Beruflich Dokumente
Kultur Dokumente
+ Rhodes - A Systematic Approach To Clinical Moral Reasoning (Clinical Ethics 2007)
Hochgeladen von
Mercea AlexOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
+ Rhodes - A Systematic Approach To Clinical Moral Reasoning (Clinical Ethics 2007)
Hochgeladen von
Mercea AlexCopyright:
Verfügbare Formate
Clinical
Ethics
http://cet.sagepub.com/
A systematic approach to clinical moral reasoning
Rosamond Rhodes and David Alfandre
Clinical Ethics 2007 2: 66
DOI: 10.1258/147775007781029582
The online version of this article can be found at:
http://cet.sagepub.com/content/2/2/66
Published by:
http://www.sagepublications.com
Additional services and information for Clinical Ethics can be found at:
Email Alerts: http://cet.sagepub.com/cgi/alerts
Subscriptions: http://cet.sagepub.com/subscriptions
Reprints: http://www.sagepub.com/journalsReprints.nav
Permissions: http://www.sagepub.com/journalsPermissions.nav
>> Version of Record - Jun 1, 2007
What is This?
Downloaded from cet.sagepub.com at Romanian Science Academy on May 22, 2013
CE07.19
6/4/07
12:15 pm
Page 1
CASE STUDIES
A systematic approach to clinical moral reasoning
Rosamond Rhodes1 and David Alfandre2
1
Department of Medical Education and 2Department of Medicine, Mount Sinai School of Medicine, New York, USA
Email: rosamond.rhodes@mssm.edu
Abstract
Because the process of moving from moral principles and facts to action-guiding moral conclusions
has not been articulated clearly enough to be useful in a practical way, we designed a systematic
approach to aid learners and clinicians in their application of ethical principles to the resolution of
clinical dilemmas. Our model for clinical moral reasoning is intended to provide a clear and replicable
structure that makes the thought process involved in reasoning about clinical cases explicit. In this
paper we present the model and demonstrate how it can be used in three clinical cases.
An understanding of the basic principles and concepts of
medical ethics is critically important for navigating the
ethical dilemmas that arise in clinical medicine. Yet clinicians also need to develop skills in recognizing ethical
problems in clinical practice and understanding how the
principles can be used to guide practice. In the medical
ethics literature, numerous authors offer advice on how to
resolve moral problems, some in terms of principles,1,2
some in terms of rules,3 some in terms of virtues4 and others in terms of the kinds of information that should be
collected.5 There have, however, been few attempts to
describe the process of moving from principles, rules,
virtues, and facts to action-guiding moral conclusions,6,7
and even there the details have not been articulated
clearly enough to be useful in a practical way. Because we
see a need for more guidance, we have designed a template for clinical moral reasoning that is intuitively compelling. It incorporates philosophical insights framed in a
structured thought process that is styled after the systematic approaches to medical thinking that clinicians are
trained to employ. We expect that this model will be useful for clinicians, ethics committee members, and in medical education with learners who are already familiar with
the basic concepts of medical ethics. This approach is
deliberately formulated to work with a range of similar
terms that convey the key concepts of medical ethics.
We have been using this model at the Mount Sinai
School of Medicine as a targeted educational intervention
specifically designed to help house staff members learn to
understand and manage clinical ethical dilemmas.
Medical teams identify cases that raise ethical issues and
Rosamond Rhodes PhD is Professor of Medical Education and Director
of Bioethics Education at the Mount Sinai School of Medicine and
Professor of Philosophy at The Graduate Center, CUNY. She writes on a
broad array of issues in bioethics. She co-edited The Blackwell Guide to
Medical Ethics (2007), Medicine and Social Justice: Essays on the Distribution
of Health Care (2002) and Physician Assisted Suicide: Expanding the Debate
(1998).
David Alfandre MD MSPH is a General Internist in the Department of
Medicine at the Mount Sinai School of Medicine. He divides his time
between patient care, research and resident teaching.
arrange a conference for their discussion. Typically, the
cases are chosen because the team experiences them as a
mess that cannot be resolved with the standard tools of a
medical armamentarium. Conference leaders distribute a
pocket-sized laminated index card with a template for our
model for clinical moral reasoning on one side and use it
to guide the medical team through the process of defining,
analysing, and resolving the ethical dilemma8 (Box 1).
The leaders role is also to clarify concepts, explain relevant legal constraints, and keep the discussion on topic so
that the conference can be concluded within its allotted
time.
At the beginning of a session, a conference leader
explains the goals, then a member of the team presents the
major clinical details of the case focusing on how they
relate to the moral problem. Other team members contribute information from their own experience with the
patient. The clinical chart is also available if needed.
During the discussion the leaders repeatedly draw
attention to the index card outline. Our faculty have
become familiar with the concepts over a long period of
working and teaching medical ethics together with different learner groups and in a variety of settings. Without
that background, however, the model does require some
explanation and justification. In what follows, we shall
explain the reasoning that lies behind each step in our systematic approach and elaborate on what each step entails.
