Beruflich Dokumente
Kultur Dokumente
Exposure To Rabies
Hochgeladen von
DannyOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Exposure To Rabies
Hochgeladen von
DannyCopyright:
Verfügbare Formate
Exposure to Rabies in Small Indian Mongooses (Herpestes
auropunctatus) from Two Regions in Puerto Rico
Author(s): Are R. Berentsen, Shylo R. Johnson, Amy T. Gilbert, and Kurt C.
VerCauteren
Source: Journal of Wildlife Diseases, 51(4):896-900.
Published By: Wildlife Disease Association
DOI: http://dx.doi.org/10.7589/2015-01-016
URL: http://www.bioone.org/doi/full/10.7589/2015-01-016
BioOne (www.bioone.org) is a nonprofit, online aggregation of core research in the
biological, ecological, and environmental sciences. BioOne provides a sustainable online
platform for over 170 journals and books published by nonprofit societies, associations,
museums, institutions, and presses.
Your use of this PDF, the BioOne Web site, and all posted and associated content
indicates your acceptance of BioOnes Terms of Use, available at www.bioone.org/page/
terms_of_use.
Usage of BioOne content is strictly limited to personal, educational, and non-commercial
use. Commercial inquiries or rights and permissions requests should be directed to the
individual publisher as copyright holder.
BioOne sees sustainable scholarly publishing as an inherently collaborative enterprise connecting authors, nonprofit
publishers, academic institutions, research libraries, and research funders in the common goal of maximizing access to
critical research.
DOI: 10.7589/2015-01-016
Journal of Wildlife Diseases, 51(4), 2015, pp. 896900
# Wildlife Disease Association 2015
Exposure to Rabies in Small Indian Mongooses (Herpestes
auropunctatus) from Two Regions in Puerto Rico
Are R. Berentsen,1,2 Shylo R. Johnson,1 Amy T. Gilbert,1 and Kurt C. VerCauteren1 1US Department of
Agriculture, Animal and Plant Health Inspection Service, Wildlife Services, National Wildlife Research Center,
4101 LaPorte Ave., Fort Collins, Colorado 80521, USA; 2Corresponding author (email: Are.R.Berentsen@
aphis.usda.gov)
in 1950, although references to rabies
date back prior to mongoose introduction
(Tierkel et al. 1952). Between 1986 and
1990, 71.5% (236/330) of suspect mongooses tested in Puerto Rico were positive
for rabies virus, as were 2.6% (4/152) of
randomly trapped mongooses (Everard
and Everard 1992). In comparison, Everard et al. (1981) reported rabies infection
in 1.3% of .11,000 mongooses in Grenada between 1968 and 1977. Velez
(1998) found 19.3% of mongooses sampled in portions of El Yunque National
Forest (YNF), Puerto Rico, positive for
rabies virusneutralizing antibodies
(RVNA) when tested by enzyme-linked
immunosorbent assay (ELISA), although
none were rabies virus positive. Few data
are available on rabies exposure in
mongooses on Puerto Rico, as most
studies have occurred on other Caribbean
islands, primarily Grenada (Everard et al.
1981; Zieger et al. 2014). We evaluate
sera for RVNA and saliva samples for
rabies virus RNA to investigate mongoose
exposure to rabies in two ecologically
different environments on Puerto Rico.
We conducted our study at YNF and
Cabo Rojo (CR) National Wildlife Refuge
(Fig. 1). The YNF is a subtropical rainforest approximately 40 km southeast of
San Juan. In YNF, samples were collected
from a 1.0-km2 region of Palo Colorado
and Sierra Palma forest types in October
2011 and March 2012. The CR is .7 km2
of subtropical dry forest in southwestern
Puerto Rico. We collected samples from
CR in two ,1-km2 regions, one each on
the eastern and western sides of the
ABSTRACT:
The small Indian mongoose (Herpestes auropunctatus) was introduced to several
Caribbean Islands to control rat (Rattus spp.)
damage to sugarcane plantations. Mongooses
failed at suppressing rat populations and are
now considered pests throughout most of their
introduced range. Importantly, mongooses are
rabies reservoirs on several Caribbean Islands.
