Beruflich Dokumente
Kultur Dokumente
Association of Mortality With Age of Blood Transfu
Hochgeladen von
DELLCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Association of Mortality With Age of Blood Transfu
Hochgeladen von
DELLCopyright:
Verfügbare Formate
1256 REPORTS OF INVESTIGATION
Association of
mortality with age
of blood transfused in F. Robert Purdy MSc DVM MD FRCPC,
Martin G. Tweeddale PhD MD FRCPC,
septic ICU patients Pamela M. Merrick BSN
Purpose: To determine, retrospectively, the age of packed red blood cell (PRBC) units transfused to patients
admitted to the ICU with the diagnosis of severe sepsis and to correlate this variable with outcome.
Methods: All patients admitted to the ICU during 1992 with a diagnosis of severe sepsis were selected retro-
spectively. The criteria for the diagnosis of severe sepsis and septic shock were based on established guidelines.
For each patient the total number of PRBC units transfused, the number of units transfused before, during and
after the septic episode, and the age of each PRBC unit transfused were recorded.
Results: Of the 31 patients admitted to the ICU with severe sepsis, 19 died and 12 survived. No statistical dif-
ferences between survivors and nonsurvivors were found with respect to age, sex, number of days in ICU, dura-
tion of sepsis, incidence of septic shock, admission Apache II score or total number of PRBC units transfused.
During sepsis the median age of PRBC units transfused to survivors was 17 days (range 5-35) vs 25 days (range
9-36) for nonsurvivors (P < 0.000 I). A negative correlation (r = -0.73) was found between the proportion of
PRBC units of a given age transfused to survivors and increasing age of PRBC.
Conclusion: This is the first study to report a correlation of mortality with the age of PRBC transfused. The
cause of this association is unclear. If this association is confirmed by a prospective randomised trial it would have
major implications for the use of PRBC in severe sepsis.
Objectif : DEterminer rEtrospectivement I'~ge des concentrEs Erythrocytaires (CE) transfuses ~ des patients
admis ~ I'unitE des soins intensifs (USI) avec un diagnostic de sepsis grave et vEriJier si cette variable a une cor-
relation avec le devenir des patients.
M & h o d e s : Tousles patients admis ~ I'USI en 1992 avec un diagnostic de sepsis grave ont fait I'objet de cette
recherche retrospective. Les signes et sympt6mes usuels ont servi ~ Etablir les critEres de sepsis grave et de choc
septique. Pour chacun des patients la quantitE totale des CE transfuses, le nombre de CE transfuses avant, pen-
dant et aprEs I'Episode septique et I'~ge de chaque CE transfuse ont EtE enregistrEs.
R ~ u l t a t s : Parmi les 31 patients admis ~ I'USI pour sepsis grave, 19 sont dEcEdEs et 12 ont surv&u. II n'y avait
pas de difference statistique entre survivants et non survivants en rapport ~ I'~ge, le sexe, la durEe du sEjour
I'USI, la durEe du sepsis, I'incidence du choc septique, le score APACHE II ~ I'admission et le nombre de CE trans-
fuses. Au cours du sepsis, I'~ge median des CE transfuses Etait de 17 jours (Ecart 5--35) vs 25 jours (&art 9-39)
pour les non survivants (P < 0,0001). On a trouvE une correlation negative (r = -0,73) entre la proportion de
CE d'un ~ge dEterminE transfuse aux survivants et I'accroissement de I'~ge des CE.
Conclusion : II s'agit ici de la premiere Etude concluant ,~ une correlation avec I'~-gedes CE transfuses. La rai-
son de cette association n'est pas claire. Si une Etude alEatoire prospective parvient ~ confirmer cette assertion,
elle aurait des repercussions majeures sur la transfusion de CE darts }e sepsis grave.
From the Intensive Care Unit and Department of.Anaesthesia, Vancouver Hospital and Health Sciences Centre, Vancouver, BC, Canada.
Address correspondenceto: M.G. Tweeddale MD, Intensive Care Unit, Vancouver Hospital and Health Sciences Centre, 855 West 12th
Ave., Vancouver, B.C. Canada V5Z IM9.
