Beruflich Dokumente
Kultur Dokumente
Comparison of Injectable Iron
Hochgeladen von
drfaruqui2551Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Comparison of Injectable Iron
Hochgeladen von
drfaruqui2551Copyright:
Verfügbare Formate
R
Safety of intravenous iron formulations: facts and folklore
Michael Auerbach1, Iain C. Macdougall2
School of Medicine Georgetown University, Washington DC, United States of America; 2Department of Nephrology,
King's College Hospital, London, United Kingdom
Sr
l
TI
S
er
v
It is unlikely that anyone reading this review was not
taught that intravenous (IV) iron is dangerous. While early
preparations were associated with an unacceptably high
rate of serious adverse events, most notably anaphylactic
shock, newer formulations with carbohydrate shells
which bind the elemental iron more tightly, allowing for
a much slower release, are very much safer with serious
toxicity being marginal to absent in prospective trials.
The perception of risk is fueled by misinterpretation and
misinformation of the clinical nature of minor infusion
reactions1, inappropriate use of premedication with
diphenhydramine2 and inferences made about the relative
safety of the available formulations using spontaneous
adverse event reporting systems, methodologies
proscribed by regulatory agencies3,4. In this article we
review published evidence on the relative safety of the
different formulations, highlight errors in interpretation
and intervention when minor infusion reactions occur,
and posit a paradigm for maximising safety with this
underutilised therapeutic tool.
Then, in 1989, erythropoiesis-stimulating agents
became available for use in dialysis patients, establishing
a real need for IV iron. Imferon, a high molecular weight
(HMW) iron dextran which is no longer available, was
the predominant product used. In 1991, Imferon was
removed from the market, but at the same time, INFeD,
a low molecular weight (LMW) iron dextran, was
introduced. This was followed by the introduction of other
iron dextrans, such as Dexferrum (another HMW iron
dextran) which was released for clinical use in the USA
only, whereas INFeD, which was branded as Cosmofer,
was also licensed in Europe. In 1999 and 2000, two iron
compounds, ferric gluconate (Ferrlecit) and iron sucrose
(Venofer), already in use in Europe, were approved for
use in the USA. The smaller carbohydrate cores limit the
dose of these agents to no more than 125 mg for ferric
gluconate and 200-400 mg for iron sucrose. While 1,000
mg of LMW INFeD can be administered safely in 1
hour8, three new products which promise to allow safe,
single-setting iron replacement dosing in 15 minutes, have
been approved for clinical use. Two of these (ferumoxytol;
Feraheme in the USA and Rienso in Europe; and ferric
carboxymaltose (Injectafer in the USA and Ferinject in
Europe) are available in both the USA and Europe, and
one, iron isomaltoside-1000 (Monofer) is available in
Europe only (Table I).
iz
i
Introduction
History of intravenous iron use
SI
The first parenteral iron infusions were associated
with severe acute reactions and unsuitable for use.
With the development of iron dextran in 19545, IV iron
could be given more easily, but severe acute reactions
still occurred infrequently. In 1964, the first report
of 37 patients receiving a total dose infusion (single
replacement dose) was published in Blood6, with one
delayed reaction consisting of fever and chills without
hypotension or wheezing. It was, however, another
16 years before the findings of the first prospective
study in 471 patients were published in JAMA 7.
While all patients responded and none died, three
developed signs of anaphylaxis, leading the authors
to conclude that IV iron should be reserved for those
clinical situations in which oral iron could not be used.
Considering the inexpensive and readily available
option of oral iron, it is not surprising that practitioners
had little enthusiasm for IV iron, a treatment modality
associated with shock, and subsequently ignored
the nearly ubiquitous gastrointestinal perturbation
and poor adherence associated with the use of oral
formulations.
Safety issues with intravenous iron
By 1990, the use of IV iron in dialysis centres
had escalated rapidly. Imferon was the formulation
most used. Although serious adverse events occurred
infrequently, the nephrology community rapidly
adopted the addition of IV iron to the treatment
paradigm of dialysis-associated anaemia with observed
improvements in haematological and haematopoietic
responses, levels of energy, activity, quality of life,
cognition, work, sexual function and even decrements
in doses of erythropoiesis-stimulating agents to achieve
similar responses. However, in 1991, a contaminated
lot of Imferon resulted in the recall of the product
worldwide. Serendipitously, at virtually the same time,
INFeD, a LMW iron dextran was approved for use and
rapidly replaced the recalled HMW iron dextran. For
5 years, based on the overwhelming preponderance of
published evidence, and with the anecdotal experience
Blood Transfus 2014; 12: 296-300 DOI 10.2450/2014.0094-14
SIMTI Servizi Srl
296
All rights reserved - For personal use only
No other uses without permission
Safety of intravenous iron
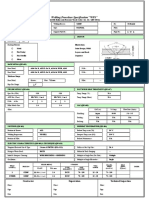
Table I - Intravenous iron preparations.
