Beruflich Dokumente
Kultur Dokumente
Normal and Altered Breath and Voice Sounds
Hochgeladen von
andarunfCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Normal and Altered Breath and Voice Sounds
Hochgeladen von
andarunfCopyright:
Verfügbare Formate
Normal and Altered Breath and Voice Sounds
The origins of breath sounds are still unclear. According to leading theories, turbulent air flow in
the central airways produces the tracheal and bronchial breath sounds. As these sounds pass
through the lungs to the periphery, lung tissue filters out their higher-pitched components, and
only the soft and lower-pitched components reach the chest wall, where they are heard as
vesicular breath sounds. Normally, tracheal and bronchial sounds may be heard over the trachea
and mainstem bronchi; vesicular breath sounds predominate throughout most of the lungs.
When lung tissue loses its air, it transmits high-pitched sounds much better. If the
tracheobronchial tree is open, bronchial breath sounds may replace the normal vesicular sounds
over airless areas of the lung. This change is seen in lobar pneumonia when the alveoli fill with
fluid, red cells, and white cellsa process called consolidation. Other causes include pulmonary
edema or hemorrhage. Bronchial breath sounds usually correlate with an increase in tactile
fremitus and transmitted voice sounds. These findings are summarized below.
Normal breath sound
Breath Sounds
Predominantly vesicular
Transmitted Voice
Sounds
Spoken words muffled and indistinct
Spoken ee heard as ee Whispered words faint and
indistinct, if heard at all
Tactile Fremitus
Normal
Crackles
Crackles have two leading explanations. (1) They result from a series of tiny explosions when
small airways, deflated during expiration, pop open during inspiration. This mechanism
probably explains the late inspiratory crackles of interstitial lung disease and early congestive
heart failure. (2) Crackles result from air bubbles flowing through secretions or lightly closed
airways during respiration. This mechanism probably explains at least some coarse crackles.
Late inspiratory crackles may begin in the first half of inspiration but must
continue into late inspiration. They are usually fine, fairly profuse, and
persist from breath to breath. They appear first at the bases of the lungs,
spread upward as the condition worsens, and shift to dependent regions with
changes in posture. Causes include interstitial lung disease (such as
fibrosis) and early congestive heart failure.
Early inspiratory crackles appear and end soon after the start of inspiration.
They are often coarse and relatively few in number. Expiratory crackles are
sometimes associated. Causes include chronic bronchitis and asthma.
Midinspiratory and expiratory crackles are heard in bronchiectasis but are
not specific for this diagnosis. Wheezes and rhonchi may be associated.
Wheezes and
Rhonchi
Wheezes occur when air flows rapidly through bronchi that are narrowed
nearly to the point of closure. They are often audible at the mouth as well as
through the chest wall. Causes of wheezes throughout the chest include
asthma, chronic bronchitis, COPD, and congestive heart failure (cardiac
asthma). In asthma, wheezes may be heard only in expiration or in both
phases of the respiratory cycle. Rhonchi suggest secretions in the larger
airways. In chronic bronchitis, wheezes and rhonchi often clear with
coughing.
Occasionally in severe obstructive pulmonary disease, the patient is unable
to force enough air through the narrowed bronchi to produce wheezing. The
resulting silent chest is ominous and warrants immediate attention.
Persistent localized wheezing suggests partial obstruction of a bronchus, as
by a tumor or foreign body. It may be inspiratory, expiratory, or both.
Stridor
A wheeze that is entirely or predominantly inspiratory is called stridor. It is
often louder in the neck than over the chest wall. It indicates a partial
obstruction of the larynx or trachea, and demands immediate attention.
Pleural Rub
Inflamed and roughened pleural surfaces grate against each other as they are
momentarily and repeatedly delayed by increased friction. These
movements produce creaking sounds known as a pleural rub (or pleural
friction rub).
Pleural rubs resemble crackles acoustically, although they are produced by
different pathologic processes. The sounds may be discrete, but sometimes
are so numerous that they merge into a seemingly continuous sound. A rub
is usually confined to a relatively small area of the chest wall, and typically
is heard in both phases of respiration. When inflamed pleural surfaces are
separated by fluid, the rub often disappears.
Mediastinal
Crunch
(Hamman's
Sign)
A mediastinal crunch is a series of precordial crackles synchronous with the
heart beat, not with respiration. Best heard in the left lateral position, it is
due to mediastinal emphysema (pneumomediastinum).