This study was presented, in part, as a poster at the combined meeting of the British and Irish Intensive Care Societies, Dublin Ireland,
April 1994 and at the Canadian Critical Care Society meeting, Toronto, September 1994.
Aecepted for publicarion September 10, 1997.
CAN J ANAESTH 1997 / 44:12 / pp 1256-1261
P u r d y et al.: MORTALITY AND AGE OF BLOOD 1257
HERE are no reports correlating clinical tion. Outcome was determined on discharge from the
T outcome with the age of packed red blood
cells (PRBC) transfused in critically ill
patients. The currently accepted limit of 35
days for PRBC storage was derived from in vitro rheo-
logical and metabolic indices and post-transfusion ery-
ICU. For each patient the following data were record-
ed: age, sex, outcome, number of days in hospital, nuna-
bet of days in ICU, admission APACHE II score,
admission diagnosis, focus of infection, organism(s) cul-
tured, duration of sepsis, inotrope use, total number of
throcyte survival percentages) Clinical trials to support PRBC units transfused, the number of milts transfused
tiffs limit have not been performed. Increased rates of before, during and after the septic episode, and the age
infection, multi-organ dysfunction syndrome and mor- of each PRBC unit transfused. The storage medium for
tality have been associated with PRBC transfusion in all PRBC was CPDA-1. Indications for transfusion were
critically iH patients, 2,s but immunological mechanisms based on the clinical judgment of the ICU attending
were postulated as the likely cause and the age of the physician.
PRBC units was not considered. These studies have Group differences were analysed by Mann-Whitney
been controversial in that PRBC transfusion may be a tests while proportional data were compared using
marker for severity of ilk ;ss and not an independent chi-square t e s t s o r F i s h e r ' s e x a c t t e s t s as a p p r o p r i a t e .
predictor of outcome. However, thcrc arc two studies Linear regression analysis was performed on the pro-
suggesting that the age of blood transfused to critically portion of PRBC units of a given age transfused to
ill patients may influence the physiological response to survivors. Differences were considered significant at
t r a n s f u s i o n 4 and the clinical outcome, s P < 0.05. Bonferroni's correction was applied when
The changes that occur with storage of red blood appropriate to adjust for multiple comparisons.
cells are well documented and include both reversible Because data were not normally distributed, restdts are
and irreversible alterations. 1 These changes include reported as medians and range.
decreased levels of 2,3-DPG and altered red blood cell
rheology both of which may adversely affect oxygen TABLE I Definitions
delivery to, and oxygen uptake by, tissues. Though it
1) Definitions from the American College o f Chest
is not common practice, it has been recommended
Physicians/Society o f Critical Care Medicine Consensus
(based on 2,3-DPG depletion studies) that patients Conference on sepsis and organ failure 1992. 6
with a compromised circulation should not receive
Sepsis: The systemic response to infection. This systemic response is
PRBC units older than 14 days) We hypothesised that manifcsted by two or more o f the following conditions as a result o f
mortality might be influenced by the transfusion of infection:
older PRBC in septic ICU patients. Therefore, we Temperature >38~ or <36~
determined, retrospectively, the age of PRBC trans- Heart ?ate >90 bpm
Respiratory rate >20 breaths.rainq or PaC02 <3 m m H g (<4.3 kPa)
fused in a group of septic ICU patients and deter-
WBC >12,000 cells.ram-s, <4000 cells.mm-s or >10% immature
mined its relationship to survival. (band) forms
Severe Sepsis."Sepsis associated with organ dysfunction, hypoperfu-
Methods sion, or hypotension. Hypoperfusion and perfusion abnormalities
All patients admitted to the ICU during the calendar may include, but are not limited to lactic acidosis, oliguria, or an
year 1992 with a diagnosis of severe sepsis were select- acute alteration in mental status.
ed retrospectively from the data base of our tertiary Septic Shock: Sepsis with hypotension, despite adequate fluid resus-
care, multidisciplinary, adult ICU. Study design was citation, along with the presence o f perfusion abnormalities that
may include, but are not limited to, lactic acidosis, oliguria, or an
approved by the UBC Clinical Screening Committee
acute alteration in mental status. Patients who are on inotropic or
for Research Involving Human Subjects. Patients devel- vasopressor agents may not be hypotensive at the time that perfu-
oping severe sepsis after ICU admission could not be sion abnormalities are measured.
