Beruflich Dokumente
Kultur Dokumente
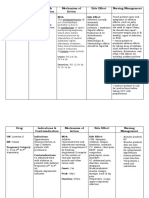
Bleomycin drug information and nursing considerations
Hochgeladen von
Vin BitzOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Bleomycin drug information and nursing considerations
Hochgeladen von
Vin BitzCopyright:
Verfügbare Formate
Name /bks_53161_deglins_md_disk/bleomycin
02/19/2014 09:11AM
High Alert
bleomycin (blee-oh-mye-sin)
Blenoxane
Classification
Therapeutic: antineoplastics
Pharmacologic: antitumor antibiotics
Pregnancy Category D
Plate # 0-Composite
pg 1 # 1
Adverse Reactions/Side Effects
CNS: aggressive behavior, disorientation, weakness. Resp: PULMONARY FIBROSIS,
pneumonitis. CV: hypotension, peripheral vasoconstriction. GI: anorexia, nausea,
stomatitis, vomiting. Derm: hyperpigmentation, mucocutaneous toxicity, alopecia,
erythema, rashes, urticaria, vesiculation. Hemat: anemia, leukopenia, thrombocytopenia. Local: pain at tumor site, phlebitis at IV site. Metab: weight loss. Misc:
ANAPHYLACTOID REACTIONS, chills, fever.
Interactions
Drug-Drug: Hematologic toxicityqwith concurrent use of radiation therapy
Treatment of: Lymphomas, Squamous cell carcinoma, Testicular embryonal cell carcinoma, Choriocarcinoma, Teratocarcinoma. Intrapleural administration to prevent
the reaccumulation of malignant effusions.
and other antineoplastics. Concurrent use with cisplatinpelimination of bleomycin and mayqtoxicity.qrisk of pulmonary toxicity with other antineoplastics or
thoracic radiation therapy. General anesthesiaqthe risk of pulmonary toxicity.
qrisk of Raynauds phenomenon when used with vinblastine.
Action
Route/Dosage
Indications
Inhibits DNA and RNA synthesis. Therapeutic Effects: Death of rapidly replicating
cells, particularly malignant ones.
Pharmacokinetics
Absorption: Well absorbed from IM and subcut sites. Absorption follows intrapleural and intraperitoneal administration.
Distribution: Widely distributed, concentrates in skin, lungs, peritoneum, kidneys, and lymphatics.
Metabolism and Excretion: 60 70% excreted unchanged by the kidneys.
Half-life: 2 hr (qin renal impairment).
TIME/ACTION PROFILE (tumor response)
ROUTE
ONSET
PEAK
DURATION
IV, IM, Subcut
23 wk
unknown
unknown
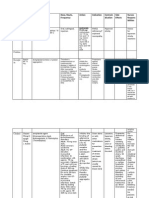
Contraindications/Precautions
Contraindicated in: Hypersensitivity; OB, Lactation: Potential for fetal, infant
harm.
Use Cautiously in: Renal impairment (doseprequired if CCr 35 mL/min); Pulmonary impairment; Nonmalignant chronic debilitating illness; Patients with childbearing potential; Geri:qrisk of pulmonary toxicity and reduction in renal function.
Canadian drug name.
Genetic Implication.
Lymphoma patients should receive initial test doses of 2 units or less for the first 2
doses.
IV, IM, Subcut (Adults and Children): 0.25 0.5 unit/kg (10 20 units/m2)
weekly or twice weekly initially. If favorable response, lower maintenance doses given
(1 unit/day or 5 units/wk IM or IV). May also be given as continuous IV infusion at
0.25 unit/kg or 15 units/m2/day for 4 5 days.
Intrapleural (Adults): 15 20 units instilled for 4 hr, then removed.
NURSING IMPLICATIONS
Assessment
Monitor vital signs before and frequently during therapy.
Assess for fever and chills. May occur 3 6 hr after administration and last 4 12
hr.
Monitor for anaphylactic (fever, chills, hypotension, wheezing) and idi-
osyncratic (confusion, hypotension, fever, chills, wheezing) reactions.
Keep resuscitation equipment and medications on hand. Lymphoma patients are
at particular risk for idiosyncratic reactions that may occur immediately or several
hours after therapy, usually after the first or second dose.
