Beruflich Dokumente
Kultur Dokumente
Out
Hochgeladen von
Pol FernandezCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Out
Hochgeladen von
Pol FernandezCopyright:
Verfügbare Formate
Unusual presentation of more common disease/injury
CASE REPORT
Endometriosis: a rare and interesting cause
of recurrent haemorrhagic ascites
Jenine Bignall,1 Kirana Arambage,2 Sotirios Vimplis3
1
Margaret Pyke Centres,
London, UK
2
Department of Gynaecology,
John Radcliffe Hospital,
London, UK
3
Department of Obstetrics and
Gynaecology, Whipps Cross
Hospital, London, UK
Correspondence to
Dr Jenine Bignall,
jbignall@yahoo.com
Accepted 5 October 2014
SUMMARY
Recurrent haemorrhagic ascites as a cause of
endometriosis is rare. We report the case of a 36-yearold woman presenting acutely with abdominal
distension, ascites and an elevated CA-125 raising the
suspicion of ovarian malignancy. Tissue biopsies retrieved
during laparoscopy conrmed the diagnosis of
endometriosis associated with haemorrhagic ascites.
Gonadotropin-releasing hormone (GnRH) analogues were
started to manage symptoms, with good effect.
Subsequently, in vitro fertilisation resulted in a successful
singleton pregnancy and by the second trimester, there
was full resolution in symptoms. During the early
puerperal period, the development of massive ascites
recurred, requiring symptomatic relief through repeated
ascitic drainage and GnRH analogues. Long-term followup is planned with the hope of continuing with medical
management at least until the patients family is
complete when the surgical option of bilateral salpingooophorectomy with or without hysterectomy will be
discussed.
BACKGROUND
Endometriosis is a common cause of morbidity in
young women. This case highlights a rare but interesting presentation of endometriosis and the obstacles faced with managing this poorly understood
disease.
polycystic. Serum tumour markers demonstrated a
markedly raised CA-125 of 1123 U/mL. A sample of
ascitic uid was obtained through paracentesis.
Cytological analysis of the ascitic uid failed to
detect any evidence of malignant cells. Owing to the
extensive volume of ascites, an ascitic drain was
inserted under ultrasound guidance. In total, 3.5 L
of blood stained uid was drained within the rst
24 h. Cultures were negative and no acid-fast bacilli
were detected.
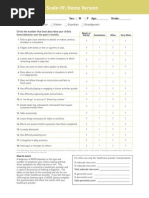
CT of the abdomen and pelvis (gure 1) further
demonstrated ascites and suggested evidence of
disease affecting the transverse colon and small
bowel with no evidence of pelvic pathology.
DIFFERENTIAL DIAGNOSIS
After discussion at a gynaecology oncology multidisciplinary team meeting, the decision was made
to perform an exploratory laparoscopy to obtain a
tissue biopsy as it was thought that an
imaging-guided attempt for biopsy carried a higher
risk of bowel injury.
Findings at laparoscopy included: 1.6 L of haemorrhagic ascites, large nodules at both uterosacral
ligaments and multiple nodules affecting the
CASE PRESENTATION
A 36-year-old Afro-Caribbean nulliparous woman
presented to the emergency department with acute
abdominal pain and bloating. Further questioning
revealed a 7 month history of worsening dysmenorrhoea, deep dyspareunia and constipation. Her menstrual cycles were regular and smear history was
normal. The patients medical history included a
long history of recurrent urinary tract infections.
There was no signicant family history and she was
not on any regular medication; she neither smoked
nor drank alcohol. Abdominal examination revealed
generalised tenderness and distension, however,
gynaecological examination was unremarkable.
INVESTIGATIONS
To cite: Bignall J,
Arambage K, Vimplis S. BMJ
Case Rep Published online:
[please include Day Month
Year] doi:10.1136/bcr-2013010052
Blood analysis showed a microcytic anaemia with a
haemoglobin of 10.8 g/dL and a lactate dehydrogenase of 405 IU/L. An ultrasound scan of the abdomen
and pelvis revealed extensive ascites with no evidence of adnexal masses. MRI of the pelvis was also
performed conrming a large amount of uid in the
pelvis with a faint uid level suggesting a collection.
The uterus was normal and both ovaries appeared
Figure 1 CT study showing gross ascites at the time of
presentation.
Bignall J, et al. BMJ Case Rep 2014. doi:10.1136/bcr-2013-010052
Unusual presentation of more common disease/injury
Figure 2 Haemorrhagic ascites.
Figure 4
ascending colon, transverse colon, small bowel and peritoneum.
The sigmoid colon was densely adherent to the left pelvic side
wall and posterior uterine wall obstructing the view of the left
adnexum (gures 24). Furthermore, a dilated oedematous right
tube was found with the right ovary adherent to the pelvic side
wall. Multiple biopsies were obtained and histology was consistent with cyclical endometrium in the proliferative phase. A diagnosis of stage IV endometriosis1 with associated recurrent
haemorrhagic ascites was made.