included since the ICU data base recorded only the Hypotension: A systolic BP o f <90 mm H g or a reduction o f >40
admission diagnosis. The criteria for the diagnosis of m m H g from baseline in the absence of other causes for h3q~otension.
severe sepsis arid septic shock were based on established Multiple Organ Dyoq~netion Syndrome: Presence o f altered organ
g u i d e l i n e s 6 (Table I). The earliest time at which the cri- function in an acutely ill patient such that homeostasis cannot be
teria for sepsis were met was identified from each record maintained without intervention.
and was considered to be the onset of the septic 2) Definitions made for this study.
episode. Resolution of sepsis was defined arbitrarily and Onset of Sepsis: The time when the criteria for sepsis are first met.
prospectively as at least 48 hr of failure to meet the cri- Resolution of Sepsis: The time when the criteria for sepsis are absent
teria for sepsis. Infection was confirmed by the finding for 48 consecutive hours.
of a clinically appropriate culture-positive site of infec-
1258 CANADIAN JOURNAL OF ANAESTHESIA
TABLE II Clinical characteristics of 31 adult patients admitted to ICU with severe sepsis.
Age* Sex APACHE II Score* Number with septic Days in ICU*
(yr) (male/female) shock
Survivors 66( 19-84 ) 7/5 31(18-45) 9 5(2-104 )
(n = 12)
Nonsurvivors 61(16-81) 10/9 33(20-55) 16 4(1-216)
(n = 19)
P 0.56 0.76 0.06 0.65 .27
*median(range)
"FABLE III Number and age of PRBC units transfused to septic patients.
During Hospital Admission During Septic Episode*
Number of units Age of units Number of units Age of units
tran~q~sed/patient (days) rranoCused/patient (days)
survivors 6(1-98) 21(5-35)[18-23] 5(2-70) 17(5-35)[16--19]
nonsurvivors 10(2-103) 24(7-36)[23-26] 8(2-103) 25(9-36)[23-27]
P 0.21 <0.0001 0.21 <0.0001
Values ,are median(range)[95% CI]
"results do not include two survivors who did not receive PRBC during sepsis
PRBC, packed red blood cells
Results between survivors (median 21 days) and nonsurvivors
O f 32 patients admitted to the ICU during 1992 with (median 24 days, Table III). Further analysis showed
the diagnosis of severe sepsis, 31 received PRBCs dur- that there was no difference between survivors and
ing their hospital admission and formed the study nonsurvivors in age of PRBC units transfused before
group. O f these 31 patients (Table II) 19 died, with all the onset of sepsis (P= 0.92), but there was a difference
deaths occurring during sepsis and in the ICU. Twelve in the age of PRBC milts transfused during sepsis.
patients survived to be discharged from hospital. When only those PRBC units transfused during sepsis
Twenty-six patients had positive blood cultures, nine were considered (excluding two survivors who did not
were survivors (75%), and 17 were nonsurvivors (89%). receive transfusions while septic), the median age
The criteria for septic shock were met by nine (75%) of PRBC units transfused to survivors was 17 days
survivors and 16 (84%) nonsurvivors. One nonsurvivor compared with 25 days in nonsurvivors (P < .0001,
was discharged from the ICU only to be readmitted Table III). The association between mortality and the
with severe multisystem organ failure from which he did age of PRBC units remained when two patients who
not recover. At no time did this patient meet our crite- received >90 units were excluded (median 16 vs 19
ria for resolution of sepsis so this was judged as a single days, P = 0.0014). The association was also present, but
septic episode. There were no differences between sur- not statistically significant with Bonferroni's correction,
vivors and nonsurvivors with respect to age, sex, days in when only those patients (five survivors and four non-
ICU, duration of sepsis, incidence of septic shock, or survivors) who received five or fewer units during sep-
APACHE II score, although the latter approached sig- sis were considered (median 23 vs 29.5 days, P--- .12).