Assess respiratory status for dyspnea and rales/crackles. Monitor chest
x-ray before and periodically during therapy. Pulmonary toxicity occurs
primarily in geriatric patients (age 70 or older) who have received 400
CAPITALS indicate life-threatening, underlines indicate most frequent.
Strikethrough Discontinued.
PDF Page #1
Name /bks_53161_deglins_md_disk/bleomycin
02/19/2014 09:11AM
or more units or at lower doses in patients who received other antineoplastics or thoracic radiation. May occur 4 10 wk after therapy. Discontinue and do not resume bleomycin if pulmonary toxicity occurs.
Assess nausea, vomiting, and appetite. Weigh weekly. Modify diet as tolerated. Antiemetics may be given before administration.
Lab Test Considerations: Monitor CBC before and periodically during
therapy. May cause thrombocytopenia and leukopenia (nadir occurs in
12 days and usually returns to pretreatment levels by day 17).
Monitor baseline and periodic renal and hepatic function.
Potential Nursing Diagnoses
Risk for injury (Side Effects)
Disturbed body image (Side Effects)
Implementation
High Alert: Fatalities have occurred with chemotherapeutic agents. Before ad-
pg 2 # 2
Y-Site Compatibility: allopurinol, amifostine, aminocaproic acid, aminophyl-
Plate # 0-Composite
ministering, clarify all ambiguous orders; double-check single, daily, and courseof-therapy dose limits; have second practitioner independently double-check
original order and dose calculations.
Prepare solution in a biologic cabinet. Wear gloves, gown, and mask while handling medication. Discard equipment in specially designated containers.
Lymphoma patients should receive a 1- or 2-unit test dose 2 4 hr before initiation
of therapy. Monitor closely for anaphylactic reaction. May not detect reactors.
Premedication with acetaminophen, corticosteroids, and diphenhydramine may
reduce drug fever and risk of anaphylaxis.
Reconstituted solution is stable for 24 hr at room temperature and for 14 days if
refrigerated.
IM, Subcut: Reconstitute vial with 1 5 mL of sterile water for injection, 0.9%
NaCl, or bacteriostatic water for injection. Do not reconstitute with diluents containing benzyl alcohol when used for neonates.
IV Administration
pH: 4.0 6.0.
Intermittent Infusion: Prepare IV doses by diluting 15-unit vial with at least 5
mL of 0.9% NaCl. Diluent: Further dilute dose in 50 to 1000 mL of D5W or 0.9%
NaCl. Rate: Administer slowly over 10 min.
line, amiodarone, anidulafungin, atracurium, aztreonam, bivalirudin, bumetanide, busulfan, calcium chloride, calcium gluconate, carboplatin, carmustine,
caspofungin, cefepime, chlorpromazine, cimetidine, cisatracurium, cisplatin, codeine, cyclophosphamide, cyclosporine, cytarabine, dacarbazine, dactinomycin,
daptomycin, daunorubicin, dexamethasone, dexmedetomidine, dexrazoxane, digoxin, diltiazem, diphenhydramine, dobutamine, docetaxel, dopamine, doxacurium, doxorubicin, doxorubicin liposome, droperidol, enalaprilat, epinephrine,
epirubicin, ertapenem, esmolol, etoposide, etoposide phosphate, famotidine, fenoldopam, filgrastim, fludarabine, fluorouracil, fospehnytoin, furosemide, gemcitabine, glycopyrrolate, granisetron, haloperidol, heparin, hetastarch, hydralazine,
hydrocortisone, idarubicin, ifosfamide, insulin, isoproterenol, ketorolac, labetalol, leucovorin calcium, levofloxacin, lidocaine, magnesium sulfate, mannitol,
mechlorethamine, melphalan, meperidine, mesna, metaraminol, methotrexate,
methyldopate, methylprednisolone, metoclopramide, metoprolol, milrinone, mitomycin, mitoxantrone, naloxone, nesiritide, nicardipine, nitroglycerin, norepinephrine, octreotide, ondansetron, oxaliplatin, paclitaxel, palonosetron, pancuronium, pantoprazole, pemetrexed, phentolamine, phenylephrine, piperacillin/
tazobactam, potassium chloride, potassium phosphates, procainamide, quinupristin/dalfopristin, rituximab, sargramostim, sodium acetate, teniposide, thiotepa, tirofiban, trastuzumab, vinblastine, vincristine, vinorelbine, voriconazole.
