Beruflich Dokumente
Kultur Dokumente
Antidepresivos Ciclicos
Hochgeladen von
Heriberto JuarezOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Antidepresivos Ciclicos
Hochgeladen von
Heriberto JuarezCopyright:
Verfügbare Formate
S E C T I O N
CENTRAL NERVOUS SYSTEM
27
Tricyclic and Other Cyclic Antidepressants
D. ERIC BRUSH, MD CYNTHIA K. AARON, MD
At a Glance
Primary toxicity related to sodium channel blockade and
subsequent effects on cardiac cell depolarization leads to
ventricular dysrhythmias. Sodium channel blockade, GABAergic
effects, and biogenic amine reuptake effects lead to seizures.
Secondary toxicity from inotropic depression and vascular
dilation leads to profound hypotension.
Hallmark of toxicity seen on electrocardiogram is QRS
prolongation and rightward axis deviation of the terminal
40 msec of the QRS complex.
Those at highest risk for seizures and ventricular dysrhythmias
have a QRS greater than 100 msec or a terminal R wave in aVR
greater than 3 mm.
Sodium bicarbonate is the primary treatment modality for
severe intoxication.
Signs of signicant toxicity mandate continuous monitoring
until symptom free for 24 hours.
Toxicity due to cyclic antidepressant (CA) overdose dates
back to 1959, shortly after the introduction of the antidepressant imipramine.1-3 For several years preceding
1993, antidepressants were deemed responsible for the
majority of deaths due to prescription drug overdose in
the United States.4,5 More recently, the number of deaths
from antidepressants, including cyclic and noncyclic
compounds, has been superseded by analgesic medications, although the number of reported exposures
involving antidepressants has not signicantly decreased.6
Evolving epidemiology of antidepressant mortality may
be due in part to prescribing practices. Preferential
prescription of selective serotonin reuptake inhibitors
(SSRIs) for depression, with their improved safety prole
compared with cyclic antidepressants, may partly explain
this trend. Some data suggest that the death-to-
prescription ratio for CAs exceeds that of other
antidepressant classes.7 Nevertheless, physicians continue
to prescribe CAs for depression as well as for neuropathic pain, migraine, obsessive-compulsive disorder,
enuresis, and a variety of other maladies. The actual
number of prescriptions written for CAs is unknown,
which limits interpretation of poison center data
regarding exposures and deaths. This fact, coupled with
underreporting of exposures and deaths to poison
centers, makes conclusions regarding decreased exposure
versus improved treatment impossible.8 Among the
antidepressant class of medications, CAs still account for
the highest number of deaths. However, according to
data from the Toxic Exposure Surveillance System
(TESS), the number of deaths caused by SSRIs is
gradually approaching that of CAs.6 Although deaths
from CAs have decreased in recent years compared to
the 1980s, the number of deaths has remained fairly
constant over the last decade, with approximately 100
deaths per year reported by the TESS.4-6,9-16 These data
are based on exposures reported to poison centers and
require careful interpretation.
The number of children under 6 years of age exposed
to CAs has remained relatively constant over the last few
years according to TESS data. The majority of these cases
are accidental exposures involving small ingestions or
possibly no ingestion. The 2002 TESS data reports 1573
exposures to CAs in children less than 6 years of age.6
The only deaths occurred from malicious poisonings. A
5-year retrospective study (years 1993 to 1997) of a single
poison centers data regarding ingestions of tricyclic
antidepressants (excluding monocyclic and tetracyclic
drugs) in children less than 6 years of age revealed no
deaths.17 The majority of the children (92%) were
asymptomatic, while the remaining patients exhibited
mild sedation. Ninety percent of patients in this study
ingested less than the age-appropriate dose. Although
this study represents a small sample of patients in a
retrospective poison centerbased review, it identies the
typical features of CA exposure in young children: small
537
538
CENTRAL NERVOUS SYSTEM
dose and low toxicity. Regardless, exposure histories in
young children are difcult to elicit. One or two tablets
may be sufcient to cause life-threatening toxicity in
small children. Therefore, all exposures in this age group
require careful evaluation.
STRUCTURE
Tricyclic antidepressants (TCAs) are a class of drugs that
contain a three-ringed nucleus with various side chains
and atomic substitutions (Fig. 27-1). The term cyclic
antidepressant is more encompassing and includes drugs
with ring structures beyond the three-ringed TCA
nucleus (see Fig. 27-1). These include tetracyclic drugs
such as amoxapine, maprotiline, and mirtazapine and
bicyclics such as mianserin. The TCAs are broadly
classied as secondary or tertiary amines in reference to
the number of methyl groups on the propylamine side
chain of the structure. The tertiary amines are imipramine,
amitriptyline, clomipramine, chloripramine, doxepin,
dothiepin, lofepramine, and trimipramine. The secondary
amines include desipramine, nortriptyline, and protriptyline. In vivo demethylation of the tertiary amines
amitriptyline and imipramine produces the active
secondary amines nortriptyline and desipramine,
respectively. Metabolism via hydroxylation creates
multiple active metabolites (Table 27-1). Intermediate
structures display differing degrees of pharmacodynamic
actions; the extent of cholinergic receptor blockade in
decreasing order of effect is tertiary amine > secondary
amine > demethylated metabolites > hydroxylated
metabolites.18-20
Structural similarities between CAs and phenothiazines
as well as other classes of antipsychotic medications yield
a likely explanation for shared toxicity as well as crossreactivity in immunoassays. Anticholinergic, antihistaminic,
and some cardiovascular effects such as sodium channel
blockade, QTc prolongation, and peripheral blockade
are shared to various extents by medications from these
classes.
R2
J CH3
CH2CHCH2N J
C
O
S
C
N
Amitriptyline
Doxepin
Dothiepin
Nortriptyline
J CH3
CH2CH2CH2N J
H
R3
CH3
CH3
CH3
H
Cyclic antidepressants exert their therapeutic action in
part by producing varying degrees of reuptake inhibition
of norepinephrine, dopamine, and serotonin at nerve
terminals in the central nervous system (CNS). While this
mechanism of action forms the basis of the monoamine
hypothesis of depression, it describes only one of the
many effects CAs exert in vivo. Although the monoamine
hypothesis remains a likely explanation for much of the
therapeutic benet of antidepressants, alterations in
other CNS signaling pathways have recently been discovered and may signicantly contribute to drug efcacy
in depression. The identication of -aminobutyric acid
(GABA) and its putative role in depression has recently
been elucidated through human brain scans and
cerebrospinal fluid analysis as well as in vivo animal and
in vitro models.21 These studies demonstrates that CAs
inhibit the influx of chloride through the GABA chloride
channel.22 The extent to which the GABAergic system
modulates depression is unclear. This drug effect
provides a potential explanation for CA-induced seizures.
Additional pharmacologic activity of CAs includes
blockade of cholinergic, histaminic, and 1-adrenergic
receptors. Chronic antidepressant dosing alters CNS
neurotransmitter receptor expression and sensitivity.
Effects on the neurohormonal system have been
demonstrated in animal models; CAs have been shown to
alter glucocorticoid mRNA receptor expression.23,24 The
signicance of this alteration is unknown.
Differences among CAs regarding their effects on
neurotransmission are detectable at therapeutic dosing.
The nontricyclic antidepressants amoxapine and maprotiline primarily affect norepinephrine while having no
effect on serotonin. Amoxapine and its 7-OH-amoxapine
metabolite block dopamine receptors to degrees comparable to thioridazine and haloperidol, respectively.25
All CAs produce some degree of sodium channel
blockade in the central and peripheral nervous tissue at
R1
R2
Pharmacodynamics
J CH2
CH2CH2CH2N J
R1
PHARMACOLOGY
C
Cl
O
Amoxapine
FIGURE 27-1 Structures of some cyclic antidepressants.
Maprotilene
R1
R2
R1
CH3
CH3
CH3
H
CH2 CO C6 H6
R2
R3
H
CH3
H
H
H
H
H
Cl
H
H
Imipramine
Trimipramine
Clomipramine
Desipramine
Lofepramine
J CH2
CHCH2CH2N J
H
Protriptylene
CHAPTER 27
Tricyclic and Other Cyclic Antidepressants
539
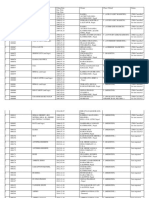
TABLE 27-1 Pharmacokinetic Parameters of Selected Cyclic Antidepressants
DRUG
ELIMINATION
HALF-LIFE (hr)*
THERAPEUTIC LEVEL
(ng/mL)
CYP METABOLISM
Amitriptyline
925
125150
1A2, 2C19, 3A4, 2D6,
Amoxapine
8, (30), (6.5)
160800
2C9
2D6
Clomipramine
21, (36)
Desipramine
Dothiepin
1323
1424 (2346)
50300
50150
Doxepin
Imipramine
824
1834 (1230)
75200
150300
1.52.5 (1230)
43 (6090)
1636
55198
23
2040
50300
50150
50150
30170
Lofepramine
Maprotiline
Nortriptyline
Protriptyline
Trimipramine
Mirtazapine
1A2, 2C19, 3A4, 2D6
2D6
2D6
1A2, 2C19, 3A4, 2D6
2D6
2D6
2D6
2D6
2D6, 1A2, 3A4
PRINCIPAL ACTIVE
METABOLITES
Nortriptyline
10-OH amitryptyline
10-OH nortryptiline
8-OH amoxapine
7-OH amoxapine
Desmethylclomipramine
2-OH despramine
Desmethyldothiepin
Dothiepin-S-oxide
Desmethyldoxepin
Desipramine
2-OH imipramine
2-OH desipramine
Desipramine
Desmethylmaprotiline
10-OH nortriptylline
Desmethyltrimipramine
Dimethylmirtazapine
CYP, cytochrome P-450.
*
Numbers in parentheses represent the half-life of the metabolites.
Data are based on small numbers of usual concentrations and may not reflect optimal dosing. Therapeutic concentrations are not well established.
Metabolic pathways are not fully established for all drugs.
therapeutic dosing. This membrane stabilizing or
quinidine-like effect leads to ventricular dysrhythmias
in the setting of overdose. The efcacy of CAs for the
treatment of neuropathic pain may stem from this effect.
