Beruflich Dokumente
Kultur Dokumente
13.a Case of Malignant Peripheral Nerve Sheath Tumor in Parapharyngeal Space
Hochgeladen von
DR K C MALLIK0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
40 Ansichten3 Seitenan official publication of otolaryngologists of India Odisha State branch
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenan official publication of otolaryngologists of India Odisha State branch
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
40 Ansichten3 Seiten13.a Case of Malignant Peripheral Nerve Sheath Tumor in Parapharyngeal Space
Hochgeladen von
DR K C MALLIKan official publication of otolaryngologists of India Odisha State branch
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 3
DOI No.: 10.21176/ ojolhns.0974-5262.2016.10.
A CASE OF MALIGNANT PERIPHERAL NERVE SHEATH TUMOR
IN PARAPHARYNGEAL SPACE
*Souvagini Acharya, **Utkal P Mishra, ***Debasish Jena
Date of receipt of article -23-2-2016
Date of acceptance -2-5-2016
DOI-10.21176/ojolhns.2016.10.1.13
ABSTRACT
Malignant peripheral nerve sheath tumors (MPNSTs) are spindle-cell sarcomas which are aggressive tumors
accounting for 510% of all soft tissue sarcomas. It is locally invasive, frequently leading to multiple recurrences
and eventual metastatic spread. In human body, the trunk and extremities are the most commonly involved sites,
with only 8-14% of all lesions appearing in the head and neck region. Diagnosis is difficult in most cases. Wide
surgical excision followed by Radiotherapy is the treatment of choice.We present a case of malignant peripheral
nerve sheath tumor involving the left parapharynx in a 25-year-old patient who complained of swelling & dysphagia
that aggravated over a month. After surgery, tumor was finally diagnosed as malignant peripheral nerve sheath
tumor by histopathologic examinations.
Key words:- Malignant peripheral nerve sheath tumor, Parapharyngeal, Neurofibrosarcoma, Malignant
schwannoma, Malignant neurilemmoma.
INTRODUCTION
CASE REPORT
Malignant peripheral nerve sheath tumour
(MPNST) is the term coined by the World Health
Organization and corresponds to the malignant
proliferation of any cell of the nerve sheath: Schawnn
cell, perineural fibroblast or endoneural fibroblast.1,5
MPNSTs account for 510 % of all soft-tissue sarcomas
and are one of the most common nonrhabdomyosarcoma
soft-tissue
sarcomas. 3
Approximately 50 % of MPNSTs are diagnosed in
patients with NF1; the lifetime risk of MPNST in NF1
is 813 % as compared to 0.001 % in the general
population.3 The histological features of MPNSTs are
those of a highly cellular, spindle-cell neoplasm
resembling a soft-tissue sarcoma, but with
differentiation toward elements of the nerve sheath,
Schwann cell, and perineural cell.4 Fifty to seventy
percent of MPNST are S-100 immunopositive.1,5 Highgrade MPNSTs metastasize widely and have a poor
prognosis, but low-grade tumors that are diagnosed
early and treated appropriately are compatible with
longterm survival.2 Complete surgical resection is the
only curative treatment for sporadic and NF1-associated
MPNSTs. The surgical goal is to resect the MPNST
with wide negative margins. If complete surgical
resection is not achieved, postoperative radiation
therapy has a role in improving local control.1
A 25 yr old man presented with a 7 month history
of gradually enlarging swelling over left side of neck &
dysphagia to solids that aggravated over a month. On
physical examination a non tender, firm to hard, fixed,
bossolated swelling measuring 12 7 cm over left side
of neck extending from infra-auricular region down to
lower border of cricoid cartillage vertically, from
posterior border of sternomastoid to midline
horizontaly which has displaced the thyroid cartilage
to opposite side.
No neck node enlargement was there. Intraoraly
the mass was extending upto nasopharynx with no
other mass palpable in the body.
Affiliations:
*Associate Professor,**,*** P G Students
Dept of ENT and Head and Neck Surgery
VIMSAR,Burla,Sambalpur,Odisha,India
Address of Correspondence:
Dr Utkal Priyadarsi Mishra
P G Students Dept of ENT and Head and Neck Surgery,
VSS Institute of Medical Science And Research, Burla,
Sambalpur, Odisha, India
Email: drutkal.mishr@gmail.com
Mob: 9439755093
61
Vol.-10, Issue-I, Jan-June - 2016
No neck node enlargement was there. Intraoraly
the mass was extending upto nasopharynx with no
other mass palpable in the body.
