Beruflich Dokumente
Kultur Dokumente
J Intensive Care Med 2013 Hinson 3 11
Hochgeladen von
Cindya PerthyCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
J Intensive Care Med 2013 Hinson 3 11
Hochgeladen von
Cindya PerthyCopyright:
Verfügbare Formate
Journal of Intensive
Care Medicine
http://jic.sagepub.com/
Hypertonic Saline and Mannitol Therapy in Critical Care Neurology
Holly E. Hinson, Deborah Stein and Kevin N. Sheth
J Intensive Care Med 2013 28: 3 originally published online 24 March 2011
DOI: 10.1177/0885066611400688
The online version of this article can be found at:
http://jic.sagepub.com/content/28/1/3
Published by:
http://www.sagepublications.com
Additional services and information for Journal of Intensive Care Medicine can be found at:
Email Alerts: http://jic.sagepub.com/cgi/alerts
Subscriptions: http://jic.sagepub.com/subscriptions
Reprints: http://www.sagepub.com/journalsReprints.nav
Permissions: http://www.sagepub.com/journalsPermissions.nav
>> Version of Record - Jan 15, 2013
OnlineFirst Version of Record - Mar 24, 2011
What is This?
Downloaded from jic.sagepub.com by guest on June 30, 2014
Analytic Reviews
Hypertonic Saline and Mannitol
Therapy in Critical Care Neurology
Journal of Intensive Care Medicine
28(1) 3-11
The Author(s) 2013
Reprints and permission:
sagepub.com/journalsPermissions.nav
DOI: 10.1177/0885066611400688
http://jicm.sagepub.com
Holly E. Hinson, MD1, Deborah Stein, MD, MPH, FACS2, and
Kevin N. Sheth, MD3
Abstract
Osmotic agents play a vital role in the reduction of elevated intracranial pressure and treatment of cerebral edema in Neurologic
critical care. Both mannitol and hypertonic saline reduce cerebral edema in many clinical syndromes, yet there is controversy over
agent selection, timing, and dosing regimens. Despite the lack of randomized, controlled trials, our knowledge base on the
appropriate clinical use of osmotic agents continues to expand. This review will summarize the evidence for the use of
mannitol and hypertonic saline in a variety of disease states causing cerebral edema, as well as outlining monitoring and safety
considerations.
Keywords
mannitol, hypertonic saline, osmotic therapy, cerebral edema
Received July 7, 2010, and in revised form September 20, 2010. Accepted for publication October 12, 2010.
Introduction
Although osmotic agents have been utilized to reduce cerebral
edema for nearly 5 decades, significant controversy regarding
choice of agent and dosing exists. While a variety of agents
have been investigated including hypertonic urea, glycerol, and
sorbitol,1-3 this review will focus on the 2 main agents used in
adult clinical practice today: mannitol and hypertonic saline
(HS). This review will summarize the evidence for the use of
these 2 agents in a variety of disease states causing cerebral
edema, as well as outlining monitoring and safety considerations.
Pharmacologic Properties
Mannitol
Mannitol has long been recognized for its ability to reduce
intracranial pressure (ICP) in animals and entered the clinical
realm in 1960s.4 It is a freely filtered, nonmetabolized solute
that decreases the reabsorption of water and, to a lesser extent,
sodium, across the renal tubule, creating diuresis. Mannitol
works in a biphasic fashion to reduce ICP. Initially, it alters
blood dynamics (rheology), specifically by reducing the
viscosity of blood. Mannitol has been shown to reduce blood
viscosity by reducing red cell rigidity, thereby easing the passage of the red cell through small blood vessels independent
of hematocrit.5 This effect disappears 4 hours after administration. Mannitol also increases intravascular volume due to
increased plasma osmolality, as well as increasing cardiac output.6 In response to reduced viscosity and intravascular volume
expansion, there is compensatory cerebral vasoconstriction
when autoregulatory pathways are intact.7 This may be explained
by Ohms law in which flow (Q) pressure difference
(DP)/resistence (R). If autoregulation is impaired, reduction
in ICP may be modest or absent. Of note, increased cerebral
blood flow (CBF) may be seen in areas of injured brain with
impaired autoregulation, largely due to decreased blood viscosity. The second phase of ICP reduction occurs as mannitol
extracts water from the cerebral extracellular space into the
intravascular compartment via the osmotic gradient between
blood and brain. It is thought that this requires an intact
blood-brain barrier to form an osmotic membrane. Controversy
exists regarding where the volume is removedfrom injured
or uninjured tissue. It appears that both injured and uninjured
tissues contribute to the volume of water lost,8,9 particularly in
the models of both diffuse and focal traumatic brain injury
1
Neurosciences Critical Care, Johns Hopkins Medical Institutions, Baltimore,
MD, USA
2
Department of Surgery, University of Maryland School of Medicine,
Baltimore, MD, USA
3
Division of Stroke and Neuro-Critical Care, Departments of Neurology,
Surgery, Neurosurgery, and Anesthesiology, University of Maryland School
of Medicine, Baltimore, MD, USA
Corresponding Author:
Kevin N. Sheth, Division of Neuro-Critical Care & Stroke, Neurology/Neurosurgery/Emergency Med/Anesthesiology, University of Maryland School of
Medicine, University of Maryland Medical Center, Adams Cowley Shock
Trauma Center, 110 South Paca Street, 3rd floor, Baltimore, MD 21201, USA
Email: ksheth@som.umaryland.edu
Downloaded from jic.sagepub.com by guest on June 30, 2014
Journal of Intensive Care Medicine 28(1)
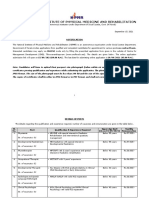
Table 1. Comparison of Osmotic Agents
Solution
Concentration
Sodium Concentration
(mEq/L)
Osmolarity
(mOsm/L)
Ringers lactate
0.009
0.02
0.03
Mannitol 20%
Mannitol 25%
0.075
0.234
130
154
242
513
n/a
n/a
1283
4004
275
308
684
1062
1098
1375
2566
8008
(TBI). Uninjured brain is the main source of water extraction,
especially with repeat dosing in ischemic stroke.10,11
Mannitol is generally dosed 0.25 to 1.0 g/kg.12 The reduction of serum sodium occurs as its resorption across the renal
tubule is inhibited by mannitol. Serum sodium may drop from
9 to 13 mEq/L depending on the patients total body water
content.13 Mannitols excretion is largely governed by the
glomerular filtration rate (GFR); however, in patients with high
amounts of total body water (eg, ascites, severe peripheral
edema) mannitol will be cleared more slowly than predicted
from GFR alone. Assuming normal GFR and total body water,
plasma mannitol concentration should fall to 10% or less of the
initial equilibrium dose after 4 hours, and may be redosed
thereafter.13
Hypertonic Saline
Hypertonic saline gained popularity initially as a volume
expander in acute resuscitation, particularly in hemorrhagic
shock.14 Investigators noted that among patients sustaining
TBI, there was an improved survival rate,15 which was attributed to reduction in cerebral edema and validated in animal
models.16,17 As a result, HS evolved over time as an alternative
to mannitol in treating cerebral edema. Hypertonic saline has
been shown in animal models to produce a biphasic reduction
in ICP, first by way of rheology followed by osmotic activity
across the blood-brain barrier.18,19 Hypertonic saline has the
additional theoretical benefit of being less permeable than
mannitol across the blood-brain barrier due to its higher reflection coefficient. As a consequence, the theoretical potential for
water to follow the solute into the brain worsening cerebral
edema is reduced.20
The majority of inquiry regarding HS has occurred in TBI,
although literature in other forms of cerebral edema exists.
