Beruflich Dokumente
Kultur Dokumente
Human Papillomavirus, Genital Warts, and Vaccines
Hochgeladen von
Mohammad Al-SalehOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Human Papillomavirus, Genital Warts, and Vaccines
Hochgeladen von
Mohammad Al-SalehCopyright:
Verfügbare Formate
J Microbiol Immunol Infect.
2009;42:101-106
Review Article
Human papillomavirus, genital warts, and vaccines
Po-Ren Hsueh
Divisions of Clinical Microbiology and Infectious Diseases, Departments of Laboratory Medicine and Internal
Medicine, National Taiwan University Hospital, National Taiwan University College of Medicine, Taipei, Taiwan
Received: February 19, 2009 Accepted: February 26, 2009
Human papillomavirus (HPV)related diseases, including cancers, low-grade neoplasia, genital warts, and
recurrent respiratory papillomatosis, have a substantial impact on public health. The increasing incidence of
HPV infection and genital warts highlights the need for an effective strategy for the management of this disease.
Immunization holds the promise of reducing the overall burden of clinical HPV-related diseases. A prophylactic
quadrivalent HPV 6/11/16/18 vaccine is highly effective for reducing the risk of HPV 6, 11, 16, and 18
associated cervical cancer, precancerous cervical lesions, and external genital lesions, including genital warts.
Key words: Condylomata acuminata; Human papillomavirus; Papillomavirus vaccines
Introduction
Human papillomavirus (HPV), a non-enveloped, doublestranded DNA, preferentially infects basal epithelium
through microabrasions and tissue disruption [1,2]. The
association of HPV infections with cervical, anal, vulvar,
vaginal, and oropharyngeal cancers, recurrent respiratory
papillomatosis (RRP), and genital warts (condylomata
acuminata) is well established [1,2]. Transmission of
anogenital HPV-associated diseases primarily occurs
through any activity that involves genital skin or oral
mucosa contact, including genital-to-genital, manual-togenital, or oral-to-genital contact [1,2]. Transmission of
at least some types of anogenital HPV infection is not
limited to penetrative sexual intercourse. HPV can also
be transmitted via non-sexual routes including mother to
newborn (vertical transmission) and fomites [1-3].
Disease Burden
The annual prevalence of HPV infection is estimated
at 1% of the sexually active population in the United
Corresponding author: Dr. Po-Ren Hsueh, Divisions of Clinical
Microbiology and Infectious Diseases, Departments of Laboratory
Medicine and Internal Medicine, National Taiwan University Hospital,
National Taiwan University College of Medicine, No. 7, Chung Shan
South Road, Taipei 100, Taiwan.
E-mail: hsporen@ntu.edu.tw
2009 Journal of Microbiology, Immunology and Infection
States and the incidence is increasing throughout
Europe [2,4-8]. More than 500,000 new cases of
anogenital warts occur every year in the United States,
and the incidence of genital warts is increasing annually [1,2,4]. The rate of new cases of genital warts
increased from 117.8/100,000 population in 1998 to
205.0/100,000 population in 2001 [2]. A report in 2003
indicated that approximately 1.4 million people in the
United States had genital warts [2,4]. The highest rates
of genital warts were noted in individuals aged 20 to
29 years. Approximately 10% of adults will develop
anogenital warts at some point in their lives [1,2,5].
In the United Kingdom, diagnoses of genital warts
increased by approximately 25% between 1996 and
2005 [9]. In 2005, new diagnoses of genital warts
were made at genitourinary medical clinics for approximately 40,000 men and 32,000 women [1,2,9].
The highest rates were concentrated in men aged 20
to 24 years (750/100,000 population), and in women
aged 16 to 19 years (700/100,000 population) and 20
to 24 years (650/100,000 population) [Fig. 1]. Young
people aged 16 to 24 years accounted for 50% of cases
of genital warts in 2007 [1,2,9].
