Beruflich Dokumente
Kultur Dokumente
Antibacterial Cell Wall and Membrane Inhibitors
Hochgeladen von
cbac1990Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Antibacterial Cell Wall and Membrane Inhibitors
Hochgeladen von
cbac1990Copyright:
Verfügbare Formate
Specific Antibacterial Agents
Lecture by Dr. Delgado
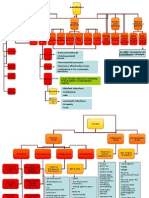
CELL WALL SYNTHESIS/CELL MEMBRANE INHIBITORS
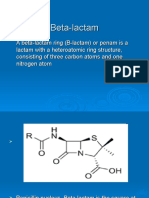
1. BETA LACTAMS
Mechanism of action:
1. Binds with one or more PBPs causing selective inhibition of transpeptidase, carboxypeptidase and
endopeptidase reactions required for cross linkage between peptide chains in the synthesis of
mucopeptide (murein, peptidoglycan)
2. Activates endogenous autolytic enzymes (autolysins and murein hydrolases) in the cell wall leading to
lysis of the bacteria; bactericidal; time dependent antimicrobials.
General mechanism of resistance to penicillins and other beta-lactams:
Inactivation by betalactamases most common
Modification of target PBPs e.g. MRSA, penicillin resistant pneumococci (PRSP) and enterococci
Impaired penetration of drug to PBPs e.g. gram negative organisms
Efflux pump e.g. gram negative organism
Beta-lactams share features of chemistry, mechanism of action, pharmacologic, and immunologic
characteristics:
1.1 PENICILLINS bind primarily with PBP-1 and PBP-3
-Basic structure: 6-aminopenicillanic acid (beta-lactam ring fused with 5-membered thializodine ring)
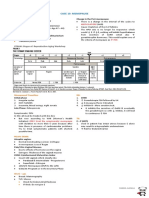
Penicillins (Penicillin
G)
Gram positive cocci
Gram negative
bacilli
Anaerobes
+
except B. fragilis
*Resistant to staphylococcal B-lactamases
Anti- staphylococcal
(Methicillin,
Oxacillin)*
+
except Enterococci
0
0
Extended-spectrum
(Ampicillin,
Piperacillin)
+
+
but limited
+
except B. fragilis
Preparation:
Oral preparation not recommended because acid labile; low bioavailability (30%) even without food
Parenteral
o Short-acting: Penicillin G aqueous (crystalline) sodium
o Repository Form (given IV): Procaine Penicillin G and Benzathine Penicillin G
! Not used for serious infections
Clinical Uses Penicillin G
Drug of choice for infections caused by
o Streptococcus pyogenes (skin and soft tissue infection)
o Susceptible Stretococcus pneumonia
o Non-B-lactamase-producing Staphylococcus aureus
o Enterococcus faecalis (NOT E. faecium)
o Neisseria meningitidis (NOT N. gonorrhoeae)
o Treponema pallidum
o Leptospira spp.
Other uses
o Clostridium tetani
o Actinomyces
Transcribed by: SPCCF B2017
Specific Antibacterial Agents
Lecture by Dr. Delgado
NOT active against Bacteroides fragilis
Clinical Uses Other Penicillins
Procaine and Benzathine Penicillin G
o Streptococcus pyogenes (pharyngitis, prophylaxis for reinfection)
o Treponema pallidum
Penicillin V (Phenoxymethylpenicillin) oral
o Streptococcus pyogenes (pharyngitis)
! Replaced by amoxicillin due to poor oral bioavailability
Clinical Uses Aminopenicillins (not active against P. aeruginosa)
Most active oral B-lactam antibiotics for susceptible Streptococcus pneumonia
Other uses of Ampicillin
o Shigella spp.
o Salmonella typhi (increasing amoxicillin resistance)
o E. coli but NOT other Enterobacteraceae
o Listeria monocytogenes
o Enterococcus faecalis but NOT E. faecium
Other uses of Amoxicillin
o Same with ampicillin
o Has the best oral bioavailability
o Unstable - not good when given IV (give ampicillin instead)
Clinical Uses Carboxypenicillins (Ticarcillin)
Pseudomonas aeruginosa (nosocomial infections)
Compared to aminopenicillins
o Broader coverage against Enterobacteriaceae
o NOT active against Enterococci
Clinical Uses Ureidopenicillins (Piperacillin)
Pseudomonas aeruginosa (nosocomial infections)
o More active than carboxypenicillins
Compared to aminopenicillins
o Broader coverage against Enterobacteriaceae (including Klebsiella spp.)
Compared to carboxypenicillins
o Active against Enterococcus faecalis
Adverse Reactions:
Common
o Hypersensitivity (cross-sensitizing, cross-reacting)
! Due to major determinants: penicilloyl(most important), penicillanic acid derivatives
o Maculopapular rash
! Occurs after 72hrs; not IgE mediated
NOT predicted by skin testing
! Common during infectious mononucleosis (amoxicillin, ampicillin)
o GI disturbances e.g. diarrhea (ampicillin), nausea/vomiting, oral candidiasis
Occasional
o Hematologic disturbances e.g. bleeding due to platelet dysfunction (ticarcillin)
! Due to binding to the adenosine diphosphate receptor site in platelets
o Pseudomembranous colitis (ampicillin)
Rare
o Anaphylactic shock (0.05)
! IgE-mediated
Transcribed by: SPCCF B2017
Specific Antibacterial Agents
Lecture by Dr. Delgado
Due to minor determinants: benzylpenicillin, benzyl penicilloate (acid hydrolysis product)
Use epinephrine
Antihistamine and corticosteroid have NOT been shown to be if benefit
Skin testing recommended for persons with history of penicillin reaction esp. anaphylaxis
4 to 6 fold increase in subsequent reaction
Serum sickness (penicillin G)
! Urticarial, fever, joint swelling, angioneurotic edema, intense pruritus, respiratory distress
! Occurs after 7-12 days
Muscle irritability, seizure (penicillin G)
! Risk factor: renal failure, rapid infusion to those with hyperkalemia and arrhythmia
Hemolytic anemia (penicillin G)
Interstitial nephritis (methicillin)
! Fever, macular rash, eosinophilia, proteinuria, eosinophiluria, hematuria, oliguria "
anuria
Hepatitis (oxacillin)
! REVERSIBLE
Agranulocytosis, neutropenia (nafcillin)
! REVERSIBLE
!
!
!
!
o
o
o
o
o
o
BETA-LACTAMASE INHIBITORS
! Competitive inhibition of many B-lactamases
o Resemble B-lactam molecules; suicide substrate
o Bind irreversibly to the catalytic site of B-lactamases rendering them inactive
! Very weak antibacterial action
Amoxicillin/
Ampicillin
0
Klebsiella
pneumonia
E. coli
+/Proteus sp.
+/Salmonella typhi
+/Acinetobacter
0
baumannii
Pseudomonas
0
aeruginosa
Bacteroides fragilis
0
+ susceptible; +/- variable; 0 resistant
AmoxicillinClavulanic Acid
+
AmpicillinSulbactam
+
+
+
+
0
+
+
+
+
Pharmacokinetics
! CSF penetration is unreliable
o NOT recommended for meningitides
! Coamoxiclav
o IV formulation very unstable
o 125mg (clavulanate) not to exceed TID
o high doses may cause diarrhea
Transcribed by: SPCCF B2017
Specific Antibacterial Agents
Lecture by Dr. Delgado
1.2 CEPHALOSPORINS
Basic structure: 7-aminocephalosporanic acid with antibacterial activity (betalactam ring fused with 6membered dihydrothiazine ring); includes cephamycins; more stable to many betalactamases hence
generally have a broader spectrum of activity than penicillins.
1st Gen
+
2nd Gen
+
3rd Gen
+/-
Gram
positive
cocci
MRSA
0
0
0
Gram
+/+
+
negative
bacilli
Pseumonas
0
0
+/Anaerobes
0
+/+/+ susceptible; +/- variable; 0 resistant
*includes coverage for Enterococcus faecalis NOT E. faecium
Pharmacokinetics Oral
1st Gen
Cephalexin
Cefadroxil
2nd Gen
Cefuroxime
Cefaclor
Cefprozil*
Loracarbef*
4th Gen
+
5th Gen
+*
0
+
+
+
+
0
+/0
3rd Gen
Cefixime
Cefpodoxime
Cefdinir
Cefditoren*
Ceftibuten*
* Not available
Absorption enhanced by ester formulations (axetil, paroxetil)
Very high urine concentration
Tissue levels lower than the serum concentration
Excreted in urine
Pharmacokinetics Intravenous
1st Gen
2nd Gen
Cefazolin
Cefuroxime
Cephamycins
Cefotetan
Cefoxitin
Cefmetazole*
3rd Gen
Ceftriaxone
Ceftazidime
Cefotaxime
Cefoperazone
Ceftizoxime
Ceftibuten*
Moxalactam
4th Gen
Cefepime
Cefpirome
5th Gen*
Ceftaroline
Ceftobiprole
*Not available
Widely distributed in body fluids and tissues (except in the eye, prostate, brain and meninges for 1st and
2nd gen)
Poor intracellular penetration
Excreted in urine except
o Ceftriaxone and Cefoperazone (bile)
Clinical Uses 1st Gen Cephalosporins
Streptococci and Staphylococci (minor skin and soft tissue infection)
Surgical prophylaxis (Cefazolin)
o NOT recommended for colorectal procedure
Transcribed by: SPCCF B2017
Specific Antibacterial Agents
Lecture by Dr. Delgado
E. coli (uncomplicated cystitis)
NOT active against Enterococci, Pseudomonas aeruginosa, and Acinetobacter spp.