Table 1 compares the concentration and osmolality of several
commonly utilized formulations. As there is no universally
agreed-upon concentration or schedule for administering HS,
comparison between studies is difficult. Additionally, higher
concentrations of HS, particularly 23.4% saline, must be given
via central venous access, making its administration less feasible for patients without a central line catheter.
Continuous infusions as well as bolus dosing of varying
concentrations of HS have been investigated as alternatives
to mannitol for reducing cerebral edema, especially in TBI and
postoperatively. However, the improvements in cerebral edema
seen in TBI have not been observed in patients with ischemic or
hemorrhagic stroke to the same degree, possibly suggesting a
more pronounced effect on vasogenic edema than cytotoxic
edema. Hypertonic saline seems to be safe when given in continuous infusion as an alternative to normal saline. Froelich
et al retrospectively compared patients with varying severe
neurologic injuries, 107 of which received continuous infusions of 3% HS, while 80 received normal saline. Continuous
hypertonic therapy was not associated with an elevated risk
of deep-vein thrombosis, rate of infection, or renal failure compared to the normal saline group.21 In contrast, others have
found continuous hypertonic therapy to be possibly detrimental. Qureshi et al found that continuous infusions of HS
(2% or 3%) did not lessen the need for cerebral edema interventions. In fact, patients receiving continuous HS had higher
in-hospital mortality than patients receiving normal saline.22
These findings lead the authors to recommend bolus dosing
for cerebral edema reduction, which is the preferred practice
in our center.
Clinical Applications
Mannitol Versus HS
Limited head-to-head comparisons exist comparing the
efficacy of mannitol to HS in reduction of ICP. Table 2 lists
5 recent prospective trials comparing the 2 agents. Vialet
et al prospectively examined a series of patients with severe
TBI and elevated ICP, comparing 7.5% saline with 20% mannitol.25 The authors found their patient cohort had fewer episodes and shorter durations of elevated ICP with 2 mL/kg of
7.5% saline compared with 2 mL/kg of body weight of 20%
mannitol. Additionally, episodes of elevated ICP requiring
external ventricular drainage and total CSF drained were fewer
in the saline group.25 However, it is critical to assure that
osmolar loads are dosed in a similar fashion to make a valid
comparison. In the Vialet study, the mannitol group received
a much smaller osmolar load, potentially driving the better
result in the saline group.25 Francony et al compared the effectiveness of a single eqimolar infusion of 20% mannitol with
7.45% HS for ICP reduction in a group of patients with a variety of neurologic injuries. They found that both agents were
equally effective at reducing ICP.24 However, only mannitol
increased cerebral perfusion pressure (CPP) and CBF velocities. Based on these results, the authors recommend mannitol
to be first line in patients with poor cerebral perfusion, and
HS to be considered in patients with hypovolemia or hyponatremia.24 The authors allude to an important clinical concern
when choosing mannitol: vigilant attention to volume status
is essential in order to not disrupt hemodynamics. If not
addressed, this point can be a potential confounder in studies
comparing mannitol with HS. Most recently, Ichai et al
compared 3% sodium lactate with 20% mannitol, both dosed at
1.5 mL/kg in a population of patients with TBI.23 Sodium lactate
Downloaded from jic.sagepub.com by guest on June 30, 2014
Hinson et al
Table 2. Recent Prospective Trials Comparing Mannitol and Hypertonic Saline
Author (Year)
Type of
Prospective Trial Agent
Ichai et al
(2009)23
Francony et al
(2008)24
Battison
(2005)25
Harutjunyan
(2005)26
Vialet et al
(2003)27
Randomized
controlled
Randomized
controlled
Randomized
controlled
Randomized
controlled
Randomized
controlled
Condition(s)
Treated
3% sodium lactate vs 20% mannitol TBI
7.5% HS vs 20% mannitol
TBI Stroke
20 mL 20% mannitol vs 100 mL 7.5% TBI SAH
HS dextran
7.2% HS 6% HES vs 15% mannitol neurosurgical
patients
7.5% HS vs 20% mannitol
TBI
Number of
Patients?
Outcome
34
HS>Mannitol for #ICP, "GOS
20
Both #ICP similarly
HS > mannitol for #ICP
40
HS > mannitol for #ICP
20
HS > Mannitol for reducing elevated
ICP episodes
Abbreviations: CBF, cerebral blood flow; CPP, cerebral profusion pressure; GOS, Glascow Outcome Score; HES, hydroxyethyl starch; HS, hypertonic saline; ICP,
intracranial pressure; NS, normal saline; TBI, traumatic brain injury; SAH, subarchnoid hemorrhage
Table 3. Avoiding Adverse Effects of Osmotic Agents
Complication
Mannitol
Hypertonic Saline
Renal Failure
Rebound
Metabolic Acidosis
Hypokalemia
Hypovolemia
Avoid continuous infusion, repeat high dosing
Allow clearance prior to repeat dosing
n/a
n/a
Concurrent volume resuscitation
Avoid prolonged hypernatremia >160 mEq/L
Allow clearance prior to repeat dosing
Reduce chloride in admixture
Add potassium to fluids
n/a
was chosen as opposed to sodium chloride because the authors
hypothesized that lactate might provide an advantage as a
fuel for the brain under ischemic-reperfusion injury based
on animal studies. Sodium lactate appeared superior in reducing ICP. The group receiving sodium lactate (either as primary
therapy or as rescue after mannitol) had improved 1-year
Glascow Outcome Scores compared to mannitol alone.23
Kerwin et al retrospectively analyzed 22 patients with severe
TBI who received either mannitol (15 to 75 g) or 30 mL of
23.4% HS for control of ICP >20 sustained for more than
5 minutes. The investigators observed significantly greater
drop in ICP in the HS group in comparison to the mannitol
group, leading them to conclude HS is more efficacious in
reducing elevated ICP in TBI.28 Unfortunately, the authors
do not explain how the dosing of mannitol was determined
(ie, a weight-based protocol), making it unclear if patients in
the mannitol group were underdosed, receiving as little as
15 g in some instances.