In Spain, the overall annual incidence of genital
warts was estimated at 160.4/100,000 population
[6]. Overall, the prevalence was calculated to be
182.1/100,000 population, corresponding to 56,446
cases annually in the 14- to 64-year-old population.
101
Human papillomavirus, genital warts, vaccines
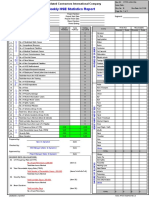
800
No. of patients/100,000 population
700
600
500
400
300
200
100
0
All ages
USA
Men
(20-24 years)
Women
(16-19 years)
Women
(20-24 years)
All ages
France
All ages
Spain
All ages
Taiwan
UK
Population
Fig. 1. Incidence of genital warts in selected countries.
In France, the overall incidence was estimated to be
228.9/100,000 population in women aged 15 to 65
years, corresponding to 47,755 cases managed by gynecologists annually [10].
In Taiwan, the overall incidence of genital warts is
unknown [11-15]. Data from the National Health Insurance Research Database showed that the number of allage patients who had visited urology and obstetrics/
gynecology departments with the diagnosis of genital
warts was 13,287 in 2002 and 14,261 in 2003. It is
estimated that the incidence of genital warts in Taiwan
was 57.8/100,000 population in 2002 and 62.0/100,000
population in 2003. Approximately 70% of these patients were women, with a mean age of 33 years (range,
1 to 94 years). More than 65% of patients were aged 20
to 39 years during 2002 and 2003 (Fig. 2).
Importantly, all of the incidence data from individual countries are likely to underestimate the real
occurrence of genital warts, because this disease is
likely to be underreported [1,2].
Human Papillomavirus Types
More than 100 different HPV types have been identified based on DNA homology, and approximately 40
of them are known to infect the anogenital tract [1].
HPV types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58,
59, 68, 73, and 82 are classified as high-risk types.
102
Among them, HPV 16 and 18 are the most common
causes of infections and cervical cancers throughout
the world. Low-risk HPVs include types 6, 11, 40, 42,
43, 44, 54, 61, 70, 72, 81, and CP6108 [1,2]. Infection
with low-risk types (particularly types 6 and 11) can
result in genital warts [1,2,4,6]. In general, more than
90% of genital warts and RRP are due to HPV types
6 and 11 [1,2]. However, HPV types 16 and 18 are
frequently (60-70%) associated with cervical dysplasia and cervical and colorectal or anorectal cancer.
Twenty five percent of low-grade cervical lesions and
50% of high-grade cervical lesions are associated with
infection by HPV types 16 and 18 [1,2,4,16].
In Taiwan, the 5 most common HPV types by
decreasing frequency for cervical cancer are HPV 16,
18, 58, 33, 52 and, for women with normal cytology,
are HPV 16, 52, 58, 18 and 51 [14]. The prevalences
of HPV in women with abnormal Papanicolaou smear
test results, including atypical squamous cells of unknown significance (ASCUS)/atypical glandular cells
of unknown significance (AGUS)negative histology,
ASCUS/AGUS, low-grade squamous intraepithelial
lesions, high-grade squamous intraepithelial lesions,
and invasive cancer are 33.8%, 38.3%, 74.9%, 84.3%,
and 100%, respectively, with an overall positive rate of
68.8% [14]. The most common HPV types are HPV 16
(18.5%), 52 (16.5%), 58 (13.2%), 33, 51, 53, 18, 39,
59, 66, MM8, and 31 [13-15].
2009 Journal of Microbiology, Immunology and Infection
Hsueh
45
2002 (n = 13,287)
2003 (n = 14,261)
40
Percent of patients
35
30
25
20
15
10
5
0
<20
20-29
30-39
40-49
50-59
60-69
>69
Age (years)
Fig. 2. Age distribution of patients who visited urology and obstetrics/gynecology departments with the diagnosis of
genital warts in 2002 and 2003 in Taiwan. Data obtained from the National Health Insurance Research Database, Taiwan.
