Beruflich Dokumente
Kultur Dokumente
Patient Blood Management To Reduce Surgical Risk
Hochgeladen von
Elias Oktovianus HaulussyOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Patient Blood Management To Reduce Surgical Risk
Hochgeladen von
Elias Oktovianus HaulussyCopyright:
Verfügbare Formate
Review
Patient blood management to reduce surgical risk
B. Clevenger1,2 , S. V. Mallett1,2 , A. A. Klein3 and T. Richards1
1
Division of Surgery and Interventional Science, University College London, and 2 Royal Free Perioperative Research Group, Department of
Anaesthesia, Royal Free Hospital, London, and 3 Department of Anaesthesia and Intensive Care, Papworth Hospital, Cambridge, UK
Correspondence to: Mr T. Richards, Division of Surgery and Interventional Science, 4th Floor, UCL Medical School Building, 21 University Street,
University College London, London WC1E 6 AU, UK (e-mail: toby.richards@ucl.ac.uk)
Background: Preoperative anaemia and perioperative blood transfusion are both identifiable and pre-
ventable surgical risks. Patient blood management is a multimodal approach to address this issue. It
focuses on three pillars of care: the detection and treatment of preoperative anaemia; the reduction
of perioperative blood loss; and harnessing and optimizing the patient-specific physiological reserve of
anaemia, including restrictive haemoglobin transfusion triggers. This article reviews why patient blood
management is needed and strategies for its incorporation into surgical pathways.
Methods: Studies investigating the three pillars of patient blood management were identified using
PubMed, focusing on recent evidence-based guidance for perioperative management.
Results: Anaemia is common in surgical practice. Both anaemia and blood transfusion are independently
associated with adverse outcomes. Functional iron deficiency (iron restriction due to increased levels of
hepcidin) is the most common cause of preoperative anaemia, and should be treated with intravenous
iron. Intraoperative blood loss can be reduced with antifibrinolytic drugs such as tranexamic acid, and
cell salvage should be used. A restrictive transfusion practice should be the standard of care after surgery.
Conclusion: The significance of preoperative anaemia appears underappreciated, and its detection
should lead to routine investigation and treatment before elective surgery. The risks of unnecessary blood
transfusion are increasingly being recognized. Strategic adoption of patient blood management in surgical
practice is recommended, and will reduce costs and improve outcomes in surgery.
Paper accepted 11 June 2015
Published online 27 August 2015 in Wiley Online Library (www.bjs.co.uk). DOI: 10.1002/bjs.9898
Introduction and best practice, with cooperative inclusion and empower-
ment of patients when possible, with the aim of improving
Surgical outcomes and 30-day mortality rates are increas-
clinical outcomes.
ingly being analysed, and are readily available to service
PBM focuses on three pillars of care in surgical patients:
commissioners, patients, the media and the general public.
the detection and treatment of preoperative anaemia;
Consequently, increased importance is placed on patient
reduction of perioperative blood loss; and harnessing and
selection and optimization for surgery to reduce patient
optimizing the patient-specific physiological reserve of
risk. However, anaemia is rarely treated in surgical patients,
and blood transfusion is the mainstay of treatment in the anaemia (including restrictive haemoglobin transfusion
perioperative period. Both anaemia and transfusion have triggers)4 (Table 1).
been associated with increased morbidity and mortality1,2 . Blood transfusion is common practice and the tradi-
The term blood management was driven towards tionally accepted solution to surgical anaemia. However,
the patients perspective with the formation of the mounting evidence now suggests that this tradition may
Society for the Advancement of Blood Management in fact be causing harm. PBM aims to integrate this
(http://www.sabm.org), when it had previously been evidence base into a readily applicable bundle of inter-
regarded as managing the supply to blood banks. A ventions to reduce the risk of unnecessary transfusion
paradigm shift towards patient-focused blood man- and optimize patient outcomes after surgery. Blood is a
agement, patient blood management (PBM), has been precious resource and its use is not without complications.