Traumatic Brain Injury
Hyperosmolar agents role in neurologic injury is probably best
understood in TBI, despite the fact that the evidence even in
TBI ranges from class II to III. Several insights have been
gained about mannitol in this population. Continuous infusion
seems to be no better, if not worse, than bolus dosing. Mannitol
becomes less effective with repeat dosing. Fast infusion seems
to be best. Mannitol works best when autoregulation is intact.
Lastly, mannitol consistently improves MAP, CPP, and CBF
while lowering ICP.29-31
More recently, HS has come to fore as an alternative to
mannitol in TBI. Initially, continuous infusions of hyertonic
saline were investigated. Qureshi et al found that a continuous
infusion of 3% saline exerted a beneficial effect on ICP as well
as improving lateral displacement of brain due to edema in
patients with head injury, spontaneous intracranial hemorrhage
(ICH) or postoperatively (after tumor resection or aneurysm
clipping).31 Like mannitol, bolus dosing of HS has shown more
promise than continuous infusions for ICP management.22
Bolus dosing for both agents might be more effective than continuous osmotic agents because continuous infusions of osmotic agents allow more time for the reestablishment of a new
osmotic set point, such that the intracellular and extracellular
compartments reequilibrate. No further water extraction can
occur once this reequilibration occurs. Several case series have
shown the effectiveness of boluses of HS for the reduction of
ICP in TBI, both as an alternative and as an adjuvant to mannitol.27,33-35 Bolus dosing regimens vary within the literature.
Some authors advocate the use of 2 mL/kg of 7.5%27 for the
control of elevated ICP, while others have used 250 mL boluses
of 3%36 or 30 mL of 23.4%.37 To date, there are no direct
comparison studies between these dosing regimens. Hypertonic
saline also appears to increase levels of brain tissue oxygenation (PbtO2) and improve hemodynamics (higher CPP and
cardiac output) when used as a Tier II therapy after mannitol
administration for elevated ICP. Mannitol had no measurable
effect on PbtO2 in this study.38 Again, these results should be
interpreted with caution as equi-osmolar doses of each agent
were not used. The HS group received a larger osmolar load
(250 mL of 7.5% saline versus 0.75 g/kg of 25% mannitol;
Downloaded from jic.sagepub.com by guest on June 30, 2014
Journal of Intensive Care Medicine 28(1)
Table 1). There is also a suggestion that use of HS may improve
biomarker profiles. Baker et al measured levels of S100B,
neuron-specific enolase (NSE), and myelin basic protein in
patients with severe TBI receiving either normal saline or
7.5% HS with 6% dextran for resuscitation, as opposed to cerebral edema. They found the lowest levels of these biomarkers
in survivors resuscitated with HS; whereas the highest levels
were seen in nonsurvivors. The link between these biomarkers
and survival benefit has not yet been definitively shown.39
As of 2007, the Brain Trauma Foundation Guidelines do not
provide guidance on administration of either mannitol or HS
for elevated ICP in TBI other than to indicate that both agents
may lower ICP.40
Ischemic Stroke
Unlike TBI, controversy exists regarding the utility of hyperosmolar agents in ischemic stroke. First, the lack of intact bloodbrain barrier in ischemic stroke is worrisome, based on the fear
that osmotic agents may leak across the compromised
membrane bringing water with the solute. This phenomenon
has been reported in animals, but may not apply to humans.41
Second, mannitol seems to reduce the water content of the
uninjured hemisphere,11 which could worsen midline shift if
present. To address these concerns, Manno et al examined a
group of patients with complete middle cerebral artery (MCA)
infarctions with cerebral edema and administered boluses of
mannitol. They found that a single, large dose of mannitol
(1.5 g/kg of body weight) did not worsen midline shift nor
precipitate neurologic decline in the first hour after administration.9 From a global outcomes perspective, a large retrospective observational study failed to find any effect of routine
mannitol use on outcome at 1 month or 1 year. Of greater concern, depending on the variables entered into the authors
regression model, mannitol appeared either to have no effect
or to be harmful, rendering the authors unable to make any recommendation on the use of mannitol in ischemic stroke.42
However, it is difficult to interpret these results as the treatment
groups were not homogenous enough to be directly comparable, and routine mannitol use is not a common clinical practiceits use usually being reserved for malignant cerebral
edema. The literature does suggest bolus dosing of mannitol
and HS can reduce ICP, but long-term outcomes in these studies were not addressed.43,44 It may be appropriate not to address
long-term outcomes, as patients requiring osmotic therapy for
cerebral edema are usually critically ill. Critical illness entails
many confounders affecting outcome such as ICU-acquired
infections, requiring large numbers of patients to account for
these confounders. Thus, ICP may be the more appropriate
measure of efficacy.
Continuous infusions of osmotic agents have shown less
promise than bolus dosing. Bhardwaj et al found hypertonic
agents might actually increase infarct volume. Utilizing an
MCA occlusion model of stroke in rats, the investigators initiated osmolar therapy with 20% mannitol, 0.9% normal saline,
3% HS, or 7.5% HS at the onset of reperfusion. The group
observed that continuous infusion hypertonic therapy initiated
at the onset of reperfusion did not reduce infarct volume, thus
may not represent an effective resuscitation strategy after
ischemic stroke. It should be noted, that reperfusion time in
humans is rarely available as a clinical parameter, thus caution
should be employed when generalizing to humans. Surprisingly, the group randomized to 7.5% saline had a statistically
significant increase in infarct volume over the other groups,
causing the authors to caution its use in ischemic stroke.45
Indeed, there has been no randomized, controlled trial addressing the use of mannitol or HS in ischemic stroke. In the
absence of definitive evidence in humans, mannitol rescue
therapy for malignant cerebral edema is the most common
clinical practice. The American Stroke Association guidelines
advise treatment of stroke-related edema and elevated ICP
with mannitol as a bridge to more definitive therapy, such as
decompressive craniectomy.46
Subarchnoid Hemorrhage
Both mannitol and HS significantly lower ICP in the animal
model of subarchnoid hemorrhage (SAH).47,48 A recent
Norwegian study compared 30-minute infusions of 2 mL/kg
of 7.2% HS or 0.9% saline (placebo) and measured ICP in
stable SAH patients. The group observed a reduction in ICP
of 3 mm Hg on average compared with 0.3 mm Hg in the
placebo group, as well as an increase in CPP of 5.6 mm Hg
compared with negligible change in CPP in the placebo group.