Currently available intravenous iron preparations
Trade name
INFeD
Ferrlecit
Venofer3
Feraheme4
Monofer5
Injectafer6
Watson
Pharmaceuticals
Inc.
Sanofi Aventis
Inc.
American
Regent Inc.
AMAG
Pharmaceuticals
Pharmacosmos
A/S
American Regent
Inc.
Carbohydrate
Dextran
Polysaccharides
Gluconate
Sucrose
Polyglucose sorbitol
carboxymethylether
Isomaltoside
Carboxymaltose
Molecular weight measured
by manufacturer (Da)
165,000
Low-molecularweight iron
dextran
289,000-444,000
34,000-60,000
750,000
150,000
150,000
Max. approved dosage (mg)
100
125
200
510
20 mg/kg
1,000 mg if patient
weighs >66 kg
TDI possible
Yes
No
No
No
Yes
No
Premedication
TDI only
No
No
No
No
No
Test dose required
Yes
No
No
No
No
No
Iron concentration (mg/mL)
50
12.5
20
30
100
50
Vial volume (mL)
17
1, 5 and 10
in Europe
2 and 10
in Europe
Black box warning
Yes
No
No
No
N/A
N/A
None
Benzyl alcohol
None
None
iz
i
er
v
Preservative
Sr
l
Manufacturer
None
None
SI
TI
S
1 - INFeD prescribing information, Watson Pharma, Inc. Morristown, NJ (USA): http://pi.actavis.com/data_stream.asp?product_
group=1251&p=pi&language=E.
2 - Ferrlecit Prescribing Information. Sanofi Aventis, Inc. Bridgewater, NJ (USA): http://products.sanofi-aventis.us/ferrlecit/ferrlecit.html.
3 - Venofer prescribing information. American Regent, Inc. Shirley, NY (USA): http://www.venofer.com/PDF/Venofer_Insert_
IN2340Rev_10-13.pdf.
4 - Feraheme prescribing information. AMAG Pharmaceuticals, Inc. Waltham, MA (USA): http://www.feraheme.com/downloads/ferahemepi.pdf.
5 - Monofer prescribing information. Pharmacosmos UK Ltd. Thame, Oxfordshire, UK: http://www.monofer.com/media/60600/monofer_
abbreviated_prescribing_information_04-2014.pdf.
6 - Injectafer prescribing information. American Regent, Inc. Shirley, NY (USA): http://www.americanregent.com/documents/
Product94PrescribingInformation.pdf.
N/A: not available; TDI: total-dose infusion. Injectafer is marketed outside the USA under the brand name Ferinject. INFeD is marketed outside the
USA under the brandname CosmoFer.
of nephrologists during that time, the use of IV iron
was associated with extremely few significant adverse
events. Then, in February 1996, another HMW
iron dextran (Dexferrum) was approved as a less
expensive alternative to INFeD. Shortly thereafter,
INFeD was briefly unavailable for administrative
reasons. Using Freedom of Information from the Food
and Drug Administration, reported adverse events
with IV iron increased 11-fold during that period9. In
1998, Case reported that virtually all serious adverse
events with iron dextran were due to Dexferrum and
recommended its avoidance10. Similar conclusions
were published by Mamula et al11. Nonetheless, large
retrospective analyses, without differentiating between
the two dextran formulations, concluded that serious
adverse events were far less common with two other
iron compounds, ferric gluconate and iron sucrose,
and subjects with previous sensitivity to iron dextran
were unlikely to react adversely to either of these two
products12-15. As a result, virtually overnight, the entire
dialysis population was switched from iron dextran to
ferric gluconate or iron sucrose.
Then, in 2004, in a review of the USA Food and Drug
Administration database of spontaneous adverse event
reports, Chertow et al. found no significant differences
in serious adverse events when ferric gluconate and iron
sucrose were compared to LMW iron dextran16. The authors
further concluded that when HMW iron dextran is avoided,
intravenous iron is safe with an estimated serious adverse
event incidence of <1:200,00017. While the Food and Drug
Administration has specifically proscribed the use of this
methodology to compare relative rates of adverse events
among formulations3, these conclusions are corroborated
by the preponderance of published evidence18 with only one
publication extant reporting similar rates of adverse events
between the two iron dextran formulations19.
