Beruflich Dokumente
Kultur Dokumente
9220735
Hochgeladen von
Muhammed BarznjiCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
9220735
Hochgeladen von
Muhammed BarznjiCopyright:
Verfügbare Formate
American Journal of Pharmacy and Pharmacology
2014; 1(4): 56-61
Published online December 20, 2014 (http://www.aascit.org/journal/ajpp)
ISSN: 2375-3900
Medication errors in pediatric
hospitals
Darya Omed Nori1, Tavga Ahmed Aziz2,
Saad Abdulrahman Hussain3, *
1
Department of Pharmacy, Sulaimani Pediatric Teaching Hospital, Kurdistan, Iraq
Department of Pharmacology and Toxicology, School of Pharmacy, Faculty of Medical Sciences,
University of Sulaimani, Kurdistan, Iraq
3
Department of Pharmacology and Toxicology, College of Pharmacy, University of Baghdad,
Baghdad, Iraq
2
Email address
saad_alzaidi@yahoo.com (S. A. Hussain)
Keywords
Citation
Pediatrics,
Medication Errors,
Antibiotics,
Prescribing Practice
Darya Omed Nori, Tavga Ahmed Aziz, Saad Abdulrahman Hussain. Medication Errors in
Pediatric Hospitals. American Journal of Pharmacy and Pharmacology.
Vol. 1, No. 4, 2014, pp. 56-61.
Abstract
Received: November 28, 2014
Revised: December 08, 2014
Accepted: December 09, 2014
Background: Drugs are a dualistic therapeutic tool, they are intended to cure, prevent or
diagnose diseases, but improper use leads to patient morbidity or mortality. Aim: The
present study was designed to evaluate medication errors (MEs) in Sulaimani Pediatric
Hospital. Method: Prospective study was performed in Sulaimani Pediatric Teaching
Hospital, Sulaimani City, Kurdistan Region, through which the physician medication
orders for newly admitted patients from 6th February to 10th June 2013 were evaluated
for MEs. A standardized questionnaire (especially adopted for the present study) was
utilized to identify all expected types of MEs that appeared in the follow up sheets of
randomly selected pediatric patients (n=100), admitted to the hospital due to different
causes. Parents, usually mothers, answer some of the questions. 85% MEs were reported
during prescribing practice. Results: They involved medications include bronchodilators
45%, anti-emetics 33%, antibiotics 32%, and analgesics and antipyretics 29%. The most
frequently used antibiotics involved in the MEs were ceftriaxone 24%,
ampicillin+cloxacillin 12% followed by cefotaxime and amikacin. The highest
percentage of errors was 75% belonged to the use of teicoplanin followed by amikacin
60%. Conclusion: The percentages of MEs in Sulaimani Pediatric Hospital are very high,
and there is irrational use of antibiotics. Most of MEs are avoidable utilizing the roles
and activities of clinical pharmacists to provide maximum health care services.
1. Introduction
Drugs are a dualistic therapeutic tool, intended to cure, prevent or diagnose diseases,
but improper use can predispose to patient morbidity and even mortality (1). It is
important to understand the risk factors and causes of pediatric medication errors (MEs)
so that effective reduction strategies can be proposed. Individualized dosing is one of the
causes of pediatric MEs, where doses in the pediatric population are usually calculated
individually, based on the patients age, degree of prematurity in neonates, weight or
body surface area, and clinical condition. This may leads to increased opportunities for
dosing errors (2,3). Many evidences confirm that some healthcare professionals have
difficulty to calculate the correct dose (4-6). This might be complicated by the fact that
57
Darya Omed Nori et al.: Medication Errors in Pediatric Hospitals
many formulations are designed for use in adults, with few
drugs being commercially available in suitable dosage
forms (7), or more importantly, the correct strength for
children. Clinicians should not prescribe for children if they
are not familiar with the pediatric population, and/or the
drugs they are using (8,9). Good communication between
the hospital, the community pharmacy and the medical
practitioner is essential in order to maintain an appropriate
supply of the childs medicine (10). Creating a prescription
is an early step in medication use; therefore, reviewing
orders and prescriptions by pharmacists and nurses is
critical for detecting errors and preventing adverse impacts
on patients. Prescription errors occur at a rate of 3 to 20%
of all prescriptions in hospitalized pediatric patients, and
10.1% of children seen in emergency departments (11).
Accumulating studies suggest that pharmacist interventions
have major impact on reducing MEs in pediatric patients,
thus improving the quality and efficiency of care provided
(12). In traditional hospital practice most of the burden of
drug therapy decision-making falls on the physician.
