Beruflich Dokumente
Kultur Dokumente
Clin View Jan2010 - E
Hochgeladen von
Ridha Surya NugrahaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Clin View Jan2010 - E
Hochgeladen von
Ridha Surya NugrahaCopyright:
Verfügbare Formate
CLINICAL Viewpoint
Expanding Treatment Options for
Diabetes: GLP-1 Receptor Agonists
t
h
g
i
r
y
Cop ercial
mm
Advancements in Diabetes Management:
on
i
t
u
b
A Canadian Diabetes Steering Committee Report
i
r
t
s
Di
d,
downloa
n
a
c
s
r
use
use
thorised
u
A
.
ersonal
d
p
e
r
it
o
f
ib
y
h
p
o
co
e pr
rised us
t a single
o
in
h
r
t
p
u
a
d
n
n
a
U
view
display,
or
e
l
a
S
r
Not fo
Co
Report 2 Objectives
After reading this report, physicians will be able to:
1.Understand the incretin system and its role in
regulating glucose homeostasis;
2.Critically assess the similarities and differences
between GLP-1 receptor agonists and DPP-4
inhibitors; and
3.Describe the potential advantages and
disadvantages of GLP-1 receptor agonists in
relation to existing antihyperglycemic agents.
In this Report
Diabetes management is continually evolving. Our
current toolbox of oral antihyperglycemic agents
includes many different drugs that work in different
Editorial Consultants
Gary Costain,
Saint John Regional Hospital,
Saint John, New Brunswick
Jean-Marie Eko,
Centre Hospitalier Universitaire,
Montreal, Quebec
Ronald Goldenberg,
North York General Hospital & LMC Endocrinology Centres,
Toronto, Ontario
Philip Hardin,
West Edmonton Diabetes Centre,
Edmonton, Alberta
Linda Sinnaeve,
Chatham-Kent Health Alliance,
Chatham, Ontario
CLINICAL Viewpoint
January 2010
ways. A new class of therapies (termed incretin
agents) has shown promise in the management of
diabetes through novel mechanisms of action. This
report will provide an introduction to agents in this
new class and contrast them with currently available
therapies.
Presenting the Incretin System
At any given level of plasma glucose, pancreatic beta
cells secrete more insulin if glucose is given orally
rather than intravenously (Figure 1).1 This difference
is termed the incretin effect. This amplification of
insulin secretion when glucose is ingested orally is
mediated by peptide hormones (incretins) secreted
from the intestinal tract. The physiologically important incretins are glucose-dependent insulinotropic
polypeptide or GIP (secreted by jejunal cells) and
glucagon-like peptide-1 or GLP-1 (secreted by ileal L
cells and colon).2-5 Both GIP and GLP-1 have short
half livesthey are rapidly metabolized by the
enzyme dipeptidyl peptidase-4 (DPP-4) leading to
their inactivation.6 In individuals with diabetes, the
biological effects of GIP are completely lost and
GLP-1 levels are significantly lower than in non-diabetics; however the functional effects of GLP-1 are
retained.2,7 For this reason, GLP-1 has been more
extensively studied in the context of drug development. Therapeutic incretin agents include modified
and unmodified biological compounds which imitate
the structure and function of the naturally occurring
gastrointestinal hormones, or substances that inhibit the inactivation of these hormones.
FIGURE 1
The Incretin Effect: Intravenous and Oral Glucose Loads
Result in Identical Glucose Responses (A), But Varied Insulin Responses (B)1
150
100
50
0
Oral glucose load
IV glucose load
120
Plasma insulin (mU/L)
Plasma glucose (mg/dL)
200
90
Incretin
effect
60
30
0
-60
60
120
Minutes
180
240
360
-60
60
120
Minutes
180
240
360
Oral glucose administered at time = 0 minutes.
The Multiple Glucoregulatory
Benefits of GLP-1 (Figure 2)
Glucose-dependent insulin secretion. As stated
above, GLP-1 augments the insulin response to
ingested glucose (Figure 3B). However, this enhancement of insulin secretion only occurs in the presence
of elevated blood glucose. Thus, agents that mimic
the effect of GLP-1 are unlikely to cause significant
hypoglycemia.
