Beruflich Dokumente
Kultur Dokumente
Basic Principles of Cancer Chemotherapy
Hochgeladen von
GerardLumCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Basic Principles of Cancer Chemotherapy
Hochgeladen von
GerardLumCopyright:
Verfügbare Formate
jslum.
com | Medicine
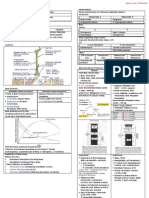
Basic Princi ples of Cancer Chemotherapy
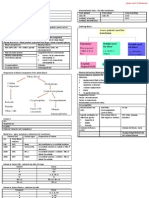
Cancer Established Treatment Modalities
Uncontrolled Multiplication & Spread of abnormal forms of body’s own cell Surgery
2nd most commonest cause of death (1st – CVD) Radiotherapy
1:3 people diagnosed with cancer during lifetime Chemotherapy (Cytotoxics – damage/kill cells)(Inhibit cell division)
Cellular Basis
Cancer arise from loss of control in normal growth
In normal tissue, rates of new growth & old cell death in balance
In cancer, balance is disrupted
Disruption causes
Uncontrolled cell growth
Loss of cell ability to apoptosis
Cancer Chemotherapy
Use of Drugs that are selectively toxic
Intended only for cancer cells
Leaving normal cells unharmed
Not possible to attack only malignant cells
Cytotoxic agents damage/ interfere with DNA synthesis
Cancer – Resistance to Apoptosis (kill all rapidly dividing cells)
Normal cell turns cancerous (1≥ Mutation takes place in DNA) All other (normal) cells affected as well
Inherited Most drugs – Antiproliferative (affect cell division)
Acquired Treatment is directed towards DNA, its precursors, anywhere in pathway
Main genetic lesions Functions of DNA
Inactivation – Tumour Suppressor Gene
Activation – Proto-Oncogene → On cogene DNA
Pathogenesis ↓
RNA
↓
Protein
Indications for Chemotherapy
Disseminated neoplasm & Not amendable to surgery
Adjuvant Neoadjuvant Maintainance
Following surgery/ Given prior to surgical ↓ dose Chemo
radiation treatment
Attacks Shrinks size Prolong remission
Micrometastases
Characteristics of Ideal Chemotherapy
Safe, Effective, Discriminating
Action limited to cancer cells only
Only few Side Effects
Return patient to former state of health
Characteristics of Cancer Cells
Uncontrolled proliferation
Dedifferentiation & Loss of function
↑ Dose Intermittent Therapy
Invasiveness
More effective than Continuous therapy
Metastases
Allow normal tissues to Recover from toxicity between doses
Tumour cells also recover
Goal of Cancer Treatments
Curative Control of Disease Palliative To prevent tumour Regrowing to its original size, ↑ dose is administered in the
next course
Total eradication of Stop cancer from Alleviation of symptoms
cancer cells enlarging/ spreading & avoidance of toxicity
Dose Calculation
Curable cancers Extend survival ↑ Quality of life
Testicular tumour Bases of Body Surface Area
Drugs may not lengthen
Wilm’s tumour Individuals have varying PK (Pharmacokinetics), PD (Pharmacodynamics)
life
Have Narrow Therapeutic Index
jslum.com | Medicine
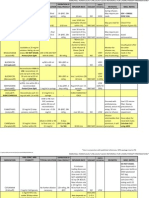
Cell Cycle Combination Therapy
Growth cycle of a cell is the major determinant of Cancer cells – Heterogenous & Respon d differently to Different drugs
responsiveness to chemotherapy Different Toxicity & Mechanism of Action (MOA )
(overcome limited cell kill of individual anti cancer agents)
Measure of cell growth = cell cycle Advantages
Prevent development of drug Resistance (↓ Chance to develop – 2 drugs)
4 Major Phases of cell cycle ↑ Cancer cell kill (Different MOA)
G1 ↓ Toxicity (Use drugs that do not have Overlapping Toxicities)