However, studies have shown that physicians sometimes
make errors in prescribing drugs (13,14). While most errors
are harmless or are intercepted, some may result in adverse
drug events (ADEs). For hospitals with a system of
pediatric clinical pharmacists, the non-intercepted errors
represent the potential risk for patient harm, and would
ideally be targeted by the institution of additional
medication safety systems (computerized physician order
entry, barcoding, and automated dispensing devices) (15).
However, the pharmacists impact might be substantially
great, if he or she could provide input earlier at the time of
prescribing. It has been shown that pharmacist consultation
with physicians and others resulted in reduced drug coast,
provide continuity in individualized pharmaco-therapeutic
care, and serve an important educational function (16). A
recent study of pediatric MEs and ADEs has shown that
pediatric ward-based pharmacists could intercept 94% of
near misses, but this assumption has not yet been
adequately tested [17]. The present study was designed to
evaluate MEs in Sulaimani Pediatric Hospital.
2. Methods
2.1. Study Design and Setting
This was a prospective study performed in Sulaimani
Pediatric Teaching Hospital, Sulaimani City, Kurdistan
Region. The physician medication orders for newly admitted
patients, during a period of four months (6th February to 10th
June, 2013), were evaluated for drugs prescribing errors. The
total capacity of Pediatric hospital was approximately 334
beds (including emergency and neonatal intensive care unit).
The cases were collected in three wards (excluding cases
from emergency and neonatal intensive care unit), which
represent approximately 61% (207 beds) of the hospital. A
standardized questionnaire, especially adopted for the present
study was utilized to identify all the expected types of MEs
appeared in the follow up sheets, which belongs to randomly
selected pediatric patients admitted to the hospital due to
different causes. Parents, usually mothers, answer some of
the questions.
2.2. Main Outcome Measures
The medication orders were hand-written, on daily bases
and whenever an additional order or change is requested, by
the authorized physicians, including rotators, permanents,
and consultants. Information on each patient profile including
age, weight, gender, residency, educational status, diagnosis
upon admission, reason and frequency of admission, any
reported allergies, and a complete medication profile for the
present hospitalization, were reviewed. All of the medication
orders were reported, reviewed and carefully assessed
according to the standard criteria globally followed
elsewhere. After collection of data, the types of prescribed
medication classes and the associated MEs were evaluated, in
addition to the types MEs associated with the prescription of
antibiotics.
3. Results
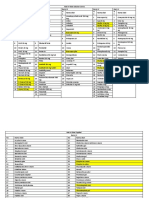
The data indicates that 73% of patients have information
about the orally taken medications and 23% have
information about parenterally administered medications.
Regarding their knowledge about the medication and
disease, only 10% have enough information (Table1).
Figure 1 shows that 55% of the evaluated case sheets
include clear diagnosis of the disease, while 45% of the
case sheets do not. Figure 2 shows that the most frequent
medication classes involved in this study were as follow:
32.4% antibiotics, 17% analgesics, 13.2% I.V. fluids, 9.3%
potassium
chloride,
8.8%
corticosteroids,
5.8%
antihistamines, 5.6% bronchodilators, 3.7% tonics and
vitamins, 2.2% and 2 % anxiolytics and anti-emetics,
respectively. In the current study, evaluation of 587
medication orders revealed the presence of 499 MEs (85%)
(Figure 3). Figure 4 shows the distribution of the selected
cases of pediatric patients according to the educational state
of their parents, in addition to the frequency of hospital
admission and having information about the medication and
diseases. The current study showed that the bronchodilators
represent the medication class with highest reported level of
errors (45%), followed by the antiemetics and antibiotics.
The data also showed that analgesics, antipyretics, and
potassium chloride represent the third level regarding the
reported MEs. Other medication classes involved in
reporting MEs are as follow: anxiolytics 15%,
corticosteroids, tonics and vitamins are 14%, antihistamines
and cough preparations 9%, and IV fluids 8% (Figure 5).
Regarding the errors during the prescription of antibiotics,
figure 6 shows the most frequently prescribed types of
antibiotics, and the percentage of error that occur with each
type.
