Beruflich Dokumente
Kultur Dokumente
Macnee1994 1
Hochgeladen von
Direvald WesterosOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Macnee1994 1
Hochgeladen von
Direvald WesterosCopyright:
Verfügbare Formate
State of the Art
Pathophysiology of Cor Pulmonale in Chronic Obstrurtive
Pulmonary Disease
Part One
W. MACNEE
Unit of Respiratory Medicine, Department of Medicine, Royal Infirmary, Edinburgh, Scotland
CONTENTS
Cor Pulmonale, Right Heart Failure, and Edema in COPO:
Problems of Definition
Structure and Function of the Normal Pulmonary Circulation
Structure
Function
The Pulmonary Circulation in COPD
Pathology
Factors Contributing to the Development of Pulmonary Arterial
Hypertension in COPO
Disruption of the Pulmonary Vascular Bed
Effects of Blood Gases
Effects of Abnormal Pulmonary Mechanics
Effects of Increased Cardiac Output
Effects of Blood Volume
Effects of Blood Viscosity
The Role of the Pulmonary Endothelium
Pulmonary Hemodynamics in COPD
The Consequences of Pulmonary Hypertension in COPD
The Natural History of Untreated Pulmonary Hypertension
in COPO
Prevalence and Incidence of Right Ventricular Hypertrophy and
Edema in COPO
Oxygen Transport in COPO
Methods of Assessing Cardiac Function in Patients with COPD
Clinical Assessment
Radiography
Electrocardiography
Echocardiography
Radionuclide Assessment of Right Ventricular Ejection Fraction
201Thallium Myocardial Scintigraphy
Right Ventricular Dimensions Measured by Magnetic
Resonance Imaging
Right Ventricular Physiology in Normal Subjects and Patients
with COPD
Normal Right Ventricular Physiology
Right Ventricular Function in Stable COPO
Right Ventricular Mechanics in COPO
Preload
Afterload
Contractility
Right Ventricular Function in Acute Exacerbations of COPD
(Received in original form May 25, 1993 and in revised form May 6, 1994)
(Part 1 of 2 parts)
Correspondence and requests for reprints should be addressed to Dr. W.
MacNee, Unit of Respiratory Medicine, Department of Medicine, Royal
Infirmary, Lauriston Place, Edinburgh EH3 9YW, Scotland, UK.
Am
J Respir Crit Care Med Vol 150. pp 833-852,1994
The pulmonary circulation in patients with chronic obstructive pulmonary disease (COPD) is often considered a no-man's land, faIling between the domains of the respirologist and the cardiologist
and understood only by the physiologist! Pulmonary arterial hypertension is the major cardiovascular complication of COPD, and
its development is a landmark in the natural history of the disease. Pulmonary hypertension is important, not only because it
is associated with right ventricular hypertrophy-so-called cor pulmonale (1)- but also because it adversely affects prognosis (2).
Progress in our understanding of pulmonary vascular disease in
COPD has been hindered by difficulties in studying the structure
and function of the pulmonary circulation and right ventricle, except by invasive techniques, and because of the paucity of treatments for patients with COPO complicated by pulmonary vascular disease.
This review covers the factors that lead to the development of
pulmonary hypertension in patients with COPD and the effects
of pulmonary hypertension on right ventricular function. The controversial issue of the etiology of the syndrome of edema in COPD
and whether it is truly associated with right ventricular failure is
discussed. The methods used to assess ventricular function are
assessed, and the noncardiac events that may mediate this syndrome are also reviewed.
Unraveling the mechanisms of pulmonary hypertension and
edema in cor pulmonale should lead to treatments for this condition
that are more logical than the limited therapy presently available.
COR PULMONALE, RIGHT HEART FAILURE, AND EDEMA
IN COPD: PROBLEMS OF DEFINITION
Pulmonary arterial hypertension in patients with COPD often attracts attention only when they develop edema. The term cor pulmonale was probably introduced by PaulO. White in 1931 and
is irrevocably entrenched in the literature. An expert committee
of the World Health Organization defined cor pulmonale as "hypertrophy of the right ventricle resulting from diseases affecting the
function and/or structure of the lungs, except when these pulmonary alterations are the result of diseases that primarily affect the
left side of the heart, as in congenital heart disease" (3). This is
a pathological rather than a functional definition and is thus of
limited clinical value, as methods of diagnosing right ventricular
hypertrophy in living subjects are imprecise and accurate diagnosis requires an autopsy (4). The definition was revised by Behnke
and colleagues (5), who replaced the term hypertrophy with alteration in the structure and function of the right ventricle. This definition is also imprecise, because it covers a spectrum of dysfunction from mild abnormality to frank right heart failure~
834
AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE VOL 150
Cor pulmonale is often misused to indicate "right heart failure"
secondary to pulmonary disease or simply the presence of pulmonary arterial hypertension or edema in a patient with capo
(6-8). The problem of defining cor pulmonale produces considerable difficulty when comparing patients from different studies
in the literature.
A further problem stems from the lack of an accepted definition of heart failure (9). The European Society of Cardiology (10)
defined heart failure as "a state of any heart disease in which,
despite adequate ventricular filling, the heart's output is decreased
or in which the heart is unable to pump blood at a rate adequate
for satisfying the requirements of the tissues, with functional
parameters remaining within normallimits~ This definition is probably more applicable to the left side of the circulation. More appropriately, right ventricular failure could be defined as "an inability of one or more chambers of the heart to accept and expel the
venous return throughout the range of physiological activity, without alteration of normal circulatory hemodynamics" (11, 12). For
most clinicians, heart failure describes a clinical syndrome,
whereas experts in the field may include an assessment of the
peripheral circulation and tissue metabolism in the definition (13).
The textbook signs of right ventricular failure, consisting of raised
jugular venous pressure, liver enlargement, and peripheral edema,
may be present in patients with hypoxic capo and in patients
with congestive cardiac failure due, for example, to ischemic heart
disease. However, the cardiac output is usually normal, and there
is no vasoconstriction of the peripheral circulation in patientswith
capo (14).
The classic view of the development of "heart failure" in patients with capo states that hypoxia leads to pulmonary hypertension, which increases right ventricular work, producing right
ventricular hypertrophy and dilation, resulting eventually in right
ventricular failure and peripheral edema (4, 13, 15, 16). However,
the notion that the edema that occurs in cor pulmonale is purely
"cardiac" in origin has been questioned (17-20). Recently it has
been proposed that the term cor pulmonale should be abandoned
in favor of a more precise description that is based on objective
evidence of right ventricular hypertrophy, enlargement, functional
abnormality, or failure (21).
STRUCTURE AND FUNCTION OF THE NORMAL
PULMONARY CIRCULATION
Structure
The pulmonary circulation perfuses rather than nourishes the
lungs. Because it is in series with the systemic circulation the pulmonary vasculature is unique, as it receives all of the cardiac output. Cumming, Horsfield, and coworkers (22-24), using postmortem casts, measured the dimensions of the human pulmonary
arterial tree. They described 17 branching orders in the human
pulmonary arterial system, from the alveoli to the main pulmonary artery, but confusingly numbered the different generations
from the peripheral to the large vessels in the direction opposite
to flow. The ratio of the number of vessels from one order to the
next, the branching ratio, is 3.0 and is relatively constant, as are
the diameter ratio at 1.6 and the average length ratio at 1.5. These
dimensions have important implications for the resistance of the
pulmonary vasculature.
The walls of the large pulmonary arteries, which are thinner
than those of the systemic arteries, consist of smooth muscle inserting into short elastic fibers and thus appear to be designed
to enable the vessel to distend rather than actively constrict or
dilate (25). The potential for the large pulmonary arteries to constrict was first demonstrated in the early animal work on Von Euler
1994
and coworkers (26, 27). The small muscular pulmonary arteri~s
seem to be the predominant site of changes in pulmonary vascular tone. The terminal branches of the pulmonary arteries also
have a larger internal diameter and a thinner wall than the corresponding systemic arteries. Medial thickening in the small arteries, which develops in patients with pulmonary hypertension, will
potentiate the increase in resistance produced by active vasoconstriction and lessen the ability of the vessels to distend passively.
This will increase the contribution that the small arteries make
to the resistance to blood flow (28).
Systemic arterioles have a coat of circular smooth muscle and
are therefore able to constrict and thus make a large contribution
to the systemic vascular resistance. By contrast, precapillary muscularized arterioles are not normally present in the pulmonary circulation, so the arterioles make a lesser contribution to the total
pulmonary vascular resistance. Moreover, the arterioles can respond to changes in blood volume by passively changing their
caliber and can thus act as a reservoir for blood.
The pulmonary capillaries are difficult to distinguish as separate structures within the alveolar walls on standard 5-J.1m histological sections of the human lung. However, scanning electron
microscopy confirms that the pulmonary capillary bed consists
of a large number of capillary segments of varying diameters and
lengths (Figure 1). The number of capillary segments in postmortem lungs has been estimated by Weibel to be 1011, with an average diameter of 5 J.1m and average length of 11 J.1m (29). The average diameter of the pulmonary capillaries is smaller than that of
the systemic capillaries. These dimensions have been confirmed
recently in resected human lungs (30).
Neutrophils and erythrocytes have a larger average diameter
(7 J.1m) than the pulmonary capillaries (5 J.1m) (31). The erythrocyte is a fairly deformable cell because of its biconcave shape
and lack of a nucleus (32). Thus, the neutrophil is 700 times less
deformable than the erythrocyte because of its nucleus and viscous cytoplasm (32). This leads to trapping or sequestration of
neutrophils during their transit through the pulmonary capillary
segments in normal lungs (33). The pulmonary capillaries have
neither contractile cells nor smooth muscle in their walls. Thus,
capillaries do not contract actively but can change their dimensions passively. A reduction in capillary diameter can be produced
by swelling of the endothelial cells, by perivascular transudates
Figure 1. Scanning electron micrograph of the human lung. The pulmonary vasculature has been perfused to show the intermeshing capillary
segments in the alveolar walls. Kindly produced and supplied by Dr. Peter Jeffery, Department of Pathology, National Heart and Lung Institute,
London.
State of the Art: Pathophysiology of Cor Pulmonale in COPO
(34), or by an increase in alveolar (35) or pleural pressure (36).
The capillaries can also distend in response to an increase in local blood volume. The pulmonary alveolar-capillary surface area
in man is on the order of 50 to 70 m2 at rest, increasing to 90 m2
at 75% of total lung capacity (37), and can increase further in normal subjects during exercise without producing an inequality between alveolar ventilation and pulmonary capillary perfusion (38).
Function
A mean pressure of only 10 mm Hg is necessary to distribute the
cardiac output within the pulmonary vasculature at rest. This low
pressure prevents fluid from passing into the interstitial space and
enables the right ventricle to function un~er conditions of low
energy expenditure. The normal pulmonary circulation offers less
than a tenth of the resistance to flow than does the systemic circulation. Basal pUlmonary vasomotor tone is also low, because
vasodilators that reduce systemic vascular pressures have little
effect on the normal resting pulmonary arterial pressure (Ppa)
(39-41). The cardiac output needs to increase by 2.5 times the
normal value to produce any increase in Ppa in normal subjects
(42). This is due to recruitment of underperfused pulmonary capillaries as cardiac output increases, particularly in zone I of West
(43). Thus, during exercise in normal subjects the mean Ppa may
rise by 3 or 4 mm Hg, with the increase in systolic pressure generally exceeding that of the diastolic pressure, which may not change
(44). After exercise, the mean Ppa often falls below the resting
values (45, 46). Pulmonary vascular resistance either remains unchanged (47) or falls during exercise (48), as a result of passive
dilation of underperfused vessels.
The factors influencing the pulmonary vascular resistance are
complex (49). Most studies of pulmonary hemodynamics have simplified the definition of the resistance as the pressure drop across
a segment of the pulmonary vasculature divided by the flow
through it. Calculation of the pulmonary vascular resistance is
often oversimplified by dividing the mean Ppa by the cardiac output to produce the total pulmonary vascular resistance. However,
this calculation does not take into account the left atrial or the
pulmonary arterial wedge pressure. This is not a problem when
the pulmonary arterial wedge pressure is low, as in normal subjects, but this may not be the case in ill subjects. Moreover, in pa~
tients with capo the wedge pressure may not be an accurate
reflection of the left atrial pressure (50). Thus, this oversimplification presents a very limited view of pulmonary hemodynamics and
may lead to errors of interpretation, particularly as changes in resistance can result from changes in the cross-sectional area of
the pulmonary vascular bed. In addition, both flow and pressure
in the pulmonary circulation are pulsatile, and the time-averaged
values for each of these variables should be used when calculating their ratio.
The transmural pressure in the pulmonary vasculature is influenced by the alveolar pressure. This is particularly true of the
pulmonary capillaries, which pass through the alveolar walls.
Changes in the surface area of the pulmonary capillaries can arise
from a change in the diameter of the vessels or from a change
in the number of parallel paths that are being perfused as a result of the recruitment of previously underperfused vessels. A practical demonstration of this effect comes from direct measurements
of the relation between pressure and flow in the pulmonary vasculature, which were made in the early 1950s. In these studies,
balloon occlusion of a pulmonary artery, usually on the right, was
performed during cardiac catheterization (51). Under these conditions, when blood flow was almost doubled through the left lung
the relation between pressure and flow was linear in normal su-
835
pine man, and the pulmonary vascular resistance remained unchanged (52, 53). However, this is not the case in the upright position, where the more dependent pulmonary blood vessels are
in a partially collapsed state and can expand in response to an
increase in flow, resulting in a fall in the pUlmonary vascular resistance (54).
Thus, changes in pulmonary vascular resistance are not necessarily an accurate r~flection of active changes in pulmonary vascular caliber, unless all of the passive mechanisms affecting caliber have been taken into account. This has led to the use of
pulmonary arterial pressure/flow curves and pulmonary vascular resistance/flow curves to detect active changes in pulmonary
vascular caliber so that both of the effects of the changes in flow
and pressure on resistance can'.be assessed (55).
THE PULMONARY CIRCULATION IN COPO
Pathology
The development of hypoxemia in patients with capo is associated with pathological changes that occur characteristically
in the peripheral arteries (56-58). The small pulmonary arteries
develop accumulations of vascular smooth muscle cells in their
intima that are laid down longitudinally along the length of the
vessels (57). More recent studies have suggested that intimal thickening is an early event that occurs in association with progressive airflow limitation (58-60). Medial hypertrophy in the muscular pulmonary arteries, and less commonly fibrinoid necrosis in
these vessels, has also been reported in patients with capo who
develop sustained pulmonary arterial hypertension (61). Thus,
structural change, rather than simply hypoxic vasoconstriction,
is the major factor in the development of sustained pulmonary
hypertension in patients with capo (62).
Pulmonary thrombosis may also occur in patients with capo,
which may be secondary to peripheral airway inflammation (63).
Indeed, pathological changes in the small airways of patients with
capo appear to correlate with the vascular changes, including
thickening of all three layers of the vascular wall, which can be
shown in postmortem studies of patients with hypertensive pulmonary vascular disease (63, 64). However, this relation was not
confirmed in a study of patients undergoing lung resection (54).
This latter study (54) also demonstrated a stepwise increase in
arterial wall thickness in a comparison of nonsmokers and smokers
with mild to moderate emphysema, which was associated with
an increase in the thickness of all three vessel layers. However
the degree of intimal thickening was out of proportion to the
changes in the media or the adventitia. This confirms an earlier
study by Hale and colleagues (64) in postmortem lungs that
demonstrated intimal thickening in muscular pulmonary arteries
in a population of smokers.
In postmortem studies it is difficult to dissociate right ventricular hypertrophy (ie, increased right ventricular free wall mass) from
right ventricular dilatation (ie, increased free wall area) (65). Thus,
hypertrophy and dilatation are often considered together and referred to as right ventricular enlargement. Chronic hypoxemia
produces right ventricular hypertrophy in animal studies (66, 67),
and this relation is well established in normal subjects at altitude
(68). A correlation has also been demonstrated between the usual
partial pressure of oxygen in a group of patients receiving longterm oxygen therapy and the degree of right ventricular hypertrophy (69), confirming previous work (70). However, there is no
significant correlation between the weight of the right ventricle
or the pulmonary vascular resistance and the extent of emphysema measured in postmortem lungs (69, 70).
836
AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
Factors Contributing to the Development of Pulmonary
Arterial Hypertension in CO PO
The increase in Ppa in patients with COPO (48, 71-73) probably
results from a combination of several factors that passively or actively affect pulmonary hemodynamics. However, the precise
mechanisms remain to be elucidated.
Disruption of the pulmonary vascular bed. In the early 1940s,
pulmonary hypertension was thought to arise from alveolar wall
and hence small vessel destruction in what was then called chronic
emphysema, which was thus considered to be irreversible (13).
Although vessel occlusion contributes to the pulmonary hypertension in thromboembolic disease (74), the destruction of alveolar vessels that occurs in emphysema is typically associated with
normal resting Ppa until late in the course of the disease (75).
The lack of a significant correlation between right ventricular hypertrophy and total alveolar surface area (76) (which reflects the size
of the capillary bed) suggests that loss of capillary bed per se
is not an important determinant of the development of sustained
pulmonary hypertension at rest in patients with COPO. However,
loss of the capillary bed may contribute to the pulmonary arterial
hypertension that develops during exercise in such patients.
Although previous studies have suggested that Ppa is raised
in the "bronchitic" and normal in the "emphysematous" clinical
types of patient with COPO (77, 78), these studies are open to
criticism because quantification of emphysema in living subjects
is difficult (79, 80). Recent studies using computed tomography
(CT) scanning to measure lung density (80), which correlates with
morphometric measurements of microscopic emphysema (81),
have shown a similar extent of emphysema in patients with the
so-called "pink and puffing" or "emphysematous" type of COPO
as in the "blue and bloated" or "bronchitic" type (82). Furthermore,
as in studies of resected or autopsy lungs (58, 60, 69), there was
no significant correlation between Ppa or resistance and the extent of emphysema, in this case as measured by CT lung density
in patients with COPO (82).
Effects ofblood gases. In 1946, Von Euler and Liljestrand (26),
in experiments in cats, were the first to show convincingly that
acute hypoxia induces pulmonary vasoconstriction. Although a
local disease in Po2produces systemic vasodilation, alveolar hypoxia is a potent arteriolar constrictor in the pulmonary circulation,
which reduces perfusion with respect to ventilation in an attempt
to restore Pa02 (67). Thus hypoxic vasoconstriction acts as a control mechanism that limits the effects of hypoxia on ventilation:perfusion ratios in the lungs.
