Beruflich Dokumente
Kultur Dokumente
Oral Surgery Final Exam: Study Online at
Hochgeladen von
okibreazyOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Oral Surgery Final Exam: Study Online at
Hochgeladen von
okibreazyCopyright:
Verfügbare Formate
Oral Surgery Final Exam
Study online at quizlet.com/_21locw
1.
2.
3.
4.
5.
6.
7.
8.
9.
apicoectomy: removal of apical 2-4mm of root
20.
apical curretage: removal by scraping of pathology from above
a root
retrograde restoration: filling apical aspect of root canal to
obtain sealage
21.
what is the first step to take in all emergencies?: stop the
procedure and monitor vital signs
hyperventilation: increase in rate and depth of breathing,
triggered by change in oxygen/CO2 balance, exhaling too much
CO2 causes anxiety which causes them to breathe even deeper
(its a cycle)
at what level of blood glucose can hypoglycemia be defined
as?: less than or equal to 60mg/dL
syncope: sudden and brief loss of consciousness due to
decreased oxygenation or glucose to the brain
how does BTA work?: being a dichain molecule, the heavy
chain binds selectively to the neurotoxin to the cholinergic
nerve terminals, the light chain prevents acetylcholine release,
inhibition of acetylcholine activity yield muscular paralysis
dynamic rhytides: occur in areas of dynamic motion, this is
where botulinum can improve wrinkling (glabellar, lateral
canthal, upper nasal, horizontal forehead, for example), can
also use for assymetric eyebrows
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
22.
23.
24.
25.
26.
27.
contraindications to botox: pregnancy/lactation,
neuromuscular disorders, those taking amino glycosides should
lower botox dosage
alternative uses for botox therapy: migraines,
hypersialorrhea, hyperhidrosis
hyaluronic acid: main component of fillers, HA serves as
ground substance of dermis/fascia, usually broken down in two
days but cross linking them makes them stronger and harder to
breakdown (6-8months)
28.
29.
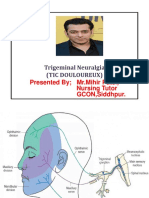
trigeminal neuralgia: sever, unilateral, more frequently
mandibular or maxillary branch (instead of ophthalmic), usually
>50yo, can be blocked by LA, more likely in multiple sclerosis pts
drug treatments for Trigem neuralgia: dilantin, tegretol,
baclofen, conazepam, neurontin
procedures for trigem neuralgia: peripheral neurectomy,
alcohol block/glycerol injection, janetta procedure, gamma knife
radiation
janetta procedure: only procedure that grants complete pain
relief without sensory loss, microvascular decompression
gamma knife radiation: ablation of benign or vascular lesion
that is etiologic towards the neuralgia
etiology of trigem neuralgia: most commonly a benign
neoplasm pushing on the nerve, aberrant artery pushing on
the nerve
glossopharyngeal neuralgia: very similar to trigem neuralgia,
pain occurs on posterior third of tongue and pharynx, may
avoid pain by not swallowing (drooling)
30.
31.
32.
33.
34.
sphenopalatine neuralgia: aka pterygopalatine neuralgia,
unilateral pain in area of sphenopalatine ganglion, this is a
longer lasting neuralgia (avg 20 minutes) unlike other
neuralgias, not confined to older aged patients
cluster headaches: unilateral headaches with orbital or
intraoral pain, occur periodically, with active period interrupted
by spontaneous remissions, affects men more frequently, s/s
include red conjunctiva, lacrimation, nasal congestion,
rinorrhea, and ptosis (all ipsilateral to the pain)
postherpetic neuralgia: occurs following herpes zoster
infection in older patients, pain occurs for more than a month
after onset of zoster eruption, usually involves CNV3, unilateral
neuritis: inflammation of a nerve, most dental pain can be
defined this way, pulpal or PDL pain
hypesthesia: decreased sensation, could be malignancy or
osteomyelitis
paresthesia: dysfunction/perversion of sensation (pins and
needles), could be malignancy or osteomyelitis
referred pain: pain originates in one area and is felt by a
patient in a nearby area, never crosses midline (usually
vertical), as sensory nerves progress centrally there is "crosstalk" when they meet
bells palsy: unilateral, idiopathic, ipsilateral facial paralysis, CNV
travels the longest distance and it is through a bony canal
making any inflammation prone to disruption, corneal abrasion,
ulceration, and blindness can occur due to inability to close eye
supratentorial mass: a mass located above the tentorium
cerebelli, increased intracranial pressure, cerebral edema,
destruction of surrounding tissue, personality and cognitive
changes, headaches (most common), seizures, papilledema
characteristics of radiation and neoplastic cells: the faster
the cellular turnover the more susceptible that tissue is to
radiation damage, therefore neoplastic cells are (relatively)
selectively destroyed, while normal tissues with rapid turnover
are also affected (heme, epithelial, endothelial cells)
initial effects of radiation on oral mucosa: erythema->mucositis w/o ulceration-->pain/dysphagia and loss of taste,
nutrition intake is difficult
evaluation of dentition before radiotherapy: extract all
questionable/poor prognosis teeth, increase patient's dental
awareness and enforce oral hygiene, weekly recall, antifungals
if candida occurs
how to extract before radiotherapy: atraumatic exodontia,
primary closure, usually surgical (flap), prophylactic antibiotics,
need to extract 3wks prior min 2 wks
impacted third molar removal prior to radiation: partially
erupted third molars need to be removed
hyperbaric oxygen for extractions, before and after
radiation: improves angiogenesis, bone metabolism, and bone
turnover, 20 "dives" of HBO (5days/week), 10 dives
postoperatively
35.