Does not cross BBB
Clinical Uses 2nd Gen Cephalosporins
Compared to 1st gen cephalosporins
o Broader coverage against gram-negative organisms [including B-lactamase-producing
Haemophilus influenza, Moraxella catarrhalis, Klebsiella spp. (sinusitis, otitis media, pneumonia,
NOT meningitis)]
Bacteroides fragilis (intraabdominal/pelvic infections cephamycins)
NOT active against Enterococci, Pseudomonas aeruginosa and Acinetobacter spp.
Does not cross BBB
Clinical Uses 3rd Gen Cephalosporins
Drug of choice for meningitis caused by Penicillin-resistant Streptococcus pneumonia (ceftriaxone or
cefotaxime)
Compared to 1st and 2nd gen cephalosporins
o Broader coverage against Enterobacteriaceae [including Citrobacter spp., Serratia marcescens,
Providencia spp. (pneumonia, pyelonephritis)]
Drug of choice for infections caused by
o Neisseria gonorrhea (ceftriaxone)
o MDR Salmonella typhi (ceftriaxone)
Other uses
o Burkholderia cepacia (ceftazidime)
o Bacteroides fragilis (intraabdominal/pelvic infections ceftizoxime)
o NOT active against Enterococci and Acinetobacter spp.
o Some are NOT very active against Staphylococci and Streptococci (cefixime, ceftibuten,
ceftazidime)
o Some do NOT cross blood-brain barrier (cefoperazone with sulbactam and all oral forms)
o Anti-pseudomonal ceftazidime > cefoperazone
Clinical Uses 4th Gen cephalosporins
Compared to 1st to 3rd gen cephalosporins
o Broader coverage against Enterobacteriaceae (including Enterobacte spp.)
Pseudomonas aeruginosa (nosocomial infections)
Not active against Enterococci, Acincetobacter spp. and anaerobes
Clinical uses 5th gen Cephalosporins
MRSA
Streptococci
Enterococcus faecalis
Enterobacteriaceae
(including E. coli, Klebsiella
spp., Enterobacter spp.)
Pseudomonas aeruginosa
Acinetobacter spp.
Anaerobes
*No longer manufactured
Transcribed by: SPCCF B2017
Ceftaroline
+
+
+
+
Ceftobiprole*
+
+
+
+
0
+
0
0
0
0
+ susceptible; 0 resistant
Specific Antibacterial Agents
Lecture by Dr. Delgado
Adverse Reactions:
Common
o GI disturbances e.g. diarrhea (cefoperazone), nausea/vomiting
o Thrombophlebitis
Occasional
o Hypersensitivity
! Cross-allergenicity with penicillins ~5-10%
o Serum sickness-like reactions (cefaclor)
o Bile sludging, pseudocholelithiasis (ceftriaxone)
o Hematologic disturbances e.g. bleeding due to antagonism of Vitamin K (cefamandole,
cefoperazone, cefmetazole, cefotetan)
! Due to methylthiotetrazole (MTT) group
o Disulfiram-like reactions
! Metallic or garlic taste, flushing, tachycardia, sweating, headache, vomiting,
neurotoxicity, hepatitis
! Due to MTT group accumulation of acetaldehyde
Rare
o Anaphylactic shock
! Do NOT give to patients with history of anaphylaxis to penicillins
o Interstitial nephritis and tubular necrosis (cephalotin)
o Pseudomembranous colitis
o Hepatitis
o Seizure
1.3 MONOBACTAM
Aztreonam only monobactam available
Staphylococci
Streptococci
Enterococci
Enterobacteriaceae (including E.
coli, Klebsiella spp., Enterobacter
spp.) NOT ESBLs
Pseudomonas aeruginosa
Acinetobacter spp.
Abaerobes
+ susceptible; +/- variable; 0 resistant
Aztreonam
0
0
0
+
Ceftazidime
0
+/0
+
+
0
0
+
0
+
Only available in intravenous form; poorly absorbed orally
Widely distributed in tissues including inflamed meninges can be given to patients with meningitis
Excreted in the urine
Similar to ceftazidime
o Poor gram + coverage
o Good gram coverage
o Pseudomonas and enterobacteriaceae coverage
Adverse Reactions
Occasional
o Hypersensitivity
! NO cross allergenicity with penicillins
o GI disturbances e.g. nausea/vomiting, diarrhea
o Transaminitis
Transcribed by: SPCCF B2017
Specific Antibacterial Agents
Lecture by Dr. Delgado
o
Rare
o
o
Local reaction e.g. pain at injection site
Hematologic disturbance e.g. thrombocytopenia
Pseudomembranous colitis
1.4 CARBAPENEM betalactam ring is attached to a five-membered ring, substitution of carbon for sulfur and
unsaturation in the five membered ring; low susceptibility to betalactamase; carbapenemase-producing aerobic
gram-negative bacilli increasing
Imipenem
Meropenem
Doripenem
Staphylococci NOT
+
+
+
MRSA
Streptococci
+
+
+
Enterococcus
+
+/+/faecalis NOT E.
faecium
Enterobacteriaceae
+
+
+
(E. coli, Klebsiella
spp., Enterobacter
spp.)
Extended spectrum
+
+
+
B-lactamases
(ESBLs)
Acinetobacter spp.
+
+
+
Pseudomonas
+
+
+*
aeruginosa
Anerobes
+
+
+
*lowest MIC (4ug/mL vs 32 for imipenem and 16 for meropenem)
Ertapenem
+
+
0
+
+
0
0
+
Mechanism of Resistance
NO cross resistance with other B-lactams
NO class resistance
o Imipenem
! OprD efflux pump
o Meropenem, Doripenem, Ertapenem
! MexA-MexB-OprM efflux system
Pharmacokinetics
Intravenous preparation
o Ertapenem may also be given intramuscularly (with 1% lidocaine)
Imipenem inactivated by dehydropeptidases
o Cilastatin prolongs the half-life of imipenem, maintains therapeutic urinary concentration, and
decreases nephrotoxicity
Meropenem, Doripenem and Ertapenem NOT degraded by dehydropeptidases
High urinary concentration
Widely distributed in body fluids and tissues (including inflamed meninges for meropenen and
imipenem)
Excreted in urine
Clinical Uses
Drug of choice for infections caused by
o ESBLs
Transcribed by: SPCCF B2017
Specific Antibacterial Agents
Lecture by Dr. Delgado
o Serious mixed aerobic and anaerobic infections
o Enterobacter spp.
NOT active against MRSA, Enterococci (except imipenem), and Stenotrophomonas maltophilia
Adverse Reactions:
Occasional
o Hypersensitivity (cross sensitizing, cross reacting)
o Hematologic disturbances e.g. anticoagulation abnormalities
o Local reaction e.g. pain at injection site
Rare
o
o
o
o
o
Seizure esp. among renal failure patients
! Most epileptogenic imipenem
Bind with greater affinity with GABA
! Least epileptogenic doripenem
Hallucination (ertapenem)
Anaphylactic shock
Serum sickness
Pseudomembranous colitis
2. GLYCOPEPTIDE
VANCOMYCIN only glycopeptide locally available
MRSA
VRSA
VISA
Streptococci
Enterococcus faecalis
E. faecium
VRE
Gram-negative bacilli
C. difficile
*Available locally
Vancomycin*
+
0
0
+
+
+/0
0
+
Teicoplanin
Televancin
Dalbavancin
+
+
+
0
0
0
0
+
+
+
+
+
+
+
+
+/+
+
0
0
0
0
0
0
+
+
+
+ susceptible; +/- variable; 0 resistant
Mechanism of Action
inhibits cell wall synthesis by binding to the D-Ala-D-Ala terminus
o inhibits transglycosylase (prevents elongation and cross-linking)
Methicillin-resistant S. aureus (MRSA)
o B-lactam antibiotics cannot bind to PBP (altered PBP)
! mecA gene produces PBP2a
o Vancomycin does NOT target PBP
Vancomycin-intermediate S. aureus (VISA)
o Vancomycin unable to reach target site
! Thick peptidoglycan layers that are less completely cross-linked together
! Vancomycin trapped in the cell wall
Pharmacokinetics
Poor oral absorption
o Administered orally only for treatment of C. difficile colitis
Widely distributed in body fluids and tissues (including inflamed meninges)
Transcribed by: SPCCF B2017
Specific Antibacterial Agents
Lecture by Dr. Delgado
o May use intraventricular injection
Excreted in urine
o Check serum trough levels esp. if renal function is unstable
o Trough level should be obtained 30mins prior to the 4th and 5th dose
Time-dependent killing
o Efficacy is directly related to time above MIC, and becomes independent of concentration once
the MIC has been reached
Clinical Uses
Drug of choice fo infection caused by MRSA (including pneumonia, bacteremia and endocarditis)
o Target trough for serious infections: 15-20ug/mL
o NOT recommended for serious S. aureus infection if susceptible to penicillin
Drug of choice for coagulase-negative staphylococci
o Prosthetic device infections, CSF shunt infections, catheter-related infections
Other uses
o Enterococci
o Penicillin-resistant Streptococcus pneumonia (meningitis)
o Metronidazole-resistant C. difficile (colitis)
! Use oral preparation, or IV as retention enema
o Surgical prophylaxis for centers with high prevalence for MRSA
Adverse Reactions
Common
o Red man or Red neck syndrome (infusion-related flushing)
! Due to histamine release
! Infusion-related
o Phlebitis to injection site
! Intramuscular route NOT recommended
o GI disturbance e.g. diarrhea, nausea/vomiting
Occasional
o Ototoxicity
! REVERSIBLE
! Risk factors: prolonged use (>10days), large doses, renal failure, advanced age
o Nephrotoxicity
! REVERSIBLE
! Risk factors: prolonged use, concomitant use with nephrotoxic agents esp.
