Beruflich Dokumente
Kultur Dokumente
MitralStenosis in China
Hochgeladen von
annis fathiaCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
MitralStenosis in China
Hochgeladen von
annis fathiaCopyright:
Verfügbare Formate
2
Mitral Stenosis
DEFINITION
Mitral stenosis is condition of pathological narrowing of mitral valve.
Normal square area of mitral valve is 4-6 square cm. When it is reduced
to half of it, significant hemodynamic changes take place (Fig. 2.1).
ETIOLOGY
Commonest - Rheumatic heart disease
Rare causes
1. Congenital
2. Lutembachers syndrome (ASD withcongenital or acquired mitral
stenosis).
3. Infective endocarditis with large vegetations causing obstruction.
4. Endomyocardial fibrosis.
5. Hurlers syndrome.
6. Carcinoid malignant.
7. Methysurgide.
Pathology
1. Commissural fusion is the hall mark.
2. Thickening of leaflets and fibrosis.
3. Stenosis develops after a latest period of about 10 years.
Fig. 2.1: Mitral valve stenosis
Mitral Stenosis 13
HEMODYNAMICS OF MITRAL STENOSIS (FIG. 2.2)
I. Rise in left atrial pressure: Mitral valve narrowing- backflow rise in
LA pressure.
II. Pulmonary venous congestion: Raised LA pressure is transmitted back
to pulmonary veins (because no valves at their junction with LA)
thus increasing pressure in pulmonary venules and capillaries-fluid
transudate into interstitial space, alveoli and causes pulmonary
edema and engorgement of lymphatics. Congested bronchial veins
cause airway obstruction.
III. Rise in pulmonary artery pressure: Rise in pulmonary venous pressure
causes constriction of corresponding pulmonary arterioles eventually
causing pulmonary. Arterial HT.
IV. Redistribution of blood flow to upper lobes: High left atrial pressure and
high hydrostatic pressure affects lower lobe vessels most. So
pulmonary arterial vasoconstriction occurs most in lower lobes and
most of blood flow as a compensation is diverted to upper lobe.
V. Rt ventricular failure: Pulmonary arterial hypertension causes strain
to emptying of Rt.V and eventually Rt heart failure.
Left Ventricular Function Remains Normal
Fig. 2.2: Hemodynamics of mitral stenosis
CLINICAL PICTURE
Symptoms
Develop 10-20 years after initial rheumatic insult.
Dyspnea on exertion.
Orthopnea, paroxysmal nocturnal dyspnea and symptoms of acute
pulmonary edema.
14
Comprehensive Cardiology
Fatigue due to low cardiac output.
Palpitation due to AF
Hemoptysis due to various mechanisms.
Signs
I. Peripheral
II. Cardiovascular
I. Peripheral: Mitral facies with malar flush, and small volume pulse,
peripheral cyanosis.
II. Cardiovascular:
1. Tapping apical impulse.
2. Diastolic thrill may be present at the apex.
3. Parasternal heave due to RVH.
4. Auscultation (Fig. 2.3)
Loud I sound at apex.
Opening snap.
Mid diastolic murmur at apex.
Presystolic accentuation.
Mechanism and description of clinical features
Loud Ist sound: High left atrial pressure holds the mitral valve wide open
until the end of diastole and ventricular systole slams it shut.
Opening snap: Produced by sudden bellowing down of mitral cusps into
left ventricle at the end of isometric relaxation period.
Loud I sound and opening snap indicate that the valve is pliable and not
fibrosed or calcified.
Opening snap is a short, sharp, snapping and high pitched sound best
heard at apex but also heard over left lower parasternal area and may
extend to cardiac base .
Fig. 2.3: Auscultatory features of mitral stenosis
Mitral Stenosis 15
Diastolic murmur
Low pitched, described as rumble.
Begins with opening snap and has varying duration.
Usually occupies mid diastole.
Best heard with bell stethoscope in left lateral position with breath held
in expiration.
