Beruflich Dokumente
Kultur Dokumente
Association Between Atopy and Allergic Contact Dermatitis in Dr. Sardjito General Hospital Yogyakarta
Hochgeladen von
vaniaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Association Between Atopy and Allergic Contact Dermatitis in Dr. Sardjito General Hospital Yogyakarta
Hochgeladen von
vaniaCopyright:
Verfügbare Formate
J Med Sci
Volume 45, No.2, June 2013: 87-94
Fitria et al., Association between atopy and allergic contact dermatitis
in Dr. Sardjito General Hospital Yogyakarta
Association between atopy and allergic
contact dermatitis in Dr. Sardjito General
Hospital Yogyakarta
Fitria1 *, Retno Danarti2 , Hardyanto Soebono2
1
Faculty of Medicine, Universitas Syiah Kuala, Banda Aceh, 2Department of
Dermato-Venereology, Faculty of Medicine, Universitas Gadjah Mada/Dr. Sardjito
General Hospital, Yogyakarta
ABSTRACT
Association between atopy and development of allergic contact dermatitis (ACD) remains controversial.
T cell disfunctions in a patient with atopy complicate the process of nickel sensitization. On the
other, the decrease of the skin barrier function and overexpression of Langerhans cells in the patient
facilitate the sensitization. This study aimed to evaluate the association between atopy and incidence
of nickel ACD. A case-control study was carried out in Allergic and Immunology Sub Department of
Dermato-Venereology Policlinic, Dr. Sardjito General Hospital, Yogyakarta, involving 54 nickel ACD
patients as case group and 74 healthy subjects as control group. All subjects underwent prick test
allergens i.e. house dust, dust mite, cockroach, mixed fungi, nuts and egg white. The skin reaction
was considered as a positive result if a wheal diameter of at least 3 mm larger than the negative
control or a minimum of half of the positive control. The relationship between atopy and the nickel
ACD incidence was analyzed using Chi-Square test with confidence interval (CI) of 95%. A significant
association between atopy and the nickel ACD incidence was observed in this study. Subjects with
atopy to 1 allergen had risk of nickel ACD 3.74 higher than subjects without atopy (odds ratio/
OR=3.74; 95%CI = 1.64-8.53). Furtheremore, subjects with atopy to 2 allergens had risk of
nickel ACD 3.74 higher than subjects without atopy (OR=2.08; 95%CI = 1.01-4.29). In conclusion,
atopy is a risk factor of nickel ACD.
ABSTRAK
Hubungan antara atopi dan munculnya dermatitis kontak alergi (DKA) masih kontroversial. Pada
penderita atopi terjadi gangguan fungsi sel T yang menghambat proses sensitisasi nikel. Di sisi
lain, fungsi sawar kulit penderita atopi menurun dan terjadi ekspresi berlebih sel Langerhans
yang mempermudah sensitisasi. Penelitian ini bertujuan untuk mengkaji hubungan antara atopi
dan kejadian DKA nikel. Penelitian menggunakan rancangan kasus kontrol dilakukan di Divisi
Alergi dan Imunologi, Poliklinik Kulit dan Kelamin, Rumah Sakit Umum Dr. Sardjito Yogyakarta
yang melibatkan 54 pasien DKA nikel positif sebagai kelompok kasus dan 74 sukarelawan sehat
sebagai kelompok kontrol. Semua subjek menjalai tes tusuk dengan beberap alergen yaitu debu
rumah, tungau debu, kecoa, mixed fungi, kacang tanah dan putih telur. Hasil tes dikatakan
positif bila diameter reaksi kulit e 3 mm dari kontrol negatif atau separo dari kontrol positif.
Hubungan antara atopi dengan kejadian DKA nikel dianalisis menggunakan uji Chi-Square dengan
taraf kepercayaan 95%. Hubungan nyata antara atopi dengan kejadian DKA nikel ditemukan
dalam penelitian ini. Subjek dengan atopi terhadap 1 alergen mempunyai risiko DKA nikel 3,74
lebih tinggi dibandingkan dengan subjek tanpa atopi (OR=3,74; 95%CI = 1,64-8,53). Selanjutnya
subjek dengan atopi terhadap 2 alergen mempunyai risiko DKA nikel 2,08 lebih tinggi
dibandingkan dengan subjek tanpa atopi (OR=2,08; 95%CI = 1,01-4,29). Dapat disimpulkan
bahwa atopi merupakan faktor risiko DKA nikel.
Keywords: atopy - allergic contact dermatitis - nickel allergy - prick test - allergen
* corresponding author: fitria.spkk@gmail.com
87
J Med Sci, Volume 45, No.2, June 2013: 87-94
INTRODUCTION
Allergic contact dermatitis (ACD) is type
IV hypersensitive reaction, mediated by cellular
response caused by contact with spesific
allergen to sensitized individuals. Allergic
contact dermatitis frequently occurs in daily life
and can influence patients quality of life.1-4
Prevalence of ACD is about 12.5-40.6% in
general population and 4-10% based on patient
visit data in dermatology clinic in Thailand and
Saudi Arabia.2-4 In Dermatology-Venereology
Policlinic of Dr. Sarjito General Hospital,
Yogyakarta in 2010, 5.3% patients of ACD case
out of the whole patient visits were diagnozed.
