Beruflich Dokumente
Kultur Dokumente
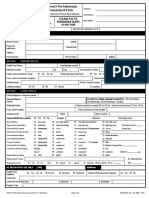
INTERACT Nursing Home To Hospital Transfer Form
Hochgeladen von
Agnieszka WaligóraOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
INTERACT Nursing Home To Hospital Transfer Form
Hochgeladen von
Agnieszka WaligóraCopyright:
Verfügbare Formate
Nursing Home to Hospital
Transfer Form
Resident Name (last, first, middle initial)______________________________________
Sent To (name of hospital )__________________________________________________
Language: English Other ____________ Resident is: SNF/rehab Long-term
Date of transfer __________ /__________ /__________
Date Admitted (most recent) _______ /_______ /_______ DOB _______ /_______ /_______
Sent From (name of nursing home)___________________________ Unit____________
Primary diagnosis(es) for admission____________________________________________
Who to Call at the Nursing Home to Get Questions Answered
Contact Person__________________________________________________________
Name / Title_______________________________________________________________
Relationship (check all that apply)
Tel ( ____________ )______________________________________________________________
Relative
Health care proxy
Guardian
Other
Tel ( ____________ )______________________________________________________________
Primary Care Clinician in Nursing Home
Notified of transfer?
Yes
No
Name ____________________________________________________________________
Aware of clinical situation?
Yes
No
Tel ( ____________ )______________________________________________________________
Code Status
Full Code
DNR
DNI
DNH
Comfort Care Only
MD
NP
PA
Uncertain
Key Clinical Information
Reason(s) for transfer _______________________________________________________________________________________________________________________________________
Is the primary reason for transfer for diagnostic testing, not admission?
No
Relevant diagnoses
CHF
Ca (active treatment) Dementia
Vital Signs
BP___________________ HR __________________RR__________________ Temp________________ O2 Sat _____________ Time taken (am/pm)_____________
COPD
CRF
DM
Yes
Tests:_________________________________________________________________
Other_________________________________________
Most recent pain level _______________________________________________________________ ( N/A)
Pain location: _____________________________________
Most recent pain med _______________________________________________________________ Date given _________ /_________ /_________ Time (am/pm)__________________
Usual Mental Status:
Usual Functional Status:
Additional Clinical Information:
Alert, oriented, follows instructions
Ambulates independently
SBAR Acute Change in Condition Note included
Alert, disoriented, but can follow simple instructions
Ambulates with assistive device
Other clinical notes included
Alert, disoriented, but cannot follow simple instructions
Ambulates only with human assistance
For residents with lacerations or wounds:
Not Alert
Not ambulatory
Date of last tetanus vaccination (if known) _______ /________ /________
Devices and Treatments
Isolation Precautions
Allergies
O2 at ________ L/min by Nasal canula Mask ( Chronic New)
MRSA
_________________________________________
Nebulizer therapy;
Site_________________________________
_________________________________________
C. difficile
_________________________________________
CPAP
( Chronic
New)
BiPAP Pacemaker IV
PICC line
VRE
Norovirus
Bladder (Foley) Catheter ( Chronic
New) Internal Defibrillator
Respiratory virus or flu
_________________________________________
Enteral Feeding
Other ___________________
Other_____________________________
_________________________________________
TPN
Risk Alerts
Anticoagulation
Personal Belongings Sent with Resident
Falls
Pressure ulcer(s)
Aspiration
Seizures
Eyeglasses
Hearing Aid
Harm to self or others
Restraints
Limited/non-weight bearing: ( Left Right )
Dental Appliance
Jewelry
May attempt to exit
Swallowing precautions
Needs meds crushed
Other__________________________________
Other__________________________________________________________________________________________________
_________________________________________
Nursing Home Would be able to Accept Resident Back Under the Following Conditions
Additional Transfer Information
on a Second Page:
ER determines diagnoses, and treatment can be done in NH
VS stabilized and follow up plan can be done in NH
Other___________________________________________________________________________________________________
Included
Will be sent later
Form Completed By (name /title)_______________________________________________________________ Signature ________________________________________________
Report Called in By (name /title)___________________________________________________________________________________________________________________________
Report Called in To (name /title)________________________________________________________________ Date ________ /_________ /_________ Time (am/pm)_______________
2011 Florida Atlantic University, all rights reserved. This document is available for clinical use, but may not be resold or incorporated in software without permission of Florida Atlantic University.