In Puerto Rico, mongooses have been implicated in up to 70% of reported animal rabies cases.
There is no rabies vaccination program for
wildlife in Puerto Rico, and data on rabies in
mongooses are limited. We conducted a serosurvey of mongooses in two different ecologic
environments in Puerto Rico: El Yunque
National Forest and Cabo Rojo National Wildlife Refuge. We collected 119 serum samples
from 112 mongooses, 44 (39.3%) of which
were positive for rabies virusneutralizing
antibodies. We also collected oral swabs from
147 mongooses, including 88 from which we
also collected serum. No oral swabs were
positive for rabies virus RNA. Our data
support previous research suggesting rabies
virus is circulating within the mongoose
population on Puerto Rico.
Key words: Caribbean, Herpestes auropunctatus, mongoose, Puerto Rico, rabies,
wildlife disease.
The small Indian mongoose (Herpestes
auropunctatus) was introduced to the
Caribbean Islands in the 1870s, primarily
to control rat (Rattus spp.) damage to
sugarcane (Hoagland et al. 1989). Mongooses are now considered pests throughout most of their introduced range and are
the primary rabies reservoir on several
Caribbean Islands (Everard and Everard
1992). In Puerto Rico, mongooses account
for up to 75% of reported rabies cases
(Krebs et al. 1998; Dyer et al. 2014). In
Puerto Rico, the first laboratory-confirmed
rabies-infected mongooses were reported
896
SHORT COMMUNICATIONS
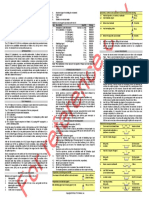
FIGURE 1.
897
El Yunque National Forest and Cabo Rojo National Wildlife Refuge, Puerto Rico.
refuge, during September 2011, April
May 2012, and August 2014. Both sample
sites are dominated by scrub-class vegetation (Weaver and Schwagerl 2008).
We used cage traps (Tomahawk Trap
Company, Hazelhurst, Wisconsin, USA)
baited with canned tuna to live capture
mongooses (Quinn and Whisson 2005).
Mongooses were hazed out of the trap
into a cone-shaped canvas bag, physically
restrained, and immobilized with an intramuscular injection of TelazolH (tiletaminezolazepam, Fort Dodge Laboratories, Fort
Dodge, Iowa, USA) at a dose rate of 5 mg/kg
(Kreeger and Arnemo 2007). We collected
0.51.0 cc of whole blood by venipuncture
of the cranial vena cava, as described for
ferrets (Briscoe and Syring 2004), and
injected a passive integrated transponder
tag (Avid Identification Systems, Inc.,
Norco, California, USA) subcutaneously
between the shoulder blades of each
captured mongoose. We used a sterile
cotton swab to collect saliva samples and
stored swabs in a bovine albumin 1 viral
transport medium to reduce potential
bacterial or fungal contamination (Shriner
et al. 2012). Blood samples were centrifuged, and sera were transferred by
pipette into cryovials. Serum samples and
oral swabs were frozen at 210 C for up to
14 d and transferred to 280 C until
analysis.
Sera were analyzed for RVNA end-point
titers by using the rapid fluorescent focus
inhibition test (Smith et al. 1996) by the
rabies laboratory at Kansas State University (Manhattan, Kansas, USA). Mongooses with sera .0.1 IU/mL were considered
positive for RVNA. We compared prevalences by using the Logistic procedure in
SAS (SAS Institute Inc., Cary, North
898
JOURNAL OF WILDLIFE DISEASES, VOL. 51, NO. 4, OCTOBER 2015
Carolina, USA). We accepted statistical
significance at a50.05.