Collect all relevant data that could
help to answer your question
The complete set of data should certainly include the
medical factors such as diagnosis, prognosis and treatment
options. It will also be crucial to ascertain the patients
preferences. Often it is important to be informed about
legal and institutional policy matters and familiar with
codes and principles of medical ethics and the relevant
guidelines from professional societies.9
Communication skills and moral imagination, in addition to medical skills, are important tools in gathering this
data. Careful listening and attending to the responses of
the patient and family helps to inform a deep understand-
Clinical Ethics 2007; 2: 6670
Downloaded from cet.sagepub.com at Romanian Science Academy on May 22, 2013
CE07.19
6/4/07
12:15 pm
Page 2
A systematic approach to clinical moral reasoning
67
Box 1 How to approach a clinical ethical dilemma*
Collect all relevant data that could help to resolving your
question.
Identify the basic principles involved and explain how
they relate to the case.
Consider whether principles conflict in this situation or
whether there is uncertainly about what a particular
principle (e.g. beneficence, respect for autonomy) directs
you to do.
Formulate a question that reflects the conflict.
Decide which principle should have priority in this case
and support that choice with factors relevant to the case,
or find an alternative that avoids the dilemma.
When uncertainty persists, note whether there is some
missing information that would help you to resolve the
dilemma. Which information? How will it help to resolve
the dilemma?
Evaluate your decision by asking if it is what a consensus
of exemplary doctors would agree to do.
Plan the practical steps that you should take, focusing on
the details of the case and the future issues that you
foresee.
* This model has developed through ongoing
conversations of the ethics faculty and through the efforts
of the faculty and Ethics Fellows involved in the design and
implementation of our ethics assessment activities,
COMPASS-1&2. We are particularly grateful for the input
of: Steven Birnbaum, Erica Friedman, Nada Gligorov, Joseph
Goldfarb, Kurt Hirschhorn, James Hitt, Ian Holzman,
Thomas Kalb, David Muller, Richard Stein, Christine Vitrano
ing of the facts in the particular context. Discussion of the
full context of the data is necessary for developing an
appreciation of the needs of the patient and family.
Information that is not addressed during the initial clinical
case presentation is added as it becomes important to the
discussion. Typically, an assessment of the patients capacity or the identification of a health care proxy are part of
the data set that could be important in resolving the clinical moral dilemma. Details of the social history, including
descriptions of the richness or absence of family relationships, baseline mental and physical function, and the
home environment should also be incorporated into this
portion of the discussion.
nently in their case. Relating the principles to the case
encourages clarification of the concepts and promotes
understanding of just why the concept is an important
component of clinical medical ethics.
Consider whether principles conflict
in this situation, or whether there is
uncertainly about what a particular
principle directs you to do
Once the principles are clearly identified and understood,
it is easy to appreciate why the case presents a moral
dilemma. This piece of the exercise allows participants to
recognize that moral problems frequently involve two
important principles of medical ethics that cannot both be
satisfied at once. It also allows participants to see how the
clash between principles gives rise to moral conflict when
two important principles direct physicians to opposing
courses of action. Sometimes, however, it may be unclear
as to what a single principle (e.g. beneficence) requires in
the situation. Requiring the team to explicitly identify the
conflict begins the process of reasoning to a resolution and
delineates the parameters for the conversation that follows.
Formulate a question that reflects the
conflict
According to our template, the next step which is analogous to the identification of a chief complaint in clinical
medicine requires the team to identify the main ethical
question. This helps them to focus the discussion on the
key dilemma, that which forms the crux of the problem. A
clearly formulated question guides the crucial discussion
that follows. Once the several relevant principles are identified and discussed, formulating a question is usually
rather straightforward. Occasionally, in an especially complex case, two or three dilemmas may be involved, so several different questions may have to be formulated.
Box 2 Some principles / duties / concepts of medical ethics
Identify principles, duties and
concepts involved, and explain how
they relate to the case
Asking participants to identify the principles that are at
issue helps them to appreciate the conflict and to focus on
the controversy raised by the case. For easy reference and
to help participants recall important concepts and duties
of medical ethics, we provide a list on the flip side of the
index card (Box 2). This list is neither intended to be in
any way definitive nor intended to connote any theoretical commitment to one sort of entity over another, but
merely to serve as a shorthand reminder of an assortment
of concepts, principles, rules, virtues, duties and hazards.
The items on the list were chosen for their salience and
frequent relevance in clinical medicine. Typically, a team
is able to identify two or three concepts that arise promi-
Duty to provide care
Assess decisional capacity
Confidentiality
Assess surrogate appropriateness
Truth telling
Respect for autonomy (patient goals)
Minimize harms
Beneficence/caring (team goals)
Duty to warn
Non-judgmental regard
Professionalism
Trust/fiduciary responsibility
Informed consent
Justice (fair allocation of scarce resources)
Justified paternalism
Futility (furthers no goals)
Note conflict of interest
Professional competence
Evidence-based practice
Responsibilities to peers and institutions
Clinical Ethics
Downloaded from cet.sagepub.com at Romanian Science Academy on May 22, 2013
2007
Volume 2
Number 2
CE07.19
6/4/07
12:15 pm
Page 3
68
Rhodes and Alfandre
Decide which principle should have
priority in this case, and support that
choice with factors relevant to the
case, or find an alternative that avoids
the dilemma
sulting with peers and adhering to the basic principles of
medical ethics which constitute the ethical standard of
care. Physicians who make this question a touchstone of
their clinical practice exemplify medical professionalism.