36.
37.
38.
39.
40.
41.
implants in irradiated patients: radiation associated with less implant survival in mandibular bone; prolonged time for
osseointegration, HBO can help, even though survival is lower the implants are still a good option
stage I of ORN treatment: 30 sessions of HBO
necrotic bone removal
10 more sessions of HBO
stage II of ORN treatment: patients didn't respond to stage I, large resection of bone and ten more sessions of HBO
stage III of ORN treatment: patients didn't respond to stage II/pathologic fracture, more resection of bone and large reconstruction
surgeries
what is the limit of WBC and platelet count in regards to dental procedures?: the patient must have a WBC count of at least
2,000mm3 and a platelet count of at least 50,000mm3
three characteristics present in order to diagnose MRONJ: current/previous tx with antiresorption or antiangiogenic agents, exposed
bone or probable bone (through fistula) that lasts for eight weeks, and no history of radiation to head and neck (or no obvious
metastasis)
why are the jaw bones so susceptible to MRONJ (mandible more)?: it is under constant remodeling, is a non-sterile environment, and
is more likely to be traumatized
42.
in Wilke's classification, where do most patients with TMD fall under?: usually class III or IV
43.
of the systemic arthritic conditions, which is the most common to cause TMD?: rheumatoid arthritis
44.
intracapsular ankylosis: infratemporal fossa is fused to condyle
45.
extracapsular akylosis: coronoid process interferes with interior of zygomatic process
46.
which seizures do you not see loss of consciousness?: simple (has aura) and absence
47.
whats the dose of benadryl for a mild hypersensitivity?: 50mg
48.
whats the dose for aspirin for an acute MI?: 325mg, non-enteric coated, tell patient to chew and swallow
49.
50.
what are the steps for a patient having an MI?: stop procedure, give oxygen, pulse oximetry, nitroglycerin sublingual (0.4mg), monitor
vitals
which areas hs botox been FDA approved for?: glabellar rhytides and crows feet (in the middle and on the outside of the eyes)
Das könnte Ihnen auch gefallen
- Middle Meatal AntrostomyDokument2 SeitenMiddle Meatal AntrostomymajidjankakakhelNoch keine Bewertungen
- Atlas of Surgical Therapy for Migraine and Tension-Type HeadacheVon EverandAtlas of Surgical Therapy for Migraine and Tension-Type HeadacheEdoardo RaposioNoch keine Bewertungen
- Craniotomy ADokument38 SeitenCraniotomy Awam.ahNoch keine Bewertungen
- Dislocation of the Temporomandibular Joint: A Guide to Diagnosis and ManagementVon EverandDislocation of the Temporomandibular Joint: A Guide to Diagnosis and ManagementNigel Shaun MatthewsNoch keine Bewertungen
- Reasons For TonsillectomyDokument8 SeitenReasons For TonsillectomyRasdumi100% (1)
- All Pulkit NotesDokument915 SeitenAll Pulkit Notesadham bani younesNoch keine Bewertungen
- All Previous Essay SurgeryDokument170 SeitenAll Previous Essay Surgeryalsfyabdullah2021Noch keine Bewertungen
- 5.nervous System PDFDokument88 Seiten5.nervous System PDFMelancholy MedicineNoch keine Bewertungen
- Temporal ArteritisDokument3 SeitenTemporal Arteritisfire_n_iceNoch keine Bewertungen
- Orthopedic EmergenciesDokument63 SeitenOrthopedic EmergenciesNasser AlQadhibNoch keine Bewertungen
- Complication Complications of SinusitisDokument4 SeitenComplication Complications of SinusitisIvan DarioNoch keine Bewertungen
- Paul Healey Trab ChapterDokument13 SeitenPaul Healey Trab ChapterPushpa RamanNoch keine Bewertungen
- Complications of OMDokument77 SeitenComplications of OMfahmimiraNoch keine Bewertungen