Acute hypoxia induces pulmonary vasoconstriction in normal
subjects (83-86) without changing pulmonary artery wedge pressure (84). The negative correlation between Ppa and Sa02 in patients with COPO was first reported by Harvey and coworkers (85)
and has been confirmed by many other authors (86-94). Shortterm supplemental oxygen, even in high concentrations, produces
a variable and often trivial fall in Ppa in patients with COPO (89,
95-97). Oespite normalization of the Pao2, normal values of Ppa
are rarely achieved in these patients. Pulmonary hypertension is
also relieved only partially when mountain dwellers exposed to
chronic hypoxia are given oxygen acutely. Normal levels of Ppa
may only be achieved after residence at low altitude for 6 wk (98).
Moreover, breathing high concentrations of oxygen increased
Paco2 in some studies of COPO patients (89, 95, 97), which together with the associated acidemia may potentiate pulmonary
vasoconstriction.
In patients with COPO there is a positive correlation between
the arterial Paco2and the Ppa (89, 99). Raising the Paco2in patients with COPO produces a rise in Ppa that is probably not due
VOL 150
1994
to the direct vasoconstrictor effect of carbon dioxide, since cardiac
output also increases (100, 101). The mechanism of this effect may
relate to a change in lung mechanics as a result of the hyperventilation induced by hypercapnia (102) or the potentiation of the hypoxic pulmonary vasoconstrictor response (103) as a result of increasing Paco2.
Although an increase in arterial hydrogen ion concentration
causes a rise in Ppa in normal subjects (99), acute changes in
hydrogen ion concentration in patients with COPO produce inconsistent changes in Ppa (104-106). Furthermore, intravenous
infusion of sodium bicarbonate in normal subjects, which increased
the arterial pH to 7.5, had no effect on the Ppa or the cardiac output (107). Induction of an alkalemia in patients with COPO also
did not change the Ppa, but the cardiac output increased substantially, suggesting that pulmonary vasodilation had occurred
(104). However, the curvilinear relationship between pressure and
flow in the pulmonary circulation in patients with COPO means
that such a change may not result from pulmonary vasodilatation. Inconsistent changes in pulmonary hemodynamics have also
been reported when the arterial hydrogen ion concentration was
increased acutely by an intravenous infusion of hydrochloric acid
in patients with COPO (105, 106) or chronically over 5 to 7 d by
giving ammonium chloride orally (108). However, hypoxia and
acidemia act synergistically to produce pulmonary vasoconstriction in patients with COPO. Thus, for a given Sao2, the mean Ppa
is higher with increasing arterial hydrogen ion concentrations (104).
Effects of abnormal pulmonary mechanics. Changes in airway
resistance may augment pulmonary vascular resistance in patients with COPO by affecting the alveolar pressure. Harris and
coworkers (102) demonstrated that the linear relationship between
pressure and flow in the pulmonary circulation when alveolar pressure is normal changes when the alveolar pressure is increased
by increasing the gas pressure at the mouth. Under these conditions the slope of the pressurelflow relation in the pulmonary circulation is steeper initially and becomes curvilinear as the pressure increases so that pressure no longer increases in proportion
to blood flow, due to compression of the resistance vessels in the
lungs as a result of increased alveolar pressure (Figure 2A). Thus,
when alveolar pressure is increased in normal subjects, the relation between pressure and flow in the pulmonary circulation resembles the relation in patients with COPO during normal tidal breathing (73, 102) (Figure 28). The effect of airway resistance on Ppa
may be particularly important when ventilation increases (such
as in acute exacerbations of COPO). In normal subjects or in patients with mild COPO (102, 109), hyperventilation does not affect
the pulmonary circulation significantly, whereas in patients with
more severe COPO, hyperventilation increases both pulmonary
arterial and pulmonary artery wedge pressures without changing cardiac output (102). Thus the consequent increase in pulmonary vascular resistance results from a' reduction in the caliber
of the vessels. At least one study has demonstrated a correlation
between Ppa and FEV. in patients with! COPO (102). Moreover,
the amplitude of the respiratory swings\of the Ppa during exercise (which is related to changes in intrathoracic pressure) in patients with moderately severe COPO correlates with the Ppa (110).
Effects of increased cardiac output. In contrast to the situation
in normal subjects (42), in patients with COPO (in whom the vascular bed may be reduced) even the small increase in flow that
occurs during mild exercise may increase Ppa significantly (111).
Effects of blood volume. The effect on Ppa of expanding the
blood volume has been studied by Abraham and colleagues (112)
in patients with COPO. Hypoxia produced an increase in Ppa associated with a small increase in cardiac index, and thus pulmo-
837
State of the Art: Pathophysiology of Cor Pulmonale in COPD
30
15
".V"~""'''''''
J
en
:z:
E
E
....-
20
/
/
'"IUUIn
c:n
:z:
E
E
....<I
rn~;);)un~
10
<I
o IC
o
LEFT LUNG FLOW (,. min1)
o 0r
B
2I
I
4
I
6
I
8
LEFT LUNG FLOW (I'min l )
Figure 2. The relation between flow and pressure in the pulmonary circulation can be studied by increasing flow through the left lung by balloon
occlusion of the right pulmonary artery. In normal subjects (A) the influence of alveolar pressure on this relation is shown by increasing mouth pressure.
The relation between pressure and flow in normal subjects is similar to the relation in five patients with COPD (B). After Harris and Heath (49).
nary vascular resistance increased in these patients; however, the
infusion of albumin increased Ppa but produced a greater increase
in cardiac index, and thus pulmonary vascular resistance fell.
These data do not support the hypothesis that an increase in blood
volume is a major factor in the development of pulmonary hypertension in COPO (113). Indeed, the pulmonary blood volume is
either normal or low in patients with COPO. Moreover, there is
no significant correlation between Ppa and the plasma or total
blood volume in such patients (114).
Effects of blood viscosity. Polycythemia can develop secondary to chronic hypoxemia in patients with COPO, resulting in an
increase in blood viscosity. Since viscosity is a factor in tl:le
Poiseuille equation, in theory any increase may contribute to the
development of pulmonary arterial hypertension. Reducing
packed cell or blood volume and hence plasma viscosity in patients with COPO produces a small reduction in Ppa without changing cardiac output, and thus pulmonary vascular resistance falls
slightly (52) without any change in arterial blood gas values
(52, 115).
The role of the pulmonary endothelium. The mechanisms that
induce hypoxic vasoconstriction leading to sustained pulmonary
hypertension are not fully elucidated (116, 117). Previous studies
have focused on the leukotriene metabolites of the 5-lipoxygenase
pathway of arachidonic acid as mediators of hypoxic vasoconstriction. Their role is supported by studies showing enhancement of
hypoxic vasoconstriction by cyclooxygenase inhibition and leukotriene receptor blockers (118, 119). Thus, one hypothesis is that
pulmonary vascular tone in hypoxia is determined by the balance
between constricting leukotrienes (84 , C4 , and 0 4 ) and dilating
prostaglandins (largely prostacylin). However, this hypothesis has
been refuted by its original proponents (120). More recent work
suggests that potassium channels may also be involved in the
mechanism by which hypoxia is sensed by vascular smooth muscle cells and the signal transduced in the cell to produce vasoconstriction (121).
The nitrovasodilators appear to act by releasing an endothelium-derived relaxing factor. This is thought to be nitric oxide (NO)
or a nitroso-compound that releases NO (122). Increased blood
flow producing an increase in shear stress seems to be the stimulus for the release of NO from the luminal surface of endothelial
cells (123). This stimulates guanylate cyclase with a resultant increase in the second messenger cyclic guanosine monophosphate
in vascular smooth muscle, producing vasodilatation (124). Several lines of circumstantial evidence suggest that NO may play
a major role in modulating pulmonary vascular tone. NO is an endogenous vasodilator that is released from endothelial cells and
produces relaxation of isolated human pulmonary artery rings
(125-127). Removal of the endothelium from isolated vascular rings
(128, 129) or preventing formation of NO by pretreatment with an
L-arginine analogue (130, 131) increases the response of isolated
vascular rings to vasoconstrictors. These studies suggest a mechanism whereby NO acts as a "braking system" to prevent an excessive rise in pulmonary vascular tone. However, whether NO
release in vivo has a role in maintaining the normally low pulmonary vascular tone remains speculative.
Inhibition of NO synthesis enhances the vasoconstrictor effect
of acute hypoxia (132), suggesting that NO also acts in this case
as a chemical brake to counteract excessive hypoxic pulmonary
vasoconstriction. Endothelial cell proliferation and thickening occur in the intima of the small pulmonary arterioles in response
to chronic hypoxia, both in animals (133) and in patients with COPO
(56-59). Moreover, endothelium-dependent dilatation is impaired
in animals that are chronically exposed to hypoxia (134) and in
isolated pulmonary rings from patients undergoing heartllung
transplantation for end-stage COPO (129). Impaired endotheliumdependent vasodilatation may result from either a reduction in
NO synthesis or release as a result of hypoxia (135). These data
lend further support to the hypothesis that the endothelium has
a central role in regulating the pulmonary vasculature (136, 137).
Thus, the normal braking mechanism that ameliorates the effect
838
AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
of vasoconstrictors on pulmonary vascular tone may be lacking
in COPO, which may relate to the structural changes in the intima
and media that occur in the small pulmonary arteries (129). A further extension of this hypothesis is that NO may inhibit cell proliferation in the pulmonary vasculature and may thus not only affect
pulmonary vasomotor tone but may also influence the vascular
remodeling that occurs in hypoxic COPO (135).
In summary, it is likely that a complex interaction occurs between the factors described above that contribute to the development of pulmonary arterial hypertension. An increase in pulmonary vascular resistance occurs, particularly during exercise, in
such patients because the ability to recruit underperfused vessels is compromised. Thus, patients with a severely restricted vascular bed with extensive loss of the pulmonary vasculature may
respond to exercise as though they started at the bend of the normal pressure/flow relation, so that any increase in cardiac output
augments pressure dramatically. Hypoxic vasoconstriction and
structural changes in the vessels will further reduce the pulmonary vascular reserve. At this stage, Ppa is elevated at rest and
the pressure/flow relation shifts upward and to the left, so that
small changes in flow produce large changes in pressure over
the entire range of the cardiac output. Changes. in plasma viscosity and alterations in pulmonary mechanics may also contribute to pulmonary arterial hypertension in patients with more severe COPO. The relative contribution of each of these factors to
the development of pulmonary hypertension in patients with COPO
is difficult to quantify and in any case varies between individuals.
The mechanism producing hypoxic vasoconstriction and the structural changes that ensue from chronic hypoxia have not been fully
elucidated. However; it seems likely that the pulmonary endothelial
cell has a central role in modulating vasomotor tone through a
mechanism that involves NO.
VOL 150
1994
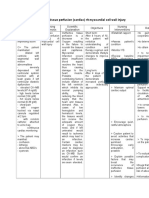
TABLE 1
HEMODYNAMICS AND BLOOD GAS VALUES IN 74 PATIENTS
WITH PREVIOUS EPISODES OF ACUTE RESPIRATORY FAILURE
(BUT STUDIED WHEN STABLE) AND 32 NORMAL SUBJECTS
COPD
Normals
Variables
Mean
Range
Mean
Range
Pao2 , mm Hg
Paco2 , mm Hg
Q, Umin/m 2
Pra, mm Hg
Ppa, mm Hg
Ppw, mm Hg
PVRI, dyne/slcm 5/m 2
RVSWI, g/m
43
51
3.8
3
35
6
660
16
23-67
33-68
2.3-5.8
0-21
15-78
0-19
213-1,377
5-29
91
38
3.6
5
13
9
58
6
75-105
32-43
2.6-4.5
2-9
8-20
5-14
40-200
3-18
Definition of abbreviations: a = arterial; Q = cardiac output; Pra = right atrial pressure;
Ppa = mean pUlmonary arterial pressure; Ppw = pulmonary artery wedge pressure; PVAI =
pUlmonary vascular resistance index; AVSWI = right ventricular stroke work index.
From Naeije (148).
normalities worsen, and with the development of chronic hypoxemia and hypercapnia, pulmonary hypertension may be present
at rest and worsen with exercise. However, even in patients with
severe COPO, the increase in Ppa is usually rather small. Naeije
(148) studied 74 patients with severe but clinically stable COPO
who had all presented in the past with episodes of acute-on-chronic
respiratory failure and almost half with peripheral edema. They
all had severe airflow limitation (FE~ 25.7 1% of predicted,
mean SO) and hypoxemia (Pao2: mean, 43 mm Hg; range,
23-67 mm Hg), and the majority were also hypercapnic (Paco2:
mean, 51 mm Hg; range, 33-68 mm Hg). However, Ppa was only
modestly raised with a mean of 35 mm Hg in this group (Table 1).
PULMONARY HEMODYNAMICS IN COPD
THE CONSEQUENCES OF PULMONARY HYPERTENSION
IN COPD
Although Ppa may be normal or only slightly elevated when measured at rest in patients with COPO rn, 138-140), it may increase
to abnormal levels during exercise (48,71, 72)-the increase being greater in subjects over the age of 50 years (71, 72). Using
the technique of balloon occlusion of the right pulmonary artery
in supine patients with COPO, as previously described in normal
subjects (51-54, 141), the initial part of the relation is steeper than
normal indicating increased resistance (54). Moreover, at higher
flow rates the relation between pressure and flow is curvilinear,
so that resistance decreases due to distension of partially collapsed vessels at high flow rates (Figure 2).
Before the development of significant hypoxemia and hypercapnia, patients with mild COPO have a normal or low cardiac
output (1, 142-147). Right atrial and right ventricular end-diastolic
pressures are normal, and Ppa may be normal or slightly elevated
but inappropriately high for the level of cardiac output. The pulmonary vascular resistance is therefore normal, or only slightly
elevated when measured at rest, but may rise markedly during
exercise (48, 71). Patients with COPO stop exercising at a lower
level of cardiac output and maximal O2consumption than normal
subjects. However, the slope of the relation between oxygen consumption and cardiac output is normal (146, 147). Thus, the limitation to exercise in patients with COPO is not cardiovascular but
results from changes in pulmonary mechanics that affect ventilation.
In patients with mild COPO, right ventricular end-diastolic pressure and right ventricular stroke work, which are normal at rest,
increase during exercise due to an increase in work against a
higher P~a (146). As airflow limitation and arterial blood gas ab-
Chronic bronchitis and emphysema usually coexist pathologically.
Those patients with either predominant chronic bronchitis or
mainly emphysema form a minority at either end of the disease
spectrum of patients with COPO (149-152). The notion of two clinical patterns in patients with chronic bronchitis and emphysema
has been attributed to Dornhurst (153). The "blue and bloated"
type (154), also known as "type B" (155) or "nonfighter" (156), was
thought to characterize the "bronchial type" of disease (149). These
patients had hypoxemia, hypercapnia, and secondary polycythemia and developed pulmonary hypertension relatively early in the
course of the disease. Right ventricular hypertrophy or cor pulmonale ensued, and repeated episodes of "right heart failure" occurred, often during acute episodes of respiratory failure. In contrast, the "pink and puffing" variety, also known as "type ~' or
"fighter:' were thought to represent the emphysematous patients,
characterized by severe breathlessness but with preservation of
blood gas values and thus no pulmonary hypertension, right ventricular hypertrophy, or "heart failure," at least until the later stages
of the disease. The hypothesis that the "pink puffer" had predominantly emphysema and the "blue bloater" had predominantly
chronic bronchitis was perpetuated in several studies in the 1960s
(157-161). However; Thurlbeck (162) showed that the degree of mucous gland hypertrophy, indicative of chronic bronchitis, was similar whatever the clinical pattern of the disease and that more than
50% of patients with the "blue and bloated" clinical pattern had
severe emphysema. These pathological observations have been
confirmed in a study of autopsies from the National Institute of
Health Nocturnal Oxygen Therapy Trial (NOfT) that showed a complete overlap in the amount of mucous gland hypertrophy and em-
839
State of the Art: Pathophysiology of Cor Pulmonale in COPO
physema in the two clinical types (163). CT scanning has also confirmed that similar degrees of emphysema occur in patients with
both patterns of the disease (82). Furthermore, there is no significant correlation between Ppa and the extent of emphysema as
measured by CT scanning. However, autopsies of patients in the
NOTT trial (163) showed that the "blue bloaters" had heavier right
ventricles than the "pink puffers," and there was a significant correlation between the degree of the right ventricular hypertrophy and
the extent of chronic inflammatory changes in the airways.
The Natural History of Untreated Pulmonary Hypertension in COPO
The Ppa has been shown in numerous studies to be only moderately elevated in patients with COPO who have mild or moderate
hypoxemia and rarely if ever reaches the levels seen in patients
with primary pulmonary hypertension (164). The progression of
pulmonary arterial hypertension in patients with COPO is slow
(143, 165-169). Weitzenblum and colleagues (178) studied the
changes in Ppa in a group of patients with COPO over an average follow-up period of 5 yr and found a mean rise in the Ppa
of only 3 mm Hg per yr. In only 33% of these patients did the Ppa
increase by more than 5 mm Hg during this period. Those in whom
pulmonary hypertension progressed (defined as an increase in
Ppa of ~ 5 mm Hg) had baseline spirometry, arterial blood gas,
and pulmonary hemodynamic values similar to the group as a
whole. However, they were distinguished by progressive hypoxemia and hypercapnia, whereas those whose Ppa remained stable showed no change in arterial blood gas values over time. These
data demonstrate the importance of worsening hypoxemia in the
progression of pulmonary hypertension in COPO. Data on the
progression in Ppa in patients in the British Medical Research
Council (MRC) long-term oxygen trial support this view (170). Thus,
the Ppa rose in the untreated group by a mean of 3 mm Hg per
yr, whereas there was no significant change in the treated group.
However, not all studies support a relation between worsening hypoxemia and progression of pulmonary arterial hypertension.
Boushy and North (143) reported a mean increase in Ppa of 7
mm Hg associated with a 6% increase in cardiac output in 136
patients with COPO who were not receiving long-term oxygen therapy, studied before and after an average interval of 25 mo. By
contrast, Schrijen and colleagues (166) found no significant deterioration in pUlmonary hemodynamics in a group of patients with
COPO not receiving oxygen therapy, studied over 3 yr, even when
the Ppa was elevated when first measured. However, in the latter
study (166), 30% of the patients demonstrated a fall in systemic
arterial pressure over time, which was attributed to the peripheral vasodilation produced by hypercapnia.
