Beruflich Dokumente
Kultur Dokumente
Gynecology AbnormalPubertyandGrowthProblems
Hochgeladen von
Bhi-An BatobalonosOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Gynecology AbnormalPubertyandGrowthProblems
Hochgeladen von
Bhi-An BatobalonosCopyright:
Verfügbare Formate
5 February 2013
ABNORMAL PUBERTY AND GROWTH
PROBLEMS
Ryan B. Capitulo, M.D., FPOGS
I.
II.
III.
Objectives
Pubertal Development
Sexual Maturity Rating
a.
Breasts
b.
Pubic Hair
IV.
Precociuos Puberty
a.
Classification of Precocious Puberty
i. Central
ii. Peripheral
iii. Incomplete
b.
Evaluation Of Precocious Puberty
c.
Management of Precocious Puberty
V.
Primary Amenorrhea
a.
Definition
b.
History
i. Patient History
ii. Family History
c.
Physical Examination
d.
Goals of Management
VI.
Quiz
Note: Dr. Capitulo said that he already made the questions for the
exam and all the questions will be based on the lecture.
OBJECTIVES
To review the following:
o Physiology of normal puberty in girls
o Tanner staging of pubertal changes in girls
o Duration of normal puberty in girls
To
discuss
the
definition,
characteristics,
pathophysiology,
types,
evaluation
and
management of precocious puberty.
To
discuss
the
definition,
characteristics,
pathophysiology,
types,
evaluation
and
management of primary amenorrhea.
PUBERTAL DEVELOPMENT
Thelarche beginning of breast development
10/8 +/- 1.10 years
Adrenarche beginning of pubic of axillary
hair growth
11.0 +/- 1.21 years
Max. growth growth spurt (earlier in
girls)
11.8 +/- 0.88 years
Menarche first menstrual
period
12.9 + 1.2 years
What was the first stage? It is breast budding or breast
development. We call that process as thelarche. In
Filipinos, it occurs at around 10 years old 1 year. So
the earliest is around 8-9 years old. Girls will start to
notice a breast bud, thats the first change. And then a
few months later, hair will develop. You will notice
axillary and pubic hair growth. We call that
adrenarche or pubarche. It occurs just a few months
after thelarche. The third is growth spurt - the period of
maximum growth. This occurs early in girls so
around the age of 12, the girls are taller than the boys.
Boys maximum growth occurs 1-2 years later.
Maximum growth occurs 1 year after breast budding.
Then the last change is menarche. It is the passage of
menstrual blood for the first time. It occurs at around
Cams, er, anj
12 years old 1.2 years. REMEMBER the pubertal
changes in girls: breast hair height mens.
So how do we evaluate teenagers? If you encounter
teenage patients, you have to do your Tanner Staging.
Dont forget that you must indicate Tanner Staging in
your physical examination.
Well review Tanner Staging. Its very easy and I ask
this in the exam so MEMORIZE!
SEXUAL MATURITY RATING
BREASTS
B1 prepubertal (no breast devt or pubic hair)
B2 breast budding
B3 enlargement of breasts with glandular tissue
without
separation of breast contour
B4 secondary mound formed by areola
B5 single contour of breast and areola
Stage 1 is always prepubertal no breast, no pubic
hair. B2 is breast budding. You will feel a marble like
structure underneath the areola. Thats the breast bud.
Thats the first change. You see that at around the age
of 10. When its slightly larger than the breast bud, it is
B3. Thats very important to differentiate it from B4
where there is no separation. Theres only one mound
for the breast. Its as if you have a small breast over
your main breast mass. B5 is the normal adult
configuration of the breast. The breast should be
pointing forward.
PUBIC HAIR
PH1 prepubertal, no pubic hair
PH2 labial hair present
PH3 labial hair spreads over mons pubis
PH4 slight lateral spread
PH5 further lateral spread to form inverse triangle
and reach medial thighs
Page 1 of 6
Stage 1, again, it is prepubertal no hair. PH2,
theres hair in the labia only. If it spreads cephalad,
going to the mons pubis area, thats PH3. If it spreads
laterally, going to the inner thigh, thats PH4. If its the
normal inverted triangle adult configuration of the
pubic hair, then thats PH5. REMEMBER these stages!
NORMAL PUBERTY
B2
10.8 + 1.10 years
PH2
11.0 + 1.21 years
Menarche
12.9 + 1.2 years
B2 to peak height velocity
1.0
+ 0.77
years
B2 to PH5
3.1 + 1.04 years
B2 to menarche
2.1 + 1.03 years
B2 to B5
4.5 + 2.04 years
I WONT be asking these. These are the normal age
among Filipinas. We expect these changes to occur.
Whats important here is the B2 to B5 breast
budding to the development of the normal adult
breast. This is the entire duration of puberty. So when
you have your normal configuration of the breast
already, then it means puberty is over. You are now an
adult. It occurs 4.5 2 years. Thats the entire
duration of puberty.
PRECOCIOUS PUBERTY
Appearance of any signs of secondary sexual
maturation at an early specific age more than 2.5
standard deviations below the mean
Initiation of secondary sexual characteristics before
age 8 or menarche before age 9 (The secondary
sexual characteristics are breast development,
pubic hair growth, maximum growth and
menarche.)