Usually grade 2 or 3 but may be loud or faint;
Usually accentuates before I heart sound.
Pre-systolic accentuation
Produced by LA contraction; may be absent in AF.
Not always absent in AF; persists in short diastole (due to high velocity).
How to demonstrate diastolic murmur in sub clinical MS?
After exercising the patient put him in left lateral and auscultate.
Pulmonary area
When pulmonary hypertension develops?
II heart sound splits,
P2 becomes loud,
Rarely Graham Steell murmur of pulmonary insufficiency occurs- caused
by dilatation of pulmonary artery.
All auscultatory features of pulmonary hypertension are listed below:
Loud P2, II heart sound split narrowly.
Pulmonary ejection click.
Ejection systolic murmur increasing with inspiration.
Graham Steell murmur early diastolic murmur at pulmonary area.
Murmur of tricuspid incompetence.
Rt atrial Gallop.
(Types of pulmonary hypertension occurring in mitral stenosis: 1. Passive.
2. Active ? 3. Organic obliteration of pulmonary vasculature)
Variability in auscultatory features- that may occur:
Soft I sound- rigid /cacific valve.
In severe MS, MDM may be absent/soft.
PSM absent when dominant mitral regargitation is pressure
Silent MS-Tight MS with large RV displacing LV posteriorly and so
masking the murmur.
Diagnostic Features
Loud I sound at apex
Opening snap
16
Comprehensive Cardiology
Low pitched rumbling mid diastolic murmur with presystolicaccentuation: best heard, with patient in left lateral position with breath
held in expiration.
Differential Diagnosis for Clinical Picture of Mitral Stenosis
1. LA myxoma,
2. Ball valve thrombus,
3. Cor triatriatum.
Left atrial myxoma - murmur varies with posture.
Differential DiagnosisFor Mid Diastolic Murmur
1. Mitral stenosis.
2. Tricuspid stenosis (murmur accentuating with inspiration)
3. Flow murmurs (caused by increased blood flow across the mitral or
tricuspid valve during diastole in the following)
Mitral regurgitation
Tricuspid regurgitation
ASD
VSD
PDA.
4. Carey coombs murmur: In acute rheumatic mitral valvulitis - functional
murmur.
5. Austin Flint murmur: Occurs in free aortic incompetence; functional
murmur mid diastolic murmur at apex (see Fig. 6.3).
Other Conditions Causing Loud I Sound
1. Tachycardia.
2. Hyperdynamic states (valve remains open at end diastole and is
forcibly closed by hyper contractile LV).
Other Conditions Causing Opening Snap
Tricuspid stenosis, myxoma.
Assessments in Mitral Stenosis
1.
2.
3.
4.
A.
Degree of stenosis (severity)
The mobility of mitral valve
Pulmonary hypertension
Presence of other lesions and dominance.
Degree of stenosis is assessed by:
1. S2 OS interval which is inversely proportional to severity
Usual range of S2- OS interval is 0.08 0.12 sec; 0.06 and less in
severe.
Mitral Stenosis 17
2. Duration of murmur: It is directly proportional to severity: longer
the duration severe the stenosis.
3. Degree of LA enlargement in X-ray and ECG and by Echo.
4. Presence of pulmonary hypertension in pure MS.
B. Mobility of valve is denoted by:
1. Presence of loud I sound
2. Opening snap
3. Absence of valve calcification.
In combined mitral lesion factors which denote dominant MS are:
Presence of opening snap
Loud I sound
Presystolic accentuation
Absence of III ht sound
(Which mitral lesion causes gaint LA? Mitral regurgitation).
Complications of mitral stenosis
I. Complications of pulmonary venous congestion
II. Complications of enlarged left atrium
III. Complications at valve level.
Complications of Pulmonary Venous Congestion
Paroxysmal nocturnal dyspnea
Acute pulmonary edema
Hemoptysis
Pulmonary arterial hypertension
Right heart failure
Precipitants of pulmonary edema: AF, pregnancy, exercise, emotion,
chest infection, anesthesia.