Glucagon secretion. In addition to glucose-dependent insulin secretion, a very important physiological
effect of GLP-1 is the inhibition of glucagon secretion
(Figure 3C).11 Glucagon has an important role in
stimulating glucose production and release from the
liver (especially in the fasting state). In non-diabetic
individuals, glucagon is suppressed with food ingestion. In individuals with diabetes, glucagon secretion
Diabetes management is continually
evolving. Our current toolbox of oral
antihyperglycemic agents includes
many different drugs that work in
different ways. A new class of
therapies (termed incretin agents)
has shown promise in the
management of diabetes through
novel mechanisms of action.
CLINICAL Viewpoint
January 2010
is not suppressed postprandially. The continued effect
of glucagon on liver glucose production contributes
significantly to hyperglycemia.2
Gastric emptying and satiety. GLP-1 can also
modulate factors associated with nutrient ingestion
and absorption. It has been shown to promote the
feeling of satiety and to decrease food intake in
humans.12 GLP-1 also delays gastric emptying,
which has the effect of slowing down glucose absorption into the blood stream.13 In fact, GLP-1-based
therapies are weight-neutral or associated with
weight loss. Other antihyperglycemic therapies
such as insulin sensitizers and secretagoguesmay
actually result in weight gain.14
Beta cell function. In vitro, GLP-1 has been shown
to promote differentiation of cells into beta cells and
to reduce beta cell death.15,16 Both observations are
intriguing as they raise the possibility that GLP-1
could prevent beta cell death and actually produce
new beta cells in humans. These findings are in contrast with in vitro data which seem to indicate that
overstimulation of the beta cells by insulin secretagogues might actually lead to beta cell death in the
long term.16
Harnessing the Therapeutic
Potential of GLP-1
GLP-1 has a half-life of approximately 1-2 minutes.
It is rapidly cleaved by the enzyme DPP-4 and eliminated by renal excretion.17 Many of the effects of
GLP-1 observed in clinical research (Table 1) were
Expanding Treatment Options for Diabetes
FIGURE 2
Diagrammatic Overview of GLP-1 Physiological Actions8-10
Meal
Active
GLP-1
DPP-4
Inactive GLP-1
Decreased glucagon secretion
Decreased gastric emptying
obtained under conditions of continuous GLP-1 infusion. Given the short half-life of GLP-1 and the
impracticality of continuous infusion in clinical practice, other means to achieve the effects of GLP-1 have
been investigated. This research has led to the development of DPP-4 inhibitors and GLP-1 receptor agonists, both of which work to restore GLP-1 action in
type 2 diabetics.
DPP-4 inhibitors prevent the inactivation of GLP-1
by DPP-4 enzymes, thereby prolonging GLP-1 availability in the body. There are two DPP-4 inhibitors
currently available in Canada: sitagliptin and saxagliptin. Both agents have demonstrated significant
A1C reductions compared to placebo and a weight
neutral effect.18-21 Sitagliptin and saxagliptin are
dosed once daily due to their long half-lives. The
most commonly reported adverse event associated
with DPP-4 inhibitors is nasopharyngitis.18,20 There
have been rare reports of pancreatitis in patients
receiving DPP-4 inhibitors.22
GLP-1 receptor agonists. Another way to prolong
the effects of GLP-1 is the development of GLP-1
receptor agonists that are resistant to enzymatic inactivation by DPP-4. Although GLP-1 receptor agonists
are not yet available in Canada, two such agents have
been extensively studied: exenatide and liraglutide.
Exenatide is a protein derived from the saliva of a
lizard known as the Gila monster and possesses
Decreased food intake
Increased insulin secretion
(glucose-dependent)
Increased satiety
Increased beta cell growth* & function
(*in vitro and animal studies)
approximately 53% homology to human GLP-1.
Development of anti-exenatide antibodies has been
noted in some patients using this agent.23 Liraglutide
is a natural human GLP-1 receptor agonist which has
been modified slightly to protect it from inactivation
by DPP-4.23 Liraglutide has 97% homology to
endogenous GLP-1 and, as a result, greatly reduced
antibody development has been observed with liraglutide administration compared to exenatide.24-26
Overall, both liraglutide and exenatide have
demonstrated significant A1C reductions of up to
1.5% and 1.11%, respectively.25,27 Further, the GLP-1
receptor agonists have also demonstrated weight
reduction, while DPP-4 inhibitors are reportedly
weight neutral.28,29 Liraglutide and exenatide have
In individuals with diabetes, the
biological effects of GIP are completely
lost and GLP-1 levels are significantly
lower than in non-diabetics; however
the functional effects of GLP-1 are
retained.1,6 For this reason, GLP-1
has been more extensively studied in
the context of drug development.