Associated with a wide range of disorders
A very rare disease (1 in 10,000 girls)
Concerns with precocious puberty
o Social stigma of child being physically
different from her peers
o Diminished ultimate height
Shorter than normal adult height due to
o Limited duration of the rapid growth spurt
(The period of maximum growth is limited
when you have precocious puberty. The
shorter the time for the maximum growth,
the shorter your height will be.)
o Accelerated bone maturation
o Premature closure of the distal epiphyseal
growth centers
Cams, er, anj
GnRH is the hormone responsible for the initiation of
pubertal
changes.
GnRH
comes
from
the
hypothalamus. At a certain time in a childs
development, the hypothalamus will start producing
and releasing in a pulsatile manner your GnRH. GnRH
will act on the pituitary gland. It stimulates the release
of gonadotropins (FSH and LH). FSH will stimulate the
follicles in the ovary. It will stimulate the granulosa
cells to secrete estrogen. Then estrogen will initiate
the pubertal changes. It will cause breast enlargement
or development. When estrogen is converted to
androgen in the peripheral tissues, it will cause pubic
hair growth and axillary hair growth. Estrogen is
involved in a lot of things, even in bone growth.
Skeletal growth is initiated by estrogen thats why you
have a period of maximum growth. When estrogen
acts on the uterus, thats the time you will experience
menarche. Thats the normal pubertal changes.
Again, GnRH will act on the pituitary and then the
gonadotropins will act on the ovary. So its a
hypothalamic-pituitary-ovarian axis with feedback
mechanisms.
edited: Sarah
CLASSIFICATION OF PRECOCIOUS PUBERTY
Central Precocious Puberty
Peripheral Precocious Puberty
Incomplete Precocious Puberty
CENTRAL PRECOCIOUS PUBERTY
GnRH-dependent precocious puberty
There is something wrong with the hypothalamus
because it secreted GnRH early. It should secrete it
around the age of 10. In patients with central
precocious puberty, it starts making GnRH at an
early age.
Physiologically normal pubertal development that
is chronologically early
Results
from
hypothalamic
GnRH-stimulated
episodic gonadotrophin secretion
GnRH, LH, FSH, sex steroid levels are similar to
those in normal puberty
Idiopathic in 70% of cases
CNS dysfunction in 30 % of cases
o Congenital defects (septooptic dysplasia)
o Destruction
from
tumors
(craniopharyngioma)
o Destruction from other lesions (arachnoid
cysts)
o Excessive exposure to sex steroids
(McCune Albright)
o Excessive pressure (hydrocephalus)
o Infection or inflammation (brain abscess,
meningitis)
o Injury (head trauma, irradiation)
o GnRH secreting tumors (hypothalamic
hamartomas)
PERIPHERAL PRECOCIOUS PUBERTY
GnRH-independent
precocious
puberty
or
pseudoprecocious puberty
Pubertal development resulting from stimulation
with a hormone other than hypothalamic GnRH
Page 2 of 6
May or may not follow the chronology of normal
pubertal development
Caused by estrogen secreting ovarian tumor in
60% of cases
o Granulosa cell tumor
o Mixed germ cell tumor
o Cystadenomas
o Gonadoblastoma
If that tumor is secreting estrogen only, then you can
have breast development (because its estrogenmediated) but sometimes these patients will not
present with pubarche or adrenarche. But these
patients can have maximum growth and menarche.
Whereas if the tumor is secreting testosterone for
example, you can have a sertoli leydig cell tumor in
the ovary that secretes androgen only. The child will
present with adrenarche only. No breast development
and maximum growth.
I have a patient, she presented with breast
development and menstruation. We worked her up and
we were looking for the cause. All the tests were
normal until the mother discovered that the child was
taking her OCP. The child taught it was candy so she
took it. She was taking 1-2 tablets a day for about a
month. In that span of time, she developed breast
developed budding and she had menarche. She was
just 3 years old! She was taking exogenous estrogen
it is also called peripheral precocious puberty.
Exogenous sex steroids or gonadotrophin
Chronic primary hypothyroidism
Feminizing adrenal tumors
INCOMPLETE PRECOCIOUS PUBERTY
Incomplete meaning she has only one pubertal
change.
Premature Thelarche
o Isolated unilateral
or bilateral breast
development
o Not accompanied by other signs of pubertal
development
o Usually occurs at age 1 to 4 years
o Benign self-limiting condition that does not
require treatment
The patient will just come to you with breast
enlargement. No axillary or pubic hair growth. No
increased in height. No menarche. This usually occurs
at the age of 1-4. It is benign self-limiting condition
that does not require any treatment, so you only have
to reassure the mother. Thats if you are sure that its
just premature thelarche. So when you encounter this
patient, you should follow her up for a couple of
months to see that she wont develop the other
changes.
Premature Pubarche or Adrenarche
o Early isolated development of pubic or
axillary hair without other signs of secondary
sexual maturation
o Self-limited but must be followed up carefully
The patient will come to you with pubic hair growth
and axillary hair growth but no breast development, no
increase in height and no menarche. It also self limited
Cams, er, anj
but we have to still have to follow up and eventually
reassure the parents that it will go away by itself.