Nursing Home to Hospital
Transfer Form (additional information)
Not critical for Emergency Room evaluation; may be forwarded later if unable to complete at time of transfer.
RECEIVER: PLEASE ENSURE THIS INFORMATION IS DELIVERED TO THE NURSE RESPONSIBLE FOR THIS PATIENT
Resident Name (last, first, middle initial)______________________________________________________________________________________________________________________
DOB ___________ /___________ /___________
Date transferred to hospital ___________ /___________ /___________
Contact at Nursing Home for Further Information
Social Worker
Name / Title_______________________________________________________________
Name____________________________________________________________________
Tel ( _______________ ) __________________________________________________________
Tel ( _______________ ) __________________________________________________________
Family and Other Social Issues (include what hospital staff needs to know
Behavioral Issues and Interventions
about family concerns )_______________________________________________________
_________________________________________________________________________
________________________________________________________________
________________________________________________________________
_________________________________________________________________________
Primary Goals of Care at Time of Transfer
Treatments and Frequency (include special treatments such as dialysis,
Rehabilitation and/or Medical Therapy with intent of returning home
chemotherapy, transfusions, radiation, TPN )
Chronic long-term care
__________________________________________________________________________
_________________________________________________________________________
Palliative or end-of-life care
Receiving hospice care
__________________________________________________________________________
Other___________________________________
__________________________________________________________________________
Skin/Wound Care
Immunizations
Influenza:
Yes
Pressure Ulcers (stage, location,
appearance, treatments)
Yes
__________________________________
Diet
Needs assistance with feeding?
No
Yes
Trouble swallowing?
No
Special consistency (thickened liquids, crush meds, etc)?
No
_________________________________________________________________________
__________________________________
Enteral tube feeding? No Yes (formula/rate )_______________________________
__________________________________
Physical Rehabilitation Therapy
Date ________ / _________ / _________
Pneumococcal:
Date ________ / _________ / _________
ADLs Mark I = Independent D = Dependent A = Needs Assistance
Resident is receiving therapy with goal of returning home?
No
Yes
Physical Therapy:
No Yes
Interventions________________________________________________________
Bathing ______________ Dressing _______________
Transfers ________________
Toileting______________ Eating _________________
Occupational Therapy: No Yes
Interventions________________________________________________________
Can ambulate independently____________________________________________________
Speech Therapy:
No Yes
Interventions________________________________________________________
Needs human assistance to ambulate______________________________________________
Impairments General
Assistive device (if applicable) ____________________________________________________
Impairments Musculoskeletal
Hearing
Amputation
Paralysis
Continence
Cognitive
Speech
Contractures
Vision
Sensation
Other________________________________________
Other________________________________________
_______________________________________________
Bowel
Bladder
Date of last BM ____________ /____________ /____________
Additional Relevant Information _________________________________________________________________________________________________________
_________________________________________________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________________________________________________
Form Completed By (name /title)__________________________________________________________________________________________________________________________
If this page sent after initial transfer: Date sent ____________ /____________ /____________
Time (am/pm)_________________________________________________________
Signature _______________________________________________________________________________________________________________________________________________