American Journal of Pharmacy and Pharmacology 2014; 1(4): 56-61
58
Table 1. The information regarding the route of administration of the
prescribed drugs and those related to the disease and type of medications
Rout of
administration
oral
Patient
information
73%
Parenteral
23%
Medication and Disease
No
Few
information information
24%
66%
Enough
information
10%
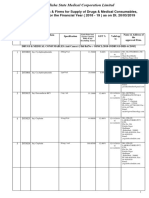
Table 2. The types of prescribing errors reported in the followed pediatric
patients
Type of Error
Omission
Delay in services
Prescription incomplete
Incorrect dose
Incorrect duration
Incorrect dosage form
Drug-drug interaction
Adverse reactions
Allergy and past history information
%
1%
2%
29%
33%
2%
2%
6%
4%
6%
Figure 3. Total Number of prescribing Errors reported in the case sheets
Figure 1. Information regarding diagnosis of the disease in the patients'
case sheets.
Figure 4. The educational statuses of the pediatric patients families, their
information about the disease and medications, frequency of admission and
percentages of medication errors
Figure 2. The classes of frequently prescribed medication that appeared in
case sheets of pediatric patients.
Figure 5. Incidence of medication errors according to the drug classes
involved
59
Darya Omed Nori et al.: Medication Errors in Pediatric Hospitals
Figure 6. Percentages of most frequently prescribed antibiotics and
percentage of errors involved with each type.
Figure 7. State of culture and sensitivity of prescribed antibiotics
4. Discussion
Hospitalized children are more susceptible to prescribing
errors and mistakes made during dosage calculation than
adults, because of their lower body weight and other
physiological characteristics (17). The data of the current
study revealed that 73% of parents have enough information
about the orally administered medications, while only 23%
have such information about parenterally administered
medications. This may be due to their educational status.
Additionally, most of parents had only primary level of
education. Another reason for such finding may be the
inactive role of ward pharmacists, or lack of communications
between the pharmacist and the parents, regarding patient
education about the proper use of medications. There is
evidence from projects, based on analysis of the types of
MEs, that improved communication could potentially reduce
medication-related errors (18,19). Pharmacists and nurses
should check the drug, the dose, patient identity and any
other relevant information before administering medicine.
When a query arises, as to whether the drug should be
administered, the patients or their parents in case of children
should be listened to attentively, and their questions should
be answered; the prescription should be double-checked with
the prescriber (20). Although the ward pharmacists routinely
checked all case sheets included in the present study, MEs
were not identified or corrected. Therefore, the main causes
behind these problems are the absence of appropriate role of
pediatric clinical pharmacist, shortage in number of clinical
pharmacists, work overload, and poor communication
between physician and pharmacists. Recently, a study done
by Fortescue et al. showed that monitoring MEs by a clinical
pharmacist may prevent 58% of all errors, and 72% of
potentially harmful errors; meanwhile, improving physicianpharmacist communication may prevent 47.4% of errors (18).
Other factors that contribute to these problems are children's
low body weight and other physiological characteristics,
which render them more vulnerable than adults to prescribing
errors during dosage calculation. Other factors include
decreased communication abilities of children, inability to
self-administer medications, and the high susceptibility of
young critically ill children to injury from medications,
particularly those with immature renal and hepatic systems
(21). Drug therapies are considered as major component of
pediatric management in health care settings like hospitals.
Effective medical treatment of a pediatric patient is based
upon accurate diagnosis and optimum course of therapy,
which usually involves a medication regimen. Infants and
children are among the most exposed population groups to
contact illnesses. At the same time, infancy and childhood are
periods of rapid growth and development. Most of these are
self-limiting (22) and often treated not only inappropriately,
but also resorting to polypharmacy (23,24). The result of the
current study shows that the most common classes of
medications involved are antibiotics (32.4%), followed by
antipyretics and analgesics (17%), then I.V. fluids (3.2%),
and to lesser extent potassium chloride, corticosteroids,
antihistamines, bronchodilators, tonics and vitamins,
anxiolytics and antiemetics. The percentage of prescribed
antibiotics in the present study is higher than other classes.
Many other studies support this finding, and concluded that
antibiotics are most commonly prescribed drugs to children,
followed by drugs for respiratory ailments or analgesics and
antipyretics (23,25). Other studies reported that 18.5-29% of
the medications used in pediatrics are antimicrobial agents
(26,27). It is important to consider the fact that only 4% of
prescribed antibiotics were prescribed depending on the
results of culture and sensitivity, while 79% were prescribed
without performing culture and sensitivity test. Antibiotics
can be used empirically without awaiting definite
identification of the causative organism after ordering
investigations aimed at making a microbiologically-based
diagnosis (if available and feasible). It is particularly
American Journal of Pharmacy and Pharmacology 2014; 1(4): 56-61
important to send cultures, diligently collected, before the
first dose of any antibiotic is administered except in sick
neonates or intoxicated child, where one cannot wait for
culture reports and need to start antibiotic urgently (28).