DOI No.: 10.21176/ ojolhns.0974-5262.2016.10.1
sympathetic chain. The cut surface of excised mass was
mostly yellowish without hemorrhage or necrosis.
Fig.1: preoperative photograph
Laryngealendoscopy revealed normal vocal cord
movements. X-ray neck suggestive of shifting of trachea
towards right. Routine blood investigations were within
normal limit. FNAC revealed benign parapharyngeal
neurofibroma CT scan revealed a large mass in
parapharyngeal space displacing carotid sheath
extending from nasopharynx upto hypopharynx
without any bone erosion.
Fig.4: the mass after removal
Microscopic examination showed alternating hypo
and hypercellular areas in spindle- or polyhedral-shaped
cells. There was a moderate degree of cellular
pleomorphism and mitoses were found frequently.
Immunohistochemistry showed a strong positive
reaction for S-100. The pathologic diagnosis was
malignant peripheral nerve sheath tumor arising from
cervical sympathetic chain.Postoperatively patient
recovered well & discharged after 7 days. Radiotherapy
was administered as an adjuvant therapy, with 6000 cGy
given to the parapharyngeal space.
The patient was grossly free of symptoms 5 months
after surgery.
DISCUSSION
Vol.-10, Issue-I, Jan-June - 2016
Fig.2:per operative photograph of the mass
Fig.3: Immediate post operative photograph
Wide excision of mass was performed by
transcervical approach with mandibular swing. At
surgery, the mass appeared pinkish white in color
attached tightly to nasopharynx, hypopharynx and
carotid sheath. Site of origin was from cervical
62
Tumors of the parapharyngeal space are relatively
uncommon, representing only 0.5% of all head and
Fig.5: Microscopic features showing alternating hypo and
hypercellular areas in spindle- or polyhedral-shaped cells.
neck tumors. [6] About half the parapharyngeal tumors
are nerve sheath tumors, and another 30% are of salivary
gland origin.7 Malignant peripheral nerve sheath tumors
are rare, highly aggressive tumors capable of arising de
novo or from pre-existing benign neurofibromas or
schwannomas. The peak incidence of disease is known
DOI No.: 10.21176/ ojolhns.0974-5262.2016.10.1
2.
Ferner RE. Neurofibromatosis 1. Ferner RE,
Huson SM, Evans DGR. Neurofibromatosis in
Clinical Practice. 1st ed. Springer; 2011. pp. 19-23.
3. Hooly M, Brigitte C, Ratner N, editors.
Malignant Peripheral Nerve Sheath Tumours:
Prognostic and Diagnostic Markers and
Therapeutic Targets. In: Upaddhyaya M, Cooper
DN. Neurofibromatosis Type 1. 1st ed. Springer;
2012. pp. 445-467.
4. Chitale AR, Dickersin GR. Electron microscopy
in the diagnosis of malignant schwannomas. A
report of six cases. Cancer. 1983;51:144861.
[PubMed]
5. M.S. Kenali, P.G. Bridger, M. Baldwin, R.
Smee.Malignant peripheral nerve sheath tumour
the tongue. Aust N Z J Surg, 69 (3) (1999), pp.
243246.
6. Barnes L, Dekker M. Surgical pathology of the
head and neck. Tumours of the Head and
Neck.2nd ed. Madison Avenue Inc; New York;
2001. p. 836-41.
7. Lee H, Lee C, Jin S, Lee S :A Case of Malignant
Peripheral Nerve Sheath Tumor in
Parapharyngeal
Spacehttp:
//synapse.
koreamed.org / DOIx.php ? doi10.3342/kjorlhns.
2012.55.3.181&vmode =PUBREADER#! po=
25.0000.
8. Wanebo JE, Malik JM, VandenBerg SR, Wanebo
JH, Driesen N, Persing JA: Malignant peripheral
nerve sheath tumors. A clinicopathologic study
of 28 cases.Cancer 1993, 71:1247-1253.
9. Kar M, Deo S, Shukla N, Malik A, Gupta S,
Mohanti B, Thulka S : Malignant peripheral nerve
sheath tumors (MPNST) Clinicopathological
study and treatment outcome of twenty-four cases.
10. Stout AP: Tumors of peripheral nervous system:
Atlas of tumor pathology, Sect. 2, fasc. 6.
Washington, D.C, Armed forces Institute of
pathology; 1949.
11. Ferner RE, Gutmann DH: International
consensus statement on malignant peripheral nerve
sheath tumors in neurofibromatosis.Cancer Res
2002, 62:1573-1577.
12. Basso-Ricci S: Therapy of malignant
schwannomas: usefulness of an integrated
radiologic. surgical therapy.J NeurosurgSci 1989,
33:253-257.