A study of HPV in 15 genital condyloma biopsy
specimens by Southern blot hybridization, reported in
1994, found that 12 (80%) of the 15 condyloma specimens contained HPV 6 or 11 sequences [12].
Treatment and Prevention
Although genital warts are not life threatening compared with cervical cancer, they are common and can
have a negative psychological impact [1,2]. The main
causes of concern among men and women with genital
warts include transmission, recurrence, local pain, cervical or penile cancer, and treatment efficacy [1,2,17,18].
Treatment for genital warts can also require multiple
clinic visits for patients, which are associated with
increased cost [5,11,19]. This cost was highest in young
adults (US$1717/1000 person-years for women aged
15 to 24 years, US$1114/1000 person-years for women
aged 25 to 34 years, and US$1692/1000 person-years
for men aged 25 to 34 years) [5].
HPV cannot be eradicated therapeutically, so the
primary treatment aim is removal of symptomatic warts
[17,18]. These therapies include surgical excision, loop
electrosurgical excision, laser treatment, and treatment
with trichloroacetic acid, imiquimod, and podophyllin
[1,17,18]. However, such treatments are often long and
painful, with a high number of recurrent and resistant
cases. Anogenital warts often recur within the first 6
months after initial diagnosis and therefore require
2009 Journal of Microbiology, Immunology and Infection
repeated treatment sessions. In rare instances, anogenital warts become locally invasive and require extensive
surgery for removal [1,2,17,18].
Total abstinence from all genital contact is the
most effective method for preventing HPV infection
[1,2,20]. Lifetime mutual monogamy is also an effective HPV prevention strategy. However, a monogamous
individual is at risk from a non-monogamous partner. In
a study of monogamous women, the risk of acquiring
HPV was 46% at 3 years after first intercourse [1,2].
Condom use, which is essential for the prevention of
other sexually transmitted diseases, reduces, but does
not eliminate, the risk of HPV infection [1,2,5,20].
For natural cervical HPV infection, the immune
response is slow and weak, occurring 6 to 12 months
after viral acquisition and not occurring for all infected
women [1,2,21]. In a study of the relationship between
HPV DNA in the genital mucosa and serum antibodies
to HPV 16, 18, and 6 performed among 588 women,
approximately 40% of women did not develop a measurable response [21]. Furthermore, antibodies against
one HPV type may not protect against subsequent reinfection with the same or another closely related type,
and antibody responses vary with HPV type [21].
Prophylactic Human Papillomavirus Vaccines
Vaccination is currently regarded as one of the most
effective strategies for controlling HPV-related diseases
103
Human papillomavirus, genital warts, vaccines
[22]. A prophylactic quadrivalent HPV vaccine (HPV
6/11/16/18 vaccine [Gardasil; Merck & Co., Inc.,
Whitehouse Station, NJ, USA]) contains virus-like
particle (VLP) viral capsid proteins L1 of HPV types 6,
11, 16, and 18, which are synthesized in Saccharomyces cerevisiae and adsorbed on amorphous aluminum
hydroxyphosphate sulfate adjuvant [23,24]. This HPV
6/11/16/18 recombinant vaccine was first licensed in
the United States in June 2006, and subsequently in
the European Union in September 2006. The vaccine
has been shown to be up to 100% effective in preventing cervical cancer, precancerous cervical lesions, and
external genital lesions, including genital warts. The
presumed prophylactic efficacy of the vaccine against
HPV 6/11/16/18related genital warts was 98.9%,
according to the United States Food and Drug Administration (FDA) in 2008 [23,24].