The authors favored HS over mannitol in the SAH patient population due to the risks of diuresis-induced hypovolemia and
the inherent risks of vasospasm. Additionally, the authors
hypothesize that SAH patients might be more suitable for the
osmotic effect of HS given a relatively intact blood-brain
barrier.49 Cerebral blood flow was of particular interest to
Tseng et al. Their group showed that infusions of 23.5% HS not
only reduced ICP but also increased CBF as evidenced by
continuous transcranial dopplar and Xenon-enhanced computed
tomography scans. Patients with the greatest increases in CBF in
response to HS seemed to also have the most favorable outcomes
as measured by discharge modified Rankin scores.50
Intracerebral Hemorrhage
Investigation of ICP management in intracerebral hemorrhage
with osmotic agents is less robust than in other disease states
like TBI. From the scant human clinical trials, it appears that
scheduled, low dose mannitol (100 mL of 20% dosed every
4 hours) did not improve outcome in ICH patients or change
CBF.51,52 While no clinical trials of HS in the setting of ICH
have been conducted, animal models suggest bolus dosing of
23.4% HS reverses transtentorial herniation and restores
regional CBF.53 In the same animal model, Quereshi et al also
compared bolus 20% mannitol, bolus 23.4% HS, and continuous 3% HS. While all 3 groups showed an initial drop in ICP
values, the investigators noted that only in the 3% group did
the animals have sustained lower ICP.54 This observation
Downloaded from jic.sagepub.com by guest on June 30, 2014
Hinson et al
represents one of the few accounts in the literature of continuous
osmotic therapy being superior to bolus dosing. This may be
related to the continuous HS group benefiting from longer term
intravascular volume expansion in the intracranial vasculature.
Studies comparing bolus doing versus continuous infusions of
lower concentration HS (2%-3%) are needed to resolve this
issue.
Liver Failure
Cerebral edema may occur as a consequence of acute,
fulminant liver failure. The presumed mechanism of cerebral
edema relates to ammonia and glutamine causing cytotoxic
injury combined with cerebral vasodilation from the loss of
autoregulation.55,56 Although the definitive therapy for fulminant hepatic failure is liver transplantation, the cerebral edema
may be imminently life-threatening. In the 1980s, mannitol
proved to be more effective than dexamethasone for reducing
cerebral edema and improving outcome in liver failure.57
More recently, interest has shifted to HS. Murphy et al induced
moderate hypernatremia (145-155 mmol/L) with a 24-hour
infusion of 30% saline at 10 mL/hour in a group of liver failure
patients with acute liver failure and Grade III or IV encephalopathy, and measured ICP. The group found that moderate
hypernatremia along with the standard of care interventions
significantly reduced ICP from baseline levels when compared
with standard of care alone. Standard of care was provided to
both patient groups, and included standardized ventilation
management, head of bed elevation, ICP monitoring, N-acetylcystine aministration, hemodynamic monitoring with intervention for hypotension, enteral feeding, prophylactic antibiotics,
and hemoglobin goals.58
Transtentorial Herniation
Mannitol, in combination with hyperventilation, has been
shown to reverse transtentorial herniation in a cohort of
28 patients with a variety of underlying illnesses causing cerebral edema (including neoplasm, ICH, TBI, and ischemic
stroke).59 Hypertonic saline has also shown promise in reversing transtentorial brain herniation. A retrospective analysis
of boluses (30-60 mL) of 23.4% HS reversed 75% of clinical
herniation events in a cohort of patients with a variety of
neurologic illnesses.60
Monitoring
Intracranial Pressure
Hyperosmolar agents are frequently used to reduce ICP and/or
reverse brain herniation events. Thus, it is recommended to
have an ICP monitor in place to aid titration.
Serum Sodium Osmolarity
Generally, fluid balance should be monitored closely as mannitol
may cause significant diuresis, while HS expands intravascular
volume. Serum sodium concentrations and plasma osmolality
are usually measured in a serial fashion after the administration
of either HS or mannitol. Target serum sodium and osmolality
values are controversial, but clinicians often strive for serum
sodium concentrations of 150 to 160 mEq/L and plasma osmolality between 300 and 320 mOsm.32 In general, an infusion of
1 mL/kg of 3% saline will raise the serum sodium by approximately 1 mEq/L, regardless of baseline serum sodium concentration.61 The literature suggests an increased risk of acute
renal failure and metabolic acidosis when plasma osmolality
>320 mOsm,12,30 however, this threshold is not absolute.62
Diringer and Zazulia explain well in their review article,
Osmotic Therapy Fact and Fiction,62 that the value of
320 mOsm was arrived at in patients receiving continuous,
high-dose mannitol infusions (0.25-0.5 g/kg per h). None of the
patients in this study developed renal failure with a serum
osmolality below 400 mOsm.63 In fact, a serum sodium of
160 mEq/L and a plasma osmolality of 340 mOsm might be a
safe upper limit.64
Osmolar Gap
Unfortunately, a test for serum mannitol concentration is not
commercially available. Despite its frequent clinical use, serum
osmolality is a poor surrogate for serum mannitol concentrations.65 To surmount this issue, some authors have advocated
the use of osmolar gap (OG) as a method of monitoring mannitol concentrations to avoid complications such as renal failure.