Blood Transfus 2014; 12: 296-300 DOI 10.2450/2014.0094-14
297
All rights reserved - For personal use only
No other uses without permission
Auerbach M, Macdougall I
Oxidative stress and infection
Sr
l
IV iron has been conjectured to have a number of
other potential adverse consequences. These include
exacerbation of oxidative stress and infections30.31.
Generally, the human body has carefully conserved
mechanisms to sequester iron safely so as to prevent
oxidative injury, utilising proteins such as ferritin and
transferrin. Because IV iron may overwhelm the ability
of these proteins to bind iron, iron may become free in
the circulation or present in excess in tissues, where
iron's oxidative properties can be injurious. Poorly bound
iron can react with hydrogen peroxide (Fenton reaction)
resulting in the generation of hydroxyl radicals. Iron
is converted back to its Fe2+ form by the Haber-Weiss
reaction. In this process, continued substrate for ongoing
iron-catalysed hydroxyl radical production and oxidative
stress is perpetuated. Hydroxyl radicals are highly toxic,
resulting in denaturing of lipids, proteins and DNA31.
Intravenous iron preparations have been shown to induce
oxidative stress and cytotoxicity in vitro, in animals, in
normal human volunteers, and in dialysis patients. In
tissue culture, IV iron causes oxidative stress and cellular
damage in endothelial cells32. A single injection of iron
dextran (500 mg/kg) to five of six nephrectomised rats
resulted in oxidative stress in cardiovascular tissues for
several weeks33. Similarly, dialysis patients experienced
a rapid rise in plasma lipid peroxidation, and DNA and
protein oxidation following the administration of IV
iron34,35. In another study conducted in haemodialysis
patients from Austria, IV iron sucrose administered
during a dialysis session induced a rise in plasma total
peroxide levels, but the magnitude of this increase was
no greater than that in control patients randomised to
receive no IV iron36.
Although these studies do appear to support at
least a transient increase in oxidative stress after IV
iron injection in haemodialysis patients, the quality
of the scientific data is questionable, with inadequate
knowledge of the most meaningful method for
measuring oxidative stress, along with a lack of clarity
on what the results obtained in a laboratory setting mean
for patients administered IV iron.
There are also no prospective data to support the
contention that IV iron exacerbates infections, and
several prospective and observational studies suggest the
opposite37,38. Nevertheless inferential reports continue to
link the use of IV iron and increased infection. Litton et
al. using a meta-analysis, with no predefined endpoint
in the pooled studies, or any dose-response association
iz
i
Management of minor infusion reactions
previous conclusion that it is misinterpretation and
misinformation about the clinical nature and frequency
of minor adverse events which fuel a still present folklore
about the danger of IV iron.
er
v
These conclusions are supported by several
prospective head-to-head comparisons, intra-institutional
retrospective studies and meta-analyses examining
relative rates of adverse events among the available IV
iron products. Two prospective studies with iron sucrose
and LMW iron dextran found no difference20,21. A
meta-analysis corroborated these findings22. In an intrainstitutional retrospective analysis, Okam et al. reported
similar findings with a higher incidence of minor adverse
events being observed with iron sucrose23. Similar
observations were made in trials comparing the newer
formulations ferumoxytol and ferric carboxymaltose to
iron sucrose24,25. There are no comparisons of the newer
formulations with LMW iron dextran. Unfortunately,
a recent study made the ill-considered decision to
prospectively compare ferric carboxymaltose with the
now unavailable HMW iron dextran, Dexferrum, and
concluded that fewer adverse events were observed
with ferric carboxymaltose26. Until a head-to-head
comparison is done with the recommended LMW iron
dextran formulation, no conclusions can or should be
drawn.
SI
TI
S
Two common interventions contribute to the
perception of serious danger with the use of IV
iron. All of the formulations can infrequently cause
minor infusion reactions at the start of the infusion
or test dose (still required with LMW iron dextan
although there is no published evidence to support the
recommendation). These reactions typically consist
of either mild arthralgia/myalgia of the chest or flank
or facial flushing1,27. All of these symptoms routinely
abate without therapy, and plasma tryptase levels
drawn after the reaction are always normal. While
unproven, the symptoms are most likely due to minor
reactions to labile plasma iron released with any of the
formulations. Iron sucrose and ferric gluconate release
the highest amounts of labile plasma iron after an
injection, requiring much lower, more frequent dosing
to administer the desired dose28, LMW iron dextran
next and the three newer agents, ferric carboxymaltose,
ferumoxytol and iron isomaltoside-1000 the least29.