Nickel ACD is the most frequent ACD that
occurs in about 10-20% out of the all patients
who underwent patch test. The high incidence
of nickel ACD is caused by many equipments
used in daily life that contain nickel.4,5 Diagnosis
of nickel ACD is easy to be performed due to
its specific clinical manifestation. However,
patch test is gold standard method to diagnose
the sensitivity existence to an allergen substance
in ACD.6
Atopy is a kind of hypersensitive reaction
to an environment allergen that associated with
multiple abnormalities including Langerhans
cell over-expression, immunoglobulin E (IgE)
dysregulation through Th2 immune response,
eosinophyl overactivities and genetic predisposition. 7
A strong predisposition toward atopy has
been reported and studies to map susceptibility
genes for atopy have been performed by
investigators. One of gene i.e. filaggrin has
become the gene with the most widely
associated to atopic eczema. Filaggrin null
mutations cause defective skinbarrier functions
lead to ease the penetration of environment
allergens, increase trans-epidermal water loss
(TEWL) and decrease skin hydration that
stimulate skin inflammation reactions by
88
increasing cytokin proinflamation production.8,9
Other gen that involved on the pathophysiology
of atopic diseases is a gene that encodes
fragment crystallizable epsilon receptor I
(Fc[RI). The Fc[RI is a protein found on the
surface of cells that binds to a part of IgE known
as the Fc (Fragment, crystallizable) region. In
atopic diseases, a strong upregulation of Fc[RI
on effector cells of anaphylaxis such as mast
cells and basophils is observed. Ligation of the
high-affinity Fc[RI on the effector cells can
induce cell activation and immediate release
of inflammatory mediator. 10
The prevalence of atopy in Western
countries is about 20-45% and it becomes the
main cause of chronic diseases among
children. 11 A person with atopy typically
presents with one or more of the following
symptoms such as allergic asthma, allergic
rhinitis, allergic conjunctivitis and atopic
dermatitis.7 Exposure to possible exacerbating
factors of environment such as aeroallergen,
irritating chemical and foods can be examined
by skin Prick test or IgE specific antigenantibody test. 12
This study was conducted to verify the
association between atopy and ACD occurrence
among patients visiting Dr. Sardjito General
Hospital, Yogyakarta, Indonesia.
MATERIALS AND METHODS
Subjects
This was a case control study conducted in
Allergic and Immunology Sub Department of
Dermato-Venereology Policlinic, Dr. Sardjito
General Hospital, Yogyakarta. The study was
started on September 2011 until the numbers of
samples obtained. The case group was all nickel
ACD patients with positive nickel result in
patch test, while the control group was healthy
individuals without dermatitis lesions. All
subjects would undergo a prick test of house
Fitria et al., Association between atopy and allergic contact dermatitis
in Dr. Sardjito General Hospital Yogyakarta
dust, dust mite, cockroach, mixed fungi, peanuts
and white egg allergen.
All subjects were asked to sign an informed
consent. The subject would be excluded from
the study in the condition of 1) consume systemic
antihistamine within 5 days before the research,
except ketotifen (15 days); 2) consume systemic
corticosteroid more than 20mg/day within 2
weeks before study; 3) topical corticosteroid
application on the test spot during 2 weeks
before study; 4) consume systemic immunomodulator agents within the last 4 weeks before
study.
The protocol of study has been approved
by the Medical and Health Research Ethic
Committee, Faculty of Medicine, Universitas
Gadjah Mada, Yogyakarta.
Protocol of study
Subject who met the inclusion and
exclusion criteria was given an explanation
concerning the background, objectives, and
benefit of the study. Subjects who were willing
to be involved in the study, an informed consent
was given to be signed. Subjects then underwent
anamnesis and clinical examination to obtain
the characteristics of subjects, history of illness,
ect. Dermatology picture were taken and used
as base line data of the skin conditions before
patch test.
The patch test was performed for subjects
suspected of suffering from nickel ACD. Left
upper arm skin was cleaned with 0.9% NaCl
solution and dried with a tissue. A
-chamber
containing 20 L Trolab 5% nickel sulphate
allergen was applied onto the skin of upper left
arm and fixed with an adhesice tape (HipaFix).
Subjects were then asked to back home with an
instruction form. The subsequent assessment of
skin reaction using a magnifying lamp was
performed by Dermatologist from Allergic and
Immunology Sub Department of DermatoVenereology Policlinic, Dr. Sardjito General
Hospital after 2, 3 and 4 days. The skin reaction
was measured based on the International
Contact Dermatitis Research Group (ICDRG)
scoring system. Dermatology picture were
taken again and used as data of the skin
conditions after the patch test. Results of the
patch test were then informed to the subjects.
All subjects in both group then underwent
a prick test. The forearm skin of the subject was
cleaned with 0.9% NaCl solution and dried with
a tissue. Skin prick solution of the appropriate
allergen (0.1 mL house dust, dust mite,
cockroach, mixed fungi, white egg and peanuts
solution) was pricked smoothly using a 23 g
syringe needle in several sites with each site
should be a minimum of 2 cm apart. The skin
reaction was measured in diameter 15-20
minutes after the skin prick. The skin reaction
was considered as a positive result if a wheal
diameter of at least 3 mm larger than the negative
control or a minimum of half of the positive
control. All measurements were recorded and
informed to the subjects.
Statistical analysis
Data analysis was conducted using non
parametric Chi-Square test to evaluate the
hypothesis dealing with the association between
atopy and nickel ACD incidence. If the ChiSquare test requirement was not fulfilled, Fisher
test would be used. Sum of risk factor was
calculated using odds ratio (OR) with
confidence interval of 95%.