Complications of Enlarged Left Atrium
Atrial fibrillation deteriorates the condition suddenly.
LA thrombus formation with thromboembolic signs
Cerebral
Renal
Coronary
Peripheral
Leriches syndrome
Pressure on esophagus causing dysphagia
Pressure on L. recurrent laryngeal nerve causing hoarseness of voice
Ortners syndrome
Lifting up of L main bronchus causing emphysema.
18
Comprehensive Cardiology
Complications at Valve Level
Infective endocarditis rare.
Causes of hemoptysis: Rupture of bronchial vein, pulmonary edema
pulmonary infarct, bronchitis, PHT.
INVESTIGATIONS
X-ray Chest
Shows features of mitralisation of heart:
1. Straightening of left border of the heart (hypoplastic aorta, prominent
MPA, enlarged left atrial appendage, all these 3, come in line with LV
border and so straightening).
2. Features of pulmonary hypertension: Dialated main pulmonary artey,
narrowing of peripheral pulmonary arteries.
3. Featurers of pulmonary venous congestion: Thin short horizontal lines
just above costophrenic angle representing interlobar septae thickened
by edema and fibrosis-Kerley b lines near costophrenic angle;
perpendicular to pleural surface.
4. Pulmonary edema: Perihilar congestion, haziness spreading from hilum
to periphery bats wing appearance and nodular opacities.
5. LA enlargement seen as opacity within RA opacity.
6. Redistribution of blood from the base to the apex causing enlarged
upper lobe bronchial veins.
7. Left upper lobe bronchus elevated causing compensatory emphysema.
8. Hemosiderosis consequent feature of repeated pulmonary congestion
Barium Swallow
Enlarged LA causes esophageal indentation in right oblique view.
X-ray and barium swallow contraindicated in pregnancy.
ECG
P pulmonale/P mitral; RVH with Rt axis deviation, atrial fibrillation;
biphasic P wave.
P mitrale: P wave duration >120 ms; prominent notched P
P pulmonale: Peaked P waves, amplitude >2.50 m V.
ECHO
Confirms the diagnosis:
Asseses the severity
Shows presence or absence of thrombus/calcification
Shows other associated lesions if any.
Mitral Stenosis 19
Also indicates mitral valve area, mitral valve morphology.
Echocardiographic mitral morphology score is derived from following
features:
1. Leaflet rigidity,
2. Leaflet thickening,
3. Valvular calcification, and
4. Subvalvular disease each graded as 1+ to 4+; score >8 fare badly.
Doppler
Shows (1)pressure gradient across mitral valve and (2) pulmonary artery
pressure.
TEE
Transesophageal echocardiogram: Shows LA thrombus, endocarditis.
Catheterization
1. Shows pressure gradient between LA and LV; measures PA, LA, LV
diastolic pressures Catheterization is indicated when clinical and
echo/Doppler data are discordant.
2. Helps to assess MR severity in those posted for balloon valvotomy
especially when clinical and other data are discordant.
Multislice CT: A new modality to assess mitral valve area.
TREATMENT
Medical:
Treatment of cardiac failure
Treatment of arrhythmia atrial fibrillation
Treatment of pulmonary edema
Prophylaxis/treatment of infective endocarditis
Secondary prophylaxis for rheumatic fever.
Avoid:
Anemia, tachyarrhythmia and vigorous exercise which can precipitate
cardiac failure.
INTERVENTION
1.
2.
3.
4.
Timingmild/moderate symptoms
MVarea <1 cm2/m2
Delay worsens prognosis.
If patient is symptomatic despite medical treatment.