Hypotension is extremely rare. Unnecessary intervention
with pressors or antihistamines can turn these minor
symptoms into haemodynamically significant serious
adverse events. The second intervention is inappropriate
use of diphenhydramine as hypersensitivity prophylaxis
for IV iron. Diphenhydramine can cause somnolence,
diaphoresis, hypotension and tachycardia and in one
prospective study of 285 patients receiving a 500 mg
infusion of LMW iron dextran was responsible for
the majority of perceived adverse events ostensibly
attributed to the IV iron 2. These data support the
Blood Transfus 2014; 12: 296-300 DOI 10.2450/2014.0094-14
298
All rights reserved - For personal use only
No other uses without permission
Safety of intravenous iron
as constipation, metallic taste, gastric cramping and
thick green tenacious stool, the adverse events with IV
iron are minor, infrequent and short-lasting. IV iron is
consequently moving rapidly forward in the treatment
paradigm. As published evidence supports a larger and
earlier role for IV iron and raises the question of whether
it should be frontline therapy in many conditions,
it is more important than ever that inferences and
conclusions on the relative safety of the available IV
iron formulations be based on credible data. Based on all
prospective and intra-institutional retrospective studies,
when HMW iron dextran is avoided the remaining
formulations are safe, and probably much safer than
most physicians realise.
Keywords: intravenous iron, safety, iron deficiency.
Sr
l
Conflict of interests disclosure
iz
i
Michael Auerbach declares no conflict of interest;
Iain Macdougall received consultancy fees, lecture
fees, honoraria, and research grant funding from Vifor
Pharma, Pharmacosmos, AMAG, and Takeda.
References
er
v
with iron and infection risk, or any difference in
mortality rates and other serious adverse events in the
IV iron groups, recently concluded that while IV iron
decreases transfusion rates, it increases infections39. In
contradistinction, Hoen et al. prospectively evaluated
985 dialysis patients receiving IV iron as part of the
treatment paradigm for dialysis-associated anaemia and
found that central venous catheters, arteriovenous grafts,
immunosuppression and a history of infection were
associated with an increased infection rate, while the use
of IV iron, total dose of IV iron and serum ferritin were
not37. Further corroboration can be found in an analysis
of 32,566 haemodialysis patients in whom no adverse
effect on 2-year survival was observed with doses of iron
of up to 1,000 mg over a 6-month period38. Supporting
those conclusions, Brookhart et al. estimated the effects
of various iron dosing patterns on risks of mortality
and infection-related hospital admissions in 776,203
exposure/follow-up pairs40. Consistent with the data
of Hoen et al., while bolus dosing (linked to catheters)
was associated with an increased risk of infection,
maintenance dosing or dose of IV iron compared with
no iron, was not. More recently, Munoz et al. reported
on 2,547 peri-operative patients who underwent elective
lower limb arthroplasty or hip fracture repair, with or
without erythropoiesis-stimulating agents, and observed
not only reduced transfusion rates and shorter time spent
in hospital (p=0.0001), but no difference in infection
rates41. Consistent with these data are the results of a
randomised, controlled trial by Anker et al. in which
patients with heart failure, including 40% with chronic
kidney disease, who received IV iron, had improvements
in quality of life and functional status without an increase
in infections42. In brief, the current literature relating
to IV iron administration and both oxidative stress and
infection risk does not allow firm conclusions to be
drawn.
1)
Conclusions
SI
TI
S
2)
Auerbach M, Ballard H, Glaspy J. Clinical update: intravenous
iron for anaemia. Lancet 2007; 369: 481-3.
Barton J, Barton E, Bertoli L, et al. Intravenous iron dextran
therapy in patients with iron deficiency and normal renal
function who failed to respond to or did not tolerate oral iron
supplementation. Am J Med 2000; 109: 27-32.
Wysoski D, Swartz L, Borders-Hemphill V, et al. Use of
parenteral iron products and serious anaphylactic-type
reaction. Am J Hematol 2010; 86: 650-4.
Auerbach M, Kane R. Caution in making references from
FDA's adverse event reporting system. Am J Health System
Pharmacy, 2012; 11: 922-3.
Baird I, Podmore D. Intramuscular iron therapy in iron
deficiency anaemia. Lancet 1954; 267: 942-6.
Marchasin S, Wallerstein R. The treatment of iron-deficiency
anemia with intravenous iron dextran. Blood 1964; 23: 354-8.
Hamstra R, Block M, Schocket A. Intravenous iron dextran
in clinical medicine. JAMA 1980; 243: 1726-31.
Auerbach M, Pappadakis J, Bahrain H, et al. Safety and
efficacy of rapidly administered (one hour) one gram of low
molecular weight iron dextran (INFeD) for the treatment of
iron deficient anemia. Am J Hematol 2011; 86: 860-2.
