Beruflich Dokumente
Kultur Dokumente
Selection of Dissolution
Hochgeladen von
GirishCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Selection of Dissolution
Hochgeladen von
GirishCopyright:
Verfügbare Formate
Dissolution Concepts and Applications.
Gregory P. Martin and Vivian A. Gray
Selection of Dissolution
Medium for QC Testing
of Drug Products
Gregory P. Martin and Vivian A. Gray
Dissolution Concepts and Applications provides a
forum for sharing information about topics associated with in vitro dissolution testing. Our objective
for this feature: Useful and practical information
applicable to daily work situations.
Reader comments, questions, and suggestions
are needed to help us fulfill the column objective.
Please send your comments and suggestions to column coordinators Vivian Gray at vagray@rcn.com
or Greg Martin at greg.martin@complectors.com,
or to managing editor Susan Haigney at shaigney@
advanstar.com.
KEY POINTS
The following key points are discussed:
Selection of the dissolution medium to be used
for quality control dissolution testing is the most
critical part of dissolution method development.
The analytical target profile (ATP) and drug substance solubility are key factors in dissolution
medium selection.
The ATP should indicate the type of dosage form
for which the test is being developed.
Drug substance solubility should be characterized
over the physiological range of pH values.
Soluble drugs exhibit good solubility across the
physiological pH range (e.g., sink conditions at
pH 1.2, 4.5, and 6.8 or BCS Class I/III).
Drugs with pH-dependent solubility exhibit adequate solubility (sink conditions) over part, but
not all, of the physiological pH range depending
on the pKa. The dissolution medium selected
for these drugs usually is at the pH that provides
sink conditions.
Poorly soluble drugs often use surfactants to
increase solubility. Surfactants may reduce surface
tension (lower concentrations) or solubilize drugs
via micelle formation at concentrations above the
critical micelle concentration.
Robustness and ruggedness of the dissolution
method should be evaluated. This includes understanding sensitivity of solubility or dissolution
results to changes in pH, solution stability of the
drug in the medium, and other considerations.
Discriminating power of the dissolution test
should be evaluated. This is done by intentionally
introducing changes to the formulation, process,
or other parameters and determining the impact
on dissolution results.
INTRODUCTION
This column previously discussed an overall approach
to the development of dissolution methods. This
discussion addresses the most critical part of that
process: selection of the medium to be used for quality
control (QC) dissolution testing.
ABOUT THE AUTHORS
For more Author
information,
go to
gxpandjvt.com/bios
gxpandjv t.com
Gregory P. Martin is president of Complectors Consulting (www.complectors.com), which provides
consulting and training in the area of pharmaceutical analytical chemistry. He may be contacted at greg.
martin@complectors.com. Vivian A. Gray has spent the last 35 years involved in all aspects of dissolution testing and evaluating new dissolution technology. In 2002, she began a consulting business, V.A.
Gray Consulting, Inc., in dissolution testing and related areas. She may be contacted at vagary@rcn.com.
Journal
of
Validation T echnology [Summer 2011]
Dissolution Concepts and Applications.
While dissolution testing is utilized for a number of
reasons including formulation selection and establishment of an in-vitro in-vivo correlation (IVIVC), by far
the most frequent application is QC testing for release
or stability purposes. And while choice of apparatus or analytical technique for samples may be fairly
straightforward, the choice of dissolution medium can
be very challenging. The dissolution medium must
meet regulatory requirements in a global environment,
balance discriminating ability with robustness, and
lead to development of an appropriate specification.
Prior to embarking on the path to identify an optimal dissolution medium, it is best to have addressed
two major items: analytical target profile (ATP) (1) and
characterization of drug substance solubility. These are
useful for selection of medium. A decision tree will be
presented that may be useful for the selection process.
Subsequent to the initial selection of candidate media,
it is necessary to generate some empirical data with
real samples to evaluate the suitability of the medium
choices. When feasible, it can be a valuable exercise to
conduct additional experiments to evaluate the discriminating ability of the dissolution method, usually
involving some manufacturing variability or stressed
samples. The establishment of acceptance criteria logically follows this sequence of events.
ANALYTICAL TARGET PROFILE
The ATP should indicate the type of dosage form for
which the test is being developed. This may have
significant impact on the selection of medium. For
instance, if the product is intended to have delayed
release (2), a two-media test starting with a low pH
medium (demonstrating lack of release under simulated gastric conditions) followed with a higher pH
medium (simulating intestinal condition) is appropriate. If the product is intended to have extended release
properties, a medium with a higher pH (simulating
intestinal conditions) is appropriate. The ATP should
also address the expectations regarding discriminating
power, which can be useful for evaluating data from
experiments designed to probe that aspect.