Y-Site Incompatibility: amphotericin B liposome, dantrolene, phenytoin, tigecycline.
Intrapleural: Dissolve 60 units in 50 100 mL of 0.9% NaCl.
May be administered through thoracotomy tube. Position patient as directed.
Patient/Family Teaching
Instruct patient to notify health care professional if fever, chills, wheezing, faint-
ness, diaphoresis, shortness of breath, prolonged nausea and vomiting, or mouth
sores occur.
Encourage patient not to smoke because this may worsen pulmonary
toxicity.
Explain to the patient that skin toxicity may manifest itself as skin sensitivity, hyperpigmentation (especially at skin folds and points of skin irritation), and skin
rashes and thickening.
Instruct patient to inspect oral mucosa for erythema and ulceration. If ulceration
occurs, advise patient to use sponge brush and rinse mouth with water after eating
and drinking. Opioid analgesics may be required if pain interferes with eating.
2015 F.A. Davis Company
CONTINUED
PDF Page #2
Name /bks_53161_deglins_md_disk/bleomycin
02/19/2014 09:11AM
Plate # 0-Composite
pg 3 # 3
3
PDF Page #3
CONTINUED
bleomycin
Discuss with patient the possibility of hair loss. Explore coping strategies.
Advise patient of the need for contraception during therapy.
Instruct patient not to receive any vaccinations without advice of health care pro-
fessional.
Emphasize need for periodic lab tests to monitor for side effects.
Evaluation/Desired Outcomes
Decrease in tumor size without evidence of hypersensitivity or pulmonary toxicity.
Why was this drug prescribed for your patient?
Canadian drug name.
Genetic Implication.
CAPITALS indicate life-threatening, underlines indicate most frequent.
Strikethrough Discontinued.
Das könnte Ihnen auch gefallen
- JSA-070 Desert Road TripDokument4 SeitenJSA-070 Desert Road TripMoaatazz NouisriNoch keine Bewertungen
- Immunization RecordDokument4 SeitenImmunization RecordVin BitzNoch keine Bewertungen
- Nccaom Biomed Exam ContentDokument12 SeitenNccaom Biomed Exam Contentapi-251021152Noch keine Bewertungen
- Annex B-1 RR 11-2018 Sworn Statement of Declaration of Gross Sales and ReceiptsDokument1 SeiteAnnex B-1 RR 11-2018 Sworn Statement of Declaration of Gross Sales and ReceiptsEliza Corpuz Gadon89% (19)
- How To Prevent Diabetes - A Guide For Those With PrediabetesDokument26 SeitenHow To Prevent Diabetes - A Guide For Those With PrediabetesDiabetes CareNoch keine Bewertungen
- Exceptions To Right of Access To InformationDokument226 SeitenExceptions To Right of Access To Informationrosalie santa florentinNoch keine Bewertungen
- Statics and Strength of Materials For Architecture and Building Construction 4th Edition Onouye Solutions ManualDokument25 SeitenStatics and Strength of Materials For Architecture and Building Construction 4th Edition Onouye Solutions ManualRobertElliottrbgq96% (26)
- Hair and Health Lifestyle ManualDokument39 SeitenHair and Health Lifestyle Manualmenna hassanNoch keine Bewertungen
- Province of Negros OrientalDokument4 SeitenProvince of Negros OrientalVin BitzNoch keine Bewertungen
- K4y Final EvaluationDokument9 SeitenK4y Final Evaluationapi-3153554060% (1)
- Drug study on chemotherapeutic alkylating agentsDokument16 SeitenDrug study on chemotherapeutic alkylating agentsPrincess CruzNoch keine Bewertungen