RESULTS
One hundred and twenty eigh subjects that
consisted of 54 subjects of nickel ACD as case
group and 74 healthy subjects as control group
were involved in this study. Subject characteristics are presented in TABLE 1. The subjects
89
J Med Sci, Volume 45, No.2, June 2013: 87-94
consisted of 86 female (67.2%) and 42 male
(32.8%). The nickel ACD group consisted of
38 female (29.7%) and 16 male (12.5%), while
the control group consisted of 48 female
(37.5%) and 26 male (20.3%). In this study, the
incidence of nickel ACD was higher on female
than male subjects. The mean of age of subjects
in the nickel ACD group was 30.69 9.447
years, while in the control group was 30.23
9.632 years.
TABLE 1. Main characteristic of subjects in both group
Positive prick test result to allergens of
house dust, dust mite, cockroach, mixed fungi,
white egg and peanuts is presented in TABLE
2. In this study, the most positive results of
allergen prick test were dust mite (38.2%) and
cockroach (28.1%). The dust mite positive
result occuring on the nickel ACD group (29 or
22.7% of subjects) was significantly hinger
(p<0.05) than on the control group (21 or 16.4
subjects).
TABLE 2. Comparison of prick test result in the nickel ACD group and the control groups
The frequency of positive reaction on prick
test to allergens in this study is presented in
TABLE 3. The TABLE 3 shows that 10 (7.8%)
subjects of the nickel ACD group and 34
(26.6%) subjects of the control group gave
negative result on prick test. Positive result on
90
prick test to one allergen was obtained on 17
(13.3%) subjects of the nickel ACD group and
16 (12.56%) of the control group, while positive
result to two allergens or more was obtained
on 27 (21.1%) subjects of the nickel ACD group
and 24 (18.7%) subjects of the control group.
Fitria et al., Association between atopy and allergic contact dermatitis
in Dr. Sardjito General Hospital Yogyakarta
TABLE 3.
Frequency of positive reaction on prick test to allergens between
the nickel ACD and the control groups
The frequency of atopy based on positive
result of prick test to one allergen or more in
the nickel ACD group and the control group is
presented on TABLE 4. This study found that in
the nickel ACD, atopy was found on 44 (34.4%)
subjects and non atopy was found on 10 (7.8%)
TABLE 4.
subjects, whereas in the control group, atopy
was found on 40 (31.3%) subjects and non atopy
was found on 34 (26.6%) subjects. Statistical
analysis showed that subjects with atopy had
risk of nickel ACD 3.74 higher than subjects
without atopy (OR=3.74; 95%CI = 1.64-8.53).
Frequency of atopy based on positive result of prick test to 1 allergen in nickel
ACD and control groups
The incidence of atopy based on positive
result on patch test to two or more allergens is
shown in TABLE 5. The TABLE 5 shows that
atopy was found on 31 (24.2%) subjects and
non atopy was found on 31 (24.2%) subjects in
the nickelACD group, while in the control group,
atopy was found on 21 (16.4%) subjects, and
non atopy was found on 45 (35.2%) subjects.
This study showed that atopy is still the risk
factor of nickel ACD. Subjects with atopy had
risk of nickel ACD 2.08 higher than subjects
without atopy (OR=2.08; 95%CI = 1.01-4.29).
Additionally, statistical analysis using Chisquare showed a significant relationship
between atopy and nickel ACD incidences.
91
J Med Sci, Volume 45, No.2, June 2013: 87-94
TABLE 5.
Incidence of atopy based on positive result of prick test to two or more allergens in
the nickel ACD and control groups
DISCUSSION
This study found that the incidence of nickel
ACD was higher on female than male subjects.
Study in Norway conducted by Dotterud and
Sivertsen 13 also reported that incidence of
nickel ACD appeared more higher on female
(31.1%) than on male (5.0%). Another study
conducted in Denmark in 1992-2009 also
reported that incidence of nickel ACD was
higher on female (21.7%) than on male
(5.2%).14 Moreover, this restrospective study
reported that the higher incidence of nickel ACD
was found on the age more than 25 years
(34.9%) compared to on the age less than 25
years (22.1%).14 The higher incidence of nickel
ACD on female and on older people due to they
tend to have more intense contact to equipments
containing nickel such as jewelries and housewares. While males tend to have sensitivity on
nickel resulted from equipments in their working
places. 15,16
This study found that the most positive
results of allergen prick test were dust mite
(38.2%) and cockroach (28.1%). This result is
similar to that which has been found in other
studies conducted in other countries. A study
conducted in China also reported that the most
common sensitizing aeroallergens are dust mite
(30.6%) and cockroach (25.2%). 17 Another
study conducted in Uganda reported that the
sensitization to house dust mite allergens
(27.7%) and cockroach (15.8%) is the most
common in the environment. 18 The high
92
sensitivity to dust mite and cockroach allergens
may be caused theses two allergens are easily
found anywhere, particularly in houses and
habitations.17,18
This study also showed that atopy is still
the risk factor of nickel ACD. Subjects with
atopy had risk of nickel ACD 2.08 higher than
subjects non atopy. This result is similar to that
which has been reported in other studies. A
study conducted by Thyssen et al.19 also reported
that subject with atopy had risk of nickel ACD
1.5 higher in comparison to subject non atopy.