At the time of caesarean section a small amount of haemorrhagic ascites was found and endometriotic implants were found
at the bladder peritoneum. The lower uterine segment was thick
and vascular, and the pouch of Douglas was obliterated with
sigmoid colon adherent to the back of the uterus. A live female
infant was delivered in good condition and admitted to the
special care baby unit. The patients postoperative recovery was
slow but she was eventually discharged home with advice to
continue regular expression of breast milk to induce lactational
amenorrhoea and prolong ovarian suppression.
Two weeks postnatally, the patient re-presented to the emergency department with acute abdominal pain and distension.
Imaging conrmed a recurrence of ascites, which was drained.
She was unable to continue with breast feeding in view of the
severe pain. She was restarted on GnRH analogues and required
a further three ascitic drains during the puerperium. After the
fth GnRH injection, an ultrasound scan showed no evidence of
ascites, and add-back tibolone was started. She is currently also
under the care of the pain team and her symptoms are well controlled on pregabalin and non-steroidal anti-inammatory medication. The surgical option of bilateral salpingo-oophorectomy
with or without hysterectomy remains an option and will be considered further when her family is complete.
TREATMENT
Owing to the widespread nature of her disease extending
beyond the pelvis, the patient was started on gonadotropinreleasing hormone (GnRH) analogues during which time her
symptoms gradually improved. Fertility implications were discussed and the couple expressed the desire to start a family.
After 5 months of GnRH analogue injections, during which
National Health Service funding was secured, the couple was
referred to a fertility clinic and underwent a cycle of in vitro fertilisation (IVF) treatment. Fourteen eggs were retrieved and
2.5 L of haemorrhagic ascitic uid was drained at the time of
egg collection. Six embryos developed to the blastocyst stage,
ve were frozen and the patient underwent a single embryo
transfer. She had a positive pregnancy test 2 weeks later.
Episodes of recurrent ascites persisted during the rst trimester;
however, by the second trimester of pregnancy, her symptoms
had settled.
OUTCOME AND FOLLOW-UP
At 32 weeks gestation she presented in preterm labour and
underwent an emergency caesarean section for fetal distress.
Figure 3 Multiple active endometriotic nodules.
2
Abdominal wall bowel adhesion.
DISCUSSION
Endometriosis is dened as the presence of endometrial tissue
located outside of the uterine cavity. In cases of pelvic endometriosis, symptoms often include chronic pelvic pain, dysmenorrhoea, deep dyspareunia and subfertility. Recurrent
haemorrhagic ascites secondary to endometriosis is a very rare
complication of the condition2 3 and is often initially mistaken
for ovarian/primary peritoneal malignancy. The rst case of
endometriosis-related ascites was described by Brews et al in
1954,4 and since then a further 63 cases have been reported
worldwide with a predominantly higher occurrence in nulliparous women of African descent.5 Most cases of endometriosisrelated ascites present with a history of dysmenorrhoea and
chronic pelvic pain alongside progressive abdominal distension.2 57 The pathophysiology of endometriosis is not completely understood, however, various theories exist.
Furthermore, the exact cause of the development of recurrent
ascites is not known, however, Bernstein et al8 described a theory
proposing the formation of ascites due to irritation of serosal surfaces by free blood released from ruptured chocolate cysts.
Elevated CA-125 levels may be associated with ovarian endometrioma and advanced endometriosis, as demonstrated in our
Bignall J, et al. BMJ Case Rep 2014. doi:10.1136/bcr-2013-010052
Unusual presentation of more common disease/injury
case. This is often a cause for concern at initial presentation,
often raising the suspicion of ovarian malignancy.
The long-term management of severe endometriosis associated with recurrent ascites is difcult. Consideration of the
patients age, surgical history and desire for preservation of fertility is important in choosing between medical and surgical
management. Currently, there are no controlled studies to determine whether surgical excision of moderate-to-severe endometriosis enhances fecundity rates and thus surgery is generally not
recommended unless performed for other indications such as
management of chronic pain. In our case, with multifocal
disease and extensive bowel involvement, it was felt that the aim
of any surgical intervention would be to excise the large
nodules rather than aim to treat all of the endometriotic
implants. This would involve extensive bowel surgery with a
high risk of resection with no good evidence of improvement in
fertility and no guaranteed resolution of ascites. In a Cochrane
review of three randomised controlled trials, 36 months of
ovarian suppression with GnRH agonists before IVF in women
with stage IIIIV endometriosis led to a fourfold increase in clinical pregnancy rates.9
Management in previously reported cases has included medical
management with GnRH analogues and surgical management in
the form of unilateral/bilateral salpingo-oophorectomy, with or
without hysterectomy in women who have completed their family.