CLINICAL Viewpoint
January 2010
FIGURE 3
Glucoregulatory Effects of GLP-1 IV
Infusion on Plasma Glucose Levels (A),
Plasma Insulin Levels (B), and Plasma
Glucagon Levels (C)11
Placebo
GLP-1 Infusion
15
Glucose (mmol/L)
*
10
*
*
5
* p < 0.05; n = 10
0
-30 0
60
120
Minutes
180
Insulin (mol/L)
15 * p < 0.05; n = 10
240
Placebo
GLP-1 Infusion
10
0
-30 0
*
60
120
Minutes
180
*
240
Glucagon (mol/L)
commonly reported adverse events.24-29,34,35 Similar
to DPP-4 inhibitors, there have also been rare reports
of pancreatitis in patients receiving GLP-1 receptor
agonists. 24,28,34-36 However, there are too few
reports to establish whether or not there is a causeand-effect relationship between the development of
pancreatitis and treatment with DPP-4 inhibitors or
GLP-1 receptor agonists. Additionally, patients with
type 2 diabetes have a 2.8-fold greater risk of developing acute pancreatitis compared to the general
population.37
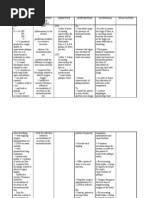
Strengths and Weaknesses of Currently
Available Antihyperglycemic Agents
15
10
*
5
* p < 0.05; n = 10
0
-30 0
60
Placebo
GLP-1 Infusion
120
Minutes
180
240
also shown beneficial effects on blood pressure (BP);
this parameter is not indicated as an endpoint in the
published phase III trials of DPP-4 inhibitors among
people living with diabetes.25,30-32
Preliminary data have demonstrated that GLP-1
receptor agonists have a beneficial effect on beta cell
function.33,34 However, further studies are required to
evaluate whether this will impact diabetes disease
progression.
GLP-1 receptor agonists are generally well-tolerated;
transient gastrointestinal symptoms are the most
CLINICAL Viewpoint
Many of the effects of GLP-1
observed in clinical research (Table 1)
were obtained under conditions of
continuous GLP-1 infusion. Given the
short half-life of GLP-1 and the
impracticality of continuous infusion
in clinical practice, other means to
achieve the effects of GLP-1 have
been investigated.
January 2010
Each class of antihyperglycemic agents possesses its
own mode of action. No class of agents is able to
address all of the abnormalities associated with diabetes. Accordingly, most individuals living with diabetes are prescribed a combined regimen of antihyperglycemic agents. Unfortunately, these regimens
eventually fail as they are unable to address the progression and evolution of the disease. Moreover, they
may expose patients to a host of adverse events
including weight gain and hypoglycemia.14,38
Blood glucose reduction. In the absence of contraindications, metformin is recommended as the
first-line therapy for diabetes. The recommendation
for metformins use first line is based upon its efficacy in lowering A1C and its relatively good adverse
effect profile. If target A1C is not met with metformin alone another agent from a different class
such as a sulfonylurea (SU) or a thiazolidinedione
(TZD)should be added. Both SUs and TZDs have
shown similar efficacy to metformin in terms of A1C
lowering.14 SUs offer a less durable reduction in A1C
Expanding Treatment Options for Diabetes
TABLE 1
Overview of GLP-1 Actions
1. Glucose-dependent insulin secretion
2. Inhibits glucagon secretion
3. Delays gastric emptying
improved control of postprandial glucose
homeostasis
4. Promotes feeling of satiety and reduced food
intake
results in weight loss
5. Possible action: promotes beta cell growth and
function
increases insulin synthesis
increases insulin sensitivity
Each class of antihyperglycemic
agents possesses its own mode of
action. No class of agents is able to
address all of the abnormalities
associated with diabetes. Accordingly,
most individuals living with diabetes
are prescribed a combined regimen of
antihyperglycemic agents.