Although the prevalence of chronic bronchitis and emphysema
has declined (171,172), COPO and allied disorders (International
Classification of Diseases, World Health Organization, Geneva,
Switzerland, 9th revised edition, category 490-496) accounted
for 4.5% of total deaths (almost 3,000 deaths) and was the fifth
leading cause of death in Scotland in 1989 (173), and resulted
in almost 28,000 deaths (5% of the total) in 1988 in England and
Wales. A large number of factors influence survival in patients with
COPO. In a recent review of the literature by Hodgkin (174), increasing age and a low postbronchodilator FEy' were the best
predictors of mortality in COPO. However, several studies have
shown that the presence of pulmonary arterial hypertension or
peripheral edema in patients with hypoxic COPO correlates with
survival (2, 175-185). Patients with COPO who develop peripheral edema have a 5-yr survival rate of only 27% to 33% (174).
Although pulmonary arterial hypertension progresses slowly
in patients with COPO, its presence infers a poor prognosis. Weitzenblum and coworkers (175) showed a 72% 4-yr survival rate in
patients whose Ppa was normal (Ppa < 20 mm Hg) compared
with a 49% survival in those with an elevated Ppa. Other investigators have also confirmed the prognostic value of Ppa (186). Burrows and colleagues (155) studied 50 patients with chronic airways obstruction over 7 yr and showed that the hemodynamic
parameter that correlated best with survival was pulmonary vascular resistance. In this study, none of the patients whose pulmonary vascular resistance exceeded 550 dyneslslcm s survived for
more than 3 yr. However, in one study of patients with COPO with
minimally raised Ppa (20 to 29 mm Hg at rest), although mortality
was 25% within 3 yr a similar percentage were alive after 10 yr
(187). These conflicting data may relate to the duration of pulmonary hypertension in an individual patient. Long-term oxygen therapy cannot account for any differences between the studies that
were carried out before the advent of this treatment. Thus, it is
clear that some patients with COPO tolerate an elevated Ppa remarkably well.
Weitzenblum and coworkers (175) also showed that although
the level of the Ppa affected survival, so did the FEy'. France and
colleagues (176), in a study of 115 patients with COPO, found that
a number of variables correlated significantly with survival, including Pao2, Paco2, FEy', and the presence of peripheral edema.
Thus, although numerous studies have shown an association between the presence of pulmonary arterial hypertension and the
prognosis in COPO, pulmonary hypertension may simply be a
reflection of the severity of the disease and may not have a direct
effect on mortality.
Prevalence and Incidence of Right Ventricular Hypertrophy
and Edema in COPO
Recent estimates of the incidence and prevalence of right ventricular hypertrophy in COPO are lacking because of the difficulty
in defining the condition clinically. In the United States, it has been
estimated that 10% to 30% of all admissions with congestive
cardiac failure are due to right ventricular hypertrophy and failure
(1, 188-193). Considering all heart diseases, cor pulmonale is
thought to account for 7% to 10% of all cases (189). An autopsy
study in the United Kingdom found evidence of right ventricular
hypertrophy in 40% of the patients with chronic bronchitis and
emphysema (190); in a larger study of 7,947 patients with chronic
lung diseases, right ventricular hypertrophy was present in 8.9%
at autopsy (20). Cor pulmonale increases in prevalence as airflow limitation worsens in patients with COPO. It is present in 40%
of patients with an FEy' < 1.0 L and in 70% when the FEy' falls
to 0.6 L (2, 152). The prevalence of cor pulmonale is also higher
in patients with hypercapnia, hypoxemia, and polycythemia (2, 152).
The development of edema in patients with hypoxic COPO occurs late in the course of the disease (194), often during acute
exacerbations of airflow limitation. However, a proportion of patients who develop pulmonary hypertension, or indeed right ventricular hypertrophy, never develop peripheral edema (195, 196).
In two studies of 100 and 59 patients with chronic bronchitis and
emphysema, respectively, who were free of edema at the time
of presentation, edema developed for the first time at a rate of
6% per annum over a 3- to 4-yr follow-up period (97, 197). In a
further study of 65 patients with COPO, of whom 58% had moderate to severe airflow limitation and most had hypoxaemia, at least
one episode of edema occurred over a follow-up period of 5.4 yr
(167).
Oxygen Transport in COPO
Survival in patients with COPO also appears to relate to oxygen
transport and mixed venous oxygenation. In a group of 50 patients with stable COPO, Kawakami and colleagues (198) assessed
840
AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
survival over 4 yr, during which time 27 of the 50 patients died.
Initial values of pulmonary hemodynamics did not distinguish between survivors and nonsurvivors, nor did the oxygen transport
or the coefficient of oxygen delivery (the ratio of oxygen transport
to oxygen consumption). However, arterial and mixed venous Po2
were significantly lower in those who died. The authors concluded
that tissue oxygenation had a greater influence on survival than
defects in oxygen transport and delivery. However, these data in
a small group of patients should be interpreted with caution (199).
Furthermore, longitudinal hemodynamic or oxygen transport data
were not available.
In theory, oxygen is supplied to the tissues by two processes.
One process is convectional transport to the tissues in the vascular system, which depends on both oxygen delivery and oxygen
consumption. The ratio of these two variables is the coefficient
of oxygen delivery (200). The other process is mixed venous oxygen tension (PV02), which is an approximation of the "mean tissue oxygen tension:' This is a determinant of the diffusion of oxygen into the tissues. Thus, PV02 can be decreased by a reduction
in Pao2 due to lung disease or due to a reduction in oxygen delivery as a result of a reduction in cardiac output caused by heart
disease. In the study by Kawakami and coworkers (198), although
there was an association between Pvo2 and mortality, the coefficient of oxygen delivery was not different between survivors and
nonsurvivors. By inference, Tenney and Mithoefer (201) suggested
that oxygen supply to the tissues is the critical factor that determines survival in such patients, and thus the diffusional (mixed
venous) component of tissue oxygen supply is more important
than the convectional transport of oxygen in the vascular system,
as measured by the coefficient of oxygen delivery.
It has been proposed that maintenance of a normal or indeed
a high cardiac output may be an adaptive mechanism in patients
with COPO to maintain a normal tissue oxygen supply. Thus, failure to maintain cardiac output may worsen survival (198). It follows that vasodilators that increase oxygen delivery by increasing cardiac output may therefore be beneficial in COPO (202).
Naeije (148) has suggested that the increase in cardiac output
induced by hypoxemia is inadequate in most patients with COPO
and hypoxemia. He studied 61 patients with COPO who were
divided into two groups on the basis of a Pvo2 greater than, less
than, or equal to 20 mm Hg. The choice of a Pvo2 above or below
20 mm Hg was based on a study by Kasnitz and colleagues (203)
that showed that a Pvo2 of ~ 20 mm Hg was associated with a
uniformly fatal outcome in patients with COPO. Oespite the presence of more severe pulmonary hypertension and a lower Pao2
in those with a low Pvo2, cardiac output was not different between
the groups. However, stroke-volume index was lower in those
whose Pvo2 was ~ 20 mm Hg (148) and may have been insufficient for the degree of hypoxemia.
Paradoxically, breathing oxygen does not always increase oxygen delivery when given to patients with COPO. In 35 patients
presenting acutely with decompensated COPO (204), 28% oxygen given for 1 h did not change cardiac output in 15 of the patients with severe hypoxemia. However, oxygen delivery increased
because of an increase in Pao2. In the remaining 20 patients with
lesser degrees of hypoxemia, oxygen delivery did not change because the increase in arterial oxygen content was offset by a fall
in cardiac output, producing no overall significant change in oxygen delivery to the tissues (204). The observation that only a
proportion of patients "respond" to oxygen therapy by increasing
oxygen delivery has been confirmed in other studies in patients
with both stable and decompensated COPO (205, 206). Thus, in
patients with COPO who develop hypoxemia, one hypothesis
VOL 150
1994
would be that an increase in cardiac output is a necessary adaptation to maintain mixed venous oxygenation in the face of a low
oxygen saturation (207). In patients with COPO, cardiac output
generally remains normal or even slightly elevated until very late
in the course of the disease (208). It follows that an inability to
increase cardiac output in the face of worsening venous hypoxemia may be a maladaption in COPO that adversely affects survival. Although unproven, this hypothesis has important implications for therapy directed at maintaining cardiac output and oxygen
delivery (209).
In summary, although the development of pulmonary arterial
hypertension and edema in patients with COPO is associated with
a poor prognosis, these features are likely to simply reflect the
severity of the underlying disease as reflected by the degree of
airflow limitation and abnormalities in gas exchange.
METHODS OF ASSESSING CARDIAC FUNCTION
IN PATIENTS WITH COPD
One of the major difficulties in assessing pulmonary hemodynamics
and right ventricular function is the need to measure pressure
and flow, which involves the use of invasive techniques such as
cardiac catheterization. Moreover, measurement of right ventricular function and chamber volumes is difficult due to the variable
and irregular shape of the right ventricle, even in normal subjects
(210). Contrast angiography was until recently the only method
to assess right ventricular volumes (211). However, this technique
is invasive and thus has not been widely used to assess patients
with COPO. More recently, noninvasive techniques have been employed to study patients with COPO. These include chest radiography, M-mode and two-dimensional echocardiography, radionuclide ventriculography, and magnetic resonance imaging.
Clinical Assessment
Clinical examinations is relatively insensitive as a means of detecting pulmonary hypertensin or right ventricular dysfunction in
patients with COPO, as clinical signs are often obscured by
hyperinflation of the chest (1, 6, 12). The jugular venous pressure
is also often difficult to assess in patients with COPO because
of large swings in intrathoracic pressure. Peripheral edema can
be due to other causes (such as hypoalbuminemia) and does not
always occur in patients with pulmonary hypertension. A systolic
left parasternal heave indicates right ventricular hypertrophy; extra heart sounds, or the murmur of tricuspid regurgitation, suggest right ventricular dysfunction, but again these are not always
present and may be modified by hyperinflation. Accentuation of
the pulmonary component of the second heart sound indicates
pulmonary hypertension but is not a sensitive indicator of pulmonary hypertension in patients with COPO.
Radiography
The presence of pulmonary arterial hypertension in patients with
COPO has been shown to relate to the width of the right descending pulmonary artery (212, 213). In a study of 61 patients with
COPO, Matthay and coworkers (213) found that the right descending pulmonary artery was> 16 mm in its widest dimension in 43
of 46 patients with pulmonary hypertension, whereas Chetty and
colleagues (214) suggested that a right descending pulmonary
artery of ~ 20 mm Hg was the best discriminant between those
patients with and without pulmonary arterial hypertension. In addition, a high value for the hilar cardiothoracic ratio was 95% sensitive and 100% specific for the presence of pulmonary hypertension in patients with COPO (214). Although measurements on
841
State of the Art: Pathophysiology of Cor Pulmonale in COPD
plain chest radiography may be useful as an initial screening test
for the presence of pulmonary arterial hypertension, they cannot
be used to predict the level of Ppa in individual patients.
Although dilation of the right ventricle gives the heart a lobular appearance, right ventricular hypertrophy or dilation is not easily discernible on a plain chest radiograph. Encroachment of the
retrosternal airspace on a lateral film can be a helpful sign to confirm that the enlarged silhouette is a result of right ventricular dilation (215).
Electrocardiography
The detection of right ventricular hypertrophy by electrocardiography appears to be highly specific but has a low sensitivity. Right
ventricular hypertrophy, identified using a number of electrocardiographic criteria, was confirmed in 75% of cases at autopsy (216).
However isolated right ventricular hypertrophy was present in only
53%, and only 25% of these patients had COPD (216).
Vector cardiography is no more sensitive than conventional
electrocardiography at predicting patients with COPD with mild
to moderate right ventricular hypertrophy (217). Similarly, there
are no advantages of other techniques such as kinetocardiography (218) or orthostatic changes in CO transfer factor, which are
also of poor predictive value for right ventricular hypertrophy in
patients with COPD (219).
Echocardiography
Hyperinflation increases the retrosternal air space, which therefore transmits sound waves poorly, making echocardiography difficult in patients with COPD. However, an adequate examination
has been reported in up to 65% to 80% of patients with COPD
(219, 220). The use of transesophageal echocardiography should
improve these results (221).
Abnormal motion of the pulmonary valve as assessed by
M-mode echocardiography has been used to detect the presence
of pulmonary hypertension. Delayed opening of the valve, midsystolic closure, and an increase in the ratio of right ventricular
pre-ejection time to total ejection time have been reported in patients with pulmonary hypertension (222, 223). Measurement of
the velocity of blood flow in the main pulmonary artery can be
used to estimate the Ppa (224). The interval between the onset
of right ventricular ejection and peak velocity, known as the time
to peak velocity, correlates fairly well with the mean Ppa in patients with COPD (r = 0.73) (225). However, a record of the flowlvelocity from the pulmonary valve may not be possible in 50% of
patients using M-mode echocardiography (226).
The addition of Doppler echocardiography has improved the
assessment of right ventricular systolic ejection flow as an estimate of Ppa (227, 228). However, relatively few studies have been
performed in patients with COPD. Two measurements are required
to estimate peak systolic Ppa: the mean right atrial pressure and
the peak systolic gradient between the right atrium and right ventricle. The addition of these two pressures yields the systolic Ppa.
It is also possible to estimate the end-diastolic Ppa noninvasively
by summing the mean right atrial pressure and the end-diastolic
gradient between the pulmonary artery and the right ventricular
outflow tract. The right atrial pressure can be estimated from the
height of the jugular venous pulse. However, there is a poor correlation between this clinical assessment and pressures measured
at catheterization, particularly in patients with COPD due to the
large swings in intrathoracic pressure (227). A fixed estimate of
right atrial pressure of between 5 and 12 mm Hg has been proposed (228); however, this can lead to considerable error. A more
accurate estimate of right arterial pressure can be obtained by
studying the degree of collapse of the proximal inferior vena cava
by echocardiography during voluntary deep inspiration (229). However, this technique becomes inaccurate in patients with COPD
because the inferior vena cava collapses spontaneously during
respiration in these patients.
Measurement of the right ventricular-atrial gradient can be assessed by Doppler echocardiography from the tricuspid valve
regurgitant jet (230). Tricuspid regurgitation occurs in normal subjects (231) and in patients with COPD (232). The high prevalence
of tricuspid regurgitation was noted as long ago as 1908 by Sir
James McKenzie during his studies of external pulses using
kymography (233). He found that tricuspid insufficiency was so
common that he was "inclined to look upon the valves as being
rarely able to close the orifice properly:' More recently, Morrison
and colleagues (232), in a study of 100 patients with COPD, found
that significant tricuspid regurgitation was present in the majority.
Similarly, in a study by Himelman and coworkers (234), tricuspid
regurgitation was detected in 20 of 36 patients with COPD. The
quality of the signal to detect tricuspid insufficiency using
continuous-wave Doppler echocardiography can be improved by
augmenting the signal with an intravenous infusion of saline (234,
235). However, this may be a problem in patients with COPD, in
whom fluid overload may already be present. From the peak velocity of the tricuspid regurgitant jet (V), the modified Bernoulli
equation (P = 4V2) enables calculation of the peak pressure difference between the right ventricle and atrium (P). As indicated
above, the addition of this pressure gradient to the mean right
atrial pressure allows calculation of the systolic Ppa.
Continuous-wave Doppler echocardiography, even with intravenous saline contrast, fails to produce an adequate assessment
in 35% of patients (236). However, pulsed-wave Doppler echocardiography appears to be an even more sensitive technique to detect tricuspid insufficiency. Using this technique, Migueres and
coworkers (225) were able to measure Ppa in 91% of patients with
COPD. Moreover, pulsed-wave Doppler echocardiography is also
capable of assessing changes in Ppa during exercise (225). Several studies have shown correlations between echocardiographic
measurements of Ppa and pressures measured at cardiac catheterization (224-228), and some of these studies are in patients
with COPD (r 0.98) (224). However, these studies are in a highly
selected group in which those patients in whom the measurement
cannot be made are "selected out."
Two-dimensional echocardiography can be used to assess right
ventricular dimensions and wall thickening and hence to detect
right ventricular volume overload in patients with COPD (219, 237,
238). This technique is more accurate than conventional M-mode
echocardiography (226). However, calculation of right ventricular
volumes is fraught with problems, including the lack of a "gold
standard" by which echocardiographic measurements of volume
can be compared (238, 239). Measurement of right ventricular
volumes by contrast angiography involves a number of assumptions and mathematical calculations, due to the irregularity of the
right ventricular cavity (214, 240).
Detection of right ventricular hypertrophy by echocardiography is limited by the ability to differentiate the right ventricular
wall from its surrounding structures. Moreover, correlations between right ventricular wall thickness and right ventricular weight
are poor, even when measured at autopsy (241,242). Measurement of right ventricular diastolic diameter by echocardiography
may be useful in detecting right ventricular enlargement. This is
particularly true in patients who have had previous episodes of
decompensated right ventricular function (219).
Changes in right ventricular function are difficult to detect by
842
AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
echocardiographyand Ooppler echocardiography in patients with
capo and pulmonary arterial hypertension. Prolongation of the
right ventricular pre-ejection time and shortening of the ejection
time may be present in such patients. However, right ventricular
systolic time intervals are also affected by increased right ventricular preload. The position and the curvature of the intraventricular septum also give an indication of right ventricular afterload.
In the normal heart, the interventricular septum moves to the left
during systolic ejection and to the right during diastolic filling. Right
ventricular volume overload tends to reverse this pattern during
cardiac ejection and filling. In addition, right ventricular pressure
overload displaces the septum further toward the left ventricle
(243).
In summary, Ooppler echocardiographic assessment of the tricuspid regurgitant jet appears to be the best method of estimating Ppa noninvasively. In patients with capo, this technique is
limited by the inability to obtain a satisfactory signal in a substantial proportion of patients and by inaccuracies in estimating the
right atrial pressure. Although impressive correlations have been
reported between Ooppler echocardiography and direct measurements of Ppa in highly selected groups of patients, this technique
cannot be used to accurately predict Ppa in individual patients
with capo.
Radionuclide Assessment of Right Ventricular Ejection Fraction
Contrast angiography has been used to measure right ventricular volumes, but the technique is difficult and tedious because
of the wide variability in right ventricular geometry (211, 214, 240,
244). Radionuclide ventriculography largely avoids this problem
and is usually performed using an intravenous injection of technetium-99m-labeled erythrocytes or human serum albumin (245).
A gamma camera is used to acquire a time/activity curve, either
during the first pass of the radiolabeled tracer through the central
circulation or by gating counts from several points throughout the
cardiac cycle once the radiotracer has equilibrated in the blood
pool (246). Because radioactive counts are proportional to volume, variations in the geometric configuration of the ventricle are
less important.