Pharmacokinetics
Cyclic antidepressants share similar pharmacokinetic
parameters. Following oral administration, drug absorption proceeds rapidly,26 with the exception of the
sustained-release (SR) formulation of clomipramine
(Anafranil Retard), which has a delayed time to maximum
concentration (Tmax) of 9 hours versus 4.8 hours with
the immediate-release (IR) formulation.27 Currently,
clomipramine SR is available only in the United
Kingdom. Peak serum concentrations of other CAs are
generally achieved within 2 to 6 hours.26 All drugs in this
class are highly lipophilic with a large apparent volume
of distribution and rapid tissue redistribution.26 Typically,
CAs exhibit a volume of distribution between 10 and
20 L/kg. Tissue concentrations often exceed serum
concentrations by 10- to 100-fold. The fraction of drug in
the serum is highly protein bound.26 Since CAs are weak
bases, they are bound to 1-acid glycoprotein in the
intravascular compartment. The fraction of free drug
in the serum can be altered with changes in serum pH.
Lowering pH creates a higher unbound fraction.
Implications of acidbase status for overdose management are discussed in later sections.
Elimination is almost entirely hepatic, with little
unchanged drug excreted in the urine. CAs do not
undergo biliary excretion in any appreciable amount.28
Biotransformation of CAs occurs via the hepatic microoxygenase P-450 enzyme system, and rst pass metabolism
signicantly reduces their oral bioavailability.29-31 Many
CAs form active metabolites following demethylation or
hydroxylation (see Table 27-1). Active metabolites may
accumulate after a period of 12 to 24 hours and could
result in signicant toxicity in therapeutic dosing.32,33
The most common hepatic enzyme isoforms involved in
the biotransformation of CAs are CYP2D6 and
CYP2C19.34 Hydroxylation occurs via CYP2D6, whereas
the 2C19 isoform is associated with N-demethylation.26
CAs inhibit CYP2D6 and CYP2C19 activity.35 Genetic
polymorphisms in certain cytochrome P-450 (CYP450)
enzymes alter the kinetics of hydroxylation for some
CAs.36 In the United States, 90% to 95% of people are
rapid hydroxylators. In that population, the half-life of
desipramine is 13 to 23 hours, whereas the half-life in the
subpopulation of slow hydroxylators is 81 to 131 hours.37
Cases of slow recovery from desipramine overdose38 and
toxicity from therapeutic dosing39 have been reported in
slow hydroxylators. Those with genetic defects in
CYP2C19 activity have signicantly higher plasma
concentration curves of amitriptyline compared with
normals.34 Age presents an additional variable that alters
serum concentrations of parent drug and metabolites.
Across all age groups an increase in serum concentrations of drug and metabolite is seen with increasing
age when dosing is weight adjusted. More efcient hepatic
biotransformation and renal clearance in children
compared with adults likely explains this phenomenon.40
Half-life of elimination for therapeutic doses of CAs
averages 8 to 30 hours with extension to 55 to 127 hours
540
CENTRAL NERVOUS SYSTEM
for protriptyline. The same drugs have longer half-lives
in the elderly.41,42 The prolonged elimination half-lives in
this population may lead to drug accumulation with daily
dosing.26
Toxicokinetic parameters for CAs are altered in the
setting of overdose. The anticholinergic properties of CAs
may lead to delayed gastric emptying, possibly prolonging
the absorptive phase, enhancing overall absorption, and
delaying time to peak serum concentrations.26 The onset
of toxicity after overdose is typically rapid, and most
deaths occur within the rst 6 hours postingestion. An
increased bioavailability following overdose may result
from a decreased rst pass metabolism as hepatic
enzymes become saturated.43 Since the unbound fraction
of CAs increases with an acid medium, acidemia will
enhance overall toxicity.
Kinetics in the postmortem state are dramatically
altered. In the steady state, CAs are normally highly
tissue bound. Following death, tissues release bound
drug, creating a false elevation in serum drug levels. The
serum concentrations increase as time proceeds postmortem. This can lead to confusion regarding the
manner of death. Strategies for postmortem laboratory
analysis are further discussed under Diagnosis.
Drug Interaction
Potential drug-drug interactions may develop through
various mechanisms (Table 27-2). Competitive inhibition
of CYP isoforms could lead to increased toxicity of
CAs or the drugs with which they compete for enzymatic
biotransformation. The competitive inhibition of
CYP2C19 by imipramine and nortriptyline has resulted
in elevated phenytoin concentrations in some patients.44,45
Induction of CYP isoforms by CAs may, conversely, lead
to decreased effectiveness of other medications.
Additional drug interactions include medications that
may potentiate the serotonergic or sympathomimetic
properties of CAs, such as monoamine oxidase inhibitors
(MAOIs), SSRIs, amphetamines, and others.
TOXICOLOGY
The most severe toxicities from CA overdose include
hypotension, dysrhythmia, coma, seizures, and hyperthermia. Cardiovascular toxicity results primarily from
effects on the cardiac cell action potential, negative
inotropy, direct effects on vascular tone, and indirect
effects mediated by the autonomic nervous system. CNS
toxicity is less well understood and is likely a combination of effects on cholinergic and GABA neurotransmission along with sodium channel effects. Deaths
are often a result of refractory hypotension.
Cardiovascular System Toxicity
CARDIAC CELL ACTION POTENTIAL
CAs alter the cardiac conduction system in a myriad of
ways. The most distinctive toxicity relates to the inhibition of the fast sodium channels in the His-Purkinje
tissue, leading to a slowing of phase 0 depolarization.46,47
This membrane stabilizing or quinidine-like effect is
analogous to that of Vaughn Williams (VW) class I
antidysrhythmic drugs.48 Impaired depolarization of cells
within the His-Purkinje system slows the propagation of
ventricular depolarization. This appears on the electrocardiogram (ECG) as prolongation of the QRS interval,
the hallmark of TCA toxicity. The degree of conduction
delay is rate-dependent and worsens with tachycardia.49
The QRS morphology is generally that of nonspecic
intraventricular conduction delay, with discrete bundle
branch block being less common. However, the longer
refractory period of the right bundle relative to the left
leads to the characteristic rightward axis deviation of the
terminal 40 msec of the QRS complex seen in many
patients with TCA toxicity.50 On the ECG this appears as
an increased R wave amplitude in lead aVR and a deep S
wave in leads I and aVL (Fig. 27-2).51 A less specic
nding is prolongation of the corrected QT interval
(QTc). This delay in myocyte repolarization may result
from a direct effect of CAs on potassium channels.52,53 A
prolonged QTc may also be seen in therapeutic dosing.
TABLE 27-2 Cyclic Antidepressant Drug Interactions
DRUG
MECHANISM
Anticoagulants
Amphetamines
Carbamazepine
Chloroquine
Cimetidine
Class Ia and Ic antidysrhythmics
MAOIs
Phenothiazines
Fluconazole
Class III antidysrhythmics
SSRIs
Inhibition of oral anticoagulant metabolism with subsequent elevated PT
Enhanced adrenergic stimulation via norepinephrine release
TCA metabolism, leading to subtherapeutic levels
Induction of additive effect of QT prolongation
Inhibition of TCA metabolism, leading to supratherapeutic levels
Additive effect of QT prolongation via Na channel blockade and QRS prolongation
Enhanced neurotransmitter release, leading to hypertensive crisis or serotonin syndrome
Additive effect on QT prolongation
Inhibition of TCA metabolism, leading to supratherapeutic levels; also increased QT interval
Additive QT prolongation
Risk of serotonin syndrome; competitive inhibition of CYP2D6 and CYP2C19, leading to
elevated steady-state TCA levels
Risk of serotonin syndrome
Risk of serotonin syndrome
Linezolid
MDMA (Ecstacy)
CHAPTER 27
FIGURE 27-2 ECG from a TCA-poisoned patient.
NEGATIVE INOTROPY AND VASCULAR SMOOTH
MUSCLE EFFECT
CAs inhibit the influx of calcium into cardiac and neural
tissue and interfere with calcium-coupled muscular contraction.54-56 This may explain the direct depressant effect
seen experimentally with isolated human myocardium in
response to CAs.57 Peripheral -adrenergic blockade may
cause postural hypotension at therapeutic doses. At toxic
doses, vasodilation contributes to hypotension.58
DYSRHYTHMIAS
Sinus tachycardia is the most common rhythm disturbance associated with CA overdose. The etiology is
multifactorial and includes anticholinergic effects,
increased norepinephrine release, and reflex tachycardia
in response to vasodilation. Although the tachycardia
does not generally cause morbidity itself, it is clearly a
sign of signicant toxicity.
Ventricular tachycardia (VT) is the most common
ventricular dysrhythmia seen in overdose. However,
discriminating this rhythm from the common underlying
sinus tachycardia with aberrant conduction (QRS
prolongation) may be difcult, since P waves are not
always visible. Some cases of VT described in the
literature may actually be supraventricular tachycardia
(SVT). P waves may be obscured by the preceding T wave
owing to the prolonged PR and QTc intervals along with
rapid heart rate. Intraesophageal electrode monitoring
may reveal P waves not visible on the standard ECG. An
alternative, less sophisticated technique useful in
discriminating these rhythms is to follow serial ECGs. A
gradual evolution of the QRS prior to loss of the P wave
suggests SVT with aberrant conduction. The presence of
fusion beats suggests a ventricular origin. Other criteria
commonly used to differentiate ventricular and supraventricular rhythms, such as QRS morphology and duration, have not been tested in patients with CA overdose
and may not be applicable in this setting.
Torsades de pointes (TdP) has been reported
following CA overdose.59,60 This phenomenon appears to
be a more common consequence of therapeutic dosing
than of overdose. The increased risk for TdP in
conjunction with a slow rhythm likely explains its higher
Tricyclic and Other Cyclic Antidepressants
541
prevalence in therapeutic dosing, since most acutely
poisoned patients are tachycardic. Several cases of
sudden death in children taking therapeutic doses of
CAs have been reported. QT prolongation with resultant
TdP is the speculated mechanism for these events.61
Other less common rhythms seen in overdose are
second- or third-degree atrioventricular block62 and
premature ventricular beats. Patients close to death are
more likely to develop bradycardia and atrioventricular
blocks.
Refractory hypotension is a common cause of death
due to CA overdose. Hypotension may occur in the
absence of other signs of cardiac toxicity such as QRS
prolongation.63 Hypotension is due in part to vasodilation from -adrenergic blockade, as well as direct
myocardial depression.57,58,64-66 This inotropic depression
is dose-dependent and independent of effects on the
cardiac conduction system.57 Signicant sinus tachycardia
may contribute to hypotension by decreasing the diastolic
period. This effect decreases ventricular lling time and
impairs coronary perfusion.