Unfortunately, these regimens
eventually fail as they are unable to
address the progression and evolution
of the disease.
promotes beta cell differentiation
promotes beta cell survival
when compared to metformin and TZDs. The
reduced durability is attributed to a decrease in beta
cell function and mass related to disease progression.39 Meglitinides are insulin secretagogues similar
to SUs. The meglitinides provide lower A1C reductions but are associated with better postprandial glucose (PPG) reductions. Alpha-glucosidase inhibitors
and DPP-4 inhibitors both lower glucose via gastrointestinal-related mechanisms but do so to a lesser extent than the other antihyperglycemic agents.
Like the meglitinides, alpha-glucosidase inhibitors
and DPP-4 inhibitors also show improved efficacy in
reducing PPG levels.14
Impact on body weight. SUs and TZDs are frequently associated with weight gain. Metformin,
alpha-glucosidase inhibitors and DPP-4 inhibitors are
generally weight neutral.14
Risk of developing hypoglycemia. Hypoglycemia
remains a major problem for patients trying to
achieve glycemic targets. Insulin secretagogues
particularly SUsare most frequently associated
with an increased risk of hypoglycemia.14 Patients
prescribed SUs should be counseled about the recognition and prevention of hypoglycemia.
Incidence of adverse effects. As with other medications, oral antihyperglycemic agents are associated
with adverse effects. Alpha-glucosidase inhibitors
and metformin are the antihyperglycemic agents
most frequently associated with gastrointestinal
adverse effects which are usually mild to moderate in
intensity.14 In addition to gastrointestinal adverse
effects, metformin is rarely associated with lactic acidosis. TZDs have been associated with fluid retention, edema, congestive heart failure and osteoporosis.14 In selecting an appropriate treatment regimen
for people with diabetes, the adverse effect profile
must be weighed against the potential benefits.
Effect on beta cell function. TZDs and incretinbased therapies have shown potential for improvements in beta cell function.40 However, long-term
data are still required to assess the impact on disease
progression and the clinical management of diabetes.
Summary: Bridging the
Gap in Diabetes Care
Current oral antihyperglycemic agents are useful in
the management of type 2 diabetes. Unfortunately, no
single agent is able to address all the pathophysiological abnormalities of diabetes. Therefore new, effective agents with novel mechanisms of action are a
welcomed addition to our treatment options. Incretinbased therapies stimulate insulin secretion only when
glucose is elevated; thus, significantly decreasing the
risk of hypoglycemia. Agents in this class are either
weight neutral (DPP-4 inhibitors) or are associated
with significant weight loss (GLP-1 receptor agonists). In view of the progressive beta cell dysfunction
in type 2 diabetes, interventions that might improve
or preserve beta cell function are particularly intriguCLINICAL Viewpoint
January 2010
ing. Incretin-based therapies show promise in this
area; however, long term data are still required to
assess the clinical relevance of in vitro observations.
In the Next Report:
The next report will address GLP-1 receptor agonists
in more detail.
The authors would like to acknowledge Adam Beveridge from ANTIBODY Healthcare Communications for
his contribution to this article.
This program is supported by an unrestricted educational grant from Novo Nordisk Canada Inc.
References:
1. Girard J. The incretins: from the concept to their use in the treatment of type 2 diabetes. Part
A: Incretins: Concept and physiological functions. Diabetes Metab 2008; 34(6 Pt 1):550-9.
2. Holst JJ, Vilsboll T, Deacon CF. The incretin system and its role in type 2 diabetes mellitus.
Mol Cell Endocrinol 2009; 297:127-36.
3. Baggio LL, Drucker DJ. Biology of incretins: GLP-1 and GIP. Gastroenterology 2007; 132:2131-57.
4. McIntyre N, Holdsworth CD, Turner DS. Intestinal factors in the control of insulin secretion. J
Clin Endocrinol Metab 1965; 25:1317-24.
5. Vilsboll T, Holst JJ. Incretins, insulin secretion and type 2 diabetes mellitus. Diabetologia
2004; 47:357-66.