In the first-pass technique, a bolus of the radiotracer is injected
intravenously and followed during a few cardiac cycles as the bolus passes through the right side of the heart to obtain time/activity curves from a region of interest around the right ventricle. From
these time/activity curves the ejection fraction can be calculated,
based on indicator dilution theory (247). The addition of electrocardiographic gating during the first pass provides better definition of end-systole the end-diastole. The right ventricular ejection fraction (RVEF) can be calculated from the difference between
the end-diastolic and end-systolic counts, divided by the enddiastolic counts. The first-pass technique has the advantage that
the ventricles can be separated both in time and space, thus avoiding the problems of overlap between the two chambers. A major
disadvantage is the difficulty in performing sequential measurements, which requires repeated bolus injections of the radiotracer,
increasing the radiation burden to the patient. A further disadvantage is the short acquisition time during the first pass, which
produces low counts and thus statistical uncertainty in calculating the ejection fraction.
Gated-equilibrium ventriculography is usually performed using
a left anterior oblique view in order to separate the ventricles (247),
which can be achieved even in patients with capo (248). However, regions of interest must be drawn both at end-systole and
end-diastole to avoid overlap between the right atrium and right
ventricle, and a correction must be made for background counts
VOL 150
1994
(246, 248). The gated-equilibrium technique has the advantage
of providing better count statistics, since data from several hundred cardiac cycles are acquired. Moreover, repeated measurements can be made over 3 h following a single injection of a radiotracer.
The reproducibility of radionuclide measurements of RVEF appears to be good when measurements are repeated in patients
with capo studied in the same position (247) but not as good
when measurements are made on the same individual on different days (249). This may reflect the inherent variability of the RVEF
in patients with capo or variable ventricular and atrial overlap
resulting from positional changes. In 30 normal subjects, the mean
RVEF was 0.50 0.09 (range, 0.47 to 0.83) (247), giving a lower
limit of normal (two standard deviations below the mean) for RVEF
of 0.40 when measured at rest. RVEF increases in normal subject during exercise by at least 0.05 (258).
Radionuclide ventriculography therefore appears to be an ideal
technique to assess right ventricular function, because it overcomes the problems of the variations in ventricular geometry. It
has proved to be an accurate, reproducible, and noninvasive
method of assessing left ventricular global and regional function
(250). However, measurement of RVEF is more problematic. This
is due to several factors, including the overlap between the right
ventricle and right atrium and the presence, at least in a proportion of patients with capo, of significant tricuspid regurgitation
that leads to an overestimation of the RVEF (232, 251). Although
the mean RVEF in most studies of patients with capo is lower
on average than in normal subjects (245, 252-265), there is considerable overlap between values of RVEF in normal subjects and
patients with capo. Some studies suggest that only those patients who are edematous at the time of study have a low RVEF
(248,266). Indeed, values of RVEF in patients with capo are rarely
as low as in patients with right ventricular infarction (266). In most
studies, mean RVEF is greater than 0.40 when measured at rest
in patients with stable capo (254-257, 263, 265). However, the
normal increase in RVEF does not occur during exercise in such
patients (253, 254, 265, 267, 268), suggesting that latent right ventricular dysfunction is present in patients with capo.
01
'
Thallium Myocardial Scintigraphy
This technique has been used to diagnose right ventricular hypertrophy in patients with pulmonary arterial hypertension from various causes (269-272), including patients with capo (272, 273).
Oata from Weitzenblum and colleagues (273) in 46 patients with
capo showed that the sensitivity of 201thallium imaging in the
diagnosis of right ventricular pressure overloading was 73%. However, this technique is qualitative rather than quantitative and, because it has no advantage over echocardiography, has not found
favor clinically.
Right Ventricular Dimensions Measured by Magnetic
Resonance Imaging
Magnetic resonance imaging is probably now the gold standard
for measuring ventricular dimensions beoause it produces the best
images of the right ventricle (274). This technique is noninvasive
and does not impose a radiation burden on the patient. However,
it is expensive and is available only in specialized centers. Studies
in patients with capo (275) have demonstrated a correlation between the right ventricular free wall volume and both the Ppa
(r = 0.72, P < 0.01) and the pulmonary vascular resistance (r =
0.65, P < 0.01). Interestingly, the right ventricular free wall volume,
as an estimate of wall mass, correlates with the PaC02 but not
with the Pao2 (275). This noninvasive technique appears to be
843
State of the Art: Pathophysiology of Cor Pulmonale in COPD
110 ..
~
--
100
C)
a:
:z
C)
LEFT VENTRICLE
RIGHT VENTRICLE
.....
::
60
90
Y..
80
:E
70
.....
::
~
::lIII:
g; 30
~
.....
a:
C)
C)
20
en
::-
.....
::lIII:
~ ~O
en
C)
50
60
10
a:
en
50.J
I
1M
0
I
0 10 20 30100 110 120 130 1~0
MEAN PULMONARY
AORTIC PRESSURElmmHg
ARTERIAL PRESSURE
ImmHg)
0 10 20 30 40
ATRIAL PRESSURE (em H2O)
Figure 3. The effects of increasing afterload (A) and preload (B) on the right and left ventricles in the dog. Stroke
volume decreases rapidly when afterload is increased in the right ventricle, in contrast to the left ventricle, which
maintains stroke volume reasonably well against an augmented afterload (A). By contrast, stroke work of the
left ventricle increases dramatically when preload is increased, which is not the case with the right ventricle (B).
Modified from Braunwald (188).
the best method of measuring right ventricular dimensions. It can
be used to define right ventricular hypertrophy in patients with
COPO and to study the effect of therapeutic interventions.
RIGHT VENTRICULAR PHYSIOLOGY IN NORMAL
SUBJECTS AND PATIENTS WITH COPD
Normal Right Ventricular Physiology
The concave free wall and convex intraventricular septum of the
right ventricle produces a crescent-shaped chamber. The differences that exist between the two ventricles in adults appear to
be due to the different flow-resistance conditions in the two circulations (276, 277). Right ventricular contraction is achieved by three
maneuvers (22, 278, 279). First, the longitudinal axis of the chamber shortens and the trabeculae and papillary muscles force the
tricuspid valve plane downward toward the apex. This initial contraction contributes very little to the effective ejection. Thereafter,
there is contraction of the concave right ventricular free wall and
the convex septum, followed by left ventricular contraction, which
increases the curvature of the intraventricular septum. The purpose of right ventricular contraction seems to be the generation
of sufficient stroke volume to maintain an adequate cardiac output rather than the generation of pressure. Thus, the right ventricle operates as a "volume" rather than as a "pressure" pump (280).
In general, the thin-walled right ventricle, contracting against the
low-pressure pulmonary circulation, is more compliant than the
thicker-walled left ventricle. The geometric configuration of the
right ventricle is therefore more suited to ejecting large volumes
of blood with minimal myocardial shortening. This enables it to
adapt to considerable variations in systemic venous return without large changes in filling pressures (277, 280, 281) because of
the greater ratio of volume to surface area in the right compared
with the left ventricle. However, the right ventricle appears less
able to cope with an acute increase in afterload (277, 280, 281).
By contrast, the left ventricle acts as a pressure pump in the highresistance systemic circulation and has a small intracavity volume relative to its surface area (282).
Studies in the dog support the view that the right ventricle is
unable to cope with an acute increase in outflow pressure. Active
constriction of the pulmonary artery, producing only a small
change in Ppa, rapidly reduces stroke volume, whereas the stroke
volume is well maintained in the face of an increase in systemic
pressure (Figure 3). By contrast, a fourfold increase in ventricular preload, or filling pressure, induced by volume expansion has
the effect of increasing left ventricular work to five times greater
than that of the right ventricle (188). An interdependence between
the ventricles has been suggested (283), particularly in the presence of right ventricular overload that may shift the intraventricular septum leftward and impair the contractility of the left ventricle (237). However, the clinical significance of this is unknown.
Pulmonary arterial pressures in most patients with COPO and
respiratory failure are not markedly elevated (94, 148) (Table 1).
Furthermore, the rate of progression of pulmonary hypertension
is slow (167, 168). Thus, the effect on right ventricular configuration, mass, and function of moderate pulmonary hypertension,
which slowly progresses in patients with COPO, is likely to be different from the effects of acute pulmonary hypertension such as occurs in massive pulmonary embolism (284) or indeed the effects
of the sustained systemic levels of Ppa present in patients with
primary pulmonary hypertension (285). Therefore, the right ventricle has time to adapt to the modest increase in pressure load
in COPO.
Right Ventricular Function in Stable COPD
As described earlier, patients with mild COPO, without severe hypoxemia or hypercapnia, have a normal or low cardiac output and
844
AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
normal right atrial and right ventricular end-diastolic pressures
(1,286,287). The Ppa may be only slightly elevated at rest, but
it is inappropriately high for the level of the cardiac output. Ouring exercise, the Ppa rises to abnormal levels (145, 288). However, as in normal subjects, the increase in cardiac output during
exercise is proportional to the increase in oxygen consumption
(145, 288, 289). Right ventricular end-diastolic pressure also rises
to abnormal levels during exercise, and the right ventricular stroke
work, which is normal at rest in these patients, increases on exercise (146) due to an increase in pressure work against a higher
Ppa. As the disease progresses, with worsening airflow limitation and the development of chronic hypoxemia, commonly associated with chronic hypercapnia, pulmonary hypertension is
present at rest and worsens on exercise (145, 146, 288, 289). Episodes of desaturation during rapid eye movement sleep may also
increase Ppa in patients with COPO (290, 291).
Once pulmonary hypertension is established, the right ventricular stroke work index increases due to an increase in pressure work. However, in patients with stable COPO, the relation
between the right ventricular stroke work index and right ventricular end-diastolic pressure suggests that despite a higher right
ventricular stroke work index, these patients operate on an extension of the normal right ventricular function curve (146). In addition, right ventricular diastolic pressure may be normal, even
in those patients who have reported episodes of peripheral edema
and who have clinical evidence of right ventricular enlargement
(145). Thus, the presence of a normal right ventricular end-diastolic
pressure at rest in patients with COPO does not necessarily indicate that right ventricular end-diastolic volume is also normal. Exercise, however, increases right ventricular end-diastolic pressure
abnormally in the majority of patients.
Right Ventricular Mechanics in COPD
The most important factors affecting right ventricular performance
are preload, afterload, contractility, and heart rate (292, 293).
Preload. Ventricular preload is the force per cross-sectional area
acting on the ventricular muscle fiber bundles immediately before they contract (293). Changes in preload affect end-diastolic
volume, an important determinant of ventricular function, which
can be assessed by the end-diastolic pressurelstoke volume curve
(294). However end-diastolic pressure is not always an accurate
substitute for end-diastolic volume, particularly in patients with
COPO (146, 147).
After/oad. Ventricular afterload is the instantaneous tension on
the ventricular wall during active contraction (243). It is directly
related to both the intracavity pressure in the ventricle and the
internal ventricular dimension and inversely related to the ventricular wall thickness. Afterload can be measured in the left ventricle as the mean midwall circumferential wall stress and has been
shown to correlate with left ventricle ejection fraction (295). This
measurement is not possible in the right ventricle due to geometric constraints (211).
The "right ventricular hypothesis" of the development of cor
pulmonale (296, 297) suggests that RVEF is highly afterload dependent. However, correlations between Ppa and RVEF vary
widely in the literature (47, 72, 252, 258, 263, 298-306). Although
this may be partly accounted for by differences in the technique
used to measure RVEF, it should be remembered that RVEF depends not only on right ventricular afterload but also on ventricular contractility and preload. Moreover, Ppa is not an accurate
reflection of the right ventricular afterload, which is more accurately
defined as the stress or tension acting on the fibers of the right
INCREASED
CONTRACTILITY
:I:
I.LJ
0:::
//
120
0:::
/// "'HEART
FAILURE
:::>
STROKE VOLUME
<{
.-oJ
0:::
,,/
I.LJ
LJ
/
/
/
180
:::>
0:::
~NORMAL
,,-
Vl
Vl
Cl..
1994
~//
~240
VOL 150
60
I.LJ
>
15
50
100
150
VENTRICULAR VOLUME ( ml )
Figure 4. A diagramatic representation of the relation between left ventricular volume and pressure. The end-systolic pressure volume relation
is linear, but it is displaced downward and to the right in heart failure and
upwards and to the left when contractility is increased. An idealized pressurelvolume loop is included (arrow), and the curvilinear line represents
the end-diastolic pressurelvolume relation.
ventricular wall immediately after the onset of shortening (307),
ie, the force per unit cross-sectional area acting on the right ventricular wall (292). The Ppa is often used as an estimate of the
right ventricular afterload; however, it represents only a fraction
of the true afterload. Pulmonary vascular resistance may be a
slightly more accurate reflection of the true right ventricular afterload, but it is still an approximation. Thus, the RVEF should not
be regarded as a noninvasive estimation of the Ppa in patients
with COPO.
Contractility. Ventricular contractility .is a measure of the ability
of cardiac muscle to perform stroke work independent of changes
in initial fiber length (293). It is useful to assess changes in ventricular contractility that are independent of those caused byalterations in preload, afterload, or both (294). It is also important
to distinguish between "myocardial contractility" and ventricular
"pump function:' Thus, adverse loading conditions can induce the
ventricle to fail as a pump without depressing myocardial contractility. Moreover, ventricular pump function may be maintained
by favorable loading conditions in the presence of poor myocardial contractility. According to Strobeck and Sonnenblick (294),
ventricular failure should be subdivided ,into "myocardial failure,"
resulting in a decrease in the speed and force of muscle contraction that (if severe) leads to "pump failur,' and a low cardiac output, and "congestive failure," which consists of the systemic responses to an inadequate pump, such as augmentation of
sympathetic nervous system activity, renal vasoconstriction, and
activation of the renin-angiotensin system. Thus, although myocardial failure always results in congestive failure, the reverse is
not always true (308). Categorizing heart failure in this way helps
to explain the incongruity between the hemodynamic findings and
the clinical picture in patients with COPO (279).
As discussed earlier, cardiac output is normal in the majority
State of the Art: Pathophyslology of Cor Pulmonale in COPO
90
80
c:TI
70
E
E
60
u
<5
iii
50
>.
II)
~
u.
40
30
20
30
50
70
90 110 130 150 170 190
ESVI mllm 2
Figure 5. Right ventricular end-systolic pressure relationship at rest (closed
circles) and during exercise (open circles) in 24 patients with COPO. The
mean values at rest (closed triangles) and during exercise (open triangles) are shown. In most patients there is a substantial increase in right
ventricular systolic pressure without large changes in end-systolic volume
index. PRV (systolic) = right ventricular systolic pressure; ESVI = right
ventricular end-systolic volume index. From Biernacki and colleagues (306).
of patients with COPO (287), even in those with clinical signs of
"congestive failure" (114, 265, 288). The RVEF is not a good measurement of intrinsic right ventricular contractility since it also depends on preload and afterload (251). Thus, to assess the contractility or inotropic state of the right ventricle rather than its global
performance, as measured by the RVEF, it is necessary to assess a function of the ventricle that is independent of changes
in preload and afterload.
Indexes of contractility, reviewed by Sagawa (309), were initially developed to assess left ventricular function. These depend
on the relationship between the pressure and volume of the ventricle at end-systole. The end-systolic pressure-volume relation was
first developed in isolated heart preparations (309-311) but has
also been shown to be applicable, in vivo, in man (312, 313).
Changes in the relation between ventricular pressure and volume
in isolated heart preparations can be plotted as a continuous
pressure-volume loop. The end-systolic pressure-volume relation
has been shown to be independent of the initial ventricular volume (314) so that for a given contractile state, an increase in atterload produces less complete emptying of the ventricle and an
increase in end-systolic volume (315). However, the end-systolic
pressure-volume ratio remains constant, indicating that this relation is also independent of changes in afterload. In conditions of
decreased contractility, such as heart failure, the relation between
end-systolic pressure and volume in the left ventricle shifts downward and to the right, whereas increased contractility shifts the
relation upward and to the left, increasing its slope (265, 311) (Figure 4). Thus, this relation defines the inotropic state of the ventricle independent of loading conditions (310). A similar relation has
also been demonstrated in the right ventricle (316).
The slope of the end-systolic pressure-volume relation describes the interaction between afterload and systolic performance
and is termed the ventricular systolic elastance (243). The peak
845
elastance is a particularly good index of the contractile state of
the ventricle (317). The slope of the end-systolic pressure-volume
relation in the right ventricle is less than that of the left ventricle,
resulting in a greater volume change for a given change in pressure (316, 317). Measurement of the end-systolic pressure-volume
relation in the right ventricle is fraught with difficulties. The relationship may not always be linear (318) and may not be entirely
independent of the loading conditions (319), because it may also
be sensitive to changes in ventricular compliance (320). Moreover,
if measurements of right ventricular volumes are made using radionuclide ventriculography, right ventricular end-ejection and true
end-systole may not always coincide (321). Furthermore, to assess the slope of the end-systolic pressure-volume relation, measurements must be made under two or more different loading conditions (322). Allowing for these constraints, simultaneous
measurements of stroke volume by right heart catheterization
using the thermodilution technique and RVEF by radionuclide ventriculography allow quantification of right ventricular volume (323).
This, together with simultaneous measurement of right ventricular pressure, enables measurement of the end-systolic pressurevolume relation in patients with COPO as an assessment of right
ventricular contractility.
In a study of 20 patients with severe but stable COPO (318) who
were hypoxemic with variable degrees of hypercapnia and pulmonary hypertension (25 9 mm Hg), the mean end-systolic
pressurelvolume index was '.IT 16 ( SO) ml/m3 . Measurements
of the right ventricular pressure-volume relation measured as a
single point or the slope of this relation which suggest relatively
well-preserved right ventricular contractility in patieAts with COPO,
even in the face of pulmonary hypertension (323). Thus, in most
patients with COPO the end-systolic pressure-volume ratio is displaced to the left, compared with the normal values, suggesting
normal if not hypernormal right ventricular contractility. These data
have been confirmed by other researchers (263). Indeed, in one
study of patients with pulmonary hypertension secondary to left
ventricular dysfunction in which the mean Ppa was 47 12 mm
Hg (ie, much higher than in patients with stable COPO), the slope
of the pressure-volume relation was more than unity in many of
the patients, again indicating a well-preserved right ventricular
contractility in the face of a substantial increase in Ppa (324). Further data in support of the presence of relatively normal right ventricular contractility in patients with hypoxic COPO come from
studies of the effect of exercise on the right ventricular pressurevolume relation. In 24 patients with COPO, most of whom had pulmonary arterial hypertension during exercise, there was relatively
little change in the end-systolic volume, even in the face of a large
increase in right ventricular systolic pressure, which suggests good
ventricular contractility (306) (Figure 5). However, Brent and coworkers (47), in a combined radionuclidelcardiac catheterization
study, found evidence of depressed right ventricular contractility
in COPO. This discrepancy in the literature is likely to be due to
differences in the technique used to measure RVEF.