- Disorders of The EyeDokument16 SeitenDisorders of The Eyelisette_sakuraNoch keine Bewertungen
- Neurological Disturbances of FaceDokument33 SeitenNeurological Disturbances of FaceDrMuskan AroraNoch keine Bewertungen
- Trauma: Accidental Temporal Bone Fractures Classification SchemesDokument12 SeitenTrauma: Accidental Temporal Bone Fractures Classification SchemesDr-Firas Nayf Al-ThawabiaNoch keine Bewertungen
- Cerebrovascular DiseaseDokument13 SeitenCerebrovascular DiseasebobtagubaNoch keine Bewertungen
- ENT Quick ReviewDokument6 SeitenENT Quick ReviewWade100% (1)
- Laryngeal Trauma 20080722Dokument44 SeitenLaryngeal Trauma 20080722IchsanJuliansyahNoch keine Bewertungen
- Ïv V V V V Ïv V V V VDokument3 SeitenÏv V V V V Ïv V V V VSelina WijayaNoch keine Bewertungen
- Aracnoditis PDFDokument18 SeitenAracnoditis PDFArockia Albert JerosonNoch keine Bewertungen
- Orthopaedic Surgery Study Guide FOR Medical Students, R1S and R2SDokument17 SeitenOrthopaedic Surgery Study Guide FOR Medical Students, R1S and R2SlanghalilafaNoch keine Bewertungen
- Eyelids, Lacrimal Apparatus and Orbit: Yonas Abraham, M.DDokument43 SeitenEyelids, Lacrimal Apparatus and Orbit: Yonas Abraham, M.DTemie EshetNoch keine Bewertungen
- Head Injury 2: (DR Mohamed A. J. Al Tamimi)Dokument10 SeitenHead Injury 2: (DR Mohamed A. J. Al Tamimi)AmmarNoch keine Bewertungen
- Functional Endoscopic Sinus SurgeryDokument3 SeitenFunctional Endoscopic Sinus SurgeryDanielicah CruzNoch keine Bewertungen
- Pre OpDokument7 SeitenPre OpSuci ZahraniNoch keine Bewertungen
- Trigeminal Neuralgia Oral SurgeryDokument48 SeitenTrigeminal Neuralgia Oral SurgeryFourthMolar.com67% (3)
- Radiotherapy in Management of Head and Neck CancerDokument51 SeitenRadiotherapy in Management of Head and Neck CancerKassim OboghenaNoch keine Bewertungen
- Cholesteatoma: Hazardous Condition of The and Destruction, Which Result TheDokument4 SeitenCholesteatoma: Hazardous Condition of The and Destruction, Which Result TheCondurache Ilie-AndreiNoch keine Bewertungen
- Diseases of External EarDokument19 SeitenDiseases of External EarMohamed Khaled TahaNoch keine Bewertungen
- Dental Management of The Patient Undergoing Radiotherapy or ChemoterapyDokument43 SeitenDental Management of The Patient Undergoing Radiotherapy or ChemoterapyJenadi Binarto100% (1)
- Trigeminal Neuralgia and Its Management: Data Supplement ReferencesDokument6 SeitenTrigeminal Neuralgia and Its Management: Data Supplement ReferencesfendiNoch keine Bewertungen
- Objective - SURGERYDokument54 SeitenObjective - SURGERYlaraNoch keine Bewertungen
- Meniere DiseaseDokument16 SeitenMeniere DiseaseNavjot Brar100% (2)
- HNN Ear SGDDokument23 SeitenHNN Ear SGDLauren LLNoch keine Bewertungen
- AMPUTATIONDokument73 SeitenAMPUTATIONmohammad farhanNoch keine Bewertungen
- Anesthesia For Opthalmological SurgeriesDokument69 SeitenAnesthesia For Opthalmological SurgeriesRajesh MunigialNoch keine Bewertungen
- Trigeminal NeuralgiaDokument15 SeitenTrigeminal NeuralgiaMihir Patel75% (4)
- Tetanus (Clostridium Tetani)Dokument29 SeitenTetanus (Clostridium Tetani)ped medNoch keine Bewertungen
- Peripheral Nerve BlocksDokument4 SeitenPeripheral Nerve Blocksakif48266Noch keine Bewertungen
- Thromboangiitis Obliterans Buergers Disease)Dokument30 SeitenThromboangiitis Obliterans Buergers Disease)drvsvasuNoch keine Bewertungen
- Microvascular Decompression For Trigeminal Neuralgia: Technical Refinement For Complication AvoidanceDokument6 SeitenMicrovascular Decompression For Trigeminal Neuralgia: Technical Refinement For Complication AvoidancefespositoNoch keine Bewertungen