6. Kieffer TJ, McIntosh CHS, Pederson RA. Degradation of glucose-dependent insulinotropic
polypeptide and truncated glucagon-like peptide 1 in vitro and in vivo by dipeptidyl peptidase
IV. Endocrinology 1995; 136(8):3585-96.
7. Vilsboll T, Krarup T, Deacon CF, et al. Reduced postprandial concentrations of intact biologically
active glucagon-like peptide 1 in type 2 diabetic patients. Diabetes 2001; 50:609-13.
8. Drucker DJ. Enhancing incretin action for the treatment of type 2 diabetes. Diabetes Care
2003; 26:2929-40.
9. Drucker DJ. Glucagon-like peptides: regulators of cell proliferation, differentiation, and
apoptosis. Mol Endocrinol 2003; 17:161-71.
10. Drucker DJ. Development of glucagon-like peptide-1-based pharmaceuticals as therapeutic
agents for the treatment of diabetes. Curr Pharm Des 2001; 7:1399-412.
11. Nauck MA, Kleine N, Orskov C, et al. Normalization of fasting hyperglycaemia by exogenous
glucagon-like peptide 1 (7-36 amide) in type 2 (non-insulin-dependent diabetic patients).
Diabetologia 1993; 36:741-44.
12. Flint A, Raben A, Astrup A, et al. Glucagon-like peptide 1 promotes satiety and suppresses
energy intake in humans. J Clin Invest 1998; 101(3):515-20.
13. Zander M, Madsbad S, Madsen JL, et al. Effect of 6-week course of glucagon-like peptide
1 on glycaemic control, insulin sensitivity, and -cell function in type 2 diabetes: a parallelgroup study. Lancet 2002; 359:824-30.
14. Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Canadian
Diabetes Association 2008 clinical practice guidelines for the prevention and management
of diabetes in Canada. Can J Diabetes 2008; 32(suppl 1):S1-S201.
15. Farilla L, Bulotta A, Hirshberg B, et al. Glucagon-like peptide 1 inhibits cell apoptosis and
improves glucose responsiveness of freshly isolated human islets. Endocrinology 2003;
144(12):5149-58.
16. Takahashi A, Nagashima K, Hamasaki A, et al. Sulfonylurea and glinide reduce insulin
content, functional expression of KATP channels, and accelerate apoptotic -cell death in the
chronic phase. Diabetes Res Clin Pract 2007; 77:343-50.
17. Elbrond B, Jakobsen G, Larson S et al. Pharmacokinetics, pharmacodynamics, safety and
tolerability of a single-dose of NN2211, a long-acting glucagon-like peptide 1 derivative in
healthy male subjects. Diabetes Care 2002; 25(8):1398-1404.
18. Januvia (sitagliptin) Canadian Product Monograph. Merck Frosst Canada LTD., June 30, 2009.
19. Richter B, Bandeira-Echtler E, Bergerhoff K, et al. Emerging role of dipeptidyl peptidase-4
inhibitors in the management of type 2 diabetes. Vascular Health and Risk Management
2008; 4(4):75368.
29. OnglyzaTM (saxagliptin) Canadian Product Monograph. AstraZeneca Canada Inc., September
14, 2009.
21. Dhillon S, Weber J. Saxagliptin. Drugs 2009;69(15):2103-114.
22. Information for Healthcare Professionals: Acute pancreatitis and sitagliptin (marketed as
Januvia and Janumet) 9/25/2009. U.S. Food and Drug Administration. Accessed on
November 10, 2009 from http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafety
InformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/ucm1
83764.htm.
23. Drucker DJ, Nauck MA. The incretin system: glucagon-like receptor 1 and dipeptidyl
peptidase-4 in inhibitors in type 2 diabetes. Lancet 2006; 368:1696705.
24. Marre M, Shaw J, Brndle M, et al. Liraglutide, a once-daily human GLP-1 analogue, added
to a sulphonylurea over 26 weeks produces greater improvements in glycaemic and weight
control compared with adding rosiglitazone or placebo in subjects with type 2 diabetes
(LEAD-1 SU). Diabetes Medicine 2009; 26:268-78.
25. Zinman B, Gerich J, Buse JB, et al. Efficacy and safety of the human glucagon-like peptide1 analog liraglutide in combination with metformin and thiazolidinedione in patients with type
2 diabetes (LEAD-4 met+TZD). Diabetes Care 2009; 32:1224-30.