Relatively normal right ventricular function in patients with
COPO and pulmonary hypertension has also been suggested in
studies in which other indexes have been used to assess right
ventricular function. Stein and coworkers (284) measured the right
ventricular maximal isovolumic rate of development of ventricular pressure, which they found to be normal, even in those patients with pulmonary hypertension and previous evidence of "right
ventricular failure," consequent on left ventricular dysfunction. In
patients with pulmonary hypertension secondary to mitral stenosis, Wroblewski and colleagues (324) assessed right ventricular
AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
846
r----------,
I
I
:,
~ Effective Renal Plasma Flow
t Filtration Fraction
t Peritibular Oncotic Pressure
r--------
: Dopami
I
I
L
H~P02
t pC0 2
RBFt
I,- Dopamine Jl-_J __
AN_
Plasma Renin
Activity
VOl150
1994
1
t Tubular Na+-H+
Exchange
1
r---
iL AN_
Angiotensin II I
1
It Plasma
Aldosterone
r---
iAN
L _
tArginine
Vasopressin
level
Na+ Retention:
Edema
1+
---I
I
I
ne
__ J
H 0 Retention;
2
Hyponatremia
Figure 6. Mechanisms of salt and water disturbance in patients with COPO. The continuous lines and boxes
indicate the abnormalities in renal functions, salt water, and hormonal balance. The dotted lines indicate proposed protective mechanisms against this disturbance. RBF = renal blood flow; ANP = atrial natriuretic peptide;
ANG II = angiotensin II; Na+ = sodium; H+ = hydrogen ion; AVP = arginine vasopressin.
performance by plotting stroke work against end-diastolic pressure and stroke volume; this was similar to the analysis done by
Khaja and Parker (146) in patients with COPO. These authors concluded that patients with stable COPO had normal right ventricular function despite the presence of pulmonary arterial hypertension.
Recently, Chappuis and colleagues (325) developed a technique to measure right ventricular function by intravenous digital
angiography. Simultaneous measurements of right ventricular volume were generated by computer from the timeJvolume curve during the cardiac cycle and measurements of right ventricular pressure using a catheter-tip manometer. This sophisticated technique
holds some promise for measuring right ventricular function, as
does magnetic resonance imaging (326).
Right Ventricular Function in Acute Exacerbations of COPO
Although the mean Ppa is between 25 and 35 mm Hg in most
studies of patients with stable hypoxic COPO (306), during exacerbations the Ppa rises to 45 to 70 mg Hg (327-329) due to
several mechanisms that include worsening hypoxia, acidosis,
and changes in pulmonary mechanics. However, not every patient who develops pulmonary hypertension during an acute exacerbation has signs of "right ventricular failure." The pathophysiology of edema formation in COPO remains unresolved but is
unlikely to be due entirely to right ventricular dysfunction as a result of the presence of chronic but mild pulmonary hypertension
(see below).
Relatively few studies have been done in patients with COPO
who present acutely with edema (50, 114, 146,330-332). An important early study was done by Abraham and coworkers (114)
in eight patients with COPO presenting with acute respiratory failure, of whom six had peripheral edema. Hemodynamics were
measured by cardiac catheterization on the day of admission, daily
thereafter for 5 d, and again upon recovery. This study showed
convincing evidence of a rise in Ppa during exacerbations of
COPO. However, right ventricular mechanics were not measured.
In a more recent study, the end-systolic and end-diastolic volumes
in patients with COPO presenting acutely with edema were higher,
and therefore the pressure-volume ratio was lower than in stable
patients, suggesting decreased contractility in the group with
edema (331). Although cardiac output was preserved in both
groups, the right ventricle, at least by its inability to "accept and
expel the venous return" (11,12), can be said to have failed. The
increase in ventricular volume in those with edema did not appear to result from an augmented right ventricular afterload alone,
since ventricular volumes were normal in a group of patients with
a similar level of Ppa and pulmonary vascular resistance but without peripheral edema (331). Thus, the cause of the decreased right
ventricular contractility in these patients with edema remains unclear.
References
1. Fishman AP. State of the art: chronic cor pulmonale. Am Rev Respir
Dis 1976;114:n5-94.
2. Renzetti AD Jr, McClement JH, Litt BD. The Veterans Administration
cooperative study of pulmonary function. III, Mortality in relation to
respiratory function in chronic obstructive pulmonary disease. Am J
Mad 1966;41:115-9.
3. World Health Organization. Chronic cor pulmonale. A report of the expert committee. Circulation 1963;27:594-8.
4. Thomas AJ. Chronic pulmonary heart dise~. Br Heart J 1972;34:653-7.
5. Behnke RH, Blount SG, Bristo W, Carrieri V, Pierce JA, Sasahara A,
Soffer A. Primary prevention of pulmonary heart disease. Circulation
1970;41 :A17-A23.
6. McFadden ER, Braunwald E. Cor pulmonale li.nd pulmonary thromboembolism. In: Braunwald E, ed. Heart disease. Philadelphia: Saunders,
1980;1643-80.
7. Hooper RG. Chronic right heart failure: pulmonary considerations. In:
Fisk RL, ed. The right heart. Philadelphia: Davis, 1987;181-90.
8. Wiedemann HP, Matthay RA. The management of acute and chronic
cor pulmonale. In: Schard SM, Cassidy SS, eds. Heart-lung interactions in health and disease. New York: Dekker, 1989;915-82.
9. Denolin H. Clinical diagnosis of right heart failure in chronic obstructive
lung disease. In: Jezek V, Morpurgo M, Tramarin R, eds. Current topics
in rehabilitation: right ventricular hypertrophy and function in chronic
lung disease. Verona: Springer-Verlag, 1992;97-9.
10. Denolin H, Kuhn H, Krayenbuehl HP, Lodgen F, Reale A. The definition
of heart failure. Eur Heart J 1983;4:445-8.
847
State of the Art: Pathophysiology of Cor Pulmonale in COPO
11. Friedberg CK. Diseases of the heart. 3rd ed. Philadelphia: Saunders,
1966.
12. Rubin W. Pulmonary heart disease. Boston: M. Nijhoff, 1984.
13. Ferrer MI. Cor pulmonale: present day status. Am Heart J 1975;89:
657-64.
14. Rubin W, Pulmonary hypertension secondary to lung diseases. In: Weir
EK, Reeves JT, eds. Pulmonary hypertension. New York: Futura,
1984;291-320.
15. Lupi-Herrera E, Sandoval J. Seoane M, Bialostozky D. Behavior of the
pulmonary circulation in chronic obstructive pulmonary disease. Am
Rev Respir Dis 1982;126:509-14.
16. Boushy SF, Broth LB. Haemodynamic changes in chronic obstructive
pulmonary disease. Chest 1971 ;72:565-72.
17. Leading article. Oedema in cor pulmonale. Lancet 1975;2:1289-90.
18. Richens JM, Howard P. Oedema in cor pulmonale. Clin Sci 1982;
62:255-9.
19. MacNee W. Right ventricular function in cor pulmonale. Cardiology
1988;75(Suppl 1):30-40.
20. Vogt P, Ruttner JR. Das cor pulmonale aus pathologisch-anatomischer
sicht. Schweiz Med Wochenschr 19n;107:549-53.
21. Jezek V, Morpurgo M. Right heart failure in chronic lung disease. Where
are we now? In: Jezek V, Morpurgo M, Tramarin R, ads. Current topics
in rehabilitation: right ventricular hypertrophy and function in chronic
lung disease. Verona: Springer-Verlag, 1992;1-9.
22. Cumming G, Harding LK, Horsfield K, Bishop JM. Morphological aspects
of the pulmonary circulation and of the airways. In: Advisory Group
for Aerospace Research and Development NATO Conference proceedings. 1970;No. 65.
23. Singhal S, Henderson R, Horsfield K, Harding K, Cumming G. Morphometry of the human pulmonary arterial tree. Circ Res 1973;33:190-7.
24. Horsfield K. Morphometry of the small pulmonary arteries in man. Circ
Res 1978;42:593-7.
25. Heath 0, Du Shane JW, Wood EH. Edwards JE. Structure of the pulmonary trunk at different ages and in cases of pulmonary hypertension
and pulmonary stenosis. J Pathol BacterioI1959;n:443-56.
26. Von Euler US, Liljestrand G. Observations on the pulmonary arterial blood
pressure in the cat. Acta Physiol 5cand 1946;12:301-20.
27. Von Euler US, Lishajko F. Catecholamines in the vascular wall. Acta
Physiol Scand 1958;42:333-41.
28. Burton AC. Relation of structure to function of tissues of walls of blood
vessels. Physiol Res 1954;34:619-23.
29. Weibel ER. Morphometry of the human lung. Berlin: Springer-Verlag,
1963;78-82.
30. Beyers N, Doerschuk CM, Coxson H, Hogg JC. Neutrophil volume and
capillary segment diameter in the rabbit, the dog, and the human. Am
Rev Respir Dis 1989;139:A297.
31. Schmid-Schonbein GW. Shih YV, Chien S. Morphometry of human leukocytes. Blood 1985;56:866--75.
32. Chien S, Schmid-Schonbein GW, Sung KLP, Schmalzer EA, Skalak R.
Viscoelastic properties of leukocytes. In: Meiselman HJ, Lichtman MA,
Lacelle PL, ads. White cell mechanics: basic science and clinical
aspects. New York: AR Liss, 1984;19-51.
33. MacNee W, Selby C. Neutrophil kinetics in the lungs. Clin Sci 1990;
79:97-107.
34. Drinkler CK. Pulmonary oedema and inflammation. Cambridge: Harvard
University Press, 1945.
35. Robotham JL, Lixfeld W, Holland L, MacGregor 0, Bryan AC. Rabson
J. Effects of respiration on cardiac performance. J Appl Physiol
1978;44:703-9.
36. Thomas W, Griffo ZJ, Roose A. Effect of negative-pressure inflation of
the lung on pulmonary vascular resistance. J Appl Physiol 1961;
16:451-6.
37. Weibel ER, Gomez OM. The architecture of the human lung. Science
1962; 137:5n-85.
38. Bainbridge FA. The physiology of muscular exercise. 3rd ed. (Rewritten
by A.V. Bock and D.B. Dill). London: Longmans & Green, 1931.
39. Knapp E, Gureiner R. Reduction of pulmonary hypertension by nitroprusside. Int J Clin Pharmacol Ther ToxicoI19n;15:75-80.
40. Pace JB. Pulmonary vascular response to sodium nitroprusside in
anesthetized dogs. Anesth Analg 1978;57:551-7.
41. Weir EK, Reeves JT, Grover RE. Prostaglandin E inhibits the pulmonary vascular pressor response to hypoXia and prostaglandin F2.
Prostaglandins 1975;10:623-31.
42. Harris P, Heath D. Normal variations in pressure and flow. In: Harris
P, Heath D. eds. The human pulmonary circulation. 3rd ed. Edinburgh:
Churchill Livingstone, 1986;149-60.
43. West JB, Dollary CT, Naimark A. Distribution of blood flow in isolated
lung: relation to vascular and alveolar pressures. J Appl Physiol
1964;19:713-24.
44. Murray JF. The normal lung. Philadelphia: Saunders, 1986.
45. Donald KW, Bishop JM, Cumming G, Wade OL. The effect of exercise
on the cardiac output and circulatory dynamics of normal subjects.
Clin Sci 1955;14:37-73.
46. Sionin MB, Rabin A, Balchum OJ, Dressler SH. The effect of mild exercise in the supine position on the pulmonary arterial pressure of five
normal human subjects. J Clin Invest 1954;33:1022-30.
47. Brent BN, Berger HJ, Matthay RA, Mahler 0, Pytlik L, Zaret BL. Physiologic correlates of right ventricular ejection fraction in chronic obstructive pulmonary disease. A combined radionuclide hemodynamic study.
Am J Cardiol 1982;50:255-62.
48. Riley RL, Himmelstein A, Morley HL, MoUey HL, Weiner HM, Cournand
A. Studies of the pulmonary circulation at rest and during exercise
in normal individuals and in patients with chronic pulmonary disease.
Am J PhysioI1948;152:372-82.
49. Harris P, Heath D. Resistance. In: Harris P, Heath 0, eds. The human
pulmonary circulation. 3rd ed. Edinburgh: Churchill Livingstone.
1986;122-35.
50. Lockhart A, Tzareva M, Nader F, Leblanc R, Schrijen F, Sadoul P.
Elevated pulmonary artery wedge pressure at rest and during exercise in chronic bronchitis-fact or fancy? Clin Sci 1969;37:503-17.
51. Carlen SE, Hansen HE, NordenstOm B. Temporary unilateral occlusion
of the pulmonary artery. J Thorac Surg 1951;22:527-36.
52. Segel N, Bishop JM. The circulation in patients with chronic bronchitis
and emphysema at rest and during exercise with special reference
to the influence of change in blood viscosity and blood volume on the
pulmonary circulation. J Clin Invest 1966;45:1555-68.
53. Widimsky J. Pressure flow and volume changes in the lesser circulation
during pulmonary artery occlusion in healthy subjects and patients
with pulmonary hypertension. Progress in Respiratory Research
1970;5:224-36.
54. Harris P, Segel N, Bishop JM. The relation between pressure and flow
in the pulmonary circulation in normal subjects and in patients with
chronic bronchitis and mitral stenosis. Cardiovasc Res 1968;2:73-83.
55. Fishman AP. Respiratory gases in the regulation of pulmonary circulation. Physiol Rev 1961;41:214-80.
56. Hasleton PS, Heath 0, Brewer DB. Hypertensive pulmonary vascular
disease in states of chronic hypoxia. J Pathol BacterioI1968;95:431-40.
57. Lamb D. Pathology of COPD. In: Brewis RAL, Gibson GJ, Geddes OM,
eds. Respiratory medicine. London: Bailliere Tindall, 1990;497-507.
58. Wilkinson M, Langhorn CA, Heath 0, Barer GR, Howard P. A pathophysioJ Med 1988;
logical stUdy of 10 cases of hypoxic cor pulmonale.
66:65-85.
59. Wright JL, Lawson L, Pare PO, Hooper RO, Peretz 01, Nelems JM, Schulzer M, Hogg JC. The structure and function of pulmonary vasculature
in mild chronic obstructive pulmonary disease;the effect of oxygen
on exercise. Am Rev Respir Dis 1983;128:702-7.
60. Magee F, Wright JL, Wiggs BR, Pare PO, Hogg JC. Pulmonary vascular structure and function in chronic obstructive pulmonary disease.
Thorax 1988;43:183-9.
61. Dunnill MS. Fibrinoid necrosis in the branches of the pulmonary artery
and chronic non-specific lung disease. British Journal of Diseases of
the Chest 1960;54:355-60.
62. Harris P, Heath D. The pulmonary vasculature in emphysema. In: Harris
P, Heath 0, eds. The human pulmonary circulation. Edinburgh: Churchill Livingstone, 1986;507-21.
63. Bignion J, Khoury F, Even P, Andre J, Brouet G. Morphometric study
in chronic obstructive broncho-pulmonary disease. Pathologic, clinical and physiologic correlations. Am Rev Respir Dis 1969;99:669-95.
64. Hale KA, Niewoehner DE, Cosio MG. Morphologic changes in the muscular pulmonary arteries: relationship to cigarette smoking, airway disease and emphysema. Am Rev Respir Dis 1980;122:273-8.
65. Horan LG, Flowers NC, Havelda CJ. Relation between right ventricular
mass and cavity size: an analysis of 1500 human hearts. Circulation
1981 ;64:135-8.
66. Abraham AS, Kay JM, Cole RB, Pincock AC. Haemodynamic and pathological study of the effect of chronic hypoxia and subsequent recovery of the heart and pulmonary vasculature of the rat. Cardiovasc Res
1971 ;5:95-102.
67. Fishman AP. Hypoxia and its effects on the pulmonary circulation. How
and where it acts. Circ Res 1979;38:221-31.
68. Penaloza 0, Sime F. Chronic cor pulmonale due to loss of altitude acclimatization (chronic mountain sickness). Am J Med 1971 ;50:728-43.
69. Calverley PMA, Howitson R, Lamb 0, Flenley DC. Clinicopathological
correlations in hypoxic cor pulmonale. Thorax 1992;47:494-8.
70. Moret PRo Hypoxia and the heart, vol 2. In: Bourne GH, ed. Hearts and
heart-like organs. New York: Academic press, 1980:338-87.
71. Hickam JB, Cargill WHo Effect of exercise on cardiac output and pulmonary arterial pressure in normal persons and in patients with cardiovascular disease and pulmonary emphysema. J Clin Invest 1948;
27:10-23.
72. Mahler DA, Brent BN, Loke J, Zaret BL, Matthay RA. Right ventricular
performance and central circulatory hemodynamics during upright exercise in patients with chronic obstructive pulmonary disease. Am Rev
Respir Dis 1984;130:722-9.
848
AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
73. limt PK, Brownlee WE. Pulmonary haemodynamics in obstructive lung
diseases. Diseases of the Chest 1968;53:113-7.
74. Wilhelmsen L, Selander S, Sonderholm B, Paulin S, Varnauskas E, Werko
l. Recurrent pulmonary embolism. Medicine 1963;42:335-55.
75. Thurlbeck WM, Henderson JA, Fraser RG, Bates DV. Chronic obstructive lung disease. A comparison between clinical, roentgenologic, functional and morphologic criteria in chronic bronchitis, emphysema,
asthma and bronchiectasis. Medicine 1970;49:81-145.
76. Hicken P, Brewer D, Heath D. The relation between the weight of the
right ventricle of the heart and the internal surface area and the number of alveoli in the human lung in emphysema. J Pathol Bacteriol
1966;92:529-46.
77. Mounsey JPD, Ritzman LW, Selverstone NH, Briscoe WA, Mclemore
GA. Circulatory changes in severe pulmonary emphysema. Br Heart
J 1952;14:153-72.
78. Weitzenblum E, Roeslin N, Hirth C, Oudet P. A comparative study of
clinical and functional data between chronic bronchitis and primary
emphysema. Respiration 1970;27:493-510.