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Cervical Radicular Pain + VideoDokument33 SeitenCervical Radicular Pain + VideoandarunfNoch keine Bewertungen
- Bagan Proposal PenelitianDokument1 SeiteBagan Proposal PenelitianandarunfNoch keine Bewertungen
- Muscle RelaxantsDokument37 SeitenMuscle RelaxantsandarunfNoch keine Bewertungen
- Protein Energy MalnutritionDokument16 SeitenProtein Energy MalnutritionandarunfNoch keine Bewertungen
- Normal and Altered Breath and Voice SoundsDokument3 SeitenNormal and Altered Breath and Voice SoundsandarunfNoch keine Bewertungen
- Thermoregulatory Concept (!) : Internal Core (Organs, CNS, and Muscles) and Outer Shell (SkinDokument4 SeitenThermoregulatory Concept (!) : Internal Core (Organs, CNS, and Muscles) and Outer Shell (SkinandarunfNoch keine Bewertungen
- DRAFT-Course&Symposium Dan Full Paper Presentation 28 Juli 2015Dokument252 SeitenDRAFT-Course&Symposium Dan Full Paper Presentation 28 Juli 2015andarunfNoch keine Bewertungen
- Bagan Proposal PenelitianDokument1 SeiteBagan Proposal PenelitianandarunfNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- What Is BronchitisDokument1 SeiteWhat Is BronchitisMelvin Lopez SilvestreNoch keine Bewertungen
- ARDS Berlin Definition JAMA 2012Dokument8 SeitenARDS Berlin Definition JAMA 2012Irfan HardiNoch keine Bewertungen
- Flyer SV300 - S (2) - 1Dokument2 SeitenFlyer SV300 - S (2) - 1Abo MaramNoch keine Bewertungen
- Jurnal Voice of Midwifery: Nomor 2 September 2019 Halaman 840 - 848Dokument9 SeitenJurnal Voice of Midwifery: Nomor 2 September 2019 Halaman 840 - 848Yadnya SaputraNoch keine Bewertungen
- What Is The Oxygen CascadeDokument27 SeitenWhat Is The Oxygen CascadeRandhir Singh90% (10)
- My Asthma Wallet CardDokument2 SeitenMy Asthma Wallet CardBella Lizy BenNoch keine Bewertungen
- Ventilatory Assistance MechanicalDokument18 SeitenVentilatory Assistance Mechanicalmardsz100% (5)
- Paroxysmal Nocturnal DyspneaDokument5 SeitenParoxysmal Nocturnal DyspneanunungNoch keine Bewertungen
- Nursing Care of Clients Nursing Care of Clients With Altered Ventilatory With Altered Ventilatory Function FunctionDokument179 SeitenNursing Care of Clients Nursing Care of Clients With Altered Ventilatory With Altered Ventilatory Function FunctionPia Rose RoqueNoch keine Bewertungen
- Thoracic Ultrasonography: Clinical Uses and ApplicationsDokument54 SeitenThoracic Ultrasonography: Clinical Uses and ApplicationsMesay AssefaNoch keine Bewertungen
- 4.3 Respi. Percussion VibrationDokument8 Seiten4.3 Respi. Percussion VibrationRiza Angela BarazanNoch keine Bewertungen
- Clinical Aspects of PneumothoraxDokument3 SeitenClinical Aspects of PneumothoraxelisabethNoch keine Bewertungen
- Endotracheal Intubation.1Dokument2 SeitenEndotracheal Intubation.1Sandro RedobleNoch keine Bewertungen
- Airway Clearance TechniquesDokument14 SeitenAirway Clearance TechniquesKhushboo DurejaNoch keine Bewertungen
- At-A-Glance Outpatient Management Reference For Chronic Obstructive Pulmonary Disease (COPD)Dokument8 SeitenAt-A-Glance Outpatient Management Reference For Chronic Obstructive Pulmonary Disease (COPD)RushdaNoch keine Bewertungen
- PhysioEx Exercise 7 Activity 1Dokument6 SeitenPhysioEx Exercise 7 Activity 1Jorge CuevaNoch keine Bewertungen
- Cues/Data Nursing Diagnosis Rationale Goals and Objectives Interventions Rationale Evaluation Subjective DataDokument5 SeitenCues/Data Nursing Diagnosis Rationale Goals and Objectives Interventions Rationale Evaluation Subjective Datatimie_reyesNoch keine Bewertungen
- Bronchitis Acute Brochitis: DefinitionDokument7 SeitenBronchitis Acute Brochitis: DefinitionhemaanandhyNoch keine Bewertungen
- A Bench Study Comparison of Demand Oxygen Delivery Systems and Continuous Flow OxygenDokument7 SeitenA Bench Study Comparison of Demand Oxygen Delivery Systems and Continuous Flow OxygenJafar JilaniNoch keine Bewertungen
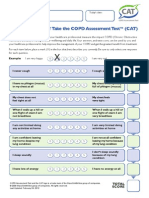
- CATest PDFDokument1 SeiteCATest PDFAsrie Sukawatie PutrieNoch keine Bewertungen
- L17. Askep Kritis Dan Gadar Pasien Dengan Ggguan Sistem Pernafan NontraumatikDokument75 SeitenL17. Askep Kritis Dan Gadar Pasien Dengan Ggguan Sistem Pernafan NontraumatikSepto KristianaNoch keine Bewertungen
- Nursing Care PlanDokument4 SeitenNursing Care Planapi-309251523Noch keine Bewertungen
- Jarvis Chapter 18 Study GuideDokument5 SeitenJarvis Chapter 18 Study GuideEmily Cheng100% (2)
- Thoracic Injuries Nis 2022Dokument24 SeitenThoracic Injuries Nis 2022StefanNoch keine Bewertungen
- Pathophysiology DyspneaDokument1 SeitePathophysiology DyspneaJoseph LimNoch keine Bewertungen
- I Made Harry Raditya (D1a019244) Uas Hukum PemdesDokument7 SeitenI Made Harry Raditya (D1a019244) Uas Hukum PemdesI Made Harry RadityaNoch keine Bewertungen
- Airway Stent Complications: The Role of Follow-Up Bronchoscopy As A Surveillance MethodDokument9 SeitenAirway Stent Complications: The Role of Follow-Up Bronchoscopy As A Surveillance MethodNugroho prasetyoNoch keine Bewertungen
- Genesis Dav Jan 23Dokument7 SeitenGenesis Dav Jan 23Nazmul Alam FarukiNoch keine Bewertungen
- Hypoxia: Name: Abdalaziz Mostafa No: 1176Dokument14 SeitenHypoxia: Name: Abdalaziz Mostafa No: 11763omar18Noch keine Bewertungen
- Pulmonary Function TestsDokument9 SeitenPulmonary Function TestsRick Frea0% (1)