Recap: Central precocious puberty is GnRH mediated,
so the patient will go through all the changes of
puberty. In peripheral precocious puberty it is no
caused by GnRH, it is caused by an individual hormone
responsible for puberty, so if the patient has a tumor
secreting estrogen, you will only expect changes due
to estrogen, if she has a tumor secreting androgen,
you will only expect changes due to androgen etc. So if
the patient has Incomplete precocious puberty then
she can only have premature thelarche or pubarche.
EVALUATION OF PRECOCIOUS PUBERTY
Meticulous history and PE
o Height
o Tanner stage
o Neurologic exam
When the patient comes to you, it is highly emphasize
that you do a very meticulous PE. Get the patients
height and compare it with her age group and then do
a tanner staging and neurologic exam because 30% of
the time, the patient would have neurologic problem if
she have central precocious puberty.
Serum estradiol, FSH, LH, androgens and thyroid
function tests
Thyroid function test is requested because sometimes,
patient with thyroid problems also presents with
central precocious puberty problem.
Bone age (hand-wrist films) repeated every 6
months
Bone aging is very important. This is done by
radiologist using hand-wrist films. They compare the
hand-wrist film of the patient with that of the film of
the same age group, and they will be able to say the
exact bone age of the patient. So if a patient comes to
you, she is age 4 but her hand-wrist film will show that
she is 7 years old then that patient has central
precocious puberty.
Imaging studies like ultrasound, skull x-ray, cranial
CT scan and MRI
Done to check for masses or tumors. Cranial CT and
MRI to rule out any CNS dysfunction that is usually
present 30% of the time.
MANAGEMENT OF PRECOCIOUS PUBERTY
Depends on the cause, extent and progression of
precocious signs
For PPP: remove the source of the hormone
o Ovarian tumor/adrenal tumor causing the
precocious puberty surgericaly removal
o Taking exogenous estrogen- stop taking it
o Incomplete precocious puberty- observe
since it is self limiting
For CPP: treat the patient if with
o PROGRESSIVE thelarche and pubarche and
menarche
o Bone age >2 years for age
Risk for having short stature
Goals of treatment of CPP:
o Reduce GnRH secretion by the hypothalamus
and peripheral actions of sex steroids.
We want to reduce and stop it! Because we know that
the menarche stage should happened around the age
edited: Sarah
Page 3 of 6
of 10! Not 3 years old! So we have to keep treating the
patient until she reach the proper age.
o Decrease growth rate to normal
o Slow
skeletal
maturation
to
allow
development of maximal adult height
GnRH analogues drug of choice
You might wonder why we are treating CPP with a
GnRH analogue instead of an antagonist. The reason
for this is because this analogue saturates the
receptors in the pituitary gland until the GnRH
produced by the hypothalamus will not be able to act
on the pituitary gland.
o Most effective in 4 to 6 year olds
o Decreases gonadotrophin and sex steroids to
prepubertal levels
o Causes regression of precocious signs
o Continue treatment until progress of puberty is
age- appropriate and consistent with emotional
maturity, current height and height potential
so if you have a patient with CPP at the age of4
years old, then you should treat the patient for
6 years until she reaches the proper age.
According to Sir, he had a patient who had a CPP but
refused treatment because the treatment is really
expensive and requires monthly injections of about
16K. Also, for the mother of the patient, the
consequence of having a short statue is not much of a
consequence.
Pubertal History
PHYSICAL EXAMINATION
Anthropometric Measurements
BMI
Dysmorphic Features congenital anomalies
Rudimentary or Absent Uterus
Pubic Hair Pattern
Striae, buffalo hump, central obesity, etc.
Tanner Staging
Thyroid Examination
Vaginal Septum or Imperforate Hymen
Signs of Virilization
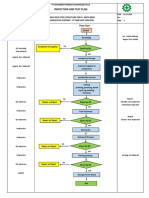
EVALUATION
History and P.E. completed
Secondary Sexual Characteristics Present?
NO
Measure FSH and LH
PRIMARY AMENORRHEA
`DEFINITION
(+) secondary sexual characteristics and
(-) menarche by age 16.5 years (16 years and 6
months)
OR
(-) secondary sexual characteristics and
(-) menarche by age 14
Low
FSH & LH
Delay puberty or primary amenorrhea. The patient has
secondary sexual characteristics BUT no Menarche at
the age of 16.5 years then we diagnose her as having
primary amenorrhea or if the patient has NO
secondary sexual characteristics and menarch at the
age of 14.