aminoglycosides (synergistic)
Rare
o Macular rash
o Hematologic disturbances e.g. neutropenia, thrombocytopenia
Transcribed by: SPCCF B2017
Specific Antibacterial Agents
Lecture by Dr. Delgado
3. LIPOPEPTIDE
DAPTOMYCIN only lipopeptide available
Daptomycin
MRSA
+
VRSA
+
VISA
+
Streptococci
+
Enterococcus faecalis
+
E. faecium
+
VRE
+
Gram-negative bacilli
0
Clostridium difficile
0
+susceptible; +/- variable; 0 resistant
Vancomycin
0
0
0
+
+
+/0
0
+
Mechanism of Action
Bind to the cell membrane via Ca-dependent insertion of its lipid tail
Depolarization of cell membrane with K efflux and rapid cell death
Pharmacokinetics
Poor oral absorption
Distributed mainly into plasma and interstitial fluid; little CNS and bone penetration
Excreted in urine
Concentration-dependent killing
o As the serum concentration is increased above the MIC, bactericidal activity is also increased
and at a more rapid rate
Clinical Uses
Drug of choice for Vancomycin-resistant strains of S. aureus and Enterococci (including bacteremia)
Alternative drug for Vancomycin for treatment of MRSA bacteremia
NOT recommended for pneumonia
o Inactivated by lung surfactant
Adverse Reactions
Common
o Myopathy elevated creatine kinase (most common)
! REVERSIBLE
Transcribed by: SPCCF B2017
10
Specific Antibacterial Agents
Lecture by Dr. Delgado
Occasional
o Interstitial pneumonitis
4. POLYMIXINS B AND E - COLISTIN
Gram-positive organism
Enterobacteriaceae except Serratia spp., Protues spp., Providencia spp., Morganella spp.
Extended-Spectrum B-lactamases (ESBLs)
Klebsiella pnuemoniae Carbapenemases (KPCs)
New Delhi metallo-B-lactamase (NDM-1)
Acinetobacter baumanni including MDR
Pseudomonas aeruginosa including MDR
Anaerobes
+ susceptible; +/- variable; 0 resistant
Colistin
0
+
+
+
+
+
+
0
Mechanism of Action
Attach and disrupt bacterial cell membrane
o Act as cationic detergent
o Bind to anionic lipopolysaccharide molecules leading to permeability changes in cell membrane
o Leakage of intracellular metabolites and nucleosides, causing cell death
Pharmacokinetics
Polymyxin B (topical)
Polymyxin E (IV)
Poor oral absorption
Widely distributed in tissues except bone, CSF, synovial fluid, pleural fluid, and pericardial fluid
Excreted in urine
Clinical Uses
Infections caused by Multidrug-resistant organism (unresponsive to other antibiotics)
o Pneumonia
o Skin and soft tissue infections
o Intraabdominal infections
o Bacteremia
NOT recommended as monotherapy
Adverse Reactions
Common
o Nephrotoxicity
! Dose >5mg/kg/day
! REVERSIBLE
Occasional
o Neurotoxicity peripheral neuropathy, paresthesias
o Neuromuscular blockade
Rare
o Hypersensitivity
Transcribed by: SPCCF B2017
11
Specific Antibacterial Agents
Lecture by Dr. Delgado
PROTEIN SYNTHESIS INHIBITORS
5. AMINOGLYCOSIDES
Streptomycin
S. aureus NOT MRSA
+
Streptococci
0
Enterococcus faecalis
+
Enterococcus faecium
0
Enterobacteriaceae
+
Pseudomonas aeruginosa
+
Atypical organisms
0
Anaerobes
0
+ susceptible; +/- variable; 0 resistant
*not locally available
# Lowest MIC
Gentamicin
+
0
+
+
+
+
0
0
Amikacin
+
0
+
0
+
+
0
0
Tobramycin*
+
0
+
0
+
+#
0
0
Mechanism of Action
Charged tRNA unit carrying amino acid binds to acceptor site
Growing amino acid chain in the donor site binds to the amino acid in the acceptor site
o Peptide bond formation
Transported to the cytoplasm by an oxygen-dependent process
o Enhanced by cell-wall active antibiotics (synergism) e.g. penicillin
o Inhibited by low extracellular pH and anaerobic condition
Bind to 30s subunit
1. Block formation of the initiation complex
2. Block translocation
3. Misreading of the mRNA
o Incorporation of incorrect amino acids into the growing peptide chain
Mechanism of Resistance
Inactivation by transferase enzyme (adenylation, acetylation, phosphorylation) most important
o NO class resistance
Impaired entry into the cell
Modification of ribosomal binding site/ribosomal protection
Transcribed by: SPCCF B2017
12
Specific Antibacterial Agents
Lecture by Dr. Delgado
Pharmacokinetics
Very poorly absorbed from intact GI tract
o Entire oral dose excreted in feces
Poorly distributed in tissues, and non-inflamed meninges except in neonates (even if given IV)
o Due to large size, polycationic charge, lipid insolubility
o May use intrathecal or intraventricular injection
Excreted in urine (if given parenteral)
o Urine concentration exceed peal plasma level
Synergism with B-lactam antibiotics if given sequentially
o Do NOT mix with B-lactam in the same solution
! Nucleophilic opening of the B-lactam ring
! Acylation of the amino group of the aminoglycoside
Antagonism with other bacteriostatic antibiotics
o Inhibition of the energy-dependent uptake of aminoglycosides
o Interference with movement of the ribosome along mRNA
Concentration-dependent killing
o As the serum concentration is increased above the MIC, bactericidal activity is also increased
and at a more rapid rate
o Better efficacy when given as a single large dose than multiple smaller dose except
! Staphylococcal and Enterococcal endocarditis
! Pregnancy
! Neonates
Clinical Uses
Used in combination with B-lactam antibiotics for serious infections
o Gram-negative septicemia
o Staphylococcal and enterococcal endocarditis (gentamicin, streptomycin)
NOT recommended as monotherapy for Pseudomonas aeruginosa pneumonia
o Poor penetration to infected lung tissue
o Low oxygen tension
NOT recommended for anaerobic infections e.g. abscess
Other uses
o M. tuberculosis (Streptomycin - most active, amikacin)
! Contraindicated during pregnancy due to risk of deafness in the newborn
Adverse Reactions
Common
o Ototoxicity
! IRREVERSIBLE; can appear after the end of treatment
! Risk factor: >5 days, higher dose, advanced age, renal insufficiency, concurrent
nephrotoxic agents (e.g. amphotericin B, vancomycin)
! Auditory/cochlear damage (up to 62%) tinnitus, sensation of fullness of ears
Initially affects perception of high frequency sound
Most common with neomycin (most toxic)
! Vestibular damage (up to 19%) ataxia, loss of balance, vertigo
Most common with streptomycin
o Nephrotoxicity (5-25%)
! REVERSIBLE
! Same risk factors
! Decreased risk with once daily dosing
! Most common with neomycin
Rare
o Hypersensitivity, anaphylaxis
Transcribed by: SPCCF B2017
13
Specific Antibacterial Agents
Lecture by Dr. Delgado
o
o
Local reaction e.g. pain at injection site
Neuromuscular blockade
! Results in respiratory paralysis
! Risk factors: bolus/fast infusion, large dose, hypocalcemia, succinylcholine
! Due to inhibition of the presynaptic release of acetylcholine, and blockade of
postsynaptic receptor
! Most common with neomycin
! Antidote: Calcium gluconate
6. TETRACYCLINE
Short-acting (t 6-8hrs)
o Chlortetracycline
o Tetracycline*
o Oxytetracycline
Intermediate-actong (t 12hrs)
o Demeclocycline
o Methacycline
o Lymecycline*
Long-acting (t 16-18hrs)**
o Doxycycline*
o Minocycline*
*Locally Available
** Second generation tetracycline
Tetracyclines
Gram-positive cocci
+/Enterobacteriaceae
+/Pseudomonas aeruginosa
0
Legionella spp.