GnRH analogue treatment is considered an effective treatment option particularly where preservation of fertility is necessary, with evidence in some cases of full remission after
2 years.10 Progestogens are also used in the medical management of endometriosis and have been shown to induce regression and apoptosis of endometriotic lesions. Potential side
effects include acne, hirsutism, weight gain and unscheduled
vaginal bleeding, which may render them unfavourable in some
women. Side effects of GnRH analogues include hot ushes,
vaginal dryness and sexual dysfunction. In our case, GnRH analogues were used prior to IVF and, after discussion about the
options, were chosen again in the puerperium.
The effectiveness of medical and/or surgical ovarian suppression supports the hypothesis of the ovary being a key element in
the pathogenesis of the disease.
It has been reported that endometriosis-related ascites has a
high risk of recurrence5 6 with a 50% recurrence risk reported
after unilateral oophorectomy or cystectomy. As a result, longterm follow-up care is important, particularly in patients undergoing medical management due to the high recurrence rates.6
Although rare, this case highlights the importance of considering endometriosis in the differential diagnosis of women of
reproductive age and African descent presenting with massive
haemorrhagic ascites. Where possible, radical surgery consisting
of hysterectomy and bilateral oophorectomy should be avoided
as evidence has demonstrated successful resolution in symptoms
with medical therapy alone.
Learning points
Consider endometriosis as a differential diagnosis in women
of reproductive age and African descent presenting with
chronic pelvic/abdominal pain, anaemia and haemorrhagic
ascites.
The long-term management of severe endometriosis
associated with recurrent ascites is difcult. Consideration of
the patients age, surgical history and desire for preservation
of fertility is important in choosing between medical and
surgical management.
Endometriosis-related ascites has a high risk of recurrence.
Multidisciplinary input including the pain team is essential
in providing holistic care.
Acknowledgements The authors thank Mr Oladimeji Olowu and Mr Anthony
Hollingworth.
Competing interests None.
Patient consent Obtained.
Provenance and peer review Not commissioned; externally peer reviewed.
REFERENCES
1
2
3
4
5
6
7
8
9
10
[No authors listed]. Revised American Society for Reproductive Medicine
classication of endometriosis:1996. Fertil Steril 1997;67:81721.
Morgan TL, Tomich EB, Heiner JD. Endometriosis presenting with hemorrhagic
ascites, severe anemia, and shock. Am J Emerg Med 2013;31:272.
Kopelman A, Schor E, Girao MJBC, et al. Massive ascites, clinical symptom in
woman with endometriosis: a case report. J Minim Invas Gyn 2009;16:S107.
Brews A. Endometriosis including endometriosis of the diaphragm and Meigs
syndrome. Proc Roy Soc Med 1954;47:461.
Gungor T, Kanat-Pektas M, Ozat M, et al. A systematic review: endometriosis
presenting with ascites. Arch Gynecol Obstet 2011;283:51318.
Ekoukou D, Guilherme R, Desligneres S, et al. Endometriosis with massive
hemorrhagic ascites: a case report and review of the literature. J Gynecol Obstet
Biol Reprod 2005;34:3519.
Ussia A, Betsas G, Corona R, et al. Pathophysiology of cyclic hemorrhagic ascites
and endometriosis. J Minim Invas Gyn 2008;15:67781.
Bernstein JS, Perlow V, Brenner JJ. Massive ascites due to endometriosis. Am J Dig
Dis 1961;6:17.
Sallam HN, Garcia-Velasco JA, Dias S, et al. Long-term pituitary down-regulation
before in vitro fertilization (IVF) for women with endometriosis. Cochrane Database
Syst Rev 2006;1:CD004635.
Sait KH. Massive ascites as a presentation in a young woman with endometriosis: a
case report. Fertil Steril 2008;90:2015.
Copyright 2014 BMJ Publishing Group. All rights reserved. For permission to reuse any of this content visit
http://group.bmj.com/group/rights-licensing/permissions.
BMJ Case Report Fellows may re-use this article for personal use and teaching without any further permission.