Cams, er, anj
High
FSH & LH
Ultrasound of Uterus
Uterus (-)
or
abnormal
Uterus (+)
or
normal
NO SECONDARY SEXUAL CHARACTERISRICS
Measure FSH and LH
HISTORY
PATIENT HISTORY
Menstrual History
Illness, Drug Use
CNS Chemotherapy or Radiation (Brain
radiation will cause ischemia of pituitary
gland)
Pelvic Radiation
Psychosocial Stressors
Sexual Activity (Consider pregnancy)
Breast Changes
Anosmia
Abdominal Pain
Vasomotor Symptoms
FAMILY HISTORY
Genetic Defects
Pubic Hair Pattern
Infertility
Menarche and Menstrual History of Mother and
Sisters
YES
Low
FSH & LH
Hypogonadotropic
Hypogonadism
Hypothalamic
Failure
Pituitary Failure
High
FSH & LH
Hypergonadotropic
Hypogonadism
KARYOTYPE
POF
(46,XX)
Turners
Syndrome (45,XO)
If the patient comes to you with NO secondary sexual
characteristics, we measure for FSH and LH, if it is low,
we call it hypogonadotropic hypogonadism
meaning the pituitary gland or the hypothalamus is
NOT functioning. And because of this, there is no
stimulation of the ovaries, hence no production of
edited: Sarah
Page 4 of 6
estrogen, and therefore absence of secondary sexual
characteristics.
If the FSH and LH are high (hypergonadotropic),
meaning the pituitary gland and the hypothalamus are
fine or are working perfectly. The reason however for
their absence of secondary sexual characteristics
(hypogonadism) is because the ovaries are not
functioning. If we have a patient with this condition,
we request for karyotyping, if the results showed that
the patient have normal karyotype, then we conclude
that the patient have POF or premature ovarian
failure, meaning that the ovaries just died at such a
young age. The other reason however, for having
hypergonadotropic hypgonadism could be that the
patient have turners syndrome, and patients with
turners syndrome have NO gonads
The other concept that we have to remember in the
hypergonadotropic hypogonadism, is the concept of
feedback mechanism. Normally, the ovaries should
produce inhibin in the event that the there is already
enough FSH and LH, but since there are no ovaries or
gonads in POF and Turners syndrome, then there
would be no production of estrogen and no production
of inhibin, hence the hyperogonadotropism.
WITH SECONDARY SEXUAL CHARACTERISTICS
If however the karyotype of the patient with no uterus,
showed that the patient is really a male (46 XY), the
patient therefore as androgen insensitivity syndrome.
AIS (androgen insensitivity syndrome)- also
known as testicular feminization syndrome; no
receptor for androgens; therefore even if they have
capability of producing androgen, there body will not
be able to read the androgens, hence the body will
not be capable of producing male characteristics. Also,
remember that all embryos are destined to become
females unless there is androgen. They are
phenotypically female.
If there is a uterus, we inspect for outflow
obstruction, the patient might have imperforate
hypemen or septum.
The hymen usually perforates just before the female
child is born. Sometimes, it doesnt perforate.
Abdominal pain every month since the patient is really
menstruating is just that the the blood is accumulated
inside, until there would be uterine enlargement.
Tx- hymenectomy. Remove a portion of the
hymen and then all the menstrual blood that
accumulated will go out.
Or the patient have transverse vaginal septum
Ultrasound of Uterus
Transverse vaginal septum- during development,
the vaginal canal should canalize. Just remove the
septum for the menstrual blood to come out.
Note: Jamie Lee Curtis actress with AIS
Uterus (-)
or
abnormal
Uterus (+)
or
normal
OUTFLOW
OBSTRUCTION?
KARYOTYPE
Mullerian
Agenesis
(46,XX)
AIS
(46,XY)
NO
Others
YES
Imperforate
Hymen or
septum
Now, in patients with primary amenorrhea BUT with
secondary sexual characteristics, we request for
ultrasound thinking that there might be NO uterus.
If on ultrasound and on PE, the patient has NO uterus,
we request again for karyotype. If the karyotype,
showed that the patient is really a female (46, XX) then
the patient must have Mullerian Agenesis.
Mullerian agenesis- mullerian ducts, which are the
precursor for fallopian tubes and uterus, disintegrated
during intrauterine development. She has no uterus,
fallopian tubes, and upper 2/3 vagina. She however,
still has ovaries (reason for having secondary sexual
characteristics) because in embryology, the origin of
ovaries is not from the mullerian ducts. This is also
known as MRKH (Mayer-Rokitansky-Kuster-Hauser
syndrome).
Cams, er, anj
GOALS OF MANAGEMENT
Progression of normal pubertal development
Preservation of fertility if possible
Prevention of complications of hypoestrogenic
state
Estrogen is involved in bone and lipid metabolism.
Upon menopause, the bones will start to soften leading
to osteoporosis. Since estrogen is involved in lipid
metabolism, they may have dyslipidemia
NO SECONDARY SEXUAL CHARACTERISTICS
Progression of normal pubertal development HRT
(pills contain estrogen and some progesterone);
she may menstruate.