It is reasonable to presume that all team members share a
commitment to the principles of medical ethics.
Nevertheless, they may prioritize them differently or see
the relevance of some as more important than others in
the case at hand. They may also have different views about
the place of the patients preferences in determining how
to proceed. Recognizing that members of the team may
give priority to different values and that the clinicians
ranking may be different from the patients is a vital feature of this exercise. Participants should note that the
medical teams primary goal may be different from that of
the patient or family and that the team and the family may
share goals yet disagree on how to achieve them. This
insight is an important starting point for the medical
teams clear and ongoing communication with the patient
and family and with one another.
It is useful to see choosing the goal to pursue as a process of communicating together to reach an acceptable
course in a difficult and unfolding situation rather than as
an exercise in dispute resolution between antagonistic and
opposing parties. In most cases, the patient, the family and
the medical team all want the same thing: the patients
good. There may, nevertheless, be legitimate disagreement
about what that entails. Reaching agreement about what
to do requires all of those involved to come to share reasons for following a particular course. Consensus can only
be achieved through a free and open discussion where
everyone has the opportunity to explain their concerns,
ask questions, challenge assumptions, introduce previously
overlooked factors, offer suggestions, and consider options.
Such a process may sometimes yield a creative solution
that avoids sacrificing either side of the dilemma.
When uncertainty persists, note whether there is some
missing information that would help you to resolve the
dilemma. Which information? How will it help to resolve
the dilemma?
There will be times when no consensus on how to proceed emerges from the discussion. Then, as in a situation
where the diagnosis remains elusive, the team has to consider what further information could be useful in answering the outstanding questions and make efforts to obtain
it. Some missing but crucial information may be medical
(e.g. the diagnosis, life expectancy with such a condition),
other required information may be personal or social (e.g.
are there any long-term care facilities near the family
home that will provide both tube feeding and ventilator
support). When pieces of information are critical to the
case, a decision cannot be reached without them.
Plan the practical steps that you
should take, focusing on the details of
the case and the future issues that you
foresee
Evaluate your decision by asking what
a consensus of exemplary doctors
would agree to do
Clinicians justify their treatment decisions by referring to
the standard of care. The same should hold true with the
ethical choices that clinicians are required to make.
Questions of clinical medical ethics are not resolved by an
individual consulting his/her heart of hearts, but by conClinical Ethics
2007
Volume 2
It is important for the participants to appreciate that they
need to do the right thing and that they also have to do it
in the right way. Once a course of action is agreed upon, it
is time for planning just how to proceed. Forethought is
required to plan for the anticipated eventualities and complications. For example, the appointment of a proxy by a
patient with a deteriorating medical condition or a discussion of blood transfusions with a pregnant Jehovahs
Witness could be important steps in ensuring that the
patients goals are achieved. The ability to communicate
effectively with patients, families and colleagues is also an
important part of this process.
Putting the model to work
To illustrate how our model can be employed, consider
these examples from actual case conferences. The first
illustrates conflicting direction from a single principle; the
second the resolution of a clash between two important
principles; the third a case where the dilemma could not
be resolved without additional information.
Case 1
An 84-year-old man with end-stage metastatic colon cancer
was admitted to the hospital with persistent nausea and vomiting. An initial evaluation revealed a large bowel obstruction
due to the progression of the primary colonic mass. After placement of a naso-gastric tube for decompression, a surgical consult was requested to evaluate him for surgical palliation of the
obstruction. He had previously undergone a course of surgery
and chemotherapy, but the cancer recurred after three years.
Before this hospitalization, the patient had been living independently at home with his wife. The patient had designated his
wife as his health care proxy and he had also expressed his
desire to return home with his wife. The medical team wanted
to honour the patients wishes, but they were unsure whether
that included exposing him to the risk of surgery.
In this case beneficence was identified as the central
concept involved. It was, however, not at all obvious just
what course a commitment to beneficence directed. The
question that the team formulated was therefore, Should
surgery be performed or avoided for this man with endstage cancer patient and a bowel obstruction?. Because
the patients condition was acute, there was little time for
waiting or for gathering additional data.
After discussion of the patients prognosis, the treatment alternatives, and the likely consequences of each
option, it was clear that there was no distinctly best or
worst course for him. It seemed that none of the options
would assure that he could return home to a significant
period of the life he had enjoyed. The choice of which
route to follow turned on how one might rank the harms
Number 2
Downloaded from cet.sagepub.com at Romanian Science Academy on May 22, 2013
CE07.19
6/4/07
12:15 pm
Page 4
A systematic approach to clinical moral reasoning
69
and benefits of each path. Surgery might give the patient
the best chance of returning home for a significant period
of time, but it could also hasten his death or leave him to
endure complications and a prolonged dying process.