- Cefoperazone and Sulbactum Combination Therapy GuideDokument3 SeitenCefoperazone and Sulbactum Combination Therapy Guideiloveit52252Noch keine Bewertungen
- Pilocarpine (Drug Monograph)Dokument1 SeitePilocarpine (Drug Monograph)Muhammad ArsalanNoch keine Bewertungen
- Filgrastim Boosts Neutrophil Recovery After ChemotherapyDokument3 SeitenFilgrastim Boosts Neutrophil Recovery After ChemotherapyKyla Barrera TabungarNoch keine Bewertungen
- Complete Albendazole Information From DrugsDokument4 SeitenComplete Albendazole Information From DrugselephantynoseNoch keine Bewertungen
- Fludrocortisone (Florinef)Dokument17 SeitenFludrocortisone (Florinef)passer byNoch keine Bewertungen
- Generic Name: Mebeverine Hydrochloride Mechanism of Action Side Effects/ Adverse Reaction Nursing Responsibility Assessment & Drug EffectsDokument4 SeitenGeneric Name: Mebeverine Hydrochloride Mechanism of Action Side Effects/ Adverse Reaction Nursing Responsibility Assessment & Drug EffectsNiziu BearsNoch keine Bewertungen
- Drug Study OrthoDokument4 SeitenDrug Study OrthoJhessa Curie Pitagan100% (1)
- Alprazolam BiperidinDokument6 SeitenAlprazolam BiperidinFionah RetuyaNoch keine Bewertungen
- Mesoridazine Drug StudyDokument5 SeitenMesoridazine Drug Studyshadow gonzalezNoch keine Bewertungen
- Methyldopa nursing management for hypertensionDokument4 SeitenMethyldopa nursing management for hypertensionRico Mae ValenciaNoch keine Bewertungen
- Managing dextrose therapyDokument2 SeitenManaging dextrose therapySanket TelangNoch keine Bewertungen
- Drug Study - BaclofenDokument5 SeitenDrug Study - BaclofenRocco WalksNoch keine Bewertungen
- Ofloxacin Drug StudyDokument4 SeitenOfloxacin Drug StudyMikko Anthony Pingol Alarcon100% (1)
- Azithromycin Nursing ConsiderationsDokument2 SeitenAzithromycin Nursing ConsiderationsKristine YoungNoch keine Bewertungen
- Name: Micaela Andrea C. Cielo Date: Year & Section: BS Nursing 2A Drug Study: AlbendazoleDokument2 SeitenName: Micaela Andrea C. Cielo Date: Year & Section: BS Nursing 2A Drug Study: AlbendazoleMicaela Andrea CieloNoch keine Bewertungen
- Obat ObgynDokument8 SeitenObat ObgynMuhammad Naqiuddin JalaluddinNoch keine Bewertungen
- Vii. Drug Study Drug Mechanism of ActionDokument7 SeitenVii. Drug Study Drug Mechanism of ActionRifa'atul MahmudahNoch keine Bewertungen
- DS (Calcium + Vit. D)Dokument6 SeitenDS (Calcium + Vit. D)Mary April MendezNoch keine Bewertungen
- Drug Study - LevothyroxineDokument1 SeiteDrug Study - LevothyroxineCarla Tongson MaravillaNoch keine Bewertungen
- Case Pre Drug StudyDokument5 SeitenCase Pre Drug StudyJoule PeirreNoch keine Bewertungen
- Drug Study Ceftriaxone SodiumDokument3 SeitenDrug Study Ceftriaxone SodiumPrincess Queenie OlarteNoch keine Bewertungen
- Dolo 650 MG (Paracetamol) : Uses, Side Effects, DosageDokument3 SeitenDolo 650 MG (Paracetamol) : Uses, Side Effects, DosageRaluca Elena Raluca ElenaNoch keine Bewertungen
- Insulin Mechanism of Action and Nursing ResponsibilitiesDokument7 SeitenInsulin Mechanism of Action and Nursing ResponsibilitiesGrape JuiceNoch keine Bewertungen
- Cyclobenzaprine Hydrochloride (Drug Study)Dokument1 SeiteCyclobenzaprine Hydrochloride (Drug Study)Franz.thenurse6888Noch keine Bewertungen
- Epirubicin 10Dokument1 SeiteEpirubicin 10PdianghunNoch keine Bewertungen
- BNP (C)Dokument2 SeitenBNP (C)Mae Ann Bueno CastillonNoch keine Bewertungen
- MisoprostolDokument3 SeitenMisoprostolMichael Aditya LesmanaNoch keine Bewertungen