Central Nervous System Toxicity
CNS depression is a common feature of all CAs in
overdose. Symptoms range from fatigue to coma. The
greatest concern in CNS toxicity in overdose is seizures.
Although they most commonly occur in patients who
also display signs of cardiac toxicity, seizures may occur
in the absence of this nding.67,68 Maprotiline and
amoxapine are more likely than other CAs to cause
seizures.69,70 Seizures due to CAs most often occur within
1 to 2 hours of presentation, are brief in duration, and
resolve without the need for anticonvulsant medications.68
However, seizures may cause a metabolic acidosis that
could predispose patients to cardiac dysrhythmias. In
some case series, 10% to 20% of patients with seizures
abruptly developed cardiovascular deterioration (hypotension, ventricular dysrhythmias) during or within
minutes after the seizure.68,71 Patients with more severe
cardiovascular toxicity before the seizure were at highest
risk. Therefore, cardiovascular deterioration may have
been imminent regardless of the seizure, or potentially
worsened by a seizure-induced acidosis. A clear cause
and effect has not been identied. Other neurologic
symptoms include delirium and myoclonus. Delirium is
characterized by agitation, disorientation, and delusions
and is most likely attributable to the anticholinergic
properties of CAs. Although delirium may appear early
in the course of intoxication, it may also manifest several
hours later, after the initial period of sedation wanes.
It is not uncommon to witness the development of a
profound central antimuscarinic syndrome after 24 hours
when patients have survived the initial cardiovascular
consequences.
Toxicity in Other Systems
Peripheral anticholinergic toxicity may be seen with
agents possessing potent anticholinergic properties such
as amitriptyline. Signs and symptoms include urinary
542
CENTRAL NERVOUS SYSTEM
retention, ileus, and dry skin. Pupil size may vary
depending on the degree of anticholinergic versus
-adrenergic blockade. Pulmonary complications include
aspiration pneumonitis and adult respiratory distress
syndrome.72 These likely represent indirect toxicity
secondary to coma, hypotension, excessive fluid administration, or increased capillary permeability from direct
endothelial toxicity. Hyperthermia may ensue following
excessive heat generation from seizures or myoclonus in
the setting of decreased ability to dissipate heat through
sweating.
Ultimately, most deaths occur prior to hospital
presentation. Of those who survive to the hospital, death
occurs within the rst few hours of presentation with the
majority of deaths occurring in the rst 24 hours.73 It is
not uncommon for a patients clinical condition to
deteriorate rapidly with progression from no symptoms
to life-threatening cardiotoxicity in less than 1 hour.74
Late-occurring death results from complications of
prolonged hypotension, status epilepticus, or aspiration.
DIAGNOSIS
Electrocardiogram
The ECG is the most rapidly available screening tool for
predicting toxicity and guiding the management of CA
poisonings. QRS interval prolongation is the most
apparent ECG nding in serious CA toxicity and is a
marker of the sodium channel blockade resulting from
this drug class. The QRS axis is typically shifted to the
right, along with the axis of the terminal 40 msec of the
QRS complex. An increase in the R wave amplitude in
aVR accompanies this nding (see Fig. 27-2).51,75,76 These
parameters are useful in predicting serious adverse
outcomes such as seizures and ventricular tachycardia.
In one retrospective study, a maximal limb-lead QRS
duration greater than 100 msec identied patients at
greatest risk for seizures.67 However, these and other
complications may occur with a lesser degree of QRS
prolongation, and patients with any degree of QRS
prolongation are considered at risk for developing lifethreatening CA toxicity.77 This was demonstrated in
another retrospective study in which a maximal 12-lead
ECG QRS duration greater than 100 msec was only 53%
sensitive for ventricular dysrhythmias or seizures.78 The
low sensitivity for predicting serious outcomes despite
the use of a more sensitive measurement (maximal 12lead QRS) suggests that life-threatening complications
may develop irrespective of narrow QRS duration.
The terminal 40 msec QRS axis deviation greater than
120 degrees has been used to diagnose TCA toxicity, with
a range of sensitivities from 29% to 100%.50,75,77,79 The
most common way to detect this measure is to identify a
deep S wave in lead I or aVL and a terminal R wave in
lead aVR (see Fig. 27-2). The height of the R wave in aVR
also provides valuable information when evaluating CA
overdoses. A height greater than or equal to 3 mm is 81%
sensitive for predicting subsequent seizures or dysrhythmias.76 This compares with a sensitivity of 82% in
the same study for a QRS duration greater than 100 msec.
However, the positive predictive values for the aVR and
QRS criteria were 43% and 35%, respectively.
The QTc interval is mildly prolonged with therapeutic
doses of CAs and becomes more prolonged with
overdose.80 A corrected QTc greater than 480 msec in the
setting of CA poisoning has been linked to an increased
risk of seizures and dysrhythmias.51 However, this marker
is not useful in the diagnosis of CA toxicity versus nonCA ingestions.75,79
Interpretation of ECG criteria should be weighed with
the knowledge that the ECG is a dynamic measurement.
An initially normal ECG may rapidly evolve to reveal the
characteristic changes cited above. At the time of
presentation in one study, the maximum recorded QRS
interval was present on the ECG in 80% of patients.81
The remaining patients reached a maximum QRS
duration in a median time of 3 hours (range, 1 to 9). The
maximum T40 msec axis occurred at the time of
presentation in 86% in this same group, with the
remaining patients reaching this maximum in a median
time of 3 hours (range, 1 to 5). Therefore, frequent
ECGs are required during the rst few hours following a
CA overdose to monitor potential changes.
Laboratory Studies
CAs can be detected qualitatively in urine by thin-layer
chromatography or liquid chromatography, or quantitatively in serum by liquid or gas chromatography. Active
demethylated metabolites are usually measured via the
latter methods. Therapeutic CA concentrations are
generally in the range of 50 to 300 ng/mL (see Table
27-1). Bedside immunoassays are available; however, they
have not been extensively tested.82 False-positive results
from CA immunoassays are well documented and
include cross-reactions with quetiapine, carbamazepine,
diphenhydramine, and many others (Table 27-3).83-86
The correlation of serum CA concentrations with
toxicity is imprecise,67,73 and their measurement adds
little to the management of CA overdose. Life-threatening toxicity is usually accompanied by a serum concentration of greater than 100 ng/mL, while concentrations greater than 300 to 500 ng/mL are often fatal.47
The serum CA concentration may increase up to vefold
postmortem. When using CA levels to determine cause
of death, the measurement of liver drug concentrations
rather than blood concentration may avoid the tissue
redistribution artifact that leads to dramatic elevations in
blood CA content, even with therapeutic dosing.87-89
Another technique involves examining the ratio of
parent drug to metabolite. Typically, the metabolites are
found in greater concentration in patients taking
therapeutic doses, whereas fatal overdoses lead to a
much higher concentration of parent drug compared to
metabolites.
Without a clear history of CA ingestion, the diagnosis
may be confused with other drugs or disease states. CA
toxicity is most likely to resemble other drugs that
produce QRS prolongation. Drugs which may induce
cardiotoxicity indistinguishable from that of CAs include
CHAPTER 27
Tricyclic and Other Cyclic Antidepressants
543
TABLE 27-3 TCA Assays and Drugs Reported to Cause False-Positive Results
ASSAY
FLUID
DRUG CROSS-REACTIVITY
Abbott TDx/TDxFlx TCA immunoassay
Syva EMIT immunoassay
Blood
Blood
DuPont automatic clinical analyzer
Triage plus TCA
Homogenous enzyme immunoassay
(Microgenics, Syva)
Liquid chromatography
High-performance liquid chromatography
Gas chromatographymass spectrometry
Blood
Urine
Urine
Carbamazepine
Thioridazine, chlorpromazine, trimeprazine, cyproheptadine,
cyclobenzaprine, norcyclobenzaprine, diphenhydramine, quetiapine
Thioridazine
Cyclobenzaprine
Quetiapine
Blood
Blood
Blood
Diphenhydramine
Thioridazine, perphenazine, cyclobenzaprine, norcyclobenzaprine
No reported drug cross-reactivity
Adapted from Matos ME, Burns MM, Shannon MW: False-positive tricyclic antidepressant drug screen results leading to the diagnosis of carbamazepine
intoxication. Pediatrics 2000;105:E66.
VW class IA (quinidine, procainamide) or IC (flecainide,
encainide, propafenone) antidysrhythmic agents. Other
drugs that may prolong QRS duration in overdose
include cocaine, propranolol, quinine, chloroquine,
hydroxychloroquine, high-dose antipsychotics (thioridazine, chlorpromazine), propoxyphene, and diphenhydramine. Nondrug causes of QRS prolongation include
hyperkalemia, cardiac ischemia, and other conduction
system abnormalities.
MANAGEMENT
Supportive Measures
Given the risk of rapid deterioration, patients with
known or suspected CA overdose should have an
intravenous line started and cardiac rhythm should be
monitored continuously. An ECG on arrival can be
compared with subsequent ECGs obtained during the
monitoring period. Frequent measurement of vital signs
including temperature is imperative. Patients with severe
toxicity on presentation, including extreme lethargy,
agitation, seizures, or dysrhythmias, require early
intubation for airway protection. Particular attention to
acidbase status is paramount in managing a severe CA
overdose. Patients who develop acidosis from increased
muscle activity, seizures, or inadequate ventilation may
develop an increase in CA-protein dissociation and
subsequent clinical deterioration.
Initial measures for blood pressure support include
intravenous fluids and vasopressors such as norepinephrine. Because CA toxicity is reversible once the drug
is metabolized and excreted, temporary mechanical
support of the circulation may prove useful in hypotensive patients who are unresponsive to other measures.
Serum CA levels often decline rapidly following overdose
owing to distribution of the drug to tissues. A temporary
period of mechanically assisted circulation might,
therefore, allow time for spontaneous improvement.
Isolated reports of a child who survived 2.5 hours of
cardiopulmonary resuscitation during nonperfusing
ventricular tachycardia and of an adult treated successfully
with femoral-femoral extracorporeal circulation for
refractory hypotension support this possibility.90,91
Preliminary data in swine suggest that cardiopulmonary
bypass may allow survival after ingestion of an otherwise
fatal dose of CA.92 Augmentation of aortic outflow
utilizing a balloon pump device could provide additional
perfusion support when myocardial depression is severe.
