Beruflich Dokumente
Kultur Dokumente
Emergent Management of Myasthenia Gravis
Hochgeladen von
Muhammad Yamin LCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Emergent Management of Myasthenia Gravis
Hochgeladen von
Muhammad Yamin LCopyright:
Verfügbare Formate
Emergent Management of Myasthenia Gravis
Overview
The most important aspect of emergent management of myasthenia
gravis is the detection and treatment of the myasthenic crisis. Myasthenia
gravis is a relatively rare autoimmune disorder of peripheral nerves in
which antibodies form against acetylcholine (ACh) nicotinic postsynaptic
receptors at the myoneural junction. A reduction in the number of ACh
receptors results in a characteristic pattern of progressively reduced
muscle strength with repeated use of the muscle and recovery of muscle
strength following a period of rest. The bulbar muscles are affected most
commonly and most severely, but most patients also develop some
degree of fluctuating generalized weakness.[1]
Epidemiology
The estimated prevalence of myasthenia gravis is approximately 20
cases per 100,000 population, with the disease affecting twice as many
women as men. The overall prevalence is approximately 150-200 per
million.[2] However, in older age groups, men are affected more often and
the disease is often misdiagnosed.[3] As a result, there is a bimodal
distribution with a female predominance in the 2nd to 3rd decade of life
and male predominance in the 6th to 8th decades.[1, 3, 2] Ocular
complaints are more common in the first year and are the presenting
symptom in 50% of cases. Often within 1 year, patients have generalized
symptoms such as weakness or fatigue and one third of patients develop
respiratory weakness, requiring mechanical ventilation.[4] Myasthenic
crisis occurs in about 20% of patients with generalized myasthenia gravis.
[3] Over the years, due to changes in treatment, prognosis and mortality
havechanged. Mortality in the last 4 decades has seen a dramatic
decrease from 75% to 4.5%.[2]
Patient History
Most patients who present to the emergency department (ED) have
an established diagnosis of myasthenia gravis and are already taking
appropriate medications. The activity of the disease fluctuates, and
adjustments in medication dosages must be made accordingly.
Noncompliance with medications, infection, and other physiologic
stressors may result in a fulminant exacerbation of the disease. The most
common cause of myasthenic crisis often is infection, although idiopathic
causes are also common.[5]
Many other factors influence cholinergic transmission, including
drugs, temperature, and emotional state. The adverse effects of many
medications may provoke exacerbations; therefore, carefully obtaining a
medication history is important. Medications reported to cause
exacerbations of myasthenia gravis include the following:
Antibiotics - Macrolides, fluoroquinolones, aminoglycosides,
tetracycline, and chloroquine. Antidysrhythmic agents - Beta blockers,
calcium channel blockers, quinidine, lidocaine, procainamide, and
trimethaphan
Antipsychotics - Phenothiazines, sulpride, atypicals [6]
Cardiovascular- Propanolol, quinidine, verapamil, bretylium,
statins [6]
Miscellaneous - Diphenylhydantoin, lithium, chlorpromazine,
muscle relaxants, levothyroxine, adrenocorticotropic hormone (ACTH),
and, paradoxically, corticosteroids [7, 8]
Thyroid disorders may be seen in as many as 10% of patients with
myasthenia gravis, and symptoms of hyperthyroidism or hypothyroidism
may be present.
Rarely does a patient present with undiagnosed myasthenia gravis.
However, if this situation does occur, typical complaints are of generalized
weakness and reduced exercise tolerance that improves with rest.[5]
Patients with myasthenia gravis do not present with primary complaints of
sleepiness or muscle pain. The patient may also complain of a specific
weakness of certain muscle groups (eg, those used when climbing stairs).
The distribution of muscle weakness follows a characteristic pattern;
initially 85% of patients have involvement of the eyelids and extraocular
muscles, resulting in ptosis and/or diplopia.[1] The involvement of the
facial muscles results in changes in expression and speech, whereas
involvement of the pharyngeal muscles results in progressive difficulty
with mastication and deglutition.