+/Chlamydophila spp.
+
Mycoplasma pneumonia
+
Ricketssiae
+
Anaerobes
+
+ susceptible; +/- variable; 0 resistant
Mechanism of Action
Susceptible organism concentrate the drug intracellularly
Bind to the 30s subunit
Prevent binding of incoming charged tRNA unit to the acceptor site
Transcribed by: SPCCF B2017
14
Specific Antibacterial Agents
Lecture by Dr. Delgado
Pharmacokinetics
Absorption impaired by food (except doxycycline, minocycline), antacids, dairy products, and divalent
cations (Ca2+, Mg2+, Fe2+), or Al3+
High protein-binding
Widely distributed to tissues except CSF
Excellent intracellular penetration
Excreted in bile and urine except
o Doxycycline (bile)
Can pass the placenta, excreted in milk
Clinical Uses Doxcycycline
Drug of choice for infections caused by Rickettsiae
Other uses
o Mycoplasma pneumonia
o Chlamydophila pneumonia and C. psittaci
! NOT recommended for Legionella spp.
o Chlamydophila trachomatis
! NOT recommended for N. gonorrhoeae
o Leptospira spp. (mild infection, prophylaxis)
o Vibrio spp.
o Borellia burgdorferi (Lyme Disease)
o Plasmodium falciparum (prophylaxis)
Adverse Reactions
Common
o GI disturbances e.g. nausea/vomiting, diarrhea (minocycline)
o Local reaction e.g. thrombophlebitis
o Oral candidiasis
o Permanent teeth discoloration and enamel hypoplasia
o Bone deformity/growth retardation Pregnancy Risk Category D
! Avoid during pregnancy and children <8yrs
Occasional
o Hepatitis (tetracycline), liver failure
! Risk factor: high parenteral dose (>1gm/day), pregnancy, renal failure
o Photosensitivity (demeclocycline)
o Esophageal ulceration
o Pancreatitis (tetracycline)
o Visual disturbances (tetracycline)
o Vestibular toxicity, vertigo (minocycline)
o Pseudomembranous colitis
o Aggravate pre-existing renal failure
! Increase azotemia due to inhibition of protein synthesis
Rare
o Hypersensitivity, drug eruption
o Pseudotumor cerebri (increased intracranial pressure in infants)
o Diabetes insipidus (demeclocycline)
o Interstitial nephritis (minocycline)
o Lupus-like syndrome (minocycline)
o Black pigmentation of thyroid (minocycline)
o Gray pigmentation of nail, skin, sclera (minocycline)
Transcribed by: SPCCF B2017
15
Specific Antibacterial Agents
Lecture by Dr. Delgado
7. GLYCYLCYCLINE
Gram (+)
Staphylococci including MRSA,
VRSA, VISA
Gram (-)
Enterobacteriaceae (except
Proteus spp., Providencia spp.,
Morganella spp.) including
ESBL, KPC, NDM-1
MDR Acinetobacter spp.
Streptococci
Enterococci including VRE
NOT active against Pseudomonas aeruginosa
Others
Atypical organisms (Legionella
spp., Mycoplasma pneumoniae,
Chlamydophila spp.)
Rickettsiae
Anaerobes
Mechanism of Action
Bind to the 30s subunit
Prevent binding of incoming charged tRNA unit
Pharmacokinetics
Tigecycline (IV)
Poorly absorbed after oral administration
Widely distributed to tissues except CSF
Excellent intracellular penetration
Low urinary concentration
Excreted in bile and urine
o Adjust dose if with liver disease (Childs-Pugh C)
Clinical Uses
Infections caused by Multidrug-resistant organisms
o Skin and soft tissues infections
o Intraabdominal infections
NOT recommended as 1st line treatment for pneumonia
o High rate of treatment failure
NOT recommended for bacteremia
Adverse Reactions
Same as tetracyclines Pregnancy Risk Category D
Hematologic disturbances e.g. thrombocytopenia, prolonged partial thromboplastin time and
prothrombin time
Pancreatitis
Transaminits
Somnolence
Transcribed by: SPCCF B2017
16
Specific Antibacterial Agents
Lecture by Dr. Delgado
8. MACROLIDES
Mechanism of Action
Susceptible organisms concentrate the drug intracellularly
Bind to the 50s subunit
Block peptide chain elongation
Erythromycin
+/+
+
0
Clarithromycin
+/+
+
0
Azithromycin
+/+
+
+/-
+
+
+
0
0
+
+
+
0
0
+
+
+
0
0
Gram-positive cocci
Moraxella catarrhalis
Haemophilus influenza
Some Enterobacteriaceae
(E. coli, Klebsiella spp.)
Legionella spp.
Chlamydophila spp.
Mycoplasma pneumoniae
Pseudomonas aeruginosa
Anaerobes
+ susceptible; +/- variable; 0 resistant
Mechanism of Resistance
Modification of ribosomal binding site/ribosomal protection (by production of methylase)
o Confers resistance to structurally related compounds (clindamycin and streptogramin B)
Efflux pump
Production of esterases
ERYTHROMYCIN
Pharmacokinetics
Absorption impaired by food
o Stearates and esters promotes better absorption; estolate best absorption
o IV formulation (gluceptate, lacbionate)
Widely distributed to tissues except CSF
Good intracellular/tissue penetration
Excreted in bile
Can pass the placenta; excreted in milk
Inhibit cytochrome P450
o Increases serum concentration of theophylline, warfarin, methylprednisolone, carbamazepine
Time-dependent killing
Clinical Uses
Drug of choice for infections caused by
o Legionella pneumophila, Mycoplasma pneumoniae, Chlamydophila spp. (atypical pneumonia)
o Corynbacterium spp. (diphtheria)
o Bordetella pertussis
Other uses
o Chlamydophila trachomatis
Penicillin substitutes for Streptococcus pyogenes to those with penicillin-allergy
Adverse Reactions
Common
o GI disturbances e.g. diarrhea, abdominal cramps, flatulence, nausea/vomiting
! Due to motilin
! Dose-related
Transcribed by: SPCCF B2017
17
Specific Antibacterial Agents
Lecture by Dr. Delgado
Occasional
o Acute cholestatic hepatitis (estolate)
! Usually occurs 20days after treatment
! REVERSIBLE
o Stomatitis
o Thrombophlebitis
Rare
o Hypersensitivity
o Infantile hypertrophic pyloric stenosis
! Due to interaction of motilin receptors to induce strong gastric and pyloric contractions
leading to pyloric hypertrophy
o QTc interval prolongation, arrhythmia (torsades de pointes, ventricular tachycardia)
o Transient hearing loss
CLARITHROMYCIN
Compared to Erythromycin
o Most active against H. influenza and Mycobacterium avium complex
o Longer half-life
o Absorption less affected by food
o Excreted in urine
o Less GI disturbance
AZITHROMYCIN
Similar spectrum of activity with Clarithromycin with additional coverage for Salmonella spp. and
Shigella spp.
Drug of choice for infection caused by Bartonella henselae (cat scratch disease)
Compared to other macrolides
o Absoprtion impaired by food
o Best tissue penetration (>10 to 100-fold than serum)
! Slowly released from tissue (t 2-4 days)
o Concentration-dependent killing
o Does not inhibit cytochrome P450
! 15-member (not 14-member) lactone ring by addition of methylated nitrogen in the
lactone ring
o Less GI disturbance
9. LINCOSAMIDE
CLINDAMYCIN derivative of lincomycin
Mechanism of Action
Bind to the 50s subunit
o Block peptide bond formation
o Block translocation
Clindamycin
+
including CA-MRSA
Streptococci
+
Enterococci
0
Gram-negative bacilli
0
Anaerobes
+
except B. fragilis
+ susceptible; +/- variable; 0 resistant
Staphylococci
Transcribed by: SPCCF B2017
Vancomycin
+
including HA-MRSA
+
+
0
+/-
18
Specific Antibacterial Agents
Lecture by Dr. Delgado
Pharmacokinetics
Clindamycin (oral, IV)
o Absorption not affected by food
High protein binding
Good distribution to tissues (including bone) except CSF
Can penetrate abscesses
Excreted in bile and urine
Can pass the placenta
Clinical Uses
Drug of choice for infections caused by Community Acquired MRSA (skin and soft tissue infection)
o NOT recommended for Hospital Acquired MRSA
o NOT recommended for bacteremia and meningitis
Other uses
o Anaerobic infections ABOVE the level of diaphragm (e.g. lung abscess) except CNS
! NOT recommended for Bacteroides fragilis (intraabdominal infection)
o Alternative treatment for staphylococcal infections (osteomyelitis, septic arthritis) to those with
penicillin-allergy
Adverse Reactions
Common
o GI disturbances e.g. diarrhea (more common with oral preparation), nausea.vomiting
o Hypersensitivity
Occasional
o Pseudomembranous colitis, toxic megacolon
! Most common cause of Clostridium difficile mediated diarrhea
10. CHLORAMPHENICOL
Chloramphenicol
Staphylococci
+/Enterococci
0
Streptococci
+
Neisseria meningitides
+
Haemophilus influenza
+
Enterobacteriaceae
+/Pseudomonas aeruginosa
0
Atypical organism
+/Anaerobes
+
+ susceptible; +/- variable; 0 resistant
Pharmacokinetics
Available as prodrug
o Succinate (IV)
o Palmitate (oral)
! Produces higher blood level of free drug than IV
Low protein binding
Widely distributed to tissues including CSF
Good intracellular penetration
Metabolized in the liver (glucoronic acid conjugation)
Excreted in urine and bile
Can pass the placenta; excreted in milk
Transcribed by: SPCCF B2017
19
Specific Antibacterial Agents
Lecture by Dr. Delgado
Inhibit cytochrome P450
o Increases serum concentration of phenytoin, warfarin
Time-dependent killing
o Efficacy is directly related to time above MIC, and becomes independent of concentration once
the MIC has been reached
Clinical Uses
Alternative drug for B-lactam for treatment of bacterial meningitis
Other uses
o Salmonella typhi
o Shigella spp.
