16.
deadspace
ventilation
When blood flow to normally ventilated
alveoli is impaired
-example: pulm emboli, any condition
that reduces cardiac output (shock)
29.
Most common
risk factors
for resp
disorders
include
smoking (eventually leads to COPD, 85% of
lung cancers)
inactivity (risk for DVTs, pulm emboli)
CV disease
obesity (increased resistance, decreased lung
vol., Apnea)
substance abuse (CNS depressants can
contribute to pnemonia)
trauma (pneumonias, hypoventilation,
atelectasis)
41.
respiratory
alkalosis
pH > 7.45 high
pCO2 < 35 low
caused by hyperventilation and blowing
off of excess CO2
42.
resp. regulator in
brain
medulla oblongata (and pons)
43.
Role of the trachea
adds moisture
protects from dust, bacteria, ozone
warms/cools air to body temp
44.
shunt ventilation
When perfusion is normal but ventilation
is inadequate, blood flows past alveoli
w/o being oxygenated
-s/s of hypoxia
-examples: atelectasis, pneumonia,
pulm edema, COPD
45.
stridor
harsh crowing high pitched,
predominately inspiration, does not
clear with coughing, caused upper
airway obstruction or croup
-moderate to severe stridor is a sign of
airway obstruction and is considered a
medical emergency
46.
subcutaneous
emphysema
crackling sensation felt during palpation
caused by air in the subcutaneous
tissue
-etiology includes pneumothorax,
ruptured bronchial tube, ruptured
esophagus, gas gangrene
47.
Symptoms of
hypoxia
Mental status changes - agitation, poor
judgement, poor memory, attention
deficit
48.
Symptoms of
increased CO2 in
blood
lethargy, HA, decreased LOC
49.
Under normal
conditions, __% of
O2 is bound to
hemoglobin
98
50.
What does O2
attach to for
transport fro
cellular
consumption?
hemoglobin
51.
What does OPQRST
stand for?
Onset( - when did it start? What were
you doing?)
Provoking/palliative factors( - what
makes it better/worse?)
Quality( - describe your symptoms)
Region/Radiation( - location? does it
move?)
Severity( - pain scale)
Time( - When does it start? how long
does it last?)
30.
a
nonproductive
cough may be
related to: (2)
ACE inhibitors
irritation to airway
31.
non-rhythmic
breathing is a
classic sign
of:
neurological dysfunction
32.
Nursing
assessment
of resp status
includes:
interview
physical
careful monitoring
tests and labs
33.
Pallor +
increased HR
=
anemic and exercise intolerant
34.
Physical
Assessment:
What should
you LOOK for
signs of distress
use of accessory muscles/nasal flaring
General appearance
35.
Pink, frothy
sputum is
classic sign
of ?
pulm edema
plerual
friction rubs
high-pitched grating or squeking, heard on
inspiration AND expiration, does NOT clear
with coughing, caused by parietal and visceral
pleura rubbing together due to inflammtion
pneumothorax
air in the pleural space that prevents lung
from fully expanding and results in collapsed
lung
36.
37.
A pt with lots
of sputum
should have
more/less
water?
more
39.
Pulmonary
Function Test
PFT
determines the ability of the lungs to
efficiently exchange O2 and CO2
-spirometry, lung vol measurements, diffusing
capacity, ABG
40.
respiratory
acidosis
pH < 7.35 low
pCO2 > 45 high
causes drowsiness and unconsciousness
treat with increased ventilation
38.
52.
What to ask for PMH: Allergies
Allergies symptoms include congestion, coughing, wheezing, anaphaylaxis, airway
obstruction
Need to know about meds, plants foods, dusts, molds, and animals
53.
What to ask for PMH: Childhood
1. Immunizations (including flu),
2. premature birth (surfacant)
3. childhood diseases genetic or not (asthma and cystic fibrosis are most common)
-also ask about frequent colds, wheezing or SOB, swimming accidents, foreign body
accidents
54.
What to ask for PMH: Meds
bronchodilators
anticholinergics
steriods
Increased dosage or failure to take meds may increase pulm symptoms
Include OTC/herbals
Have pt demonstrate inhaler use
Bipap/Cpap and O2 are meds
55.
What to ask for PMH: Med/Surg
asthma exacerbation, infectious diseases, hospitalizations,
Trach, chest tube, intubation, prolonged O2 use, cardiac disease, thyroid tx for goiter,
liver failure
56.
wheezes aka rhonchi
musical, mostly expiration, usually not cleared with coughing, caused by airway
narrowing, secretions, inflammation
57.