Oral swabs were processed by Atlanta
Health Associates (Cumming, Georgia,
USA). Total RNA was extracted by using
TRIZol reagent (InvitrogenTM, AmbionH,
Carlsbad, California, USA). Heminested
reverse-transcription PCR was performed
for amplification of a partial sequence of
the rabies virus nucleoprotein gene by
using primers 1066:304 for the primary
and 1087:304 for the heminested reactions. Positive (RNA from mouse brain
infected with the mongoose-variant rabies
virus) and negative (water) control samples were used with each PCR run.
Reaction products were visualized by gel
electrophoresis (Freuling et al. 2015).
We collected 41 sera from 39 mongooses at YNF. Fourteen sera were RVNA
positive from 13 mongooses (nine males
and four females), including one recaptured female whose titer decreased from
2.8 to 1.2 IU/mL between sampling
periods (138 d). The geometric mean titer
of positive mongooses at YNF was 0.52
IU/mL (range: 0.12.8 IU/mL), and antibody prevalence was 33% (13 unique
positives and 39 unique captures; 95%
confidence interval [CI]: 1948%). At CR,
78 sera were collected from 73 mongooses. Thirty-two sera were RVNA positive
from 31 individuals (20 males and 11
females). Five animals were recaptured
during subsequent seasons: two females
and one male, initially captured in 2011,
were recaptured in 2012. Among recaptures, one male and one female seroconverted between captures (from ,0.1 IU/mL
to 0.4 and 1.4 IU/mL for the male and
female, respectively), while the second
female remained antibody negative. One
male captured in 2012 (recaptured in 2014)
seroconverted between captures (,0.1 IU/
mL in 2012 and 10.7 IU/mL in 2014). A
positive female captured in 2011 was
recaptured in 2014, and the RVNA titer
had decreased from 0.6 IU/mL to 0.5 IU/
mL (1,073 d). Geometric mean titer of
antibody-positive mongooses at CR was
1.62 IU/mL (range: 0.150.0 IU/mL), and
antibody-prevalence was 42% (31 positive
and 73 unique captures; 95% CI: 3154%).
Antibody prevalence (including recaptured
animals) did not differ between sites
(x250.53; P50.46) or seasons (wet vs. dry;
x250.02; P50.88), or among years (x25
1.28; P50.53).
Oral swabs from 146 unique mongooses
(72 from CR and 74 from YNF) were
tested for rabies virus RNA. This included
swabs from 88 individual mongooses
whose sera were screened, and 33 of
which were RVNA positive. All swabs
were negative for viral RNA.
The RVNA detected in mongoose sera
suggests prior peripheral virus exposure
and adaptive immune response induction
rather than an active nervous system
infection at the time of sampling. A
peripheral neutralizing antibody response
may not be routinely induced or if it is
induced, tends to be observed during late
stages of clinical infection (Lafon 2013),
which were not observed among mongooses in this study. Furthermore, viral
shedding in saliva by infected rabid
animals is intermittent and, though possible to detect several days in advance of
clinical signs, is typically detected during
clinical infection (Hanlon et al. 2007).
Zieger et al. (2014) found that of 171
mongooses sampled on Grenada, only two
(1.7%) were positive for rabies virus,
whereas 33 (19.3%) had RVNA titers at
the 0.1 IU/mL threshold. Rabies virus
RNA was not found in saliva from either
infected mongoose in the Zieger et al.
(2014) study, and neither mongoose
showed clinical signs of infection.
Overall, 39% of mongooses sampled in
this study were RVNA positive. This is
slightly higher than previous estimates
from Puerto Rico (19.3%; Velez 1998)
and Grenada (30.0%, Everard et al. 1981;
19.3%, Zieger et al. 2014), although
caution must be exercised during comparison as Velez (1998) used an ELISA assay
for antibody detection and Everard et al.