63
Vol.-10, Issue-I, Jan-June - 2016
to occur sporadically between the age of 20s and 50s,
and is usually associated with the neurofibromatosis
type I. About 40-50% of MPNSTs are associated with
a family history of neurofibromatosis-1.7
Microscopically the tumour consists of spindle
cells with a high mitotic rate and indistinct cytoplasmic
borders arranged in bundles or fascicles. The diagnosis
of MPNST is difficult and elusive in the soft tissue
disease due to lack of standardized criteria. It is not
always possible to demonstrate the origin from a nerve,
especially when it arises from a small peripheral branch.
Immuno-histochemistry plays an important part in the
diagnosis, with tumor cells showing specific positivity
for S-100.1
Radical surgical resection is the treatment of choice
in MPNST. A good three-dimensional clearance is
mandatory for a successful outcome. Routine nodal
dissection is not indicated. However, when a major
nerve is identified, the cut end should be sent for frozen
section to assess the tumor free margin of the
resection.Although MPNSTs are generally considered
chemotherapy and radiotherapy resistant tumors.9
Currently, postoperative radiotherapy is recommended
by oncology consensus group as part of a uniform
treatment policy for MPNSTs, much like other high
grade soft tissue sarcomas [8][10], despite having clear
surgical margins. 11
Basso-Ricci demonstrated 56% disease free survival
using combined surgery and radiation therapy for
MPNST.12
CONCLUSION
MPNST is a highly aggressive tumour, which
could be difficult to treat, despite substantial progress
in treatment modalities available in present era. The
wide spreading nature of this tumour has a strong hold
in determining the prognosis. Early detection of this
aggressive tumour may help reduce morbidity.
DISCLOSURES
(a) Competing interests/Interests of Conflict- None
(b) Sponsorships - None
(c) Funding - None
(d) No financial disclosures
REFERENCES
1. F.M. Enzinger, S.W. Weiss. Malignant tumors of
the peripheral nerves. F.M. Enzinger, S.W. Weiss
(Eds.), Soft tissues tumors, Mosby-Year Book, St.
Louis (1995), pp. 889928
Das könnte Ihnen auch gefallen
- A Rare Case Report - Intact Eye Ball in MaxillaryDokument4 SeitenA Rare Case Report - Intact Eye Ball in MaxillaryDR K C MALLIKNoch keine Bewertungen
- OJOLNS-10 - II - Comparative Outcome PDFDokument6 SeitenOJOLNS-10 - II - Comparative Outcome PDFDR K C MALLIKNoch keine Bewertungen
- OJOLHNS-11 Issue-I Jan-June-2017Dokument72 SeitenOJOLHNS-11 Issue-I Jan-June-2017DR K C MALLIKNoch keine Bewertungen
- OJOLNS-10 - II - Effects of GLOSSOPHARYNGEAL PDFDokument5 SeitenOJOLNS-10 - II - Effects of GLOSSOPHARYNGEAL PDFDR K C MALLIKNoch keine Bewertungen
- Ojolhns-10 Issue-IIDokument66 SeitenOjolhns-10 Issue-IIDR K C MALLIKNoch keine Bewertungen
- OJOLNS-10 - II - Invited Editorial PDFDokument5 SeitenOJOLNS-10 - II - Invited Editorial PDFDR K C MALLIKNoch keine Bewertungen
- OJOLNS-10 - II - Endoscopic Trans PDFDokument6 SeitenOJOLNS-10 - II - Endoscopic Trans PDFDR K C MALLIKNoch keine Bewertungen
- OJOLNS-10 - II - Role of Bilateral PDFDokument4 SeitenOJOLNS-10 - II - Role of Bilateral PDFDR K C MALLIKNoch keine Bewertungen
- 13.diagnostic Dilemmas Leading To Fatality inDokument6 Seiten13.diagnostic Dilemmas Leading To Fatality inDR K C MALLIKNoch keine Bewertungen
- OJOLNS-10 - II - Invited Editorial PDFDokument5 SeitenOJOLNS-10 - II - Invited Editorial PDFDR K C MALLIKNoch keine Bewertungen
- OJOLNS-10 - II - Endoscopic Trans PDFDokument6 SeitenOJOLNS-10 - II - Endoscopic Trans PDFDR K C MALLIKNoch keine Bewertungen