S Principles for Combination Therapy
G2 Each drug should be active when used alone (against any particular CA)
M Drugs combined should have different MOA
Drugs combined should have different Toxic Effects Profile
Minimal Cross-Resistance between drugs
Hodgkin’s Non-H odgkin’s Testicular CA Breast CA
MOPP CHOP PVB CMF
Anticancer Drugs & Cell Cycle Mechlorethamine Cyclophosphamide Platinol Cyclophosphamide
Rapidly dividing cells - ↑ susceptible to Anticancer drugs (cisplatin)
Non-proliferating cells (G0 phase) – Not affected (Generally) Oncovin Hydroxydaunorubicin Vinblastine Methotrex ate
Cell-cycle spe cific (CCS) Cell-cycle Non-s pecific (CCNS) (vincristine)
Effective only in Replicating cells Kill tumour cells Procarbazine Oncovin Bleomycin Fluorouracil
(Not in G0 – resting phase) (Cycling & G0 resting phase) (vincristine) (+/- tamoxifen)
Prednisone Prednisone
Effective in ↑ Growth Fraction Effective for ↓ Growth Fraction
ABVD CAF
(↑ Rapid cell turn-over, ↑ effe ctive) (usually solid tumours)
Adriamycin Cyclophosphamide
Effective also in ↑ Growth Fraction (doxorubicin)
malignancies Bleomycin Adriamycin
Generally ↑ active in Haematology Most toxic in cycling cells Vinblastine Fluorouracil
malignancies – relatively large Dacarbazine
proportion of cells are proliferating Hodgkin’s lymphoma
(↑ Growth Fraction) MOPP induce remission in 80% of patients (Replaced by ABVD due to S/E)
When given individually, induce remission in only <40%
ABVD is as effective as MOPP, with ↓ S/E of Sterility & 2° Malignancy (Leukaemia)
May alternate MOPP with ABVD if neoplasm become resistant
Cancer Cure Rates
50% of patients with CA can be cured (17% by chemotherapy)
CA Chemotherapy curative for
Testicular CA
Diffuse Large Cell Lymphoma
Hodgkin’s Lymphoma
Choriocarcinoma
Childhood Tumours
(ALL, Burkitt’s Lymphoma, Wilm’s Tumour, Embryonal Rhabdomyosarcoma)
Initial Surgery + Chemotherapy Difficult for CA Chemotherapy
Growth Fraction curative for to be curative
Ratio of Proliferating cells to cells in G0 Early stage Breast CA Colon CA
↑ Proliferating cells, ↓ G0 cells = ↑ Growth Fraction Osteogenic sarcoma Lung CA
↓ ProliferaƟng cells, ↑ G0 cells = ↓ Growth FracƟon
Growth Fraction & Tumour size Problems in Chemotherapy
As Tumour size ↑, Growth FracƟon ↓ Resistance
• ↓ O2 & Nutrient 1° Acquired
• Eg. Growth Fraction <10% in slow-growing Colon & Lung carcinoma Absence of response on 1st Mutation
Debulking (surgery, radiotherapy) can stimulate remaining cells into active exposure
proliferation Eg. Non-Small cell CA of Lung, Colon Particularly with prolonged
• ↑ SuscepƟbility to cancer Chemotherapy suboptimal drug dose
Solid cancer Tumours Disseminated cancers
↓ Growth FracƟon ↑ Growth FracƟon Mechanism of Resistance Multidrug Resistance
Respond p oorly to Chemotherapy Respond well to Chemotherapy ↓ Uptake of Drugs Associated with ↑ expression of
Need to be removed by Surgery Deletion of enzyme to Activate Drug normal gene (MDR1 gene) for cell
↑ Detoxification of Drug surface glycoprotein
Log Kill Hypothesis ↑ Concentration of Target enzyme (P-glycoprotein)
Chemotherapeutic agents kill a Constant Fraction of cells (1st order kinetics) Rapid repair of Drug-Induced Le sion
(rather than a specific number of cells ) ↓ No. of Rece ptors for Drug MDR1 gene – involved in drug Efflux
RED ↑ Drug Efflux Results – Pumping of drugs Out of
Untreated patients cell through P-glycoprotein
DARK BLUE Toxicity
Late Rx (to take) Damage DNA, initiate apoptosis