(1981) used a lower cutoff than our study
SHORT COMMUNICATIONS
to report positive RVNA results. The
number of rabies-positive mongooses in
our study is unknown because mongooses
were not lethally sampled, but prevalence
estimates from similar environments of
Grenada are 1.7% (Zieger et al. 2014) and
1.3% (Everard et al. 1981). Rabies transmission routes among mongooses are
poorly understood, but bite contacts
during intraspecific aggression are likely
the primary route.
Phylogenetic studies suggest the rabies
virus circulating in mongooses of Puerto
Rico is related to the North Central skunk
variant and cosmopolitan dog lineages of
rabies virus (Nadin-Davis et al. 2008).
Virus strains from Puerto Rico (NadinDavis et al. 2008), Grenada (Zieger et al.
2014), and Cuba (Nadin-Davis et al. 2006)
do not cluster in a monophyletic group,
suggesting independent introductions to
different Caribbean islands.
Rabies is maintained by mongooses as
a reservoir species rather than a spillover
host. Although domestic dogs (Canis
familiaris) can account for up to 26% of
rabies cases in Puerto Rico, infection is
typically attributed to the mongoose variant (Dyer et al. 2014). It is not possible to
distinguish whether multiple exposures
occurred among recaptured animals in
this study, but our findings support
reports by Everard et al (1981), indicating
potential for long-term maintenance of
RVNA in mongoose. The seroconversion
events detected among recaptured animals provides strong evidence of active
rabies virus circulation among mongooses
in Puerto Rico. Future research should
include virus isolation from saliva of
actively infected mongooses. With no
wildlife vaccination program in place,
mongoose rabies in Puerto Rico continues
to pose a threat to domestic animal and
human health.
We thank P. Quinones, N. Mooers, C.
Ellis, E. Blizzard, and S. Eaton for field
assistance. We also thank F. Cano, O.
Diaz, and R. Lopez-Ortiz for logistic
assistance. Capture and handling of mon-
899
gooses was approved by the US Department of Agriculture National Wildlife
Research Centers animal care and use
committee under protocol QA1856.
LITERATURE CITED
Briscoe JA, Syring R. 2004. Techniques for emergency airway and vascular access in special
species. Semin Avian Exot Pet Med 13:118131.
Dyer JL, Yager P, Orciari L, Greenberg L, Wallace
R, Hanlon CA, Blanton JD. 2014. Rabies
surveillance in the United States during 2013.
J Am Vet Med Assoc 245:11111123.
Everard COR, Baer GM, Alls ME, Moore SA. 1981.
Rabies serum neutralizing antibody in mongooses from Grenada. Trans R Soc Trop Med Hyg
5:654666.
Everard COR, Everard JD. 1992. Mongoose rabies in
the Caribbean. Ann N Y Acad Sci 653:356366.
Freuling CM, McElhinney LM, Fooks AR, Muller
TF. 2015. Gel-based reverse transcription-polymerase chain reaction. In: Current laboratory
techniques in rabies diagnosis, research and prevention, Vol. 2, Rupprecht CE, Nagarajan T,
editors. Elsevier, San Diego, California,
pp. 119128.
Hanlon CA, Niezgoda M, Rupprecht CE. 2007.
Rabies in terrestrial animals. In: Rabies, 2nd
Ed., Jackson AC, Wunner WH, editors. Academic Press, London, UK, pp. 201258.
Hoagland DB, Horst GR, Kilpatrick CW. 1989.
Biogeography and population biology of the
mongoose in the West Indies. In: Biogeography
of the West Indies, past, present and future,
Woods CA, editor. Sandhill Crane Press, Gainesville, Florida, pp. 611634.
Krebs JW, Smith JS, Rupprecht CE, Childs JE. 1998.
Rabies surveillance in the United States during
1997. J Am Vet Med Assoc 213:17131728.
Kreeger TJ, Arnemo JM. 2007. Handbook of wildlife
chemical immobilization, 3rd Ed. Sunquest
Printing, Vancouver, British Columbia, Canada,
432 pp.
Lafon M. 2013. Immunology. In: Rabies, 3rd Ed.,
Jackson A, editor. Academic Press, San Diego,
California, pp. 387408.