nificance (P = 0.06). When analysed from a different perspective, the pro-
A total of 555 PRBC units were transfused during portion of PRBC units < 16 days of age transfused dur-
hospital admission to the 31 study patients. Ninety ing sepsis to survivors was 79/163 (48%) vs 7 5 / 2 8 4
seven PRBC units were transfused before the onset of (26%) to nonsurvivors (Figure 1, P < 0.0001). To
sepsis, 447 dtmng sepsis and 11 units after resolution of examine this difference further, PRBC units given dur-
sepsis. The latter were too few to analyse. While there ing sepsis were grouped by age and in each age group
was no difference in the total number of units of PRBC the proportion of PRBC transfused to survivors and
transfused to survivors and nonsurvivors (Table III), nonsurvivors was determined (Figure 2). Although
there was a difference (P < 0.0001) with respect to the PRBC of ages 10-20 days were evenly distributed
age of PRBC units transfused during hospitalisation among survivors and nonsurvivors, survivors received a
Purdy et al.: MORTALITY AND AGE OF BLOOD 1259
greater proportion of PRBC <10 days old (85%) while Discussion
nonsurvivors received a greater proportion of PRBC This is the first study to report an association between
>20 days old (76%). Linear regression analysis of the mortality and the age of PRBC units transfused in crit-
proportion of PRBC units of a given age transfused to ically ill patients. While this is an important subject for
survivors against the age of those units demonstrated a further investigation, the association cannot be consid-
negative correlation (r = -.73, P < .0001). ered proven or causal. Several limitations of this prelim-
inary study must be acknowledged. The study is small
and retrospective with neither randomisation nor con-
trol over the age of PRBC units transfused. Individual
patients often received PRBC units with a wide age
range and over a variable time. A few patients received
a large number of PRBC units. Despite these limita-
tions, the association of mortality with the age of PRBC
units transfused which we have described is compatible
with the known changes in PRBC which occur with
storage, 1 and is supported by a recent publication
reporting increased mortality in a septic rat model fol-
l o ~ n g transfusion with older stored red blood cells. 7
Further indirect support for possible adverse effects of
transfusion of older PRBC is provided by the report
that older PRBC units did not improve splanchnic per-
fusion (as assessed by ultramucosal gastric pH) in septic
patients, 4 and that increased ICU length of stay is asso-
ciated with the transfusion of older PRBC. s
Our study provides no information about the possi-
ble cause(s) for the association which we have described.
However, altered regional and microcirculatory blood
flow and oxygen utilisation are believed to be central to
the development of organ dysfunction in sepsis, s This
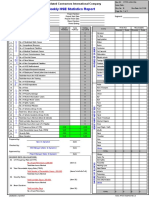
F I G U R E 1 Proportion o f PRBC units o f different age transfused may be due in part to sepsis-induced rheologic changes
to survivors and nonsurvivors during sepsis
in blood cells. 9,1~ The changes in erythrocytes during
(P< .0001). n = number o f PRBC units in each subgroup. storage, many of which are irreversible, have been well
documented and include decreased deformability, sur-
face area and fluidity, with increased viscosity and serial
enzyme, membrane protein and ion changes. Oxygen
affinity is increased due to depletion of 2,3-DPG. 1
Transfusion of PRBC, while increasing global oxygen
delivery during sepsis,-may not improve regional blood
flow4,11 and transfusion older PRBC units may not be
associated with increased oxygen uptake. 6 One plausible
hypothesis is that, in the septic patient, the decreased
deformability and increased oxygen affinity of transfused
older PRBC results in decreased splancl'mic blood flow
and oxygen utilisation. This may lead to increased gut
permeability to bacteria and/or bacterial by-products
with a resultant intensification of the septic response.