Infrequent sched uling Affect rapidly dividing normal cells – toxicity (side effects)
LIGHT BLUE • Hyperuricaemia & Tumour Lysis Syndrome (TLS)
Early Rx (to take) • Extravasation of IV drugs
↑ Intensive Combination Chemo • Nausea, Vomiting (CTZ stimulation)
GREEN • BM suppression
Early Surgery
• Impaired Immune response
Followed by Adjuvant Chemo (Myelosuppression ↓ WBC)
Amount of cells before Therapy determines the success of Chemotherapy • Alopecia (reversible)
Better results achieved with • Reproductive function (Impair Gametogenesis) (Teratogenic 1st trimester)
Early Treatment Treatment induced Tumours
Small Tumours Anticancer agents are also Mutagens (particularly, alkylating agents)
Intensive Treatment Acute Non-Lymp hocytic Leukaemia (eg. AML)
Combination Che motherapy
Early Surgical Removal – followed by Adjuvant Chemo (for solid tumours)
Das könnte Ihnen auch gefallen
- Diagnostic Problems in Tumors of Gastrointestinal Tract: Selected TopicsVon EverandDiagnostic Problems in Tumors of Gastrointestinal Tract: Selected TopicsNoch keine Bewertungen
- Fast Facts: Measurable Residual Disease: A clearer picture for treatment decisionsVon EverandFast Facts: Measurable Residual Disease: A clearer picture for treatment decisionsNoch keine Bewertungen
- Diagnostic Problems in Tumors of Female Genital Tract: Selected TopicsVon EverandDiagnostic Problems in Tumors of Female Genital Tract: Selected TopicsNoch keine Bewertungen
- The American Cancer Society's Principles of Oncology: Prevention to SurvivorshipVon EverandThe American Cancer Society's Principles of Oncology: Prevention to SurvivorshipThe American Cancer SocietyNoch keine Bewertungen
- ChemotherapyDokument1 SeiteChemotherapyGerardLum100% (2)
- Hemostasis and Thrombosis: Practical Guidelines in Clinical ManagementVon EverandHemostasis and Thrombosis: Practical Guidelines in Clinical ManagementHussain I. SabaNoch keine Bewertungen
- Introduction to Clinical OncologyVon EverandIntroduction to Clinical OncologyStanley T. CrookeNoch keine Bewertungen
- Ion Channels in Health and DiseaseVon EverandIon Channels in Health and DiseaseGeoffrey S. PittNoch keine Bewertungen
- ChemotherapyDokument44 SeitenChemotherapyJohn Mark ParacadNoch keine Bewertungen
- Tietz's Applied Laboratory MedicineVon EverandTietz's Applied Laboratory MedicineMitchell G. ScottBewertung: 3 von 5 Sternen3/5 (1)
- Fast Facts: Cholangiocarcinoma: Diagnostic and therapeutic advances are improving outcomesVon EverandFast Facts: Cholangiocarcinoma: Diagnostic and therapeutic advances are improving outcomesNoch keine Bewertungen
- Understanding Cancer: From Basics to TherapeuticsVon EverandUnderstanding Cancer: From Basics to TherapeuticsBewertung: 5 von 5 Sternen5/5 (2)
- Thrombosis and Bleeding Disorders: Theory and MethodsVon EverandThrombosis and Bleeding Disorders: Theory and MethodsNils U. BangBewertung: 2 von 5 Sternen2/5 (1)
- Pharm Chemo Drugs SauldDokument6 SeitenPharm Chemo Drugs Sauldneal100% (1)
- Clinical Oncology For StudentsDokument132 SeitenClinical Oncology For StudentsJay KayNoch keine Bewertungen
- 18 Lymphoma - Libre PathologyDokument13 Seiten18 Lymphoma - Libre PathologyfadoNoch keine Bewertungen
- Oncology NotesDokument9 SeitenOncology NotesmyrkNoch keine Bewertungen
- Cancer ChemotherapyDokument9 SeitenCancer ChemotherapyJennicaNoch keine Bewertungen
- ChemotherapyDokument30 SeitenChemotherapyHealth Education Library for People100% (3)