Nadin-Davis SA, Torres G, de Los Angeles Ribas M,
Guzman M, Cruz de La Paz R, Morales M,
Wandeler AI. 2006. A molecular epidemiological
study of rabies in Cuba. Epidemiol Infect
134:13131324.
Nadin-Davis SA, Velez J, Malaga C, Wandeler AI.
2008. A molecular epidemiological study of
rabies in Puerto Rico. Virus Res 131:815.
Quinn JH, Whisson DA. 2005. The effects of
anthropogenic food on the spatial behavior of
small Indian mongooses (Herpestes javanicus) in
a subtropical rainforest. J Zool 267:339350.
900
JOURNAL OF WILDLIFE DISEASES, VOL. 51, NO. 4, OCTOBER 2015
Shriner SA, VanDalen KC, Mooers N, Ellis JW,
Sullivan HJ, Root JJ, Pelzel AM, Franklin AB.
2012. Low-pathogenic avian influenza virus in
wild house mice. PLoS One 7:e39206.
Smith JS, Yager PA, Baer GM. 1996. A rapid
fluorescent focus inhibition test (RFFIT) for
determining rabies virus-neutralizing antibody.
In: Laboratory techniques in rabies, 4th Ed.,
Meslin FX, Kaplan MM, Koprowski H, editors.
World Health Organization, Geneva, Switzerland,
pp. 181190.
Tierkel ES, Arbona G, Rivera A, De Juan A. 1952.
Mongoose rabies in Puerto Rico. Public Health
Rep 67:274.
Velez JV. 1998. Presencia de anticuerpos
antirabicos y diagnostico de la rabia en mangostas
(Herpestes auropunctatus) capturadas en El
Bosque Nacional del Caribe (El Yunque). MS
Thesis, University of Puerto Rico, San Juan,
Puerto Rico, 125 pp.
Weaver PL, Schwagerl JJ. 2008. Secondary forest
succession and tree planting at the Laguna
Cartagena and Cabo Rojo wildlife refuges in
southwestern Puerto Rico. Ambio 37:598603.
Zieger U, Marston DA, Sharma R, Chikweto A,
Tiwari K, Sayyid M, Louison B, Goharriz H,
Voller K, Breed AC, et al. 2014. The phylogeography of rabies in Grenada, West Indies, and
implications for control. PLoS Negl Trop Dis
8:e3251.
Submitted for publication 22 January 2015.
Accepted 25 March 2015.
Das könnte Ihnen auch gefallen
- Dsur I Chapter 19 Multilevel Linear ModelsDokument50 SeitenDsur I Chapter 19 Multilevel Linear ModelsDannyNoch keine Bewertungen
- Dsur I Chapter 18 Categorical DataDokument47 SeitenDsur I Chapter 18 Categorical DataDannyNoch keine Bewertungen
- Dsur I Chapter 14 Mixed Designs GLM 5Dokument26 SeitenDsur I Chapter 14 Mixed Designs GLM 5DannyNoch keine Bewertungen
- Dsur I Chapter 12 Two Way Independent Anova GLM 3Dokument26 SeitenDsur I Chapter 12 Two Way Independent Anova GLM 3DannyNoch keine Bewertungen
- MANOVA Analysis of Psychotherapy Treatment GroupsDokument39 SeitenMANOVA Analysis of Psychotherapy Treatment GroupsDannyNoch keine Bewertungen
- Dsur I Chapter 11 Analysis of Covariance Ancova Glm2Dokument29 SeitenDsur I Chapter 11 Analysis of Covariance Ancova Glm2DannyNoch keine Bewertungen
- Dsur I Chapter 15 Nonparametric StatsDokument44 SeitenDsur I Chapter 15 Nonparametric StatsDannyNoch keine Bewertungen
- PCA Factor Analysis Reliability Cronbachs AlphaDokument47 SeitenPCA Factor Analysis Reliability Cronbachs AlphaDannyNoch keine Bewertungen