Rejecting surgery would involve a sooner death than he
might have with a successful surgery. Appreciating that
there were no optimal alternatives and that there were no
clear medical reasons for ranking one alternative over the
other made it easy for the team to accept the idea that the
resolution of this case turned on a ranking of the personal
priorities of those who were most immediately affected by
the decision. They concluded that the options had to be
explained to the patient and his wife and that the couple
had to be offered the teams support in which ever option
they chose.
This case illustrates how several different answers may
be ethically acceptable and there need not be a single
right answer.
Case 2
A 78-year-old high-functioning woman with congestive heart
failure, chronic renal insufficiency, and decubitus ulcers was
admitted to the hospital because of an exacerbation of heart failure. She had been living with her sister for 30 years, and when
her illness recently worsened, her sister became her primary
care giver. The sister, who was also designated as the patients
health care proxy, was present in the hospital daily where she
made significant personal efforts to clean and debride her sisters
decubiti, using non-traditional and unsanitary methods. The
sister refused both nurse and physician requests to leave these
procedures to the hospital staff. The patient never made any
attempt to intervene with her sisters behaviour, and she did not
raise any objections to it.
The patient did not respond to the treatment for her heart
failure and her renal insufficiency worsened to the point of
uraemia requiring dialysis. In spite of treatment, the patients
mental status worsened from the uraemia. At this point the
patients prognosis was poor.
As the patient lay in bed obtunded, the sister refused to
allow the resident physicians to enter the room for an evaluation, although she did allow the attending senior physician. In
spite of maximal medical therapy, the patient eventually developed irreversible multi-organ failure due to her severe progressive cardiac and renal disease. After discussion with the medical
team, the sister agreed to pursue palliative care for the patients
shortness of breath and declining level of consciousness, which
she said was consistent with the patients prior wishes.
Using our systematic approach to clinical ethics, the
basic concepts involved in this case were identified as
beneficence, respect for autonomy, assess decisional capacity and surrogate decision making. Beneficence was noted
in the teams insistence that the patients welfare was
paramount. So long as first the patient, and later the sister,
had decisional capacity, respect for autonomy required
their decisions be accepted. Team members had raised
important questions about the patients decisional capacity
early on in her hospitalization, whether factors related to
her illness, such as depression, fear, anxiety and dependence, as well as her medical illness, may have impaired
her ability to meaningfully participate in the treatment
decision process. They also raised questions about the sisters involvement. Her behaviour suggested to them that
she may not have been acting in the patients best interest.
Even though the patient did not object to her sisters
interventions, the team considered whether they should
have allowed them. If the patient actually had decisional
capacity, the sisters behaviour could be accepted because
it was consistent with the patients stated preference. But
as the patients mental status declined, the sisters decisions became more of an issue. One concern was whether
or not the sister actually had decisional capacity herself.
Ultimately, the ethical question that they formulated
was, Should the medical team abide by the surrogates
decisions?. In this case, although there was clash between
the principles of beneficence and respect for autonomy, a
crucial dilemma concerned the capacity of both the
patient and her sister. Even after lengthy discussion of
whether or not the patient had capacity before she developed severe uraemia, and whether or not the sister had
decisional capacity, the answers remained in doubt. When
dealing with a surrogate decision, clinicians have to evaluate both the surrogate and the surrogates decisions. In this
case, the surrogate certainly demonstrated appropriate
concern for the patients well being, and while her strange
behaviour raised questions about her capacity, it did not
quite rise to the level of demonstrating a lack of capacity.
Because there was no medical intervention that could
have significantly reversed the patients inevitable decline,
the surrogates decisions would not change the outcome in
any appreciable way. Therefore, the group concluded that
any exemplary physician in such a situation should accept
the sister as an appropriate surrogate and abide by her
decisions.
To proceed, they decided to focus on improving communication with the surrogate. This approach was deemed
preferable to more strong-arm confrontational techniques
to achieve the best possible outcome, which would not
make much of a difference in the ultimate result. The
team reasoned that disrupting the enduring relationship
between the patient and her sister would do more harm
than good and interfere with the trust in clinicians that
was essential to providing any beneficial interventions for
the patient.
Case 3
A 56-year-old woman who was employed as a home health aide
was admitted to the hospital with a cocaine-associated myocardial infarction. Three months earlier she had been admitted
with the same diagnosis. No grossly evident heart damage was
detected. The inpatient medical team was, however, concerned
that the patients cocaine use exposed her clients to harm. They
were also concerned that notifying her employer would violate
their patients confidentiality.
Further information was presented about the extent of
the patients drug use and the likelihood of her using
cocaine in the future. She was thought to have a drug
abuse illness because she had continued her use of cocaine
despite missing work and sustaining a previous myocardial
infarction.