Decontamination
Prompt administration of activated charcoal is indicated
if the ingestion occurs within 1 hour of presentation.
Charcoal may be given after this time period; however, its
effectiveness diminishes rapidly with time. Patients who
appear drowsy and are unable to drink the charcoal
without assist should be protected with tracheal intubation
prior to charcoal administration to prevent aspiration of
charcoal and subsequent serious pulmonary sequelae.
Laboratory Monitoring
As discussed above, measurement of serum CA concentrations provides little information regarding emergent
care of poisoned patients. However, qualitative screening
immunoassays may occasionally prove useful in the
detection of occult ingestion when overt clinical toxicity
is not detected. Measurement of serum electrolytes,
blood urea nitrogen, creatinine, creatine kinase,
hematocrit, and liver function tests provide information
regarding co-ingestions and other disease states that may
affect drug metabolism and excretion. Arterial blood gas
determinations are indicated for intubated patients and
for monitoring acidbase status when sodium bicarbonate
infusion is employed as a therapy for CA toxicity.
Antidotes
NaHCO3
When CAs were introduced into clinical practice, the
clinical characteristics of overdose were noted as sharing
many features of quinidine toxicity, for which hypertonic
sodium lactate (which is rapidly metabolized to bicarbonate) resulted in clinical improvement. The proposed
544
CENTRAL NERVOUS SYSTEM
mechanisms for this therapy include increased plasma
protein binding of CAs resulting from alkalemia,
reduced binding of CAs within the cardiac myocytes, and
overcoming the Na channel blockade via sodium
loading.93
Controlled animal studies clearly established that
hypertonic NaHCO3 is effective in reducing QRS prolongation, increasing blood pressure, and suppressing
ventricular ectopy due to CA toxicity.94-96 This effect is
demonstrated experimentally to be independent of and
additive to the effect of vasopressors.97 Some animal data
suggest that hypertonic sodium chloride infusions
provide additional benet with respect to treating
hypotension and ventricular tachycardia.98 However, the
amount of sodium delivered in these experiments was
15 mEq/kg or 10 mL/kg of 7.5% NaCl, a dose likely to
cause severe toxicity in humans. Intracellular pH elevation has been shown to reverse the toxicity of imipramine in cardiac myocytes.99 This intracellular alkalosis
is correlated with a decreased binding of imipramine.100
In human serum, alkalosis causes a decrease in the free
CA concentration.101
No randomized controlled human trials are published
relating to the efcacy of NaHCO3 infusion for the
treatment of CA poisoning.93 Retrospective reviews of a
few hundred patients in conjunction with case series and
case reports provide the basis of conrmation for the
effectiveness of NaHCO3 therapy in the treatment of
CA-induced hypotension, cardiac conduction delays, and
dysrhythmias in humans.93,102-105
Indications for therapy with NaHCO3 infusion are
acidemia (serum pH < 7.35), QRS width greater than or
equal to 100 msec, R wave in aVR greater than 3 mm, or
wide complex tachydysrhythmias. Optimal serum pH is
not well established. The target pH recommended by
various clinicians, as determined by survey, vary dramatically and range from a maximum of 7.45 to 7.8.106
However, the majority of clinicians recommend a
maximum serum pH of 7.55.106 Dosing protocols also
vary widely. The most common approach is to administer
1 mEq/kg NaHCO3 as an intravenous bolus in the
setting of a widened QRS or dysrhythmia. This may be
increased to achieve resolution of the dysrhythmia or
narrowing of the QRS (Fig. 27-3; see also Fig. 27-2).
Serum pH should not be permitted to exceed 7.55.
Continuous infusion may begin after improved cardiac
parameters are achieved with the bicarbonate bolus.
Adding 150 mEq of NaHCO3 to 1 L of D5W yields an
isotonic solution that can be infused at a rate 1.5 times
maintenance for the patients weight. The infusion rate
may be titrated to hourly serum pH measurements to
ensure adequate treatment without overalkalinization.
Frequent measurement of serum potassium is critical
owing to enhanced renal elimination of potassium in the
setting of alkalemia.
PHENYTOIN
Phenytoin was reported to improve QRS duration in an
uncontrolled series of patients and one preliminary
report that showed more rapid improvement of cardiovascular toxicity in patients randomized to phenytoin.107,108
FIGURE 27-3 ECG from a TCA-poisoned patient after NaHCO3
administration.
Controlled animal studies have not conrmed a benet,
and possible aggravation of ventricular ectopy was noted
in one report.109-111 These data do not support the clinical use of phenytoin for CA cardiotoxicity.
TCA ANTIBODIES
The use of TCA-specic antibody Fab fragments for the
treatment of TCA overdose, analogous to those used to
treat digoxin overdose, has been studied in rats. Fab
doses capable of binding 10% to 30% of the TCA body
burden rapidly reverse QRS prolongation and hypotension and prolong survival.112,113 The toxic dose of TCAs is
more than 100 times higher than that of digoxin,
however, and the theoretical Fab dose required to
reverse toxicity is also much higher (1 to 3 g/kg). One
case report details the successful use of experimental
ovine Fab in a human amitriptyline overdose.114 The
total dose of Fab administered was only 6% of the molar
quantity of TCA ingested. The authors reported a rapid
decrease in QRS and QTc intervals as well as an
improvement in mental status. No acute adverse reactions
were noted. The ability of the antibodies to bind
tetracyclic drugs such as amoxapine and maprotiline is
unknown. More extensive experience is required before
Fab fragments become part of routine therapy for TCA
poisoning.
1-ACID GLYCOPROTEIN
1-Acid glycoprotein (AAG) has demonstrated some
efcacy in the treatment of CA toxicity in animal models.
Because CAs are bound to AAG in plasma, the
administration of additional AAG would theoretically
bind a portion of the free CA fraction, thereby reducing
toxicity. Swine and rat studies have shown a trend toward
decrease in CA-induced QRS prolongation after the
administration of AAG.115,116 Currently, no evidence
suggests that administration of AAG in humans has any
role in the treatment of CA toxicity.
PHYSOSTIGMINE
Physostigmine was initially advocated as a treatment for
CA poisoning in the 1970s.117 Indications at the time
included seizures, coma, and tachydysrhythmias.118 The
rst case reports of asystole following the use of
CHAPTER 27
physostigmine were in the context of treating CAinduced seizures.119 Anecdotal reports of successful
treatment of seizures and dysrhythmias are not
substantiated by controlled data. Balancing the reported
successes are claims that physostigmine induces seizures
and asystole when used for CA poisoning. Unfortunately,
these are known complications of both CA poisoning as
well as physostigmine in isolation. The reported cases
linking physostigmine to these complications when used
for CA poisonings do not demonstrate a conclusive cause
and effect relationship.120 Thus, seizures may have
ceased in response to physostigmine or ceased despite
this therapy. Seizures occurring after the administration
of physostigmine may have occurred in response to
therapy or may have occurred regardless of this drug.
Similar logic applies to cases of asystole and bradycardia.
Many conclusions may be drawn, and these are based on
deductive reasoning rather than scientic evidence.
The pathophysiology of cardiac conduction delays
and seizures resulting from CA poisonings is poorly
explained by the anticholinergic properties of the drugs.
These features are not seen in pure anticholinergic
poisonings such as atropine and scopolamine. Rather,
the sodium channel effects of CAs provide a more
reasonable explanation. Therefore, the use of a purely
cholinergic drug for reversal of seizures and dysrhythmias
caused by sodium channel blockade lacks a rational
basis. In view of the known toxicities including seizures
and asystole from physostigmine in the absence of CA
poisoning, its use in the context of CA poisoning, where
seizures and cardiac dysrhythmias are a known
complication, is not recommended. However, patients
who survive the acute phase of CA poisoning and have
no evidence of cardiac conduction delay may continue to
suffer from the anticholinergic drug effects more than
24 hours after the ingestion. Physostigmine could be of
benet for controlling agitated delirium in this subset of
patients provided that a patient has demonstrated
cardiac stability for a prolonged period of monitoring.
Elimination Enhancement
Enhancing elimination of the CAs is difcult owing to
their large volume of distribution. Several uncontrolled
case reports note shorter than expected elimination halflives for CAs with the use of repeated doses of activated
charcoal. These data are of limited value because early
sampling may have misconstrued the CA distribution
phase as evidence of shortened half-life. In controlled
studies, repeated oral doses of activated charcoal have
been reported either to have no effect on the clearance
of subtoxic doses of imipramine121 or to shorten the
elimination half-life of doxepin or amitriptyline by
20%.122 Most deaths from CA overdose occur within
hours of drug ingestion, thereby limiting the utility of a
therapy that requires multiple doses over time. It is
possible, however, that repeated doses of charcoal might
shorten the duration of toxicity in slow hydroxylators
who display long CA half-life kinetics. Little active CA is
excreted in urine, and measures that enhance urinary CA
excretion have a negligible effect on total clearance.122
Tricyclic and Other Cyclic Antidepressants
545
Hemodialysis is ineffective in enhancing the
elimination of CAs because of their extensive protein
binding and lipid solubility. Hemoperfusion overcomes
these limitations but is relatively ineffective because of
the drugs large volume of distribution.123 One case
report noted removal of less than 2% of the ingested
dose of imipramine as parent drug or active metabolite
during 6 hours of hemoperfusion.32 Nevertheless, rapid
improvement in cardiotoxicity after CA overdose has
been anecdotally reported during hemoperfusion.124-126
However, rapid decline in serum CA levels secondary
to drug distribution may explain this observation. In
addition, improvements in acidbase status likely
contributed to improved cardiovascular status. In the
absence of supporting data, there is no role for
hemoperfusion in the treatment of CA poisoning.