Preservation of fertility HMG or pulsatile GnRH
(to stimulate FSH and LH secretion)
Prevention of complications of hypoestrogenic
state HRT, calcium, vitamin D
Remove gonads if with Y chromosome-AIS
(HRT = Hormone Replacement Therapy)
(HMG= Human Menopausal Gonadotropin)
Sidenote: women with our age should already start
taking calcium, except for women on the heavy side,
since women on the heavy side actually developed
stronger bones. In fact, women who are thin their
entire life, are most at risk for having osteoporosis.
edited: Sarah
ANDROGEN INSENSITIVITY SYNDROME
Page 5 of 6
Progression of normal pubertal development
remove gonads after full breast development and
epiphyseal closure or after puberty, then give
them HRT
Preservation of fertility- indefinitely, they cant get
pregnant, they have no mullerian ducts in the first
place
Prevention of complications of hypoestrogenic
state estrogen replacement therapy
MULLERIAN AGENESIS
Progression of normal pubertal development
Prevention of complications of hypoestrogenic
state
Surgical reconstruction of absent vagina
Note: these patients will never get pregnant. However,
since they have no vaginal canal, we can surgically
reconstruct so that they can have a vaginal canal so
that when they get married they can make talik
OUTFLOW TRACT OBSTRUCTION
Hymenectomy
Resection of Vaginal Septum
End
QUIZ
1) Proper order of Pubertal Development?
2) Tanner stage: Enlargement of breasts with
glandular tissue without separation of breast
contour?
3) Tanner stage: Pubic hair over mons pubis?
4) Precocious puberty is initiation of secondary
sexual characteristic before age 8 and
menarche before age ___?
5) Most common ovarian neoplasm is ____?
Answers:
1) Thelarche Adrenarche Max Growth Menarche
2) B3
3) PH3
4) 9
5) Granulosa cell tumor
Cams, er, anj
edited: Sarah
Page 6 of 6
Das könnte Ihnen auch gefallen
- Clinical AnestesiaDokument432 SeitenClinical AnestesiaAde Putra100% (1)
- Medical Response to Child Sexual Abuse: A Resource for Professionals Working with Children and FamiliesVon EverandMedical Response to Child Sexual Abuse: A Resource for Professionals Working with Children and FamiliesNoch keine Bewertungen
- Paediatric & Adolescent GynaecologyDokument78 SeitenPaediatric & Adolescent GynaecologyMichelle FynesNoch keine Bewertungen
- Kuan Yin 100 Divine Lots InterpretationDokument30 SeitenKuan Yin 100 Divine Lots InterpretationEsperanza Theiss100% (2)
- Spleen/Liver Trauma DiagnosisDokument34 SeitenSpleen/Liver Trauma DiagnosissanjayNoch keine Bewertungen
- Medad Andrology Special Note NMT13 PDFDokument70 SeitenMedad Andrology Special Note NMT13 PDFSelim TarekNoch keine Bewertungen
- The Reproductive SystemDokument266 SeitenThe Reproductive SystemNatia DemetradzeNoch keine Bewertungen
- 2014 Pediatric & Adolescent GynecologyDokument77 Seiten2014 Pediatric & Adolescent GynecologyJai CarungayNoch keine Bewertungen
- Pediatric Gynecology Care & ExamsDokument70 SeitenPediatric Gynecology Care & ExamsBianca Denise FranciscoNoch keine Bewertungen
- El Bill PDFDokument2 SeitenEl Bill PDFvinodNoch keine Bewertungen
- Pap Smear Guidelines: Baylor College of Medicine Anoop Agrawal, M.DDokument22 SeitenPap Smear Guidelines: Baylor College of Medicine Anoop Agrawal, M.Dshygirl72Noch keine Bewertungen
- Hormonal ContraceptivesDokument25 SeitenHormonal Contraceptivesmd easarur rahmanNoch keine Bewertungen
- Infertility IDokument36 SeitenInfertility Idr_asaleh100% (1)
- Complications of Spinal and Epidural AnesthesiaDokument45 SeitenComplications of Spinal and Epidural AnesthesiashikhaNoch keine Bewertungen
- S6MT 1Q w1 3 MELC1 SLM MIXTURES FinalCopy09082020Dokument26 SeitenS6MT 1Q w1 3 MELC1 SLM MIXTURES FinalCopy09082020Rona Dindang100% (1)
- Genital Anatomy in Non-Abused Preschool GirlsDokument10 SeitenGenital Anatomy in Non-Abused Preschool Girlsวินจนเซ ชินกิNoch keine Bewertungen
- Peugeot 206 Fuse Diagram PDFDokument6 SeitenPeugeot 206 Fuse Diagram PDFDedi dwi susanto100% (2)
- And Tab 1Dokument4 SeitenAnd Tab 1Bella SuratmonoNoch keine Bewertungen
- Physical Exam in Adolescent GynecologyDokument13 SeitenPhysical Exam in Adolescent GynecologyEric FatrinNoch keine Bewertungen