SOLUBILITY CHARACTERIZATION
The solubility should be characterized over the physiological range of pH values, generally pH 1.2 to 6.8
for immediate release products, and pH 1.2 to 7.5 for
extended release products (3). It is also useful to identify the pKa value(s) for the drug substance, if there are
any, because ionization can have a profound impact
on aqueous solubility and should be well understood.
8
Journal
of
Validation T echnology [Summer 2011]
When the drug is poorly water soluble, solubility in
surfactant solutions may be investigated (4).
There are a few ways to define poorly soluble. Traditionally with dissolution, the term sink has been
used, with a definition (in recent years) that volume
of medium is at least three times that required to form
a saturated solution (3). Alternatively, the Biopharmaceutics Classification System (BCS) stipulates that the
dose should be soluble in 250 mL (5). The definitions
are similar, and both describe a dissolution system that
is sufficiently dilute so that the dissolution process is
not impeded by saturation of the compound of interest. Sink conditions are generally recommended but
not always required, and non-sink conditions may
lead to greater discrimination.
WATER SOLUBLE DRUGS
Soluble drugs exhibit good solubility across the physiological pH range (e.g., sink conditions at pH 1.2, 4.5,
and 6.8 or BCS Class I/III). The choice of dissolution
medium pH is flexible for these drugs. Also, it is less
likely that the dissolution test will be discriminating
for these drugs.
The pH of the medium should be chosen from
the physiological pH range. Ionic strength of buffers
should be the same as in the United States Pharmacopeia (USP) (6). Note that for some drugs, incompatibility of the drug with certain buffers or salts may
influence the choice of buffer. Water is a potential
choice, although it is not recommended because test
conditions, such as pH and surface tension, can vary
depending on the source of water and may change
during the dissolution test itself due to the influence
of the active and inactive ingredients (4). Dissolution
medium with pH similar to that of a pKa (+/- 1 pH
unit) should be avoided because variation in the degree
of ionization could have an impact on the ruggedness
of the dissolution procedure. Selection of a pH where
the solubility is at a minimum may assist in accomplishing a discriminating method. Solution stability
can be an issue, even if it appears the drug is soluble.
Solution stability in the dissolution medium should
be understood before investing significant effort in
dissolution testing.
When water solubility is good, typically media with
pH of 1.2, 4.5, and 6.8 are starting points for medium
selection. USP buffers (e.g., hydrochloric, acetate, and
phosphate buffers, respectively) are recommended.
Empirical data using manufactured dosage forms
and potential media may be useful for selecting the
actual dissolution conditions. Results, such as the time
iv thome.com
Gregory P. Martin and Vivian A. Gray.
to reach full dissolution or variability between vessels,
may influence the selection of the medium chosen.
During the method development phase, it is often
useful to make visual observations during the dissolution procedure. It is especially important to make
notes when observations among vessels are different
when using the same medium.
It is useful to check the pH both before and after
the dissolution test to assess whether the medium had
sufficient buffer capacity to maintain consistent pH. If
the pH changes during the dissolution test (which may
be due to the properties of the drug substance or the
excipients), consider increasing the buffer concentration, using a different buffer, or using a different pH.
In some cases, the concentration of the USP buffers
(nominally 0.05M) may result in precipitation during
the analysis of the samples, particularly when using
HPLC with a mobile phase with a high percentage of
organic. It is acceptable to reduce the buffer concentration, as long as a consistent pH is maintained during
the dissolution test. Changes in the concentration of
the buffer may result in changes in the dissolution rate.
When dissolution is rapid (>80% dissolved in 15
minutes) at the three pH values mentioned, it may
be possible to use disintegration instead of dissolution. A decision tree in International Conference on
Harmonisation (ICH) Q6 permits this if a relationship
can be established between dissolution and disintegration results.
If the product is being developed for global marketing, it may be prudent to avoid acidic conditions (e.g.,
pH 1.2 or simulated gastric fluid) due to a preference
of the Japanese regulators to avoid this condition (7).