Will a decrease/increase in pH stimulate
increased RR?
decrease (acidemia)
Das könnte Ihnen auch gefallen
- Wall ChartDokument2 SeitenWall ChartAhmed Fittoh Mosallam0% (1)
- Knorr FinalDokument25 SeitenKnorr Finalimbree100% (3)
- Exam 1 (NUR-152)Dokument5 SeitenExam 1 (NUR-152)davidvpnNoch keine Bewertungen
- Midterm Quiz - NCM 106.2016Dokument4 SeitenMidterm Quiz - NCM 106.2016Andrea BroccoliNoch keine Bewertungen
- Annotated BibliographyDokument7 SeitenAnnotated Bibliographyapi-208209967Noch keine Bewertungen
- What is Intermodulation InterferenceDokument3 SeitenWhat is Intermodulation InterferencedekcarcNoch keine Bewertungen
- Load Summary for Premise Under 100kVADokument2 SeitenLoad Summary for Premise Under 100kVAMuhammad Zulhelmi ZawawiNoch keine Bewertungen
- AC7101.1 Rev G 2Dokument37 SeitenAC7101.1 Rev G 2Namelezz ShadowwNoch keine Bewertungen
- Basic Concept of OxygenationDokument50 SeitenBasic Concept of OxygenationWiradianto PutroNoch keine Bewertungen
- Nclex review: Pneumonia, COPD, Asthma StudyDokument11 SeitenNclex review: Pneumonia, COPD, Asthma Studymj078Noch keine Bewertungen
- Amoebiasis: An Overview of Its Causes, Symptoms, Diagnosis and TreatmentDokument8 SeitenAmoebiasis: An Overview of Its Causes, Symptoms, Diagnosis and TreatmentCheska ت HortelanoNoch keine Bewertungen
- LECTURE BY: Asst. Prof. Margaret M. Natividad, Ed.D., RN ImmunologyDokument21 SeitenLECTURE BY: Asst. Prof. Margaret M. Natividad, Ed.D., RN ImmunologyZhantelle A. SantosNoch keine Bewertungen
- Common Medical AbbreviationsDokument3 SeitenCommon Medical AbbreviationsBráian Tzéims άλμπαNoch keine Bewertungen
- Dissociative Identity Disorder Case Study W Mil W JeongDokument15 SeitenDissociative Identity Disorder Case Study W Mil W JeongHomework PingNoch keine Bewertungen
- Pleural Fluid Analysis: How The Test Is PerformedDokument4 SeitenPleural Fluid Analysis: How The Test Is PerformedKevin LlorenteNoch keine Bewertungen
- RESPIRATORY SYSTEM Nclex Iloilo 4Dokument27 SeitenRESPIRATORY SYSTEM Nclex Iloilo 4Barangay Centro SurNoch keine Bewertungen
- BODY Weight 100%: Balance/Imbalances & TherapyDokument11 SeitenBODY Weight 100%: Balance/Imbalances & TherapyVictoria Castillo TamayoNoch keine Bewertungen
- EKG Quick ViewDokument1 SeiteEKG Quick ViewJe KirsteneNoch keine Bewertungen
- CD-RESPI TBDokument3 SeitenCD-RESPI TBNae OrdanozoNoch keine Bewertungen
- Nursing CS CroupDokument1 SeiteNursing CS Croupreuben kadarajaNoch keine Bewertungen
- Fabs and Onco Post TestDokument20 SeitenFabs and Onco Post TestJe KirsteneNoch keine Bewertungen
- Research Practice QuestionsDokument18 SeitenResearch Practice QuestionsmiaaNoch keine Bewertungen
- Amoebiasis in Wild Mammals: Ayesha Ahmed M Phil. Parasitology 1 Semester 2013-Ag-2712Dokument25 SeitenAmoebiasis in Wild Mammals: Ayesha Ahmed M Phil. Parasitology 1 Semester 2013-Ag-2712Abdullah AzeemNoch keine Bewertungen
- Chapter 01: Professional Nursing Practice Lewis: Medical-Surgical Nursing, 10th EditionDokument5 SeitenChapter 01: Professional Nursing Practice Lewis: Medical-Surgical Nursing, 10th EditionKenyia CheatumNoch keine Bewertungen
- Gastrointestinal SystemDokument17 SeitenGastrointestinal SystempreetNoch keine Bewertungen
- Pedia Drug StudyDokument11 SeitenPedia Drug StudyPeetah PanNoch keine Bewertungen
- ValvularDokument2 SeitenValvularJulia Rae Delos SantosNoch keine Bewertungen
- Case Study (Asthma)Dokument3 SeitenCase Study (Asthma)AIM100% (1)