- Dsur I Chapter 15 Nonparametric StatsDokument44 SeitenDsur I Chapter 15 Nonparametric StatsDannyNoch keine Bewertungen
- Dsur I Chapter 14 Mixed Designs GLM 5Dokument26 SeitenDsur I Chapter 14 Mixed Designs GLM 5DannyNoch keine Bewertungen
- Dsur I Chapter 12 Two Way Independent Anova GLM 3Dokument26 SeitenDsur I Chapter 12 Two Way Independent Anova GLM 3DannyNoch keine Bewertungen
- Repeated measures designs (GLM 4Dokument44 SeitenRepeated measures designs (GLM 4DannyNoch keine Bewertungen
- Dsur I Chapter 09 Comparing Two MeansDokument32 SeitenDsur I Chapter 09 Comparing Two MeansDannyNoch keine Bewertungen
- Dsur I Chapter 10 GLM 1Dokument71 SeitenDsur I Chapter 10 GLM 1DannyNoch keine Bewertungen
- Dsur I Chapter 07 Linear RegressionDokument18 SeitenDsur I Chapter 07 Linear RegressionDannyNoch keine Bewertungen
- Dsur I Chapter 08 Logistic RegressionDokument41 SeitenDsur I Chapter 08 Logistic RegressionDannyNoch keine Bewertungen
- Dsur I Chapter 06 CorrelationDokument42 SeitenDsur I Chapter 06 CorrelationDannyNoch keine Bewertungen
- Dsur I Chapter 09 Comparing Two MeansDokument32 SeitenDsur I Chapter 09 Comparing Two MeansDannyNoch keine Bewertungen
- Exploring Statistical AssumptionsDokument26 SeitenExploring Statistical AssumptionsDannyNoch keine Bewertungen
- Dsur I Chapter 04 Exploring Data With Graphs 2Dokument52 SeitenDsur I Chapter 04 Exploring Data With Graphs 2DannyNoch keine Bewertungen
- Chapter 2: The Chemical Context of LifeDokument40 SeitenChapter 2: The Chemical Context of LifeDannyNoch keine Bewertungen
- Dsur I Chapter 03 The R Environment 3Dokument17 SeitenDsur I Chapter 03 The R Environment 3DannyNoch keine Bewertungen
- Mongoose Population in LuquilloDokument7 SeitenMongoose Population in LuquilloDannyNoch keine Bewertungen
- Dsur I Chapter 02 Everything You Ever Wanted To Know About StatisticsDokument36 SeitenDsur I Chapter 02 Everything You Ever Wanted To Know About StatisticsDannyNoch keine Bewertungen
- Mongoose BiologyDokument8 SeitenMongoose BiologyDannyNoch keine Bewertungen
- History of ConnecticutDokument10 SeitenHistory of ConnecticutDannyNoch keine Bewertungen
- Dsur I Chapter 01 Why Do We Need StatisticsDokument32 SeitenDsur I Chapter 01 Why Do We Need StatisticsDannyNoch keine Bewertungen
- Rabies in MongooseDokument6 SeitenRabies in MongooseDannyNoch keine Bewertungen
- Mongoose RabiesDokument6 SeitenMongoose RabiesDannyNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Lecture 13 Tumor ImmunologyDokument99 SeitenLecture 13 Tumor Immunologyمحمود محمد100% (1)
- Anti-HCV Reagent Kit: B8P060 G71272R05Dokument8 SeitenAnti-HCV Reagent Kit: B8P060 G71272R05LoloNoch keine Bewertungen
- Presentation 4Dokument21 SeitenPresentation 4URS AasuNoch keine Bewertungen
- Zika Virus and Its CharacteristicsDokument4 SeitenZika Virus and Its CharacteristicsTitus LeeNoch keine Bewertungen
- Conversion MG - DL To Mmol - LDokument6 SeitenConversion MG - DL To Mmol - LshrinivastNoch keine Bewertungen