Another HPV vaccine (HPV16/18 vaccine [Ceravix; GlaxoSmithKline Biologicals, Rixensart, Belgium]), a mixture of VLPs derived from the L1 capsid
proteins of HPV types 16 and 18, is formulated with the
AS04 adjuvant system [25-29]. This HPV16/18 vaccine
was licensed in Taiwan in March 2008 for women aged
10 to 25 years for the prevention of cervical cancer by
protecting against incident and persistent infections,
cervical intraepithelial neoplasia (CIN), and precancerous lesions causally related to HPV types 16 and 18.
The indication is based on demonstration of efficacy in
women aged 15 to 25 years following vaccination with
HPV 16/18 and on the immunogenicity of the vaccine
in girls and women aged 10 to 25 years. However, this
vaccine doesnt provide any protection against genital
warts, which are mainly caused by HPV 6/11 [25-29].
In Taiwan, the quadrivalent, HPV 6/11/16/18
recombinant vaccine has recently received regulatory
approval (in October 2006) for the prevention of cervical carcinoma, high-grade cervical dysplasia (CIN
2/3), low-grade cervical dysplasia (CIN 1), high-grade
vulvar and vaginal dysplasia, and external genital
warts for females aged 9 to 26 years [11].
The United States FDA has not approved the
use of the HPV 6/11/16/18 recombinant vaccine for
boys or men [1,2]. There are currently no published
data demonstrating that the vaccine can protect men
from getting genital warts or developing HPV-related
cancers (such as penile cancer) [1,2]. A randomized,
double-blind, placebo-controlled, phase III study of
the efficacy of HPV 6/11/16/18 recombinant vaccine
for preventing HPV-related external genital disease
(genital warts, penile/perineal/perianal intraepithelial
104
neoplasia or cancer) in men aged 16 to 26 years
(men having sex with men [MSM] and heterosexual
men) with 0 to 5 lifetime partners has been ongoing
globally since 2003 (since 2005 in Taiwan) [1,2].
All participants were given vaccine or placebo at
enrollment, month 2, and month 6, and underwent
detailed anogenital examinations and sampling from
the penis, scrotum, and anal (MSM cohort only)
and perianal regions at enrollment, month 7, and
every 6 months thereafter. The endpoints of this trial
include HPV 6/11/16/18 infection and the incidence
of HPV 6/11/16/18related external genital lesions at
36 months. Preliminary data from this trial of 4065
participants at a mean duration of 29 months followup revealed that the reduction rate (compared with the
placebo group) for all external genital lesions, genital
warts, and penile/perineal/perianal intraepithelial
neoplasia was 90.4% (case no. of vaccine group/case
no. of placebo group, 3/31; p < 0.001), 89.4% (3/29;
p < 0.001), and 100% (0/3), respectively.
A recent cost-effectiveness study using a transmission dynamic model to estimate the long-term epidemiologic and economic consequences of quadrivalent
HPV vaccination was reported in 2008 [11]. Two
vaccination strategies were evaluated, including vaccination of 12-year-old girls and vaccination of 12-yearold girls with a temporary 5-year catch-up vaccination
for girls and women aged 12 to 24 years [11]. This
study revealed that both vaccination strategies would
reduce the overall incidence of HPV 16/18related
cervical cancer by 91% during year 100 following
vaccine introduction. Thus, both vaccination strategies
would reduce the incidence of CIN 2/3, CIN 1, and
genital warts by approximately 90%, 86%, and 94%,
respectively, at this time point [1,2,11]. The catch-up
strategy is both more effective and efficient than the
strategy that vaccinates 12-year-old girls only, with an
incremental cost-effectiveness ratio of NT$410,477
or US$12,439/quality-adjusted life-year gained [11].
These researchers concluded that vaccination of women may not only substantially reduce genital warts,
CIN, and cervical cancer, but also improve quality of
life, survival, and cost-effectiveness [11].
In Spain, the mean management cost was 833
and 1056/patient from the Third Party Payer (TTP)
and societal perspective, respectively [7]. The overall
annual cost was estimated at 47 million and 59.6
million from the TPP and societal perspective, respectively [7]. In France, the annual direct cost of genital
warts management was estimated at 23.1 million, of
2009 Journal of Microbiology, Immunology and Infection
Hsueh
which 16.4 million was funded by the French health
care system [10].