- Drugs Used in AnesthesiaDokument33 SeitenDrugs Used in AnesthesiaDelvine AderoNoch keine Bewertungen
- Sample QuestionnaireDokument10 SeitenSample QuestionnaireJess Fernandez BorgaNoch keine Bewertungen
- Test Quiz Hypo Kale MiaDokument6 SeitenTest Quiz Hypo Kale MiaVivian Montesena BreganzaNoch keine Bewertungen
- Registered Nurse Rushed to Help Injured Elderly Woman Hit by MotorcycleDokument26 SeitenRegistered Nurse Rushed to Help Injured Elderly Woman Hit by MotorcycleNina OaipNoch keine Bewertungen
- Communicable DiseaseDokument3 SeitenCommunicable Diseasemiss RNNoch keine Bewertungen
- Managing Heat Exhaustion and HeatstrokeDokument6 SeitenManaging Heat Exhaustion and HeatstrokeMark Elben TeodoroNoch keine Bewertungen
- KABC - Respiratory Assessment QuestionsDokument15 SeitenKABC - Respiratory Assessment QuestionsKim Anulacion100% (1)
- 780 Adult Cardio Resp Assess DSTDokument10 Seiten780 Adult Cardio Resp Assess DSTGursangeet Kaur100% (1)
- A 58 Year Old Client Is Admitted With A Diagnosis of Lung CancerDokument9 SeitenA 58 Year Old Client Is Admitted With A Diagnosis of Lung CancerNur SanaaniNoch keine Bewertungen
- Assessing Clients with Endocrine and Metabolic DisordersDokument4 SeitenAssessing Clients with Endocrine and Metabolic DisordersFelimon BugtongNoch keine Bewertungen
- Day 2 SensesDokument5 SeitenDay 2 SensesMarie Kelsey Acena MacaraigNoch keine Bewertungen
- Lecture Pharma Part 1 - 2011-2012Dokument34 SeitenLecture Pharma Part 1 - 2011-2012Harley Justiniani Dela CruzNoch keine Bewertungen
- Autoimmune DisordersDokument13 SeitenAutoimmune Disordersinah krizia lagueNoch keine Bewertungen
- University of Perpetual Help System DALTA: College of Radiologic TechnologyDokument2 SeitenUniversity of Perpetual Help System DALTA: College of Radiologic TechnologyJynrose Kaye GulpanyNoch keine Bewertungen
- Community Health Nursing ReviewerDokument10 SeitenCommunity Health Nursing ReviewerNicole CastillaNoch keine Bewertungen
- Fuck ShitDokument11 SeitenFuck Shitkrull243100% (2)
- CopdDokument14 SeitenCopdMohd Farid Bin RosliNoch keine Bewertungen
- Medical Surgical by Nursing CribDokument7 SeitenMedical Surgical by Nursing Cribnursegian13100% (1)
- Mcqs - Biochemistry - Immune Response - PFMSG ForumDokument4 SeitenMcqs - Biochemistry - Immune Response - PFMSG ForumDillu SahuNoch keine Bewertungen
- NeuroSensory ExamsDokument26 SeitenNeuroSensory Examsquidditch07100% (1)
- Part 1 RenalDokument8 SeitenPart 1 RenalKatherine ApostolNoch keine Bewertungen
- Medical Surgical: SNS (Anti-Cholinergic/adrenergic)Dokument12 SeitenMedical Surgical: SNS (Anti-Cholinergic/adrenergic)Pedro SorianoNoch keine Bewertungen
- ABG analysis for respiratory failure therapy effectivenessDokument25 SeitenABG analysis for respiratory failure therapy effectivenessHan Nah0% (1)
- Endo GI Extra QuestionsDokument3 SeitenEndo GI Extra QuestionsToni Marie Buenconsejo PunzalanNoch keine Bewertungen
- Drugs Acting On Functions of Respiratory SystemDokument73 SeitenDrugs Acting On Functions of Respiratory SystemMarin ChianuNoch keine Bewertungen
- Asthma and COPD NCLEXDokument17 SeitenAsthma and COPD NCLEXPotchiee PfizerNoch keine Bewertungen
- Fluid and electrolyte practice questionsDokument5 SeitenFluid and electrolyte practice questionspbiluanNoch keine Bewertungen
- Chapter 13: Clients With Fluid ImbalancesDokument6 SeitenChapter 13: Clients With Fluid ImbalancesTrixie AlvarezNoch keine Bewertungen