- Trigeminal Neuralgia: Dr. Deepthi AthuluruDokument69 SeitenTrigeminal Neuralgia: Dr. Deepthi AthuluruLakshya NainNoch keine Bewertungen
- OMFS Prometric PDFDokument29 SeitenOMFS Prometric PDFMohammed Qasim Al-Watary67% (3)
- Ent ExamDokument5 SeitenEnt ExamShanon LimNoch keine Bewertungen
- Complications of Parotid SurgeryDokument22 SeitenComplications of Parotid SurgeryAsline JesicaNoch keine Bewertungen
- Eye & ENTDokument12 SeitenEye & ENTShandar SadafNoch keine Bewertungen
- Untitled PresentationDokument41 SeitenUntitled PresentationOmar KojerNoch keine Bewertungen
- Medical and Surgical ProcedureDokument13 SeitenMedical and Surgical Procedureprathamesh patilNoch keine Bewertungen
- 2 Lez I One MedicinaDokument44 Seiten2 Lez I One MedicinaAntonio MoscarielloNoch keine Bewertungen
- EOP AssessmentDokument13 SeitenEOP AssessmentNuruliznie RosezaideeNoch keine Bewertungen
- Questions 1 - 100Dokument15 SeitenQuestions 1 - 100Vicky Cezar Villanueva50% (2)
- Oral SurgeryDokument52 SeitenOral Surgerykhaled alahmadNoch keine Bewertungen
- Sub-Tenon's Anaesthesia For Ophthalmic ProceduresDokument5 SeitenSub-Tenon's Anaesthesia For Ophthalmic ProceduresKarthikNoch keine Bewertungen
- ANESTHESIA For VASCULAR SURGERY - mw05 2003-2Dokument77 SeitenANESTHESIA For VASCULAR SURGERY - mw05 2003-2Muhammad Umer SaeedNoch keine Bewertungen
- Trigeminal Neuralgia (Tic Douloureux) : Presented by MR - Mihir Patel, Nursing Tutor GCON, SiddhpurDokument15 SeitenTrigeminal Neuralgia (Tic Douloureux) : Presented by MR - Mihir Patel, Nursing Tutor GCON, Siddhpurandreas kevinNoch keine Bewertungen
- AAO Network OculoplasticsDokument53 SeitenAAO Network OculoplasticsSafa Abdualrahaman Ali HamadNoch keine Bewertungen
- AAO MCQ Recent Web PDFDokument510 SeitenAAO MCQ Recent Web PDFNoorNoch keine Bewertungen
- Orbital CellulitisDokument21 SeitenOrbital CellulitisElsa Octavia100% (1)
- Assessment of The Esthetic Smile in Young Japanese Women: Research PaperDokument9 SeitenAssessment of The Esthetic Smile in Young Japanese Women: Research PaperokibreazyNoch keine Bewertungen
- U.S. Powerboating Class: Saturday & Sunday August 26 & 27 or September 16 & 17Dokument4 SeitenU.S. Powerboating Class: Saturday & Sunday August 26 & 27 or September 16 & 17okibreazyNoch keine Bewertungen
- Maxillary Blocks: Block Area Affected Needle Depth Landmark and Orientation ImageDokument2 SeitenMaxillary Blocks: Block Area Affected Needle Depth Landmark and Orientation ImageokibreazyNoch keine Bewertungen
- Coco - Remember MeDokument1 SeiteCoco - Remember MeokibreazyNoch keine Bewertungen
- Army Strategic Language List DTD 18 Jan 19Dokument5 SeitenArmy Strategic Language List DTD 18 Jan 19okibreazyNoch keine Bewertungen
- Jazz Guitar CurriculumDokument3 SeitenJazz Guitar CurriculumokibreazyNoch keine Bewertungen
- Diabetes Mellitus in The US:: PrevalenceDokument48 SeitenDiabetes Mellitus in The US:: PrevalenceokibreazyNoch keine Bewertungen
- LP6 Guitar Scales SystemDokument29 SeitenLP6 Guitar Scales SystemokibreazyNoch keine Bewertungen
- Analysis of Misty (Errol Garner)Dokument4 SeitenAnalysis of Misty (Errol Garner)okibreazyNoch keine Bewertungen
- A Better Affirmative ActionDokument76 SeitenA Better Affirmative ActionokibreazyNoch keine Bewertungen
- OMF PathologyDokument12 SeitenOMF PathologyokibreazyNoch keine Bewertungen
- Whitening TraysDokument68 SeitenWhitening TraysokibreazyNoch keine Bewertungen
- CPR Aha Written ExamDokument4 SeitenCPR Aha Written Examokibreazy100% (3)