DISPOSITION
Patients displaying signicant signs and symptoms of CA
toxicity such as QRS prolongation, lethargy, or
hypotension require admission and monitoring until
symptom-free for 24 hours.127,128 QRS duration may be
considered normal if it is less than 100 msec or similar to
the patients baseline QRS. When QRS duration is
marginally prolonged (100 to 120 msec) and no baseline
ECG is available, it may be unclear whether the observed
QRS duration is normal for that patient or prolonged
from the overdose. In this situation, measurement of the
serum CA concentration may be helpful later in
hospitalization as grounds for discontinuing therapy and
monitoring when drug concentrations are therapeutic or
low. A clearly elevated CA concentration would suggest
that the QRS prolongation is drug induced, and
therefore continued cardiac monitoring is indicated and
NaHCO3 therapy should continue. With the exception of
overdoses involving a sustained-release drug, patients
who are asymptomatic on presentation and do not
manifest signs of toxicity after 6 hours require no further
medical monitoring other than psychiatric evaluation.
ACKNOWLEDGMENTS
The authors acknowledge Paul R. Pentel, Daniel E.
Keyler, and Lester M. Haddad for their contribution to
the previous edition of this chapter.
REFERENCES
1. Lancaster NP, Foster AR: Suicidal attempt by imipramine
overdosage. BMJ 1959;5164:1458.
2. Azima H, Vispo RH: Imipramine: a potent new anti-depressant
compound. Am J Psychiatry 1958;115:245246.
3. Mann AM, Catterson AG, Macpherson AS: Toxicity of
imipramine: report on serious side effects and massive
overdosage. Can Med Assoc J 1959;81:2328.
4. Litovitz TL, Holm KC, Clancy C, et al: 1992 annual report of the
American Association of Poison Control Centers Toxic Exposure
Surveillance System. Am J Emerg Med 1993;11:494555.
5. Litovitz TL, Clark LR, Soloway RA: 1993 annual report of the
American Association of Poison Control Centers Toxic Exposure
Surveillance System. Am J Emerg Med 1994;12:546584.
546
CENTRAL NERVOUS SYSTEM
6. Watson WA, Litovitz TL, Rodgers GC II, et al: 2002 annual report
of the American Association of Poison Control Centers Toxic
Exposure Surveillance System. Am J Emerg Med 2003;21:353421.
7. Henry JA, Alexander CA, Sener EK: Relative mortality from
overdose of antidepressants. BMJ 1995;310:221224.
8. Hoppe-Roberts JM, Lloyd LM, Chyka PA: Poisoning mortality in
the United States: comparison of national mortality statistics and
poison control center reports. Ann Emerg Med 2000;35:440448.
9. Litovitz TL, Felberg L, Soloway RA, et al: 1994 annual report of
the American Association of Poison Control Centers Toxic
Exposure Surveillance System. Am J Emerg Med 1995;13:551597.
10. Litovitz TL, Felberg L, White S, et al: 1995 annual report of the
American Association of Poison Control Centers Toxic Exposure
Surveillance System. Am J Emerg Med 1996;14:487537.
11. Litovitz TL, Klein-Schwartz W, Caravata EM, et al: 1998 annual
report of the American Association of Poison Control Centers
Toxic Exposure Surveillance System. Am J Emerg Med
1999;17:435487.
12. Litovitz TL, Klein-Schwartz W, Dyer KS, et al: 1997 annual report
of the American Association of Poison Control Centers Toxic
Exposure Surveillance System. Am J Emerg Med 1998;16:443497.
13. Litovitz TL, Klein-Schwartz W, Rodgers GC II, et al: 2001 annual
report of the American Association of Poison Control Centers
Toxic Exposure Surveillance System. Am J Emerg Med
2002;20:391452.
14. Litovitz TL, Klein-Schwartz W, White S, et al: 1999 annual report
of the American Association of Poison Control Centers Toxic
Exposure Surveillance System. Am J Emerg Med 2000;18:517574.
15. Litovitz TL, Klein-Schwartz W, White S, et al: 2000 annual report
of the American Association of Poison Control Centers Toxic
Exposure Surveillance System. Am J Emerg Med 2001;19:337395.
16. Litovitz TL, Smilkstein M, Felberg L, et al: 1996 annual report of
the American Association of Poison Control Centers Toxic
Exposure Surveillance System. Am J Emerg Med 1997;15:447500.
17. McFee RB, Caraccio TR, Mofenson HC: Selected tricyclic
antidepressant ingestions involving children 6 years old or less.
Acad Emerg Med 2001;8:139144.
18. Snyder SH, Yamamura HI: Antidepressants and the muscarinic
acetylcholine receptor. Arch Gen Psychiatry 1977;34:236239.
19. Richelson E, Nelson A: Antagonism by antidepressants of
neurotransmitter receptors of normal human brain in vivo. J
Pharmacol Exp Ther 1984;230:94102.
20. Wagner A, et al: Weak binding of 10-hydroxymetabolites of
nortriptyline to rat brain muscarinic acetylcholine receptors. Life
Sci 1984;35:13791383.
21. Tunnicliff G, Malatynska E: Central GABAergic systems and
depressive illness. Neurochem Res 2003;28:965976.
22. Malatynska E, Crites GJ, Harrawood D, et al: Antidepressant
effects on GABA-stimulated 36Cl(-) influx in rat cerebral cortex
are altered after treatment with GABA(A) receptor antisense
oligodeoxynucleotides. Brain Res 2000;869:7884.
23. Barden N: Modulation of glucocorticoid receptor gene
expression by antidepressant drugs. Pharmacopsychiatry 1996;
29:1222.
24. Barden N: Regulation of corticosteroid receptor gene expression
in depression and depressant action. J Psychiatry Neurosci
1999;24:2539.
25. Calvo B, Garcia MJ, Pedraz JL, et al: Pharmacokinetics of
amoxapine and its active metabolites. Int J Clin Pharmacol Ther
Toxicol 1985;23:180185.
26. Rudorfer MV, Potter WZ: Metabolism of tricyclic antidepressants.
Cell Mol Neurobiol 1999;19:373409.
27. Herrera D, Mayet L, Galindo MC, et al: Pharmacokinetics of a
sustained-release dosage form of clomipramine. J Clin Pharmacol
2000;40:14881493.
28. Breyer-Pfaff U, Prox A, Wachsmuth H, et al: Phenolic metabolites
of amitriptyline and nortriptyline in rat bile. Drug Metab Dispos
1987;15:882889.
29. Greenblatt DJ, von Moltke LL, Shader RI: The importance of
presystemic extraction in clinical psychopharmacology. J Clin
Psychopharmacol 1996;16:417419.
30. Alvan G, Borga O, Lind M, et al: First pass hydroxylation of
nortriptyline: concentrations of parent drug and major
metabolites in plasma. Eur J Clin Pharmacol 1977;11:219224.
31. Sutn TA, DeVane CL, Jusko WJ: The analysis and disposition of
imipramine and its active metabolites in man. Psychopharmacology (Berl) 1984;82:310317.
32. Pentel PR, Bullock ML, DeVane CL: Hemoperfusion for
imipramine overdose: elimination of active metabolites. J Toxicol
Clin Toxicol 1982;19:239248.
33. Gram LF, Bjerre M, Kragh-Sorensen P, et al: Imipramine
metabolites in blood of patients during therapy and after
overdose. Clin Pharmacol Ther 1983;33:335342.
34. Jiang ZP, Shu Y, Chen XP, et al: The role of CYP2C19 in
amitriptyline N-demethylation in Chinese subjects. Eur J Clin
Pharmacol 2002;58:109113.
35. Shin JG, Park JY, Kim MJ, et al: Inhibitory effects of tricyclic
antidepressants (TCAs) on human cytochrome P450 enzymes in
vitro: mechanism of drug interaction between TCAs and
phenytoin. Drug Metab Dispos 2002;30:11021107.
36. Spina E, Steiner E, Ericsson D, et al: Hydroxylation of
desmethylimipramine: dependence on the debrisoquin hydroxylation phenotype. Clin Pharmacol Ther 1987;41:314319.
37. Brosen K, Otton SV, Gram LF: Imipramine demethylation and
hydroxylation: impact of the sparteine oxidation phenotype. Clin
Pharmacol Ther 1986;40:543549.
38. Spina E, Henthorn TK, Eleborg L, et al: Desmethylimipramine
overdose: nonlinear kinetics in a slow hydroxylator. Ther Drug
Monit 1985;7:239241.
39. Bluhm RE, Wilkinson GR, Shelton R, et al: Genetically determined drug-metabolizing activity and desipramine-associated
cardiotoxicity: a case report. Clin Pharmacol Ther 1993;53:8995.
40. Wilens TE, Biederman J, Baldessarini RJ, et al: Developmental
changes in serum concentrations of desipramine and 2hydroxydesipramine during treatment with desipramine. J Am
Acad Child Adolesc Psychiatry 1992;31:691698.
41. Schulz P, Turner-Tamiyasu K, Smith G, et al: Amitriptyline
disposition in young and elderly normal men. Clin Pharmacol
Ther 1983;33:360366.
42. Dawling S, Crome P, Braithwaite R: Pharmacokinetics of single
oral doses of nortriptyline in depressed elderly hospital patients
and young healthy volunteers. Clin Pharmacokinet 1980;5:394401.
43. Brosen K, Gram LF: First-pass metabolism of imipramine and
desipramine: impact of the sparteine oxidation phenotype. Clin
Pharmacol Ther 1988;43:400406.
44. Houghton GW, Richens A: Inhibition of phenytoin metabolism by
other drugs used in epilepsy. Int J Clin Pharmacol Biopharm
1975;12:210216.
45. Perucca E, Richens A: Interaction between phenytoin and
imipramine. Br J Clin Pharmacol 1977;4:485486.
46. Weld FM, Bigger JT II: Electrophysiological effects of imipramine
on ovine cardiac Purkinje and ventricular muscle bers. Circ Res
1980;46:167175.
47. Biggs JT, Spiker DG, Petit JM, et al: Tricyclic antidepressant
overdose: incidence of symptoms. JAMA 1977;238:135138.
48. Connolly SJ, Mitchell LB, Swerdlow CD, et al: Clinical efcacy and
electrophysiology of imipramine for ventricular tachycardia. Am
J Cardiol 1984;53:516521.
49. Nattel S: Frequency-dependent effects of amitriptyline on
ventricular conduction and cardiac rhythm in dogs. Circulation
1985;72:898906.
50. Niemann JT, Bessen HA, Rothstein RJ, et al: Electrocardiographic
criteria for tricyclic antidepressant cardiotoxicity. Am J Cardiol
1986;57:11541159.
51. Caravati EM, Bossart PJ: Demographic and electrocardiographic
factors associated with severe tricyclic antidepressant toxicity.