DRUGS WITH
pH-DEPENDENT SOLUBILITY
Drugs with pH-dependent solubility exhibit adequate
solubility (sink conditions) over part, but not all, of
the physiological pH range. The dissolution medium selected for these drugs usually is at the pH that
provides sink conditions. Knowledge of the pKa, the
impact of pKa on the solubility, and the ruggedness
of the dissolution procedure must be considered.
In this situation, start with conditions where sink
conditions have been demonstrated (usually one or
two of the initial target values of pH 1.2, 4.5, or 6.8).
It often makes sense to investigate intermediate pH
values. Where solubility increases with increasing pH,
buffers with pH up to 8.0 may be selected, if justified
(i.e., the ATP requirements are not met at pH below
pH 6.8, but are met at higher pH).
gxpandjv t.com
As in the case of water-soluble drugs, once candidate pH values have been identified, empirical data
and visual observations are useful for selecting the
final medium conditions for the dissolution procedure. The probability of identifying a discriminating
dissolution procedure is greater than in the case of
a water-soluble drug. Experiments for evaluating
ability to discriminate are described later in this
discussion.
POORLY WATER-SOLUBLE DRUGS
The incidence of new drug candidates that are poorly water-soluble has been increasing. A variety of
approaches to solubilize these drugs including nanoformulations, hot-melt extrusion, and oil-filled soft
gelatin capsules (8) are being used. These formulations
create a challenge for choosing a dissolution medium.
Addition of surfactants is often used to increase
solubility. Sodium dodecyl sulfate (SDS) and polysorbate 80 (Tween 80) have been used most frequently.
A number of other surfactants have also been used (9,
10). The US Food and Drug Administration discourage
the use of hydroalcoholic media (4). A recent search
of USP monographs indicated over 60 monographs
that use SDS as a dissolution medium, and at least
20 monographs that use polysorbate 80 (11). Endogenous surfactants, including sodium taurocholate
and sodium deoxycholate, have been used for some
biorelevant dissolution procedures (12). These are
generally not appropriate for a quality control application due to cost and difficulty in preparation. Global considerations can influence choice of medium.
Japanese regulators have been known to favor use of
polysorbate 80 for poorly water-soluble compounds,
as described in their guideline for bioequivalence of
generic products (13).
When using surfactants, several parameters must be
investigated. Select the lowest concentration that meets
the requirements of the ATP (typically >80% within a
specified time frame, and acceptable reproducibility).
As with aqueous solutions, control of pH can be critical. There may be effects of counter-ions or pH on the
solubility or solution stability of the surfactant solutions.
There are two mechanisms by which surfactants can
enhance dissolution results: reduction of surface tension
(at lower concentrations) or solubilization via micelle
formation at concentrations above the critical micelle
concentration (CMC). For dissolution of poorly watersoluble compounds, typically concentrations above the
CMC are employed. The Table lists the CMC concentration for typical surfactants used in dissolution testJournal
of
Validation T echnology [Summer 2011]
Dissolution Concepts and Applications.
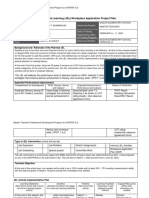
Table: Critical micelle concentrations
of common surfactants.
Name
CMC (% wt/volume)
Sodium dodecyl sulfate (SDS,
sodium lauryl sulfate, SLS)
0.23% (14)
Polysorbate 80 (Polyoxyethylene 80) sorbitan monooleate,
Tween 80)
0.002% (15)
Cetyltrimethyl ammonium
bromide (CTAB, hexadecyltrimethylammonium bromide)
0.04% (14)
ing. However, if the drug substance or drug product has
poor wetability, then using surfactants at relatively low
concentrations (below CMC) to reduce surface tension
may be successful in improving dissolution results. Normally, the lowest effective concentration is used for the
dissolution procedure, based on empirical results using
manufactured dosage forms.
Experience has demonstrated that it is important to
control the grade and consistency of surfactants used
for dissolution testing. For example, SDS is available in
both a technical grade and a high purity grade; also, the
source of polysorbate 80 can affect its suitability when
using a chromatographic determination.
EVALUATION OF
ROBUSTNESS AND RUGGEDNESS
A phase-appropriate approach to evaluation of variability in dissolution testing is recommended. Early
in development, when there is relatively little experience with the dissolution method, results are generally accepted at face value. However, as development progresses, it is well recognized that issues with
robustness and ruggedness are not uncommon. These
may have profound effects, including additional testing and potential generation of out-of-specification
results. For these reasons, it is prudent to understand
the potential impact of variability as early in development as practical. This should include understanding sensitivity of solubility or dissolution results
to changes in pH around the value chosen for the
medium. Solution stability of the drug in the medium
and stability of the dissolution medium itself must
be understood. Apparatus-to-apparatus and batch-tobatch effects should also be evaluated. The impact of
storage conditions on the dissolution characteristics of
the dosage form should be studied. It may be feasible
to reduce variability in dissolution results by choosing
an alternative dissolution medium.