20
Comprehensive Cardiology
Mitral Balloon Valvuloplasty
Indications for:
Significant symptoms class II-IV
Isolated mitral stenosis
No or trivial mitral regurgitation
No calcification or rigidity of the valve-valve must be mobile
Left atrium- free of thrombus
Pulmonary hypertension 50-60 mm of Hg
Valve area of,<1sq cm.
Technique of Balloon Valvuloplasty
Valvotomy is done by inflating a balloon mounted on a cardiac catheter,
Via rt femoral vein balloon mounted catheter is passed trans septally;
Advanced into LA over a curly guide wire, now the distal portion of
balloon is inflated slightly and balloon is advanced up to apex of LV.
Then balloon is gradually withdrawn, until positioned across mitral
valve. At this position the balloon is inflated procedurally, splitting the
commissural adhesions.
Valvuloplasty only requires light sedation, like for cardiac
catheterization.
After 7-10 years of valvuloplasty, valve usually restenoses and mitral
valve replacement is indicated.
Complications of Balloon Valvuloplasty
Mitral regurgitation
Left to Rt shunt
Thromboembolism
Pericardial tamponade
Myocardial infarction.
Surgery for Mitral Stenosis
Mitral Valvotomy
Surgical separation of fused commissures
Adhesions that cause the mitral orifice to be narrowed, are lysed
mechanically (by hand or by dilator). Valvotomy can be closed or open.
Valvotomy is done if facilities or expertise for balloon valvuloplasty is
not available.
Closed Valvotomy
Prerequisite: Flexible, non-calcified valves with no LA thrombus.
Performed through a left thoracotomy without a bypass.
Mitral Stenosis 21
Contraindication are same as for balloon valvuloplasty and additional
contraindications are chest deformity, severe lung disease and elderly
frail patients.
Closed valvotomy is rarely performed now a days in developed countries.
Open Valvotomy
Prerequisite: Flexible, non-calcified valves.
Performed on a cardiopulmonary bypass through a mid sternotomy.
Indications: Failure of balloon valvulopasty/closed commissurotomy.
Associated mild MR, LA thrombus.
After valvuloplasty or valvotomyAntibiotic prophylaxis for endocarditis is a must and yearly follow up
for restenosis is done.
MITRAL VALVE REPLACEMENT
Indications
1. Restenosis
2. Severe advanced MS Valve area < 1sq cm (But patient must have good
LV function).
3. Class II, III, IV symptoms.
4. Severe MS unfit for valvotomy or valvuloplasty: calcified, rigid valve
5. Severe associated MR, thickened fused chordae
6. Pulmonary artery systolic pressure of > 60-80 mm of Hg.
7. Recurrent thrombo embolic manifestations.
Types of Prosthetic Valves (Fig. 2.4)
1. Bioprosthetic valve
2. Mechanical prosthetic valve.
Fig. 2.4: Prosthetic valves
22
Comprehensive Cardiology
Mechanical
Caged Ball valve: e.g. Starr-Edward valve:
AdvantageGood durability
DisadvantageBulky and space occupying.
Complications
Periprosthetic mitral regurgitation
Hemolytic anemia
Jaundice
Thromboembolism
Life long anticoagulation needed
Infective endocarditis
Paravalvular ring abscess.
Tilting disc valve: e.g. St. Jude valve,
Bjrk-Shiley valve (not being used now)
Bioprosthetic valve:
Autograft: from patients pericardium
Advantageanticoagulants not so much necessary: disadvantagenot
durable: just 10 years or less
Porcine tissuethromboembolism less.
Following valve replacement long term anticoagulant therapy is indicated.
Patient with prosthetic valve replacement put on warfarin for rest of
their life.
But xenograft (porcine) or homograft (cadaver) do not require
anticoagulation, except in presence of large LA and AF.
Note: Patients after valvuloplasty/valvotomy require prophylaxis for
inf.endocarditis.
Complications of Valve Replacement
Restenosis
Thromboembolic phenomenon
Hemolytic anemia
Mechanical or material defects of valve itself.
e.g., failure of closure or opening/detachment partial /full.