Auerbach M, Coyne D, Ballard H. Intravenous iron: from
anathema to standard of care. Am J Hematol 2008; 48: 455-7.
Case G. Maintaining iron balance with total-dose infusion of
intravenous iron dextran. ANNA J 1998; 25: 65-8.
Mamula P, Piccoli D, Peck S, et al. Total dose intravenous
infusion of iron dextran for iron-deficiency anemia in children
with inflammatory bowel disease. J Pediatr Gastroenterol Nutr
2002; 34: 286-90.
Faich G, Strobos J. Sodium ferric gluconate complex in
sucrose: safer intravenous iron therapy than iron dextran. Am
J Kidney Dis 1999; 33: 464-70.
Michael B, Coyne D, Fishbane S, et al. Sodium ferric gluconate
complex in hemodialysis patients: adverse reactions compared
to placebo and iron dextran. Kidney Int 2002; 61: 1830-9.
Coyne D, Adkinson N, Nissenson A, et al. Sodium ferric
gluconate complex in hemodialysis patients. II. Adverse
reactions in iron dextran-sensitive and dextran tolerant
patients. Kidney Int 2003; 63: 217-24.
3)
4)
5)
6)
7)
8)
Several recent prospective studies report the
safety, ease, convenience and efficacy of complete or
near-complete replacement doses of IV iron
administered in a single setting (total dose infusion
over 15-60 minutes)8,43-45. For subjects with disorders
for which oral iron cannot overcome ongoing losses,
such as heavy uterine bleeding, gastrointestinal bleeding,
malabsorption syndromes and gastric bypass surgery,
Osler-Weber-Rendu syndrome (hereditary haemorrhagic
telangiectasia) and other causes of angiodysplasia, or
associated with worsening of the underlying condition,
as in inflammatory bowel disease, a total dose infusion
is a more convenient and less expensive method of
replacing iron. Compared to the side-effects present in
the majority of people taking oral preparations, such
9)
10)
11)
12)
13)
14)
Blood Transfus 2014; 12: 296-300 DOI 10.2450/2014.0094-14
299
All rights reserved - For personal use only
No other uses without permission
Auerbach M, Macdougall I
iz
i
Sr
l
34) Salahudeen A, Oliver B, Bower J, et al. Increase in plasma
esterified F2 isoprostanes following intravenous iron infusion
in patients on hemodialysis. Kidney Int 2001; 60: 1525-31.
35) Tovbin D, Mazor T, Vorobiov M, et al. Induction of protein
oxidation by intravenous iron in hemodialysis patients: role of
inflammation. Am J Kidney Dis 2002; 40: 1005-12.
36) Scheiber-Mojdehkar B, Lutzky B, Schaufler R, et al. Nontransferrin-bound iron in the serum of hemodialysis patients
who receive ferric saccharate: no correlation to peroxide
generation. J Am Soc Nephrol 2004; 15: 1648-55.
37) Hoen B, Paul-Dauphin A, Kessler M. Intravenous iron
administration does not significantly increase the risk of
bacteremia in chronic hemodialysis patients. Clin Nephrol
2002; 57: 457-61.
38) Feldman H, Jaffe M, Robinson B, et al. Administration of
parenteral iron and mortality among hemodialysis patients. J
Am Soc Nephrol 2004; 15: 1623-32.
39) Litton E, Xiao J, Ho KM. Safety and efficacy of intravenous
iron therapy in reducing requirement for allogeneic blood
transfusion: systematic review and meta-analysis of
randomised clinical trials. BMJ 2013; 347: f4822.
40) Brookhart M, Freburger J, Ellis A, et al. Infection risk
with bolus versus maintenance iron supplementation in
hemodialysis patients. J Am Soc Nephrol 2013; 24: 1151-8.
41) Munoz M, Gomez-Ramirez, Cuena J, et al. Very-shortterm perioperative intravenous iron administration and
postoperative outcome in major orthopedic surgery: a pooled
analysis of observational data from 2547 patients. Transfusion
2014; 54: 289-99.
42) Anker SD, Comin Colet J, Filippatos G, et al. Ferric
carboxymaltose in patients with heart failure and iron
deficiency. N Engl J Med 2009; 361: 2436-48.
43) Auerbach M, Strauss W, Auerbach A, et al. Safety and efficacy
of total dose infusion of 1020 mg of ferumoxytol administered
in 15 minutes. Am J Hematol 2013; 88: 944-7.