10
Journal
of
Validation T echnology [Summer 2011]
EVALUATION OF
DISCRIMINATING POWER
Having selected a dissolution medium or a few candidates for dissolution media, it is often useful to
probe the discriminating power of the dissolution test.
Regulators are often interested in knowing whether
the dissolution medium is capable of discriminating between good and poor batches. In an ideal
world, batches with acceptable and unacceptable
characteristics in patients would be available, and
the evaluation straightforward. This is rarely the case.
Nonetheless, to probe the discriminating power of the
dissolution procedure, in addition to evaluating the
robustness and ruggedness of the procedure, it may
be useful to intentionally introduce changes to the
formulation. This may be accomplished by modifying
the manufacturing process or by stressing samples
in a manner that is more intense than typical stability testing. For example, manufacturing parameters
such as compression force or formulation lubricant
levels might be varied and the impact on dissolution
results determined. This type of data may be valuable as justification of dissolution conditions in the
regulatory filing.
CONCLUSIONS
Selection of dissolution medium is a multi-step process. Early steps include identification of the requirements in the ATP and characterizing the solubility and
pKa(s) of the drug substance. With this information in
hand, selection of candidate media that exhibit sink
conditions can be undertaken. Final selection of the
actual medium for the test is based on empirical data
using dissolution results from manufactured dosage
forms in the various candidate media. This process is
enhanced when visual observations are made. When
appropriate for the phase of development, additional
data demonstrating robustness, ruggedness, and discriminatory power can be used to refine the selection
of the medium.
REFERENCES
1. Nethercote, P., Borman, P., Bennett, T., Martin, G.P.,
McGregor, P., QbD for Better Method Validation and
Transfer, Pharmaceutical Manufacturing, 37-49, April
2010.
2. USP, General Chapter 711 Dissolution, USP 34-NF 29,
May 2011.
3. USP, General Chapter 1092 The Dissolution Procedure
Development and Validation, USP 34-NF 29, May 2011.
iv thome.com
Gregory P. Martin and Vivian A. Gray.
4. FDA, Guidance for Industry Dissolution Testing of Immediate Release Solid Oral Dosage Forms, FDA, CDER, August
1997.
5. Amidon G. L., Lennerns H., Shah V. P., Crison J. R.,
A Theoretical Basis For A Biopharmaceutic Drug Classification: The Correlation of In Vitro Drug Product
Dissolution and In Vivo Bioavailability, Pharm Res.;
12(3):413420, 1995.
6. USP, Buffer Solutions, USP 34-NF 29, May 2011.
7. Vivian Gray, Meeting Report: University of Wisconsin/
AAPS/FDA Workshop-Applied Biopharmaceutics and
Quality by Design for Dissolution/Release Specification
Stting: Product Quality for Patient Benefit, Dissolution
Technologies, November 2009.
8. K. Gowthamarajan1 and Sachin Kumar Singh, Dissolution Testing for Poorly Soluble Drugs: A Continuing Perspective, Dissolution Technologies, 24-32, August
2010.
9. Carol Noory, Nhan Tran, Larry Ouderkirk, and Vinod
Shah, Steps for Development of a Dissolution Test for
Sparingly Water-Soluble Drug Products, American Pharmaceutical Review, 16-21, Winter 2002.
10. Cynthia K. Brown, Hitesh P. Chokshi, Beverly Nickerson, Robert A. Reed, Brian R. Rohrs, and Pankaj A.
Shah, Acceptable Analytical Practices for Dissolution
Testing of Poorly Soluble Compounds, Pharmaceutical
Technology, 56-65, December 2004.
11. USP, USP 34-NF 29, May 2011.
12. R aimar L benberg , Johannes K rmer, Vinod P.
Shah,Gordon L. Amidon and Jennifer B. Dressman,
Dissolution Testing as a Prognostic Tool for Oral Drug
Absorption: Dissolution Behavior of Glibenclamide,
Pharmaceutical Research, Vol. 17, No. 4, 2000.
gxpandjv t.com
13. NIHS, Guideline for Bioequivalence Studies of Generic
Products, National Institute of Health Sciences (NIHS),
Japan.