taking place3 . PBM is not an intervention per se, but Throughout the history of transfusion practice, new dis-
goal-oriented patient care based on published evidence coveries have mandated change to improve transfusion
2015 BJS Society Ltd BJS 2015; 102: 13251337
Published by John Wiley & Sons Ltd
1326 B. Clevenger, S. V. Mallett, A. A. Klein and T. Richards
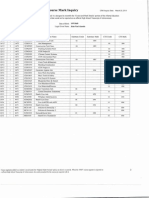
Table 1 Pillars of patient blood management
Pillar 1 Pillar 2 Pillar 3
Optimize erythropoiesis Minimize blood loss Manage anaemia
Preoperative Diagnose anaemia Identify and manage bleeding risk Compare estimated blood loss with
Identify, evaluate and treat anaemia (past medical and family history) patient-specific tolerable blood loss
Treat absolute or functional iron Review medications (antiplatelet, Assess and optimize patients physiological
deficiency anticoagulation therapy) reserve, e.g. pulmonary and cardiac
Consider preoperative autologous Minimize iatrogenic blood loss function
blood donation Procedure planning and rehearsal Formulate patient-specific management plan
Consider erythropoiesis-stimulating using appropriate blood-conservation
agents if nutritional anaemia is ruled modalities
out/treated
Refer for further evaluation as
necessary
Intraoperative Schedule surgery with optimization of Meticulous haemostasis and surgical Optimize cardiac output
red cell mass techniques Optimize oxygenation and ventilation
Anaesthetic blood-sparing strategies Evidence-based transfusion thresholds
Acute normovolaemic haemodilution
Cell salvage/reinfusion
Pharmacological haemostatic agents
Postoperative Stimulate erythropoiesis Monitor and manage bleeding Maximize oxygen delivery
Manage nutrition and correctable Avoid secondary haemorrhage Minimize oxygen consumption
anaemia (e.g. avoid folate Maintain normothermia (unless Avoid/treat infections promptly
deficiency, iron-restricted indicated specifically) Evidence-based transfusion thresholds
erythropoiesis) Autologous blood salvage
Beware of drug interactions that can Minimize iatrogenic blood
increase anaemia sampling loss
Haemostasis/anticoagulation
management
Be aware of adverse effects of
medicines
Prophylaxis of upper gastrointestical
haemorrhage
safety. Syphilis testing began in 1947 and the discovery of The benefits of PBM appear to be clear, particularly in
human immunodeficiency virus in the 1980s brought about surgery, to address the triad of independent risk factors that
another paradigm shift: the introduction of routine blood- affect outcome in surgical patients: anaemia, blood loss and
borne virus screening. Hepatitis C infected as many as 10 transfusion. Significant direct and indirect cost savings can
per cent of blood transfusion recipients from the 1970s be achieved in the surgical setting9 , and early data suggest
and 1980s5 . The risks from prions and other unknown that implementation of PBM strategies is associated with
pathogens remain an area of concern and research. The improved clinical outcomes10 .
Serious Hazards of Transfusion (SHOT) haemovigilance This article reviews why PBM is needed, and how sev-
scheme began in 1996, and the UK Department of Health eral strategies can be incorporated simply and readily into
began to issue Better Blood Transfusion health service surgical pathways. Although much evidence for PBM has
circulars to implement the lessons being learned. arisen from the surgical specialties in which bleeding risk
PBM is the culmination and formalization of such is highest, such as cardiac surgery, this article focuses on
approaches to apply the best current evidence to the the application of PBM to non-cardiac surgery. Major
practice of blood transfusion. It has been adopted by the transfusion protocols are not discussed; the focus is on
World Health Organization6 , and has been proposed by elective clinical practice.
the National Blood Transfusion Committee in the UK.
In recent years, it has developed in a sporadic manner Methods
in Europe7 . Recommendations have since been released
for the implementation of PBM in the National Health Recent studies investigating the three pillars of patient
Service (NHS), with the aim of decreasing avoidable and blood management were identified in PubMed using
inappropriate transfusions of blood and blood products, the keywords patient blood management, bleeding
and optimizing patient care8 . transfusion and preoperative anaemia. Studies
2015 BJS Society Ltd www.bjs.co.uk BJS 2015; 102: 13251337
Published by John Wiley & Sons Ltd
Patient blood management 1327
Table 2 General risks of transfusion
Hazard Mechanism
Transfusion-related immunomodulation Immune mediators accumulate in stored blood
Transfusion-associated circulatory overload Precipitation of congestive cardiac failure or acute left ventricular failure
Transfusion-related acute lung injury Immune-mediated: donor antibodies react with recipient white blood cells, creating
leucoagglutinates that are trapped within the lung
Non-immune-mediated: endothelium suffers an initial insult (e.g. sepsis, surgery or trauma),
attracting neutrophils that are activated by biologically active compounds in stored blood
Injury caused by both mechanisms leads to capillary leak, and neutrophil extravasation and
activation
Haemolytic transfusion reactions Immediate: donor red blood cell membrane antigens react with existing antibodies within recipients
plasma
Delayed: re-exposure to antigen-positive red blood cells in an alloimmunized recipient with specific
antibodies causes a reaction
Acute non-haemolytic transfusion reactions Febrile: recipient white cell antibodies react to donor leucocyte antigens
Allergic: soluble donor antigens react in an already sensitized recipient
Post-transfusion purpura Previous sensitization produces antibodies that attack donor platelet antigens as well as destroying
circulating natural platelets
Transfusion-associated graft versus host Donor lymphocytes proliferate in an immunocompromised recipient, attacking host cells as foreign
disease
Infection13 Viral: estimated risk of infectious donation entering UK blood supply hepatitis B, less than 1 in 12
million donations; HIV, 1 in 7 million, hepatitis C, < 1 in 28 million
Bacterial: 7 cases reported to SHOT, 19962012
Prion: 4 reported cases of vCJD transmission by transfusion in the UK (all before the introduction of
universal leucoreduction of red blood cells in 1999). No practical test for screening donors yet
available
HIV, human immunodeficiency virus; SHOT, Serious Hazards Of Transfusion; vCJD, variant CreutzfeldtJakob disease.