- Angina PectorisDokument8 SeitenAngina PectorisJoanne LagusadNoch keine Bewertungen
- Medical Surgical Nursing IDokument11 SeitenMedical Surgical Nursing IAJ DalawampuNoch keine Bewertungen
- Infectious Disease Medications ModuleDokument8 SeitenInfectious Disease Medications ModuleSheril MarekNoch keine Bewertungen
- Pharmacology Bullet ReviewDokument36 SeitenPharmacology Bullet ReviewNa Young You100% (1)
- A. A Sudden Change in How Brain Cells Send Electrical Signals To One AnotherDokument70 SeitenA. A Sudden Change in How Brain Cells Send Electrical Signals To One AnotherMwansaay Twain HolyNoch keine Bewertungen
- Answer and Rationale Communicable Disease NursingDokument17 SeitenAnswer and Rationale Communicable Disease NursingCharles Gerard B. BeluanNoch keine Bewertungen
- Chapter 19Dokument16 SeitenChapter 19missy23pap100% (1)
- Chronic Bronchitis GuideDokument5 SeitenChronic Bronchitis GuideJemalyn M. Saludar100% (2)
- 1.2 Immunity Response TransDokument10 Seiten1.2 Immunity Response TransJoshua SaanNoch keine Bewertungen
- Acute & Chronic Bronchitis & COPDDokument49 SeitenAcute & Chronic Bronchitis & COPDHendraDarmawanNoch keine Bewertungen
- Set 719e8be6Dokument7 SeitenSet 719e8be6davidvpnNoch keine Bewertungen
- Health Assessment Exam 1 - RlblackmoreDokument2 SeitenHealth Assessment Exam 1 - RlblackmoredavidvpnNoch keine Bewertungen
- Set Dab0a2b4Dokument2 SeitenSet Dab0a2b4davidvpnNoch keine Bewertungen
- Set 4c16c8b0Dokument4 SeitenSet 4c16c8b0davidvpnNoch keine Bewertungen
- NCLEX Study Guide: Key Pain Management ConceptsDokument2 SeitenNCLEX Study Guide: Key Pain Management Conceptsdavidvpn100% (2)
- Set 312e56c8Dokument2 SeitenSet 312e56c8davidvpnNoch keine Bewertungen
- Set 4713b79cDokument3 SeitenSet 4713b79cdavidvpnNoch keine Bewertungen
- Set 7067f7c2Dokument4 SeitenSet 7067f7c2davidvpnNoch keine Bewertungen
- Set 64522153Dokument1 SeiteSet 64522153davidvpnNoch keine Bewertungen
- Set 4afee412Dokument1 SeiteSet 4afee412davidvpnNoch keine Bewertungen
- Set 09f64a69Dokument13 SeitenSet 09f64a69davidvpnNoch keine Bewertungen
- Block 2 Lab QuizDokument1 SeiteBlock 2 Lab QuizdavidvpnNoch keine Bewertungen
- Set 4c16c8b0Dokument4 SeitenSet 4c16c8b0davidvpnNoch keine Bewertungen
- NCLEX Questions Pain-MusculoskeletalDokument3 SeitenNCLEX Questions Pain-MusculoskeletaldavidvpnNoch keine Bewertungen
- Study Guide - Exam 5 - Nursing 151Dokument3 SeitenStudy Guide - Exam 5 - Nursing 151davidvpnNoch keine Bewertungen
- Exam 1: Who Is Florence Nightingale? Principles of Nightingales TheoryDokument1 SeiteExam 1: Who Is Florence Nightingale? Principles of Nightingales TheorydavidvpnNoch keine Bewertungen
- Block One Nursing ProcessDokument2 SeitenBlock One Nursing ProcessdavidvpnNoch keine Bewertungen
- Exam 1 - Mobilization - Potter-PerryDokument8 SeitenExam 1 - Mobilization - Potter-PerrydavidvpnNoch keine Bewertungen
- EMCC Block One Nursing - Exam 1 Study GuideDokument2 SeitenEMCC Block One Nursing - Exam 1 Study GuidedavidvpnNoch keine Bewertungen
- NUR-151 Exam 4Dokument3 SeitenNUR-151 Exam 4davidvpnNoch keine Bewertungen
- Test 1 NUR 151Dokument3 SeitenTest 1 NUR 151davidvpnNoch keine Bewertungen
- Vocabulary Skin Hair NailsDokument2 SeitenVocabulary Skin Hair NailsdavidvpnNoch keine Bewertungen
- Spring 16-Injectable Check-Off Schedule-Traditional SVDokument1 SeiteSpring 16-Injectable Check-Off Schedule-Traditional SVdavidvpnNoch keine Bewertungen