Moreover, it was reported that the rate of atopy
in patients with nickel ACD showed an increase
from 23% in 1982 to 33% in 1997. Nickel is
thought to be a contributory factor in causing
occupational dermatitis. 20
The higher prevalence of nickel ACD on
subjects with atopy could be caused by the
increase of absorption and penetration of nickel
allergens due to the decrease of skin barrier
function in subject with atopy. It leads the
catching of hapten-protein complex by Langerhans cells easier. The decrease of the skin barrier
function is caused by the down regulation of
filaggrin and loricrin, as well as numbers of
ceramide, the increase of endogen proteolitic
enzyme prodction and the higher loss of transepidermal water. 21,22 Filaggrin is crucial for the
maintenance of the skin barrier function. Lossof-function mutations within the filaggrin gene
are associated with skin barrier diseases. In
addition, filaggrin deficiency may also represent
Fitria et al., Association between atopy and allergic contact dermatitis
in Dr. Sardjito General Hospital Yogyakarta
a risk factor for contact sensitization to allergens
especially nickel allergen. 21 Tanaka et al. 23
reported that subject with atopy had disfunction
of skin barrier characterized by lower skin
surface hydration levels that caused allergen
agents or irritants easier crossed the skin barrier.
It was also reported that approximately 77%
subjects with atopy had positive patch test result
indicating that atopy has an impotant role in the
incidence of contact hypesensitivity.24
Other factors that have an impotant role in
the etiology of atopy is cytokines proinflammatory such as like TNF and IL-1 and
keratinocyte cytokines such as IL-6, IL-8, IL10, GM-CSF and TGF produced on a skin
barrier disfunction. The increase of TNF and
IL-1 production leads to upregulation of MCH
class I and II, but downregulation of E-cadherin
that binds to Langerhans cells in epidermis. It
stimulates migration of the Langerhans cells
from epidermis to lymph nodes tissue and
induces an antigen presentation to specific T
cell. This process causes an excessive Langerhans cells response to allergens and increases
an incidence of sensitization.25
CONCLUSION
In conclusion, atopy is a risk factor of nickel
ACD.
ACKNOWLEDGEMENTS
Authors would like to thank the Head of
Department of Dermato-Venerology, Faculty of
Medicine, Universitas Gadjah Mada/Dr.
Sardjito General Hospital for his permission
to conduct this study, as well as all subjects
who have participated in this study.
REFERENCES
1.
Kimber I, Basketter DA, Gerberick GF, Dearman
RJ. Allergic contact dermatitis. Int Immunopharmacol. 2002; 2 (23): 20111.
2.
Heine G. 2004. Frequently of contact allergy in
German children and adolescent patch test
between 1995-2002. Contact Dermatitis. 2004;
51: 111.
3. Thyssen JP, Linneberg A, Menne T, Johansen JD.
The epidemiology of contact allergy in the general
population prevalence and main findings.
Contact Dermatitis. 2007; 57(5): 287-99.
4. Omar M and Bukhari IA. Result of patch testing at
dermatology clinic of King Fahd hospital of the
university during the years 2001 to 2006. J
Chinese Clin Med. 2008; 3:228-30.
5. Matilla L, Kilpelainen M, Terho EO, Koskenvuo
M. Prevalence of nickel allergy among Finnish
university student in 1995. Contact Dermatitis.
2001; 44(4): 218-23.
6. Lachapelle JM, Maibach HI. The methodology of
patch testing. In: Lachapelle JM, Maibach HI
editors. Patch testing prick testing a practical
guide. New York: Springer-Verlag, 2003;7-66.
7. Modlin RL, Kim J, Maure D, Bangert C, Stingi J.
Innate and adaptive immunity in the skin. In: Wolff
K, Goldsmith LA, Katz SI, Gilchrest BA, Paller
AS, Leffell DJ, editors. Fitzpatricks Dermatology
in General Medicine . 7 th eds, New York:
McGrawHill, 2008:106-12.
8. Baurecht H, Irvine AD, Novak N, Illig T, Bhler B,
et al. Toward a major risk factor for atopic
eczema: Meta-analysis of filaggrin polymorphism
data. J Allergy Clin Immunol. 2007;120(2):140612.
9. Cork MJ, Robinson DA, Vasilopoulos Y, Ferguson
A, Moustafa M, McGowan A, et al . New
perspectives on epidermal barrier dysfunction in
atopic dermatitis: gene-environment interactions.
J Allergy Clin Immunol. 2006;118(1):3-21.
10. Novak N, Tepel C, Koch S. Evidence for a
differential expression of the Fc epsilon RI gamma
chain in dendritic cells of atopic and nonatopic
donors. J Clin Invest. 2003; 111(7):104756.
11. Mortz CG, Lauritsen JM, Jensen CB, Andersen K.
Prevalence of atopic dermatitis, asthma, allergic
rhinitis, and hand and contact dermatitis in
adolescents. The Odense adolescence cohort
study on atopic disease and dermatitis. Br J
Dermatol. 2001; 144(3): 523-32.
12. Wuthrich B. What is atopy? Condition, disease and
a syndrome? In: Wuthrich B editor. The atopy
syndrome in the Third Millennium. Curr Probl
Dermatol. Basel, Karger, 1999; 28: 1-8.
93
J Med Sci, Volume 45, No.2, June 2013: 87-94
13. Dotterud L and Sivertsen TS. Allergic contact
sensitization in the general adult population: A
population-based study from Nothern Norway.
Contact Dermatitis. 2007; 56(1): 10-5.