Another possible explanation for the association
reported here is that the number of PRBC units trans-
fused and/or the duration of storage resulted in increased
immunosupression. Enhanced kidney graft survival, 12
F I G U R E 2 Proportion o f PRBC units in different age strata
transfused during sepsis in survivors and nonsurvivors. Under each increased tumour recurrencO s,14 and increased rates of
age stratum, the summation o f the proportions transfused to sur- post-operative infection Is-19 have all been reported fol-
vivors and nonsurvivors equals one. lowing PRBC transfusion. While plasma has been shown
1260 CANADIAN JOURNAL OF ANAESTHESIA
to have immunomodulatory effects, the primary cellular Acknowledgments
constituent of PRBC units responsible for immtmosu- Dr. G. Growe scientific advisor. Dr. S. Naiman,
pression may be white blood cells. 19a~ Leucocyte deple- Dr. D. Bevan, Dr. J. Fenwick and Dr. D. Parsons for
tion greatly attenuates the immunosupressive effect of review o f this manuscript. Mrs. P. Lessard and the
PRBC transfusion. 19~~The PKBC units in our study were medical records d e p a r t m e n t o f the Vancouver
not leucocyte depleted. Increasing mitogenic activity21 Hospital for their assistance with patient records.
and histamine release22 have both been associated with
PRBC storage time but there is some evidence to suggest References
that the inamunosupressive effect of PRBC may be maxi- 1 Hogman CF. Liquid storage of human erythrocytes.
mal at two weeks of storage and that PRBC units stored In: Harris JR (Ed.). Blood Separation and Plasma
for greater than three weeks may have tittle immunosu- Fractionation. New York: Wiley-Liss, 1991: 63-97.
pressive effect.23 If this is true it suggests that immunosu- 2 Busund R, Straume B, Revhaug A. Fatal course in severe
pression was not responsible for the association reported meningococcemia: clinical predictors and effect of trans-
in our study since, on this basis, patients receiving older fusion therapy. Crit Care Med 1993; 21: 1699-705.
PRBC units should have been less immunocompromised. 3 Chiu P, Roy PD, MarshallJC. Blood transfusion is a
Confounding (and possibly interacting) variables risk factor for ICU-acquired infection and the multiple
which we could not separate out in this study may organ dysfimction syndrome (MODS) (Abstract).
account for the association which we have described. Crit Care Med 1993; 21: $226.
For example, the patients that died received a greater 4 Marik PE, Sibbald WJ. Effect of stored-blood
number o f PRBC units (though this was not statisti- transfusion on oxygen delivery in patients with sepsis.
cally significant). This could be either a marker for JAMA 1993; 269: 3024-9..
severity o f illness (APACHE II scores also tended to 5 Martin CM, Sibbald W~, Hebert P, Schweitzer [. Age of
be higher in nonsurvivors) or the larger transfusion transfused red blood cells'is associated with ICU length
load could have had an adverse effect on outcome. of stay (Abstract). Clin Invest Med 1994; 17: B21,124.
Similarly subtle interactions between the severity o f ill- 6 Membersof the ACCP/CCM Consensus Conference
ness and length o f stay in survivors and nonsurvivors Committee. American College of Chest Physicians/Society
might have resulted in the latter receiving more PRBC of Critical Care Medicine Consensus Conference:
units over a longer time period. Because blood bank definitions for sepsis and organ failure and guidelines for
policy releases older PRBC units first, this could have the use of innovative therapies in sepsis. Crit Care Med
resulted in nonsurvivors receiving a greater propor- 1992; 20: 864-74.
tion o f older PRBC units, and hence the relationship 7 SielenkdimperA, Martin CM, d'Almeida M, Sibbald
which we have described. WJ, Chin-Yee I. Transfusion of "old" blood is associat-
Few general inferences can be drawn from this ed with increased mortality in septic rats (Abstract).
study which was confined to adult I C U patients Proceedings from the Canadian Society of Transfusion
admitted with the diagnosis o f severe sepsis. Whether Medicine annual meeting, 1996: 036.
other patient groups would show a similar association 8 Sibbald WJ, Fox G, Martin C. Abnormalities of vascular
is unknown. Similarly, no deduction can be made as to reactivity in the sepsis syndrome. Chest 1991; 100:
what constitutes an acceptable duration o f PRBC stor- $155-9.
age for the septic patient. However, review o f studies 9 Machiedo GW, Powell RJ, Rush BFJr, Swisloeki NI,
measuring 2,3-DPG depletion during PRBC storage Dikdan G. The incidence of decreased red blood cell
has led to the recommendation that in patients with deformability in sepsis and the association with oxygen
compromised circulation PRBC storage for 14 days free radical damage and multiple-system organ failure.
or less may be preferred. 1 This recommendation is Arch Surg 1989; 124: 1386-9.