- ASCO 2017 Edbook PDFDokument871 SeitenASCO 2017 Edbook PDFf2ko4100% (2)
- CD Marker HandbookDokument47 SeitenCD Marker HandbookSteph Vee100% (1)
- Anticancer Drugs: Pharmacology of Chemotherapy AgentsDokument126 SeitenAnticancer Drugs: Pharmacology of Chemotherapy AgentsZaina MasriNoch keine Bewertungen
- OncologyDokument247 SeitenOncologyMaris Angelica Ayuyao100% (2)
- Chemo MedsDokument17 SeitenChemo MedsSophia Smartz100% (1)
- Introduction of Clinical OncologyDokument52 SeitenIntroduction of Clinical OncologyThis is Pony100% (1)
- Oncology Mnemonics: Tumors that Metastasize to SkinDokument4 SeitenOncology Mnemonics: Tumors that Metastasize to SkinMuhammad Luqman Nul Hakim100% (2)
- LeukemiaDokument169 SeitenLeukemiawhite7100% (4)
- Breast CancerDokument31 SeitenBreast Cancerstarskyhutch0000Noch keine Bewertungen
- Flash Card PatologyDokument529 SeitenFlash Card PatologyXiomara Cuadros0% (1)
- Oncology Drug ListDokument11 SeitenOncology Drug Listashrafh100% (1)
- Cell Adaptation & Response To Injury by NikitaDokument3 SeitenCell Adaptation & Response To Injury by NikitaMedical Student NotesNoch keine Bewertungen
- Quiz Hematology Oncology Part 2 of 2Dokument60 SeitenQuiz Hematology Oncology Part 2 of 2MedShare100% (5)
- Key chemotherapy drugs and their mechanismsDokument7 SeitenKey chemotherapy drugs and their mechanismsNoelani-Mei AscioNoch keine Bewertungen
- Heme Onc Quick Reference REV0112Dokument5 SeitenHeme Onc Quick Reference REV0112arthurgonzalezNoch keine Bewertungen
- Acute Lymphoblastic Leukemia QuestionsDokument22 SeitenAcute Lymphoblastic Leukemia Questionsđoàn lươngNoch keine Bewertungen
- ESMO 2012 Cancer Chemotherapy HandbookDokument226 SeitenESMO 2012 Cancer Chemotherapy HandbookHeTranDuc100% (2)
- Chemotherapy Protocols and Infusion Sequence Schedule Considerations in Cancer TreatmentDokument330 SeitenChemotherapy Protocols and Infusion Sequence Schedule Considerations in Cancer TreatmentVirgilio Rafael Tovar Vasquez100% (4)
- Anti-Coagulants, Anti-Platelets, FibrinolyticsDokument1 SeiteAnti-Coagulants, Anti-Platelets, FibrinolyticsGerardLum100% (1)
- Introduction To TransplantationDokument3 SeitenIntroduction To TransplantationGerardLumNoch keine Bewertungen
- WBC Neoplasms Review - PathologyDokument6 SeitenWBC Neoplasms Review - Pathologylas100% (6)
- Anemia PDFDokument36 SeitenAnemia PDFJANoch keine Bewertungen
- Fundamentals of OncologyDokument1.012 SeitenFundamentals of Oncologyainie88% (8)
- Leukemias & Lymphomas - HY USMLEDokument87 SeitenLeukemias & Lymphomas - HY USMLEMatt McGlothlinNoch keine Bewertungen
- Summary of All AnemiaDokument2 SeitenSummary of All Anemiabenlarsena93% (14)
- Case Study Oncology Supportive CareDokument3 SeitenCase Study Oncology Supportive CareJude Micko Bunyi AlipitNoch keine Bewertungen
- Acute Leukemia RodaksDokument14 SeitenAcute Leukemia RodaksLoiLoiChanNoch keine Bewertungen
- Handbook of Systemic Treatments For Cancer - 8th EditionDokument186 SeitenHandbook of Systemic Treatments For Cancer - 8th EditionLaurențiu Acostioaei67% (3)
- Basic OncologyDokument42 SeitenBasic Oncologybudiagungnugraha100% (1)
- General Principles of Combination ChemotherapyDokument40 SeitenGeneral Principles of Combination Chemotherapyoncology KMC-KnlNoch keine Bewertungen
- Robbins Basic Pathology Chapter 1Dokument15 SeitenRobbins Basic Pathology Chapter 1Salman AsgharNoch keine Bewertungen