Confidentiality and duty to warn, particularly in the
case of a health care professional, were identified as the
key principles involved. It was noted that the well-recognized importance of safeguarding the patients confidentiality-protected health information conflicted with the
Clinical Ethics
Downloaded from cet.sagepub.com at Romanian Science Academy on May 22, 2013
2007
Volume 2
Number 2
CE07.19
6/4/07
12:15 pm
Page 5
70
Rhodes and Alfandre
importance of protecting the patients wards from the possibility of her potentially negligent behaviour. The extensive discussion of the principles and their relevance to this
case made the source of the dilemma very clear. The special opportunities for abuse that arise from providing
health care in the unsupervised home setting were also
noted as being particularly relevant to this case. Using the
card to guide the discussion, the group formulated their
question: In order to mitigate harm, should the medical
team notify the patients employer about her cocaine use
when the patient does not want that information disclosed?.
The patients goal was to return to her work. She did
not want to directly address her substance abuse and she
wanted to keep her medical problems confidential. Yet the
medical team wanted to ensure the safety of her wards.
They were also sensitive to the importance of safeguarding
the patients confidentiality and to the fact that revealing
confidential information could undermine her willingness
to pursue needed treatment in the future.
The team also noted that many people who work as
home care providers are not actually professionals in the
sense of having participated in a special educational programme, being licensed by the state, and being accorded
the powers and privileges of a health care professional, or
even having an agency employer. Because this seemed to
be a key point in determining a course of action, the team
resolved to investigate the matter in detail with the
patient. It was decided that if she was, in fact, a health
care professional, that they would have a professional duty
to report her drug use to the State, but that reasons for
reporting would be far less compelling if she was not a
health care professional.
Another critical concern was the assessment of the
danger to our patients patients. The team identified two
components of this issue. Because they envisioned that the
patient could be working without direct supervision or
oversight in the home of someone who could be significantly impaired, and therefore vulnerable to neglect or
abuse, they were concerned about the danger that their
patient could present to the health and well being of her
charge(s) just by being in the home. They were also concerned about whether their patients drug use would affect
her behaviour or impair her judgement while at work. To
make a decision about reporting the patient or safeguarding her confidentiality, they decided that both of these
issues had to be explored further and that any exemplary
physician should take that path. Once they knew more of
the details about the patients use of cocaine and the situation in which she was employed they would be in a better
position to reach a decision. Yet, even after fact finding,
because the information was likely to remain incomplete
and somewhat unreliable, it would be hard to have confidence in any decision.
Further investigation revealed that the patient was
not a health professional in any official sense and she did
not work for any health care agency. She was therefore not
subject to the professional standards expected from
Clinical Ethics
2007
Volume 2
providers in fiduciary relationships with patients, and the
team had no duty of professional oversight that required
reporting her drug use. Upon questioning, the patient
explained that her work involved taking care of an elderly
man who lived with his extended family. She also confided
that she used cocaine only at weekend parties. Based on
that information about the patients drug use pattern and
her work situation, the team concluded that it was reasonably safe to maintain the patients confidentiality. The
team continued with the practical strategy of recommending that the patient obtain treatment for her substance
abuse problem, and offering assistance in providing access
to such services.
Conclusions
Our systematic approach to clinical moral reasoning is
specifically designed as a guide for health professionals and
ethics committee members. It is structured to function as a
tool for navigating the common ethical dilemmas that
arise in the inpatient and outpatient clinical setting by
providing a clear and replicable structure that makes
explicit a thought process that was previously only intuitive. Although conference participants had sometimes
reached similar conclusions about what to do prior to the
conference and without the aid of the systematic
approach, the model explained why the conclusion was
appropriate to the case and provided confidence in the resolution.
We expect that learning to use the model will facilitate participants ability to navigate future ethical dilemmas, provide them with a basis for assessing their intuitive
convictions about other cases, and become a means for
approaching the dilemmas that they find most puzzling. In
these ways, we expect that our template for clinical moral
reasoning will provide clinicians with a structure on which
to build and be useful to them in the future when they
encounter complicated clinical ethics dilemmas.
References
1 Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 5th edn.