- Idiopathic Central Precocious Puberty A Case ReportDokument8 SeitenIdiopathic Central Precocious Puberty A Case ReportCarolyn CapisnonNoch keine Bewertungen
- Intermediate-Level Adolescent and Adult Sexual Assault Assessment: SANE/SAFE Forensic Learning SeriesVon EverandIntermediate-Level Adolescent and Adult Sexual Assault Assessment: SANE/SAFE Forensic Learning SeriesNoch keine Bewertungen
- Treatment and Outcomes of Precocious Puberty: An UpdateDokument11 SeitenTreatment and Outcomes of Precocious Puberty: An UpdateAbdurrahman Hasanuddin100% (1)
- Kegel Handout PDFDokument1 SeiteKegel Handout PDFMini ManojNoch keine Bewertungen
- Physical Findings in Child Sexual AbuseDokument14 SeitenPhysical Findings in Child Sexual AbusemeganitaNoch keine Bewertungen
- Identification and Management of Ambiguous GenitaliaDokument31 SeitenIdentification and Management of Ambiguous Genitaliateslimolakunleraji100% (1)
- Tall StatureDokument24 SeitenTall StaturedianmutiaNoch keine Bewertungen
- Medicolegal Issues in Obstetrics and Gynaecology: Swati Jha Emma FerrimanDokument374 SeitenMedicolegal Issues in Obstetrics and Gynaecology: Swati Jha Emma Ferrimankhalid balshaNoch keine Bewertungen
- Levin2004 Sexual Arousal PDFDokument7 SeitenLevin2004 Sexual Arousal PDFHenriqueSimãoNoch keine Bewertungen
- MCQ AnsDokument65 SeitenMCQ AnsFatima Hasnain100% (7)
- Growth & Development of An Adolescent (2380)Dokument8 SeitenGrowth & Development of An Adolescent (2380)ta CNoch keine Bewertungen
- Uterine FibroidsDokument21 SeitenUterine FibroidsPrasun BiswasNoch keine Bewertungen
- Puberty: Normal Development and Causes of Precocious PubertyDokument8 SeitenPuberty: Normal Development and Causes of Precocious Pubertyclear mindNoch keine Bewertungen
- The Use of Aromatase Inhibitors in Infertility and GynecologyDokument9 SeitenThe Use of Aromatase Inhibitors in Infertility and Gynecologyalan lowusNoch keine Bewertungen
- Puberty Normal and AbnormalDokument41 SeitenPuberty Normal and AbnormalTonyScariaNoch keine Bewertungen
- Movie Ethics ReviewDokument4 SeitenMovie Ethics ReviewpearlydawnNoch keine Bewertungen
- Physiology and PubertyDokument8 SeitenPhysiology and PubertynofiajahNoch keine Bewertungen
- Inspection and Test Plan: Flow Chart Start IncomingDokument1 SeiteInspection and Test Plan: Flow Chart Start IncomingSinden AyuNoch keine Bewertungen
- Reproductive EndocrinologyDokument18 SeitenReproductive EndocrinologyAnonymous hkWIKjoXFVNoch keine Bewertungen
- Anatomy and PhysiologyDokument8 SeitenAnatomy and PhysiologyAironne ManguilimotanNoch keine Bewertungen
- Diploma Pharmacy First Year - Hap - MCQSDokument13 SeitenDiploma Pharmacy First Year - Hap - MCQSAnitha Mary Dambale91% (33)
- Male InfertilityDokument57 SeitenMale InfertilityUsha AnengaNoch keine Bewertungen
- Conder Separator Brochure NewDokument8 SeitenConder Separator Brochure Newednavilod100% (1)
- Primary and Secondary AmenorrhoeaDokument72 SeitenPrimary and Secondary Amenorrhoead clarkeNoch keine Bewertungen
- Taking History and Physical Examination in YouthDokument99 SeitenTaking History and Physical Examination in Youthlinda ratna watiNoch keine Bewertungen
- Abnormal Development of Female Genital TractDokument69 SeitenAbnormal Development of Female Genital TractJerry CreedNoch keine Bewertungen
- Medical Findings and Child Sexual AbuseDokument26 SeitenMedical Findings and Child Sexual AbuseEdgar Aleman CruzNoch keine Bewertungen
- Genital examination findings - Understanding what is normalDokument36 SeitenGenital examination findings - Understanding what is normalMuhammad AuliaNoch keine Bewertungen
- Sexual Precocity PDFDokument5 SeitenSexual Precocity PDFmist73Noch keine Bewertungen
- 05 Skin AssessmentDokument31 Seiten05 Skin AssessmentHerlinaNababanNoch keine Bewertungen
- Precocious PubertyDokument30 SeitenPrecocious PubertyNeha SharmaNoch keine Bewertungen
- Precociou S Puberty: BY Vishnupriya Ravimohandoss Year-6 Group-1Dokument31 SeitenPrecociou S Puberty: BY Vishnupriya Ravimohandoss Year-6 Group-1Priya RaviNoch keine Bewertungen
- Precocious VS Early Puberty, SiskaDokument21 SeitenPrecocious VS Early Puberty, SiskapuspaNoch keine Bewertungen