Some controversy about the vaccine does exist.
There is little information available on the duration of
HPV vaccineinduced immunity [1-3]. There are no
published data demonstrating that HPV vaccination in
men can prevent transmission of HPV virus to women.
For already-exposed women (women receiving HPV
vaccine who have evidence of past or current HPV
infection with HPV vaccine types), current vaccine
trial data have demonstrated equivalent safety but no
equivalent efficacy. HPV testing before initiating vaccination is not recommended because there are no good
measures of past exposure and current clinically available testing reflects only recent viral shedding [2,3].
Conclusions
The increasing incidence of HPV infection and genital
warts highlights the need for an effective strategy for
the management of this disease. Even though many
different treatment modalities exist, none of these have
been proven to cure the disease. Increasing public
knowledge about prevention and transmission of HPV
and genital warts is essential in the fight against these
conditions. Immunization with HPV 6/11/16/18 recombinant vaccine holds promise for reducing the overall
burden of clinical HPV-related diseases. Studies are ongoing to evaluate vaccine efficacy in girls and women
aged 9 to 45 years and boys and women aged 9 to 26
years. A 10-year planned long-term efficacy and safety
analysis, as well as pilot programs to evaluate vaccine
impact on oropharyngeal HPV infection, particularly
among human immunodeficiency virus-infected men,
are also underway.
References
1. Wiley D, Masongsong E. Human papillomavirus: the burden
of infection. Obstet Gynecol Surv. 2006;61(Suppl 1):S3-14.
2. Saslow D, Castle PE, Cox JT, Davey DD, Einstein MH,
Ferris DG, et al. American Cancer Society Guideline for
human papillomavirus (HPV) vaccine use to prevent cervical
cancer and its precursors. CA Cancer J Clin. 2007;57:7-28.
3. Wang SS, Hildesheim A. Viral and host factors in human
papillomavirus persistence and progression. J Natl Cancer
Inst Monogr. 2003;31:35-40.
4. Koutsky L. Epidemiology of genital human papillomavirus
infection. Am J Med. 1997;102:3-8.
5. Insinga RP, Dasbach EJ, Myers ER. The health and
economic burden of genital warts in a set of private health
2009 Journal of Microbiology, Immunology and Infection
plans in the United States. Clin Infect Dis. 2003;36:
1397-403.
6. Castellsagu X, Cohet C, Puig-Tintor LM, Acebes LO,
Salinas J, Martin MS, et al. Epidemiology and cost of treatment of genital warts in Spain. Eur J Public Health. 2009;
19:106-10.
7. Lattimore S, Yin Z, Logan L, Rice B, Thornton A, Molinar
D, et al. Situation of HIV infections and STIs in the United
Kingdom in 2007. Euro Surveill. 2008;13 pii:19059.
8. Fenton KA, Lowndes CM. Recent trends in the epidemiology of sexually transmitted infections in the European
Union. Sex Trans Infect. 2004;80:255-63.
9. Langley PC, White DJ, Drake SM. The costs of treating
external genital warts in England and Wales: a treatment
pattern analysis. Int J STD AIDS. 2004;15:501-8.
10. Monsongo J, Breugelmans JG, Boue S, Lafuma A,
Bnard S, Rmy V. Anogenital warts incidence, medical
management and costs in women consulting gynaecologists
in France. Gynecol Obstet Fertil. 2007;35:107-13. [Article
in French].
11. Dasbach EJ, Insinga RP, Yang YC, Pwu RF, Lac C, Elbasha
EH. The cost-effectiveness of a quadrivalent human papillomavirus vaccine in Taiwan. Asian Pac J Cancer Prev. 2008;
9:459-66.