New York: Oxford University Press, 2001
2 R Gillon. Education and debate, Medical ethics: four principles plus
attention to scope. BMJ 1994;309:184
3 Gert B, Culver R, Clouser KD. Bioethics: A Systemic Approach. New
York: Oxford University Press, 2006
4 Pellegrino ED, Thomasma DC. The Virtues in Medical Practice. New
York: Oxford University Press, 1993
5 Jonsen AR, Siegler M, Winslade WJ. Clinical Ethics. 6th edn. New
York: McGraw-Hill, 2002
6 Lo B. Resolving Ethical Dilemmas: A Guide for Clinicians. San
Francisco: Lippincott, 2005
7 Kaldjian L, Weir R, Duffy T. A clinicians approach to clinical ethical reasoning. J Gen Intern Med 2005;20:30611
8 The following faculty members have served as leaders of these clinical conferences: David Alfandre, Thomas Kalb, David Muller,
Rosamond Rhodes and Richard Stein
9 In conversation, Robert Baker pointed out the importance of consulting professional codes and ethics statements
Number 2
Downloaded from cet.sagepub.com at Romanian Science Academy on May 22, 2013
Das könnte Ihnen auch gefallen
- Medical Ethics EssayDokument7 SeitenMedical Ethics EssaylettersforjulieNoch keine Bewertungen
- Metatron Resonance Brochure WebsiteDokument3 SeitenMetatron Resonance Brochure WebsiteShaun DennisNoch keine Bewertungen
- Understand Cancer & Reduce Cancer Risk - Based On The Teachings Of Dr. Andrew Huberman: Empowering You To Safeguard Against ItVon EverandUnderstand Cancer & Reduce Cancer Risk - Based On The Teachings Of Dr. Andrew Huberman: Empowering You To Safeguard Against ItNoch keine Bewertungen
- Drug Addiction Treatment and Rehabilitation-Imran Ahmad SajidDokument108 SeitenDrug Addiction Treatment and Rehabilitation-Imran Ahmad Sajidimranahmadsajid0% (1)
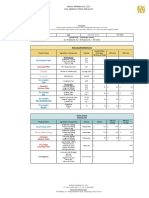
- 2021 Nexus Pharma Injection Price List FinalDokument5 Seiten2021 Nexus Pharma Injection Price List FinalRyu SanurNoch keine Bewertungen
- How To Achieve Good Health & Longevity?Dokument57 SeitenHow To Achieve Good Health & Longevity?lauchen32100% (1)
- The Accuracy of Substituted Judgments in Patients With Terminal DiagnosesDokument9 SeitenThe Accuracy of Substituted Judgments in Patients With Terminal DiagnosesgremnisayNoch keine Bewertungen
- Theory and Application of Law and Ethical Reasoning in Nursing Practice - EditedDokument15 SeitenTheory and Application of Law and Ethical Reasoning in Nursing Practice - EditedKristin Muriuki100% (1)
- Health Care Ethics 2024Dokument13 SeitenHealth Care Ethics 2024celestineNoch keine Bewertungen
- Orthodontics!!Dokument9 SeitenOrthodontics!!Ayesha AwanNoch keine Bewertungen
- Neurology Case SheetDokument9 SeitenNeurology Case SheetAshwaq TpNoch keine Bewertungen
- Capstone OutlineDokument2 SeitenCapstone Outlineapi-282099234Noch keine Bewertungen
- E Learning Geriatric Oncology An IntroductionDokument65 SeitenE Learning Geriatric Oncology An IntroductionHarold JeffersonNoch keine Bewertungen
- Medical Ethics Manual En.2ndedition2009Dokument140 SeitenMedical Ethics Manual En.2ndedition2009giosancristianNoch keine Bewertungen
- NURS 12 - ReviewerDokument8 SeitenNURS 12 - ReviewerRina Lyzea PunongbayanNoch keine Bewertungen
- NMBA Case Studies Code of Conduct For Nurses and Code of Conduct For MidwivesDokument7 SeitenNMBA Case Studies Code of Conduct For Nurses and Code of Conduct For Midwivestom doyleNoch keine Bewertungen
- FP TrainedProviders 2Dokument9 SeitenFP TrainedProviders 2Bharma LogisticsNoch keine Bewertungen
- EthicsDokument48 SeitenEthicsTadesse Fenta100% (1)
- (Bioethics) Introduction of EthicsDokument2 Seiten(Bioethics) Introduction of EthicsVivien IgnacioNoch keine Bewertungen
- German Marine Agencies, Inc., Et Al. Petitioners, vs. Teodolah R. Caro, in Behalf of Her Husband Eduardo v. Caro, Respondent.Dokument5 SeitenGerman Marine Agencies, Inc., Et Al. Petitioners, vs. Teodolah R. Caro, in Behalf of Her Husband Eduardo v. Caro, Respondent.Francis Coronel Jr.Noch keine Bewertungen
- Post Dam and Relief Chamber FullDokument35 SeitenPost Dam and Relief Chamber FullnaomiNoch keine Bewertungen
- NHS-FPX4000 Developing A Health Care PerspectiveDokument9 SeitenNHS-FPX4000 Developing A Health Care PerspectiveCate sizNoch keine Bewertungen
- Time To Learn. Understanding Patient Centered CareDokument7 SeitenTime To Learn. Understanding Patient Centered CareAden DhenNoch keine Bewertungen