o Ricketssia spp.
Adverse Reactions
Common
o Dose-related anemia (REVERSIBLE)
o Due to inhibition of mitochondrial protein synthesis
o Usually accompanied by leukopenia and/or thrombocytopenia
o 4g/day for 1-2 weeks
o Gray baby syndrome (gray color/cyanosis, vomiting, flaccidity, hypothermia, shock)
Pregnancy Risk Category C
! Due to lack of effective glucuronic acid conjugation in newborn infants
! Limit dose to <50mg/kg/d during 1st week of life
! NOT recommended during term pregnancy and lactation, and in neonates
Occasional
o GI disturbance e.g. diarrhea, nausea/vomiting, anorexia
o Oral candidiasis
Rare
o Aplastic anemia (idiosyncratic; IRREVERSIBLE)
! May occur weeks to months after completion of treatment
! NOT dose-related
o Hypersentivity
o Peripheral neuropathy
o Optic neuritis
o Pseudomembranous colitis
11. OXAZOLIDINONE
LINEZOLID only oxazolidinone available
Linezolid
MRSA
+
VRSA
+
VISA
+
Streptococci
+
Enterococcus faecalis
+
E. faecium
+
VRE
+
Gram-negative bacilli
0
Anaerobes
+/+ susceptible; +/- variable; 0 resistant
Transcribed by: SPCCF B2017
Vancomycin
+
0
0
+
+
+/0
0
+
Daptomycin
+
+
+
+
+
+
+
0
0
20
Specific Antibacterial Agents
Lecture by Dr. Delgado
Mechanism of Action
Bind to 50s subunit
Inhibit formation of ribosome complex that initiates protein synthesis
NO cross-resistance with other drug classes
Pharmacokinetics
Linezolid (oral, IV)
o 100% bioavailability after oral administration
Widely distributed to tissues including CSF
Excreted in urine
Clinical Uses
Infections caused by Multidrug-resistant Gram-positive cocci (MRSA, VRE)
o Skin and soft tissue infections
o Pneumonia
NOT recommended for MRSA bacteremia
Other use
o MDR M. tuberculosis
Adverse Reactions
Common
o Hematologic disturbance (REVERSIBLE)
! Thrombocytopenia (most common); prolonged use >10days
! Anemia, neutropenia
Occasional
o GI disturbance e.g. nausea/vomiting, diarrhea
o Optic, and peripheral neuropathy
! Due to mitochondrial protein synthesis
! May lead to blindness if drug is not discontinued
12. STREPTOGRAMINS
Streptogramin B Quinupristin
Streptogramin A Dalfopristin
Displays synergism
o Bactericidal unlike other protein synthesis inhibitors
MRSA
VRSA
VISA
Streptococci
Enterococcus faecalis
E. faecium
VRE
Gram-negative
Anaerobes
*Not locally available
Quinupristin Dalfopristin*
Linezolid
+
+
+
+
+
+
+
+
0
+
+
+
+/+
0
0
0
+/+ susceptible; +/- variable; 0 resistant
Mechanism of Action
Bind to the 50s subunit
Interfere with peptidyl transferase (dalfopristin)
Inhibit peptide chain elongation (quinupristin)
Transcribed by: SPCCF B2017
21
Specific Antibacterial Agents
Lecture by Dr. Delgado
Mechanism of Resistance
Modification of ribosomal binding site/ ribosomal protection (by production of methylase)
o Confers resistance to structurally related compounds (macrolides and clindamycin)
Efflux pump
Pharmacokinetics
Quinupristin-Dalfopristin (IV), 30:70 ratio
Widely distributed in tissues except CSF
Excreted in stool
Inhibit CYP3A4
o Increases serum concentration of warfarin, diazepam
Clinical Uses
Infection caused by Multidrug-resistant Gram-positive cocci except Enterococcus faecalis
o Skin and soft tissue infections
o Pneumonia
o Bacteremia
Adverse Reactions
Common
o Infusion-related reactions e.g. phlebitis
! Administer using a central line
o Arthralgia-myalgia syndrome
o Direct hyperbilirubinemia
Transcribed by: SPCCF B2017
22
Specific Antibacterial Agents
Lecture by Dr. Delgado
NUCLEIC ACID SYNTHESIS INHIBITORS
13. COTRIMOXAZOLE
SMX sulfanilamide nucleus (similar to p-aminobenzoic acid [PABA])
TMP benzypyrinamide
Combination is bactericidal
S. aureus Including MRSA
Streptococci
Enterococci
Enterobacteriaceae
Pseudomonas aeruginosa
Burkholderia cepacia
Stenotrophonomas maltophilia
Anaerobes
+ susceptible; +/- variable; 0 resistant
TMP-SMX
+
+/0
+/0
+
+
0
Mechanism of Action
SMX (structural analog of PABA) inhibit dihydropteroate
synthase
o Inhibit production of dihydrofolic acid
TMP inhibit dihydrofolate reductase
o Inhibit production of tetrahydrofolic acid (essential for
purine/DNA)
TMP-SMX blocks sequential step in folic acid synthesis
(synergism)
Mehanism of Resistance
SMX
o Overproduction of PABA
o Overproduction of dihydropteroate synthase with reduced
drug binding
o Impaired entry into the cell
TMP
o Overproduction of dihydrofolate reductase with reduced drug binding
o Impaired entry into the cell
Pharmacokinetics
TMP-SMX (oral, IV), 1:5 ratio
o Single strength (SS): 80/400mg (well-absorbed)
o Double strength (DS): 160/800mg
Widely distributed in body fluids and tissues including CSF and prostate
Metabolized in the liver (glucuronic acid conjugation)
Can pass the placenta
Excreted in urine
Time-dependent killing
Clinical Uses
Drug of choice for infections caused by Stenotrophomonas maltophilia
Other uses
o Susceptible MRSA
Transcribed by: SPCCF B2017
23
Specific Antibacterial Agents
Lecture by Dr. Delgado
o Burkholderia cepacia
o Salmonella typhi
o Shigella spp.
o Nocardia spp.
May be used for prostatitis
NOT recommended empiric therapy for pneumonia
Other uses
o Drug of choice for Pneumocystic jiroveci pneumonia (PCP)
o Alternative treatment for Toxoplasama gondii
! Drug of choice is pyrimethamine-sulfadiazine
Adverse Reactions
Common
o Rash, exfoliative dermatitis, photosensitivity (SMX)
Occasional
o Hematologic disturbances
! SMX: aplastic anemia, hemolytic anemia (those with G6PD deficiency)
granulocytopenia, thrombocytopenia
! TMP: megaloblastic anemia, leukopenia, granulocytopenia
Occasional
o Kernicterus (SMX) Pregnancy Risk Category C
! Due to lack of effective glucuronic acid conjugation in newborn infants
! NOT recommended during term pregnancy and lactation, and in neonates
o Urinary tract disturbances e.g. crystalluria, hematuria, obstruction
! Due to precipitation of SMX in the urine
o Hyperkalemia
o Pseudomembranous colitis
Rare
o Stevens-Johnson syndrome (SMX)
! Rash with mucosal involvement; <1%
o Hepatitis, cholestasis
o CNS distubances e.g. confusion, depression, hallucinations, ataxia
o Methemoglobinemia
o Pancreatitis
o Lupus-like syndrome (SMX)
14. FLUOROQUINOLONES
Nor
Oflo
Cipro
Levo
Moxi
Gemi
Staphylococci
+/+
+
+
+
+
Streptococci
+/+/+/+
+
+*
Enterococcus faecalis
0
0
0
+
+
+
N. gonorrhoeae
+/+/+/+/+/+/Enterobacteriaceae
+/+
+
+
+
+/Pseudomonas spp.