- Congenital Anomelies of Reproductive OrgansDokument47 SeitenCongenital Anomelies of Reproductive Organsdr_shamimrNoch keine Bewertungen
- Management of Foreskin ConditionsDokument26 SeitenManagement of Foreskin ConditionsSarif CassanovaNoch keine Bewertungen
- Hypospadias Surgery: An Illustrated GuideVon EverandHypospadias Surgery: An Illustrated GuideAhmed HadidiBewertung: 5 von 5 Sternen5/5 (1)
- Kuliah Penis & ScrotumDokument13 SeitenKuliah Penis & ScrotumEmallia Phypiet FitrianiNoch keine Bewertungen
- Circumcision Using The Mogen ClampDokument4 SeitenCircumcision Using The Mogen ClampJorge AndrésNoch keine Bewertungen
- Anatomi PenisDokument1 SeiteAnatomi Penischouko catNoch keine Bewertungen
- Proper Circumcision Techniques for Infants and AdultsDokument6 SeitenProper Circumcision Techniques for Infants and Adultsntambik21Noch keine Bewertungen
- Congenital Malformations of The Female Genital TractDokument7 SeitenCongenital Malformations of The Female Genital TractDo le QuangNoch keine Bewertungen
- PenisDokument23 SeitenPenisWira DharmaNoch keine Bewertungen
- Fertilisasi Askeb IDokument19 SeitenFertilisasi Askeb IPutry Utami0% (1)
- Kipp Mandatory Penis InspectionDokument1 SeiteKipp Mandatory Penis InspectionJeff barkerNoch keine Bewertungen
- Male and Female Infertility GuideDokument35 SeitenMale and Female Infertility GuideJalajarani AridassNoch keine Bewertungen
- Sign of Hyperandrogenism PDFDokument6 SeitenSign of Hyperandrogenism PDFmisbah_mdNoch keine Bewertungen
- StratOG Vaginal BreechDokument17 SeitenStratOG Vaginal BreechNalin AbeysingheNoch keine Bewertungen
- Malereproductive (Author T.globa)Dokument40 SeitenMalereproductive (Author T.globa)Cristina caimac100% (1)
- 3 - Precocious PubertyDokument9 Seiten3 - Precocious PubertyJohnM.GiraldoNoch keine Bewertungen
- I-3 Pediatric and Adolescent GynecologyDokument8 SeitenI-3 Pediatric and Adolescent GynecologyuvioscribdNoch keine Bewertungen
- Female Reproductive SystemDokument6 SeitenFemale Reproductive SystemAlyanna L. ArquillanoNoch keine Bewertungen
- WP GynaeExams4Dokument37 SeitenWP GynaeExams4Ahsan JamNoch keine Bewertungen
- Pre-Operative Conference Anesthetic Considerations For Laryngectomy and Total Thyroidectomy in GeriatricsDokument4 SeitenPre-Operative Conference Anesthetic Considerations For Laryngectomy and Total Thyroidectomy in GeriatricsBhi-An BatobalonosNoch keine Bewertungen
- Morbidity and MortalityDokument2 SeitenMorbidity and MortalityBhi-An BatobalonosNoch keine Bewertungen
- Pedia Census: Ruby Anne D. BatobalonosDokument57 SeitenPedia Census: Ruby Anne D. BatobalonosBhi-An BatobalonosNoch keine Bewertungen
- CP# CP Eval: Covid RT-PCR: CCDokument2 SeitenCP# CP Eval: Covid RT-PCR: CCBhi-An BatobalonosNoch keine Bewertungen
- Preop Conference AnesthesiaDokument33 SeitenPreop Conference AnesthesiaBhi-An BatobalonosNoch keine Bewertungen
- Clinical Clerks Report Case PresDokument8 SeitenClinical Clerks Report Case PresBhi-An BatobalonosNoch keine Bewertungen
- Respiratory Function in Anesthesia: Ruby Anne D. Batobalonos, M.D Anesthesia Pre ResidentDokument17 SeitenRespiratory Function in Anesthesia: Ruby Anne D. Batobalonos, M.D Anesthesia Pre ResidentBhi-An BatobalonosNoch keine Bewertungen
- Protocol LaryngectomyDokument3 SeitenProtocol LaryngectomyBhi-An BatobalonosNoch keine Bewertungen
- Application in ResDokument1 SeiteApplication in ResBhi-An BatobalonosNoch keine Bewertungen
- Organ Dysfunction in SepsisDokument20 SeitenOrgan Dysfunction in SepsisBhi-An BatobalonosNoch keine Bewertungen
- Anesthetic Implications of Guillain-Barre Syndrome in PregnancyDokument34 SeitenAnesthetic Implications of Guillain-Barre Syndrome in PregnancyBhi-An BatobalonosNoch keine Bewertungen
- Pedia Census 5Dokument62 SeitenPedia Census 5Bhi-An BatobalonosNoch keine Bewertungen
- Screenshot 2022-01-24 at 11.15.59 AMDokument1 SeiteScreenshot 2022-01-24 at 11.15.59 AMBhi-An BatobalonosNoch keine Bewertungen
- Pedia Census ArrythmiaDokument48 SeitenPedia Census ArrythmiaBhi-An BatobalonosNoch keine Bewertungen
- NORA Case 2Dokument3 SeitenNORA Case 2Bhi-An BatobalonosNoch keine Bewertungen