- Autonomy Vs BeneficenceDokument2 SeitenAutonomy Vs Beneficencedr fikriNoch keine Bewertungen
- Beauchamp and Rauprich 2016 PDFDokument12 SeitenBeauchamp and Rauprich 2016 PDFRazero4Noch keine Bewertungen
- PH 251 PaperDokument7 SeitenPH 251 PaperfreeromanticsNoch keine Bewertungen
- Original EssayDokument3 SeitenOriginal EssayAj AquinoNoch keine Bewertungen
- K6-Ethical Aspect in Physicians and ColleaguesDokument15 SeitenK6-Ethical Aspect in Physicians and ColleaguesJamali GagahNoch keine Bewertungen
- Evidence Based Medicine: What It Is and What It Isn'tDokument3 SeitenEvidence Based Medicine: What It Is and What It Isn'tCristian EstradaNoch keine Bewertungen
- Mod 1 Theories and Principles of Healthcare EthicsDokument58 SeitenMod 1 Theories and Principles of Healthcare EthicsKelly Arceo100% (1)
- A Field Guide To Designing A Health Communication StrategyDokument308 SeitenA Field Guide To Designing A Health Communication StrategynonimugoNoch keine Bewertungen
- Ethics Applied in NursingDokument3 SeitenEthics Applied in NursingGil GanibanNoch keine Bewertungen
- Ethics AssignmentDokument3 SeitenEthics Assignmenttonydickpatakesseh100% (4)
- Evidence Paper JpeacottricardosDokument7 SeitenEvidence Paper Jpeacottricardosapi-302415380Noch keine Bewertungen
- Correctedintro Personal Philosophy of Nursing PaperDokument5 SeitenCorrectedintro Personal Philosophy of Nursing Paperapi-269170045Noch keine Bewertungen
- Intro Page - Philosophy of NursingDokument2 SeitenIntro Page - Philosophy of Nursingapi-467110214Noch keine Bewertungen
- Early Clinical Exposure (Ece)Dokument30 SeitenEarly Clinical Exposure (Ece)sandeepNoch keine Bewertungen
- Pta Observation ReflectionDokument5 SeitenPta Observation Reflectionapi-349410803Noch keine Bewertungen
- AdvocacyassignmentintropagefinalDokument3 SeitenAdvocacyassignmentintropagefinalapi-290938460Noch keine Bewertungen
- Nurs 403 Practice Summary PaperDokument17 SeitenNurs 403 Practice Summary Paperapi-369824515Noch keine Bewertungen
- Withholding and Withdrawing Life SupportDokument3 SeitenWithholding and Withdrawing Life SupportNURSETOPNOTCHERNoch keine Bewertungen
- Humanistic Nursing Theory: Application To Hospice and Palliative CareDokument9 SeitenHumanistic Nursing Theory: Application To Hospice and Palliative CareNYONGKERNoch keine Bewertungen
- Ethics and The Covid-19 Pandemic Everyday Challenges Uams LGG No NarrationDokument42 SeitenEthics and The Covid-19 Pandemic Everyday Challenges Uams LGG No Narrationapi-136237609Noch keine Bewertungen
- Annotated Bibliography On ADHDDokument6 SeitenAnnotated Bibliography On ADHDkepha otienoNoch keine Bewertungen
- Ethics in Research: Historical OverviewDokument9 SeitenEthics in Research: Historical OverviewJmarie Brillantes PopiocoNoch keine Bewertungen
- Recent Global Epidemiology in StrokeDokument73 SeitenRecent Global Epidemiology in StrokeratuhamimNoch keine Bewertungen
- ExtubationDokument7 SeitenExtubationbalab2311Noch keine Bewertungen
- Experiential Learning and AndragogyDokument7 SeitenExperiential Learning and Andragogychu_chiang_3Noch keine Bewertungen
- Essay - Health Insurance Portability and Accountability ActDokument4 SeitenEssay - Health Insurance Portability and Accountability ActPatrick TylerNoch keine Bewertungen
- Code of Ethics For NursesDokument5 SeitenCode of Ethics For NursesKamran Khan100% (1)
- Unit 29 Health PromotionDokument4 SeitenUnit 29 Health Promotionchandni0810100% (1)
- HypothesisDokument42 SeitenHypothesisGautam PoudelNoch keine Bewertungen
- Group ProtocolDokument5 SeitenGroup Protocolapi-455072421Noch keine Bewertungen
- NURS 328: Understanding Research: Assignment 1 Facilitating Evidence-Based Practice: Dissemination ProjectDokument11 SeitenNURS 328: Understanding Research: Assignment 1 Facilitating Evidence-Based Practice: Dissemination ProjectKuharaj TharmakulasinghamNoch keine Bewertungen
- Article For Journal 2Dokument5 SeitenArticle For Journal 2awuahbohNoch keine Bewertungen
- Educ638 CTP Reflectiveanalysis PhelpsDokument7 SeitenEduc638 CTP Reflectiveanalysis Phelpsapi-421981605Noch keine Bewertungen
- Modul 1Dokument30 SeitenModul 1Riyan WahyudoNoch keine Bewertungen