26. Russell-Jones D, Vaag A, Schmitz O, et al. Liraglutide vs. insulin glargine and placebo in
combination with metformin and sulfonylurea therapy in type 2 diabetes mellitus (LEAD-5
met+SU): a randomised controlled trial. Diabetologia 2009; 52(10):2046-55.
27. Heine RJ, Van Gaal RF, Johns D, et al. Exenatide versus insulin glargine in patients with
suboptimally controlled type 2 diabetes. Ann Intern Med 2005; 143(8):559-70.
28. Buse JB, Rosenstock J, Sesti G, et al. Liraglutide once a day versus exenatide twice a day
for type 2 diabetes: a 26-week randomized, parallel-group multinational, open-label trial
(LEAD-6). Lancet 2009; 374(9683):39-47.
29. DeFronzo RA, Ratner RE, Han J, et al. Effects of exenatide (exendin-4) on glycemic control
and weight over 30 weeks in metformin-treated patients with type 2 diabetes. Diabetes Care
2005; 28:1092-1100.
30. Colagiuri S, Frid A, Zdravkovic M, et al. Poster presented at the 44th Annual Meeting of the
European Association for the Study of Diabetes, September 7-11, 2008; Rome, Italy.
31. Klonoff DC, Buse JB, Nielsen LL, et al. Exenatide effects on diabetes, obesity, cardiovascular
risk factors and hepatice biomarkers in patients with type 2 diabetes treated for at least 3
years. Curr Med Res Opin 2008; 24(1):275-86.
32. Madsbad S, Krarup T, Deacon CF, et al. Glucagon-like peptide receptor agonists and
dipeptidyl peptidase-4 inhibitors in the treatment of diabetes: a review of clinical trials. Curr
Opin Clin Nutr Metab Care 2008; 11(4):491-9.
33. Nauck M, Duran S, Kim D, et al. A comparison of twice-daily exenatide and biphasic insulin
aspart in patients with type 2 diabetes who were suboptimally controlled with sulfonylurea
and metformin: a non-inferiority study. Diabetologia 2007; 50:259-67.
34. Nauck M, Frid A, Hermansen K, et al. Efficacy and safety comparison of liraglutide,
glimepiride and placebo, all in combination with metformin, in type 2 diabetes: the LEAD
(liraglutide effect and action in diabetes)-2 study. Diabetes Care 2009; 32:84-90.
35. Garber A, Henry R, Ratner R, et al. Liraglutide versus glimepiride monotherapy for type 2
diabetes (LEAD-3 Mono): a randomised, 52-week, phase III, double-blind, parallel-treatment
trial. Lancet 2009; 373(9662):473-81.
36. Information for Healthcare Professionals: Exenatide (marketed as Byetta) 8/2008 Update.
U.S. Food and Drug Administration. Accessed on November 1, 2009 from
http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProvi
ders/ucm124713.htm.
37. Noel RA, Braun DK, Patterson RE, et al. Increased risk of acute pancreatitis and biliary
disease observed in patients with type 2 diabetes: a retrospective cohort study. Diabetes
Care 2009; 32(5):834-838.
38. Virally M, Blickl J-F, Girard J, et al. Type 2 diabetes mellitus: epidemiology, pathophysiology,
unmet needs and therapeutical perspectives. Diabetes Metab 2007; 33:231-44.
39. Matthews DR, Cull CA, Stratton IM, et al. UKPDS 26: Sulphonylurea failure in non-insulindependent diabetic patients over six years. UK Prospective Diabetes Study (UKPDS) Group.
Diabet Med 1998; 15(4):297-303.
40. Wajchenberg BL. Beta-cell failure in diabetes and preservation by clinical treatment. Endocr
Rev 2008;28(2):187-218.
Copyright 2010 STA HealthCare Communications Inc. All rights reserved. This program is published by STA HealthCare Communications Inc. as a
professional service to physicians through an unrestricted educational grant by Novo Nordisk Canada Inc. The information and opinions contained
herein reflect the views and experience of the authors and not necessarily those of Novo Nordisk Canada Inc. or STA HealthCare Communications Inc.
Any products mentioned herein should be used in accordance with the prescribing information contained in their respective product monograph.