- Case Management Conference: Department of Anesthesiology April 19, 2021Dokument8 SeitenCase Management Conference: Department of Anesthesiology April 19, 2021Bhi-An BatobalonosNoch keine Bewertungen
- SynchronousDokument4 SeitenSynchronousBhi-An BatobalonosNoch keine Bewertungen
- Basic ReportDokument1 SeiteBasic ReportBhi-An BatobalonosNoch keine Bewertungen
- Blunt Trauma Abdomen: (Operative V/S Conservative Management)Dokument41 SeitenBlunt Trauma Abdomen: (Operative V/S Conservative Management)Bhi-An BatobalonosNoch keine Bewertungen
- Interesting Case Report Hepatectomy DR B Perez2Dokument10 SeitenInteresting Case Report Hepatectomy DR B Perez2Bhi-An BatobalonosNoch keine Bewertungen
- Anesthetic Management of Non-Fasted Patients Requiring Emergency SurgeryDokument17 SeitenAnesthetic Management of Non-Fasted Patients Requiring Emergency SurgeryBhi-An BatobalonosNoch keine Bewertungen
- Regional Anesthesia - FinalDokument46 SeitenRegional Anesthesia - Finalvan016_bunnyNoch keine Bewertungen
- Guidelines For The Management of AsymptomaticDokument9 SeitenGuidelines For The Management of AsymptomaticBhi-An BatobalonosNoch keine Bewertungen
- Pediatric AnesthDokument213 SeitenPediatric AnesthJyoti Agarwal BhallaNoch keine Bewertungen
- Census - High SpinalDokument30 SeitenCensus - High SpinalBhi-An BatobalonosNoch keine Bewertungen
- Wide Excision With Frozen Section of Malignant Neoplasm Righ Flank July 1Dokument2 SeitenWide Excision With Frozen Section of Malignant Neoplasm Righ Flank July 1Bhi-An BatobalonosNoch keine Bewertungen
- Carbon Cycle Game Worksheet - EportfolioDokument2 SeitenCarbon Cycle Game Worksheet - Eportfolioapi-264746220Noch keine Bewertungen
- TSB 20230831 - Reconnect FATL WM Error Code & Troubleshooting GuideDokument6 SeitenTSB 20230831 - Reconnect FATL WM Error Code & Troubleshooting GuideNavjot KaurNoch keine Bewertungen
- T1D Report September 2023Dokument212 SeitenT1D Report September 2023Andrei BombardieruNoch keine Bewertungen
- Rise School of Accountancy Test 08Dokument5 SeitenRise School of Accountancy Test 08iamneonkingNoch keine Bewertungen
- AnxietyDokument5 SeitenAnxietydrmadankumarbnysNoch keine Bewertungen
- Morningstar Bakery: Business PlanDokument14 SeitenMorningstar Bakery: Business PlanbakhtawarNoch keine Bewertungen
- Bibie Evana OsmanDokument6 SeitenBibie Evana OsmanStabat Jaya TrademarkNoch keine Bewertungen
- Grade 9 P.EDokument16 SeitenGrade 9 P.EBrige SimeonNoch keine Bewertungen
- Vacuum Conveyin 5.0Dokument56 SeitenVacuum Conveyin 5.0Mostafa AtwaNoch keine Bewertungen
- Density of Aggregates: ObjectivesDokument4 SeitenDensity of Aggregates: ObjectivesKit Gerald EliasNoch keine Bewertungen
- Darnell's Father Goes StrictDokument2 SeitenDarnell's Father Goes StrictDavid Theodore Richardson IIINoch keine Bewertungen
- Platinum Gazette 29 November 2013Dokument12 SeitenPlatinum Gazette 29 November 2013Anonymous w8NEyXNoch keine Bewertungen
- ZP Series Silicon Rectifier: Standard Recovery DiodesDokument1 SeiteZP Series Silicon Rectifier: Standard Recovery DiodesJocemar ParizziNoch keine Bewertungen
- Gsis - Ra 8291Dokument33 SeitenGsis - Ra 8291RoySantosMoralesNoch keine Bewertungen
- Informática Ejercicios IDokument10 SeitenInformática Ejercicios IAlejandroMendezNoch keine Bewertungen
- Edna Adan University ThesisDokument29 SeitenEdna Adan University ThesisAbdi KhadarNoch keine Bewertungen
- The Bresle Method: Improving Accuracy of Soluble Salt MeasurementsDokument4 SeitenThe Bresle Method: Improving Accuracy of Soluble Salt MeasurementsMuthuKumarNoch keine Bewertungen
- Berman Et Al-2019-Nature Human BehaviourDokument5 SeitenBerman Et Al-2019-Nature Human BehaviourMira mNoch keine Bewertungen
- 3.SAFA AOCS 4th Ed Ce 2-66 1994Dokument6 Seiten3.SAFA AOCS 4th Ed Ce 2-66 1994Rofiyanti WibowoNoch keine Bewertungen
- 1 The Fifth CommandmentDokument10 Seiten1 The Fifth CommandmentSoleil MiroNoch keine Bewertungen
- Kidde Ads Fm200 Design Maintenance Manual Sept 2004Dokument142 SeitenKidde Ads Fm200 Design Maintenance Manual Sept 2004José AravenaNoch keine Bewertungen
- Notes Lecture No 3 Cell Injury and MechanismDokument5 SeitenNotes Lecture No 3 Cell Injury and MechanismDr-Rukhshanda RamzanNoch keine Bewertungen