14. P. Mukerjee and K. J. Mysels, Critical Micelle Concentration of Aqueous Surfactant Systems, NSRDS-NBS
36, US. Government Printing Office, Washington, D.C.,
1971.
15. Chou DK, Krishnamurthy R, Randolph TW, Carpenter
JF, Manning MC, Effects of Tween 20 and Tween 80 on
the stability of Albutropin during agitation, J Pharm Sci
94 (6): 136881, June 2005. JVT
ARTICLE ACRONYM LISTING
ATP
BCS
CMC
FDA
ICH
IVIVC
pKa
QC
SDS
USP
Analytical Target Profile
Biopharmaceutics Classification System
Critical Micelle Concentration
US Food and Drug Administration
International Conference on Harmonisation
In Vitro In Vivo Correlation
(Acid) dissociation constant or ionization
constant
Quality Control
Sodium Dodecyl Sulfate
United States Pharmacopeia
Journal
of
Validation T echnology [Summer 2011]
11
Das könnte Ihnen auch gefallen
- Oral Controlled Release Formulation Design and Drug Delivery: Theory to PracticeVon EverandOral Controlled Release Formulation Design and Drug Delivery: Theory to PracticeHong WenNoch keine Bewertungen
- 1088 in Vitro & in Vivo Evaluation of Dosage Forms - USP 36 PDFDokument10 Seiten1088 in Vitro & in Vivo Evaluation of Dosage Forms - USP 36 PDFKarlaBadongNoch keine Bewertungen
- Propofol - Injectable Injection - RLD 19627 - RC06-16 PDFDokument3 SeitenPropofol - Injectable Injection - RLD 19627 - RC06-16 PDFAhmed SalehinNoch keine Bewertungen
- Development and Validation of Dissolution ProceduresDokument7 SeitenDevelopment and Validation of Dissolution ProceduresVenkatesh KoppuNoch keine Bewertungen
- Patel Riddhiben M., Patel Piyushbhai M., Patel Natubhai MDokument9 SeitenPatel Riddhiben M., Patel Piyushbhai M., Patel Natubhai Msandriss-2Noch keine Bewertungen
- Forced Degradation StudiesDokument9 SeitenForced Degradation Studiesppiccolini100% (1)
- Regulatory Aspects of Pharmaceutical Quality System: Brief IntroductionVon EverandRegulatory Aspects of Pharmaceutical Quality System: Brief IntroductionNoch keine Bewertungen
- Use and Limitations of in Vitro Dissolution Testing: Topic Introduction and OverviewDokument114 SeitenUse and Limitations of in Vitro Dissolution Testing: Topic Introduction and OverviewMuthu Venkatesh100% (1)
- CMCDokument3 SeitenCMCSri harsha reddyNoch keine Bewertungen
- Bio-Relevant Dissolution MediaDokument30 SeitenBio-Relevant Dissolution Mediavinay_anand50% (2)
- FDA Guidance For CMC For Clinical TrialsDokument27 SeitenFDA Guidance For CMC For Clinical TrialsNelson Alejandro FierroNoch keine Bewertungen
- Industrial Training PRESENTATION (Benazir)Dokument6 SeitenIndustrial Training PRESENTATION (Benazir)Benazir ShuguftaNoch keine Bewertungen
- Quality by Design Approaches For Topical Dermatological Dosage FormsDokument19 SeitenQuality by Design Approaches For Topical Dermatological Dosage FormsDoinița UrsuNoch keine Bewertungen
- Content Uniformity (CU) Testing For The 21st Century CDER PerspectiveDokument36 SeitenContent Uniformity (CU) Testing For The 21st Century CDER PerspectiveRezaul Razib100% (1)
- Bioburden Recovery Method Using Swabbing TechniqueDokument8 SeitenBioburden Recovery Method Using Swabbing TechniquePiruzi MaghlakelidzeNoch keine Bewertungen
- Suppositories SampleDokument20 SeitenSuppositories SamplePriyanka S. SutarNoch keine Bewertungen
- ICH Guidelines IndexDokument5 SeitenICH Guidelines Indexyashpandya01Noch keine Bewertungen
- Biopharmaceutical Classification System and Formulation DevelopmentDokument18 SeitenBiopharmaceutical Classification System and Formulation DevelopmentAshish Mittal100% (1)