In 15-20% of patients, myasthenia gravis affects the bulbar muscles
alone. The other patients progress to generalized myasthenia gravis.[1]
Neck and proximal limb weakness may occur. Eighty percent of
patients with bulbar weakness go on to develop generalized weakness
involving the limbs.[3] Respiratory weakness may be present. Respiratory
failure occurs in 1% of patients.
Physical Examination
Severe exacerbations
Severe exacerbations of myasthenia gravis may present
dramatically and should be considered a true neurological emergency.[6]
Findings can include the following:
Facial muscles may be slack, and the face may be expressionless
The patient may be unable to support his or her head, which will
fall onto the chest while the patient is seated
Jaw is slack
Voice has a nasal quality
Body is limp
Gag reflex is often absent, and such patients are at risk for
aspiration of oral secretions [9]
Respiratory distress
The patient's ability to generate adequate ventilation and to clear
bronchial secretions is of utmost concern with severe exacerbations of
myasthenia gravis.
Inability to cough leads to an accumulation of secretions; therefore,
rales, rhonchi, and wheezes may be auscultated locally or diffusely. The
patient may have evidence of pneumonia (ie, fever, cough, dyspnea,
consolidation).
The patient may appear anxious, with rapid and shallow breathing.
Paradoxical chest movements due to diaphragmatic weakness may be
present.[5]
Cholinergic crisis
One of the confusing factors in treating patients with myasthenia
gravis is that insufficient medication (ie, myasthenic crisis) and excessive
medication (ie, cholinergic crisis) can present in similar ways.
Cholinergic crisis results from an excess of cholinesterase inhibitors
(ie, neostigmine, pyridostigmine, physostigmine) and resembles
organophosphate poisoning. In this case, excessive ACh stimulation of
striated muscle at nicotinic junctions produces flaccid muscle paralysis
that is clinically indistinguishable from weakness due to myasthenia
gravis. Despite muscle weakness, deep tendon reflexes are preserved.
Both myasthenic crisis and cholinergic
bronchospasm with wheezing, bronchorrhea,
diaphoresis, and cyanosis.[9]
crisis may cause
respiratory failure,
Miosis and the SLUDGE syndrome (ie, salivation, lacrimation, urinary
incontinence, diarrhea, gastrointestinal [GI] upset and hypermotility,
emesis) also may mark cholinergic crisis. However, these findings are not
inevitably present.
Neonatal myasthenia gravis
Although most of these cases are apparent within 48 hours, the
presentation may be delayed as long as 10 days after delivery. This
delayed presentation should be kept in mind when evaluating newborn
infants in the ED for weakness or poor feeding.
Imaging Tests
Chest radiography
Chest radiography is indicated to determine the presence of
aspiration or other pneumonias, which commonly occur in patients with
myasthenia gravis.
CT scanning and MRI
Computed tomography (CT) scanning and magnetic resonance
imaging (MRI) of the chest are each highly accurate in detecting
thymomas. Every patient with myasthenia gravis should be screened for
these neoplasms. Chest radiography is relatively insensitive in screening
for thymomas, as it does not detect them in up to 30% of cases.
Tensilon (Edrophonium) Challenge Test
The Tensilon (edrophonium) challenge test is useful in diagnosing
myasthenia gravis and in distinguishing myasthenic crisis from cholinergic
crisis, due to its rapid onset and short duration of action.[10, 11] A
positive response is not completely specific for myasthenia gravis,
because several other conditions (eg, amyotrophic lateral sclerosis) may
also respond to edrophonium with increased strength.
Once the patient's airway and ventilation are secured, an initial test
dose of edrophonium is given. Some patients may respond noticeably to a
small dose (1 mg). If no adverse reaction occurs following the test dose,
another dose (3 mg) of edrophonium should produce noticeable
improvement in muscle strength within 1 minute.[11] If no improvement
occurs, an additional dose of 5 mg can be administered to total no more
than 10 mg.[10]
Patients who respond generally show dramatic improvement in
muscle strength, regaining facial expression, posture, and respiratory
function within 1 minute.