SUMMARY
i. In most case of MS: Balloon valvotomy is successful.
ii. If valve anatomy is unfavourable for valvotomy: valve replacement
Timing of valve replacement:
a. NYHA functional class 3 or 4.
b. Pulmonary hypertension (pulmonary arterial systolic pressure <50
mm Hg)
Mitral Stenosis 23
Bioprosthetic valve can degenerate within a decade and necessitatereoperation with attendant increased surgical risk.
iii. In young women who wish to bear children:
If in these women balloon valvuloplasty is not feasible, valve
replacement is advised but it is complicated: Mechanical valve
needs anticoagulation; warfarin causes
High incidence of fetal malformation; heparin has been shown
to have
Serious complication.
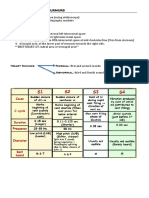
Management of Mitral Stenosis
Procedure
1. Percutaneous balloon mitral
vavotomy
2. Mitral valve repair for MS.
Closed or open mitral
valvotomy
3. Mitral valve replacement
for MS
Indications
Symptomatic NYHA class II, III, IV
Mitral valve area <1 cm2
With no MR, no LA thrombus, no
calcification
NYHA Class III-IV
Mitral valve area <1 cm2
If balloon valvotomy is not available
Valve morphology favourable
for repair with no MR, no calcification, no LA thrombus.
NYHA Class III-IV
Moderate/severe MS with valve area
<1 cm2 who are unfit for valvotomy or
repair
-Those with LA clot or mitral calcification or rigid mitral valvecombined
MS and MR
Mitral valve restenosis.
Note:
In addition to factors mentioned above, various parameters like EF,
LVEDD, PHT, AF, Valve morphology and others have to be considered
in details in deciding about surgery.
Das könnte Ihnen auch gefallen
- Medicine in Brief: Name the Disease in Haiku, Tanka and ArtVon EverandMedicine in Brief: Name the Disease in Haiku, Tanka and ArtBewertung: 5 von 5 Sternen5/5 (1)
- Mitral StenosisDokument12 SeitenMitral StenosisFasihi Junior0% (1)
- Mitral StenosisDokument19 SeitenMitral StenosisAbdur RaqibNoch keine Bewertungen
- Cardiology-1 ValvDokument34 SeitenCardiology-1 ValvMahmoud RamadanNoch keine Bewertungen
- Congenital Heart DiseasesDokument10 SeitenCongenital Heart DiseasesRohit NaiduNoch keine Bewertungen
- DR Abdulkareem Al Othman Valvular HDDokument10 SeitenDR Abdulkareem Al Othman Valvular HDDarawan MirzaNoch keine Bewertungen
- 1 Mitral Stenosis: InstructionDokument8 Seiten1 Mitral Stenosis: Instructionrashid.scribdNoch keine Bewertungen
- Rheumatic Heart Disease2Dokument61 SeitenRheumatic Heart Disease2Puji Yunisyah RahayuNoch keine Bewertungen
- Mitral StenosisDokument2 SeitenMitral StenosisKing Bal94Noch keine Bewertungen
- Differential Diagnosis of Valvular Heart DiseaseDokument10 SeitenDifferential Diagnosis of Valvular Heart DiseaseAbhisek ChatterjeeNoch keine Bewertungen
- Mengapa VSR Lebih Sering Terjadi Pada PerempuanDokument2 SeitenMengapa VSR Lebih Sering Terjadi Pada PerempuanIde Yudis TiyoNoch keine Bewertungen
- Valvular Heart Disease: Dr. Nigussie BerihunDokument43 SeitenValvular Heart Disease: Dr. Nigussie Berihunsisay tigabuNoch keine Bewertungen