14. Caroe C, Andersen KE, Mortz CG. Fluctuations
in the prevalence of nickel and cobalt allergy in
eczema patients patch tested after implementation
of the nickel regulation in Denmark. Contact
Dermatitis. 2011; 64(3): 126-31.
15. Uter W, Pfahlberg A, Gefeller O, Geier J, Schnuch
A. Risk factors for contact allergy to nickel
results of a multifactorial analysis. Contact
Dermatitis. 2003; 48(1): 33-8.
16. Modjtahedi BS, Modjtahedi SP, Maibach HI. The
sex of the individual as a factor in allergic contact
dermatitis. Contact Dermatitis. 2004; 50(2): 539.
17. Kim JS, Ouyang F, Pongracic J, Fang Y, Wang B,
Liu X, et al. Dissociation between the prevalence
of atopy and allergic disease in rural china among
children and adults. J Allergy Clin Immunol. 2008;
122(5): 929-35.
18. Mpairwe H, Muhangi L, Ndibazza J, Tumusiime J,
Muwanga M, Rodrigues LC, et al. Skin prick test
reactivity to common allergens among women in
Entebbe, Uganda. Trans R Soc Trop Med Hyg.
2008; 102(4): 367-73.
19. Thyssen JP, Milting K, Bregnhj A, Ssted H,
Duus Johansen J, Menn T. Nickel allergy in
94
20.
21.
22.
23.
24.
25.
patch-tested female hairdressers and assessment
of nickel release from hairdressers scissors and
crochet hooks. Contact Dermatitis. 2009; 61(5):
281-6.
Dawn G, Gupta G, Forsyth A. The trend of nickel
allergy from a Scottish tertiary referral centre.
Contact Dermatitis. 2000; 43(1): 27-30.
Novak N, Baurecht H, Schafer T, Rodriguez E,
Wagenpfeil S, Klopp N, et al. Loss of function
mutation in the filaggrin gene and allergic contact
sensitization to nickel. J Invest Dermatol. 2008;
128(6): 1430-5.
Chu DH. Overview of biology, development, and
structure of the skin. In: Wolff K, Goldsmith LA,
Katz SI, Gilchrest BA, Paller AS, Leffell DJ,
editors. Fitzpatricks dermatology in general
medicine. 7 th ed. New York: McGrawHill,
2008:57-67.
Tanaka M, Okada M, Zhen XY, Inamra N, Kitano
T, Shirai S, et al. Decreased hydration state of the
stratum corneum and reduced amino acid content
of the skin surface in patient with seasonal allergic
rhinitis. Br J Dermatol. 1998; 139 (4): 618-21.
Manzini BM., Ferdani, G, Simoneti, V, Donini, M,
Seidenari, S. Contact sensitization in children.
Pediatr Dermatol. 1998; 15(1): 12-7.
McFadden JP, Basketter DA. Contact allergy,
irritancy and danger. Contact Dermatitis.2000;
42(3): 123-7.
Das könnte Ihnen auch gefallen
- Practical Patch Testing and Chemical Allergens in Contact DermatitisVon EverandPractical Patch Testing and Chemical Allergens in Contact DermatitisNoch keine Bewertungen
- Jurnal Reading Dermatitis KontakDokument14 SeitenJurnal Reading Dermatitis Kontaksulesa askawiNoch keine Bewertungen
- Specific Immunotherapy in Atopic Dermatitis: ReviewDokument9 SeitenSpecific Immunotherapy in Atopic Dermatitis: ReviewEsty GusmelisaNoch keine Bewertungen
- Allergic Contact Dermatitis - TranslateDokument9 SeitenAllergic Contact Dermatitis - Translatewahyuni taslimNoch keine Bewertungen
- Apa 1 80Dokument7 SeitenApa 1 80Rosyid PrasetyoNoch keine Bewertungen
- Prevalence of Allergic Rhinitis Symptoms and Positive Skin Prick Test Results in Children With Recurrent EpistaxisDokument6 SeitenPrevalence of Allergic Rhinitis Symptoms and Positive Skin Prick Test Results in Children With Recurrent EpistaxisKevinFeraldyNoch keine Bewertungen
- Nickel Sensitization and Dietary Nickel Are A Substantial Cause of Symptoms Provocation in Patients With Chronic Allergic-Like Dermatitis SyndromesDokument8 SeitenNickel Sensitization and Dietary Nickel Are A Substantial Cause of Symptoms Provocation in Patients With Chronic Allergic-Like Dermatitis SyndromesDwi PurwantiNoch keine Bewertungen
- Associated Factors of Widespread Pattern of Dermatitis Among Patch Test Population: 12-Year Retrospective StudyDokument6 SeitenAssociated Factors of Widespread Pattern of Dermatitis Among Patch Test Population: 12-Year Retrospective StudyDerryAryaPratamaNoch keine Bewertungen
- Research Letters: Urticaria Caused by DimenhydrinateDokument2 SeitenResearch Letters: Urticaria Caused by DimenhydrinateNauroh NaurohNoch keine Bewertungen
- Allergy & Therapy: Contact Dermatitis: Therapeutics When Avoidance FailsDokument4 SeitenAllergy & Therapy: Contact Dermatitis: Therapeutics When Avoidance FailsIda AmsiyatiNoch keine Bewertungen
- Do Not Copy: Skin Testing in AllergyDokument3 SeitenDo Not Copy: Skin Testing in AllergyHusni mubarakNoch keine Bewertungen