CLINICAL Viewpoint
January 2010
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- PTSD DBQ 21-0960P-4Dokument5 SeitenPTSD DBQ 21-0960P-4Christopher Reece100% (1)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Aging AdultDokument18 SeitenAging AdultGladz C CadaguitNoch keine Bewertungen
- Senses Review WorksheetDokument6 SeitenSenses Review WorksheetpicassaaNoch keine Bewertungen
- Types of Anaesthesia: Prof. Med. Nabil H. MohyeddinDokument30 SeitenTypes of Anaesthesia: Prof. Med. Nabil H. MohyeddinRidha Surya NugrahaNoch keine Bewertungen
- Form Kosong Ppi Bulanan by Ma ItingDokument4 SeitenForm Kosong Ppi Bulanan by Ma ItingRidha Surya NugrahaNoch keine Bewertungen
- Surgical Positioning 2010Dokument74 SeitenSurgical Positioning 2010Ridha Surya NugrahaNoch keine Bewertungen
- Generalanaesthesia Drdhriti 111223120647 Phpapp01Dokument64 SeitenGeneralanaesthesia Drdhriti 111223120647 Phpapp01Ridha Surya NugrahaNoch keine Bewertungen
- Patient Monitoring1370Dokument53 SeitenPatient Monitoring1370Ridha Surya NugrahaNoch keine Bewertungen
- Cardiovascular Physiology: The Autonomic Nervous SystemDokument8 SeitenCardiovascular Physiology: The Autonomic Nervous SystemRidha Surya NugrahaNoch keine Bewertungen
- Classification of General AnaestheticsDokument24 SeitenClassification of General AnaestheticsRidha Surya NugrahaNoch keine Bewertungen
- Glucagon-Like Peptide 1 and Appetite: Megan J. Dailey and Timothy H. MoranDokument7 SeitenGlucagon-Like Peptide 1 and Appetite: Megan J. Dailey and Timothy H. MoranRidha Surya NugrahaNoch keine Bewertungen
- Practical Use of Glucagon-Like Peptide-1 Receptor Agonist Therapy in Primary CareDokument10 SeitenPractical Use of Glucagon-Like Peptide-1 Receptor Agonist Therapy in Primary CareRidha Surya NugrahaNoch keine Bewertungen
- Types of Anaesthesia: Prof. Med. Nabil H. MohyeddinDokument30 SeitenTypes of Anaesthesia: Prof. Med. Nabil H. MohyeddinRidha Surya NugrahaNoch keine Bewertungen
- Jp27784 Ifu en Glp-1 Elisa Sym2Dokument4 SeitenJp27784 Ifu en Glp-1 Elisa Sym2Ridha Surya NugrahaNoch keine Bewertungen
- Efficacy of GLP-1 Receptor Agonists and DPP-4 Inhibitors: Meta-Analysis and Systematic ReviewDokument34 SeitenEfficacy of GLP-1 Receptor Agonists and DPP-4 Inhibitors: Meta-Analysis and Systematic ReviewRidha Surya NugrahaNoch keine Bewertungen
- ECBCM - Oral Meds T2 Diab - Clinician06282011Dokument8 SeitenECBCM - Oral Meds T2 Diab - Clinician06282011Ridha Surya NugrahaNoch keine Bewertungen
- Ibit 06 I 4 P 231Dokument7 SeitenIbit 06 I 4 P 231Ridha Surya NugrahaNoch keine Bewertungen
- FDA AnalysisDokument7 SeitenFDA AnalysisRidha Surya NugrahaNoch keine Bewertungen
- Vitro and in Vivo Gastric Actions: Vagally Mediated Effects of Glucagon-Like Peptide 1: inDokument11 SeitenVitro and in Vivo Gastric Actions: Vagally Mediated Effects of Glucagon-Like Peptide 1: inRidha Surya NugrahaNoch keine Bewertungen
- F 2433 CMED Saxagliptin A Selective DPP 4 Inhibitor For The Treatment of Type 2 D.PDF 3311Dokument12 SeitenF 2433 CMED Saxagliptin A Selective DPP 4 Inhibitor For The Treatment of Type 2 D.PDF 3311Ridha Surya NugrahaNoch keine Bewertungen
- Common Causes of BlindnessDokument58 SeitenCommon Causes of BlindnesskaunaNoch keine Bewertungen