- Guitar Scales PentatonicDokument1 SeiteGuitar Scales PentatonicokibreazyNoch keine Bewertungen
- Principles of Panoramic RadiographsDokument52 SeitenPrinciples of Panoramic RadiographsokibreazyNoch keine Bewertungen
- Pharmacology Crossword PuzzleDokument3 SeitenPharmacology Crossword Puzzleokibreazy100% (2)
- Emergency Medicine SummaryDokument4 SeitenEmergency Medicine SummaryokibreazyNoch keine Bewertungen
- Short HaikuDokument1 SeiteShort HaikuokibreazyNoch keine Bewertungen
- Ultrasone Hfi Pro DJDokument6 SeitenUltrasone Hfi Pro DJokibreazy100% (1)
- Siren Suicides: Second EditionDokument298 SeitenSiren Suicides: Second EditionKsenia AnskeNoch keine Bewertungen
- Amino AcidsDokument18 SeitenAmino AcidsShreesh MohanNoch keine Bewertungen
- Allergy Genu Ection? It's Surmount With Special Focus On Ear, Nose and ThroatDokument11 SeitenAllergy Genu Ection? It's Surmount With Special Focus On Ear, Nose and ThroatAna BrankovićNoch keine Bewertungen
- Laboratory Result Proteolytic EnzymeDokument2 SeitenLaboratory Result Proteolytic EnzymeWinter SnowNoch keine Bewertungen
- Pink Salt BenifitsDokument12 SeitenPink Salt BenifitsakhtarNoch keine Bewertungen
- Anatomy & Physiology of Farm Animals: By: Eddie C. Bautista Jr. DVM, MSADokument221 SeitenAnatomy & Physiology of Farm Animals: By: Eddie C. Bautista Jr. DVM, MSAJayson BasiagNoch keine Bewertungen
- 10 Current Research Articles Related To Our SystemDokument11 Seiten10 Current Research Articles Related To Our Systemhomework solutionNoch keine Bewertungen
- Ki Breathing TranslationDokument52 SeitenKi Breathing TranslationNataly Kur100% (1)
- Cholesterol SynthesisDokument19 SeitenCholesterol Synthesisbrian mgabiNoch keine Bewertungen
- Reproduction of Prokaryotic CellDokument29 SeitenReproduction of Prokaryotic CellNurrazanahKarmanNoch keine Bewertungen
- The Resveratrol StoryDokument7 SeitenThe Resveratrol StoryCliusNoch keine Bewertungen
- BSC2011 Study Guide DouglasDokument7 SeitenBSC2011 Study Guide DouglasPetey 书维 ChangNoch keine Bewertungen
- Lecture 2 Tooth Eruption and SheddingDokument35 SeitenLecture 2 Tooth Eruption and SheddingAMIT GUPTANoch keine Bewertungen
- Bhatia LMRP Neetpgsurgeonpdf PDF FreeDokument288 SeitenBhatia LMRP Neetpgsurgeonpdf PDF FreedgraghavNoch keine Bewertungen
- Reticulocyte - Wikipedia, The Free EncyclopediaDokument2 SeitenReticulocyte - Wikipedia, The Free EncyclopediaAniket MittalNoch keine Bewertungen
- Resusitasi Pada AnakDokument43 SeitenResusitasi Pada AnakSondang Herikson PanjaitanNoch keine Bewertungen
- Handbook of Pediatric Eye and Systemic Disease PDFDokument650 SeitenHandbook of Pediatric Eye and Systemic Disease PDFBangun Said SantosoNoch keine Bewertungen
- European Journal Nutrition Curcumin PDFDokument10 SeitenEuropean Journal Nutrition Curcumin PDFAndres FacuNoch keine Bewertungen
- Fluid, Electrolyte, Acid Base BalanceDokument42 SeitenFluid, Electrolyte, Acid Base BalanceSutrisno YangNoch keine Bewertungen
- Difference of Arterial and Venous InsufficiencyDokument6 SeitenDifference of Arterial and Venous InsufficiencyBeep TerradoNoch keine Bewertungen
- Wedel PDFDokument120 SeitenWedel PDFAbhishek VermaNoch keine Bewertungen
- RLE 001-Assessment FormDokument7 SeitenRLE 001-Assessment FormArnzz AgbulosNoch keine Bewertungen
- The Structure and Function of The Ear and Its Role in Hearing and Balance1Dokument4 SeitenThe Structure and Function of The Ear and Its Role in Hearing and Balance1Khushbakht QureshiNoch keine Bewertungen
- High-Voltage Pulsed Galvanic Stimulation (HVPGS)Dokument12 SeitenHigh-Voltage Pulsed Galvanic Stimulation (HVPGS)akheel ahammed100% (1)