2011 Florida Atlantic University, all rights reserved.
Das könnte Ihnen auch gefallen
- Physician Order SheetDokument4 SeitenPhysician Order SheetResci Angelli Rizada-NolascoNoch keine Bewertungen
- The Intersection: Where Evidence Based Nursing and Information Literacy MeetVon EverandThe Intersection: Where Evidence Based Nursing and Information Literacy MeetSue PhelpsBewertung: 2 von 5 Sternen2/5 (1)
- Guidelines for Measuring Household and Individual Dietary DiversityVon EverandGuidelines for Measuring Household and Individual Dietary DiversityNoch keine Bewertungen
- HOME HEALTH NURSE: Passbooks Study GuideVon EverandHOME HEALTH NURSE: Passbooks Study GuideNoch keine Bewertungen
- The Nurse Practitioner in UrologyVon EverandThe Nurse Practitioner in UrologyMichelle LajinessNoch keine Bewertungen
- NURSING ADMINISTRATION, ADVANCED: Passbooks Study GuideVon EverandNURSING ADMINISTRATION, ADVANCED: Passbooks Study GuideNoch keine Bewertungen
- IDCAP Clinical Assessment ToolsDokument4 SeitenIDCAP Clinical Assessment ToolsIDCAP2011100% (1)
- Blank Basic Nursing Physical AssessmentDokument1 SeiteBlank Basic Nursing Physical AssessmentAmeliaM100% (3)
- Patient Admission Assessment FormDokument1 SeitePatient Admission Assessment Formprasanna_326avanthiNoch keine Bewertungen
- Nursing Assessment Form: A. Demographic DataDokument5 SeitenNursing Assessment Form: A. Demographic Datacat_w0m4nNoch keine Bewertungen
- Role of The Professional Nurse in Health PolicyDokument9 SeitenRole of The Professional Nurse in Health PolicytaniaNoch keine Bewertungen
- Obstetric Triage RecordDokument1 SeiteObstetric Triage RecordpramonolentNoch keine Bewertungen
- Asessment of Marilynn e DoengesDokument26 SeitenAsessment of Marilynn e DoengesMuhammad PanduNoch keine Bewertungen
- General Consent Form English 29-IV-09Dokument3 SeitenGeneral Consent Form English 29-IV-09rubenguzNoch keine Bewertungen
- Obstetric Assessment ToolDokument5 SeitenObstetric Assessment ToolDudil GoatNoch keine Bewertungen
- Physical Assessment FormDokument5 SeitenPhysical Assessment FormJo MaldonadoNoch keine Bewertungen
- Pediatric Assessment (1 - 12)Dokument11 SeitenPediatric Assessment (1 - 12)Rose Ann Salanap80% (5)
- Cagayan de Oro City College of Nursing Assessment FormDokument12 SeitenCagayan de Oro City College of Nursing Assessment Formsticdo_nursing2011Noch keine Bewertungen
- New Assessment Form 2Dokument5 SeitenNew Assessment Form 2api-3739910100% (2)
- Med Surg Pico-2Dokument11 SeitenMed Surg Pico-2Jason Kennedy100% (1)
- Pediatric Fluid and Electrolyte TherapyDokument8 SeitenPediatric Fluid and Electrolyte TherapyWildan Wisnu WardayaNoch keine Bewertungen
- Infection Control Self Assessment Tool Complete Set FinalDokument248 SeitenInfection Control Self Assessment Tool Complete Set FinalAndy Molina100% (1)
- Heparin Drip - PortfolioDokument20 SeitenHeparin Drip - Portfolioapi-306657745100% (1)
- Admission and DischargeDokument3 SeitenAdmission and DischargePhilip Jay Braga100% (1)
- Emergency Department Handbook PDFDokument461 SeitenEmergency Department Handbook PDFdmallozziNoch keine Bewertungen
- Medication Errors Paper 2019Dokument6 SeitenMedication Errors Paper 2019api-485472556100% (1)
- Template For Morning Rounds Patient PresentationDokument2 SeitenTemplate For Morning Rounds Patient Presentationwow321Noch keine Bewertungen