79. Thurlbeck WM, Simon G., Radiographic appearance of the chest in emphysema. Am J Roentogenol 1978;130:429-40.
80. MacNee W, Gould G, lamb D. Quantifying emphysema by CT scanning: clinicopathological correlates. In: Ann N Y Acad Sci
1991;624:179-94.
81. Gould GA, MacNee W, Mclean A, Warren PM, Redpath A, Best JJK,
Lamb D, Flenley DC. CT measurements of lung density in life can quantitate distal airspace enlargement-an essential defining feature of
human emphysema. Am Rev Respir Dis 1988;137:380-92.
82. Biernacki W, Gould GA, Whyte KF, Flenley DC. Pulmonary
hemodynamics, gas exchange and the severity of emphysema as assessed by quantitative CT scan in chronic bronchitis and emphysema.
Am Rev Respir Dis 1989;139:1509-15.
83. Fritts HW, Odell JE, Harris P, Braunwald EW, Fishman AO. Effects of
acute hypoxia on the volume of blood in the thorax. Circulation
1960;22:216-9.
84. Harris P, Bishop JM, Segel N. The influence of guanethidine on hypoxic pulmonary hypertension in normal man. Clin SCi 1961 ;21 :295-300.
85. Harvey RM, Ferrer MI, Richards OW, Cournand A. Influence of chronic
pulmonary disease on the heart and circulation. Am J Med 1951;
10:719-38.
86. Fishman AP, Fritts HW, Cournand A. Effects of acute hypoxia and exercise on the pulmonary circulation. Circulation 1960;22:204-15.
87. Emirgil C, Sobol BJ, Herbert WHo Routine pulmonary function studies
as a key to the status of the lesser circulation in chronic obstructive
pulmonary disease. Am J Med 1971 ;50:191-9.
88. Fowler NO, Westcott RN, Scott RG, Hess E. The cardiac output in chronic
cor pulmonale. Circulation 1952;6:888-93.
89. Horsfield K, Segal N, Bishop JM. The pulmonary circulation in chronic
bronchitis at rest and during exercise breathing air and 80% oxygen.
Clin Sci 1968;34:473-83.
90. Millard J, Reid l. Right ventricular hypertrophy and its relationship to
chronic bronchitis and emphysema. British Journal of Diseases of the
Chest 1974;68:103-10.
91. Whitaker W. Pulmonary hypertension in congestive heart failure complicating chronic lung disease. Q J Med 1954;23:57-72.
92. Williams JF, Behuke RH. The effect of pulmonary emphysema upon cardiopulmonary hemodynamics at rest and during exercise. Ann Intern
Med 1964;60:824-42.
93. Yu PN, Lovejoy FW, Joos HA, Nye RE, McCann WS. Studies of pulmonary hypertension. I, Pulmonary circulatory haemodynamics in patients with pulmonary emphysema at rest. J Clin Invest 1953;32:130-7.
94. Bishop JM, Cross KW. Use of other physiological variables to predict
pulmonary arterial pressure in patients with chronic respiratory
disease-a multicentre study. Eur Heart J 1981;2:509-17.
95. Wilson RH, Hoseth W, Dempsey MG. The effects of breathing 99.6%
oxygen on pulmonary vascular resistance and cardiac output in patients with pulmonary emphysema and chronic hypoxia. Ann Intern
Med 1955;42:629-37.
96. Kitchen AH, lowther CP, Mathews MD. The effects of exercise and breathing oxygen-enriched air on the pulmonary circulation in emphysema.
Clin SCi 1961;21:93-106.
97. Aber GM, Harris AM, Bishop JM. Effect of acute changes in inspired
oxygen concentration on cardiac, respiratory, and renal function in
patients with chronic obstructive airways disease. Clin Sci 1964;
26:133-43.
98. Sirna F, Penaloza 0, Ruiz l. Bradycardia, increased cardiac output, and
reversal of pulmonary hypertension in altitude natives living at sea
level. Br Heart J 1971;33:647-57.
99. Aber GM, Bayley TJ, Bishop JM. Inter-relationships between renal and
cardiac function and respiratory gas exchange in obstructive airways
disease. Clin Sci 1963;25:159-70.
100. Kilburn KH, Asmundsson T, Britt RC, Cardon R. Effects of breathing
VOL 150
1994
100k carbon dioxide on the pulmonary circulation of human subjects.
Circulation 1969;39:639-53.
101. Rokseth R. The effect of altered blood carbon dioxide tension and pH
on the human pulmonary circulation. Scand J Clin Lab Invest 1966;
18(Suppl):90-4.
102. Harris P, Segel N, Green J, Housley E. The influence of the airways
resistance and alveolar pressure on the pulmonary vascular resistance
in chronic bronchitis. Cardiovasc Res 1968;2:84-94.
103. Durand J, leroy-ladurie M, Ransom-Bitker B. Effects of hypoxia and
hypercapnia on the repartition of pulmonary blood flow in supine subjects. Progress in Respiratory Research 1970;5:156-65.
104. Enson Y, Guintini C, lewis Ml, Morris TQ, Ferrer MI, Harvey RM. The
influence of hydrogen ion concentration and hypoxia on the pulmonary circulation. J Clin Invest 1964;43:1146-62.
105. Harvey RM, Enson Y, Betti R, Lewis ML, Rochester DF, Ferrer MI. Further considerations of the causes of pulmonary hypertension in cor
pulmonale. Bulletin European de Physiopathologie Respiratoire
1967;3:623-32.
106. Housley E E, Clarke SW, Hedworth-Whitty RB, BishopJM. Effect of acute
and chronic acidaemia and associated hypoxia on the pulmonary circulation of patients with chronic bronchitis. Cardiovasc Res 1970;
4:482-9.
107. Bergofsky EH, Lehr DE, Fishman AP. Effect of changes in the hydrogen ion concentration on the pulmonary circulation. J Clin Invest
1962;41 :1492-501.
108. Campbell EJM, Short OS. The cause of oedema in 'cor pulmonale.' lancet 1960;1 :1184-6.
109. lockhart A, Nader F, Tzareva M, Schrijen F. Comparative effects of exercise and isocapnic voluntary hyperventilation on pulmonary haemodynamics in chronic bronchitis and emphysema. Eur J Clin Invest
1970;1 :69-76.
110. Weitzenblum E, el-Gharbi T, Vandevenne A, Bleger A, Hirth C, Oudet
P. Pulmonary haemodynamic changes during muscular exercise in
non-decompensated chronic bronchitis. Bulletin European de Physiopathologie Respiratoire 1972;8:49-71.
111. Matthay RA, Niederman MS, Weidemann HP. Cardiovascular-pulmonary
interaction in chronic obstructive pulmonary disease with special reference to the pathogenesis and management of core pulmonale. Med
Clin North Am 1990;74:571-618.
112. Abraham AS, Hedworth-Whitty RB, Bishop JM. Effects of acute hypoxia and hypervolemia singly and together upon the pulmonary circulation in patients with chronic bronchitis. Clin Sci 1967;33:371-80.
113. Raffestin B, Valette H, Herbert Jl, Duhaze P, lockhart A. Pulmonary
blood volume in chronic bronchitis. Clinical Science and Molecular
Medicine 1977;53:587-93.
114. Abraham AS, Cole RB, Green 10, Hedworth-Whitty RB, Clarke SW, Bishop
JM. Factors contributing to the reversible pulmonary hypertension in
patients with acute respiratory failure studied by serial observations
during recovery. Circ Res 1969;26:51-60.
115. Wedzicha JA, Rudd RM, Apps MC, Cotter FE, Newland AC, Empey OW.
Erythrapheresis in patients with polycythemia secondary to hypoxic
lung disease. Br Med J 1983;286:511-4.
116. Fishman AP. Pulmonary circulation. In: Handbook of physiology. The
respiratory system. Circulation and non-respiratory function, vol 1.
Bethesda MD: American Physiological Society 1985;93-166.
117. Reeves JT, Voelkel NF. Mechanisms of chronic pulmonary hypertension: basic considerations. In: Wagenvoort A, Denolin H, eds. Pulmonary circulation, advances and controversies. Amsterdam: Elsevier,
1989;27-39.
118. Leeman M, Neite R, lejeune P, Melot C. Influence of cyclooxygenase
inhibition and leukotriene receptor blockade on pulmonary vascular
pressure: cardiac index relationships in hyperoxic and in hypoXic dogs.
Clin Sci 1987;72:717-24.
119. Morganroth MI, ReevesJT, Murphy RC, Voelk~1 F.leukotriene synthesis and receptor blockers, block hypoxic pulmonary vasoconstriction.
J Appl Physiol 1984;56:1340-6.
120. McDonnell TJ, Wescott JY, Czartolomna J, Voelkel N. Role of peptidoleukotrines in hypoxic pulmonary vasoconstriction in the rat. Am J Physiol 1990;259:H751-58.
121. Post JM, Hume JR, Archer SL, Weir EK. Direct ~ole for potassium channel inhibition in hypoxic pulmonary vasoconstriction. Am J Physiol
1992;262:C882-90.
122. Myers PR, Minor Rl, Guerra R, Bates IN, Harrison DG. Vasorelaxant
properties of the endothelium-derived relaxing factor more closely
resemble S-nitrosocysteine nitric oxide. Nature 1990;345:167-73.
123. Rubanyi GM, Romero JC, Van Houtte PM. Flow induced release of
endothelium-derived relaxing factor. Am J PhysioI1986;250:H1105-49.
124. Murad F. Cyclic guanosine monophosphate as a mediator of vasodilatation. J Clin Invest 1986;78:1-5.
125. Thorn S, Hughes A, Martin G, Sever PS. Endothelium-dependent relaxation in isolated human arteries and veins. Clin Sci 1987;73:547-52.
State of the Art: Pathophysiology of Cor Pulmonale in COPD
126. Greenberg B, Rhoden K, Barnes PJ. Endothelium-relaxation of human
pulmonary arteries. Am J Physiol 1987;252:H434-8.
127. Dinh-Xuan AT, Higenbollam TW, Clelland CA, Pepke-ZabaJ, Wells FC,
Wallwork J. Acetylcholine and adenosine diphosphate cause endothelium-dependent relaxation of isolated human pulmonary arteries.
Eur Respir J 1990;3:633-8.
128. Yamaguchi T, Rodman DM, O'Brian RF, McMurty I. Modulation of pulmonary artery contraction by endothelium-relaxing factor. Eur J Pharmacol 1989;161 :259-62.
129. Din-Xuan AT, Higenbollam TW, Clelland CA, Pepke-Zaba J, Cremona
G, BUll AY, Large SR, Wells FC, Wallwork J. Impairment of
endothelium-dependent pulmonary artery relaxation in chronic obstructive lung disease. N Engl J Med 1991;324:1539-47.
130. Palmer RMJ, Ashton DS, Moncad AS. Vascular endothelial cells synthesise oxide from L-arginine. Nature 1988;333:664-6.
131. Crawley DE, Liu SF, Evans TW, Barnes PJ. Inhibitory role of endotheliumderived relaxing factor in rat and human pulmonary arteries. Br J Pharmacol 1990;101:166-70.
132. Liu SF, Crawley DE, Barnes PJ, Evans TW. Endothelium-derived relaxing factor inhibits hypoxic pulmonary vasoconstriction in rats. Am Rev
Respir Dis 1991 ;143:32-7.
133. Meyrick B, Reid L. The effect of continued hypoxia on rat pulmonary
arterial circulation: an ultra-structural study. Lab Invest 1978;38:
188-200.
134. Adnot S, Raffestin B, Addahibi S, Braquet P, Chabrier PE. Loss of
endothelium-dependent relaxant activity in the pulmonary circulation
of rats exposed to chronic hypoxia. J Clin Invest 1991 ;87:155-62.
135. Moncada S, Palmer RMJ, Higgs EA. Prostacyclin and endothelial-derived
relaxing factor: biological interactions and significance. In: Verstraete
M, Verrmylen J, Lijnen RH, eds. Thombosis and haemostasis. Belgium: University Press Leuven, 1987;597-618.
136. Ignarro LJ, Biological actions and proporties of endothelium-derived nitric oxide formed and released from artery and vein. Circ Res
1989;65:1-21.
137. Dinh-Xuan AT. Endothelial modulation of pulmonary vascular tone. Eur
Respir J 1992;5:757-62.
138. Gurtner HP, Walser P, Fassler B. Normal values for pulmonary haemodynamics at rest and during exercise in man. Progress in Respiratory Research 1975;9:295-315.
139. Guyton AC, Lindsay AW, Gilluly J. The limits of right ventricular compensation following acute increase in pulmonary circulation resistance.
Circ Res 1954;2:326-32.
140. Howarth S, McMichael J, Sharpey-8chafer EP. Effects of oxygen venesection and digitalis on chronic heart failure from disease of the lungs.
Clin Sci 1947;287:1159-60.
141. Even P, Duroux P, Ruff R, Caubarrere I, Brouet G, de Vernejoul P. The
pressure-flow relationship of the pulmonary circulation in normal man
and in chronic obstructive pulmonary disease: effects of muscular exercise. Scandinavian Journal of Respiratory Disease 1971 ;Suppl
77:72-6.
142. Burrows B, Strauss RH, Nider AH. Chronic obstructive lung disease.
III, Interrelationships of pulmonary function data. Am Rev Respir Dis'
1965;91 :861-8.
143. Boushy SF, North LB. Haemodynamic changes in chronic obstructive
pulmonary disease. Chest 1977;72:565-70.
144. Burrows B, Kellel LJ, Niden AH, Rabinowitz M, Dierer CF. Pallerns of
cardiovascular dysfunction in chronic obstructive lung disease. N Engl
J Med 1972;286:912-8.
145. Jezek V, Schrijen F, Sadoul P. Right ventricular function and pulmonary haemodynamics during exercise in patients with chronic obstructive bronchopulmonary disease. Cardiology 1973;58:20-31.
146. Khaja F, Parker JO. Right and left ventricular performance in chronic
obstructive lung disease. Am Heart J 1971 ;82:319-27.
147. Harris P, Heath D. Pulmonary haemodynamics in chronic bronchitis and
emphysema. In: Harris P, Heath D, eds. The human pulmonary circulation, 3rd ed. Edinburgh: Churchill Livingstone, 1977;522-44.
148. Naeije R. Should pulmonary hypertension be treated in chronic obstructive
pulmonary disease? In: Weir EK, Archer SL, Reeves JT, eds. The diagnosis and treatment of pulmonary hypertension. New York: Futura
Publishing, 1992;209-39.
149. Burrows B, FletcherCM, Heard BE, Jones NL, WoatliffJS. Emphysematous and bronchial types of chronic airways obstruction: clinicopathological study of patients in London and Chicago. Lancet 1966;1 :830-5.
150. Burrows B, Strauss RH, Nider AH. Chronic obstructive lung disease.
III, Interrelationships of pulmonary function data. Am Rev Respir Dis
1965;91:861-8.
151. Medical Research Council. Definition and classification of chronic bronchitis for clinical and epidemiological purposes. Lancet 1965;1 :775-9.
152. Mitchell RS, Vincent TN, Filley GF. Chronic obstructive bronchopulmonary disease. IV, The clinical and physiological differential of chronic
bronchitis and emphysema. Am J Med Sci 1964;247:513-7.
849
153. Dornhorst AC. Respiratory insufficiency. Lancet 1955;1:1185-7.
154. Scadding JG. Meaning of diagnostic terms in bronchopulmonary disease. Br Med J 1963;2:1425-30.
155. Burrows B, Fletcher CM, Heard BE, Jones NL, Woalliff JS. Clinical types
of chronic obstructive lung disease in London and in Chicago: a study
of 100 patients. Am Rev Respir Dis 1964;90:14-27.
156. Robin ED, O'Neill RP. The fighter versus the non-fighter. Control of ventilation in chronic obstructive pulmonary disease. Arch Environ Health
1963;7:125-9.
157. Filley GF. Emphysema and chronic bronchitis: clinical manifestations
and their physiologic significance. Med Clin North Am 1967;51 :283-92.
158. Filley GF, Beckwill HJ, Reeves JT, Mitchell RS. Chronic obstructive bronchopulmonary disease. II, Oxygen transport in two clinical types. Am
J Med 1968;44:26-38.
159. College of General Practitioners. Chronic bronchitis in Great Britain. Br
Med J 1961 ;2:973-9.
160. Mitchell RS, Maisel JC, Dart GA, Silvers GW. The accuracy of the death
certificate in reporting cause of death in adults: with special reference
to chronic bronchitis and emphysema. Am Rev Respir Dis 1971 ;104:
844-50.
161. Richards DW. Pulmonary emphysema: etiologic factors and clinical forms.
Ann Intern Med 1960;53:1105-20.
162. Thurlbeck WM. Chronic airflow obstruction in lung disease. In: Bennington
JL, ed. Major problems in pathology. London: Saunders, 1976;350-444.
163. Jamal K, Fleetham JA, Thurlbeck WM. Cor pulmonale: correlation with
central airways lesions, peripheral airway lesions, emphysema, and
control of breathing. Am Rev Respir Dis 1990;141:1172-7.
164. Fishman AP. Primary pulmonary hypertension more light or more tunnel? Ann Intern Med 1981;94:815-7.
165. Sadoul P, Schrijen F, Uffholtz H, Pham QT. Evolution clinique de 195
pulmonares soumis a un catheterisme du coeur droit entre 1957 et
1965. Bulletin European de Physiopathologie Respiratoire 1968;
4:225-40.
166. Schrijen F, Uffholtz H, Polu JM, Poincelot F. Pulmonary and systemic
hemodynamic evaluation in chronic bronchitis. Am Rev Respir Dis
1978;117:25-31.
167. Weitzenblum E, Hirth C, Parini JP, Rasaholinjanahary J, Oudet P. Clinical, functional and pulmonary haemodynamic course of patients with
COPD followed up over 3 years. Respiration 1978;36:1-9.
168. Weitzenblum E, Loiseau A, Hirth C, Mirhom R, Rasaholinjanahary J.
Course of pulmonary haemodynamics in patients with chronic obstructive pulmonary disease. Chest 1979;75:656-62.
169. Weitzenblum E, Sautejeau A, Ehrhart M, Mammosser M, Pelletier A.
Long-term course of pulmonary arterial pressure in chronic obstructive pulmonary disease. Am Rev Respir Dis 1984;130:993-8.
170. Medical Research Council Working Party. Long-term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic
bronchitis and emphysema. Lancet 1981;1:681-6.
171. Reid LM. Chronic obstructive pulmonary disease. In: Fishman AP, ed.
Pulmonary disease and disorders. 2nd ed. New York: Marcel Dekker,
1979;387-426.