Overuse of antibiotics is known to cause drug resistance,
increased side effects and make the treatment expensive
(26,27). Furthermore, in a study conducted in USA, the most
common type of prescription drugs were bronchodilators for
children and central nervous system stimulants for
adolescents (26). The most common medication classes
detected during recording of errors in the present study were
bronchodilators, anti-emetics, antibiotics, antipyretic and
analgesics, respectively. These data are in tune with that
reported by Kaushal et al., where the most common drugs
involved in MEs are anti-infective agents, analgesics and
sedatives, electrolytes and fluids, and bronchodilators (17).
Al-Jeraisy et al., found that error rates are highest in
prescriptions for electrolytes (17.17%), antibiotics (13.72%)
and bronchodilators (12.97%) (29). Meanwhile, Folli et al.
reported that antibiotics are the class of drugs mostly
commonly responsible for dosing errors. Orders for
bronchodilators, analgesics, and fluid and electrolytes were
also frequently predispose to prescribing errors (15).
5. Conclusions
The percentages of MEs in Sulaimani Pediatric Hospital
are very high, and there is irrational use of antibiotics. Most
of MEs are avoidable utilizing the roles and activities of
clinical pharmacists to provide maximum health care services.
Acknowledgement
The authors thank the University of Sulaimani and
Sulaimani Pediatric Hospital for supporting the project.
References
[1]
[2]
[3]
[4]
[5]
[6]
Kohn L, Corrigan J, Donaldson M, (Eds.), To Err Is Human:
Building a Safer Health System. Committee on Quality of
Health Care in America, Institute of Medicine, Washington,
DC, National Academy Press, 1999.
Koren G, Barzilay Z, Greenwald M. Ten-fold errors in
administration of drug doses: a neglected iatrogenic disease in
pediatrics. Pediatrics 1986; 77:848-849.
Koren G, Haslam RH. Pediatric medication errors: predicting
and preventing ten-fold disasters. Journal of Clinical
Pharmacology 1994; 34:1043-1045.
Rowe C, Koren T, Koren G. Errors by pediatric residents in
calculating drug doses. Archive of Disease in Children 1998;
79:56-58.
Glover ML, Sussmane JB. Assessing pediatrics residents
mathematical skills for prescribing medication: a need for
improved training. Academic Medicine 2002; 77:1007-1010.
Gladstone J. Drug administration errors: a study into the
factors underlying the occurrence and reporting of drug errors
in a district general hospital. Journal of Advanced Nursing
60
1995; 22:628-637.
[7]
Yeung YW, Tuleu CL, Wong ICK. National study of
extemporaneous preparations in English paediatric hospital
pharmacies. Pediatric and Perinatal Drug Therapy 2004;
6:75-80.
[8]
Chappell K, Newman C. Potential tenfold drug overdoses on a
neonatal unit. Archive of Diseases in Children, Fetal and
Neonatal Education 2003; 89:F483-484.
[9]
Tan E, Cranswick NE, Rayner CR, et al. Dosing information
for paediatric patients: are they really therapeutic orphans?
Medical Journal Australia 2003; 179:195-198.
[10] Wong ICK, Basra N, Yeung V, et al. Supply problems of
unlicensed and off-label medicines after discharge. Archive of
Disease in Children 2006; 91:686-688.
[11] Lesar TS, Mitchell A, Sommo P. Medication safety in
critically ill children. Clinical Pediatrics and Emergency
Medicine 2006; 7:215-225.
[12] Korin G. Trend of medication errors in hospitalized children.
Journal of Clinical Pharmacology 2002; 42:707-710.
[13] Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse
drug events and potential adverse drug events implications of
prevention. Journal of American Medical Association 1995;
274:29-34.
[14] Leape LL, Bates DW, Cullen DJ, et al. Systemic analysis of
adverse drug events. Journal of American Medical Association
1995; 274:35-43.
[15] Folli HL, Poole RL, Benitz WE, Russo JC. Medication error
prevention by clinical pharmacists in two children's hospitals.
Pediatrics 1987; 79:718-722.
[16] Montazeri M, Cook DJ. Impact of clinical pharmacist in a
multi-disciplinary intensive care unit. Critical Care Medicine
1994; 22:1044-1048.