supported by our findings and by those previously 10 Astiz ME, DeGent GE, Lin RY, Rackow EC.
reported .4,5 Microvascular function and theologic changes in hyper-
The association we have described between mortal- dynamic sepsis. Crit Care Med 1995; 23: 265-71.
ity and age o f PRBC transfusion, if confirmed by a 11 Lorente JA, Landln L, De Pablo R, Renes E, Rodrlgue
prospective randomised study, would have major Z-Diaz R, Liste D. Effects of blood transfusion on oxy-
implications for blood banking and the use o f PRBC gen transport variables in severe sepsis. Crit Care Med
in the critically ill septic patient. Further studies are 1993; 21: 1312-8.
urgently needed to confirm or refute this association 12 Rodey GE. Blood transfusions and their influence on
and to determine whether or not there are deleterious renal allograft survival. Prog Hematol 1986; 14:
effects from the transfusion o f older PRBC units. 99-122.
Purdyetal.: MORTALITY AND AGE OF BLOOD 1261
13 ClarkePJ, TarinD. Effectofpre-operative bloodtransfu-
sionon mmourmetastases. Br J Surg1987;74: 520-2.
14 ChungM, Steinmetz (91(,GordonPH. Perioperative
bloodtransfusion andoutcomeafterresection for col-
orectalcarcinoma. Br J Surg 1993;80: 427-32.
15 JensenLS, Andersen AJ, Christiansen PM, etal.
Postoperative infectionandnaturalkiller cell function
followingbloodtransfusion in patientsundergoing
electivecolorectal surgery.Br J Surg 1992;79: 513-6.
16 TartzerPI. Bloodtransfusion andinfectious
complications followingcolorectal cancersurgery.
Br J Surg 1988;75: 789-92.
17 MiholicJ, HudecM, DomanigE, etal. Risk factorsfor
severebacterialinfections aftervalvereplacement and
aortocoronary bypassoperations: analysisof 246 casesby
logisticregression.Ann ThoracSurg1985;40: 224-8.
18 TriulziDJ, Vanek1(,RyanDH, Blumberg N. A clinical
andimmunologic studyof bloodtransfusion andpostop-
erativebacterialinfectionin spinalsurgery.Transfusion
1992;32: 517-24.
19 JensenLS, Kissmeyer-Nielsen P, WolffB, QvistN.
Randomised comparison of leucocyte-depleted versus
buffy-coat-poor bloodtransfusion andcomplications
aftercolorectal surgery.Lancet1996;348:841-5.
20 Blumberg iV, HealJM. Effectsof transfusion on
immunefunction.Cancerrecurrence andinfection.
Arch PathLab Med 1994;118:371-9.
21 HohH, Umpleby H, CooperA, TaylorL Recurrence of
colorectalcancerandperioperative bloodtransfusion.
Is bloodstoragetimeimportant? Dis Colon Rectum
1990;33: 127-30.
22 NielsenH], Edvardsen L, Vangsgaard K, Dybkj~rE,
SkovPS. Time-dependent histamine releasefromstored
humanbloodproducts.Br J Surg 1996;83: 259-62.
23 MincheffMS,MerymanHT. Blood transfusion, blood
storageandimmunomodulation. Immunological
Investigations 1995;24: 303-9.
All in-text references underlined in blue are linked to publications on ResearchGate, letting you access and read them immediately.
