Beruflich Dokumente
Kultur Dokumente
Test Yourself Anaesthesiology
Hochgeladen von
Ho Yong WaiCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Test Yourself Anaesthesiology
Hochgeladen von
Ho Yong WaiCopyright:
Verfügbare Formate
Test Yourself !
1.1 Describe three methods of assessing a patients exercise capacity preoperatively.
1.2 Describe the bedside assessments that you could use to try and predict difficulty with
tracheal intubation.
1.3 Describe the characteristics that define each of the ASA grades. What ASA grade would you assign to a 67year-old woman with type II diabetes, hypertension, a BMI of 38 and exercise tolerance of 100m on the flat and
why?
1.4 In the preoperative assessment clinic, what investigations would you do on a 70-year-old woman, with
controlled hypertension and COPD from smoking 20 cigarettes per day for 50 years, who is scheduled for a total
hip replacement and why?
1.5 A 43-year-old woman seen in the clinic prior to having a laparoscopic cholecystectomy is assessed as being
ASA II due to well controlled hypertension. She asks what are the risks of having a general anaesthetic? What
would you tell her?
Mild or early:
circumoral paraesthesia;
numbness of the tongue;
visual disturbances;
lightheadedness;
slurred speech;
twitching;
restlessness;
mild hypotension and bradycardia.
Severe or late:
grand mal convulsions followed by coma:
respiratory depression and eventually apnoea;
cardiovascular collapse with profound hypotension
and bradycardia;
_ cardiac arrest.
_
_
_
_
_
_
_
_
_
_
_
_
_
Management of LAST
Stop giving the local anaesthetic immediately,
get help;
Maintain the airway using basic techniques.
Tracheal intubation will be needed if the
protective reflexes are absent to protect against
aspiration;
Give oxygen (100%) with support of ventilation
if inadequate;
Raise the patients legs to encourage venous
return and start an IV infusion of crystalloid or
colloid. Treat a bradycardia with IV atropine;
Treat convulsions with diazepam 510mg IV.
If the patient has a cardiac arrest, start lipid emulsion
therapy:
give 1.5 mL/kg 20% lipid emulsion (approximately
100 ml) over 1 min;
start an infusion of 20% lipid emulsion at a rate of
15 mL/kg/h.
Prevention of LAST
TABLE 1. Recommendations for Preventing LAST
& There is no single measure that can prevent LAST in clinical
practice.
& Use the lowest effective dose of local anesthetic (dose = product
of volume _ concentration) (I, C).
& Use incremental injection of local anestheticsVadminister 3- to
5-mL aliquots, pausing 15Y30 secs between each injection.
When using a fixed needle approach, eg, landmark,
paresthesia-seeking, or electrical stimulation, time between
injections should encompass 1 circulation time (30Y45 secs);
however, this ideal may be balanced against the risk of needle
movement between injections. Circulation time may be increased
with lower-extremity blocks. Use of larger dosing increments
would dictate the need for longer intervals to reduce the
cumulative dose from stacked injections before an event of LAST.
Incremental injection may be less important with ultrasound
guidance, given that frequent needle movement is often used
with the technique (I, C).
& Aspirate the needle or catheter before each injection, recognizing
that there is 2% false-negative rate for this diagnostic
intervention (I, C).
& When injecting potentially toxic doses of local anesthetic, use of
an intravascular marker is recommended. Although epinephrine
is an imperfect maker and its use is open to physician judgment,
its benefits likely outweigh its risks in the majority of patients
(IIa, B):
) Intravascular injection of epinephrine 10Y15 Kg/mL in adults
produces a Q10-beat HR increase or a Q15Ymm Hg SBP
increase in the absence of A-blockade, active labor, advanced
age, or general/neuraxial anesthesia.
) Intravascular injection of epinephrine 0.5 Kg/kg in children
produces a Q15Ymm Hg increase in SBP.
) Appropriate subtoxic doses of local anesthetic can produce
subjective symptoms of mild systemic toxicity (auditory
changes, excitation, metallic taste, etc) in unpremedicated
patients.
) Fentanyl 100 Kg produces sedation if injected intravascularly
in laboring patients.
& Ultrasound guidance may reduce the frequency of intravascular
injection, but actual reduction of LAST remains unproven in
humans. Individual reports describe LAST despite the use of
ultrasound-guided regional anesthesia. The overall effectiveness
of ultrasound guidance in reducing the frequency of LAST
remains to be determined (IIa, C).