- Seminar (Photostability)Dokument12 SeitenSeminar (Photostability)Mr. HIMANSHU PALIWALNoch keine Bewertungen
- Dissolution WHO PresentationDokument64 SeitenDissolution WHO PresentationnkszoneNoch keine Bewertungen
- Limit Test For Heavy MetalsDokument19 SeitenLimit Test For Heavy MetalsnutrimakeNoch keine Bewertungen
- An Overview On Tablet CoatingDokument4 SeitenAn Overview On Tablet Coatingronahaniifah11Noch keine Bewertungen
- Pre-Formulation and FormulationDokument32 SeitenPre-Formulation and FormulationNanaNanakura100% (2)
- Chemistry, Manufacturing and Controls Requirements: Exhibit 1: CMC Requirements For A New PharmaceuticalDokument3 SeitenChemistry, Manufacturing and Controls Requirements: Exhibit 1: CMC Requirements For A New PharmaceuticalPranav Patel100% (1)
- Factors Affecting Drug Dissolution RatesDokument25 SeitenFactors Affecting Drug Dissolution RatesYuppie Raj100% (1)
- GMPs Workshop - Analytical Method Validation (Regulatory Perspective - Linda NG, FDA)Dokument31 SeitenGMPs Workshop - Analytical Method Validation (Regulatory Perspective - Linda NG, FDA)Helena DordioNoch keine Bewertungen
- SC I E. Dissolution Testing of Solid Oral Dosage FormsDokument4 SeitenSC I E. Dissolution Testing of Solid Oral Dosage FormsCioroiu BogdanNoch keine Bewertungen
- Phospholipid-Based Matrix Effects in LC-MS Bioana Lysis: DitorialDokument4 SeitenPhospholipid-Based Matrix Effects in LC-MS Bioana Lysis: DitorialrostaminasabNoch keine Bewertungen
- Workshop - Specifications in Early Development (Regulatory Perspective-Stephen Miller, FDA)Dokument30 SeitenWorkshop - Specifications in Early Development (Regulatory Perspective-Stephen Miller, FDA)lhthang1990Noch keine Bewertungen
- DEC Study in Formulation DevelopmentDokument9 SeitenDEC Study in Formulation Developmentfad12345Noch keine Bewertungen
- Biopharmaceutical Considerations in Drug Product Design and in Vitro Introduction (Biopharm)Dokument22 SeitenBiopharmaceutical Considerations in Drug Product Design and in Vitro Introduction (Biopharm)vipinkv99Noch keine Bewertungen
- Quality by Design For Biotechnology Products-Part 2 - Process Development ForumDokument7 SeitenQuality by Design For Biotechnology Products-Part 2 - Process Development ForumGyro9Noch keine Bewertungen
- USP 1086 Impurities in Drug Substances and Drug ProductsDokument3 SeitenUSP 1086 Impurities in Drug Substances and Drug ProductsMuhammad JamilNoch keine Bewertungen
- Foto StabilityDokument14 SeitenFoto StabilityDalton WattsNoch keine Bewertungen
- Quality by Design For ANDAs - MR TabletsDokument161 SeitenQuality by Design For ANDAs - MR TabletsShilpa Kotian100% (1)
- Microbiological Pharmaceutical Quality Control LabsDokument7 SeitenMicrobiological Pharmaceutical Quality Control LabsDede Kizzy BlackNoch keine Bewertungen
- Impurity ProfileDokument17 SeitenImpurity ProfileNishit SuvaNoch keine Bewertungen
- Analytical Methods Transfer ConsiderationsDokument26 SeitenAnalytical Methods Transfer ConsiderationsamolNoch keine Bewertungen
- Biopharmaceutics Classification SystemDokument3 SeitenBiopharmaceutics Classification SystemAnti MariantiNoch keine Bewertungen
- Unit 8 High Performance Liquid Chromatography HPLCDokument57 SeitenUnit 8 High Performance Liquid Chromatography HPLCNathanianNoch keine Bewertungen
- Alternative Methods for Real-Time Microbiological Quality ControlDokument10 SeitenAlternative Methods for Real-Time Microbiological Quality ControlLEPESANTNoch keine Bewertungen
- OriginalDokument32 SeitenOriginalAlexandra MilenkovicNoch keine Bewertungen