0
0
+*
+
0
0
Atypical organisms
+
+
+
+
+
+
Anaerobes
0
0
0
0
+
0
+Susceptible; +/- variable; 0 resistant
*Lowest MIC
Atypical organisms Legionella spp., Chlamydophila spp., Mycoplasma spp.
Transcribed by: SPCCF B2017
24
Specific Antibacterial Agents
Lecture by Dr. Delgado
Analogs of nalidixic acid
1st generation
o norfloxacin*
2nd generation
o Ciprofloxacin*, Ofloxacin*, Pefloxacin
3rd generation
o Levofloxacin*, Gatifloxacin, Gemifloxacin*, Moxifloxacin
*Available locally
Mechanism of Resistance
Modification of target enzyme (DNA gyrase)
Impaired entry into the cell
Pharmacokinetics
Oral, IV
o 80-95% bioavailability after oral administration
o absorption impaired by divalent cations or Al3+
Widely distributed in body fluids and tissues including CSF and prostate
High intracellular/tissue penetration
Excreted urine except Gemifloxacin (urine,bile), Moxifloxacin (bile)
Clinical Uses
NOT recommended for Neisseria gonorrhoeae
Other use
o MDR M. tuberculosis (ciprofloxacin, ofloxacin, levofloxacin, moxifloxacin)
! Moxifloxacin most active
Adverse Reactions
Occasional
o GI disturbances e.g. nausea/vomiting, diarrhea, abdominal pain
o CNS disturbances e.g. insomnia, headache, dizziness, tremors, restlessness, confusion
! Due to inhibition of GABA
o Rash (macular)
o Oral candidiasis
o Transaminitis, hepatitis (trevafloxacin*, sparfloxacin*) *no longer manufactured
o Hematologic disturbance e.g. leukopenia, neutropenia, eosinophilia, anemia (norfloxacin)
o Hyperglycemia in diabetics; hypoglycemia when combined with oral hypoglycemic agents
(gatifloxacin no longer manufactured)
o Arthropathy (reversible), damages growing cartilage Pregnancy Risk Category C
! Due to chelation og Mg++ damaging chondrocyte interaction
! Not routinely recommended for children <18yrs during pregnancy
Rare
o Tendinitis, tendon rupture
! Risk factors: advanced age, renal failure, concurrent corticosteroids use
! Achilles tendon most common
o Retinal detachment due to destruction of ocular collagen
o Anaphylaxic (often fatal)
o CNS disturbances e.g. hallucinations, delirium, convulsions
o Peripheral neuropathy
o Pseudomembranous colitis
o Interstitial nephritis
o Vaculitis
o QTc prolongation
Transcribed by: SPCCF B2017
25
Specific Antibacterial Agents
Lecture by Dr. Delgado
OTHER ANTIBACTERIAL AGENTS
16. NITROMIDAZOLE
METRONIDAZOLE
Gram-positive organisms
Gram-negative organism
Anaerobes including B. fragilis and Clostridium difficile
+ susceptible; +/- variable; 0 resistant
Metronidazole
0
0
+
Mechanism of Action
Nitro group reduced intracellularly by reacting with reduced ferredoxin
o Catalyzed by pyruvate:ferredoxin oxidoreductase
o This process only happens in anaerobic bacteria
Produce toxic metabolites which are taken up into bacterial DNA
o Loss of helical DNA structure and strand breakage
Pharmacokinetics
Oral, IV, recta (suppository)
o Approaches 100% oral bioavailability (not affected by food)
Widely distributed in body fluids and tissues including CSF
Penetrate abscesses including those in the brain
Excreted in urine and feces
Concentration-dependent killing
Clinical Uses
Drug of choice for Clostridium difficile colitis
Anaerobic infections BELOW the level of diaphragm (e.g. intraabdominal infection)
Brain abscess
Other uses
o Clostridium tetani
o Entamoeba histolytica
o Trichomonas vaginalis
o Giargia lamblia
Adverse Reactions
Common
o Gi disturbances e.g. nausea/vomiting, diarrhea
o Dry mouth, furry tongue
o Metallic taste
Occasional
o Insomnia
o Urethral burning
o Darkening of urine
o Phlebitis
o Disulfiram-like effect (may cause psychosis)
Rare
o CNS disturbance e.g. seizure, ataxia, dysarthria, encephalopathy (reversible)
! Risk factors: prolonged therapy, large doses (~4g/day)
o Peripheral and optic neuropathy
o Pancreatitis
Transcribed by: SPCCF B2017
26
Specific Antibacterial Agents
Lecture by Dr. Delgado
TINIDAZOLE
Same coverage as metronidazole but NOT yet approved by U.S. FDA for anaerobic infection
Advantage of once daily dosing
17. NITROFURANTOIN
Nitrofurantoin
Staphylococci including MRSA
+
Streptococci
+
Enterococci
+
E. coli
+
Other Enterobacteriaceae
0
Pseudomonas aeruginosa
0
Anaerobes
0
+ susceptible; +/- variable; 0 resistant
Pharmacokinetics
Well absorbed after oral administration
Very rapid excretion in urine
o NO systemic antibacterial effect
Clinical Use
Urinary antiseptic (uncomplicated acute cystitis)
NOT recommended during renal failure (creatinine clearance <60mL/min)
o Urine levels are insufficient for antibacterial action
o High blood levels may produce toxicity
NOT recommended for upper urinary tract infection (pyelonephritis)
Adverse Reactions
Common
o GI disturbances e.g. nausea/vomiting, diarrhea
Occasional
o Neuropathy
o Hemolytic anemia (those with G6PD deficiency)
o Rash
o Pulmonary infiltration, fibrosis
18. FOSFOMYCIN
Staphylococci including MRSA
Streptococci
Enterococcus faecalis NOT E. faecium
Enterobacteriaceae
Extended-spectrum B-lactamases (ESBLs)
Klebsiella pneumoniae Carbapenemases (KPCs)
Pseudomonas aeruginosa
Anaerobes
+ susceptible; +/- variable; 0 resistant
Transcribed by: SPCCF B2017
Fosfomycin
+
+/+
+
+
+
0
+
27
Specific Antibacterial Agents
Lecture by Dr. Delgado
Mechanism of Action
Inhibit the very early stage of cell wall synthesis
o Inhibit enolpyruvate transferase
o Block the addition of phosphoenolpyruvate to UDP-N-acetylglucosamine (first step in the
formation of N-acetylmuramic acid)
Pharmacokinetics
40% bioavailability after oral administration
Poorly distributed in tissues
Excreted in the urine
o Urinary concentration exceeding MICs for most urinary tract pathogens
Clinical Use
Uncomplicated acute cystitis
NOT recommended as first line agent for treatment of MDR infections
Transcribed by: SPCCF B2017
28
Das könnte Ihnen auch gefallen
- Chemotherapy AntibioticsDokument23 SeitenChemotherapy AntibioticsMubarak Abubakar yaroNoch keine Bewertungen
- AntibioticsDokument9 SeitenAntibioticsAudrey Beatrice ReyesNoch keine Bewertungen
- Gastrointestinal System: Miranda KhidesheliDokument155 SeitenGastrointestinal System: Miranda KhidesheliTanmay NainNoch keine Bewertungen
- CS1 AntibioticsDokument4 SeitenCS1 AntibioticsTaraKyleUyNoch keine Bewertungen
- Gyne - Case 15 Benign Lesions of The Vulva & VaginaDokument2 SeitenGyne - Case 15 Benign Lesions of The Vulva & Vaginacbac1990Noch keine Bewertungen
- IM-Module B Summarized Notes (IBD)Dokument69 SeitenIM-Module B Summarized Notes (IBD)DeepbluexNoch keine Bewertungen
- Pedia CaseDokument65 SeitenPedia CaseJason MirasolNoch keine Bewertungen
- Pneumonia Guide: Causes, Symptoms, Diagnosis and TreatmentDokument6 SeitenPneumonia Guide: Causes, Symptoms, Diagnosis and TreatmentRem AlfelorNoch keine Bewertungen
- MSPH Biostatistics FlyerDokument2 SeitenMSPH Biostatistics FlyerJoyce MalitNoch keine Bewertungen
- 1.10 CPG For TBDokument9 Seiten1.10 CPG For TBMaikka IlaganNoch keine Bewertungen
- Hemoptysis 1Dokument27 SeitenHemoptysis 1Aida SiregarNoch keine Bewertungen