- MSU-IIT Student Drug Study on TygacilDokument2 SeitenMSU-IIT Student Drug Study on TygacilVanessa Egao100% (1)
- Quinine anti-malarial drugDokument3 SeitenQuinine anti-malarial drugDoubleHeartedNoch keine Bewertungen
- CoversylDokument3 SeitenCoversylianecunarNoch keine Bewertungen
- Furosemid Citicoline Clexane, LevofloxacinDokument9 SeitenFurosemid Citicoline Clexane, Levofloxacincotyboy50% (2)
- Atropine SulfateDokument1 SeiteAtropine SulfateTrishaaMayolNoch keine Bewertungen
- Isoprenaline Infusion 2016Dokument3 SeitenIsoprenaline Infusion 2016Glory Claudia KarundengNoch keine Bewertungen
- Clotrimazole skin infection cream guideDokument2 SeitenClotrimazole skin infection cream guideshajahanputhusseriNoch keine Bewertungen
- Urokinase Dosage WheelDokument2 SeitenUrokinase Dosage WheelNidhiNoch keine Bewertungen
- DUPHASTON Drug StudyDokument6 SeitenDUPHASTON Drug StudyAngela ReyesNoch keine Bewertungen
- Drug Study: NCM 106 Pharmacology: Patient MonitoringDokument2 SeitenDrug Study: NCM 106 Pharmacology: Patient Monitoringpoleene de leonNoch keine Bewertungen
- DrugsDokument10 SeitenDrugsRebecca JolieNoch keine Bewertungen
- PethidineDokument9 SeitenPethidineAnonymous VZtcCECtNoch keine Bewertungen
- Drug Study on CelecoxibDokument11 SeitenDrug Study on CelecoxibPrincess Brigitte R. PATE�ANoch keine Bewertungen
- Glipizide Glucotrol XL Drug CardDokument1 SeiteGlipizide Glucotrol XL Drug CardSheri490Noch keine Bewertungen
- Phenobarbitone InjectionDokument13 SeitenPhenobarbitone InjectionBrian HarrisNoch keine Bewertungen
- Drug Study Quinine SulfateDokument7 SeitenDrug Study Quinine SulfateKathlyn_Matic_6376Noch keine Bewertungen
- Drug Study - CefradoxilDokument13 SeitenDrug Study - CefradoxilJohara G'naid0% (1)
- Indications and Usage: M M M M M M M M M M MDokument4 SeitenIndications and Usage: M M M M M M M M M M MJesthony Lee CorderoNoch keine Bewertungen
- Stugeron® TabletsDokument3 SeitenStugeron® TabletsmahgadNoch keine Bewertungen
- AldactoneDokument2 SeitenAldactoneianecunarNoch keine Bewertungen
- Depot-Ped: 3 Months: 11.25 MG or 30 MG Q12weeks. (SQ) Lupron: Children: Initially, 50Dokument3 SeitenDepot-Ped: 3 Months: 11.25 MG or 30 MG Q12weeks. (SQ) Lupron: Children: Initially, 50thuey epeNoch keine Bewertungen
- Drug StudyDokument32 SeitenDrug StudyKeepItSecretNoch keine Bewertungen
- Lyrica (Pregabalin)Dokument2 SeitenLyrica (Pregabalin)Laromac RolandNoch keine Bewertungen
- DRug Study PhenytoinDokument1 SeiteDRug Study Phenytoinmichelle marquezNoch keine Bewertungen
- Generic Name: Acute Aspirin ToxicityDokument1 SeiteGeneric Name: Acute Aspirin ToxicityShermayne Mallapre HernandezNoch keine Bewertungen
- DesyrelDokument1 SeiteDesyrelKatie McPeekNoch keine Bewertungen
- CefotaximeDokument3 SeitenCefotaximeMargotNoch keine Bewertungen
- Medications Sheet PreopDokument37 SeitenMedications Sheet Preopapi-503879428Noch keine Bewertungen
- EtoposideDokument3 SeitenEtoposideNoamiNoch keine Bewertungen
- Drug Study Clindamycin, Ipatropium BromideDokument8 SeitenDrug Study Clindamycin, Ipatropium Bromidepaupaulala100% (2)
- Drug StudyDokument6 SeitenDrug StudyFloramae Celine BosqueNoch keine Bewertungen
- Enzaza PDFDokument169 SeitenEnzaza PDFChrezavelle MoonNoch keine Bewertungen