- QBD Approach To Dissolution Through Understanding of The Release Mechanisms and Critical in Vivo ParametersDokument61 SeitenQBD Approach To Dissolution Through Understanding of The Release Mechanisms and Critical in Vivo Parametersvg_vvgNoch keine Bewertungen
- FDS StudyDokument8 SeitenFDS StudyAnnisaIndahPNoch keine Bewertungen
- Fda'S Question-Based Review (QBR) : A Risk-Based Pharmaceutical Quality Assessment ToolDokument50 SeitenFda'S Question-Based Review (QBR) : A Risk-Based Pharmaceutical Quality Assessment Toollalooprasad15Noch keine Bewertungen
- Formulation Development of Albendazole-Loaded Self PDFDokument20 SeitenFormulation Development of Albendazole-Loaded Self PDFDiah100% (1)
- 〈56〉 Methods for Determination of Resistance of Microorganisms to Sterilization ProcessesDokument4 Seiten〈56〉 Methods for Determination of Resistance of Microorganisms to Sterilization Processesjafranco.tfs100% (1)
- FDA Draft Guidance on Dexamethasone; Tobramycin Ophthalmic Suspension StudiesDokument5 SeitenFDA Draft Guidance on Dexamethasone; Tobramycin Ophthalmic Suspension Studiesjaiminrshah1990Noch keine Bewertungen
- FDA Perspective - QBD Considerations For Analytical MethodsDokument20 SeitenFDA Perspective - QBD Considerations For Analytical MethodssamxuNoch keine Bewertungen
- Pharmaceutical EngineringDokument24 SeitenPharmaceutical EngineringKedai Kado UnikNoch keine Bewertungen
- Dosage Form Development and CharacterizationDokument74 SeitenDosage Form Development and CharacterizationMuhd Khairul AmriNoch keine Bewertungen
- Stability Studies: Gabriel K. Kaddu Head, Drug Assessment and Registration National Drug Authority UgandaDokument38 SeitenStability Studies: Gabriel K. Kaddu Head, Drug Assessment and Registration National Drug Authority Ugandanajiha0% (1)
- Gradient HPLCDokument20 SeitenGradient HPLCharoonjdasanNoch keine Bewertungen
- Generation and Validation of Standard Operating Procedure For Dissolution ApparatusDokument18 SeitenGeneration and Validation of Standard Operating Procedure For Dissolution ApparatusAbhishek JhaNoch keine Bewertungen
- 31 Slides Final 2-5 - FormulationDevelopment - Solid-OralsDokument32 Seiten31 Slides Final 2-5 - FormulationDevelopment - Solid-OralsmmssNoch keine Bewertungen
- 논문 - A stability-indicating HPLC method for the determination of glucosamine in pharmaceutical formulationsDokument7 Seiten논문 - A stability-indicating HPLC method for the determination of glucosamine in pharmaceutical formulationsjs_kim5781Noch keine Bewertungen
- ICH Quality Guidelines: An Implementation GuideVon EverandICH Quality Guidelines: An Implementation GuideAndrew TeasdaleNoch keine Bewertungen
- STABILITY OF DRUGS: FACTORS AND PRESERVATIONDokument41 SeitenSTABILITY OF DRUGS: FACTORS AND PRESERVATIONLinda ErlinaNoch keine Bewertungen
- HPLC Method DevelopmentDokument26 SeitenHPLC Method DevelopmentsmadhusudansNoch keine Bewertungen
- FDA Orange Book Preface Provides Drug Approval Process DetailsDokument15 SeitenFDA Orange Book Preface Provides Drug Approval Process DetailsGirishNoch keine Bewertungen
- FDA Guide To Investigate OOSDokument13 SeitenFDA Guide To Investigate OOSGirishNoch keine Bewertungen
- Us 7563930Dokument13 SeitenUs 7563930GirishNoch keine Bewertungen
- FDA Guide To Investigate OOSDokument13 SeitenFDA Guide To Investigate OOSGirishNoch keine Bewertungen
- Ep 05012919 Nwa 1Dokument11 SeitenEp 05012919 Nwa 1GirishNoch keine Bewertungen