- Case PresentationDokument21 SeitenCase PresentationMae Alleslie TolentinoNoch keine Bewertungen
- DVT Assessment FormDokument1 SeiteDVT Assessment FormLoy ZiNoch keine Bewertungen
- YersiniaDokument16 SeitenYersiniaAlexandra Ançã PiresNoch keine Bewertungen
- Sop of Clo2Dokument4 SeitenSop of Clo2Anup RanjanNoch keine Bewertungen
- Carpal Tunnel SyndromeDokument43 SeitenCarpal Tunnel SyndromePra YudhaNoch keine Bewertungen
- NCM Digestive 2 PDFDokument11 SeitenNCM Digestive 2 PDFsamantha lumapasNoch keine Bewertungen
- Esmr 2Dokument1 SeiteEsmr 2Martina FitriaNoch keine Bewertungen
- Assignment On Health Assessment 1Dokument5 SeitenAssignment On Health Assessment 1Sumit YadavNoch keine Bewertungen
- Surgery OSCE Stations With KeyDokument274 SeitenSurgery OSCE Stations With KeyMoazzam AliNoch keine Bewertungen
- Age NCPDokument3 SeitenAge NCPMartin Allen ClaudioNoch keine Bewertungen
- Acute Tonsillopharyngitis - NonexudativeDokument12 SeitenAcute Tonsillopharyngitis - NonexudativeLemuel GuevarraNoch keine Bewertungen
- Bile Duct DilatedDokument4 SeitenBile Duct DilatedAmit GauravNoch keine Bewertungen
- NCP On Bpad (Bipolar Affective Disorder) : SGRD College of Nursing Vallah AmritsarDokument18 SeitenNCP On Bpad (Bipolar Affective Disorder) : SGRD College of Nursing Vallah AmritsarMonika100% (2)
- Febrile Seizure PDFDokument14 SeitenFebrile Seizure PDFgetnaniNoch keine Bewertungen
- 2007 Clinical Manual of Eating Disorders PDFDokument483 Seiten2007 Clinical Manual of Eating Disorders PDFPsiquiatría CESAME100% (4)
- Public Health COC ExamDokument19 SeitenPublic Health COC ExamTut Kong RuachNoch keine Bewertungen
- Pharmacotherapy of Anxiety Disorders: Current and Emerging Treatment OptionsDokument21 SeitenPharmacotherapy of Anxiety Disorders: Current and Emerging Treatment OptionsGabriel Vargas CuadrosNoch keine Bewertungen
- Juicing Cleanse: by Brenda T BradleyDokument14 SeitenJuicing Cleanse: by Brenda T Bradleylicda0% (1)
- Neonatal Seizures : Types, Etiology and Long Term Neurodevelopmental Out-Come at A Tertiary Care HospitalDokument7 SeitenNeonatal Seizures : Types, Etiology and Long Term Neurodevelopmental Out-Come at A Tertiary Care HospitalAgung NohuNoch keine Bewertungen
- 3family Case Presentation-Powerpoint1Dokument10 Seiten3family Case Presentation-Powerpoint1MrLarry DolorNoch keine Bewertungen
- Vol 10, No 2 (2019) H. 163-172: Jurnal Pendidikan Matematika Dan IpaDokument10 SeitenVol 10, No 2 (2019) H. 163-172: Jurnal Pendidikan Matematika Dan Ipaazmi azhariNoch keine Bewertungen
- NCP For Ineffective Airway ClearanceDokument3 SeitenNCP For Ineffective Airway ClearanceJennelyn BayleNoch keine Bewertungen
- Infecciones Necrotizantes de Tejidos Blandos TheLancet 2023Dokument14 SeitenInfecciones Necrotizantes de Tejidos Blandos TheLancet 2023Nicolás LaverdeNoch keine Bewertungen
- 12b1705 Andrographis Paniculata SambilotoDokument2 Seiten12b1705 Andrographis Paniculata Sambilotofajar1987Noch keine Bewertungen
- FRCPath Part 1 Course - Day 1Dokument11 SeitenFRCPath Part 1 Course - Day 1Marvi UmairNoch keine Bewertungen
- Pneumonia IntroductionDokument3 SeitenPneumonia Introductiondareine22Noch keine Bewertungen