Osmolar gap is the difference between osmolality and osmolarity, which is used to detect the presence of unmeasured osmoles
such as mannitol.62 If the OG falls within the normal range
(varying by formula and patient population), Garcia-Morales
et al assert a patient has sufficiently cleared the mannitol,
and may be redosed.66 It has been suggested that maintaining
an OG below 55 mmol/kg of H2O will help to prevent renal
failure.67 OG may be calculated by several different formulas;
Diringer et al report utilizing 1.86 (Na K) (blood urea
nitrogen/2.8) (glucose/18) 10 provided the best correlation
to measured mannitol levels.62
Complications
Renal Failure
Of particular interest is avoiding renal failure. Mannitol may
become nephrotoxic by several mechanisms, including dosedependent vasoconstriction of the renal artery and intravascular
volume depletion from osmotic diuresis.68,69 In one study, the
mean total dose of mannitol that precipitated acute renal failure
in healthy kidneys was 626 + 270 g over 2 to 5 days.70 There is
an association between prolonged hypernatremia (serum
sodium concentration >160 mEq/L) and oliguric acute renal
failure observed in burn patients receiving HS as resuscitation
fluid.71 Observations of renal failure associated with HS in neurological patients is limited;72,73 however, close monitoring of
renal function is advised. Patients that already require intermittent or continuous renal replacement pose a special challenge to
Downloaded from jic.sagepub.com by guest on June 30, 2014
Journal of Intensive Care Medicine 28(1)
the use of osmotic agents. If mannitol is to be used when renal
failure is already present, the smallest effective dose possible
should be used (consider 0.5 g/kg). Use of hemodialysis to
remove mannitol will expedite the half-life of the drug to
6 hours versus 5 or more days with GFR <50 mL/min. With
regard to sodium balance, the standard sodium concentration
of dialysate is 140 mEq/L. Serum sodium levels will trend
toward 140 mEq/L as dialysis is applied, particularly for continuous renal replacement therapy (CRRT).74 In the authors
experience, frequent redosing of HS is often needed to maintain
hypernatremic goals.
Osmotic Demyelinating Syndrome
Osmotic demyelinating syndrome or more specifically central
pontine myelinolysis (CPM) may occur when sodium levels are
rapidly increased with HS, causing demyelination of white
matter in the CNS or specifically in the pons. Patients are most
at risk when hyponateremia exists at baseline. To date, there are
no case reports of CPM occurring after the administration of
HS for elevated ICP60 nor has CPM been reported in any of the
trials using HS for elevated ICP.72,73
Conclusion
Nearly a century after mannitol was noted to reduce cerebral
edema, osmotic agents including mannitol still play an important role in the medical management of both cerebral edema
and elevated ICP. Despite the lack of randomized, controlled
trials, our knowledge base on the appropriate clinical use of
osmotic agents continues to expand. While not definitively
superior to mannitol, HS shows promise in not only reducing
ICP but also in reversing neurologic deterioration and improving hemodynamics. Future work will further define agent
selection and dosing regimen. The disease state as well as the
type of edema encountered (vasogenic versus cytotoxic) will
likely guide agent selection as clinical practice evolves.
Authors Note
KNS is supported by an American Academy of Neurology Clinical
Research Award
Declaration of Conflicting Interests
The authors declared no potential conflicts of interests with respect to
the authorship and/or publication of this article.
Rebound Phenomenon
After exposure to osmotic agents, ICP may precipitously rise
back to an elevated level after an initial response. This is
termed the rebound phenomenon and occurs particularly
after mannitol administration. Previously rebound was feared
as a consequence of the osmotic agent leaking into injured tissue across a damaged blood-brain barrier, and pulling water
with it, promoting swelling in the injured area. However, observations of mannitol exiting the brain down its concentration
gradient make this explanation less compelling.62 Rebound is
more likely related to osmotic compensation within the central
nervous system, allowing for increased intracellular concentrations of electrolytes. Repeated administration of osmotic
agents, especially in the setting of poor CNS compliance where
small volemic changes result in dramatic changes in ICP,
promote the rebound phenomenon.75 Additionally, repeat
dosing or continuous infusions of these agents without time
allotted for the osmotic agent to clear might also contribute
to this phenomenon.
Metabolic Acidosis
Hypertonic saline inhibits the resorption of bicarbonate from
the proximal renal tubules. It may also produce hyperchloremic
metabolic acidosis from the large amount of chloride delivered
in the fluid. One possible solution to this problem is to change
the fluid admixture to 50:50 sodium chloride-sodium acetate.76
Hypokalemia
Hypokalemia might also be encountered as the kidney
exchanges potassium for sodium in the distal tubule. Addition
of potassium to maintenance fluids may correct this.
Funding
The authors received no financial support for the research and/or
authorship of this article.
References
1. Javid M, Settlage P. Effect of urea on cerebrospinal fluid pressure
in human subjects; preliminary report. J Am Med Assoc. 17
1956;160(11):943-949.
2. Cantore G, Guidetti B, Virno M. Oral glycerol for the reduction of
intracranial pressure. J Neurosurg. 1964;21:278-283.
3. Hemmer R. Comparative studies on the drug-induced decrease in
cerebral pressure. Med Klin. 20, 1961;56:105-108.
4. Wise BL, Chater N. The value of hypertonic mannitol solution in
decreasing brain mass and lowering cerebro-spinal-fluid pressure.
J Neurosurg. 1962;19:1038-1043.
5. Burke AM, Quest DO, Chien S, Cerri C. The effects of mannitol
on blood viscosity. J Neurosurg. 1981;55(4):550-553.
6. Willerson JT, Watson JT, Hutton I, Fixler DE, Curry GC,
Templeton GH. The influence of hypertonic mannitol on regional
myocardial blood flow during acute and chronic myocardial
ischemia in anesthetized and awake intact dogs. J Clin Invest.
1975;55(5):892-902.
7. Muizelaar JP, Lutz HA 3rd, Becker DP. Effect of mannitol on ICP
and CBF and correlation with pressure autoregulation in severely
head-injured patients. J Neurosurg. 1984;61(4):700-706.
8. Wisner DH, Schuster L, Quinn C. Hypertonic saline resuscitation
of head injury: effects on cerebral water content. J Trauma. Jan
1990;30(1):75-78.
9. Manno EM, Adams RE, Derdeyn CP, Powers WJ, Diringer MN.
The effects of mannitol on cerebral edema after large hemispheric
cerebral infarct. Neurology. Feb 1999;52(3):583-587.
Downloaded from jic.sagepub.com by guest on June 30, 2014
Hinson et al
10. Paczynski RP, He YY, Diringer MN, Hsu CY. Multiple-dose
mannitol reduces brain water content in a rat model of cortical
infarction. Stroke. 1997;28(7):1437-1443; discussion 1444.
11. Videen TO, Zazulia AR, Manno EM, et al. Mannitol bolus
preferentially shrinks non-infarcted brain in patients with
ischemic stroke. Neurology. 11 2001;57(11):2120-2122.
12. Bratton SL, Chestnut RM, Ghajar J, et al. Guidelines for the
management of severe traumatic brain injury. II. Hyperosmolar
therapy. J Neurotrauma. 2007;24(Suppl 1):S14-S20.
13. Oken DE. Renal and extrarenal considerations in high-dose
mannitol therapy. Ren Fail. 1994;16(1):147-159.
14. Vassar MJ, Fischer RP, OBrien PE, et al. A multicenter trial for
resuscitation of injured patients with 7.5% sodium chloride.