During this procedure, the patient must be monitored carefully,
because edrophonium can cause significant bradycardia, heart block, and
asystole. The risk of serious bradyarrhythmias and syncope is reportedly
only 0.16%, but atropine still should be available at the bedside.[10] The
return of muscle weakness after edrophonium wears off, combined with
residual, increased oral secretions, can exacerbate respiratory distress
and the risk of aspiration.
Patients with a cholinergic crisis may respond to edrophonium
challenge by increasing salivation and bronchopulmonary secretions,
diaphoresis, and gastric motility (ie, SLUDGE syndrome).[11, 12] These
changes should be managed expectantly, as the half-life of edrophonium
is short (ie, approximately 10 min).
If muscle strength fails to improve following the maximum dose of
edrophonium, the patient is having a cholinergic crisis or has another
cause of weakness that is unrelated to myasthenia gravis.
Because the effects of edrophonium are brief, repeated doses may
be required before oral anticholinesterase medication can take effect.[11]
In patients with less severe exacerbations, the degree of
improvement with edrophonium may be subtle. Many authors recommend
having several blinded observers assess the patient's response in these
cases. Some authors also suggest that a clear endpoint, such as
improvement in eyelid ptosis or extraocular movements, since these
muscles are independent of voluntary effort.[10]
Ice Pack Test
Cooling may improve neuromuscular transmission. In a patient with
myasthenia gravis who has ptosis, placing ice over an eyelid will lead to
cooling of the lid, which leads to improvement of the ptosis.
Lightly placing ice that is in a surgical glove or that is wrapped in a
towel over the eyelid will cool it within 2 minutes.[2] A positive test is
clear resolution of the ptosis.[10, 3]
This test has a pooled sensitivity and specificity of 82% and 96%,
respectively. However, the literature generally overestimates the tests
usefulness, since most of the studies were case-control designs.[13]
Additional Testing
Additional tests (eg, standard electromyography, single-fiber
electromyography, repetitive nerve stimulation, assays for ACh receptor
antibody [ARA]) are used to confirm the diagnosis of myasthenia gravis,
but these tests usually are not available on an emergent basis.[10] The
ARA test offers the highest specificity of these additional tests, since these
other tests only reveal a disorder of neuromuscular conduction.[13]
Patients with respiratory distress should have an evaluation of
pulmonary function, providing that the patient is not in obvious respiratory
failure. This evaluation includes pulse oximetry, a measure of pulmonary
function (ie, peak expiratory flow, forced expiratory volume in 1 second
[FEV1]), and arterial blood gas (ABG) sampling to determine partial
pressure of carbon dioxide (PCO2).[9] A negative inspiratory force (NIF) of
30 cm H2O or less or a forced vital capacity (FVC) of 20ml/Kg are
indicative of a myathenic crisis and airway compromise.[6]
Evidence of hypoxemia, poor respiratory effort, or CO2 retention is
an indication for intubation and mechanical ventilation.[9]
Patients can also undergo other testing, which, while useful for
neurologists for outpatient care, does not apply in the ED. Examples of
these tests are the Oculobulbar Facial Respiratory score and the MGActivities of Daily Life (MG-ADL) score, which yield data on bulbar function
but are most useful in long-term or serial assessment of patient function
and therefore do not have a significant role in the ED.[14] A small
retrospective study has shown that the MG-ADL score was higher on
admission in patients requiring a stay in the ICU.[15]
Prehospital Care
Field personnel should recognize generalized muscle weakness of
any etiology as a potential cause of respiratory failure. Patients with
generalized weakness require transport to the hospital, and provisions for
active airway intervention should be made en route.
Patients in frank respiratory arrest should be intubated and
ventilated prior to transport, if possible. Suctioning of pulmonary
secretions may be required to adequately ventilate the patient.
Supplemental oxygen is indicated in all cases, and intravenous access is
desirable prior to initiating transport.
Emergency Department Care
Patients with myasthenia gravis who are in respiratory distress may
be experiencing a myasthenic crisis or a cholinergic crisis. Before these
possibilities can be differentiated, ensuring adequate ventilation and
oxygenation is important. Patients with myasthenic crisis can develop
apnea very suddenly, and they must be observed closely. Evidence of
respiratory failure may be noted through ABG determination, pulmonary
function tests, or pulse oximetry.