- Ojolhns Vol II Issue II 2008Dokument53 SeitenOjolhns Vol II Issue II 2008DR K C MALLIKNoch keine Bewertungen
- OJOLNS-10 - II - Comparative Outcome PDFDokument6 SeitenOJOLNS-10 - II - Comparative Outcome PDFDR K C MALLIKNoch keine Bewertungen
- OJOLNS-10 - II - Study of Crushing PDFDokument5 SeitenOJOLNS-10 - II - Study of Crushing PDFDR K C MALLIKNoch keine Bewertungen
- 12.bilateral Antrochoanal Polyp inDokument4 Seiten12.bilateral Antrochoanal Polyp inDR K C MALLIK0% (1)
- 11.second Branchial Sinus Presenting PDFDokument5 Seiten11.second Branchial Sinus Presenting PDFDR K C MALLIKNoch keine Bewertungen
- 4.anterior Nasal Packing and Eustachian Tube DysfunctionDokument5 Seiten4.anterior Nasal Packing and Eustachian Tube DysfunctionDR K C MALLIKNoch keine Bewertungen
- 2.importance of Pre-Operative HRCT Temporal Bone PDFDokument5 Seiten2.importance of Pre-Operative HRCT Temporal Bone PDFDR K C MALLIKNoch keine Bewertungen
- 9.nasal Glioma in 18 Month ChildDokument5 Seiten9.nasal Glioma in 18 Month ChildDR K C MALLIKNoch keine Bewertungen
- 8.solitary Parotid Mass Presenting As Sarcoidosis Unusual PresentationDokument5 Seiten8.solitary Parotid Mass Presenting As Sarcoidosis Unusual PresentationDR K C MALLIKNoch keine Bewertungen
- Editorial A Tailor Made Approach To Endoscopic Sinus Surgery ForDokument3 SeitenEditorial A Tailor Made Approach To Endoscopic Sinus Surgery ForDR K C MALLIKNoch keine Bewertungen
- Insular Carcinoma of Thyroid - Unusual VariantDokument5 SeitenInsular Carcinoma of Thyroid - Unusual VariantDR K C MALLIKNoch keine Bewertungen
- 8-Ojolns-9 Issue-1 F (With Dio No)Dokument61 Seiten8-Ojolns-9 Issue-1 F (With Dio No)DR K C MALLIKNoch keine Bewertungen
- 10.congenital Choanal AtresiaDokument5 Seiten10.congenital Choanal AtresiaDR K C MALLIKNoch keine Bewertungen
- Insular Carcinoma of Thyroid - Unusual VariantDokument5 SeitenInsular Carcinoma of Thyroid - Unusual VariantDR K C MALLIKNoch keine Bewertungen
- Tissue Myringoplasty PDFDokument6 SeitenTissue Myringoplasty PDFDR K C MALLIKNoch keine Bewertungen
- 1-Roleof Ultrasonography in Thyroid SwellingsDokument6 Seiten1-Roleof Ultrasonography in Thyroid SwellingsDR K C MALLIKNoch keine Bewertungen
- Editorial... Vol.-9 Issue-I Jan-June - 2015Dokument1 SeiteEditorial... Vol.-9 Issue-I Jan-June - 2015DR K C MALLIKNoch keine Bewertungen
- 6.paediatric BronchosDokument7 Seiten6.paediatric BronchosDR K C MALLIKNoch keine Bewertungen
- 2.importance of Pre-Operative HRCT Temporal Bone PDFDokument5 Seiten2.importance of Pre-Operative HRCT Temporal Bone PDFDR K C MALLIKNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Our Lady of Fatima University College of Nursing - Cabanatuan CityDokument3 SeitenOur Lady of Fatima University College of Nursing - Cabanatuan CityDanica FrancoNoch keine Bewertungen
- Differential Diagnosis of Liver NoduleDokument46 SeitenDifferential Diagnosis of Liver NoduleJoydip SenNoch keine Bewertungen
- Hypertension - Management in Pregnancy Guideline (GL952) : ApprovalDokument55 SeitenHypertension - Management in Pregnancy Guideline (GL952) : ApprovalhestiNoch keine Bewertungen
- The Comorbidities of Dysmenorrhea: A Clinical Survey Comparing Symptom Profile in Women With and Without EndometriosisDokument14 SeitenThe Comorbidities of Dysmenorrhea: A Clinical Survey Comparing Symptom Profile in Women With and Without EndometriosisSeptian WidiantoNoch keine Bewertungen
- Kdigo 2013. CKDDokument110 SeitenKdigo 2013. CKDcvsmed100% (1)
- 009the Automated Nucleated Red Cell Count On The Sysmex XE-2100Dokument5 Seiten009the Automated Nucleated Red Cell Count On The Sysmex XE-2100blanket_thNoch keine Bewertungen