J Toxicol Clin Toxicol 1991;29:3143.
52. Terstappen GC, Pula G, Carignani C, et al: Pharmacological
characterization of the human small conductance calciumactivated potassium channel hSK3 reveals sensitivity to tricyclic
antidepressants and antipsychotic phenothiazines. Neuropharmacology 2001;40:772783.
53. Cuellar-Quintero JL, Garcia DE, Cruzblanca H: The antidepressant imipramine inhibits the M-type K+ current in rat
sympathetic neurons. Neuroreport 2001;12:21952198.
54. Joshi PG, Singh A, Ravichandra B: High concentrations of tricyclic
antidepressants increase intracellular Ca2+ in cultured neural
cells. Neurochem Res 1999;24:391398.
CHAPTER 27
55. Park TJ, Shin SY, Suh BC, et al: Differential inhibition of
catecholamine secretion by amitriptyline through blockage of
nicotinic receptors, sodium channels, and calcium channels in
bovine adrenal chromafn cells. Synapse 1998;29:248256.
56. Watts JA, Yates KM, Bader SK, et al: Mechanisms of Ca2+
antagonism in imipramine-induced toxicity of isolated adult rat
cardiomyocytes, Toxicol Appl Pharmacol 1998;153:95101.
57. Heard K, Cain BS, Dart RC, et al: Tricyclic antidepressants directly
depress human myocardial mechanical function independent
of effects on the conduction system. Acad Emerg Med 2001;
8:11221127.
58. Langou RA, Van Dyke C, Tahan SR, et al: Cardiovascular
manifestations of tricyclic antidepressant overdose. Am Heart J
1980;100:458464.
59. Davison ET: Amitriptyline-induced Torsade de Pointes: successful
therapy with atrial pacing. J Electrocardiol 1985;18:299301.
60. Alter P, Tontsch D, Grimm W: Doxepin-induced torsade de
pointes tachycardia. Ann Intern Med 2001;135:384385.
61. Alderton HR: Tricyclic medication in children and the QT interval:
case report and discussion. Can J Psychiatry 1995;40:325329.
62. Thorstrand C: Clinical features in poisonings by tricyclic antidepressants with special reference to the ECG. Acta Med Scand
1976;199:337344.
63. Shannon M, Merola J, Lovejoy FH II: Hypotension in severe tricyclic
antidepressant overdose. Am J Emerg Med 1988;6:439432.
64. Langslet A, Johansen WG, Ryg M, et al: Effects of dibenzepine and
imipramine on the isolated rat heart. Eur J Pharmacol 1971;
14:333339.
65. Sigg EB, Osborne M, Korol B: Cardiovascular effects of
imipramine. J Pharmacol Exp Ther 1963;141:237243.
66. Cairncross KD, McCulloch MW, Mitchelson F: The action of
protriptyline on peripheral autonomic function. J Pharmacol Exp
Ther 1965;149:365372.
67. Boehnert MT, Lovejoy FH II: Value of the QRS duration versus the
serum drug level in predicting seizures and ventricular
arrhythmias after an acute overdose of tricyclic antidepressants.
N Engl J Med 1985;313:474479.
68. Ellison DW, Pentel PR: Clinical features and consequences of
seizures due to cyclic antidepressant overdose. Am J Emerg Med
1989;7:510.
69. Litovitz TL, Troutman WG: Amoxapine overdose: seizures and
fatalities. JAMA 1983;250:10691071.
70. Rudorfer MV, Potter WZ: Antidepressants: a comparative review
of the clinical pharmacology and therapeutic use of the newer
versus the older drugs. Drugs 1989;37:713738.
71. Taboulet P, Michard F, Muszynski J, et al: Cardiovascular
repercussions of seizures during cyclic antidepressant poisoning.
J Toxicol Clin Toxicol 1995;33:205211.
72. Shannon M, Lovejoy FH II: Pulmonary consequences of severe
tricyclic antidepressant ingestion. J Toxicol Clin Toxicol 1987;
25:443461.
73. Hulten BA, Heath A: Clinical aspects of tricyclic antidepressant
poisoning. Acta Med Scand 1983;213:275278.
74. Callaham M, Kassel D: Epidemiology of fatal tricyclic antidepressant ingestion: implications for management. Ann Emerg
Med 1985;14:19.
75. Lavoie FW, Gansert GG, Weiss RE: Value of initial ECG ndings
and plasma drug levels in cyclic antidepressant overdose. Ann
Emerg Med 1990;19:696700.
76. Liebelt EL, Francis PD, Woolf AG: ECG lead aVR versus QRS
interval in predicting seizures and arrhythmias in acute tricyclic
antidepressant toxicity. Ann Emerg Med 1995;26:195201.
77. Caravati EM: The electrocardiogram as a diagnostic discriminator
for acute tricyclic antidepressant poisoning. J Toxicol Clin Toxicol
1999;37:113115.
78. Foulke GE, Albertson TE: QRS interval in tricyclic antidepressant
overdosage: inaccuracy as a toxicity indicator in emergency
settings. Ann Emerg Med 1987;16:160163.
79. Wolfe TR, Caravati EM, Rollins DE: Terminal 40-ms frontal plane
QRS axis as a marker for tricyclic antidepressant overdose. Ann
Emerg Med 1989;18:348351.
80. Pentel P, Sioris L: Incidence of late arrhythmias following tricyclic
antidepressant overdose. Clin Toxicol 1981;18:543548.
Tricyclic and Other Cyclic Antidepressants
547
81. Liebelt EL, Ulrich A, Francis PD, et al: Serial electrocardiogram
changes in acute tricyclic antidepressant overdoses. Crit Care Med
1997;25:17211726.
82. Schwartz JG, Hurd IL, Carnahan JJ: Determination of tricyclic
antidepressants for ED analysis. Am J Emerg Med 1994;12:513516.
83. Hendrickson RG, Morocco AP: Quetiapine cross-reactivity among
three tricylic immunoassays. J Toxicol Clin Toxicol 2003;41:105108.
84. Chattergoon DS, Verjee Z, Anderson M, et al: Carbamazepine
interference with an immune assay for tricyclic antidepressants in
plasma. J Toxicol Clin Toxicol 1998;36:109113.
85. Sloan KL, Haver VM, Saxon AJ: Quetiapine and false-positive
urine drug testing for tricyclic antidepressants. Am J Psychiatry
2000;157:148149.
86. Matos ME, Burns MM, Shannon MW: False-positive tricyclic
antidepressant drug screen results leading to the diagnosis of
carbamazepine intoxication. Pediatrics 2000;105:E66.
87. Apple FS: Postmortem tricyclic antidepressant concentrations:
assessing cause of death using parent drug to metabolite ratio.
J Anal Toxicol 1989;13:197198.
88. Apple FS, Bandt CM: Liver and blood postmortem tricyclic
antidepressant concentrations. Am J Clin Pathol 1988;89:794796.
89. Davis G, Park K, Kloss J, et al: Tricyclic antidepressant fatality:
postmortem tissue concentrations. J Toxicol Clin Toxicol
2001;39:649650.
90. Southall DP, Kilpatrick SM: Imipramine poisoning: survival of a
child after prolonged cardiac massage. BMJ 1974;4:508.
91. Williams JM, Hollingshed MJ, Vasilakis A, et al: Extracorporeal
circulation in the management of severe tricyclic antidepressant
overdose. Am J Emerg Med 1994;12:456458.
92. Larkin GL, Graeber GM, Hollingsed HM: Experimental amitriptyline
poisoning: treatment of severe cardiovascular toxicity with
cardiopulmonary bypass. Ann Emerg Med 1994;23:480486.
93. Blackman K, Brown SG, Wilkes GJ: Plasma alkalinization for
tricyclic antidepressant toxicity: a systematic review. Emerg Med
(Fremantle) 2001;13:204210.
94. Nattel S, Keable H, Sasyniuk BI: Experimental amitriptyline
intoxication: electrophysiologic manifestations and management.
J Cardiovasc Pharmacol 1984;6:8389.
95. Nattel S, Mittleman M: Treatment of ventricular tachyarrhythmias
resulting from amitriptyline toxicity in dogs. J Pharmacol Exp
Ther 1984;231:430435.
96. Pentel P, Benowitz N: Efcacy and mechanism of action of sodium
bicarbonate in the treatment of desipramine toxicity in rats. J
Pharmacol Exp Ther 1984;230:1219.
97. Knudsen K, Abrahamsson J: Epinephrine and sodium bicarbonate
independently and additively increase survival in experimental
amitriptyline poisoning. Crit Care Med 1997;25:669674.
98. McCabe JL, Cobaugh DJ, Menegazzi JJ, et al: Experimental
tricyclic antidepressant toxicity: a randomized, controlled
comparison of hypertonic saline solution, sodium bicarbonate,
and hyperventilation. Ann Emerg Med 1998;32:329333.
99. Bou-Abboud E, Nattel S: Relative role of alkalosis and sodium ions
in reversal of class I antiarrhythmic druginduced sodium channel
blockade by sodium bicarbonate. Circulation 1996;94:19541961.
100. Bou-Abboud E, Nattel S: Molecular mechanisms of the reversal of
imipramine-induced sodium channel blockade by alkalinization
in human cardiac myocytes. Cardiovasc Res 1998;38:395404.
101. Levitt MA, Sullivan JB II, Owens SM, et al: Amitriptyline plasma
protein binding: effect of plasma pH and relevance to clinical
overdose. Am J Emerg Med 1986;4:121125.
102. Hoffman JR, McElroy CR: Bicarbonate therapy for dysrhythmia
and hypotension in tricyclic antidepressant overdose. West J Med
1981;134:6064.
103. Koppel C, Wiegreffe A, Tenczer J: Clinical course, therapy, outcome
and analytical data in amitriptyline and combined amitriptyline/
chlordiazepoxide overdose. Hum Exp Toxicol 1992;11:458465.
104. Brown TC: Sodium bicarbonate treatment for tricyclic antidepressant arrhythmias in children. Med J Aust 1976;2:380382.
105. Brown TC, Barker GA, Dunlop ME, et al: The use of sodium
bicarbonate in the treatment of tricyclic antidepressantinduced
arrhythmias. Anaesth Intensive Care 1973;1:203210.
106. Seger DL, Hantsch C, Zavoral T, et al: Variability of recommendations for serum alkalinization in tricyclic antidepressant
548
107.
108.