Airway maneuvers
Open the airway by suctioning secretions after positioning the jaw
and tongue. Administer high-flow oxygen, and measure oxygen saturation
by pulse oximetry. If respirations remain inadequate, ventilate by bagvalve mask while preparing to intubate. In the patient without an intact
gag reflex, an oral airway may be placed.
Endotracheal intubation
Rapid sequence intubation should be modified, because depolarizing
paralytic agents (eg, succinylcholine) have less predictable results in
patients with myasthenia gravis. The relative lack of ACh receptors makes
these patients relatively resistant to succinylcholine; therefore, higher
doses must be used to induce paralysis. Once paralysis is achieved, it may
be prolonged.[9]
A rapid-onset, nondepolarizing agent (ie, rocuronium, vecuronium) is
the preferred paralytic agent for these patients. Although nondepolarizing
agents delay the onset of paralysis, compared with succinylcholine, these
medications do not result in unwanted prolonged paralysis. Following
paralysis, intubation is accomplished as usual. ABG sampling guides
ventilator settings.
Preliminary studies suggest that bilevel positive airway pressure
(BiPAP) can prevent intubation in patients with myasthenic crisis without
overt hypercapnia and should be considered in the patient who can be
closely monitored.[9, 16] Hypercapnia present at the time of BiPAP
initiation can predict failure and the need to proceed to endotracheal
intubation.[17, 6]
Investigation and treatment
Once the airway is secured, investigation into the cause of the
exacerbation of myasthenia gravis may proceed, with the most common
reason for an exacerbation being infection, followed by inadequate
treatment with cholinesterase inhibitors. However, up to 30% of patients
will not have an identified cause of their exacerbation.[5] Differentiation
from cholinergic crisis can proceed as described above.
In less severely ill patients, oral pyridostigmine can be administered
until clinical improvement is seen. The patient should be closely observed
and monitored during this trial. Other reasons for the exacerbation can
then be investigated.
Although patients with myasthenia gravis can develop any common
infection that can result in decompensation, the most likely source of
infection is pulmonary. Cultures of blood, sputum, and urine may be
indicated on an individual basis. Chest radiography is important in
detecting pneumonia. Appropriate broad-spectrum antibiotics are
indicated for sepsis and pneumonia. It is important to consider that
fluoroquinolones and antibiotics may adversely affect cholinergic
transmission in patients with myasthenia gravis, and these antibiotics
should be avoided if possible.
Patients with myasthenia gravis are sensitive to high temperatures
(core or ambient), and their muscle strength can improve when
temperature is lowered with cooling measures or antipyretics.
Inpatient Care
Patients who present to the ED with myasthenic or cholinergic crisis
will often require admission to an intensive care unit[6] ; while patients
with increasing muscle weakness of a less severe degree require
admission to a monitored setting, because their course is unpredictable.
[18] Patients with complications of the disease or treatment are admitted
to a level of care corresponding to the nature and severity of the
complication.
Patients with pneumonia should be admitted because they often are
taking immunosuppressant medications and are at a high risk for
aspiration pneumonia.[19]
Plasmapheresis has been found to be an effective short-term
treatment of acute exacerbations of myasthenia gravis. Plasmapheresis
removes circulating antibodies, including the autoimmune antibodies
responsible for the disease. Clinical improvement takes several days to
occur and lasts up to 3 weeks.[20] Because of the delayed onset of
beneficial effects, plasmapheresis has limited utility in the ED setting, but
often is used in the ICU setting. Some disagreement exists between
various national societies on the amount of evidence supporting plasma
exchange. The American Society for Apheresis considers therapeutic
plasma exchange a first-line therapy for myasthenia gravis, whereas the
American Academy of Neurology (AAN) states that the current evidence
does not support or refute a benefit.[4, 21, 22]
Multiple observational and case series studies have shown a shortterm benefit from plasma exchange, especially in myasthenic crisis.