- Knowledge, Attitude and Practice of Self-Medication Among Medical StudentsDokument8 SeitenKnowledge, Attitude and Practice of Self-Medication Among Medical StudentsInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Lower Genital Infections GuideDokument2 SeitenLower Genital Infections Guidecbac1990Noch keine Bewertungen
- Thesis 2Dokument70 SeitenThesis 2Angeline Alpure MoralesNoch keine Bewertungen
- Case Simu 104Dokument4 SeitenCase Simu 104Princess Levie CenizaNoch keine Bewertungen
- Detailed Learning Module 7.2.PdDokument10 SeitenDetailed Learning Module 7.2.PdRanz Kenneth G. FrandoNoch keine Bewertungen
- Sepsis and SIRSDokument24 SeitenSepsis and SIRSFryda 'buona' YantiNoch keine Bewertungen
- Pharmacist Code of EthicsDokument12 SeitenPharmacist Code of EthicsShimul HalderNoch keine Bewertungen
- Statement of Principle Self-Care Including Self-Medication - The Professional Role of The PharmacistDokument5 SeitenStatement of Principle Self-Care Including Self-Medication - The Professional Role of The PharmacistAprilia R. Permatasari0% (1)
- Primary Headache: Mohamad Dawoud 6 Course Kharkiv National Medical UniversityDokument17 SeitenPrimary Headache: Mohamad Dawoud 6 Course Kharkiv National Medical UniversityMhamad DawoudNoch keine Bewertungen
- Case 2 Pre-Op & Post-Op CareDokument1 SeiteCase 2 Pre-Op & Post-Op Carecbac1990Noch keine Bewertungen
- Infective Endocarditis: Akriti DahalDokument79 SeitenInfective Endocarditis: Akriti DahalAkriti100% (1)
- Pharm 231: Hospital Pharmacy: Iii. Medication ProfileDokument3 SeitenPharm 231: Hospital Pharmacy: Iii. Medication ProfileTESORO Zeus DavidNoch keine Bewertungen
- The Human Body A Nutrition PerspectiveDokument50 SeitenThe Human Body A Nutrition PerspectiveRichard GelmanNoch keine Bewertungen
- Module 6.5 MycologyDokument4 SeitenModule 6.5 MycologyPNoch keine Bewertungen
- TB in ChildrenDokument26 SeitenTB in ChildrenReagan PatriarcaNoch keine Bewertungen
- Case Histo PDFDokument19 SeitenCase Histo PDFsomayya waliNoch keine Bewertungen
- Case 2Dokument14 SeitenCase 2Je KirsteneNoch keine Bewertungen
- Pharma CNS DRUGS Part 1Dokument13 SeitenPharma CNS DRUGS Part 1reference booksNoch keine Bewertungen
- Pharmacology 1Dokument53 SeitenPharmacology 1Dawn WRein LegaspiNoch keine Bewertungen
- Analgesic OintmentDokument1 SeiteAnalgesic OintmentLorenNoch keine Bewertungen
- Most Common Complication: Sabay SilaDokument6 SeitenMost Common Complication: Sabay SilaSheryl Layne Lao-SebrioNoch keine Bewertungen
- Powerpoint: Sequelae of Gastric SurgeryDokument86 SeitenPowerpoint: Sequelae of Gastric Surgeryj.doe.hex_87Noch keine Bewertungen
- Anti Helminthic DrugsDokument3 SeitenAnti Helminthic Drugsdhainey100% (2)
- Autacoids: H1 Receptor Allergic and Anaphylactic Responses H2 Receptor Secretion of Acid and PepsinDokument3 SeitenAutacoids: H1 Receptor Allergic and Anaphylactic Responses H2 Receptor Secretion of Acid and PepsinMarkyNoch keine Bewertungen
- Chapter 01 History of PharmacyDokument26 SeitenChapter 01 History of PharmacyAįmz DìvşNoch keine Bewertungen
- Antibiotic Resistance QuestionsDokument4 SeitenAntibiotic Resistance Questionspriya swathiNoch keine Bewertungen
- PHARMACOLOGY - Midterms 1.6-Fluid and Electrolyte TRANSDokument13 SeitenPHARMACOLOGY - Midterms 1.6-Fluid and Electrolyte TRANSNooneNoch keine Bewertungen
- Wine Production ProcessDokument2 SeitenWine Production ProcessJanice Malafu De GuiaNoch keine Bewertungen
- Beta LactamDokument18 SeitenBeta LactamCesar Saba0% (1)
- Micro For Nursing Lecture - Chapter 3Dokument25 SeitenMicro For Nursing Lecture - Chapter 3Degee O. GonzalesNoch keine Bewertungen
- Characteristics and Treatment of Hypertension in PheochromocytomaDokument17 SeitenCharacteristics and Treatment of Hypertension in PheochromocytomaJunior TorresNoch keine Bewertungen
- List of Clotting FactorsDokument1 SeiteList of Clotting FactorsGNiqMNoch keine Bewertungen
- Mishba +pharmacology + Tapan ShahDokument232 SeitenMishba +pharmacology + Tapan ShahRaushan BlakeNoch keine Bewertungen
- Asthma Pathophysiology and Risk FactorsDokument98 SeitenAsthma Pathophysiology and Risk FactorsyayayanizaNoch keine Bewertungen
- Guidelines for Measuring Household and Individual Dietary DiversityVon EverandGuidelines for Measuring Household and Individual Dietary DiversityNoch keine Bewertungen
- Immunization Policy Guidline - Kenya 2013Dokument72 SeitenImmunization Policy Guidline - Kenya 2013okwadha simionNoch keine Bewertungen
- AntibioticsDokument58 SeitenAntibioticsKamal GhimireNoch keine Bewertungen
- BacteriaDokument168 SeitenBacteriadenekeNoch keine Bewertungen
- Nurse's Study Guide To BurnsDokument14 SeitenNurse's Study Guide To BurnsCassie GonzalezNoch keine Bewertungen
- Oral Revalida Im Cases Dec. 12 and 13 2020Dokument16 SeitenOral Revalida Im Cases Dec. 12 and 13 2020Bea Y. Bas-ongNoch keine Bewertungen
- Pharmacotherapy of Diabetes MellitusDokument8 SeitenPharmacotherapy of Diabetes MellitusSheryl Layne Lao-SebrioNoch keine Bewertungen
- New Patient Assessment and Care PlanDokument4 SeitenNew Patient Assessment and Care PlanRalph Lawrence Ruiz Tagorda0% (1)
- Stroke and HypertensionDokument4 SeitenStroke and HypertensionKhessie Laye Garcia JacintoNoch keine Bewertungen
- GI Pharmacology OverviewDokument24 SeitenGI Pharmacology OverviewjenniferluzonNoch keine Bewertungen
- Management of Poisoning - Booklet PDFDokument344 SeitenManagement of Poisoning - Booklet PDFkrysteenNoch keine Bewertungen
- Oncology Nursing-2 PDFDokument22 SeitenOncology Nursing-2 PDFHebsiba PonnayyanNoch keine Bewertungen
- Introduction To Antibiotics: Mrs Natasha MahajanDokument17 SeitenIntroduction To Antibiotics: Mrs Natasha Mahajannatasha jadhavNoch keine Bewertungen
- Asthma Triggers, Symptoms, Diagnosis & Treatment GuideDokument10 SeitenAsthma Triggers, Symptoms, Diagnosis & Treatment GuideRem AlfelorNoch keine Bewertungen
- Case Study FinalDokument22 SeitenCase Study FinalDave Cabuyadao0% (1)
- Gynecology - Case 14 - Benign Lesions For Ovaries (Gonzalez)Dokument2 SeitenGynecology - Case 14 - Benign Lesions For Ovaries (Gonzalez)cbac1990Noch keine Bewertungen
- Gynecology - Case 13 - Benign Lesions of The Uterus (Gonzalez)Dokument2 SeitenGynecology - Case 13 - Benign Lesions of The Uterus (Gonzalez)cbac1990Noch keine Bewertungen
- Gyne - Case 17 - Intraepithelial & Neoplastic Lesions of The Uterus (Gonzalez)Dokument1 SeiteGyne - Case 17 - Intraepithelial & Neoplastic Lesions of The Uterus (Gonzalez)cbac1990Noch keine Bewertungen
- Gyne - Case 16 - Intraepithelial & Neoplastic Lesions of Cervix (Gonzalez)Dokument2 SeitenGyne - Case 16 - Intraepithelial & Neoplastic Lesions of Cervix (Gonzalez)cbac1990Noch keine Bewertungen
- Gyne Notes Abnormal Uterine Bleeding - Dra TrinidadDokument3 SeitenGyne Notes Abnormal Uterine Bleeding - Dra Trinidadcbac1990Noch keine Bewertungen
- Gyne - Lec 03 CytologyDokument3 SeitenGyne - Lec 03 Cytologycbac1990Noch keine Bewertungen