109.
110.
111.
112.
113.
114.
115.
116.
CENTRAL NERVOUS SYSTEM
overdose: a survey of U.S. Poison Center medical directors.
J Toxicol Clin Toxicol 2003;41:331338.
Hagerman GA, Hanashiro PK: Reversal of tricyclic antidepressantinduced cardiac conduction abnormalities by phenytoin.
Ann Emerg Med 1981;10:8286.
Boehnert M, Lovejoy FH II: The effect of phenytoin on cardiac
conduction and ventricular arrhythmias in acute tricyclic
antidepressant (TCA) overdose. Vet Hum Toxicol 1985;27:297.
Callaham M, Schumaker H, Pentel P: Phenytoin prophylaxis
of cardiotoxicity in experimental amitriptyline poisoning.
J Pharmacol Exp Ther 1988;245:216220.
Kulig K, et al: Phenytoin as treatment for tricyclic antidepressant
cardiotoxicity in a canine model. Vet Hum Toxicol 1984;26:399.
Mayron R, Ruiz E: Phenytoin: does it reverse tricyclic antidepressantinduced cardiac conduction abnormalities? Ann Emerg
Med 1986;15:876880.
Dart RC, Sidki A, Sullivan JB II, et al: Ovine desipramine antibody
fragments reverse desipramine cardiovascular toxicity in the rat.
Ann Emerg Med 1996;27:309315.
Pentel PR, Scarlett W, Ross CA, et al: Reduction of desipramine
cardiotoxicity and prolongation of survival in rats with the use of
polyclonal drug-specic antibody Fab fragments. Ann Emerg Med
1995;26:334341.
Heard K, OMalley GF, Dart RC: Treatment of amitriptyline
poisoning with ovine antibody to tricyclic antidepressants. Lancet
1999;354:16141615.
Pentel PR, Keyler DE: Effects of high dose alpha-1-acid
glycoprotein on desipramine toxicity in rats. J Pharmacol Exp
Ther 1988;246:10611066.
Seaberg DC, Weiss LD, Yealy DM, et al: Effects of alpha-1-acid
glycoprotein on the cardiovascular toxicity of nortriptyline in a
swine model. Vet Hum Toxicol 1991;33:226230.
117. Manoguerra AS, Ruiz E: Physostigmine treatment of anticholinergic poisoning. JACEP 1976;5:125127.
118. Slovis TL, Ott JF, Teitebaum DT, et al: Physostigmine therapy in
acute tricyclic antidepressant poisoning. Clin Toxicol 1971;
4:451459.
119. Pentel P, Peterson CD: Asystole complicating physostigmine
treatment of tricyclic antidepressant overdose. Ann Emerg Med
1980;9:588590.
120. Linden C: ACMT net discussion of physostigmine use in the
context of TCA poisoning. ACMT.net.
121. Goldberg MJ, Park GD, Spector R, et al: Lack of effect of oral
activated charcoal on imipramine clearance. Clin Pharmacol Ther
1985;38:350353.
122. Karkkainen S, Neuvonen PJ: Pharmacokinetics of amitriptyline
influenced by oral charcoal and urine pH. Int J Clin Pharmacol
Ther Toxicol 1986;24:326332.
123. Heath A, Wickstrom I, Martensson E, et al: Treatment of
antidepressant poisoning with resin hemoperfusion. Hum Toxicol
1982;1:361371.
124. Diaz-Buxo JA, Farmer CD, Chandler JT: Hemoperfusion in the
treatment of amitriptyline intoxication. Trans Am Soc Artif Intern
Organs 1978;24:699703.
125. Marbury T, Mahoney J, Fuller T, et al: Treatment of amitriptyline
overdosage with charcoal hemoperfusion. Kidney Int 1977;
12:485.
126. Pedersen RS, Jorgensen KA, Olesen AS, et al: Charcoal haemoperfusion and antidepressant overdose. Lancet 1978;1:719720.
127. Frommer DA, Kulig KW, Marx JA, Rumack B: Tricyclic
antidepressant overdose: a review. JAMA 1987;257:521526.
128. Goldberg RJ, Capone RJ, Hunt JD: Cardiac complications
following tricyclic antidepressant overdose: issues for monitoring
policy. JAMA 1985;254:17721775.
Das könnte Ihnen auch gefallen
- Neuro-Psychopharmacology: Proceedings of the 11th Congress of the Collegium Internationale Neuro-Psychopharmacologicum, Vienna, July 9-14, 1978Von EverandNeuro-Psychopharmacology: Proceedings of the 11th Congress of the Collegium Internationale Neuro-Psychopharmacologicum, Vienna, July 9-14, 1978B. SaletuNoch keine Bewertungen
- Second and Third Generation Antipsychotics: A Comprehensive HandbookVon EverandSecond and Third Generation Antipsychotics: A Comprehensive HandbookBewertung: 5 von 5 Sternen5/5 (1)
- Hu Kira Inotrope and Vasopressor Use in CardiogenicDokument7 SeitenHu Kira Inotrope and Vasopressor Use in CardiogenicnhunhuochachNoch keine Bewertungen
- Toxicología Clínica Goldfrank Capítulo Intoxicación triciclicosDokument9 SeitenToxicología Clínica Goldfrank Capítulo Intoxicación triciclicosDavid Andrés BravoNoch keine Bewertungen
- The New Antiepileptic Drugs: Their Neuropharmacology and Clinical IndicationsDokument16 SeitenThe New Antiepileptic Drugs: Their Neuropharmacology and Clinical IndicationsAbdul RahmanNoch keine Bewertungen
- Comparative Tolerability Profiles of The Newer Versus Older AntidepressantsDokument29 SeitenComparative Tolerability Profiles of The Newer Versus Older AntidepressantsJucas EscobarNoch keine Bewertungen
- Goulet 1992Dokument6 SeitenGoulet 1992DANIEL - PRISMANoch keine Bewertungen
- Serotonin vs neuroleptic disorders contrastDokument8 SeitenSerotonin vs neuroleptic disorders contrastRonald ReaganNoch keine Bewertungen
- Terapia SimpatomoduladoraDokument10 SeitenTerapia SimpatomoduladorajijocasoNoch keine Bewertungen
- 1 s2.0 S0753332221008386 MainDokument7 Seiten1 s2.0 S0753332221008386 MainIsaura MendezNoch keine Bewertungen
- DocumentDokument5 SeitenDocumentTop MusicNoch keine Bewertungen
- Glassman, A - Cardiovascular Effects of Therapeutic Doses of Tricyclic AntidepressantsDokument6 SeitenGlassman, A - Cardiovascular Effects of Therapeutic Doses of Tricyclic AntidepressantsEduardo FrancoNoch keine Bewertungen
- Current Pharmacological and Non Pharmacological Treatments For Obsessive-Compulsive DisorderDokument14 SeitenCurrent Pharmacological and Non Pharmacological Treatments For Obsessive-Compulsive DisorderKelvin PangestuNoch keine Bewertungen
- SNM America PsikiatriDokument7 SeitenSNM America PsikiatriMuhammad Abdul RahmanNoch keine Bewertungen
- C102 1461-1474 PDFDokument14 SeitenC102 1461-1474 PDFstein godoy pachecoNoch keine Bewertungen
- Important Questions of Pharmacology by Medical Study CenterDokument10 SeitenImportant Questions of Pharmacology by Medical Study CenterLin YunNoch keine Bewertungen
- Serotonin Syndrome Vs Neuroleptic Malignant Syndrome: A Contrast of Causes, Diagnoses, and ManagementDokument9 SeitenSerotonin Syndrome Vs Neuroleptic Malignant Syndrome: A Contrast of Causes, Diagnoses, and ManagementMauro JacobsNoch keine Bewertungen
- Westjmed00231 0013Dokument9 SeitenWestjmed00231 0013Sitti AuraNoch keine Bewertungen
- Laboratory Testing in PsychiatryDokument29 SeitenLaboratory Testing in PsychiatrySera ChunNoch keine Bewertungen
- New Developments in Antidepressant TherapyDokument5 SeitenNew Developments in Antidepressant TherapyDoyin AwodeleNoch keine Bewertungen
- Alcohol Withdrawal KindlingDokument7 SeitenAlcohol Withdrawal KindlingMarco Macavilca CruzNoch keine Bewertungen
- Relationship Neurotransmitters Symptoms Major DepressiveDokument4 SeitenRelationship Neurotransmitters Symptoms Major DepressiveLilian LópezNoch keine Bewertungen
- Chap 118Dokument5 SeitenChap 118theodoruskevinNoch keine Bewertungen
- Predicting Neurological Outcome in Post Cardiac Arrest Patients Treated With HypothermiaDokument2 SeitenPredicting Neurological Outcome in Post Cardiac Arrest Patients Treated With HypothermiaDedi SutiaNoch keine Bewertungen
- Lecanemab SubmDokument21 SeitenLecanemab SubmHenrique OliveiraNoch keine Bewertungen
- (JOURNAL) What Is Neuroleptic Malignant SyndromeDokument3 Seiten(JOURNAL) What Is Neuroleptic Malignant SyndromeAndi Rizki TenryayuNoch keine Bewertungen
- Overview of Al-Adrenoceptor Antagonism and Recent Advances in Hypertensive TherapyDokument11 SeitenOverview of Al-Adrenoceptor Antagonism and Recent Advances in Hypertensive Therapyحمزة جمالNoch keine Bewertungen
- Overview of Al-Adrenoceptor Antagonism and Recent Advances in Hypertensive TherapyDokument11 SeitenOverview of Al-Adrenoceptor Antagonism and Recent Advances in Hypertensive Therapyحمزة جمالNoch keine Bewertungen
- Overview of Al-Adrenoceptor Antagonism and Recent Advances in Hypertensive TherapyDokument11 SeitenOverview of Al-Adrenoceptor Antagonism and Recent Advances in Hypertensive Therapyحمزة جمالNoch keine Bewertungen
- BurkeDokument10 SeitenBurkeMary FallNoch keine Bewertungen
- RTMS Reduces Craving and Alcohol Use in Patients WithDokument15 SeitenRTMS Reduces Craving and Alcohol Use in Patients WitharturohcuervoNoch keine Bewertungen