[17] Kaushal R, Bates DW, Landrigan C, et al. Medication errors
and adverse drug events in pediatric inpatients. Journal of
American Medical Association 2001; 285:2114-2120.
[18] Fortescue EB, Kaushal R, Landrigan CP, et al. Prioritizing
strategies for preventing medication errors and adverse drug
events in pediatric inpatients. Pediatrics 2003; 111:722-729.
[19] Stebbing C, Wong ICK, Kausha R, et al. The role of
communication in pediatric drug safety. Archive of Diseases in
Children 2007; 92:440-445.
[20] Wong ICK, Wong LYL, Cranswick NE. Minimizing
medication errors in children. Archive of Diseases in Children
2009; 94:161-164.
[21] Kaushal R, Jaggi T, Walsh K, Fortescue EB, Bates DW.
Pediatric medication errors. Ambulatory Pediatrics 2004;
4(1):73-81.
[22] Straand J, Rokstad K, Heggedal U. Drug prescribing for
children in general practice: A report from the More and
Romsdal prescription study. Acta Pediatrica 1998; 87:218-224.
[23] Sanz EJ, Bergman U, Dahlstorm M. Pediatric drug prescribing.
European Journal of Clinical Pharmacology 1989; 37:65-68.
[24] Ghai OP, Paul VK. Rational drug therapy in pediatric practice.
Indian Pediatrics 1988; 25:1095-1109.
61
Darya Omed Nori et al.: Medication Errors in Pediatric Hospitals
[25] Neubert A, et al. Databases for pediatric medicine research in
Europe:
assessment
and
critical
appraisal.
Pharmacoepidemiology and Drug Safety 2008; 17:1155-1167.
[28] Yewale VN, Dharmapalan D. Promoting appropriate use of
drugs in children. International Journal of Pediatrics 2012;
10:9065-9070.
[26] Dimri S, Tiwari P, Basu S, Parmar VR. Drug use pattern in
children at a teaching hospital. Indian Pediatrics 2009;
46(2):165-167.
[29] Al-Jeraisy M, Alanazi MQ, Abolfotouh M. Medication
prescribing errors in a pediatric inpatient tertiary care setting
in Saudi Arabia. BMC Research Notes 2011; 4:294.
[27] Khaled A, Sami M, Majed I, Mostafa A. Antibiotic prescribing
in a pediatric emergency setting in central Saudi Arabia. Saudi
Medical Journal 2011; 32(2):197-198.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Dosage Calculations 3 Worksheet 1Dokument6 SeitenDosage Calculations 3 Worksheet 1Ayeza DuaNoch keine Bewertungen
- 10-TCT 2012fyughklDokument196 Seiten10-TCT 2012fyughklMuhammed BarznjiNoch keine Bewertungen
- Pharmacology Questions and AnswersDokument42 SeitenPharmacology Questions and AnswersAnnum BukhariNoch keine Bewertungen
- Transdermal Delivery SystemsDokument58 SeitenTransdermal Delivery SystemsFazrul AlamNoch keine Bewertungen
- Teach ManualDokument78 SeitenTeach ManualShouvik DebnathNoch keine Bewertungen
- DetailedapproaDokument65 SeitenDetailedapproaMuhammed BarznjiNoch keine Bewertungen
- Early MiscarriageretrjytkuyiulDokument6 SeitenEarly MiscarriageretrjytkuyiulMuhammed BarznjiNoch keine Bewertungen
- Respiratory Examination: The Position of The PatientDokument24 SeitenRespiratory Examination: The Position of The PatientMuhammed Barznji100% (1)
- Local AnestheticsgfhgjhkjlkDokument3 SeitenLocal AnestheticsgfhgjhkjlkMuhammed BarznjiNoch keine Bewertungen
- Lung & Thorax Exams: Charlie Goldberg, M.D. Professor of Medicine, UCSD SOMDokument33 SeitenLung & Thorax Exams: Charlie Goldberg, M.D. Professor of Medicine, UCSD SOMMuhammed BarznjiNoch keine Bewertungen
- What Is Gestational Trophoblastic Disease?Dokument42 SeitenWhat Is Gestational Trophoblastic Disease?Muhammed BarznjiNoch keine Bewertungen
- Cranial Nerve Examination: OverviewDokument8 SeitenCranial Nerve Examination: OverviewMuhammed BarznjiNoch keine Bewertungen