- Patch Testing of Experimentally Sensitized Beagle Dogs - Development of A Model For Skin Lesions of Atopic Dermatitis (Pages 95-102)Dokument8 SeitenPatch Testing of Experimentally Sensitized Beagle Dogs - Development of A Model For Skin Lesions of Atopic Dermatitis (Pages 95-102)jenNoch keine Bewertungen
- Single Nucleotide Polymorphism-Based Genome-Wide Linkage Analysis in Japanese Atopic Dermatitis FamiliesDokument8 SeitenSingle Nucleotide Polymorphism-Based Genome-Wide Linkage Analysis in Japanese Atopic Dermatitis FamiliesdermRounds Dermatology NetworkNoch keine Bewertungen
- Immediate Hypersensitivity and Serum IgE AntibodyDokument9 SeitenImmediate Hypersensitivity and Serum IgE AntibodyMini LaksmiNoch keine Bewertungen
- Relationship Between Rhinitis Severity, Skin Prick Test Reactivity and Mite-Specific Immunoglobulin E in Allergic Rhinitis Patients in MakassarDokument9 SeitenRelationship Between Rhinitis Severity, Skin Prick Test Reactivity and Mite-Specific Immunoglobulin E in Allergic Rhinitis Patients in MakassarrifkywownoidNoch keine Bewertungen
- Spiewak 2008 To Allergy JDokument11 SeitenSpiewak 2008 To Allergy JAJITH KUMARNoch keine Bewertungen
- Allergic Conjunctivitis and The Most Common Allergens in Northern GreeceDokument5 SeitenAllergic Conjunctivitis and The Most Common Allergens in Northern GreeceivanputrasNoch keine Bewertungen
- Wollenberg Et Al 2013 AllergyDokument11 SeitenWollenberg Et Al 2013 AllergyArturo VeraNoch keine Bewertungen
- The Efficiency and Safety of Olopatadine Against Rupatadine in Chronic Urticaria of Idiopathic Origin: A Comparative StudyDokument6 SeitenThe Efficiency and Safety of Olopatadine Against Rupatadine in Chronic Urticaria of Idiopathic Origin: A Comparative StudyArezoo JamNoch keine Bewertungen
- Characteristics of Atopic Dermatitis in Puskesmas (Public Health Center) Masaran 1 Sragen RegencyDokument8 SeitenCharacteristics of Atopic Dermatitis in Puskesmas (Public Health Center) Masaran 1 Sragen RegencyShafira Nur LNoch keine Bewertungen
- Contact Dermatitis BJD Guidelines May 2009Dokument9 SeitenContact Dermatitis BJD Guidelines May 2009Cynthia OktariszaNoch keine Bewertungen
- Makieieva Atopic Dermatitis, Allergic Rhinitis 21-34153Dokument22 SeitenMakieieva Atopic Dermatitis, Allergic Rhinitis 21-34153Ibtissame BadadNoch keine Bewertungen
- Contact Eczema of Hands Caused by Contact With Potato ProteinDokument2 SeitenContact Eczema of Hands Caused by Contact With Potato ProteinNurvita WidyastutiNoch keine Bewertungen
- Allergic Contact DermatitisDokument4 SeitenAllergic Contact DermatitisAnnisa Chaerani BurhanuddinNoch keine Bewertungen
- Atopic Dermatitis 2013Dokument32 SeitenAtopic Dermatitis 2013Bagus Maha ParadipaNoch keine Bewertungen
- RiccaDokument4 SeitenRiccastanleyNoch keine Bewertungen
- IdjofDokument7 SeitenIdjofGisda AzzahraNoch keine Bewertungen
- Environmental Exogenous Factors and Facial Dermatitis: A Case Control StudyDokument5 SeitenEnvironmental Exogenous Factors and Facial Dermatitis: A Case Control StudyRafly FairuzNoch keine Bewertungen
- Double-blind trial compares eczema creamsDokument7 SeitenDouble-blind trial compares eczema creamsguugle gogleNoch keine Bewertungen
- The Susceptibility of Pathogens Associated With Acne Vulgaris To AntibioticsDokument7 SeitenThe Susceptibility of Pathogens Associated With Acne Vulgaris To AntibioticsMuhammad AdiNoch keine Bewertungen
- IndianJOphthalmol6791400-3383915 092359Dokument5 SeitenIndianJOphthalmol6791400-3383915 092359diancahyaNoch keine Bewertungen
- 90-Article Text With Names and Affiliation-154-1!10!20190919Dokument4 Seiten90-Article Text With Names and Affiliation-154-1!10!20190919Agharid Ali HusseinNoch keine Bewertungen
- DermatitisDokument9 SeitenDermatitisKevin HartonoNoch keine Bewertungen
- Gribbles Heska Gvmar BF Nat 01542Dokument32 SeitenGribbles Heska Gvmar BF Nat 01542Emna BouhajjaNoch keine Bewertungen
- Alternaria in Patients With Allergic Rhinitis.Dokument8 SeitenAlternaria in Patients With Allergic Rhinitis.Dasi HipNoch keine Bewertungen
- Statistic of ACDDokument17 SeitenStatistic of ACDyensan26Noch keine Bewertungen
- IgE Allergy Testing World Allergy Position PaperDokument50 SeitenIgE Allergy Testing World Allergy Position PaperAlfred AlfredNoch keine Bewertungen