- CVS PdaDokument23 SeitenCVS PdaDr.P.NatarajanNoch keine Bewertungen
- Aortic RegurgitationDokument18 SeitenAortic RegurgitationAbdur RaqibNoch keine Bewertungen
- 7th Heart Sounds and MurmursDokument6 Seiten7th Heart Sounds and MurmursbabibubeboNoch keine Bewertungen
- Css JantungDokument12 SeitenCss JantungRegi FauzanNoch keine Bewertungen
- 2 Valvular Heart Disease1Dokument87 Seiten2 Valvular Heart Disease1Danny DesuNoch keine Bewertungen
- Mitral Stenosis: Dr. Mohammed Asrafur Rahman MBBS, Bcs (H), MD Resident (Internal Medicine) (P-A) Chattogram Medical CollegeDokument16 SeitenMitral Stenosis: Dr. Mohammed Asrafur Rahman MBBS, Bcs (H), MD Resident (Internal Medicine) (P-A) Chattogram Medical CollegeAsrafur RahmanNoch keine Bewertungen
- Rheumatic Heart DiseaseDokument30 SeitenRheumatic Heart DiseaseDhiraj PantNoch keine Bewertungen
- CVS VSDDokument31 SeitenCVS VSDDr.P.NatarajanNoch keine Bewertungen
- Ventricular Septal DefectDokument43 SeitenVentricular Septal DefectmalekNoch keine Bewertungen
- Mitral StenosisDokument25 SeitenMitral StenosisPradeepa Hari100% (1)
- Congenital Heart DiseasesDokument27 SeitenCongenital Heart DiseasesShreyas KotadiyaNoch keine Bewertungen
- Heart MurmursDokument13 SeitenHeart MurmursChen BrionesNoch keine Bewertungen
- PericarditisDokument45 SeitenPericarditisBrenda WardshoneNoch keine Bewertungen
- Valvular Heart DiseaseDokument54 SeitenValvular Heart DiseaseRommanah AzmiNoch keine Bewertungen
- Angelina A Joho MSC in Critical Care and TraumaDokument50 SeitenAngelina A Joho MSC in Critical Care and TraumaZabron LuhendeNoch keine Bewertungen
- Congestive Heart FailureDokument4 SeitenCongestive Heart Failureepoi89Noch keine Bewertungen
- Valvular Heart Disease1Dokument80 SeitenValvular Heart Disease1Abnet WondimuNoch keine Bewertungen
- Rheumatic Heart DiseaseDokument39 SeitenRheumatic Heart DiseaseRezwanul Hoque Bulbul100% (1)
- Dr. Mohammad Shaikhani. Sulaimani University, College of Medicine. Sulaimanya-Iraqi KurdistanDokument51 SeitenDr. Mohammad Shaikhani. Sulaimani University, College of Medicine. Sulaimanya-Iraqi KurdistanHNINNoch keine Bewertungen
- CardiomyopathyDokument17 SeitenCardiomyopathyRashed ShatnawiNoch keine Bewertungen
- MRCP Revision NotesDokument41 SeitenMRCP Revision NotesMudassar Waseem100% (1)
- Cardiovascular System: by DR - Nuha Abdel GhaffarDokument41 SeitenCardiovascular System: by DR - Nuha Abdel GhaffarMohammed Alaa EldeanNoch keine Bewertungen
- Valvular Heart Disease 2Dokument46 SeitenValvular Heart Disease 2Topea BogdanNoch keine Bewertungen
- Valvular Heart DiseaseDokument5 SeitenValvular Heart DiseaseElyas MehdarNoch keine Bewertungen
- Mitral RegurgitationDokument9 SeitenMitral RegurgitationNefvi Desqi AndrianiNoch keine Bewertungen
- Cor Pulmonale IkaDokument19 SeitenCor Pulmonale IkaIka Lukita SariNoch keine Bewertungen