- Limb Length DiscrepancyDokument2 SeitenLimb Length DiscrepancyMuhammed BarznjiNoch keine Bewertungen
- Cerebellar ExaminationDokument1 SeiteCerebellar ExaminationMuhammed BarznjiNoch keine Bewertungen
- Crying - Dr. Shwan: Causes?!Dokument2 SeitenCrying - Dr. Shwan: Causes?!Muhammed BarznjiNoch keine Bewertungen
- Respiratory Emergencies in PediatricsDokument49 SeitenRespiratory Emergencies in PediatricsMuhammed BarznjiNoch keine Bewertungen
- Statistics in Drug Research PDFDokument372 SeitenStatistics in Drug Research PDFpromaNoch keine Bewertungen
- A Textbook of Clinical Pharmacology and Therapeutics PDFDokument6 SeitenA Textbook of Clinical Pharmacology and Therapeutics PDFMovie Box MoviesNoch keine Bewertungen
- DR, REDDY LABORATORIES LTD. (Pitch Book)Dokument8 SeitenDR, REDDY LABORATORIES LTD. (Pitch Book)Priya SharmaNoch keine Bewertungen
- Daftar Obat Ranap - MiraRevisiDokument6 SeitenDaftar Obat Ranap - MiraRevisiMiraNoch keine Bewertungen
- Prometric Mcqs Plus CaculationsDokument147 SeitenPrometric Mcqs Plus CaculationsShanaz KhanNoch keine Bewertungen
- Early Drug Discovery ProcessDokument58 SeitenEarly Drug Discovery ProcessFrietzyl Mae Generalao100% (1)
- Lecture 4 170824065306 PDFDokument19 SeitenLecture 4 170824065306 PDFSami SamiNoch keine Bewertungen
- Module 4 - Case Study ReportDokument7 SeitenModule 4 - Case Study ReportAlbert BugasNoch keine Bewertungen
- Berno 2Dokument32 SeitenBerno 2Try AdipradanaNoch keine Bewertungen
- Chap 3. Drug Utilization EvaluationDokument28 SeitenChap 3. Drug Utilization EvaluationAizaz AhmadNoch keine Bewertungen
- Department of Pharmacology Class Routine-April, 2020 (3, 4, 5 & Bds-Semester) Jnims, Porompat ImphalDokument1 SeiteDepartment of Pharmacology Class Routine-April, 2020 (3, 4, 5 & Bds-Semester) Jnims, Porompat ImphalNeerajeigya ManoharNoch keine Bewertungen
- 909-Hazardous Drugs Table - EviqDokument9 Seiten909-Hazardous Drugs Table - EviqMd Al AminNoch keine Bewertungen
- Counter Transfer Vipin MishraDokument6 SeitenCounter Transfer Vipin Mishravipin mishraNoch keine Bewertungen
- Poisons PharmacistsDokument20 SeitenPoisons PharmacistsHenry SpencerNoch keine Bewertungen
- GSKDokument5 SeitenGSKHK KhanNoch keine Bewertungen
- Syllabus IOM B.pharmaDokument56 SeitenSyllabus IOM B.pharmaks0259415Noch keine Bewertungen
- ScriptDokument4 SeitenScriptAlika HNoch keine Bewertungen
- Odisha Rate Contract For MedicinesDokument66 SeitenOdisha Rate Contract For MedicinesSahil KargwalNoch keine Bewertungen
- EMS Result 2Dokument2 SeitenEMS Result 2bhushanNoch keine Bewertungen
- List ABC TestDokument66 SeitenList ABC Testtiwa ramadanNoch keine Bewertungen
- MRM COLLEGE OF PHARMACY 5th Year ClerkshipDokument13 SeitenMRM COLLEGE OF PHARMACY 5th Year ClerkshipkushalNoch keine Bewertungen
- SeLnIkRaj - Ligand ScoutDokument26 SeitenSeLnIkRaj - Ligand ScoutselnikrajNoch keine Bewertungen
- General Molecular Principle in Drug Design: Dr. Rudi Hendra Sy. M.SC., AptDokument27 SeitenGeneral Molecular Principle in Drug Design: Dr. Rudi Hendra Sy. M.SC., AptRifqi Ahmad IrzamiNoch keine Bewertungen
- Pharmacology Course OutlineDokument2 SeitenPharmacology Course OutlineChinedu H. DuruNoch keine Bewertungen
- TetrabenazinaDokument23 SeitenTetrabenazinanieve2010Noch keine Bewertungen
- Paracetamol A Review of Three Routes of AdministrationDokument3 SeitenParacetamol A Review of Three Routes of AdministrationMohd MiqdamNoch keine Bewertungen