- Rapid Sterility Testing Using PallchekDokument29 SeitenRapid Sterility Testing Using Pallchekvkumar6883Noch keine Bewertungen
- Introduction To The Body As A WholeDokument29 SeitenIntroduction To The Body As A Wholekhizer hayatNoch keine Bewertungen
- Handout Orthopedic Nursing Assisstive DevicesDokument14 SeitenHandout Orthopedic Nursing Assisstive DevicesPaul Christian P. Santos, RN100% (2)
- ACLS Practice Exam 1Dokument10 SeitenACLS Practice Exam 1Ken Evans87% (15)
- Glycolysis ClickerDokument44 SeitenGlycolysis ClickerDineth GunasekeraNoch keine Bewertungen
- LeavesDokument26 SeitenLeavesRochelle AntigNoch keine Bewertungen
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (34)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDVon EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDBewertung: 5 von 5 Sternen5/5 (4)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Von EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Bewertung: 3 von 5 Sternen3/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsVon EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsBewertung: 4 von 5 Sternen4/5 (4)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 4.5 von 5 Sternen4.5/5 (82)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeVon EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeBewertung: 4.5 von 5 Sternen4.5/5 (254)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsVon EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsBewertung: 4.5 von 5 Sternen4.5/5 (170)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBewertung: 2 von 5 Sternen2/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisVon EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (44)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsVon EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsBewertung: 5 von 5 Sternen5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaVon EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesVon EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesBewertung: 4.5 von 5 Sternen4.5/5 (1412)
- The Comfort of Crows: A Backyard YearVon EverandThe Comfort of Crows: A Backyard YearBewertung: 4.5 von 5 Sternen4.5/5 (23)
- The Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeVon EverandThe Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeBewertung: 4.5 von 5 Sternen4.5/5 (2)
- The Obesity Code: Unlocking the Secrets of Weight LossVon EverandThe Obesity Code: Unlocking the Secrets of Weight LossBewertung: 4 von 5 Sternen4/5 (6)
- To Explain the World: The Discovery of Modern ScienceVon EverandTo Explain the World: The Discovery of Modern ScienceBewertung: 3.5 von 5 Sternen3.5/5 (51)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Von EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Bewertung: 4.5 von 5 Sternen4.5/5 (110)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisVon EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisBewertung: 3.5 von 5 Sternen3.5/5 (2)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsVon EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNoch keine Bewertungen
- Hearts of Darkness: Serial Killers, The Behavioral Science Unit, and My Life as a Woman in the FBIVon EverandHearts of Darkness: Serial Killers, The Behavioral Science Unit, and My Life as a Woman in the FBIBewertung: 4 von 5 Sternen4/5 (20)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 4.5 von 5 Sternen4.5/5 (6)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryVon EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryBewertung: 4 von 5 Sternen4/5 (46)