- #3 Pancreatic Hormones & Antidiabetic Drugs 14 PDFDokument14 Seiten#3 Pancreatic Hormones & Antidiabetic Drugs 14 PDFOmar BasimNoch keine Bewertungen
- Anatomy Final Exam Notes PDFDokument45 SeitenAnatomy Final Exam Notes PDFLydia LalalandNoch keine Bewertungen
- BrucellosisDokument10 SeitenBrucellosisMARK ARQUE LACANARIANoch keine Bewertungen
- Literature Review of Cervix CancerDokument6 SeitenLiterature Review of Cervix Cancerzyfepyfej0p2100% (1)
- 2020 3RD Quarter Science 10Dokument5 Seiten2020 3RD Quarter Science 10Marvin ObraNoch keine Bewertungen
- Urosepsis: Dr. Tameem Mohammed Department of Anesthesia and Intensive Care San Fernando General HospitalDokument22 SeitenUrosepsis: Dr. Tameem Mohammed Department of Anesthesia and Intensive Care San Fernando General HospitalRicky AliNoch keine Bewertungen
- Inserto Vitamina B12 CTKDokument2 SeitenInserto Vitamina B12 CTKLilian Carolina Loreto MachadoNoch keine Bewertungen
- Diversity of MICROBIAL WORLDDokument47 SeitenDiversity of MICROBIAL WORLDAdya Arradikha100% (1)
- HAY! Isn’t That A ProtistDokument2 SeitenHAY! Isn’t That A ProtistJohnkevin NocheNoch keine Bewertungen
- Chapter 1: An Overview of Clinical LaboratoryDokument13 SeitenChapter 1: An Overview of Clinical LaboratoryAshley Tañamor100% (2)
- July 6 Core Concepts in GeneticsDokument14 SeitenJuly 6 Core Concepts in Geneticsiam_maria1997Noch keine Bewertungen
- Differential GENE EXPRESSIONDokument20 SeitenDifferential GENE EXPRESSIONUsama ElahiNoch keine Bewertungen
- Gabatilla Genbio q3m1-18Dokument23 SeitenGabatilla Genbio q3m1-18GABATILLA JAN RYLNoch keine Bewertungen
- Molecular MarkersDokument42 SeitenMolecular Markerssaroj Burlakoti100% (1)
- Implantation and Placental DevelopmentDokument26 SeitenImplantation and Placental DevelopmentMich Therese AbejeroNoch keine Bewertungen
- Prokaryotic Vs Eukaryotic CellsDokument55 SeitenProkaryotic Vs Eukaryotic CellsRufaro SadindiNoch keine Bewertungen
- Erc Cap PDFDokument299 SeitenErc Cap PDFSilvia Ramos YllescasNoch keine Bewertungen
- Reference Ranges: Mksap 17Dokument2 SeitenReference Ranges: Mksap 17deasy noviasariNoch keine Bewertungen
- Different Systems of BodyDokument16 SeitenDifferent Systems of BodygracetingNoch keine Bewertungen
- Bsmmu DDV Curriculum 2012 New EdDokument18 SeitenBsmmu DDV Curriculum 2012 New Edshahed100% (1)
- 7th Science Final Exam Study GuideDokument8 Seiten7th Science Final Exam Study Guideapi-233736029Noch keine Bewertungen
- 32 Oet Reading Summary 2.0-697-717Dokument21 Seiten32 Oet Reading Summary 2.0-697-717Santhus100% (6)
- ANormal Values Saunders 6th, 7th, Uworld 2017 JimirDokument4 SeitenANormal Values Saunders 6th, 7th, Uworld 2017 JimirAce LabosNoch keine Bewertungen
- Disease Detectives Cheat SheetDokument2 SeitenDisease Detectives Cheat SheetBereket LakiNoch keine Bewertungen
- Blood Group SystemsDokument7 SeitenBlood Group SystemshamaadaNoch keine Bewertungen