However, there is only 1 randomized clinical trial that showed no
difference between the 2 treatment arms of plasma exchange versus
intravenous immunoglobulin (IVIG).[23] Additionally the plasma exchange
group had a higher mortality rate.[4]
Immunotherapy with intravenous gamma globulin appears to
diminish the activity of the disease for unknown reasons.[24] The benefit
begins within 2 weeks and may last for several months. Approximately
65% of patients with myasthenia gravis respond to intravenous gamma
globulin.[25, 26] The AAN considers IVIG an effective therapy for
moderate-to-severe cases of myasthenia gravis, as per their 2012
guidelines.[27]
Thymectomy is associated with clinical improvement in 85% of
cases, and 35% of patients appear to have complete remission.[1]
Patients past the age of puberty and younger than 50 years should have
elective thymectomy as part of their treatment.[28]
The need for anticholinesterase medication fluctuates significantly
in the postoperative period but overall is less than it was prior to
thymectomy.[7]
Transfer, Consultations, and Monitoring
Patients with severe exacerbations of myasthenia gravis or
cholinergic crisis should be transferred only after they have been
stabilized and the airway has been secured. Persistent hypoxemia,
hypercarbia, dysrhythmias, or unstable vital signs make transfer unwise,
unless appropriate care cannot be delivered at the original facility.
Emergent consultation with a neurologist is indicated. Patients with
severe exacerbations requiring intubation and mechanical ventilation are
managed in an intensive care setting with appropriate consultation.[5]
With regard to patient monitoring, all patients with myasthenia
gravis should be referred to a neurologist for ongoing care.
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Drug Dosage Calculations NCLEX Exam 4Dokument4 SeitenDrug Dosage Calculations NCLEX Exam 4Heather ClemonsNoch keine Bewertungen
- Sanofi-Aventis Presentation On FlagylDokument24 SeitenSanofi-Aventis Presentation On FlagylNasir Ali100% (3)
- Intellectual Property rights-II: AssignmentDokument25 SeitenIntellectual Property rights-II: AssignmentAvinash Mishra100% (2)
- Memorial On Behalf of AppellantDokument37 SeitenMemorial On Behalf of AppellantZahid Hashmi64% (14)
- !pharmaceuticals in Myanmar - Law and ProcedureSJICL-2000-115Dokument33 Seiten!pharmaceuticals in Myanmar - Law and ProcedureSJICL-2000-115Zin ZaeNoch keine Bewertungen
- Antipsychotic DrugsDokument94 SeitenAntipsychotic DrugsPatricia StratNoch keine Bewertungen
- Medical FormDokument2 SeitenMedical FormPushpendra KumarNoch keine Bewertungen
- REFERENSIDokument3 SeitenREFERENSIMuhammad Yamin LNoch keine Bewertungen
- WORDDokument1 SeiteWORDMuhammad Yamin LNoch keine Bewertungen
- Water Deprivation Test in AdultsDokument4 SeitenWater Deprivation Test in AdultsMuhammad RizkiNoch keine Bewertungen
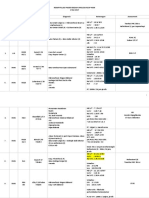
- TIME Table-NewwDokument5 SeitenTIME Table-NewwMuhammad Yamin LNoch keine Bewertungen
- Writing Detailed Paragraph OutlineDokument1 SeiteWriting Detailed Paragraph OutlineMuhammad Yamin LNoch keine Bewertungen
- REKAP URO 1 Mei 2017Dokument9 SeitenREKAP URO 1 Mei 2017Muhammad Yamin LNoch keine Bewertungen
- TIME Table-NewwDokument5 SeitenTIME Table-NewwMuhammad Yamin LNoch keine Bewertungen
- Emergent Management of Myasthenia GravisDokument8 SeitenEmergent Management of Myasthenia GravisMuhammad Yamin LNoch keine Bewertungen