- Tear Levels of Interleukin (IL) 2 &4 in Patients With Allergic Conjunctivitis (Levels of Cytokines in Tear)Dokument5 SeitenTear Levels of Interleukin (IL) 2 &4 in Patients With Allergic Conjunctivitis (Levels of Cytokines in Tear)International Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Profile of allergy sufferers with positive skin prick test results for housedust mitesDokument5 SeitenProfile of allergy sufferers with positive skin prick test results for housedust mitesDimas Gramer ManiaNoch keine Bewertungen
- Vitamin D Deficiency and Its Relation To Allergic Diseases A Cross Sectional Study Among Allergic Patients From Jeddah City Saudi ArabiaDokument17 SeitenVitamin D Deficiency and Its Relation To Allergic Diseases A Cross Sectional Study Among Allergic Patients From Jeddah City Saudi ArabiaAthenaeum Scientific PublishersNoch keine Bewertungen
- IL-4 and IFN-y in Atopic and Non-Atopic Patients with Occupational Allergic Contact DermatitisDokument6 SeitenIL-4 and IFN-y in Atopic and Non-Atopic Patients with Occupational Allergic Contact DermatitisshaviraNoch keine Bewertungen
- Atopic Dermatitis Pathophysiology DiagnosisDokument9 SeitenAtopic Dermatitis Pathophysiology Diagnosiswe sagara dewiNoch keine Bewertungen
- Clinico-Microbiological Study of Pyodermas: Research Article Janardhan. B, Prasad - GK, Nandeshwar - AJ and Vidyavathi.NDokument5 SeitenClinico-Microbiological Study of Pyodermas: Research Article Janardhan. B, Prasad - GK, Nandeshwar - AJ and Vidyavathi.NradiNoch keine Bewertungen
- Contact Allergy in The Population of Patients With Chronic Inflammatory Dermatoses and Contact Hypersensitivity To CorticosteroidsDokument7 SeitenContact Allergy in The Population of Patients With Chronic Inflammatory Dermatoses and Contact Hypersensitivity To CorticosteroidsKulit SukapuraNoch keine Bewertungen
- BagusDokument45 SeitenBagusDesty Adjaahh LaahhNoch keine Bewertungen
- Konjungtivitis AlergiDokument8 SeitenKonjungtivitis AlergipitkerenNoch keine Bewertungen
- Allergic Rhinitis Slides 070926 PDFDokument57 SeitenAllergic Rhinitis Slides 070926 PDFmhamad kabraNoch keine Bewertungen
- Out 4Dokument3 SeitenOut 4Musthafa Afif WardhanaNoch keine Bewertungen
- Alergi - Allergen Standardization and Skin TestsDokument10 SeitenAlergi - Allergen Standardization and Skin TestsIntan Siti HulaimaNoch keine Bewertungen
- Etiology of Allergic Contact DermatitisDokument5 SeitenEtiology of Allergic Contact DermatitisChichi Dita VirllianaNoch keine Bewertungen
- Hwang 2002Dokument7 SeitenHwang 2002Adel AdielaNoch keine Bewertungen
- Role of Environmental Allergens On Atopic DermatitisDokument4 SeitenRole of Environmental Allergens On Atopic DermatitisLediraNoch keine Bewertungen
- Content ServerDokument8 SeitenContent Serverdesta israwandaNoch keine Bewertungen
- DermatitisDokument6 SeitenDermatitisAmalia Zulfa AmandaNoch keine Bewertungen
- A Study of Clinical Types of Contact Allergic Dermatitis of Hands and Its Association With AllergensDokument8 SeitenA Study of Clinical Types of Contact Allergic Dermatitis of Hands and Its Association With AllergensRika FitriaNoch keine Bewertungen
- Roles of Adapalene in The Treatment of Pityriasis VersicolorDokument5 SeitenRoles of Adapalene in The Treatment of Pityriasis VersicolorexaNoch keine Bewertungen
- Laboratory Diagnosis and Prevalence Study: of Corneal Infections From A Tertiary Eye Care HospitalDokument5 SeitenLaboratory Diagnosis and Prevalence Study: of Corneal Infections From A Tertiary Eye Care HospitalSilih Pulihan MedrofaNoch keine Bewertungen
- Original Article Paederus Dermatitis in South IndiaDokument6 SeitenOriginal Article Paederus Dermatitis in South Indiasoumalya481Noch keine Bewertungen
- 8 - Reversal of Atopic Dermatitis With Narrow-Band UVB Phototherapy and Biomarkers - Tintle ShemerDokument15 Seiten8 - Reversal of Atopic Dermatitis With Narrow-Band UVB Phototherapy and Biomarkers - Tintle ShemerSandrine SinsoulieuNoch keine Bewertungen
- 2 Ijesroct20172Dokument10 Seiten2 Ijesroct20172TJPRC PublicationsNoch keine Bewertungen
- Undang Undang No1 2009Dokument267 SeitenUndang Undang No1 2009vaniaNoch keine Bewertungen
- 8 FragranceDokument13 Seiten8 FragranceAlmira IsmaryadiNoch keine Bewertungen
- Original Aticle Hand EczemaDokument6 SeitenOriginal Aticle Hand EczemaAlmira IsmaryadiNoch keine Bewertungen