related to the perioperative setting were focused on, P = 038)14 . Trials are ongoing in this area, including a
and supplemented by current national guidelines and randomized clinical trial15 of standard-issue versus fresher
recommendations. RBCs in intensive care patients.
In a systematic review of over 20 000 patients with
Hazards and risks of blood transfusion colorectal cancer, Acheson and colleagues16 found that
588 per cent of patients received a blood transfusion.
Blood transfusion is typically regarded as the solution to Blood transfusion was associated with increased all-cause
anaemia and blood loss in surgery. Aside from the use of mortality (odds ratio (OR) 172, 95 per cent c.i. 155 to
transfusion to replace acute blood loss, surgical patients 191; P < 0001) and an increased OR for cancer-related
receive either preoperative, perioperative or postoperative mortality, combined recurrencemetastasisdeath, post-
top up blood transfusions. Although blood transfusion is operative infection and surgical reintervention, with a
a highly efficient and effective service, there is increasing mean(s.d.) duration of observation of 628(288) months in
evidence to suggest that intraoperative blood transfusions the analysed studies.
increase risk11 , and lead to a dose-dependent increase in In the UK, over 2 million units of RBCs were transfused
morbidity and mortality2 . Even a single unit of transfused in 2012, with more than 2600 adverse events included in
red blood cells (RBCs) has been shown significantly to the 2012 SHOT report17 . This included major morbidity
increase 30-day mortality, composite mortality, pneumonia in 134 patients, four deaths where transfusion contributed
and sepsis12 . to death and five other deaths where transfusion was possi-
The hazards of transfusion include immunomodulatory bly contributory. Separate to this is the cost of transfusion;
effects, risks of circulatory overload, transfusion reactions the cost per unit of RBCs is 169 (122, exchange rate
and infective complications. The immunomodulatory 14 June 2015), at an overall cost of provision to the NHS
effects of transfused blood include increased cancer recur- of 300 million (217 million). However, the cumulative
rence, metastasis and postoperative infection (Table 2). The total NHS costs (including nursing time, patient transport,
effect of storage on RBCs has been of concern, although treatment costs, etc.) are estimated to be nearly three times
the recent ABLE (Age of Blood Evaluation) trial reported this at 878 (635) per unit transfused. In the UK, audits
no significant difference in hazard of death after receiving of transfusion rates by operation and hospital are planned,
transfused fresh blood cells versus standard-issue blood and preoperative anaemia has been proposed as a Key
cells (hazard ratio (HR) 11, 95 per cent c.i. 09 to 12; Performance Indicator.
2015 BJS Society Ltd www.bjs.co.uk BJS 2015; 102: 13251337
Published by John Wiley & Sons Ltd
1328 B. Clevenger, S. V. Mallett, A. A. Klein and T. Richards
Pillar 1: detection and treatment of 120
preoperative anaemia 110
100
Anaemia is a potentially correctable risk in surgery
90
Anaemia, defined as an insufficient circulating RBC mass, 80
Mortality (%)
with a haemoglobin concentration of less than 130 g/l for 70
men and below 120 g/l for women, is common in surgi- 60
cal practice. Its prevalence is generally between 20 and 40 50
per cent in surgical populations, and over 60 per cent in
40
some studies of colorectal surgery18 . The effect of anaemia
30
is well known; even mild anaemia leads to impaired func-
20
tional capacity, physical performance and a reduced qual-
10
ity of life19 . This situation is significant in the surgical
0
population, with ever more elderly patients, and patients
1 8 0
36 38 0
1 0
34 36 0
33 35 0
1 0
31 33 0
1 0
29 31 0
28 30 0
27 29 0
26 28 0
1 0
24 26 0
23 25 0
0
1 0
0
0 0
35 37
32 34
30 32
25 27
22 24
20 23
22
with co-morbidities such as cardiac and pulmonary disease,
>3
<2
1
1
1
1
1
undergoing increasingly complex surgery20 . Normal levels
37
of oxygen delivery are maintained at a haemoglobin con- Preoperative haematocrit (%)
centration of between 60 and 100 g/l as the reduced blood
Fig. 1Mortality rate per unit (per cent) preoperative decrease in
viscosity leads to increased blood flow. Beyond this, tissue
haematocrit from normal baseline (over 38 per cent). Error bars
hypoxia and organ dysfunction become apparent.