- Chapter 2Dokument3 SeitenChapter 2aznknight323Noch keine Bewertungen
- General Nursing Assessment FormDokument2 SeitenGeneral Nursing Assessment FormMarites BarnidoNoch keine Bewertungen
- Assessment of An ICU PatientDokument71 SeitenAssessment of An ICU PatientTito Tesfaye100% (1)
- Skills Checklist-Critical CareDokument3 SeitenSkills Checklist-Critical CareRom Anog100% (4)
- Medication Administration Case Study 1Dokument2 SeitenMedication Administration Case Study 1Lamirah ThomasNoch keine Bewertungen
- Responding To A Code BlueDokument33 SeitenResponding To A Code Blueamanrup randhawaNoch keine Bewertungen
- Medication AdministrationDokument1 SeiteMedication AdministrationJery JsNoch keine Bewertungen
- Pretest IV TherapyDokument3 SeitenPretest IV TherapyMeranda Martin0% (2)
- History Taking Form in Gynecology Obstetrics - CompressDokument8 SeitenHistory Taking Form in Gynecology Obstetrics - CompresskeightNoch keine Bewertungen
- Trauma Case Studies: Teamwork Leading To Great SavesDokument46 SeitenTrauma Case Studies: Teamwork Leading To Great SavesBrett DoddNoch keine Bewertungen
- 10 Infectious DiseaseDokument42 Seiten10 Infectious Diseaseandirio7486Noch keine Bewertungen
- Float Pool - Orientation - RN Critical Care Competency ChecklistDokument19 SeitenFloat Pool - Orientation - RN Critical Care Competency Checklistpurwadis100% (2)
- LWW BATES 03 Head To Toe Child Transcript FINALDokument12 SeitenLWW BATES 03 Head To Toe Child Transcript FINALfrank garrettNoch keine Bewertungen
- Minutes Infection Control Committee Mar 08Dokument5 SeitenMinutes Infection Control Committee Mar 08Czarina Guinto100% (1)
- Oncology Skills ChecklistDokument7 SeitenOncology Skills Checklistnorthweststaffing100% (2)
- NCM 107 Rle: Indication of Use) : Name, Dose, Timing, Route Indication ObjectiveDokument5 SeitenNCM 107 Rle: Indication of Use) : Name, Dose, Timing, Route Indication ObjectiveDud AccNoch keine Bewertungen
- General Nursing Departmental ManualDokument532 SeitenGeneral Nursing Departmental Manualarahman16850% (2)
- Importance of Effective Clinical Documentation by Medical Doctors To Patient Care Management in Federal Teaching Hospital, Ido Ekiti, Ekiti State, NigeriaDokument9 SeitenImportance of Effective Clinical Documentation by Medical Doctors To Patient Care Management in Federal Teaching Hospital, Ido Ekiti, Ekiti State, NigeriaInternational Journal of Innovative Science and Research Technology100% (1)
- Clinical ExemplarDokument4 SeitenClinical Exemplarapi-272451466Noch keine Bewertungen
- Sample Three: Physician and Hospital ContractDokument12 SeitenSample Three: Physician and Hospital ContractMario Lopez100% (1)
- Critical Care - ICU Skills ChecklistDokument2 SeitenCritical Care - ICU Skills ChecklistRandi Brown0% (1)
- Picot ProposalDokument6 SeitenPicot Proposalapi-282602935100% (3)
- Pilot Project ReportDokument26 SeitenPilot Project ReportInclusionNorthNoch keine Bewertungen
- Utilization Review RNDokument2 SeitenUtilization Review RNapi-121451258Noch keine Bewertungen
- Medication Administration SDokument3 SeitenMedication Administration SHannah Naki MedinaNoch keine Bewertungen
- Patient A KARDEX 1Dokument2 SeitenPatient A KARDEX 1Franz Patrick Legria, CPAC - SNNoch keine Bewertungen
- NU 260-Pediatric Assessment FormDokument3 SeitenNU 260-Pediatric Assessment FormMarie Holder67% (6)
- OBGYN History FormDokument2 SeitenOBGYN History FormSandeep GhosthNoch keine Bewertungen