- People'S College of Nursing and Research Center.: Submitted To Presented byDokument49 SeitenPeople'S College of Nursing and Research Center.: Submitted To Presented byabhishek dadhichNoch keine Bewertungen
- Medical Oncology JNR HandbookDokument50 SeitenMedical Oncology JNR Handbookhmudeveloper100% (1)
- Quiz Hematology Oncology Part 1 of 2Dokument84 SeitenQuiz Hematology Oncology Part 1 of 2MedShare100% (11)
- Pharmacology ChemotherapyDokument28 SeitenPharmacology ChemotherapyDartiguesNoch keine Bewertungen
- Urinary Tract InfectionDokument4 SeitenUrinary Tract InfectionGerardLum100% (2)
- Posterior Pituitary SyndromeDokument1 SeitePosterior Pituitary SyndromeGerardLumNoch keine Bewertungen
- Vesico Ureteral RefluxDokument1 SeiteVesico Ureteral RefluxGerardLumNoch keine Bewertungen
- Urinary Tract Infections in ChildrenDokument1 SeiteUrinary Tract Infections in ChildrenGerardLumNoch keine Bewertungen
- Pituitary Gland PathologyDokument4 SeitenPituitary Gland PathologyGerardLumNoch keine Bewertungen
- Sexually Transmitted DiseasesDokument6 SeitenSexually Transmitted DiseasesGerardLum100% (3)
- ThalassaemiaDokument4 SeitenThalassaemiaGerardLum100% (4)
- Thyroid PhysiologyDokument2 SeitenThyroid PhysiologyGerardLum100% (2)
- ThrombophiliaDokument3 SeitenThrombophiliaGerardLum100% (1)
- Renal Function in Disease StateDokument2 SeitenRenal Function in Disease Statedamai140390Noch keine Bewertungen
- Soft Tissue InfectionsDokument3 SeitenSoft Tissue InfectionsGerardLum100% (1)
- Pituitary DysfunctionDokument2 SeitenPituitary DysfunctionGerardLum0% (1)
- Soft Tissue TumoursDokument8 SeitenSoft Tissue TumoursGerardLum100% (2)
- Skeletal Muscle RelaxantsDokument1 SeiteSkeletal Muscle RelaxantsGerardLum100% (2)
- Renal Excretion of DrugsDokument3 SeitenRenal Excretion of DrugsGerardLum100% (3)
- Prostate GlandsDokument3 SeitenProstate GlandsDragan PetrovicNoch keine Bewertungen
- Pathology of TestesDokument4 SeitenPathology of TestesGerardLum100% (1)
- Principles of Blood TransfusionDokument2 SeitenPrinciples of Blood TransfusionGerardLum100% (3)
- Pathology GlomerulonephritisDokument4 SeitenPathology GlomerulonephritisGerardLum100% (2)
- Pathology of DiabetesDokument4 SeitenPathology of DiabetesGerardLum100% (4)
- Pathophysiology of Calcium, Phosphate HomeostasisDokument5 SeitenPathophysiology of Calcium, Phosphate HomeostasisGerardLum100% (1)
- Pathophysiology of Nerve InjuryDokument2 SeitenPathophysiology of Nerve InjuryGerardLum100% (1)
- Pathology of Thyroid DiseasesDokument5 SeitenPathology of Thyroid DiseasesGerardLum100% (2)
- Pathogenesis Chronic Complications DiabetesDokument5 SeitenPathogenesis Chronic Complications DiabetesGerardLum100% (1)
- Paediatrics OrthopaedicsDokument5 SeitenPaediatrics OrthopaedicsGerardLumNoch keine Bewertungen
- Pathogenesis Bleeding DisordersDokument4 SeitenPathogenesis Bleeding DisordersGerardLumNoch keine Bewertungen
- Overview of AnaemiaDokument2 SeitenOverview of AnaemiaGerardLumNoch keine Bewertungen
- Nsaids DrugsDokument2 SeitenNsaids DrugsIrene Zae MwandotoNoch keine Bewertungen
- Obstructive UropathyDokument3 SeitenObstructive UropathyGerardLum100% (1)
- Nocturnal EnuresisDokument1 SeiteNocturnal EnuresisGerardLumNoch keine Bewertungen
- Common Symptoms and Signs of GIDokument103 SeitenCommon Symptoms and Signs of GIapi-3858544Noch keine Bewertungen
- Hemorrhagic Shock Signs, Assessment and ManagementDokument114 SeitenHemorrhagic Shock Signs, Assessment and ManagementclaudiaNoch keine Bewertungen