- REKAP URO 1 Mei 2017Dokument9 SeitenREKAP URO 1 Mei 2017Muhammad Yamin LNoch keine Bewertungen
- Referensi SumenDokument1 SeiteReferensi SumenMuhammad Yamin LNoch keine Bewertungen
- JURNAL OK 5 Cara Kerja Kunyit D CurcumaDokument12 SeitenJURNAL OK 5 Cara Kerja Kunyit D CurcumaMuhammad Yamin LNoch keine Bewertungen
- Syphilis and Hi V InfectionDokument7 SeitenSyphilis and Hi V InfectionMuhammad Yamin LNoch keine Bewertungen
- Article1380536366 - Shahzadi Et AlDokument5 SeitenArticle1380536366 - Shahzadi Et AlSilene A. RiveraNoch keine Bewertungen
- Benzocaine (Dermoplast, Lanacane, Unguentine) 2. Chloroprocaine (Nesacaine) 3. Procaine (Novocaine)Dokument4 SeitenBenzocaine (Dermoplast, Lanacane, Unguentine) 2. Chloroprocaine (Nesacaine) 3. Procaine (Novocaine)Gretchen BadayosNoch keine Bewertungen
- Administration of Pediatric PDFDokument14 SeitenAdministration of Pediatric PDFeny RusmiyatiNoch keine Bewertungen
- Guide To ExtrusionDokument26 SeitenGuide To ExtrusionchevypickupNoch keine Bewertungen
- Pharmacotherapy PlanDokument25 SeitenPharmacotherapy PlanMahum SohailNoch keine Bewertungen
- Epilepsy in PregnancyDokument10 SeitenEpilepsy in PregnancyHabib G. Moutran BarrosoNoch keine Bewertungen
- BioPharm Asia 2007, Speaker's BiographiesDokument25 SeitenBioPharm Asia 2007, Speaker's Biographiesmabs008014Noch keine Bewertungen
- Abidec DropsDokument6 SeitenAbidec DropsRouag AbdelkarimNoch keine Bewertungen
- Evmlu Uganda.2020Dokument124 SeitenEvmlu Uganda.2020ALINOMUGASHA EMMANUELNoch keine Bewertungen
- The Biopharmaceutical Classification System (BCS) : DR Mohammad IssaDokument24 SeitenThe Biopharmaceutical Classification System (BCS) : DR Mohammad IssaDevi IndrianiNoch keine Bewertungen
- Good Manufacturing Practice (GMP) : History, Structure and Its SignificanceDokument9 SeitenGood Manufacturing Practice (GMP) : History, Structure and Its SignificanceMarco El ShaddollNoch keine Bewertungen
- Understanding Pharmacology For Pharmacy Technician 230904 234215Dokument862 SeitenUnderstanding Pharmacology For Pharmacy Technician 230904 234215Sohail AdnanNoch keine Bewertungen
- SDTM TerminologyDokument512 SeitenSDTM TerminologySuri VijayNoch keine Bewertungen
- In Komp A Tibi LitasDokument54 SeitenIn Komp A Tibi LitasHifi Rizki.RNoch keine Bewertungen
- Pcol2 New SyllabusDokument15 SeitenPcol2 New SyllabusChynna Ulep AlbertNoch keine Bewertungen
- M7 Pharmaceutical Policy Analysis (10-14 July 2017) : Course DirectorsDokument2 SeitenM7 Pharmaceutical Policy Analysis (10-14 July 2017) : Course DirectorsHananAhmedNoch keine Bewertungen
- Emergency Trolley ListDokument2 SeitenEmergency Trolley ListaristyaNoch keine Bewertungen
- 2614 PDFDokument11 Seiten2614 PDFAdriani HasyimNoch keine Bewertungen
- El AfrancesadoDokument6 SeitenEl AfrancesadoBrandi BranBran NickelsNoch keine Bewertungen
- Job DescriptionDokument2 SeitenJob DescriptionswethashakiNoch keine Bewertungen
- Market Overview Consumption Map Major ConsumersDokument1 SeiteMarket Overview Consumption Map Major ConsumersPrakrutiShahNoch keine Bewertungen
- Ianswer: Bps 4125/Chm 4123 Medicinal Chemistry Midterm 1 (October 5, 2018)Dokument7 SeitenIanswer: Bps 4125/Chm 4123 Medicinal Chemistry Midterm 1 (October 5, 2018)Halima AdenNoch keine Bewertungen
- 100-Article Text-392-1-10-20170918Dokument2 Seiten100-Article Text-392-1-10-20170918arun sNoch keine Bewertungen