- Bedside Nurse: Name of Student: Jela Mae V. Pates Score: - /25Dokument8 SeitenBedside Nurse: Name of Student: Jela Mae V. Pates Score: - /25janna mae patriarcaNoch keine Bewertungen
- Adult Assessment Tool 2014Dokument8 SeitenAdult Assessment Tool 2014Charm PradoNoch keine Bewertungen
- Clinical Evaluation Tool 432Dokument9 SeitenClinical Evaluation Tool 432api-470941612100% (1)
- Digestive System-Presentation PDFDokument149 SeitenDigestive System-Presentation PDFAgnieszka WaligóraNoch keine Bewertungen
- Code of Professional Conduct and EthicsDokument36 SeitenCode of Professional Conduct and EthicsAgnieszka Waligóra100% (1)
- NHS LA - Duty of Candour 2014 - SlidesDokument10 SeitenNHS LA - Duty of Candour 2014 - SlidesAgnieszka WaligóraNoch keine Bewertungen
- Taking Adult Patient BP Read NPSDokument9 SeitenTaking Adult Patient BP Read NPSAgnieszka WaligóraNoch keine Bewertungen
- BuccalMidazolamTraining PDFDokument21 SeitenBuccalMidazolamTraining PDFAgnieszka WaligóraNoch keine Bewertungen
- Advice For EmployersDokument24 SeitenAdvice For EmployersAgnieszka WaligóraNoch keine Bewertungen
- Buccal Midazolam CEWT Pi MidazDokument2 SeitenBuccal Midazolam CEWT Pi MidazAgnieszka WaligóraNoch keine Bewertungen
- 6 Moving and Positioning WorkbookDokument30 Seiten6 Moving and Positioning WorkbookAgnieszka WaligóraNoch keine Bewertungen
- Good Practice Guidance 4. Expiry Dates For MedicationDokument5 SeitenGood Practice Guidance 4. Expiry Dates For MedicationAgnieszka WaligóraNoch keine Bewertungen
- Crew Role Description PDFDokument1 SeiteCrew Role Description PDFAgnieszka WaligóraNoch keine Bewertungen
- NMC Standards For Competence For Registered NursesDokument21 SeitenNMC Standards For Competence For Registered NursesAgnieszka WaligóraNoch keine Bewertungen
- Falls Pathway V 1.6 2Dokument2 SeitenFalls Pathway V 1.6 2Agnieszka WaligóraNoch keine Bewertungen
- CS Chapter032Dokument1 SeiteCS Chapter032Agnieszka WaligóraNoch keine Bewertungen
- Missing Patients ProcedureDokument16 SeitenMissing Patients ProcedureAgnieszka WaligóraNoch keine Bewertungen
- Crew Role DescriptionDokument1 SeiteCrew Role DescriptionAgnieszka WaligóraNoch keine Bewertungen
- Learning Disability Bite SizeDokument9 SeitenLearning Disability Bite SizeAgnieszka WaligóraNoch keine Bewertungen
- Safeguarding Alerts PolicyDokument16 SeitenSafeguarding Alerts PolicyAgnieszka WaligóraNoch keine Bewertungen
- English For Medical Students PDFDokument130 SeitenEnglish For Medical Students PDFAgnieszka WaligóraNoch keine Bewertungen
- Community Nursing ProcessDokument10 SeitenCommunity Nursing Processbuhari rabiuNoch keine Bewertungen
- CryptosporidiumDokument2 SeitenCryptosporidiumViktri MusicNoch keine Bewertungen
- HayalllDokument41 SeitenHayalllchalie tarekegnNoch keine Bewertungen
- Negative Impact of Social Media: A Qualitative Inquiry Towards Student of Arellano University Jose Rizal CampusDokument30 SeitenNegative Impact of Social Media: A Qualitative Inquiry Towards Student of Arellano University Jose Rizal Campusisabel ysaNoch keine Bewertungen
- Collection of Biological Samples in Forensic ToxicologyDokument16 SeitenCollection of Biological Samples in Forensic ToxicologyAbdulazizNoch keine Bewertungen
- Anaphylactic Shock Treatment KitDokument2 SeitenAnaphylactic Shock Treatment KitSurya DilaNoch keine Bewertungen