- Transition Theory - To Post.2015Dokument34 SeitenTransition Theory - To Post.2015LucasNoch keine Bewertungen
- Nursing Epistemological Stance 608 Assignment 2Dokument22 SeitenNursing Epistemological Stance 608 Assignment 2api-700386478Noch keine Bewertungen
- Course Reflection-Culture in NursingDokument6 SeitenCourse Reflection-Culture in NursingSserumaga JohnBaptistNoch keine Bewertungen
- Doctor-Patient Relationship: Dr. Truong Trong Hoang, M.DDokument44 SeitenDoctor-Patient Relationship: Dr. Truong Trong Hoang, M.DQuỳnh NguyễnNoch keine Bewertungen
- ProblembasedresearchpaperDokument7 SeitenProblembasedresearchpaperapi-449184986Noch keine Bewertungen
- Recommended Topics For PCORI Research On Multiple Chronic ConditionsDokument3 SeitenRecommended Topics For PCORI Research On Multiple Chronic ConditionsPartnership to Fight Chronic DiseaseNoch keine Bewertungen
- Human Becoming TheoryDokument7 SeitenHuman Becoming TheoryDelvianaNoch keine Bewertungen
- Nursing Philosophy Apa PaperDokument7 SeitenNursing Philosophy Apa Paperapi-449016836Noch keine Bewertungen
- Spirituality in Healthcare: Perspectives for Innovative PracticeVon EverandSpirituality in Healthcare: Perspectives for Innovative PracticeNoch keine Bewertungen
- Advances in Cattle WelfareVon EverandAdvances in Cattle WelfareCassandra TuckerNoch keine Bewertungen
- Ethical Challenges of Organ Transplantation: Current Debates and International PerspectivesVon EverandEthical Challenges of Organ Transplantation: Current Debates and International PerspectivesSolveig Lena HansenNoch keine Bewertungen
- Daftar PustakaDokument3 SeitenDaftar PustakaJessie NovaNoch keine Bewertungen
- Jurnal Ria Suak 091511195Dokument6 SeitenJurnal Ria Suak 091511195resyaNoch keine Bewertungen
- Ummer Roject Resentation ON Herbal Healthcare Industry in IndiaDokument14 SeitenUmmer Roject Resentation ON Herbal Healthcare Industry in IndiaSaurabh RustagiNoch keine Bewertungen
- Recovery Road (Excerpt)Dokument13 SeitenRecovery Road (Excerpt)I Read YA100% (1)
- Case Study AnalysisDokument13 SeitenCase Study Analysisapi-317809407Noch keine Bewertungen
- Nursing Practice IDokument45 SeitenNursing Practice IWilmaBongotanPadawilNoch keine Bewertungen
- Form 4 Medical Certificate For Non-Gazetted Officer Recommended For Leave or Extension or Commutation of LeaveDokument2 SeitenForm 4 Medical Certificate For Non-Gazetted Officer Recommended For Leave or Extension or Commutation of LeaveDr RajaNoch keine Bewertungen
- Antimicrobial Properties of Allicin From GarlicDokument3 SeitenAntimicrobial Properties of Allicin From GarlicEdward Kenneth DragasNoch keine Bewertungen
- Cicatrización ImplanteDokument18 SeitenCicatrización Implantejorge sepulvedaNoch keine Bewertungen
- Silver Is The New BlackDokument30 SeitenSilver Is The New BlackSeptriyani KaswindiartiNoch keine Bewertungen
- Ahuja, Motiani - 2004 - Current and Evolving Issues in Transfusion PracticeDokument8 SeitenAhuja, Motiani - 2004 - Current and Evolving Issues in Transfusion Practicesushmakumari009Noch keine Bewertungen
- Nurse Writing 016 OET Practice Letter Darryl MahnDokument3 SeitenNurse Writing 016 OET Practice Letter Darryl Mahnchoudharysandeep50163% (8)
- DRISHTIDokument1 SeiteDRISHTIsumitha SNoch keine Bewertungen
- The Effects of Skin Bleach in SocietyDokument8 SeitenThe Effects of Skin Bleach in SocietySalma BahNoch keine Bewertungen
- YogaDokument4 SeitenYogakunalNoch keine Bewertungen
- Optimum Detox Foot Pads, Natural Cleansing Ginger Detox Foot PatchesDokument1 SeiteOptimum Detox Foot Pads, Natural Cleansing Ginger Detox Foot PatchesBrooke GuntherNoch keine Bewertungen
- Aetna Insurance DecisionDokument13 SeitenAetna Insurance DecisionJeffStelling1Noch keine Bewertungen
- Effects of Vasopressors On Cerebral Circulation.6Dokument11 SeitenEffects of Vasopressors On Cerebral Circulation.6diego morenoNoch keine Bewertungen
- Case Study 103Dokument8 SeitenCase Study 103Jonah MaasinNoch keine Bewertungen
- Case Study For Beta Acute Lymphoblastic Leukemia (B-All)Dokument15 SeitenCase Study For Beta Acute Lymphoblastic Leukemia (B-All)Shakira HashimNoch keine Bewertungen
- User Manual For Applications Xformer Exe EnglishLightDokument51 SeitenUser Manual For Applications Xformer Exe EnglishLightNunoClaudinoNoch keine Bewertungen