Das könnte Ihnen auch gefallen
- Obs History MandarinDokument1 SeiteObs History MandarinHo Yong WaiNoch keine Bewertungen
- Dengue CaseDokument4 SeitenDengue CaseHo Yong WaiNoch keine Bewertungen
- Dengue CaseDokument4 SeitenDengue CaseHo Yong WaiNoch keine Bewertungen
- Dengue CaseDokument4 SeitenDengue CaseHo Yong WaiNoch keine Bewertungen
- Cerebellar SyndromeDokument2 SeitenCerebellar SyndromeHo Yong WaiNoch keine Bewertungen
- Approach To The Patient With Dysphagia PDFDokument7 SeitenApproach To The Patient With Dysphagia PDFHo Yong Wai100% (1)
- Approach To The Patient With Dysphagia PDFDokument7 SeitenApproach To The Patient With Dysphagia PDFHo Yong Wai100% (1)
- Department Coordinator BioDokument1 SeiteDepartment Coordinator BioHo Yong WaiNoch keine Bewertungen
- Bipolar DisorderDokument1 SeiteBipolar DisorderHo Yong WaiNoch keine Bewertungen
- HivDokument1 SeiteHivHo Yong WaiNoch keine Bewertungen
- Paediatrics at A GlanceDokument2 SeitenPaediatrics at A GlanceHo Yong WaiNoch keine Bewertungen
- Taking A Gynaecological HistoryDokument21 SeitenTaking A Gynaecological Historyasif_siddiqui_2100% (1)
- Ob-Gyn Clinical Cases (From Apgo Site)Dokument221 SeitenOb-Gyn Clinical Cases (From Apgo Site)jamieNoch keine Bewertungen
- Part 1Dokument18 SeitenPart 1Ho Yong WaiNoch keine Bewertungen
- Common Long Cases IM Sem 7Dokument3 SeitenCommon Long Cases IM Sem 7Ho Yong WaiNoch keine Bewertungen
- Reflective ReportDokument2 SeitenReflective ReportHo Yong WaiNoch keine Bewertungen
- Common ENT ComplaintsDokument9 SeitenCommon ENT ComplaintsHo Yong WaiNoch keine Bewertungen
- BVMDokument3 SeitenBVMHo Yong WaiNoch keine Bewertungen
- CPG Management of Dengue Infection in Adults (Revised 2nd Edition)Dokument68 SeitenCPG Management of Dengue Infection in Adults (Revised 2nd Edition)umiraihana1Noch keine Bewertungen
- HomeworkDokument12 SeitenHomeworkHo Yong WaiNoch keine Bewertungen
- Lesson 3 ReviewDokument4 SeitenLesson 3 ReviewHo Yong WaiNoch keine Bewertungen
- Internal Medicine Venepuncture IM & SC Injection Cannulation ABGDokument1 SeiteInternal Medicine Venepuncture IM & SC Injection Cannulation ABGHo Yong WaiNoch keine Bewertungen
- Lesson 6 ReviewDokument2 SeitenLesson 6 ReviewHo Yong WaiNoch keine Bewertungen
- Lesson 9 ReviewDokument2 SeitenLesson 9 ReviewHo Yong WaiNoch keine Bewertungen
- TBL RheumatologyDokument16 SeitenTBL RheumatologyHo Yong WaiNoch keine Bewertungen
- Lesson 8 ReviewDokument3 SeitenLesson 8 ReviewHo Yong WaiNoch keine Bewertungen
- Lesson 5 ReviewDokument4 SeitenLesson 5 ReviewHo Yong WaiNoch keine Bewertungen
- TBL PaedsDokument10 SeitenTBL PaedsHo Yong WaiNoch keine Bewertungen
- Psy Case DiscussionDokument16 SeitenPsy Case DiscussionHo Yong WaiNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- 1 Introduction Clinical Pharmacy 2Dokument54 Seiten1 Introduction Clinical Pharmacy 2Sajid Hassan GhafoorNoch keine Bewertungen
- Final 2019 Mue Report Vancomycin CTR With GraphsDokument6 SeitenFinal 2019 Mue Report Vancomycin CTR With Graphsapi-493355126Noch keine Bewertungen
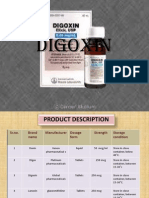
- DigoxinDokument20 SeitenDigoxinAbdulRehmanChaudaryNoch keine Bewertungen
- Stevens-Johnson Syndrome Triggered by A Combination of Clobazam, Lamotrigine and Valproic Acid in A 7-Year-Old ChildDokument6 SeitenStevens-Johnson Syndrome Triggered by A Combination of Clobazam, Lamotrigine and Valproic Acid in A 7-Year-Old ChildFARMASIRSUMAMPANGNoch keine Bewertungen