12. Tsao YP, Yang KY, Han CP, Yin CS, Yang YF, Chen SL.
Genital human papillomavirus infections in Taiwan. Int J
Gynaecol Obstet. 1994;44:39-45.
13. Lee YM, Leu SY, Chiang H, Fung CP, Liu WT. Human
papillomavirus type 18 in colorectal cancer. J Microbiol
Immunol Infect. 2001;34:87-91.
14. Tay SK, Ngan HY, Chu TY, Cheung AN, Tay EH. Epidemiology of human papillomavirus infection and cervical
cancer and future perspectives in Hong Kong, Singapore
and Taiwan. Vaccine. 2008;26(Suppl 12):M60-70.
15. Chen CA, Liu CY, Chou HH, Chou CY, Ho CM, Twu
NF, et al. The distribution and differential risks of human
papillomavirus genotypes in cervical preinvasive lesions: a
Taiwan Cooperative Oncologic Group Study. Int J Gynecol
Cancer. 2006;16:1801-8.
16. Castle PE. Beyond human papillomavirus: the cervix,
exogenous secondary factors, and the development of cervical precancer and cancer. J Low Genital Tract Dis. 2004;8:
224-30.
17. Von Krogh G. Management of anogenital warts (condylomata acuminata). Eur J Dermatol. 2001;11:598-603.
18. Scheinfeld N, Lehman DS. An evidence-based review of
medical and surgical treatments of genital warts. Dermatol
Online J. 2006;12:5.
19. Van der Meijden WI, Notowicz A, Blog FB, Langley PC. A
retrospective analysis of costs and patterns of treatment for
105
Human papillomavirus, genital warts, vaccines
external genital warts in The Netherlands. Clin Ther. 2002;
24:183-96.
20. Maw RD, Reitano M, Roy M. An international survey of
patients with genital warts: perceptions regarding treatment
and impact on lifestyle. Int J STD AIDS. 1998;9:571-8.
21. Carter JJ, Koutsky LA, Hughes JP, Lee SK, Kuypers J,
Kiviat N, et al. Comparison of human papillomavirus types
16, 18, and 6 capsid antibody responses following incident
infection. J Infect Dis. 2000;181:1911-9.
22. Barr E, Sings HL. Prophylactic HPV vaccines: new interventions for cancer control. Vaccine. 2008;26:6244-57.
23. FUTURE II Study Group. Quadrivalent vaccine against
human papillomavirus to prevent high-grade cervical lesions. N Engl J Med. 2007;356:1915-27.
24. Garland SM, Hernandez-Avila M, Wheeler CM, Perez
G, Harper DM, Leodolter S, et al. Quadrivalent vaccine
against human papillomavirus to prevent anogenital diseases. N Engl J Med. 2007;356:1928-43.
25. Carter JJ, Madeleine MM, Shera K, Schwartz SM, Cushing-
106
Haugen KL, Wipf GC, et al. Human papillomavirus 16 and
18 L1 serology compared across anogenital cancer sites.
Cancer Res. 2001;61:1934-40.
26. Keam SJ, Harper DM. Human papillomavirus types 16
and 18 vaccine (recombinant, AS04 adjuvanted, adsorbed)
[Cervarix]. Drugs. 2008;68:359-72.
27. Jenkins D. A review of cross-protection against oncogenic
HPV by an HPV-16/18 AS04-adjuvanted cervical cancer
vaccine: importance of virological and clinical endpoints
and implications for mass vaccination in cervical cancer
prevention. Gynecol Oncol. 2008;110(Suppl 1):S18-25.
28. Schwarz TF. AS04-adjuvanted human papillomavirus-16/18
vaccination: recent advances in cervical cancer prevention.
Expert Rev Vaccines. 2008;7:1465-73.