- Carmen Best Background InformationDokument15 SeitenCarmen Best Background InformationKING 5 NewsNoch keine Bewertungen
- Sexually Transmitted Diseases in MalesDokument15 SeitenSexually Transmitted Diseases in MalesSam Raven AndresNoch keine Bewertungen
- Reading Comprehension - Food FrightDokument4 SeitenReading Comprehension - Food FrightStephanie RetamarNoch keine Bewertungen
- IbmsbrochureDokument36 SeitenIbmsbrochureadipoliachayan52350% (1)
- Multigrade Lesson Plan in English3Dokument13 SeitenMultigrade Lesson Plan in English3Nick Bantolo100% (11)
- Laboratory Diagnosis of Bacterial Gastroenteritis: Romney M. Humphries, Andrea J. LinscottDokument29 SeitenLaboratory Diagnosis of Bacterial Gastroenteritis: Romney M. Humphries, Andrea J. LinscottFatah Jati PNoch keine Bewertungen
- NOFRNCompetencies Updated March2016 PDFDokument63 SeitenNOFRNCompetencies Updated March2016 PDFamandeep kaurNoch keine Bewertungen
- Distinguishes Aerobic From MuscleDokument2 SeitenDistinguishes Aerobic From MuscleVolley PilgrimsNoch keine Bewertungen
- Integrating Medicinal Plant Diversity in Post-COVID Uganda For Holistic Healthcare ManagementDokument10 SeitenIntegrating Medicinal Plant Diversity in Post-COVID Uganda For Holistic Healthcare ManagementKIU PUBLICATION AND EXTENSIONNoch keine Bewertungen
- Functional Motor AssessmentDokument5 SeitenFunctional Motor AssessmentLoren EstefanNoch keine Bewertungen
- ICAM Dog Population ManagementDokument24 SeitenICAM Dog Population ManagementJasmina SevicNoch keine Bewertungen
- Food Power For AthletesDokument3 SeitenFood Power For AthletesVegan Future100% (1)
- Mcqs - Obstetrics and Gynaecology (For Post Graduate Preparing For FNB and Professionals) Obstetrics and GynaecologyDokument27 SeitenMcqs - Obstetrics and Gynaecology (For Post Graduate Preparing For FNB and Professionals) Obstetrics and GynaecologyAnonymous kQCQ30Rq5ONoch keine Bewertungen
- Metabical CBDokument31 SeitenMetabical CBKumar AbhishekNoch keine Bewertungen
- Know Diabetes For No Diabetes: DR U.S Shilpi M.D, (Physician) BhelhospitalDokument37 SeitenKnow Diabetes For No Diabetes: DR U.S Shilpi M.D, (Physician) BhelhospitalAnonymous ysrxggk21cNoch keine Bewertungen
- Minimal Invasive Dentistry: Review ArticleDokument4 SeitenMinimal Invasive Dentistry: Review ArticleKarissa NavitaNoch keine Bewertungen
- Borrescio-Higa Valenzuela - Gender Inequality and Mental Health.Dokument9 SeitenBorrescio-Higa Valenzuela - Gender Inequality and Mental Health.Firdaus Silabi Al-AttarNoch keine Bewertungen
- Literature ReviewDokument3 SeitenLiterature Reviewapi-609233193Noch keine Bewertungen
- PMFIAS CA 2019 05 12 SciDokument107 SeitenPMFIAS CA 2019 05 12 SciShivy SwarnkarNoch keine Bewertungen
- Ultrasonido en El Paciente Crítico Daniel Lichtenstein PDFDokument33 SeitenUltrasonido en El Paciente Crítico Daniel Lichtenstein PDFVallejo Romo Alberto CristianNoch keine Bewertungen
- A2 1021V en Bowen w7Dokument47 SeitenA2 1021V en Bowen w7Gareth GriffithsNoch keine Bewertungen
- R.A. No. 6969 - Brown GroupDokument35 SeitenR.A. No. 6969 - Brown GroupAngelNoch keine Bewertungen
- 4TH Grading Gateway DrugsDokument84 Seiten4TH Grading Gateway DrugsMirela CalubayanNoch keine Bewertungen
- Community Health Nursing (Learning Feedback Diary (LFD #23)Dokument2 SeitenCommunity Health Nursing (Learning Feedback Diary (LFD #23)Angelica Malacay RevilNoch keine Bewertungen