- Heart Sounds: They Are The Sounds Produced by The Mechanical Activities of The Heart During Each Cadiac CycleDokument19 SeitenHeart Sounds: They Are The Sounds Produced by The Mechanical Activities of The Heart During Each Cadiac Cyclevishnudurga100% (1)
- 2 5404863613531850140 PDFDokument51 Seiten2 5404863613531850140 PDFzaid auglaNoch keine Bewertungen
- Kuliah MITRAL STENOSISDokument19 SeitenKuliah MITRAL STENOSISAdi TrisnoNoch keine Bewertungen
- Cha Pte R 1 1 Con Ge Nit Al Heart DiseasesDokument70 SeitenCha Pte R 1 1 Con Ge Nit Al Heart DiseasessanjivdasNoch keine Bewertungen
- Cardio-Respiratory Conditions: by DR Priscus MushiDokument73 SeitenCardio-Respiratory Conditions: by DR Priscus MushiMusaNoch keine Bewertungen
- Guidelines For Examination of Cardiovascular System: Bendehiba Latroche, MD, DIS, DIUDokument22 SeitenGuidelines For Examination of Cardiovascular System: Bendehiba Latroche, MD, DIS, DIUkskamkalpanaNoch keine Bewertungen
- Jansenkoh MRCP PacesDokument209 SeitenJansenkoh MRCP PacesBob Yong83% (6)
- 6. Митральные пороки. Клиника, диагностика, лечениеDokument42 Seiten6. Митральные пороки. Клиника, диагностика, лечениеabarna abiNoch keine Bewertungen
- PE and Blunt Thoracic TraumaDokument3 SeitenPE and Blunt Thoracic TraumaRachana GudipudiNoch keine Bewertungen
- PericarditisDokument45 SeitenPericarditisJorge Luis Ibarra NaranjoNoch keine Bewertungen
- CardiovascularDokument51 SeitenCardiovascularhanthuanNoch keine Bewertungen
- Cardiac Tamponade and ManagementDokument42 SeitenCardiac Tamponade and Managementأم حمدNoch keine Bewertungen
- Valvular Heart Disease IM 8-12 NewDokument80 SeitenValvular Heart Disease IM 8-12 NewRachilla Arandita SaraswatiNoch keine Bewertungen
- Cardiac II Study GuideDokument6 SeitenCardiac II Study GuiderunnermnNoch keine Bewertungen
- X-Ray CVSDokument67 SeitenX-Ray CVSmdjohariNoch keine Bewertungen
- Kuliah MITRAL STENOSISDokument19 SeitenKuliah MITRAL STENOSISekaseptiani312Noch keine Bewertungen
- Valvular Heart DiseaseDokument105 SeitenValvular Heart DiseasesenthilmnurseNoch keine Bewertungen
- Principles Auscultatory Areas: ND NDDokument5 SeitenPrinciples Auscultatory Areas: ND NDPinay YaunNoch keine Bewertungen
- Myocardial InfarctionDokument15 SeitenMyocardial InfarctionameerNoch keine Bewertungen
- Teori & Model Keperawatan Dan Penerapan Dalam Asuhan KeperawatanDokument81 SeitenTeori & Model Keperawatan Dan Penerapan Dalam Asuhan Keperawatanannis fathiaNoch keine Bewertungen
- Gibs Cycle and Jhon CycleDokument3 SeitenGibs Cycle and Jhon Cycleannis fathiaNoch keine Bewertungen
- FamilyDokument17 SeitenFamilyannis fathiaNoch keine Bewertungen
- Berpikir ReflektifDokument10 SeitenBerpikir Reflektifannis fathiaNoch keine Bewertungen
- Fisiopatologia Del Shock Cardiogenico Por Iam PDFDokument12 SeitenFisiopatologia Del Shock Cardiogenico Por Iam PDFYESSICA CARENALGANoch keine Bewertungen
- Concept Map 1Dokument3 SeitenConcept Map 1Rubie Ann TillorNoch keine Bewertungen
- Heart and PericardiumDokument26 SeitenHeart and PericardiumpalNoch keine Bewertungen