The effect of added dextran 70. The Multicenter Group for the
Study of Hypertonic Saline in Trauma Patients. Arch Surg.
1993;128(9):1003-1011; ; discussion 1011-1003.
15. Wade CE, Grady JJ, Kramer GC, Younes RN, Gehlsen K,
Holcroft JW. Individual patient cohort analysis of the efficacy
of hypertonic saline/dextran in patients with traumatic brain
injury and hypotension. J Trauma. 1997;42(suppl 5):S61-S65.
16. Anderson JT, Wisner DH, Sullivan PE, et al. Initial small-volume
hypertonic resuscitation of shock and brain injury: short- and
long-term effects. J Trauma. 1997;42(4):592-600; ; discussion
600-591.
17. Bacher A, Wei J, Grafe MR, Quast MJ, Zornow MH. Serial
determinations of cerebral water content by magnetic resonance
imaging after an infusion of hypertonic saline. Crit Care Med.
1998;26(1):108-114.
18. Prough DS, Whitley JM, Taylor CL, Deal DD, DeWitt DS.
Regional cerebral blood flow following resuscitation from hemorrhagic shock with hypertonic saline. Influence of a subdural mass.
Anesthesiology. 1991;75(2):319-327.
19. Schmoker JD, Zhuang J, Shackford SR. Hypertonic fluid
resuscitation improves cerebral oxygen delivery and reduces
intracranial pressure after hemorrhagic shock. J Trauma. 1991;
31(12):1607-1613.
20. Ziai WC, Toung TJ, Bhardwaj A. Hypertonic saline: first-line
therapy for cerebral edema? J Neurol Sci. 15 2007;261(1-2):
157-166.
21. Froelich M, Ni Q, Wess C, Ougorets I, Hartl R. Continuous
hypertonic saline therapy and the occurrence of complications in
neurocritically ill patients. Crit Care Med. 2009;37(4):1433-1441.
22. Qureshi AI, Suarez JI, Castro A, Bhardwaj A. Use of hypertonic
saline/acetate infusion in treatment of cerebral edema in patients
with head trauma: experience at a single center. J Trauma. 1999;
47(4):659-665.
23. Ichai C, Armando G, Orban JC, et al. Sodium lactate versus
mannitol in the treatment of intracranial hypertensive episodes
in severe traumatic brain-injured patients. Intensive Care Med.
2009;35(3):471-479.
24. Francony G, Fauvage B, Falcon D, et al. Equimolar doses of
mannitol and hypertonic saline in the treatment of increased intracranial pressure. Crit Care Med. 2008;36(3):795-800.
25. Battison C, Andrews PJ, Graham C, Petty T. Randomized, controlled trial on the effect of a 20% mannitol solution and a 7.5%
saline/6% dextran solution on increased intracranial pressure after
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
brain injury. Crit Care Med. Jan 2005;33(1):196-202; discussion
257-198.
Harutjunyan L, Holz C, Rieger A, Menzel M, Grond S, Soukup J.
Efficiency of 7.2% hypertonic saline hydroxyethyl starch 200/0.5
versus mannitol 15% in the treatment of increased intracranial
pressure in neurosurgical patients - a randomized clinical trial
[ISRCTN62699180]. Crit Care. Oct 5 2005;9(5):R530-540.
Vialet R, Albanese J, Thomachot L, et al. Isovolume hypertonic
solutes (sodium chloride or mannitol) in the treatment of refractory posttraumatic intracranial hypertension: 2 mL/kg 7.5% saline
is more effective than 2 mL/kg 20% mannitol. Crit Care Med.
2003;31(6):1683-1687.
Kerwin AJ, Schinco MA, Tepas JJ 3rd, Renfro WH, Vitarbo EA,
Muehlberger M. The use of 23.4% hypertonic saline for the
management of elevated intracranial pressure in patients with
severe traumatic brain injury: a pilot study. J Trauma. 2009;
67(2):277-282.
James HE. Methodology for the control of intracranial pressure
with hypertonic mannitol. Acta Neurochir (Wien). 1980;51(3-4):
161-172.
Becker DP. The alleviation of increased intracranial pressure by the
chronic adminitration of osmotic agents. Berlin: Springer; 1972.
Mendelow AD, Teasdale GM, Russell T, Flood J, Patterson J,
Murray GD. Effect of mannitol on cerebral blood flow and cerebral perfusion pressure in human head injury. J Neurosurg. 1985;
63(1):43-48.
Qureshi AI, Suarez JI, Bhardwaj A, et al. Use of hypertonic (3%)
saline/acetate infusion in the treatment of cerebral edema: effect
on intracranial pressure and lateral displacement of the brain. Crit
Care Med. 1998;26(3):440-446.
Horn P, Munch E, Vajkoczy P, et al. Hypertonic saline solution
for control of elevated intracranial pressure in patients with
exhausted response to mannitol and barbiturates. Neurol Res.
1999;21(8):758-764.
Munar F, Ferrer AM, de Nadal M, et al. Cerebral hemodynamic
effects of 7.2% hypertonic saline in patients with head injury and
raised intracranial pressure. J Neurotrauma. 2000;17(1):41-51.
Schatzmann C, Heissler HE, Konig K, et al. Treatment of elevated
intracranial pressure by infusions of 10% saline in severely head
injured patients. Acta Neurochir Suppl. 1998;71:31-33.
White H, Cook D, Venkatesh B. The use of hypertonic saline for
treating intracranial hypertension after traumatic brain injury.
Anesth Analg. 2006;102(6):1836-1846.
Ware ML, Nemani VM, Meeker M, Lee C, Morabito DJ,
Manley GT. Effects of 23.4% sodium chloride solution in reducing intracranial pressure in patients with traumatic brain injury: a
preliminary study. Neurosurgery. 2005;57(4):727-736; ; discussion 727-736.
Oddo M, Levine JM, Frangos S, et al. Effect of mannitol and
hypertonic saline on cerebral oxygenation in patients with severe
traumatic brain injury and refractory intracranial hypertension.
J Neurol Neurosurg Psychiatry. 2009;80(8):916-920.
Baker AJ, Rhind SG, Morrison LJ, et al. Resuscitation with
hypertonic saline-dextran reduces serum biomarker levels and
correlates with outcome in severe traumatic brain injury patients.
J Neurotrauma. 2009;26(8):1227-1240.
Downloaded from jic.sagepub.com by guest on June 30, 2014
10
Journal of Intensive Care Medicine 28(1)
40. Guidelines for the management of severe traumatic brain injury.
J Neurotrauma. 2007;24(suppl 1):S1-S106.