44) Qunibi W, Martinez C, Smith M, et al. A randomized controlled
trial comparing intravenous ferric carboxymaltose with oral
iron for treatment of iron deficiency of non-dialysis-dependent
chronic kidney disease patients. Nephrol Dial Trans 2011;
26: 1599-607.
45) Onken J, Bregman D, Harrington R, et al. A multicenter,
randomized, active-controlled study to investigate the efficacy
and safety of intravenous ferric carboxymaltose in patients
with iron deficiency anemia. Transfusion 2014; 54: 306-15.
SI
TI
S
er
v
15) Silverberg D, Iaina A, Peer G, et al. Intravenous iron
supplementation for the treatment of the anemia of moderate
to severe chronic renal failure patients not receiving dialysis.
Am J Kidney Dis 1996; 27: 234-8.
16) Chertow G, Mason P, Vaage-Nilsen O, et al. On the relative
safety of parenteral iron formulations. Nephrol Dial Transplant
2004; 19: 1571-5.
17) Chertow G, Mason P, Vaage-Nilsen, et al. Update on adverse
drug events associated with parenteral iron. Nephrol Dial
Transplant 2006; 21: 378-82.
18) Rodgers G, Auerbach M, Cella D, et al. High molecular weight
iron dextran: a wolf in sheep's clothing. J Am Soc Nephrol
2009; 19: 933-4.
19) Walters B, Van Wyck D. Benchmarking iron dextran
sensitivity: reactions requiring resuscitative medication in
incident and prevalent patients. Nephrol Dial Transplant
2005; 7: 1438-42.
20) Sav T, Tokgoz B, Sipahioglu M, et al. Is there a difference
between the allergic potencies of the iron sucrose and low
molecular weight iron dextran? Ren Fail 2007; 29: 423-6.
21) Critchley J, Dunbar Y. Adverse events associated with
intravenous iron infusion (low-molecular weight iron dextran
and iron sucrose): a systematic review Transfus Alternat
Transfus Med 2007; 9: 8-36.
22) Moniem KA, Bhandari S. Tolerability and efficacy of
parenteral iron therapy in hemodialysis patients, a comparison
of preparations. Transfus Alternat Transfus Med 2007; 9:
37-42.
23) Okam M, Mandell E, Hevelone N, et al. Comparative rates
of adverse events with different formulations of intravenous
iron. Am J Hematol 2012; 87: E123.
24) Macdougall IC, Strauss WE, McLaughlin J, et al. A
randomized comparison of ferumoxytol and iron sucrose for
treating iron deficiency anemia in patients with CKD. Clin J
Am Soc Nephrol 2014; 9: 705-12.
25) Bisbe E, Garcia-Erce J, Diez-Lobo A, et al. A multicentre
comparative study on the efficacy of intravenous ferric
carboxymaltose and iron sucrose for correcting preoperative
anaemia in patients undergoing major elective surgery. Br J
Anaesth 2011; 107: 477-8.
26) Hussain I, Bhoyroo J, Butcher A, et al. Direct comparison of
the safety and efficacy of ferric carboxymaltose versus iron
dextran in patients with iron deficiency anemia. Anemia 2013;
2013: 169107.
27) Fishbane S, Ungureanu, Maesake J, et al. The safety of
intravenous iron dextran in hemodialysis patients. Am J
Kidney Dis 1996; 28: 529-34.
28) Chandler G, Harchowal J, Macdougall I. Intravenous iron
sucrose: establishing a safe dose. Am J Kidney Dis 2001;
38: 988-91.
29) Jahn M, Andreasen H, Futterer S, et al. A comparative study
of the physicochemical properties of iron isomaltoside 1000
(Monofer), a new intravenous iron preparation and its
clinical implications. Eur J Pharm Biopharm 2011; 78: 480-91.
30) Fishbane S, Mathew A, Vaziri ND. Iron toxicity relevance for
dialysis patients. Nephrol Dial Transplant 2014; 29: 255-9.
31) Vaziri N. Understanding iron: promoting its safe use in patient
with chronic kidney failure treated by hemodialysis. Am J
Kidney Dis 2013; 61: 992-1000.
32) Kamanna VS, Ganji SH, Shelkovnikov S, et al. Iron sucrose
promotes endothelial injury and dysfunction and monocyte
adhesion/infiltration. Am J Nephrol 2011; 35: 114-9.
33) Lim CS, Vaziri ND. The effects of iron dextran on the oxidative
stress in cardiovascular tissues of rats with chronic renal
failure. Kidney Int 2004; 5: 1802-9.