- MU-MCQs - Internal-MedicineDokument481 SeitenMU-MCQs - Internal-MedicineAbdullah AlAkhrasNoch keine Bewertungen
- Adult Congenital Heart Disease Board ReviewDokument76 SeitenAdult Congenital Heart Disease Board ReviewOQAB13Noch keine Bewertungen
- Se Non-IschaemicDokument40 SeitenSe Non-IschaemicRui FonteNoch keine Bewertungen
- Talley Sum UpDokument51 SeitenTalley Sum UpRozana Bawareth100% (1)
- Aortic StenosisDokument37 SeitenAortic Stenosissarguss14Noch keine Bewertungen
- Nur2731 3rd Semester Final ReviewDokument196 SeitenNur2731 3rd Semester Final Reviewjanet rooseveltNoch keine Bewertungen
- Definition, Classification, Etiology, and Pathophysiology of Shock in Adults - UpToDateDokument16 SeitenDefinition, Classification, Etiology, and Pathophysiology of Shock in Adults - UpToDatevara prasadNoch keine Bewertungen
- Acquired Heart DiseasesDokument41 SeitenAcquired Heart DiseasesSaman SarKoNoch keine Bewertungen
- Fishbein 2019Dokument8 SeitenFishbein 2019hawk.man8Noch keine Bewertungen
- Valvular Heart DiseaseDokument27 SeitenValvular Heart DiseaseOwen J. WieseNoch keine Bewertungen
- Eacvi Recommendations Valvular Regurgitation Summary PDFDokument34 SeitenEacvi Recommendations Valvular Regurgitation Summary PDFstoicea_katalinNoch keine Bewertungen
- Common MurmurDokument2 SeitenCommon MurmurKyWoNoch keine Bewertungen
- Rheumatic Fever and Rheumatic Heart DiseaseDokument54 SeitenRheumatic Fever and Rheumatic Heart DiseaseFian AldyNoch keine Bewertungen
- Valvular Aortic Stenosis: Acute Myocardial InfarctionDokument3 SeitenValvular Aortic Stenosis: Acute Myocardial InfarctionCM NajitoNoch keine Bewertungen
- Example 001Dokument13 SeitenExample 001Priya SelvarajNoch keine Bewertungen
- Medical Surgical QandADokument63 SeitenMedical Surgical QandAAlona Lumidao100% (8)
- HEART MURMURS by NISHDokument41 SeitenHEART MURMURS by NISHurtikikeNoch keine Bewertungen
- Mitral Valve ProlapseDokument4 SeitenMitral Valve Prolapseapi-306423962Noch keine Bewertungen
- Prosth ValvesDokument74 SeitenProsth ValvesRavi ZoreNoch keine Bewertungen
- Valvular Heart Disease: Etiology PathophysiologyDokument34 SeitenValvular Heart Disease: Etiology PathophysiologyensiNoch keine Bewertungen
- Anaesthesia in Dogs and Cats With Cardiac DiseaseDokument19 SeitenAnaesthesia in Dogs and Cats With Cardiac DiseaseALEJANDRA MADRIGALNoch keine Bewertungen
- Free Nclex QuestionsDokument161 SeitenFree Nclex QuestionspadmaNoch keine Bewertungen
- Logiq P5 DatasheetDokument14 SeitenLogiq P5 DatasheetRUCEG1971Noch keine Bewertungen
- Quantification of Severity of Mitral Regurgitation With The New ASE GuidelinesDokument20 SeitenQuantification of Severity of Mitral Regurgitation With The New ASE GuidelinesPanfilAlinaNoch keine Bewertungen
- 3 ValvulopatiasDokument31 Seiten3 ValvulopatiasLeonardoLapasNoch keine Bewertungen
- Step 2 CK NotesDokument95 SeitenStep 2 CK NotesKevin Yang100% (3)
- 3Dokument265 Seiten3Carlos HernándezNoch keine Bewertungen