41. Kaufmann AM, Cardoso ER. Aggravation of vasogenic cerebral
edema by multiple-dose mannitol. J Neurosurg. 1992;77(4):584-589.
42. Bereczki D, Mihalka L, Szatmari S, et al. Mannitol use in acute stroke:
case fatality at 30 days and 1 year. Stroke. 2003;34(7):1730-1735.
43. Schwarz S, Schwab S, Bertram M, Aschoff A, Hacke W. Effects
of hypertonic saline hydroxyethyl starch solution and mannitol in
patients with increased intracranial pressure after stroke. Stroke.
1998;29(8):1550-1555.
44. Schwarz S, Georgiadis D, Aschoff A, Schwab S. Effects of hypertonic (10%) saline in patients with raised intracranial pressure
after stroke. Stroke. 2002;33(1):136-140.
45. Bhardwaj A, Harukuni I, Murphy SJ, et al. Hypertonic saline
worsens infarct volume after transient focal ischemia in rats.
Stroke. 2000;31(7):1694-1701.
46. Adams HP Jr, del Zoppo G, Alberts MJ, et al. Guidelines for the
early management of adults with ischemic stroke: a guideline
from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular
Radiology and Intervention Council, and the Atherosclerotic
Peripheral Vascular Disease and Quality of Care Outcomes in
Research Interdisciplinary Working Groups: the American
Academy of Neurology affirms the value of this guideline as an
educational tool for neurologists. Stroke. 2007;38(5):1655-1711.
47. Bermueller C, Thal SC, Plesnila N, Schmid-Elsaesser R, Kreimeier U,
Zausinger S. Hypertonic fluid resuscitation from subarachnoid
hemorrhage in rats: a comparison between small volume resuscitation and mannitol. J Neurol Sci. Feb 15 2006;241(1-2):73-82.
48. Zausinger S, Thal SC, Kreimeier U, Messmer K, SchmidElsaesser R. Hypertonic fluid resuscitation from subarachnoid
hemorrhage in rats. Neurosurgery. 2004;55(3):679-686; discussion
686-677.
49. Bentsen G, Breivik H, Lundar T, Stubhaug A. Hypertonic saline
(7.2%) in 6% hydroxyethyl starch reduces intracranial pressure
and improves hemodynamics in a placebo-controlled study
involving stable patients with subarachnoid hemorrhage. Crit
Care Med. 2006;34(12):2912-2917.
50. Tseng MY, Al-Rawi PG, Czosnyka M, et al. Enhancement of
cerebral blood flow using systemic hypertonic saline therapy
improves outcome in patients with poor-grade spontaneous subarachnoid hemorrhage. J Neurosurg. 2007;107(2):274-282.
51. Misra UK, Kalita J, Ranjan P, Mandal SK. Mannitol in intracerebral hemorrhage: a randomized controlled study. J Neurol Sci.
15 2005;234(1-2):41-45.
52. Kalita J, Misra UK, Ranjan P, Pradhan PK, Das BK. Effect of
mannitol on regional cerebral blood flow in patients with intracerebral hemorrhage. J Neurol Sci. 15, 2004;224(1-2):19-22.
53. Qureshi AI, Wilson DA, Traystman RJ. Treatment of transtentorial herniation unresponsive to hyperventilation using hypertonic
saline in dogs: effect on cerebral blood flow and metabolism.
J Neurosurg Anesthesiol. 2002;14(1):22-30.
54. Qureshi AI, Wilson DA, Traystman RJ. Treatment of elevated
intracranial pressure in experimental intracerebral hemorrhage:
comparison between mannitol and hypertonic saline. Neurosurgery.
1999;44(5):1055-1063; ; discussion 1063-1054.
55. Jalan R. Pathophysiological basis of therapy of raised intracranial
pressure in acute liver failure. Neurochem Int. 2005;47(1-2):78-83.
56. Blei AT. The pathophysiology of brain edema in acute liver
failure. Neurochem Int. 2005;47(1-2):71-77.
57. Canalese J, Gimson AE, Davis C, Mellon PJ, Davis M, Williams R.
Controlled trial of dexamethasone and mannitol for the cerebral
oedema of fulminant hepatic failure. Gut. 1982;23(7):625-629.
58. Murphy N, Auzinger G, Bernel W, Wendon J. The effect of
hypertonic sodium chloride on intracranial pressure in patients
with acute liver failure. Hepatology. 2004;39(2):464-470.
59. Qureshi AI, Geocadin RG, Suarez JI, Ulatowski JA. Long-term
outcome after medical reversal of transtentorial herniation in
patients with supratentorial mass lesions. Crit Care Med. 2000;
28(5):1556-1564.
60. Koenig MA, Bryan M, Lewin JL, 3rd, Mirski MA, Geocadin RG,
Stevens RD. Reversal of transtentorial herniation with hypertonic
saline. Neurology. 25 2008;70(13):1023-1029.
61. Rosner MH, Ronco C. Dysnatremias in the intensive care unit.
Contrib Nephrol. 2010;165:292-298.
62. Diringer MN, Zazulia AR. Osmotic therapy: fact and fiction.
Neurocrit Care. 2004;1(2):219-233.
63. Becker D, Vries J. The Alleviation of Increased Intracranial
Pressure by the Chronic Administration of Osmotic Agents.
New York: Springer; 1972.
64. Aiyagari V, Deibert E, Diringer MN. Hypernatremia in the neurologic intensive care unit: how high is too high? J Crit Care. 2006;
21(2):163-172.
65. Cloyd JC, Snyder BD, Cleeremans B, Bundlie SR,
Blomquist CH, Lakatua DJ. Mannitol pharmacokinetics and
serum osmolality in dogs and humans. J Pharmacol Exp Ther.
1986;236(2):301-306.
66. Garcia-Morales EJ, Cariappa R, Parvin CA, Scott MG,
Diringer MN. Osmole gap in neurologic-neurosurgical intensive care unit: Its normal value, calculation, and relationship
with mannitol serum concentrations. Crit Care Med. 2004;32(4):
986-991.
67. Rabetoy GM, Fredericks MR, Hostettler CF. Where the kidney is
concerned, how much mannitol is too much? Ann Pharmacother.
1993;27(1):25-28.
68. Temes SP, Lilien OM, Chamberlain W. A direct vasoconstrictor
effect of mannitol on the renal artery. Surg Gynecol Obstet.
1975;141(2):223-226.
69. Whelan TV, Bacon ME, Madden M, Patel TG, Handy R. Acute
renal failure associated with mannitol intoxication. Report of a
case. Arch Intern Med. 1984;144(10):2053-2055.