Become a Fellow of BMJ Case Reports today and you can:
Submit as many cases as you like
Enjoy fast sympathetic peer review and rapid publication of accepted articles
Access all the published articles
Re-use any of the published material for personal use and teaching without further permission
For information on Institutional Fellowships contact consortiasales@bmjgroup.com
Visit casereports.bmj.com for more articles like this and to become a Fellow
Bignall J, et al. BMJ Case Rep 2014. doi:10.1136/bcr-2013-010052
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Experience of Health Professionals Around An Exorcism: A Case ReportDokument4 SeitenExperience of Health Professionals Around An Exorcism: A Case ReportsorinfNoch keine Bewertungen
- Dyslexia and DyscalculiaDokument15 SeitenDyslexia and DyscalculiaSarah BaczanskiNoch keine Bewertungen
- Future of The Pharmaceutical Industry in The GCC 2017 PDFDokument3 SeitenFuture of The Pharmaceutical Industry in The GCC 2017 PDFJeet MehtaNoch keine Bewertungen
- All India Network Hospitals GeneralDokument630 SeitenAll India Network Hospitals GeneralPankajNoch keine Bewertungen
- Screening ADHDDokument2 SeitenScreening ADHDPsiholog Alina Mirela CraiuNoch keine Bewertungen
- Mo2vate Issue 15 - March 2022Dokument74 SeitenMo2vate Issue 15 - March 2022Mo2vate MagazineNoch keine Bewertungen
- HIV/AIDS Education GuideDokument12 SeitenHIV/AIDS Education GuideDutch EarthNoch keine Bewertungen
- Shulbi@merseta.o RG - Za 010 219 3367Dokument111 SeitenShulbi@merseta.o RG - Za 010 219 3367Michael NcubeNoch keine Bewertungen
- GMC Handwara Recruitment 2023Dokument4 SeitenGMC Handwara Recruitment 2023Ummar WaniNoch keine Bewertungen
- The China Study Diiet Plan - MP TiwariDokument3 SeitenThe China Study Diiet Plan - MP Tiwarirajanlko100% (1)
- Meditation and Energy HealingDokument16 SeitenMeditation and Energy HealingCristian CatalinaNoch keine Bewertungen
- Infection Control: Principles in Medical Laboratory Science Practice 1Dokument10 SeitenInfection Control: Principles in Medical Laboratory Science Practice 1Greggory John Tiu CequiñaNoch keine Bewertungen
- FW02 Phy ActivitiesDokument13 SeitenFW02 Phy Activitiesjojo basenNoch keine Bewertungen
- The Prevalence of Malaria Among Pregnant Women On Addmission in Imo State Specialist Hospital OwerriDokument34 SeitenThe Prevalence of Malaria Among Pregnant Women On Addmission in Imo State Specialist Hospital OwerriDaniel ObasiNoch keine Bewertungen
- Learners Individual Reading Assessment ToolDokument7 SeitenLearners Individual Reading Assessment ToolMhen AcenasNoch keine Bewertungen
- XII EnglishDokument11 SeitenXII EnglishNancy GautamNoch keine Bewertungen
- Blood Pressure Variability: How To Deal?: NR Rau, Gurukanth RaoDokument5 SeitenBlood Pressure Variability: How To Deal?: NR Rau, Gurukanth RaoRully SyahrizalNoch keine Bewertungen
- Regulatory Bodies of Nursing in India: Dr. Maheswari JaikumarDokument75 SeitenRegulatory Bodies of Nursing in India: Dr. Maheswari Jaikumarkalla sharonNoch keine Bewertungen
- Cataract PTDokument9 SeitenCataract PTPreeti SharmaNoch keine Bewertungen
- Personal Development 11 Q1 LAS Week4Dokument8 SeitenPersonal Development 11 Q1 LAS Week4Ruben100% (1)
- MSDS Ultrachem Bond AcrDokument5 SeitenMSDS Ultrachem Bond Acrjohan tindiNoch keine Bewertungen
- Tor WFP Food Assistance For Assets ProjectDokument15 SeitenTor WFP Food Assistance For Assets Projectsabri HanshiNoch keine Bewertungen
- Project Management Contractor Wellness Report: Saudi Aramco: Company General UseDokument1 SeiteProject Management Contractor Wellness Report: Saudi Aramco: Company General UseSabre AlamNoch keine Bewertungen
- Breastfeeding ManagementDokument12 SeitenBreastfeeding ManagementtitisNoch keine Bewertungen
- Paramyxovir Idae: Disease/Viral FactorsDokument22 SeitenParamyxovir Idae: Disease/Viral FactorsMary ChristelleNoch keine Bewertungen
- Cancer Bathinda's Dubious DistinctionDokument2 SeitenCancer Bathinda's Dubious DistinctionPardeepSinghNoch keine Bewertungen
- VutaminDokument66 SeitenVutamindyla nabillaNoch keine Bewertungen
- Doh NOTES-1Dokument196 SeitenDoh NOTES-1norabilbaoNoch keine Bewertungen
- Aspek Etik Dan Legal Dalam Keperawatan BencanaDokument11 SeitenAspek Etik Dan Legal Dalam Keperawatan BencanaPhiioNoch keine Bewertungen
- Presentation by DR Madhur Rai - Case Studies of Patients Practising Sahaja Yoga MeditationDokument16 SeitenPresentation by DR Madhur Rai - Case Studies of Patients Practising Sahaja Yoga Meditationtanaha100% (3)