- Spot 2023 Brochure - FinalDokument3 SeitenSpot 2023 Brochure - FinalMontesqieu SilalahiNoch keine Bewertungen
- Piroxicam StudyDokument4 SeitenPiroxicam StudyRishabh SarawagiNoch keine Bewertungen
- Adrenergic DrugsDokument10 SeitenAdrenergic DrugsMr VoralpenNoch keine Bewertungen
- Pharmaceuticals For Small Animal Internal MedicineDokument11 SeitenPharmaceuticals For Small Animal Internal Medicineahmet öztürkNoch keine Bewertungen
- Dispensing AnsDokument197 SeitenDispensing AnsPrincess Ronsable100% (1)
- Comparison of Double-Flap Incision To Periosteal Releasing Incision For Flap AdvancementDokument8 SeitenComparison of Double-Flap Incision To Periosteal Releasing Incision For Flap AdvancementAnthony LiNoch keine Bewertungen
- Valsartan Recall: Angiotensin Ii Receptor Blockers (Arbs) Equivalent DosingDokument2 SeitenValsartan Recall: Angiotensin Ii Receptor Blockers (Arbs) Equivalent DosingGlory Claudia KarundengNoch keine Bewertungen
- Tranexamic Acid Drug StudyDokument3 SeitenTranexamic Acid Drug Studyswitchlers anneNoch keine Bewertungen
- Polygynax Vaginal CapsuleDokument4 SeitenPolygynax Vaginal Capsuleemmanuelquaye846Noch keine Bewertungen
- Antifungal Drugs: Dr:Samah AlshygiDokument19 SeitenAntifungal Drugs: Dr:Samah AlshygiKhan Khan100% (1)
- The New Advanced Cardiac Life Support GuidelinesDokument52 SeitenThe New Advanced Cardiac Life Support GuidelinesFandy Hazzy AlfataNoch keine Bewertungen
- FArmasi RS Dan Klinik KomprehensifDokument8 SeitenFArmasi RS Dan Klinik Komprehensifklinik dktNoch keine Bewertungen
- Electro Convulsive Therapy APADokument214 SeitenElectro Convulsive Therapy APAastral055356Noch keine Bewertungen
- Pacu Tylenol PresentationDokument10 SeitenPacu Tylenol PresentationStanford AnesthesiaNoch keine Bewertungen
- Placida Plus 0.5 Mg10 MG Tablet - Uses, Side Effects, Substitutes, Composition and More LybrateDokument1 SeitePlacida Plus 0.5 Mg10 MG Tablet - Uses, Side Effects, Substitutes, Composition and More LybrateJuzer SongerwalaNoch keine Bewertungen
- Prelim (Drug Delivery System)Dokument133 SeitenPrelim (Drug Delivery System)Vanessa DL100% (1)
- Research On The Different Pharmacy Setting of Other ASEAN CountriesDokument11 SeitenResearch On The Different Pharmacy Setting of Other ASEAN CountriesAngel Rose GeraldeNoch keine Bewertungen
- Annisa Fitriani-19.008-THE TASK OF MAKING SENTENCESDokument2 SeitenAnnisa Fitriani-19.008-THE TASK OF MAKING SENTENCESAnnisa FitrianiNoch keine Bewertungen
- Exam MarchDokument2 SeitenExam MarchkathlynmangasiNoch keine Bewertungen
- Mag NMM022009Dokument60 SeitenMag NMM022009DanceportugalNoch keine Bewertungen
- Neuromuscular Blocking DrugsDokument5 SeitenNeuromuscular Blocking DrugsTherese Jane TiradorNoch keine Bewertungen
- Daftar Obat: InjeksiDokument3 SeitenDaftar Obat: InjeksiDolsky MessiNoch keine Bewertungen
- Name of Pharmacy: ................................. CityDokument1 SeiteName of Pharmacy: ................................. Cityravi sheladiyaNoch keine Bewertungen
- Claris Life SciencesDokument20 SeitenClaris Life Sciencesten_ishan88Noch keine Bewertungen
- Laporan Penggunaan Februari 2022Dokument7 SeitenLaporan Penggunaan Februari 2022Rara LaveniaNoch keine Bewertungen
- Clinical ToxicologyDokument79 SeitenClinical ToxicologySaddam HossainNoch keine Bewertungen