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- AminoglycosidesDokument20 SeitenAminoglycosidesHassan.shehri100% (5)
- Outline SpecificationDokument13 SeitenOutline SpecificationDELL100% (3)
- Hse Statistics Report Pp701 Hse f04 Rev.bDokument1 SeiteHse Statistics Report Pp701 Hse f04 Rev.bMohamed Mouner100% (1)
- Clinical Chemistry Review 1 110Dokument6 SeitenClinical Chemistry Review 1 110DELLNoch keine Bewertungen
- Cataract Consent FormDokument4 SeitenCataract Consent FormHitesh Sharma100% (1)
- Assisting IV BTDokument89 SeitenAssisting IV BTmhelshy villanuevaNoch keine Bewertungen
- DEVPSY Reviewer - Chapters 1-6 PDFDokument19 SeitenDEVPSY Reviewer - Chapters 1-6 PDFKathleen Anica SahagunNoch keine Bewertungen
- A Detailed Lesson Plan Practical Research 2Dokument29 SeitenA Detailed Lesson Plan Practical Research 2Erica CanonNoch keine Bewertungen
- What Is Genetic Modification?Dokument4 SeitenWhat Is Genetic Modification?DELLNoch keine Bewertungen
- Hematology ReviewDokument4 SeitenHematology ReviewDELLNoch keine Bewertungen
- OoDokument6 SeitenOoDELLNoch keine Bewertungen
- 09 - Chapter 3 PDFDokument21 Seiten09 - Chapter 3 PDFDELLNoch keine Bewertungen
- OoDokument6 SeitenOoDELLNoch keine Bewertungen
- Kinyoun Carbol Fuchsin Stain: Formulation Per 100 MLDokument3 SeitenKinyoun Carbol Fuchsin Stain: Formulation Per 100 MLDELLNoch keine Bewertungen
- Histopathology Unit 1Dokument6 SeitenHistopathology Unit 1DELLNoch keine Bewertungen
- CM Machine With Orig. ArticleDokument4 SeitenCM Machine With Orig. ArticleDELLNoch keine Bewertungen
- Lecture 6 Antibody Structure and Function1Dokument25 SeitenLecture 6 Antibody Structure and Function1DELLNoch keine Bewertungen
- Human Resources Management Case StudyDokument6 SeitenHuman Resources Management Case Studyren180Noch keine Bewertungen
- UTILITIES EPG ModelDokument1 SeiteUTILITIES EPG ModelDELLNoch keine Bewertungen
- Treatment of DataDokument1 SeiteTreatment of DataDELLNoch keine Bewertungen
- Antibodies: Structure and FunctionDokument27 SeitenAntibodies: Structure and FunctionDELLNoch keine Bewertungen
- Histopath Classification of DiseasesDokument8 SeitenHistopath Classification of DiseasesDELLNoch keine Bewertungen
- BhutanNationalStandardsBTServices PDFDokument98 SeitenBhutanNationalStandardsBTServices PDFDELLNoch keine Bewertungen
- Histopathology Unit 1Dokument6 SeitenHistopathology Unit 1DELLNoch keine Bewertungen
- 2013 05 22 Structural Dwgs PDFDokument31 Seiten2013 05 22 Structural Dwgs PDFDELLNoch keine Bewertungen
- 7.2P CLINPATH Platelets, Blood Coagulation and Fibrinolysis Disorders Leukocytic Disorders Dr. EspirituDokument8 Seiten7.2P CLINPATH Platelets, Blood Coagulation and Fibrinolysis Disorders Leukocytic Disorders Dr. EspirituDELLNoch keine Bewertungen
- Growth Patterns On Plated Medium: Experiment 16: Cultural CharacteristicsDokument3 SeitenGrowth Patterns On Plated Medium: Experiment 16: Cultural CharacteristicsDELLNoch keine Bewertungen
- " Three Star Hotel ": Basement Power Layout Ground Floor Power Layout Mezzanine Power LayoutDokument1 Seite" Three Star Hotel ": Basement Power Layout Ground Floor Power Layout Mezzanine Power LayoutDELLNoch keine Bewertungen
- FunctionalismDokument5 SeitenFunctionalismDELLNoch keine Bewertungen
- Why Bahay Kubo Is Considered A Cultural IconDokument1 SeiteWhy Bahay Kubo Is Considered A Cultural IconDELLNoch keine Bewertungen
- HistoryDokument2 SeitenHistoryDELLNoch keine Bewertungen
- Productive InfectionDokument1 SeiteProductive InfectionDELLNoch keine Bewertungen