172. Howard P. The changing face of chronic bronchitis with airways obstruction. Br Med J 1974;2:89-93.
173. Registrar General Scotland. Annual report. Edinburgh: HMSO Bookshops, 1989.
174. Hodgkin JE. Prognosis in chronic obstructive pulmonary disease. Clin
Chest Med 1990;11 :555-69.
175. Weitzenblum E, Hirth C, Ducolone A, Mirhom R, Rasaholinjanahary J,
Ehrhart M. Prognostic value of pulmonary artery pressure in chronic
obstructive pulmonary disease. Thorax 1981 ;36:752-8.
176. France AJ, Prescoll RJ, Biernacki W, Muir AL, MacNee W. Does right
ventricular function predict survival in patients with chronic obstructive pulmonary disease? Thorax 1988;43:621-6.
177. Cooper CB, Waterhouse J, Howard P. Twelve year clinical study of patients with hypoxic cor pulmonale given long-term domiciliary oxygen
therapy. Thorax 1987;42:105-10.
178. Boushy SF, Adhikari PK, Sakamoto A, Lewis BM. Factors affecting prognosis in emphysema. Respiratory Diseases 1964:45:402-11.
179. Kanner RE, Renzelli AD, Stanish WM, Barkman HW, Klauber MR. Predictors of survival in subjects with chronic airflow limitation. Am J Med
1983;74:249-55.
180. Kawakami Y. Prognostic factors in COPD: the importance of pulmonary
haemodynamic variables. Practical Cardiology 1985;11 :124-37.
181. Kok-Jensen A, Sorenson E, Damsgaard T. Prognosis in severe chronic
obstructive pulmonary disease. Scandinavian Journal of Respiratory
Disease 1974;55:120-8.
182. Mitchell RS, Webb NF, Filley GF. Chronic obstructive bronchopulmonary disease. III, Factors influencing prognosis. Am Rev Respir Dis
1964;89:878-96.
183. Sahn SA, Nell LM, Pelly TL. Ten-year follow-up of a comprehensive rehabilitation program for severe COPD. Chest 1980;77(Suppl):311-4.
850
AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
184. Simpson T. Chronic bronchitis and emphysema with special reference
to prognosis. British Journal of Diseases of the Chest 1968;62:57-69.
185. Traver GA, Cline MG, Burrows B. Predictors of mortality in chronic obstructive pulmonary disease. Am Rev Respir Dis 1979;119:895--902.
186. Massin N, WestphalJL, Schrijen F, Polu JM, Sadoul P. Valeur prognostique du bilan hamodynamique des bronchiteaux chroniques. Bulletin Europeen de Physiopathologie Respiratoire 1979;15:821-37.
187. Ourednik A, Susa Z. How long does the pulmonary hypertension last
in chronic obstructive bronchopulmonary disease? Progress Respiratory Disease 1975;9:24-8.
188. Braunwald E. Pathophysiology of heart failure. In: Braunwald E, ed. Heart
disease. A textbook of cardiovascular medicine. Philadelphia: Saunders, 1980;453-71.
189. Feldman NT, Ingram RH Jr. Chronic cor pulmonale. In: Hutst JW, Logue
RB, Schlant RC, Wenger NK, eds. The heart, arteries and veins. New
York: McGraw Hill, 1978;1485.
190. Heath D, Brewer D, Hicken P. Mechanisms and Pathology In: Thomas
CC, ed. Cor pulmonale in emphysema. Springfield: Thomas, 1968;
1-37.
191. Intersociety Commission for Heart Disease Resources. Primary prevention
of pulmonary heart disease. Circulation 1970;41:A17-23.
192. Bouchy SF, Adhikari PK, Sakamoto A. Lewis BM. Factors affecting prognosis in emphysema. Diseases of the Chest 1964;45:402-11.
193. Burrow SB, Earle RH. Course and prognosis of chronic obstructive lung
disease: a prospective study of 200 patients. N Engl J Med 1969;
280:397-404.
194. Berbel LN, Miro RE. Pulmonary hypertension in the pathogenesis of cor
pulmonale. Cardiovasc Rev 1983;4:356-63.
195. Diener CF, Burrows B. Further observations on the course and prognosis of chronic obstructive lung disease. Am Rev Respir Dis 1975;
111 :719-24.
196. Jones NL, Burrows B, Fletcher CM. Serial study of 100 patients with
chronic airway obstruction in London and Chicago. Thorax
1967;22:327-35.
197. Bates DV, KnottJMS, Christie RV. Respiratory function in emphysema
J Med 1956;25:137-57.
in relation to prognosis.
198. Kawakami Y, Kishi F, Yamamoto H, Miyamoto K. Relation of oxygen
delivery, mixed venous oxygenation and pulmonary hemodynamics
to progress in chronic obstructive pulmonary disease. N Engl J Med
1983;308:1046-9.
199. Tockman MS, Permutt S, Kennedy T. Prognosis in chronic obstructive
pulmonary disease (letter). N Engl J Med 1983;308:992-3.
200. Mithoefer JC, Holford FD, Keighley JFH. The effect of oxygen administration on mixed venous oxygenation in chronic obstructive pulmonary disease. Chest 1974;66:122-32.
201. Tenney SM, Mithoefer JC. The relationship of mixed venous oxygenation to oxygen transport: with special reference to high altitude and
pulmonary disease. Am Rev Respir Dis 1982;125:474-9.
202. Kawakami Y, Terai T, Yamamato H, Murao M. Exercise and oxygen inhalation in relation to prognosis of chronic obstructive pulmonary disease. Chest 1982;81 :182-8.
203. Kasnitz P, Druger GL, Yorra F, Simmons DH. Mixed oxygen tension and
hyperlactatemia. Survival in severe cardiopulmonary disease. JAMA
1976;236:570-4.
204. Degaute D, Domenighetti G, Naeije R, Vincent JL, Treyvaud D, Perret
CI. Oxygen delivery in acute exacerbation of chronic obstructive pulmonary disease. Effects of controlled oxygen therapy. Am Rev Respir
Dis 1981;124:26-30.
205. Corriveau ML, Rosen BJ, Dolan GF. Oxygen transport and oxygen consumption during supplemental oxygen administration in patients with
chronic obstructive pulmonary disease. Am J Med 1989;87:633-7.
206. Bergofsky EH. Tissue oxygen delivery and cor pulmonale in chronic obstructive pulmonary disease with and without heart failure. Am J Cardiol
1963;11 :477-82.
207. Bergofsky EH. Tissue oxygen delivery and cor pulmonale in chronic obstructive pulmonary disease. N Engl J Med 1983;308:1092-4.
208. Finlay M, Middleton HC, Peake MD, Howard P. Cardiac output pulmonary hypertension, hypoxaemia and survival in patients with chronic
obstructive airways disease. Eur J Respir Dis 1983;64:252-63.
209. Howard P. Drugs or oxygen for hypoxic cor pulmonale? Br Med J
1983;287:1159-60.
210. Arcilla RA, Tsai P, Thilenus 0, Ranniger K. Angiographic method for
volume estimation of the right and left ventricles. Chest 1971 ;60:446-54.
211. Gentzler R, Briselli M, Gault J. Angiographic estimation of right ventricular volume in man. Circulation 1974;4:1-55.
212. Kirch E. Die pathologische anatomie des cor pulmonale. Verh Deutsch
Ges Kreislaufforsch 1955;21:163-81.
213. Matthay RA, Schwarz MI, EllisJH, Steele PP, Siebert PE, DurranceJR,
Levin DC. Pulmonary artery hypertension in chronic obstructive pulmonary disease: chest radiographic assessment. Invest Radiol
1981;16:95-100.
214. Chetty KG, Brown SE, Light RW. Identification of pulmonary hyperten-
VOL 150
1994
sion in chronic obstructive pulmonary disease from routine chest ra
diographs. Am Rev Respir Dis 1982;126:338-41.
215. Konstam MA, Pandian N. Assessment of right ventricular function. In:
Konstam MA, Isner JM, eds. The right ventricle. Boston: Kluwer Academic, 1988;1-15.
216. Lehtonen J, Sutinen S, Ikaheimo P, Paakko P. Electrocardiographic
criteria for the diagnosis of right ventricular hypertrophy verified at
autopsy. Chest 1988;93:839-42.
217. Moccetti T, Morpurgo M. Contribution of vector cardiography to the diagnosis of chronic cor pulmonale. In: Daum S, ed. Cor pulmonale cronicum. Munchin: European Society for Clinical Respiratory Physiology
and the European Society of Cardiology. 1988;299-314.
218. Bancroft WH, Eddleman EE. Methods and physical characteristics of
the kinetocardiographic and apexcardiographic systems for recording low-frequency precordial motion. Am Heart J 1967;73:756-64.
219. Weitzenblum E, Zielinski J, Bishop JM. The diagnosis of "cor pulmonale"
by noninvasive methods: a challenge for pulmonologists and cardiol
ogists. Bulletin Europeen de Physiopathologie Respiratoire 1983;
19:423-6.
220. Danchin N, Cornette EA, Henriquez A, Godenir JP, Ethevenot G, Polu
JM, Sadoul P. Two dimensional echocardiographic assessment of the
right ventricle in patients with chronic obstructive lung disease. Chest
1987;92:229-33.
221. Marchandise B, De Bruyne B, Delaunois L, Kremer R. Non-invasive
prediction of pulmonary hypertension in chronic obstructive pulmonary disease by echocardiography. Chest 1987;91 :361-5.
222. Berger HJ, Matthay RA. Noninvasive radiographic assessment of cardiovascular function in acute and chronic respiratory failure. Am J
Cardiol 1981 ;47:950-62.
223. Matthay RA, Berger HJ. Non-invasive assessment of right and left ven
tricular function in acute and chronic respiratory failure. Crit Care Med
1983;11 :329-38.
224. Schiller NB, Sahn DJ. Pulmonary pressure measurement by doppler
and two-dimensional echocardiography in adult and paediatric populations. In: Weir EK, Archer SL, Reeves JT, eds. The diagnosis and
treatment of pulmonary hypertension. New York: Futura, 1992;41-59.
225. Migueres M, Escamilla R, Coca F, Didier A, Krempf M. Pulsed doppler
echocardiography in the diagnosis of pulmonary hypertension and
COPD. Chest 1990;98:280-5.
226. Morpurgo M, Saviotti M, Dickele MC, Casazza F, Torbicki J, Weitzenblum E, Zielinski J. Echocardiographic aspect of pulmonary arterial
hypertension in chronic lung disease. Bulletin Europeen de Physiopathologie Respiratorie 1984;20:251-5.
227. Yock PJ, Popp RL. Non-invasive estimation of right ventricular systolic
pressure by doppler ultrasound in patients with tricuspid regurgitation. Circulation 1984;70:657-62.
228. Masuyama T, Kodama K, Kitabatake A, Sato H, Nanto S, Inoue M. Continuous wave doppler echocardiographic detection of pulmonary regurgitation and its application to non-invasive estimation of pulmonary
arterial pressure. Circulation 1986;74:484-92.
229. Kirchir B, Himelman RB, Schiller MB. Right atrial pressure estimation
in respiratory behavior of the inferior vena cava. Circulation 1988;78:11550 (2196).
230. Stevenson G, Kawabori I, Guntheroth W. The validation of doppler diagnosis of tricuspid regurgitation. Circulation 1981 ;64:255.
231. Berger M, Hecht S, Van Tosh A, Lingam U. Pulse and continuous wave
doppler echocardiographic assessment of valvular regurgitation in normal subjects. J Am Coli Cardiol 1989;13:1540-5.
232. Morrison DA, Ovitt T, Hammermeister KE. Functional tricuspid regurgitation and right ventricular dysfunction in pulmonary hypertension.
Am J Cardiol 1988;62:108-12.
233. McKenzie J. Disease of the heart. London: Oxford Medical Publishing,
1908;229.
234. Himelman RB, Stulbarg K, Kircher B, Lee E, Kee M, Dean NK, Golden
J, Wolfe CL, Schiller NB. Non-invasive evaluation of pulmonary arterial pressure during exercise by saline enhanced doppler echocardiography in chronic pulmonary disease. Circulation 1989;79:863-71.
235. Beard JT, Byrd BF. Saline contrast enhancement of trivial doppler tricuspid regurgitation signals for estimating pulmonary artery pressure.
Am J CardioI1988;62:486-8.
236. Laaban JP, Diebold B, Raffoul H, Lafay M, Poirier T, Rochemaure J,
Peronneau M. Non-invasive estimation of systolic pulmonary arterial
pressure (Pps) using continuous wave doppler ultrasound in COPD.
Am Rev Respir Dis 1988;137:150.
237. Bommer W, Weinert L, Neumann A, Neef J, Mason DT, DeMaria A. Determination of right atrial and right ventricular size by two-dimensional
echocardiography. Circulation 1979;60:91-100.
238. Starling MR, Crawford MH, Sorensen SG, O'Rourke RA. Two-dimensional
echocardiographic technique evaluating right ventricular size and performance in patients with obstructive lung disease. Circulation
1982;66:612-20.
239. Watanabe T, Katsume H, Matsukubo H, Furukawa K, Ijichi H. Estima-
State of the Art: Pathophysiology of Cor Pulmonale in COPO
tion of right ventricular volume with two-dimensional echocardiography. Am J Cardiol 1982;49:1946-53.
240. Ferlinz J. Measurements of right ventricular volumes in man from single plain cineangiograms. Am Heart J 1977;94:87-90.
241. Mitchell RS, Stanford RE, Silvers GW, Dart G. The right ventricle in chronic
airway obstruction: a clinico-pathologic study. Am Rev Respir Dis
1976;11 :147-54.
242. Murphy ML. The pathology of the right heart in chronic hypertrophy and
failure. In: Fisk RL, ed. The right heart. Philadelphia: Davis, 1987;
159-69.
243. Konstam MA, Levine HA. Effects of afterload and preload on right ventricular systolic performance. In: Konstam MA, Isner JM, eds. The right
ventricle. Boston: Kluwer Academic, 1988;17-35.
244. Reedy T, Chapman CB. Measurement of right ventricular volume by
cineangiofluorography. Am Heart J 1963;66:221-5.
245. Berger HJ, Matthay RA, Loke J, Marshal RC, Gottschalk A, Zaret BL.
Assessment of cardiac performance with quantitative radionuclide angiography: right ventricular ejection fraction with reference to findings
in chronic obstructive pulmonary disease. Am J Cardiol 1978;41:
897-905.
246. Maddahi J, Bermon OS, Matsuoka DT, Waxman AD, Stankus KE, Forrester JS, Swan HJ. A new technique for assessing right ventricular
ejection fraction using rapid multiple gated equilibrium cardiac blood
pool scintigraphy. Circulation 1979;60:581-9.
247. Xue OF, MacNee W, Flenley DC, Hannan WJ, Adie CJ, Muir AL. Can
right ventricular performance be assessed by gated equilibrium ventriculography? Thorax 1983;38:486-93.
248. MacNee W, Xue OF, Hannan WJ, Flenley DC, Adie CJ, Muir AL. Assessment by radionuclide angiography of right and left ventricular function in chronic bronchitis and emphysema. Thorax 1983;38:494-500.
249. Wathen CG, Hannan WJ, Flenley DC, Muir AL. Reproducibility of radionuclide right ventricular ejection fraction (RVEF) in chronic bronchitis and emphysema (COLD). Clin Sci 1988;74(Suppl 18):60P.
250. Dewhurst NF, Muir AL. Comparative prognostic value of radionuclide
ventriculography at rest and on exercise in 100 patients after first myocardial infarction. Br Heart J 1983;49:111-21.
251. Altschule MD. Limited usefulness of the so-called ejection fraction measurement in clinical practice. Chest 1986;90:134-5.
252. Ellis JH, Kirch 0, Steele PP. Right ventricular ejection-fraction in severe chronic airway obstruction. Chest 1977;71(Suppl):281-2.
253. Olvey SK, Reduto LA, Stevens PM, Deaton WJ, Miller RR. First pass
radionuclide assessment of right and left ventricular ejection fraction
in COPD. Chest 1980;78:4-9.
254. Matthay RA, Berger HJ. Cardiovascular performance in chronic obstructive pulmonary disease. Med Clin North Am 1981 ;65:489-520.
255. Slutsky RA, Hooper W, Ackerman W, Moser KM. The response of the
right ventricular size function and pressure to supine exercise: a comparison of patients with chronic obstructive lung disease and normal
subjects. Eur J Nucl Med 1982;7:553-8.
256. Mathur PN, Powles P, Pugsley SO, McEwan MP, Campbell EJ. Effect
of digoxin on right ventricular function in severe chronic airflow obstruction. Ann Intern Med 1981;95:283-8.
257. Hooper WW, Slutsky RA, Kocienski DE. Right and left ventricular response to subcutaneous terbutaline in patients with chronic obstructive pulmonary disease: radionuclide angiography assessment of
cardiac size and function. Am Heart J 1982;104:1027-32.
258. Dahlstrom JA. Simultaneous assessment of right ventricular ejection
fraction and central haemodynamics at rest and during exercise in
patients with pulmonary hypertension. Clin PhysioI1983;3:267-79.
259. Erickson AD, Golden WA, Claunch BC, Donat WE, Kaemmerlen JT. Acute
effects of phlebotomy on right ventricular size and performance in polycythemic patients with chronic obstructive pulmonary disease. Am J
Cardiol 1983;53:163-6.
260. Brown SE, Pakron FJ, Milne N, Linden GS, Stansbury OW, Fischer CE,
Light RW. Effects of digoxin on exercise capacity and right ventricular function during exercise in chronic airflow obstruction. Chest
1984;85:187-91.
261. Tuxen DV, Powles ACP, Mathur PN, Pugsley SO, Campbell EJ. Detrimental effects of hydralazine in patients with chronic airflow obstruction
and pulmonary hypertension. A controlled hemodynamic and radionuclide study. Am Rev Respir Dis 1984;129:388-95.
262. Brent BN, Mahler 0, Matthay RA, Berger HJ, Zaret BL. Non-invasive
diagnosis of pulmonary arterial hypertension in chronic obstructive
pulmonary disease: right ventricular ejection fraction at rest. Am J
Cardiol 1984;53:1349-53.
263. Burghuber OC, Bergmann H. Right ventricular contractility in chronic
obstructive pulmonary disease. A combined radionuclide and haemodynamic stUdy. Respiration 1988;53:1-12.