Arrived: 09 April 2014 - Revision accepted: 03 June 2014
Correspondence: Michael Auerbach
Georgetown University School of Medicine
3900 Reservoir Rd. NW
Washington DC 20007, USA
e-mail: mauerbachmd@abhemonc.com
Blood Transfus 2014; 12: 296-300 DOI 10.2450/2014.0094-14
300
All rights reserved - For personal use only
No other uses without permission
Das könnte Ihnen auch gefallen
- A Handbook of Hajj and UmrahDokument89 SeitenA Handbook of Hajj and UmrahUzaima SiddiquiNoch keine Bewertungen
- Rites of Hajj and Umrah by Sheikh Muhammad Nasiruddin Al-AlbaniDokument23 SeitenRites of Hajj and Umrah by Sheikh Muhammad Nasiruddin Al-AlbaniMuhammad ZameerNoch keine Bewertungen
- Activity Proposal Form: Proposed Date: Proposed TimeDokument2 SeitenActivity Proposal Form: Proposed Date: Proposed Timedrfaruqui2551Noch keine Bewertungen
- Bacillus Clausii As A Treatment of Small Intestinal Bacterial OvergrowthDokument2 SeitenBacillus Clausii As A Treatment of Small Intestinal Bacterial Overgrowthdrfaruqui2551Noch keine Bewertungen
- Efficacy of Bacillus Probiotics in Prevention of Antibiotic-Associated Diarrhoea: A Randomized, Double-Blind, Placebo-Controlled Clinical TrialDokument6 SeitenEfficacy of Bacillus Probiotics in Prevention of Antibiotic-Associated Diarrhoea: A Randomized, Double-Blind, Placebo-Controlled Clinical Trialdrfaruqui2551Noch keine Bewertungen
- Haj SummaryDokument16 SeitenHaj Summarydrfaruqui2551Noch keine Bewertungen
- Female Embryology, Anatomy and HistologyDokument43 SeitenFemale Embryology, Anatomy and Histologydrfaruqui2551Noch keine Bewertungen
- 27 Times Better Topical Versus OralDokument9 Seiten27 Times Better Topical Versus Oraldrfaruqui2551Noch keine Bewertungen
- ADR Form PDF File PDFDokument2 SeitenADR Form PDF File PDFdrfaruqui2551Noch keine Bewertungen
- 5GM BD For IbsDokument8 Seiten5GM BD For Ibsdrfaruqui2551Noch keine Bewertungen
- Dosages For ChildrenDokument1 SeiteDosages For Childrendrfaruqui2551Noch keine Bewertungen
- Aceclofenac A Reappraisal of Its Use in The.12Dokument30 SeitenAceclofenac A Reappraisal of Its Use in The.12drfaruqui2551Noch keine Bewertungen
- Coto StudyDokument8 SeitenCoto Studydrfaruqui2551Noch keine Bewertungen
- Curcumin and Chronic InflammationDokument32 SeitenCurcumin and Chronic Inflammationdrfaruqui2551Noch keine Bewertungen
- Visual-Procedural Memory Consolidation During Sleep Blocked by Glutamatergic Receptor AntagonistsDokument6 SeitenVisual-Procedural Memory Consolidation During Sleep Blocked by Glutamatergic Receptor Antagonistsdrfaruqui2551Noch keine Bewertungen
- Bacterial VaginosisDokument3 SeitenBacterial Vaginosisdrfaruqui2551Noch keine Bewertungen
- What Is DiabetesDokument2 SeitenWhat Is Diabetesdrfaruqui2551Noch keine Bewertungen
- Screening For DiabetesDokument2 SeitenScreening For Diabetesdrfaruqui2551Noch keine Bewertungen
- Antenatal CareDokument4 SeitenAntenatal Caredrfaruqui2551100% (1)
- CPHI2011Dokument2 SeitenCPHI2011drfaruqui2551Noch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Rwamagana s5 Mathematics CoreDokument4 SeitenRwamagana s5 Mathematics Coreevariste.ndungutse1493Noch keine Bewertungen
- Beng (Hons) Telecommunications: Cohort: Btel/10B/Ft & Btel/09/FtDokument9 SeitenBeng (Hons) Telecommunications: Cohort: Btel/10B/Ft & Btel/09/FtMarcelo BaptistaNoch keine Bewertungen
- FM Testbank-Ch18Dokument9 SeitenFM Testbank-Ch18David LarryNoch keine Bewertungen
- Wps For Carbon Steel THK 7.11 GtawDokument1 SeiteWps For Carbon Steel THK 7.11 GtawAli MoosaviNoch keine Bewertungen