29. Harper DM, Franco EL, Wheeler CM, Moscicki AB,
Romanowski B, Roteli-Martins CM, et al. Sustained efficacy
up to 4.5 years of a bivalent L1 virus-like particle vaccine
against human papillomavirus types 16 and 18: follow-up
from a randomized control trial. Lancet. 2006;367:1247-55.
2009 Journal of Microbiology, Immunology and Infection
Das könnte Ihnen auch gefallen
- Genetic Analysis of Human Extrapair Mating Heritability, Between-Sex Correlation, and Receptor Genes For Vasopressin and OxytocinDokument7 SeitenGenetic Analysis of Human Extrapair Mating Heritability, Between-Sex Correlation, and Receptor Genes For Vasopressin and OxytocinMohammad Al-SalehNoch keine Bewertungen
- StrongChess The Evolution of ChessDokument46 SeitenStrongChess The Evolution of ChessKala KingNoch keine Bewertungen
- Journal of Marriage and The FamilyDokument11 SeitenJournal of Marriage and The FamilyMohammad Al-SalehNoch keine Bewertungen
- Azari2001 PDFDokument4 SeitenAzari2001 PDFMohammad Al-SalehNoch keine Bewertungen
- Subjective Relative Income and Lottery Ticket PurcDokument14 SeitenSubjective Relative Income and Lottery Ticket PurcMohammad Al-SalehNoch keine Bewertungen
- Theory of Mind in Nonhuman Primates: C. M. HeyesDokument14 SeitenTheory of Mind in Nonhuman Primates: C. M. HeyesMohammad Al-SalehNoch keine Bewertungen
- Aron Et Al - The Experimental Generation of Interpersonal ClosenessDokument15 SeitenAron Et Al - The Experimental Generation of Interpersonal Closenessasda asdaNoch keine Bewertungen
- Gender Differences and Similarities in Sexuality FinalDokument5 SeitenGender Differences and Similarities in Sexuality FinalMohammad Al-SalehNoch keine Bewertungen
- There Is Nothing Paranormal About Near-Death PDFDokument3 SeitenThere Is Nothing Paranormal About Near-Death PDFMohammad Al-SalehNoch keine Bewertungen
- Gender Differences and Similarities in Sexuality FinalDokument5 SeitenGender Differences and Similarities in Sexuality FinalMohammad Al-SalehNoch keine Bewertungen
- Journal of Marriage and The FamilyDokument11 SeitenJournal of Marriage and The FamilyMohammad Al-SalehNoch keine Bewertungen
- 100 Clinical CasesDokument30 Seiten100 Clinical CasesAdil Shabbir100% (1)
- Algorithms Computability Laboratory Project Initial MethodologyDokument3 SeitenAlgorithms Computability Laboratory Project Initial MethodologyMohammad Al-SalehNoch keine Bewertungen
- Attraction in Cross-Sex Friendship PDFDokument28 SeitenAttraction in Cross-Sex Friendship PDFPalinuroNoch keine Bewertungen
- Houston Complex AnalysisDokument98 SeitenHouston Complex Analysissticker592Noch keine Bewertungen
- Essential Neurology 4Th Ed PDFDokument290 SeitenEssential Neurology 4Th Ed PDFPutu 'yayuk' Widyani WiradiraniNoch keine Bewertungen
- The Essential Von Mises PDFDokument138 SeitenThe Essential Von Mises PDFMohammad Al-SalehNoch keine Bewertungen
- 6th Central Pay Commission Salary CalculatorDokument15 Seiten6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- DISEASE DETECTION IN VEGETABLES (TOMATO) USING DEEP LEARNINgDokument38 SeitenDISEASE DETECTION IN VEGETABLES (TOMATO) USING DEEP LEARNINgA ANoch keine Bewertungen