- PancreasDokument1 SeitePancreasDELLNoch keine Bewertungen
- I. Introduction To EndocrinologyDokument7 SeitenI. Introduction To EndocrinologyDELLNoch keine Bewertungen
- Bone Marrow StudiesDokument3 SeitenBone Marrow StudiesDELLNoch keine Bewertungen
- Bile Esculine TestDokument2 SeitenBile Esculine TestVincent OngNoch keine Bewertungen
- Occupational HealthDokument8 SeitenOccupational HealthFemale calm0% (1)
- Left Thigh Pain: I. Chief Complaint/ Other ComplaintsDokument9 SeitenLeft Thigh Pain: I. Chief Complaint/ Other ComplaintsDominic BristolNoch keine Bewertungen
- ReferensiDokument2 SeitenReferensiYuanita RosalinaNoch keine Bewertungen
- Material Safety Data Sheet: 80W-90 Gear LubeDokument4 SeitenMaterial Safety Data Sheet: 80W-90 Gear LubeFrank RodriguezNoch keine Bewertungen
- AdrDokument9 SeitenAdrvizzladNoch keine Bewertungen
- Ent AssessmentDokument23 SeitenEnt AssessmentPdianghunNoch keine Bewertungen
- Factory Farming in The Developing WorldDokument10 SeitenFactory Farming in The Developing WorldDaisyNoch keine Bewertungen
- PhysioEx 9,1: Exercise 7 Activity 3: PEX-07-03Dokument7 SeitenPhysioEx 9,1: Exercise 7 Activity 3: PEX-07-03mishael_baig100% (8)
- Effect of Nasapana in The Management of Avabahuka A Case StudyDokument5 SeitenEffect of Nasapana in The Management of Avabahuka A Case StudyEditor IJTSRDNoch keine Bewertungen
- B12.Knowledge and Perceptions About COVID-19 Among The Medical and Allied Health Science Students in IndiaDokument6 SeitenB12.Knowledge and Perceptions About COVID-19 Among The Medical and Allied Health Science Students in IndiaWislianaNoch keine Bewertungen
- Rufenal EmulgelDokument2 SeitenRufenal EmulgelDr.2020Noch keine Bewertungen
- Blood Grouping ReagentsDokument7 SeitenBlood Grouping ReagentsDominic EmerencianaNoch keine Bewertungen
- Morena E. Dail, RMT, MT (Amt), Mls (Ascpi) : Mors CodeDokument53 SeitenMorena E. Dail, RMT, MT (Amt), Mls (Ascpi) : Mors CodemeriiNoch keine Bewertungen
- Detect Pharmaceutical Health Hazards and ActDokument81 SeitenDetect Pharmaceutical Health Hazards and Acttemesgen dinsaNoch keine Bewertungen
- CCRT Cervix2Dokument27 SeitenCCRT Cervix2Marfu'ah Nik EezamuddeenNoch keine Bewertungen
- ECGC PO Descriptive BookDokument74 SeitenECGC PO Descriptive BookAmar Pandey100% (2)
- Veterinary Internal Medicne - 2008 - Bruchim - Heat Stroke in Dogs A Retrospective Study of 54 Cases 1999 2004 andDokument9 SeitenVeterinary Internal Medicne - 2008 - Bruchim - Heat Stroke in Dogs A Retrospective Study of 54 Cases 1999 2004 andGuillermo MuzasNoch keine Bewertungen
- Low-Dose Naltrexone (LDN) Fact Sheet 2016: Contact: Linda Elsegood Email: Skype Phone No'sDokument8 SeitenLow-Dose Naltrexone (LDN) Fact Sheet 2016: Contact: Linda Elsegood Email: Skype Phone No'scristiNoch keine Bewertungen
- Important Classifications PDFDokument42 SeitenImportant Classifications PDF330 Himank MehtaNoch keine Bewertungen
- SPM Biology 2019 State Trial Papers Item AnalysisDokument12 SeitenSPM Biology 2019 State Trial Papers Item AnalysisNuan Ting NgNoch keine Bewertungen
- Cardiovascular Responses To An Isometric Handgrip Exercise in Females With PrehypertensionDokument7 SeitenCardiovascular Responses To An Isometric Handgrip Exercise in Females With PrehypertensionGuilherme LimaNoch keine Bewertungen
- Do No Harm by Henry Marsh ExtractDokument15 SeitenDo No Harm by Henry Marsh ExtractAyu Hutami SyarifNoch keine Bewertungen
- Assessment, Northwick ParkDokument2 SeitenAssessment, Northwick ParkMelian Anita100% (1)