- Vaccine Card - 20231120 - 175739 - 0000Dokument2 SeitenVaccine Card - 20231120 - 175739 - 0000MarilynNoch keine Bewertungen
- A Study To Assess The Knowledge, Attitude and Practice of Health Workers Regarding Nosocomial Infection at Selected Hospitals of Birtamode Municipality, JhapaDokument5 SeitenA Study To Assess The Knowledge, Attitude and Practice of Health Workers Regarding Nosocomial Infection at Selected Hospitals of Birtamode Municipality, JhapaIJCRM Research JournalNoch keine Bewertungen
- Emerging and Re Emerging DiseasesDokument63 SeitenEmerging and Re Emerging DiseasesAljun MansalapusNoch keine Bewertungen
- I. The Problem and Its Background Ii. Demand and Analysis Review of Related Literature and Case StudiesDokument3 SeitenI. The Problem and Its Background Ii. Demand and Analysis Review of Related Literature and Case StudiesPaulyn Mae Dela CruzNoch keine Bewertungen
- Therapeutic and Toxic Blood Levels of Over 800 DrugsDokument28 SeitenTherapeutic and Toxic Blood Levels of Over 800 DrugsAndreia AndreiutzaNoch keine Bewertungen
- Format OpnameDokument21 SeitenFormat OpnamerestutiyanaNoch keine Bewertungen
- Pictotrans: Pathology of The Breast Quiz From Dra. Edna May Lasap-GoDokument32 SeitenPictotrans: Pathology of The Breast Quiz From Dra. Edna May Lasap-Go2012Noch keine Bewertungen
- Hypertensive EmergenciesDokument28 SeitenHypertensive EmergenciesluonganhsiNoch keine Bewertungen
- Central Maine Healthcare Cancer Institute Certificate of Need ApplicationDokument33 SeitenCentral Maine Healthcare Cancer Institute Certificate of Need ApplicationMaine Trust For Local NewsNoch keine Bewertungen
- Clinical Aspect of Exercise PhysiologyDokument34 SeitenClinical Aspect of Exercise PhysiologyAnn LoricaNoch keine Bewertungen
- WHO Guidelines On Assessing Donor Suitability For Blood DonationDokument128 SeitenWHO Guidelines On Assessing Donor Suitability For Blood DonationKiky AN100% (1)
- Taklimat Perubatan Forensik - PENGENALANDokument62 SeitenTaklimat Perubatan Forensik - PENGENALANzahariNoch keine Bewertungen
- Experienced Pharmaceutical Sales LeaderDokument3 SeitenExperienced Pharmaceutical Sales LeaderchadiresidencyNoch keine Bewertungen
- Personality DisordersDokument63 SeitenPersonality DisordersEcel AggasidNoch keine Bewertungen
- MCR FormDokument2 SeitenMCR FormJi Keon LooiNoch keine Bewertungen
- The Geriatric Anxiety Inventory in Primary CareDokument4 SeitenThe Geriatric Anxiety Inventory in Primary CareYudistiro Adi NugrohoNoch keine Bewertungen
- Health Assessment Project Assignment CultureDokument8 SeitenHealth Assessment Project Assignment CultureJennifer PortilloNoch keine Bewertungen
- Aloe Vera as an Alternative Treatment for Wound HealingDokument5 SeitenAloe Vera as an Alternative Treatment for Wound HealingJeffllanoNoch keine Bewertungen
- Bone Marrow Biopsy SheetDokument2 SeitenBone Marrow Biopsy SheetSouvik BairagyaNoch keine Bewertungen
- Toxoplasma Gondii.Dokument21 SeitenToxoplasma Gondii.Sean MaguireNoch keine Bewertungen
- GE - MS Accessories GuideDokument50 SeitenGE - MS Accessories GuidemaruthaiNoch keine Bewertungen
- Passive Movements PDFDokument18 SeitenPassive Movements PDFIndrajith Liyanage100% (8)
- JADWAL PELATIHAN IhcaDokument1 SeiteJADWAL PELATIHAN Ihcalilik ari prasetyoNoch keine Bewertungen
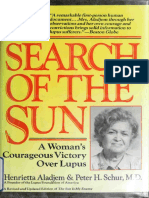
- Aladjem - The Sun Is My Enemy - in Search of The Sun - A Woman's Courageou - Aladjem, Henrietta, 1917 (Orthomolecular Medicine)Dokument310 SeitenAladjem - The Sun Is My Enemy - in Search of The Sun - A Woman's Courageou - Aladjem, Henrietta, 1917 (Orthomolecular Medicine)Anonymous gwFqQcnaX100% (1)