- An Approach To The Diagnostic Study On Annavaha Srotodusti in Urdwaga Amlapitta WSR To Oesophagogastroduodenoscopic ChangesDokument4 SeitenAn Approach To The Diagnostic Study On Annavaha Srotodusti in Urdwaga Amlapitta WSR To Oesophagogastroduodenoscopic ChangesEditor IJTSRDNoch keine Bewertungen
- Disability Category ChartDokument4 SeitenDisability Category Chartapi-325700981100% (1)
- BIO K 211 TDS (EN) Fasciola Hepatica SeroDokument4 SeitenBIO K 211 TDS (EN) Fasciola Hepatica SeroPia Loreto Cid TroncosoNoch keine Bewertungen
- Jurnal Forensik - Luka TembakDokument8 SeitenJurnal Forensik - Luka Tembakrosa snakNoch keine Bewertungen
- COVID-19 Isolation Effects on Mental Health and EconomyDokument10 SeitenCOVID-19 Isolation Effects on Mental Health and EconomyRimsHa ShAbbirNoch keine Bewertungen
- Health Screening Form For EmployeesDokument5 SeitenHealth Screening Form For EmployeesArun MmohantyNoch keine Bewertungen
- Influenza PATHOPHYSIOLOGYDokument3 SeitenInfluenza PATHOPHYSIOLOGYElle RosalesNoch keine Bewertungen
- Hypo Kale MiaDokument13 SeitenHypo Kale MiaMuhammad IqbalNoch keine Bewertungen
- OrifDokument2 SeitenOrifGene Edward D. ReyesNoch keine Bewertungen
- Adult Vancomycin Dosing Guidelines DefinitionsDokument2 SeitenAdult Vancomycin Dosing Guidelines DefinitionsPhạm DuyênNoch keine Bewertungen
- Bernabe Ncm109 LabDokument4 SeitenBernabe Ncm109 LabKarl LintanNoch keine Bewertungen
- PAVSDMAPCAsDokument3 SeitenPAVSDMAPCAsRajesh SharmaNoch keine Bewertungen
- Ayurvedic Diabetes CureDokument13 SeitenAyurvedic Diabetes CureYassine KrineNoch keine Bewertungen
- Prelim ProgrammeDokument7 SeitenPrelim Programmeasalizwa ludlalaNoch keine Bewertungen
- Dentigerous Cyst RadiolucencyDokument25 SeitenDentigerous Cyst RadiolucencyDr. Deepanshi SutariaNoch keine Bewertungen
- PSA and Psoriasis Exam ChecklistDokument2 SeitenPSA and Psoriasis Exam ChecklistChaken ManiyanNoch keine Bewertungen
- PE1 ReviewerDokument4 SeitenPE1 ReviewerZoe BeatrizNoch keine Bewertungen
- DUPUYTREN'S SYNDROME TestDokument15 SeitenDUPUYTREN'S SYNDROME TestreyNoch keine Bewertungen
- Neuroanatomical Changes After Eye Movement Desensitization and Reprocessing (EMDR) Treatment in Posttraumatic Stress DisorderDokument2 SeitenNeuroanatomical Changes After Eye Movement Desensitization and Reprocessing (EMDR) Treatment in Posttraumatic Stress DisorderClaudio PeñafielNoch keine Bewertungen
- Acute Myeloid LeukemiaDokument1 SeiteAcute Myeloid LeukemiaAlleah Salbo KepusNoch keine Bewertungen
- Functional neurological disorder new subtypes and shared mechanisms - CLINICALKEY - Dr Rivas (1)Dokument14 SeitenFunctional neurological disorder new subtypes and shared mechanisms - CLINICALKEY - Dr Rivas (1)Fernando Pérez MuñozNoch keine Bewertungen
- Case Pres A1 SurgDokument14 SeitenCase Pres A1 SurgWyen CabatbatNoch keine Bewertungen
- PNSS Drug StudyDokument2 SeitenPNSS Drug Studyrain peregrinoNoch keine Bewertungen
- Epilepsy GuidelinesDokument94 SeitenEpilepsy GuidelinesAyu Cliquers100% (1)
- Diabetes Mellitus in Children 1Dokument89 SeitenDiabetes Mellitus in Children 1Vinay PatilNoch keine Bewertungen
- Oral Pathology in Paediatric Patients-Mini-Systematic ReviewDokument7 SeitenOral Pathology in Paediatric Patients-Mini-Systematic ReviewYuganya SriNoch keine Bewertungen
- Obg MCQSDokument11 SeitenObg MCQSShriyansh ChaharNoch keine Bewertungen
- Vocal Cord ParalysisDokument74 SeitenVocal Cord ParalysisWaqas KhanNoch keine Bewertungen