70. Dorman HR, Sondheimer JH, Cadnapaphornchai P. Mannitolinduced acute renal failure. Medicine (Baltimore). 1990;69(3):
153-159.
71. Huang PP, Stucky FS, Dimick AR, Treat RC, Bessey PQ,
Rue LW. Hypertonic sodium resuscitation is associated with renal
failure and death. Ann Surg. 1995;221(5):543-554; ; discussion
554-547.
72. Khanna S, Davis D, Peterson B, et al. Use of hypertonic saline in
the treatment of severe refractory posttraumatic intracranial
hypertension in pediatric traumatic brain injury. Crit Care Med.
2000;28(4):1144-1151.
Downloaded from jic.sagepub.com by guest on June 30, 2014
Hinson et al
11
73. Peterson B, Khanna S, Fisher B, Marshall L. Prolonged hypernatremia controls elevated intracranial pressure in head-injured
pediatric patients. Crit Care Med. 2000;28(4):1136-1143.
74. Kraus MA. Selection of dialysate and replacement fluids and
management of electrolyte and Acid-base disturbances. Semin
Dial. Mar-2009;22(2):137-140.
75. Nau R. Osmotherapy for elevated intracranial pressure: a critical
reappraisal. Clin Pharmacokinet. 2000;38(1):23-40.
76. Forsyth LL, Liu-DeRyke X, Parker D Jr, Rhoney DH. Role of
hypertonic saline for the management of intracranial hypertension
after stroke and traumatic brain injury. Pharmacotherapy. 2008;
28(4):469-484.
Downloaded from jic.sagepub.com by guest on June 30, 2014
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Why-Most Investors Are Mostly Wrong Most of The TimeDokument3 SeitenWhy-Most Investors Are Mostly Wrong Most of The TimeBharat SahniNoch keine Bewertungen
- Theology and Pipe Smoking - 7pDokument7 SeitenTheology and Pipe Smoking - 7pNeimar HahmeierNoch keine Bewertungen
- Disorders of NewbornDokument4 SeitenDisorders of NewbornBRUELIN MELSHIA MNoch keine Bewertungen
- Edir AdminDokument916 SeitenEdir AdminSELIMNoch keine Bewertungen
- Feb 1 - ScottDokument17 SeitenFeb 1 - ScottNyannnNoch keine Bewertungen
- NIPMR Notification v3Dokument3 SeitenNIPMR Notification v3maneeshaNoch keine Bewertungen
- Erythrocyte Sedimentation RateDokument16 SeitenErythrocyte Sedimentation Rateapi-3823785100% (2)
- Fault Detection of Gear Using Spectrum and CepstruDokument6 SeitenFault Detection of Gear Using Spectrum and Cepstruराकेश झाNoch keine Bewertungen
- 150 Years of PharmacovigilanceDokument2 Seiten150 Years of PharmacovigilanceCarlos José Lacava Fernández100% (1)
- MInor To ContractsDokument28 SeitenMInor To ContractsDakshita DubeyNoch keine Bewertungen
- SKI Report2008 - 50 2Dokument46 SeitenSKI Report2008 - 50 2nada safitriNoch keine Bewertungen
- An Improved Version of The Skin Chapter of Kent RepertoryDokument6 SeitenAn Improved Version of The Skin Chapter of Kent RepertoryHomoeopathic PulseNoch keine Bewertungen
- World of Warcraft 5e RPG Core DocumentDokument152 SeitenWorld of Warcraft 5e RPG Core DocumentHugo Moreno100% (1)
- Autobiography of A 2nd Generation Filipino-AmericanDokument4 SeitenAutobiography of A 2nd Generation Filipino-AmericanAio Min100% (1)
- Neuromarketing EssayDokument3 SeitenNeuromarketing Essayjorge jmzNoch keine Bewertungen
- Elementary Linear Algebra Applications Version 11th Edition Anton Solutions ManualDokument36 SeitenElementary Linear Algebra Applications Version 11th Edition Anton Solutions Manualpearltucker71uej95% (22)
- They Cried MonsterDokument13 SeitenThey Cried MonstermassuroNoch keine Bewertungen
- The Students Ovid Selections From The Metamorphoses by Ovid, Margaret Worsham MusgroveDokument425 SeitenThe Students Ovid Selections From The Metamorphoses by Ovid, Margaret Worsham MusgroveMiriaam AguirreNoch keine Bewertungen
- Chapter 3 SIP MethodologyDokument43 SeitenChapter 3 SIP MethodologyMáxyne NalúalNoch keine Bewertungen
- Acc 106 Ebook Answer Topic 4Dokument13 SeitenAcc 106 Ebook Answer Topic 4syifa azhari 3BaNoch keine Bewertungen
- Dwnload Full Conceptual Physics 12th Edition Hewitt Test Bank PDFDokument36 SeitenDwnload Full Conceptual Physics 12th Edition Hewitt Test Bank PDFscreamsoaring.pm7hcv100% (13)
- Book Review Leffel Cateura, Oil Painting SecretsDokument4 SeitenBook Review Leffel Cateura, Oil Painting SecretsAnonymous H3kGwRFiENoch keine Bewertungen
- Final BasantDokument22 SeitenFinal BasantMuqaddas IsrarNoch keine Bewertungen
- Chargezoom Achieves PCI-DSS ComplianceDokument2 SeitenChargezoom Achieves PCI-DSS CompliancePR.comNoch keine Bewertungen
- Stephen Law Morality Without GodDokument9 SeitenStephen Law Morality Without GodJiReH MeCuaNoch keine Bewertungen
- Rainfall Runoff ModellingDokument23 SeitenRainfall Runoff ModellingmansikakaniNoch keine Bewertungen
- CRM Project (Oyo)Dokument16 SeitenCRM Project (Oyo)Meenakshi AgrawalNoch keine Bewertungen
- Early Pregnancy and Its Effect On The Mental Health of Students in Victoria Laguna"Dokument14 SeitenEarly Pregnancy and Its Effect On The Mental Health of Students in Victoria Laguna"Gina HerraduraNoch keine Bewertungen
- Elements of Visual Design in The Landscape - 26.11.22Dokument15 SeitenElements of Visual Design in The Landscape - 26.11.22Delnard OnchwatiNoch keine Bewertungen
- The Impact of Video Gaming To The Academic Performance of The Psychology Students in San Beda UniversityDokument5 SeitenThe Impact of Video Gaming To The Academic Performance of The Psychology Students in San Beda UniversityMarky Laury GameplaysNoch keine Bewertungen