- REGISTRY: OHA-Approved Cultural Competence Continuing Education Trainings (8/20/21 Update)Dokument4 SeitenREGISTRY: OHA-Approved Cultural Competence Continuing Education Trainings (8/20/21 Update)Vin BitzNoch keine Bewertungen
- DBM Circular 04-2013 on Payment of Honoraria to GPPB TrainersDokument1 SeiteDBM Circular 04-2013 on Payment of Honoraria to GPPB TrainersVin BitzNoch keine Bewertungen
- Quality Coverage When You Need It Most: Critical Illness InsuranceDokument8 SeitenQuality Coverage When You Need It Most: Critical Illness InsuranceVin BitzNoch keine Bewertungen
- Instruction To Install Lightroom Mobile PresetsDokument4 SeitenInstruction To Install Lightroom Mobile PresetsVin BitzNoch keine Bewertungen
- AspDokument3 SeitenAspVin BitzNoch keine Bewertungen
- Knowledge, Attitude, and Practice Regarding Sterilization Among Health-Care Staff in A Tertiary Hospital of Western IndiaDokument6 SeitenKnowledge, Attitude, and Practice Regarding Sterilization Among Health-Care Staff in A Tertiary Hospital of Western IndiaVin BitzNoch keine Bewertungen
- Philippines hospital room use policyDokument1 SeitePhilippines hospital room use policyVin BitzNoch keine Bewertungen
- Registered Nurse or LPN Endorsement Licensure RequirementsDokument4 SeitenRegistered Nurse or LPN Endorsement Licensure RequirementsVin BitzNoch keine Bewertungen
- Make It Your Mission: To Heal and Care For VeteransDokument12 SeitenMake It Your Mission: To Heal and Care For VeteransVin BitzNoch keine Bewertungen
- 5b - Controlling CDI Park Nicollet Methodist Hospital Hand Hygiene Auditing ToolDokument2 Seiten5b - Controlling CDI Park Nicollet Methodist Hospital Hand Hygiene Auditing ToolVin BitzNoch keine Bewertungen
- 5 Nursing Services Scheduling PolicyDokument7 Seiten5 Nursing Services Scheduling PolicyVin BitzNoch keine Bewertungen
- Ams DiagnosisDokument19 SeitenAms DiagnosisVin BitzNoch keine Bewertungen
- Noph Nursing Service Organization Strategic PlanDokument5 SeitenNoph Nursing Service Organization Strategic PlanVin BitzNoch keine Bewertungen
- 18 2012 PDFDokument3 Seiten18 2012 PDFrainNoch keine Bewertungen
- 4.early Detection of Maternal Deterioration 1 PDFDokument13 Seiten4.early Detection of Maternal Deterioration 1 PDFVin BitzNoch keine Bewertungen
- Standards Nursing of CareDokument7 SeitenStandards Nursing of CareVin BitzNoch keine Bewertungen
- DBM Circular 04-2013 on Payment of Honoraria to GPPB TrainersDokument1 SeiteDBM Circular 04-2013 on Payment of Honoraria to GPPB TrainersVin BitzNoch keine Bewertungen
- Noph Personnel Assignment RecordDokument1 SeiteNoph Personnel Assignment RecordVin BitzNoch keine Bewertungen
- The Application of John Dewey S ProgressDokument37 SeitenThe Application of John Dewey S ProgressVin BitzNoch keine Bewertungen
- EssentialismDokument7 SeitenEssentialismVin BitzNoch keine Bewertungen
- Personnel Ward Rotation Record for Negros Oriental Provincial HospitalDokument1 SeitePersonnel Ward Rotation Record for Negros Oriental Provincial HospitalVin BitzNoch keine Bewertungen
- WI Medication AdministrationDokument11 SeitenWI Medication AdministrationVin BitzNoch keine Bewertungen
- NSO SUP Checklist3Dokument3 SeitenNSO SUP Checklist3Vin BitzNoch keine Bewertungen
- The Role of The Supervisor in Managing AbsenteeismDokument5 SeitenThe Role of The Supervisor in Managing AbsenteeismVin BitzNoch keine Bewertungen