- Test Name Result Unit Reference Interval EndocrinolgyDokument1 SeiteTest Name Result Unit Reference Interval Endocrinolgygeetha kodaliNoch keine Bewertungen
- Bile Esculine TestDokument2 SeitenBile Esculine TestVincent OngNoch keine Bewertungen
- Common Mistakes-BiologyDokument8 SeitenCommon Mistakes-BiologyteahockNoch keine Bewertungen
- Respiratory PhysiologyDokument16 SeitenRespiratory PhysiologyYsabel Salvador DychincoNoch keine Bewertungen
- Ent AssessmentDokument23 SeitenEnt AssessmentPdianghunNoch keine Bewertungen
- Animal Genetic Engineering 110816 (1) Unit 4Dokument29 SeitenAnimal Genetic Engineering 110816 (1) Unit 4Rupal ChoudharyNoch keine Bewertungen
- Hse Statistics Report Pp701 Hse f04 Rev.bDokument1 SeiteHse Statistics Report Pp701 Hse f04 Rev.bMohamed Mouner100% (1)
- Presentation 1Dokument12 SeitenPresentation 1Rizka FarahinNoch keine Bewertungen
- Case Studies - EditedDokument5 SeitenCase Studies - EditedFunny LifeNoch keine Bewertungen
- Card Medical HistoryDokument4 SeitenCard Medical HistoryDanonino12Noch keine Bewertungen
- Spontaneous Pneumothorax - Management Feb15Dokument12 SeitenSpontaneous Pneumothorax - Management Feb15samuelNoch keine Bewertungen
- CBST LastDokument5 SeitenCBST LastMozma AwanNoch keine Bewertungen
- Do No Harm by Henry Marsh ExtractDokument15 SeitenDo No Harm by Henry Marsh ExtractAyu Hutami SyarifNoch keine Bewertungen
- Budget Justification Fy2021Dokument418 SeitenBudget Justification Fy2021Lisa FabianNoch keine Bewertungen
- Low Platelet CountDokument9 SeitenLow Platelet Countfatimah_zkhanNoch keine Bewertungen
- Cognitive Impairment Along The Course of Depression: Non-Pharmacological Treatment OptionsDokument11 SeitenCognitive Impairment Along The Course of Depression: Non-Pharmacological Treatment OptionsCarolina PradoNoch keine Bewertungen
- 5.RTRI Principle and Performance 8may2019Dokument34 Seiten5.RTRI Principle and Performance 8may2019ABCDeNoch keine Bewertungen
- Circulatory Disease ProjectDokument2 SeitenCirculatory Disease Projectapi-517831630Noch keine Bewertungen
- B12.Knowledge and Perceptions About COVID-19 Among The Medical and Allied Health Science Students in IndiaDokument6 SeitenB12.Knowledge and Perceptions About COVID-19 Among The Medical and Allied Health Science Students in IndiaWislianaNoch keine Bewertungen
- Occupational HealthDokument8 SeitenOccupational HealthFemale calm0% (1)
- Book 28Dokument56 SeitenBook 28Er Sana WarsiNoch keine Bewertungen
- Encouraging TeenagersDokument17 SeitenEncouraging TeenagersTahNoch keine Bewertungen
- Formative Gen EdDokument119 SeitenFormative Gen EdDan GertezNoch keine Bewertungen
- Traditional Indian MedicineDokument3 SeitenTraditional Indian MedicineShashvita RatraNoch keine Bewertungen
- DEVPSY Reviewer - Chapters 1-6 PDFDokument19 SeitenDEVPSY Reviewer - Chapters 1-6 PDFKathleen Anica SahagunNoch keine Bewertungen
- Adoption Foster ApplicationDokument4 SeitenAdoption Foster Applicationlb8757Noch keine Bewertungen
- De So 3Dokument6 SeitenDe So 3To Minh PhuongNoch keine Bewertungen
- Zat Aktif & PBFDokument153 SeitenZat Aktif & PBFnabilaNoch keine Bewertungen
- Bilirubin Metabolism Jaundice PPP 9Dokument27 SeitenBilirubin Metabolism Jaundice PPP 9Regina Marsha Xaveria100% (1)