- QbD Approach for Developing Generic Immediate-Release Acetriptan TabletsDokument107 SeitenQbD Approach for Developing Generic Immediate-Release Acetriptan TabletsDaniela CerianiNoch keine Bewertungen
- Onsemi ATX PSU DesignDokument37 SeitenOnsemi ATX PSU Designusuariojuan100% (1)
- The Forty Nine StepsDokument312 SeitenThe Forty Nine Stepsoldnic67% (3)
- Science of Happiness Paper 1Dokument5 SeitenScience of Happiness Paper 1Palak PatelNoch keine Bewertungen
- Discrete Mathematics - Logical EquivalenceDokument9 SeitenDiscrete Mathematics - Logical EquivalenceEisha IslamNoch keine Bewertungen
- Pin Block Formats Explained in DetailDokument3 SeitenPin Block Formats Explained in DetailJinay SanganiNoch keine Bewertungen
- People vs. LorenzoDokument8 SeitenPeople vs. LorenzoMRose SerranoNoch keine Bewertungen
- ASBMR 14 Onsite Program Book FINALDokument362 SeitenASBMR 14 Onsite Program Book FINALm419703Noch keine Bewertungen
- BUMANGLAG - CLASS D - JEL PlanDokument3 SeitenBUMANGLAG - CLASS D - JEL PlanMAUREEN BUMANGLAGNoch keine Bewertungen
- Comprehension Used ToDokument2 SeitenComprehension Used TomarialecortezNoch keine Bewertungen
- Sri Dakshinamurthy Stotram - Hindupedia, The Hindu EncyclopediaDokument7 SeitenSri Dakshinamurthy Stotram - Hindupedia, The Hindu Encyclopediamachnik1486624Noch keine Bewertungen
- H-1 Nationalism in Europe NotesDokument5 SeitenH-1 Nationalism in Europe Noteskanishk kumarNoch keine Bewertungen
- Sengoku WakthroughDokument139 SeitenSengoku WakthroughferdinanadNoch keine Bewertungen
- The Art of Woodworking Shaker FurnitureDokument147 SeitenThe Art of Woodworking Shaker Furnituremalefikus100% (2)
- 14-15 TDP HandbookDokument28 Seiten14-15 TDP Handbookapi-266268398Noch keine Bewertungen
- Bob Jones - Science 4Dokument254 SeitenBob Jones - Science 4kage_urufu100% (4)
- Infanrix Hexa RSMKL July 2023Dokument37 SeitenInfanrix Hexa RSMKL July 2023Bayu KurniawanNoch keine Bewertungen
- Universitas Alumni Psikotest LolosDokument11 SeitenUniversitas Alumni Psikotest LolosPsikotes BVKNoch keine Bewertungen
- EY The Cfo Perspective at A Glance Profit or LoseDokument2 SeitenEY The Cfo Perspective at A Glance Profit or LoseAayushi AroraNoch keine Bewertungen
- Telesure Mock 8Dokument13 SeitenTelesure Mock 8Letlhogonolo RatselaneNoch keine Bewertungen
- PIC16 F 1619Dokument594 SeitenPIC16 F 1619Francisco Martinez AlemanNoch keine Bewertungen
- AwsDokument8 SeitenAwskiranNoch keine Bewertungen
- DRR Module 4 Detailed Lesson PlanDokument8 SeitenDRR Module 4 Detailed Lesson PlanFe Annalie Sacal100% (2)
- Raman Spectroscopy: 1 Theoretical BasisDokument9 SeitenRaman Spectroscopy: 1 Theoretical BasisJèManziNoch keine Bewertungen
- The Perfect Prayer by by Jon Courson - Matthew 6 9-13 The Lords PrayerDokument6 SeitenThe Perfect Prayer by by Jon Courson - Matthew 6 9-13 The Lords PrayerRobert Beaupre100% (1)
- Levenbach Causal2017Dokument15 SeitenLevenbach Causal2017Jenna GrantNoch keine Bewertungen
- Ashe v. Swenson, 397 U.S. 436 (1970)Dokument25 SeitenAshe v. Swenson, 397 U.S. 436 (1970)Scribd Government DocsNoch keine Bewertungen
- Team Fornever Lean 8 Week Strength and Hypertrophy ProgrammeDokument15 SeitenTeam Fornever Lean 8 Week Strength and Hypertrophy ProgrammeShane CiferNoch keine Bewertungen
- HCF and LCMDokument3 SeitenHCF and LCMtamilanbaNoch keine Bewertungen
- Introduction To Vitamin C, (Chemistry STPM)Dokument2 SeitenIntroduction To Vitamin C, (Chemistry STPM)NarmeenNirmaNoch keine Bewertungen
- We Don't Eat Our: ClassmatesDokument35 SeitenWe Don't Eat Our: ClassmatesChelle Denise Gumban Huyaban85% (20)