- The Impact of Personnel Behaviour in Clean RoomDokument59 SeitenThe Impact of Personnel Behaviour in Clean Roomisrael afolayan mayomiNoch keine Bewertungen
- DLL in Health 7 3rd QuarterDokument2 SeitenDLL in Health 7 3rd QuarterJuna Lyn Hermida ArellonNoch keine Bewertungen
- Note Hand-Soldering eDokument8 SeitenNote Hand-Soldering emicpreampNoch keine Bewertungen
- Retailing PPT (Shailwi Nitish)Dokument14 SeitenRetailing PPT (Shailwi Nitish)vinit PatidarNoch keine Bewertungen
- Papalia Welcome Asl 1 Guidelines 1 1Dokument14 SeitenPapalia Welcome Asl 1 Guidelines 1 1api-403316973Noch keine Bewertungen
- Lugam Annex Elementary School Second Quarter Second Periodical Test in EPP 6 H.EDokument4 SeitenLugam Annex Elementary School Second Quarter Second Periodical Test in EPP 6 H.Ejess amielNoch keine Bewertungen
- Vertical Cutoff WallsDokument18 SeitenVertical Cutoff WallsMark LaiNoch keine Bewertungen
- Assignment & Case Marketing Week 1: Max Van Neerven: 1664172 Mounir Trabelsi: 1705839 Renaldas Zlatkus: 1701775Dokument8 SeitenAssignment & Case Marketing Week 1: Max Van Neerven: 1664172 Mounir Trabelsi: 1705839 Renaldas Zlatkus: 1701775Ren ZkNoch keine Bewertungen
- ProjectDokument22 SeitenProjectSayan MondalNoch keine Bewertungen
- Oral Com Reviewer 1ST QuarterDokument10 SeitenOral Com Reviewer 1ST QuarterRaian PaderesuNoch keine Bewertungen
- Company Registration Procedure Handbook in Cambodia, EnglishDokument124 SeitenCompany Registration Procedure Handbook in Cambodia, EnglishThea100% (16)
- Turnbull CV OnlineDokument7 SeitenTurnbull CV Onlineapi-294951257Noch keine Bewertungen
- University of Southern Philippines Foundation. College of Engineering and ArchitectureDokument7 SeitenUniversity of Southern Philippines Foundation. College of Engineering and ArchitectureJason OwiaNoch keine Bewertungen
- Dash8 200 300 Electrical PDFDokument35 SeitenDash8 200 300 Electrical PDFCarina Ramo LakaNoch keine Bewertungen
- Assesment Test in English 9Dokument3 SeitenAssesment Test in English 9Chazz SatoNoch keine Bewertungen
- Thompson, Damon - Create A Servitor - How To Create A Servitor and Use The Power of Thought FormsDokument49 SeitenThompson, Damon - Create A Servitor - How To Create A Servitor and Use The Power of Thought FormsMike Cedersköld100% (5)
- Alienation Thesis StatementDokument8 SeitenAlienation Thesis Statementafbteepof100% (2)
- WeldingDokument23 SeitenWeldingMathan EverNoch keine Bewertungen
- Bobcat E34 - E35Z Brochure - Adare MachineryDokument8 SeitenBobcat E34 - E35Z Brochure - Adare MachineryNERDZONE TVNoch keine Bewertungen
- Annex A - Scope of WorkDokument4 SeitenAnnex A - Scope of Workمهيب سعيد الشميريNoch keine Bewertungen
- S P99 41000099DisplayVendorListDokument31 SeitenS P99 41000099DisplayVendorListMazen Sanad100% (1)
- Weekly Lesson Plan: Pry 3 (8years) Third Term Week 1Dokument12 SeitenWeekly Lesson Plan: Pry 3 (8years) Third Term Week 1Kunbi Santos-ArinzeNoch keine Bewertungen
- TRAVEL POLICY CARLO URRIZA OLIVAR Standard Insurance Co. Inc - Travel Protect - Print CertificateDokument4 SeitenTRAVEL POLICY CARLO URRIZA OLIVAR Standard Insurance Co. Inc - Travel Protect - Print CertificateCarlo OlivarNoch keine Bewertungen
- Ericsson For Sale From Powerstorm 4SA03071242Dokument8 SeitenEricsson For Sale From Powerstorm 4SA03071242wd3esaNoch keine Bewertungen
- Under Suitable Conditions, Butane, C: © OCR 2022. You May Photocopy ThisDokument13 SeitenUnder Suitable Conditions, Butane, C: © OCR 2022. You May Photocopy ThisMahmud RahmanNoch keine Bewertungen
- Sweat Equity SharesDokument8 SeitenSweat Equity SharesPratik RankaNoch keine Bewertungen