- Chapter 1 ResearchDokument17 SeitenChapter 1 ResearchVin BitzNoch keine Bewertungen
- EuthanasiaDokument14 SeitenEuthanasiaVin BitzNoch keine Bewertungen
- Viral Exanthems and EnanthemsDokument2 SeitenViral Exanthems and Enanthemsclark146Noch keine Bewertungen
- Vitamin C. USAGE, FUNCTIONDokument20 SeitenVitamin C. USAGE, FUNCTIONANURAG ALOKNoch keine Bewertungen
- Nature's Role in Reducing Mental FatigueDokument9 SeitenNature's Role in Reducing Mental FatigueCrăciun RalucaNoch keine Bewertungen
- EfAD BenchmarkJune2005 UKDokument55 SeitenEfAD BenchmarkJune2005 UKCristina Dobrin ClaudiaNoch keine Bewertungen
- 2014 12 04 Memoria Imim 2013Dokument310 Seiten2014 12 04 Memoria Imim 2013michorizoNoch keine Bewertungen
- 1104 Marshall RobertDokument37 Seiten1104 Marshall RobertAris TsangaridesNoch keine Bewertungen
- Medical AnthropologyDokument5 SeitenMedical AnthropologyAnanya ShresthaNoch keine Bewertungen
- City of Dayton Board of Zoning Appeals Staff ReportDokument36 SeitenCity of Dayton Board of Zoning Appeals Staff ReportChelsea ElizabethNoch keine Bewertungen
- Disciplines and Ideas in CounselingDokument36 SeitenDisciplines and Ideas in CounselingMarianne Sy-Quimsiam Ignacio100% (2)
- Global ContextsDokument14 SeitenGlobal Contextsapi-279222151Noch keine Bewertungen
- BP Environmental CleaningDokument250 SeitenBP Environmental CleaningFaruque SathiNoch keine Bewertungen
- Anatomy Physiology ReproductionDokument12 SeitenAnatomy Physiology ReproductionHERALD LISINGNoch keine Bewertungen
- Problem Statement WORLD Cancer Afflicts All Communities WorldwideDokument30 SeitenProblem Statement WORLD Cancer Afflicts All Communities Worldwidesalma0430100% (2)
- 2 - Determinants of Acute Malnutrition Among Children Aged 6-59 Months Visiting Public Health Facilities in Gambella Town, Southwest Ethiopia Unmatched Case-Control StudyDokument10 Seiten2 - Determinants of Acute Malnutrition Among Children Aged 6-59 Months Visiting Public Health Facilities in Gambella Town, Southwest Ethiopia Unmatched Case-Control StudyRezki Purnama YusufNoch keine Bewertungen
- Performance Task Unit PlanDokument10 SeitenPerformance Task Unit Planapi-314719374Noch keine Bewertungen
- CHN 2 Session 1 SASDokument6 SeitenCHN 2 Session 1 SASrica sebabillonesNoch keine Bewertungen
- Stress Reduction ActivityDokument4 SeitenStress Reduction ActivityBramwel Muse (Gazgan bram)Noch keine Bewertungen
- Measuring Women's Quality of Life During Pregnancy: Kontakt November 2017Dokument7 SeitenMeasuring Women's Quality of Life During Pregnancy: Kontakt November 2017DrAnisha PatelNoch keine Bewertungen
- Joyce Travelbee's Human-to-Human Relationship ModelDokument4 SeitenJoyce Travelbee's Human-to-Human Relationship ModelHugMoco Moco Locah ÜNoch keine Bewertungen
- Antimaleria Drug ModelsDokument33 SeitenAntimaleria Drug ModelsMehari AsratNoch keine Bewertungen
- Recovering From PsychosisDokument2 SeitenRecovering From PsychosisTalha SaeedNoch keine Bewertungen
- Compensation To Clinical Trial Participants in India - A Gap AnalysisDokument8 SeitenCompensation To Clinical Trial Participants in India - A Gap AnalysisMeghna SinghNoch keine Bewertungen
- Shoulder Presentation Diagnosis and ManagementDokument20 SeitenShoulder Presentation Diagnosis and ManagementCrevins NyarikiNoch keine Bewertungen
- ParamyxoviridaeDokument27 SeitenParamyxoviridaeFarrah BenoitNoch keine Bewertungen