264. Morrison 0, Goloman S, Wright AL, Henry R, Sorenson S, Caldwell J,
Ritchie J. The effect of pulmonary hypertension on systolic function
of the right ventricle. Chest 1983;84:250-7.
265. MacNee W. Clinical importance of right ventricular function in pulmo-
851
nary hypertension. In: Weir EK, Archer SL, Reeves JT, eds. The diagnosis and treatment of pulmonary hypertension. New York: Futura,
1992;13-40.
266. Tobinick E, Schelbert HR, Henning H, Lewinter M, Taylor A, Ashburn
WL, Karliner JS. Right ventricular ejection fraction in patients with acute
anterior and inferior infarction assessed by radionuclide angiography.
Circulation 1978;57:1078-84.
267. Berger HJ, Matthay RA, Davies RA, Zaret BL, Gottschalk A. Comparison of exercise right ventricular performance in chronic obstructive
pulmonary disease and coronary artery disease: non-invasive assessment by quantitative radionuclide angiocardiography. Invest Radiol
1979;14:342-53.
268. MacNee W, Morgan AD, Wathen CG, Muir AL, Flenley DC. Right ventricular performance during exercise in chronic obstructive pulmonary
disease. Respiration 1985;48:206-11.
269. Cohen HA, Baird MG, Rouleau JR, Fuhrmann CF, Bailey IK, Summer
WR, Strauss HW, Pitt B. Thallium 201 myocardial imaging in patients
with pulmonary hypertension. Circulation 1976;54:790-5.
270. Khaja F, Alam M, Goldstein S, Anbe DT, Marks OS. Diagnostic value
of visualization of the right ventricle using Thallium 201 myocardial
imaging. Circulation 1979;59:182-8.
271. Ohsuzu F, HandaS, Kondo M, Yamazaki Hm, TsuguT, KuboA, Takagi
Y, Nakamura Y. Thallium 201 myocardial imaging to evaluate right
ventricular overloading. Circulation 1980;61 :620-5.
272. Berger H, Wackers F, Mahler 0, Davis R, Matthay R, Zaret B. Right ventricular visualization on Thallium 201 myocardial images in chronic
obstructive pulmonary disease: relationship to right ventricular function and hypertrophy (abstract). Circulation 1980;62:11I-103.
273. Weitzenblum E, Moyses B, Dickele M, Methlin G. Detection of right ventricular pressure overloading by Thallium-201 myocardial scintigraphy: results in 57 patients with chronic respiratory diseases. Chest
1984;85:164-9.
274. Longmore DB, Klipstein RH, Underwood SR, Firmin ON, Hounsefield
GN, Watanabe M, Bland C, Fox K, Poole-Wilson PA, Rees RSO, Denison 0, Burman ED. Dimensional accuracy of magnetic resonance
studies of the heart. Lancet 1985;1:1360-2.
275. Turnbull LW, Ridgeway JP, Biernacki W, McRitchie H, Muir AL, Best
JJK, MacNee W. Assessment of the right ventricle by magnetic resonance imaging in chronic obstructive lung disease. Thorax 1990;
45:597-601.
276. Becker GA, Galletti PM. Functional anatomy of cardiac pumping. In:
Hamilton AF, Dow P, eds. Handbook of physiology. Washington, DC:
American Physiological Society, 1963;759-98.
277. Laks MM, Garner 0, Swan HJC. Volumes and compliances measured
simUltaneously in the right and left ventricles of the dog. Circ Res
1967;20:565-9.
278. Rushmer R. Functional anatomy and control of the heart. In: Cardiovascular dynamics. 4th ed. Philadelphia: Saunders, 1976;89:98.
279. Morpurgo M, Jezek V. Evaluation of right heart failure: controversies
in definition and methods of evaluation. In: Jezek V, Morpurgo M, Tamarin R, eds. Current topics in rehabilitation. Right ventricular hypertrophy and function in chronic lung disease. Verona: Springer-Verlag,
1992;79-95.
280. Furey SA, Zieska HA, Levy MN. The essential function of the right ventricle. Am Heart J 1984;107:404-10.
281. Fishman AP. Cor pulmonale: general aspects. In: Pulmonary diseases
and disorders. New York: McGraw-Hili, 1980;853-82.
282. Abel RL. Effects of alterations in peripheral resistance on left ventricular function. Proc Soc Exp Bioi Med 1965;120:52-6.
283. Bahler RC. Does increased work of the right ventricle diminish left ventricular function? Chest 1977;72:551-2.
284. Stein PO, Sabbah NH, Anbe DT, Marzilli M. Performance of the failing
and nonfailing right ventricle of patients with pulmonary hypertension.
Am J Cardiol 1979;44:1050-5.
285. Wagenvoort CA, Wagenvoort N. Primary pulmonary hypertension; a
pathological stUdy of the lung vessels in 156 clinically diagnosed cases.
Circulation 1970;42:1163-84.
286. Weber KT, Janicki JS. Pulmonary hyprtension. In: Cardiopulmonary exercise testing: physiological principles and clinical applications.
Philadelphia: Saunders, 1986;220-34.
287. Niederman MS, Matthay RA. Cardiovascular function in secondary pulmonary hypertension. Heart Lung 1986;15:341-51.
288. Light RW, Mintz HM, Linden GS, Brown SE. Hemodynamics of patients
with severe chronic obstructive pulmonary disease during progressive upright exercise. Am Rev Respir Dis 1984;130:391-5.
289. Bristow JD, Morris JF, Kloster FE. Haemodynamics of cor pulmonale.
Proc Cardiovasc Dis 1966;9:239-58.
290. Douglas NJ, Claverley PMA, Leggett RJE, Brash HM, Flenley DC,
Brezinova V. Transient hypoxemia during sleep in chronic bronchitis
and emphysema. Lancet 1979;1:1-4.
291. Fletcher EC, Levin DC. Cardiopulmonay hemodynamics during sleep
in subjects with chronic obstructive pulmonary disease: the effect of
852
AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
short and long-term oxygen. Chest 1984;85:6-14.
292. Green JF. Fundamental cardiovascular and pulmonary physiology.
Philadelphia: Lea & Febiger, 1987;45-55.
293. Goerke J, Mines AH. Cardiovascular physiology. New York: Raven Press,
1988;99-152.
294. Strobeck JE, Sonnenblick EH. Pathophysiology of heart failure. In: Levine HJ, Gaasch WH, ads. The ventricle. Boston: Martinus Nijhoff PUbl,
1985;209-24.
295. Gunther S, Grossman W. Determinants of ventricular function in pressure overload hypertrophy in man. Circulation 1979;59:679-88.
296. Morrison DA. Pulmonary hypertension in chronic obstructive pulmonary
disease. The right ventricular hypothesis. Chest 1987;92:387-9.
297. Klinger JR, Hill NS. Right ventricular dysfunction in chronic obstructive
pulmonary disease. Evaluation and management. Chest 1991 ;99:
715-23.
298. Konstam MA, Salem ON, Isner JM, Zile MR, Kahn PC, Bonin JD, Cohen
SR, Levine HJ. Vasodilator effect on right ventricular function in congestive heart failure and pulmonary hypertension: end-systolic pressure volume relation: Am J Cardiol 1984;54:132-6.
299. Winzelberg GG, Boucher CA, Pohost GM, McKusick KA, Bingham JB,
Okada RD, Strauss HW. Right ventricular function in aortic and mitral
valve disease. Relation of gated first pass radionuclide angiography
to clinic and haemodynamic findings. Chest 1981;79:520-8.
300. Korr KS, Grandsman EJ, Winkler ML, Shulman RS, Bough EW.
Hemodynamic correlates of right ventricular ejection fraction measured
with gated radionuclide angiography. Am J Cardiol 1982;49:71-7.
301. Friedman BJ, Holman BL. SCintigraphic prediction of pulmonary arterial
systolic pressure by regional right ventricular ejection fraction during
the second half of systole. Am J Cardiol 1978;50:1114-9.
302. Morrison DA, Sorenson S, Caldwell J, Wright AL, Richie J, Kennedy
JW, Hamilton G. The normal right ventricular response to supine exercise. Chest 1982;82:686-91.
303. Marmor AT, Mijiritsky Y, Plich M, Frenkel A, Front D. Improved radionuclide method for assessment of pulmonary artery pressure. Chest
1986;89:64-9.
304. Mols P, Huynh CH, Dechamps P, Naeije N, Guillauml M, Hamh R. Prediction of pulmonary pressure in chronic obstructive pulmonary disease
by radionuclide ventriculography. Chest 1989;96:1280-4.
305. Burghuber OC, Bergman H, Silberbauer K, Hofer R. Right ventricular
performance in chronic airflow obstruction. Respiration 1984;45:
124-30.
306. Biemacki W, Flenley DC, Muir Al, MacNae W. Pulmonary hypertension and right ventricular function in patients with COPO. Chest
1988;94:1169-75.
307. Caro CG, Pedley TJ, SChroter RC. The mechanics of the circulation.
Oxford: Oxford University Press, 1981;213-4.
308. Taylor SH. Cardiovascular consequences of heart failure. Eur Heart J
1988;9(Suppl H):41-7.
309. S8gawa K. The end-systolic pressure volume relation of the ventricle:
definition, modifications and clinical use. Circulation 1981 ;63:1223-7.
310. Sagawa K, Suga H, Shoukas AA, Bakalar KM. End-systolic pressure/volume ratio: a new index of ventricular contractility. Am J Cardiol
1977;40:748-53.
311. Sagawa K. The ventricular pressure-volume diagram revisited. Circ Res
1978;43:677-86.
312. Grossman W, Braunwald E, Mann T,McLaurin LP, Green LH. Contractile state of the left ventricle in man as evaluated from end-systolic
pressure volume relations. Circulation 1977;56:845-52.
VOL 150
1994
313. Mehmel HC, Stockins B, Ruffmann K, von Oishausen K, Schuler G, Kubler W. Linearity of the end-systolic pressure-volume relationship in
man and its sensitivity for assessment of left ventricular function. Cir
culation 1981;63:1216-22.
314. Suga H, S8gawa K, Shoukas AA. Load independence of the instantaneous
pressure volume ratio of the canine left ventricle and effects of epi
nephrine and heart rate on the ratio. Circ Res 1973;32:314-21.
315. Weber KT, Janicki JS, Shroff S, Fishman AP. Contractile mechanics
and interaction of right and left ventricles. Am J Cardioll981 ;47:686-95.
316. Maughan WL, Oikawa PY. Right ventricular function. In: SCharf SM, ed.
Heart Lung Interactions in Health and Disease. New York: Marcel Dekker, 1989;179-220.
317. Weber KT, Janicki JA, Shroff SJ. The heart as a mechanical pump. In:
Weber KT, Janicki JS, eds. Cardiopulmonary exercise testing. Philadelphia: Saunders, 1986;34-56.
318. Noble MIM. The pressure-volume relationship of the intact heart. In: ter
Jeyrs HEDJ, Noble MIM, eds. Starling's law of the heart revisited.
Dordrecht: Kluwer Academic PUbl, 1988;126.
319. Redington AN, Gray HH, Hodson ME. Characterisation of the normal
right ventricular pressure-volume relation by biplane angiography and
simultaneous micromanometer pressure measurements. Br Heart J
1988;59:23-30.
320. Parmley WW. Mechanics of ventricular muscle. In: Levine HJ, Gaasch
WH, eds. The ventricle. Boston: Martinus Nijhoff Publ, 1985;41-62.
321. Sagawa R, Sunagawa K, Maughan WL. Ventricular end-systolic pressurevolume relations. In: Levine HJ, Gaasch WH, eds. The ventricle. Boston: Martinus Nijhoff Publ, 1985;79-103.
322. Wasserman K. New concepts in assessing cardiovascular function. Circulation 1988;78:1060-71.
323. MacNee W, Wathen CG, Hannan WJ, Flenley DC, Muir AL. Effects of
pirbuterol and sodium nitroprusside on pulmonary haemodynamics
in hypoxic cor pulmonale. Br Med J 1983;287:1169-72.
324. Wroblewski E, James F, Spann JF, Bove AA. Right ventricular parlormance in mitral stenosis. Am J CardioI1981;47:51-6.
325. Chappuis E, Dorsaz PA, Rutishauser W. New method for the assessment of right ventricular function by intravenous digital angiography.
First International Workshop on New Trends in Cardiovascular Therapy and Technology, Genoa, 1989;25P.
326. Smith MA, Ridgway JP, Brydon JWE, Been M, Douglas RH, Kean OM,
Muir AL, Best JJ. ECG-gated T1 images of the heart. Phys Med Biol
1986;3:771~.
327. Hertes F, Jezek V, Daum S. Site of pulmonary resistance in cor pulmonale
in chronic bronchitis. Br Heart J 1988;30:~.
328. lapoI WM, Snider MT. Pulmonary hypertension in severe acute respiratory failure. N Engl J Med 1970;296:476-80.
329. Maragoni S, Scalvini S, Schena M, Vitacca M, Quadri A, Levi G. Right
ventricular diastolic function in chronic obstructive lung disease. Eur
Respir J 1992;5:438-43.
330. Lejeune P, Mols P, Naeije R, Hallemans R, MelO! C. Acute hemodynamic
effects of controlled oxygen therapy in decompensated chronic obstructive pulmonary disease. Crit Care Med 1984;12:1032-5.
331. MacNee W, Wathen CG, Flenley DC, Muir AL. The effects of controlled
oxygen therapy on ventricular function in acute and chronic respiratory failure. Am Rev Respir Dis 1988;137:1289-95.
332. Aber GM, Bishop JM. Serial changes in renal function arterial gas tensions and the acid base state in patients with chronic bronchitis and
oedema. Clin Sci 1965;28:511-25.
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Acute Coronary Syndrome NCP 02Dokument6 SeitenAcute Coronary Syndrome NCP 02AgronaSlaughterNoch keine Bewertungen
- Inotropes: Learning ObjectivesDokument7 SeitenInotropes: Learning ObjectivesOrion JohnNoch keine Bewertungen
- The Role of Nitric Oxide in Heart Failure PDFDokument237 SeitenThe Role of Nitric Oxide in Heart Failure PDFSujok SwadeshNoch keine Bewertungen
- Biology STPM Chapter 11 Term 2Dokument26 SeitenBiology STPM Chapter 11 Term 2Suraya Nadzrah100% (3)
- Compounded Pimobendan: FeatureDokument8 SeitenCompounded Pimobendan: FeatureMadelineNoch keine Bewertungen
- Blood Vessels Lecture Slides PDFDokument32 SeitenBlood Vessels Lecture Slides PDFRaluca AlexandraNoch keine Bewertungen
- Drug Profiling PHARMACOLOGYDokument71 SeitenDrug Profiling PHARMACOLOGYJay MagsaysayNoch keine Bewertungen
- Controlled Hypotensive Anaesthesia What Is Safe ?: DR Hussain Almejadi AL RAZI HospitalDokument50 SeitenControlled Hypotensive Anaesthesia What Is Safe ?: DR Hussain Almejadi AL RAZI HospitalcommandityNoch keine Bewertungen
- Allergy and Immunology: Immunodeficiency 10 Warning Signs of ImmunodeficiencyDokument24 SeitenAllergy and Immunology: Immunodeficiency 10 Warning Signs of Immunodeficiencyacque100% (2)
- Fundamentals of Nursing Exam 2Dokument23 SeitenFundamentals of Nursing Exam 2eka100% (2)
- 06 Cardiovascular Response To ExerciseDokument50 Seiten06 Cardiovascular Response To ExerciseÑùmãñ MùghãlNoch keine Bewertungen
- Physiology of Thermoregulation (Dr. Herman)Dokument59 SeitenPhysiology of Thermoregulation (Dr. Herman)stella pangestikaNoch keine Bewertungen
- Renal Blood Flow Until Regulation of RBF and GFRDokument5 SeitenRenal Blood Flow Until Regulation of RBF and GFRDoogie ReynaldoNoch keine Bewertungen
- Diabetes and Hypertension Physiopathology and Therapeutics: Journal of Human Hypertension May 2000Dokument7 SeitenDiabetes and Hypertension Physiopathology and Therapeutics: Journal of Human Hypertension May 2000chandra9000Noch keine Bewertungen
- Drugs Affecting Cardiovascular SystemDokument24 SeitenDrugs Affecting Cardiovascular SystemKhalid MortajaNoch keine Bewertungen
- Visceral Vascular Manipulation, 2011Dokument270 SeitenVisceral Vascular Manipulation, 2011kkalu_just_funky91% (11)
- Clinical Pharmacology of Dobutamine and Dopamine in Preterm NeonatesDokument9 SeitenClinical Pharmacology of Dobutamine and Dopamine in Preterm Neonatesmateri posNoch keine Bewertungen
- Himalayan Salt Health BenefitsDokument0 SeitenHimalayan Salt Health BenefitsturbobrikNoch keine Bewertungen
- Use of Sthanika (External) Basti in Spondylitis DiseasesDokument5 SeitenUse of Sthanika (External) Basti in Spondylitis DiseasesIJAR JOURNALNoch keine Bewertungen
- CIRCULATION PHYSIOLOGY MCQs Test PDFDokument6 SeitenCIRCULATION PHYSIOLOGY MCQs Test PDFMiles Hui67% (3)
- Congestive Heart FailureDokument74 SeitenCongestive Heart FailureNiharikaNoch keine Bewertungen
- Cardiovascular Failure, Inotropes and Vasopressors: Oxygen DeliveryDokument4 SeitenCardiovascular Failure, Inotropes and Vasopressors: Oxygen DeliveryMarlin Berliannanda TawayNoch keine Bewertungen
- DocumentDokument5 SeitenDocumentSg89Noch keine Bewertungen
- Biophysics of Lasers - Part IIDokument6 SeitenBiophysics of Lasers - Part IIIznogud02Noch keine Bewertungen
- Pathologic Basis of Veterinary Disease 7Th Edition James F Zachary Full Chapter PDF ScribdDokument67 SeitenPathologic Basis of Veterinary Disease 7Th Edition James F Zachary Full Chapter PDF Scribdtodd.feuer645100% (6)
- Controlled Hypotensive AnesthesiaDokument24 SeitenControlled Hypotensive AnesthesiaSuresh Kumar100% (1)
- MedicationsDokument30 SeitenMedicationsvamshidhNoch keine Bewertungen
- CH 11+12 MCQDokument13 SeitenCH 11+12 MCQHungryPanda’s KitchenNoch keine Bewertungen
- Questions PharmaDokument176 SeitenQuestions Pharmaminakshi boss100% (3)
- Terapia Shock VasoplejicoDokument11 SeitenTerapia Shock VasoplejicorjerezrNoch keine Bewertungen