- Original Aticle Hand EczemaDokument6 SeitenOriginal Aticle Hand EczemaAlmira IsmaryadiNoch keine Bewertungen
- Human Contact May Reduce Stress in Shelter DogsDokument5 SeitenHuman Contact May Reduce Stress in Shelter DogsFlorina AnichitoaeNoch keine Bewertungen
- Advanced Level Biology 2015 Marking SchemeDokument29 SeitenAdvanced Level Biology 2015 Marking SchemeAngiee FNoch keine Bewertungen
- Growth and DevelopmentDokument10 SeitenGrowth and DevelopmentPiyush DuttaNoch keine Bewertungen
- 0610 IECR P3 Q1 v2 PDFDokument9 Seiten0610 IECR P3 Q1 v2 PDFGAIA Educators - Home TuitionNoch keine Bewertungen
- WCH03 01 Que 20180124Dokument16 SeitenWCH03 01 Que 20180124Rameez Mazhar SiddiqiNoch keine Bewertungen
- Bioinformatic Analysis of HBBDokument1 SeiteBioinformatic Analysis of HBBfrank2689Noch keine Bewertungen
- PMLSP 2 ReviewerDokument38 SeitenPMLSP 2 ReviewerSophia Mae ClavecillaNoch keine Bewertungen
- Physiological Psychology ReviewerDokument13 SeitenPhysiological Psychology ReviewerLeopando Rod CyrenzNoch keine Bewertungen
- Microbiological Test of Medical DevicesDokument5 SeitenMicrobiological Test of Medical Devicesbijendra_sinhaNoch keine Bewertungen
- Agilent ASMS 2019 ThP762 PosterDokument4 SeitenAgilent ASMS 2019 ThP762 PostersppNoch keine Bewertungen
- Psychiatric Mental Health Nursing Concepts of Care in Evidence Based Practice 8th Edition Townsend Test BankDokument36 SeitenPsychiatric Mental Health Nursing Concepts of Care in Evidence Based Practice 8th Edition Townsend Test Bankquemefuloathableilljzf100% (26)
- Organizing A TextDokument3 SeitenOrganizing A TextMercedes Jimenez RomanNoch keine Bewertungen
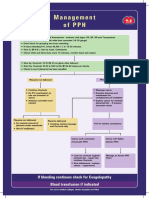
- Management of PPHDokument1 SeiteManagement of PPH098 U.KARTHIK SARAVANA KANTHNoch keine Bewertungen
- Ficha Técnica SpotcheckDokument5 SeitenFicha Técnica SpotcheckJuan PazNoch keine Bewertungen
- Kenya's Natural Capital AtlasDokument139 SeitenKenya's Natural Capital AtlasElvis Ole Sankale Ntimama100% (7)
- Conference on Global Issues in Agricultural, Environmental and Forestry SciencesDokument16 SeitenConference on Global Issues in Agricultural, Environmental and Forestry SciencesShirish NarnawareNoch keine Bewertungen
- Ewh Ix PDFDokument80 SeitenEwh Ix PDFOR Premium FreeNoch keine Bewertungen
- Analisis Kualitatif Dan Kuantitatif Kandungan Kimia Dari Ekstrak Heksan, Aseton, Etanol Dan Air Dari Umbi Bawang Putih (Allium Sativum Linn.)Dokument11 SeitenAnalisis Kualitatif Dan Kuantitatif Kandungan Kimia Dari Ekstrak Heksan, Aseton, Etanol Dan Air Dari Umbi Bawang Putih (Allium Sativum Linn.)Tari PratiwiNoch keine Bewertungen
- Citric Acid Production Stirred TankDokument9 SeitenCitric Acid Production Stirred TankKarliiux MedinaNoch keine Bewertungen
- Essay On Physical SelfDokument2 SeitenEssay On Physical Selfcmestrada03Noch keine Bewertungen
- 10th Standard Tamilnadu State Board Science (English Medium)Dokument283 Seiten10th Standard Tamilnadu State Board Science (English Medium)Karthick NNoch keine Bewertungen
- The "Five Families" College Essay ExampleDokument1 SeiteThe "Five Families" College Essay ExampleKishor RaiNoch keine Bewertungen
- Lec.6.Varietal & Hybrid Seed Production in RiceDokument75 SeitenLec.6.Varietal & Hybrid Seed Production in RiceAmirthalingam KamarajNoch keine Bewertungen
- Evolution of Pharmacy in the PhilippinesDokument2 SeitenEvolution of Pharmacy in the PhilippinesRosemarie OngNoch keine Bewertungen
- Paul Atriedes (PL 6/181pp) : Bene Gesserit Training (Container, Active 11)Dokument2 SeitenPaul Atriedes (PL 6/181pp) : Bene Gesserit Training (Container, Active 11)dfgdfNoch keine Bewertungen
- Effects of Climate on Living Things"This title "TITLE "Effects of Climate on Living ThingsDokument2 SeitenEffects of Climate on Living Things"This title "TITLE "Effects of Climate on Living ThingsMelannie Magalong100% (1)
- DNA Replication Practice PDFDokument2 SeitenDNA Replication Practice PDFKim100% (1)
- MDU Open Elective 3rd Sem Date Sheet May 2019Dokument1 SeiteMDU Open Elective 3rd Sem Date Sheet May 2019Ratan DeshNoch keine Bewertungen
- HHS Public Access: Structure and Function of The Human Skin MicrobiomeDokument20 SeitenHHS Public Access: Structure and Function of The Human Skin MicrobiomeEugeniaNoch keine Bewertungen
- LWT - Food Science and TechnologyDokument8 SeitenLWT - Food Science and TechnologyAzb 711Noch keine Bewertungen