- Neuroleptic malignant syndrome - UpToDateDokument26 SeitenNeuroleptic malignant syndrome - UpToDateBárbara LimaNoch keine Bewertungen
- Essential Guide to Diagnosing and Treating Ischemic StrokeDokument21 SeitenEssential Guide to Diagnosing and Treating Ischemic Strokekuchaibaru90Noch keine Bewertungen
- Cuma Abstraknya Aja: TTG Risperidone: Stroke Therapy TreatmentsDokument6 SeitenCuma Abstraknya Aja: TTG Risperidone: Stroke Therapy TreatmentsChandz ChanDra ErryandariNoch keine Bewertungen
- CHR2012 GrassiDokument6 SeitenCHR2012 Grassipatrimonio79Noch keine Bewertungen
- Deprivacion Alcohol NEJM Review 2014Dokument5 SeitenDeprivacion Alcohol NEJM Review 2014paulioasisNoch keine Bewertungen
- Anestesicos Locales y La Respuesta InflamatoriaDokument18 SeitenAnestesicos Locales y La Respuesta InflamatoriarichabertNoch keine Bewertungen
- Acetylcholine and Delirium: Larry E. Tune Susan EgeliDokument3 SeitenAcetylcholine and Delirium: Larry E. Tune Susan EgelipppijkNoch keine Bewertungen
- Notes For ReportDokument20 SeitenNotes For ReportD'ArcyNoch keine Bewertungen
- Electro Convulsive TherapyDokument19 SeitenElectro Convulsive TherapyDeepshikha AhlawatNoch keine Bewertungen
- Wei Zheng, 2018Dokument8 SeitenWei Zheng, 2018Hananya ManroeNoch keine Bewertungen
- Presentation 1Dokument24 SeitenPresentation 1Seraj KhanNoch keine Bewertungen
- ClozapineDokument5 SeitenClozapineFebelina IdjieNoch keine Bewertungen
- Receptors Involved in Mental Disorders and The UseDokument17 SeitenReceptors Involved in Mental Disorders and The Usedabafe4365Noch keine Bewertungen
- Neuroleptic Malignant SyndromeDokument21 SeitenNeuroleptic Malignant SyndromeAndreea BujorNoch keine Bewertungen
- Neurophysiology of Depression and Bipolar Affective DisorderDokument17 SeitenNeurophysiology of Depression and Bipolar Affective DisorderShivan A.C.Noch keine Bewertungen
- 2 Pharmaco Oct 2018Dokument7 Seiten2 Pharmaco Oct 2018Nav ThiranNoch keine Bewertungen
- Ef Cardiov Nov AntideprDokument5 SeitenEf Cardiov Nov AntideprCamilla CristinaNoch keine Bewertungen
- Neuroleptic Malignant Syndrome: Author: Section Editor: Deputy EditorDokument11 SeitenNeuroleptic Malignant Syndrome: Author: Section Editor: Deputy EditoraureliasartikaNoch keine Bewertungen
- AANA Journal Course: Update For Nurse Anesthetists Neuroleptic Malignant SyndromeDokument6 SeitenAANA Journal Course: Update For Nurse Anesthetists Neuroleptic Malignant SyndromeMamenn DicinieNoch keine Bewertungen
- Neurohormonal Hypothesis in Heart FailureDokument11 SeitenNeurohormonal Hypothesis in Heart FailureCypress Trixia Mananquil MacapagalNoch keine Bewertungen
- Side Effects of Antipsychotic Drugs: A Pharmacovigilance Study Using VigiBase DataDokument13 SeitenSide Effects of Antipsychotic Drugs: A Pharmacovigilance Study Using VigiBase DataHazem JawishNoch keine Bewertungen
- (R) Alpha Lipoic Assists With Control of Neurogenic Orthostatic Hypotension, Hypertension, and Reduces Sudden Cardiac Death in Geriatric DiabeticsDokument21 Seiten(R) Alpha Lipoic Assists With Control of Neurogenic Orthostatic Hypotension, Hypertension, and Reduces Sudden Cardiac Death in Geriatric DiabeticsPharma Scientific NetworksNoch keine Bewertungen
- Posterior Reversible Encephalopathy Syndrome: A Review: Jai Shankar, DM, MSC, Jillian Banfield, PHDDokument7 SeitenPosterior Reversible Encephalopathy Syndrome: A Review: Jai Shankar, DM, MSC, Jillian Banfield, PHDkidNoch keine Bewertungen
- High-Dose Methotrexate With R-CHOP Therapy For The Treatment of Patients With Primary Central Nervous System LymphomaDokument7 SeitenHigh-Dose Methotrexate With R-CHOP Therapy For The Treatment of Patients With Primary Central Nervous System LymphomaFariz NurNoch keine Bewertungen
- Pi Is 1933287417302908Dokument11 SeitenPi Is 1933287417302908Anonymous yptjlwJNoch keine Bewertungen
- Psychiatric Comorbidities in Epilepsy PatientsDokument24 SeitenPsychiatric Comorbidities in Epilepsy PatientsSueNoch keine Bewertungen
- Systematic Review With Network Meta Analysis .492 PDFDokument1 SeiteSystematic Review With Network Meta Analysis .492 PDFPathiwat M ChantanaNoch keine Bewertungen
- Managing Cardiovascular Complications in DiabetesVon EverandManaging Cardiovascular Complications in DiabetesNoch keine Bewertungen
- Marketing Pharmaceutical ComplaintsDokument10 SeitenMarketing Pharmaceutical ComplaintskrizelNoch keine Bewertungen
- Tablet Sept'12 - Aprl 2015 - VeraDokument120 SeitenTablet Sept'12 - Aprl 2015 - VeraisyeabdullahNoch keine Bewertungen
- Sandoseacidplanet Com Product ActavisDokument5 SeitenSandoseacidplanet Com Product ActavisSandoseacidplanetNoch keine Bewertungen
- Analgesic Used in Oral SurgeryDokument70 SeitenAnalgesic Used in Oral SurgeryAkram ThabetNoch keine Bewertungen
- Treatments For Schizophrenia: A Critical Review of Pharmacology and Mechanisms of Action of Antipsychotic DrugsDokument26 SeitenTreatments For Schizophrenia: A Critical Review of Pharmacology and Mechanisms of Action of Antipsychotic DrugsMaria Jose CastañedaNoch keine Bewertungen
- SPLE Q ADokument90 SeitenSPLE Q AZahra Ahmed AlzaherNoch keine Bewertungen
- June 24, 2008: Statements by Dea Before CongressDokument55 SeitenJune 24, 2008: Statements by Dea Before CongressSTOUFFLET JusticeNoch keine Bewertungen
- Operating Room DrugsDokument3 SeitenOperating Room DrugsIan Kenneth Da Silva67% (3)
- Drugs BipolarDokument4 SeitenDrugs BipolarSheana TmplNoch keine Bewertungen
- PHA 070 Dispensing 2 P1 REVIEWER From QuizzizDokument6 SeitenPHA 070 Dispensing 2 P1 REVIEWER From Quizzizjenet soleilNoch keine Bewertungen
- LAPORAN MUTASI BHP LABORATORIUM BULAN JANUARI 2019Dokument32 SeitenLAPORAN MUTASI BHP LABORATORIUM BULAN JANUARI 2019tely rodjaNoch keine Bewertungen
- 601126KZ PDFDokument32 Seiten601126KZ PDFHari PriyaNoch keine Bewertungen
- Class 5Dokument430 SeitenClass 5Subash NeupaneNoch keine Bewertungen
- Sublingual Morphine for Cancer Pain: Limited Data on EfficacyDokument9 SeitenSublingual Morphine for Cancer Pain: Limited Data on EfficacysalamredNoch keine Bewertungen
- Tabel 2.1 - Tabel 2.2 Spesialit Dan TermDokument3 SeitenTabel 2.1 - Tabel 2.2 Spesialit Dan TermElsa SeptinaNoch keine Bewertungen
- D.G. Pugh, DVM, MS (Auth.) - Sheep & Goat Medicine (2002) PDFDokument2 SeitenD.G. Pugh, DVM, MS (Auth.) - Sheep & Goat Medicine (2002) PDFJose Carlos Pascual HernándezNoch keine Bewertungen
- Prescription AuditDokument23 SeitenPrescription Auditkanchan waghmareNoch keine Bewertungen
- Lampiran Telahan Staf Obat dan Perlengkapan MedisDokument13 SeitenLampiran Telahan Staf Obat dan Perlengkapan MedisIna Rama BahtiarNoch keine Bewertungen
- Formularium Obat Viva Generik Kebraon: AntibiotikDokument8 SeitenFormularium Obat Viva Generik Kebraon: AntibiotikLahar SatryaNoch keine Bewertungen
- Drug Study CHNDokument3 SeitenDrug Study CHNelijahdale.guillergan-05Noch keine Bewertungen
- Calcium CarbonateDokument1 SeiteCalcium CarbonateMikko EnocNoch keine Bewertungen
- List of PMPF products with validity from September 1st, 2021Dokument94 SeitenList of PMPF products with validity from September 1st, 2021Gabriel SilvaNoch keine Bewertungen
- Midterm Exam Review for Pharmacology Nursing StudentsDokument11 SeitenMidterm Exam Review for Pharmacology Nursing StudentsMark Jheran Alvarez100% (1)
- Meet Top PFS Experts, Network With 100+ Pharma and Biotech Industry Leaders Next Week in BostonDokument3 SeitenMeet Top PFS Experts, Network With 100+ Pharma and Biotech Industry Leaders Next Week in BostonPR.comNoch keine Bewertungen
- Curriculum VitaeDokument2 SeitenCurriculum VitaedeepajolyNoch keine Bewertungen
- Gopal Satyanarayan Karva: Formulation Research ScientistDokument4 SeitenGopal Satyanarayan Karva: Formulation Research ScientistgopalNoch keine Bewertungen
- Chapter 13: Antiparkinsonian DrugsDokument5 SeitenChapter 13: Antiparkinsonian DrugsKT100% (1)
- 13 Chapter 5Dokument64 Seiten13 Chapter 5yoganaNoch keine Bewertungen
- Biologicals and Biosimilars: An OverviewDokument8 SeitenBiologicals and Biosimilars: An OverviewBaru Chandrasekhar RaoNoch keine Bewertungen
- Morphine and Alternative Opioids in Cancer Pain: The EAPC RecommendationsDokument7 SeitenMorphine and Alternative Opioids in Cancer Pain: The EAPC RecommendationsSri HariNoch keine Bewertungen