- Gynecology - Case 13 - Benign Lesions of The Uterus (Gonzalez)Dokument2 SeitenGynecology - Case 13 - Benign Lesions of The Uterus (Gonzalez)cbac1990Noch keine Bewertungen
- Gyne - Case 18 - Neoplastic Lesions of The Ovaries (Gonzalez) PDFDokument3 SeitenGyne - Case 18 - Neoplastic Lesions of The Ovaries (Gonzalez) PDFcbac1990Noch keine Bewertungen
- Gyne - Case 18 - Neoplastic Lesions of The Ovaries (Gonzalez) PDFDokument3 SeitenGyne - Case 18 - Neoplastic Lesions of The Ovaries (Gonzalez) PDFcbac1990Noch keine Bewertungen
- Cervical Cancer and Neoplastic LesionsDokument1 SeiteCervical Cancer and Neoplastic Lesionscbac1990Noch keine Bewertungen
- Gyne - Case 17 - Intraepithelial & Neoplastic Lesions of The Uterus (Gonzalez)Dokument1 SeiteGyne - Case 17 - Intraepithelial & Neoplastic Lesions of The Uterus (Gonzalez)cbac1990Noch keine Bewertungen
- Gyne - Case 12 Upper Genital UTIDokument2 SeitenGyne - Case 12 Upper Genital UTIcbac1990Noch keine Bewertungen
- Gyne - Case 14 Benign Lesions of The OvariesDokument2 SeitenGyne - Case 14 Benign Lesions of The Ovariescbac1990Noch keine Bewertungen
- Gyne - Case 10 MenopauseDokument2 SeitenGyne - Case 10 Menopausecbac1990Noch keine Bewertungen
- Lower Genital Infections GuideDokument2 SeitenLower Genital Infections Guidecbac1990Noch keine Bewertungen
- Gyne - Case 08 Dysmenorrhea & Endometriosis PDFDokument3 SeitenGyne - Case 08 Dysmenorrhea & Endometriosis PDFcbac1990Noch keine Bewertungen
- Uterine Lesions GuideDokument2 SeitenUterine Lesions Guidecbac1990Noch keine Bewertungen
- Gyne - Case 07 Secondary Amenorrhea (Hyperprolactinemia)Dokument1 SeiteGyne - Case 07 Secondary Amenorrhea (Hyperprolactinemia)cbac1990Noch keine Bewertungen
- Gyne - Case 07 Secondary Amenorrhea (Hyperprolactinemia)Dokument1 SeiteGyne - Case 07 Secondary Amenorrhea (Hyperprolactinemia)cbac1990Noch keine Bewertungen
- Case 4 Anatomic Defect On Pelvic Floor & UrogynecologyDokument1 SeiteCase 4 Anatomic Defect On Pelvic Floor & Urogynecologycbac1990Noch keine Bewertungen
- Gyne - Case 06 Secondary Amenorrhea (Hyperandrogenism)Dokument2 SeitenGyne - Case 06 Secondary Amenorrhea (Hyperandrogenism)cbac1990Noch keine Bewertungen
- Case 2 Pre-Op & Post-Op CareDokument1 SeiteCase 2 Pre-Op & Post-Op Carecbac1990Noch keine Bewertungen
- Gyne - Case 05 Abnormal Uterine BleedingDokument3 SeitenGyne - Case 05 Abnormal Uterine Bleedingcbac1990Noch keine Bewertungen
- Case 3 Congenital Anomalies, Primary AmenorrheaDokument3 SeitenCase 3 Congenital Anomalies, Primary Amenorrheacbac1990Noch keine Bewertungen
- AMC-Residency CV Worksheet-III PDFDokument1 SeiteAMC-Residency CV Worksheet-III PDFcbac1990Noch keine Bewertungen
- Case 9 Infertility PDFDokument4 SeitenCase 9 Infertility PDFcbac1990Noch keine Bewertungen
- Case 3 Congenital Anomalies, Primary AmenorrheaDokument3 SeitenCase 3 Congenital Anomalies, Primary Amenorrheacbac1990Noch keine Bewertungen
- Case 1 History & PEDokument3 SeitenCase 1 History & PEcbac1990Noch keine Bewertungen
- PTAL Residency CaliforniaDokument24 SeitenPTAL Residency Californiacbac1990Noch keine Bewertungen
- BBL CrystalDokument9 SeitenBBL CrystalYsrad Dante RmzNoch keine Bewertungen
- Cell Wall Synthesis Inhibitors (CompleteDokument44 SeitenCell Wall Synthesis Inhibitors (CompletegrayNoch keine Bewertungen
- Introduction of Klebsiella PneumoniaeDokument189 SeitenIntroduction of Klebsiella PneumoniaeAnia sahaNoch keine Bewertungen
- Ceftriaxone ResistantDokument5 SeitenCeftriaxone ResistantRafiq EsufzaeNoch keine Bewertungen
- 2015 - Laboratory Based Nationwide SurveillanceDokument12 Seiten2015 - Laboratory Based Nationwide SurveillanceYulia HandayaniNoch keine Bewertungen
- Industrial Production of Beta-Lactam AntibioticsDokument8 SeitenIndustrial Production of Beta-Lactam AntibioticsSyarif AlmubarakNoch keine Bewertungen
- Antibiotics, Misuse and ConsequencesDokument67 SeitenAntibiotics, Misuse and Consequencestummalapalli venkateswara raoNoch keine Bewertungen
- 10.beta Lactamase InhibitorsDokument15 Seiten10.beta Lactamase InhibitorsJagirNoch keine Bewertungen
- Maria BJ Theresa A. Aque Alan Louise Y. Bualat Umaynah E. AhmedDokument35 SeitenMaria BJ Theresa A. Aque Alan Louise Y. Bualat Umaynah E. AhmedMaria BJ Theresa AqueNoch keine Bewertungen
- M C - A P: Clinical PracticeDokument7 SeitenM C - A P: Clinical PracticeKak DhenyNoch keine Bewertungen
- AntibioticsDokument17 SeitenAntibioticsnehal.nehal92Noch keine Bewertungen
- Infectiuos Disease PDFDokument248 SeitenInfectiuos Disease PDFntnquynhpro0% (1)
- AntibioticsDokument6 SeitenAntibioticsyezan27100% (8)
- Dipslides vs Contact Plates for Hospital Environmental SamplingDokument6 SeitenDipslides vs Contact Plates for Hospital Environmental SamplingIwan RidwantoNoch keine Bewertungen
- ATCC Multidrug Resistant Antimicrobial Resistant Strains 1689505028Dokument20 SeitenATCC Multidrug Resistant Antimicrobial Resistant Strains 1689505028Ralf Kevin Piano,RMTNoch keine Bewertungen
- Fosfomycin-An Old-New AntibioticDokument4 SeitenFosfomycin-An Old-New Antibioticvetma1Noch keine Bewertungen
- Pharma Lecture With Dr. Maria Yña Eluisia T. Pereyra-Borlongan 1Dokument13 SeitenPharma Lecture With Dr. Maria Yña Eluisia T. Pereyra-Borlongan 1Sammy GirlNoch keine Bewertungen
- Cefiget-Range-Leaflet-PakistanDokument2 SeitenCefiget-Range-Leaflet-PakistanZafran KhanNoch keine Bewertungen
- Pneumonia Pathway Final 2010 Rev4Dokument7 SeitenPneumonia Pathway Final 2010 Rev4lyuen600Noch keine Bewertungen
- Nursing Care Note PharmaDokument6 SeitenNursing Care Note PharmaamitNoch keine Bewertungen
- Nelson's Pediatric Antimicrobial Therapy 24th Edition 2018Dokument325 SeitenNelson's Pediatric Antimicrobial Therapy 24th Edition 2018Eduardo Rios Dubois100% (2)
- CIDSCON 2017 - AbstractsDokument179 SeitenCIDSCON 2017 - AbstractsMohammad AlthafNoch keine Bewertungen
- Augmentin Duo TabletsDokument12 SeitenAugmentin Duo TabletsAshish SharmaNoch keine Bewertungen
- Pharmaceutical Organic Chemistry - RED PACOP FinalDokument452 SeitenPharmaceutical Organic Chemistry - RED PACOP FinalHaze GrayNoch keine Bewertungen
- BP 601T MCQ Unit1Dokument27 SeitenBP 601T MCQ Unit1Swati PwarNoch keine Bewertungen
- BCCA Febrile Neutropenia GuidelinesDokument2 SeitenBCCA Febrile Neutropenia GuidelinesdenokayuMRNoch keine Bewertungen
- BP601T Unit 1-3Dokument668 SeitenBP601T Unit 1-3Solomon GyampohNoch keine Bewertungen
- Sabrina Püntener-Simmen, Katrin Zurfluh, Sarah Schmitt, Roger Stephan and Magdalena Nüesch-InderbinenDokument8 SeitenSabrina Püntener-Simmen, Katrin Zurfluh, Sarah Schmitt, Roger Stephan and Magdalena Nüesch-InderbinenRamón RicardoNoch keine Bewertungen
- 2019 Book PolymyxinAntibioticsFromLaboraDokument364 Seiten2019 Book PolymyxinAntibioticsFromLaboraDaniel JiménezNoch keine Bewertungen
- Organic Medicinal and Pharmaceutical Chemistry AUDokument109 SeitenOrganic Medicinal and Pharmaceutical Chemistry AUAshley DayagNoch keine Bewertungen