- Spring 16 Traditional Group Project Sign UpDokument2 SeitenSpring 16 Traditional Group Project Sign UpdavidvpnNoch keine Bewertungen
- Spring 16 Blended Group Project Sign UpDokument2 SeitenSpring 16 Blended Group Project Sign UpdavidvpnNoch keine Bewertungen
- Spring 16-Injectable Check-Off Schedule-Blended SVDokument1 SeiteSpring 16-Injectable Check-Off Schedule-Blended SVdavidvpnNoch keine Bewertungen
- BSN-2D 1st Semester ScheduleDokument2 SeitenBSN-2D 1st Semester ScheduleReyjan ApolonioNoch keine Bewertungen
- My PRC Form-Censored Case NumbersDokument5 SeitenMy PRC Form-Censored Case NumbersLeah Lou Gerona MontesclarosNoch keine Bewertungen
- Curtain WallDokument11 SeitenCurtain WallZameer AhmedNoch keine Bewertungen
- Book 1Dokument100 SeitenBook 1Devasyruc100% (1)
- Colours of the RainbowDokument16 SeitenColours of the RainbowMd A RAZZAKNoch keine Bewertungen
- Being ProfessionalDokument3 SeitenBeing ProfessionalPutra SyahrezaNoch keine Bewertungen
- Comparison of Infrastructure in Punjab and Andhra PradeshDokument7 SeitenComparison of Infrastructure in Punjab and Andhra PradeshDivyam GXNoch keine Bewertungen
- Oplan Nena (Violation of RA 10364 Expanded Anti-Trafficking in Person Act of 2012)Dokument3 SeitenOplan Nena (Violation of RA 10364 Expanded Anti-Trafficking in Person Act of 2012)Jhunary MunarNoch keine Bewertungen
- Portfolio FOR ANADokument6 SeitenPortfolio FOR ANAholdap toNoch keine Bewertungen
- Statistics of Design Error in The Process IndustriesDokument13 SeitenStatistics of Design Error in The Process IndustriesEmmanuel Osorno CaroNoch keine Bewertungen
- Dladla Effect 2013Dokument231 SeitenDladla Effect 2013TheDreamMNoch keine Bewertungen
- Annex C Olp On The RoadDokument7 SeitenAnnex C Olp On The RoadCabanglasanfs OLPNoch keine Bewertungen
- What It Is and The Six Steps Necessary To Achieve ItDokument40 SeitenWhat It Is and The Six Steps Necessary To Achieve ItMalory RobayoNoch keine Bewertungen
- Amnesia With Focus On Post Traumatic AmnesiaDokument27 SeitenAmnesia With Focus On Post Traumatic AmnesiaWilliam ClemmonsNoch keine Bewertungen
- Insulation MBMA-NAIMA Acousticical Performance Guide Noise SoundDokument26 SeitenInsulation MBMA-NAIMA Acousticical Performance Guide Noise SoundDianna LambertNoch keine Bewertungen
- Rorschach y SuicidioDokument17 SeitenRorschach y SuicidioLaura SierraNoch keine Bewertungen
- Cobb 500 PDFDokument14 SeitenCobb 500 PDFNeil Ryan100% (1)
- PatternPro Variable Pitch GunDokument2 SeitenPatternPro Variable Pitch GunVõ HòaNoch keine Bewertungen
- JP - Health and Wholeness Through The Holy CommunionDokument62 SeitenJP - Health and Wholeness Through The Holy Communionjevontan90% (10)
- MSDS - ENTEL BatteryDokument3 SeitenMSDS - ENTEL BatteryChengNoch keine Bewertungen
- Soa Group Health TrackDokument2 SeitenSoa Group Health TrackwasabiwafflesNoch keine Bewertungen
- Acute Atelectasis Prevention & TreatmentDokument9 SeitenAcute Atelectasis Prevention & TreatmentmetabolismeproteinNoch keine Bewertungen
- Reflexes Guide: 20+ Human Reflexes ExplainedDokument37 SeitenReflexes Guide: 20+ Human Reflexes ExplainedSalman KhanNoch keine Bewertungen
- GP Series Portable Generator: Owner's ManualDokument48 SeitenGP Series Portable Generator: Owner's ManualWilliam Medina CondorNoch keine Bewertungen
- Caregiving Learning Activity SheetDokument7 SeitenCaregiving Learning Activity SheetJuvy Lyn Conda100% (5)