represent 95 per cent c.i.; the shaded circle represents data that
Preoperative anaemia is not simply an abnormal labo- were too minimal to be analysed (previously unpublished graph
ratory value, but an important modifiable risk factor for from data presented in Musallam et al.1 )
perioperative morbidity and mortality that compounds the
stress of surgery. Mounting data from a series of stud-
laparoscopic colectomies, Leichtle and colleagues26 found
ies have shown anaemia to be an independent risk factor
that preoperative anaemia was associated with the adverse
for increased morbidity and mortality in cardiac21 and composite outcome of myocardial infarction, stroke, renal
non-cardiac22 24 surgery. insufficiency and 30-day mortality.
Recently, several authors have looked at the effect In a secondary analysis of 39 309 patients undergoing
of anaemia on outcomes using the database from the non-cardiac surgery in the European Surgical Outcomes
American College of Surgeons National Surgical Quality Study (EuSOS)27 , multivariable analysis showed that
Improvement Program (NSQIP). NSQIP prospec- patients with severe or moderate anaemia had a higher
tively collects preoperative patient data, risk factors and in-hospital mortality rate than those with a normal pre-
laboratory results, perioperative complications and 30-day operative haemoglobin concentration: OR 228 (95 per
postoperative outcomes for patients undergoing major cent c.i. 206 to 385) and 199 (167 to 237) respectively.
surgery in more than 200 participating hospitals (https://
www.facs.org/quality-programs/acs-nsqip). In a detailed
multivariable logistic regression analysis of 227 425 Detection of preoperative anaemia
patients undergoing elective major non-cardiac surgery, The significance of preoperative anaemia appears under-
69 229 patients had preoperative anaemia1 . Preoperative appreciated, and its detection should lead to routine inves-
anaemia was associated with a 35 per cent increased risk tigation and treatment. The Network for Advancement
of one major postoperative complication and a 42 per of Transfusion Alternatives (NATA) guidelines28 recom-
cent increased risk of death. This effect of preoperative mend that the haemoglobin level is measured 28 days
anaemia was independent, adjusted for over 60 potential before scheduled surgery in patients undergoing elective
confounders and present for even mild anaemia, with the orthopaedic surgery. European Society of Anaesthesiology
additional effect of a relationship between anaemia severity guidelines29 recommend that patients at risk of bleeding
and outcome: a severityresponse curve (Fig. 1). In a study be assessed for anaemia 48 weeks before surgery. This
of 310 311 veterans from 132 centres, Wu and co-workers25 leaves adequate time to investigate and manage diagnosed
showed that anaemia (in predominantly elderly men) was anaemia without resorting to blood transfusion or delaying
associated with an increased risk of 30-day postoperative surgery.
mortality and cardiac events in elective and emergency There are various reasons for anaemia in surgical
surgery. In a smaller subgroup of 23 348 elective open and patients. The increasingly elderly surgical population is
2015 BJS Society Ltd www.bjs.co.uk BJS 2015; 102: 13251337
Published by John Wiley & Sons Ltd
Patient blood management 1329
Non-elective surgery Elective surgery
Probability of blood Probability of blood
transfusion < 10% transfusion 10%
(independent of anaemia)
Male Hb 130 g/l Anaemia of unknown origin
Female Hb 120 g/l Male Hb < 130 g/l
Female Hb < 120 g/l
Iron status?
Iron deficiency Iron deficiency unlikely
(transferrin saturation < 20%
+ ferritin <30 ng/ml)
Surgical PBM Intravenous iron Further PBM and
checklist (if applicable) evaluation of anaemia
+
surgery
Fig. 2 Preoperative patient blood management (PBM) algorithm. Hb, haemoglobin (adapted from Meybohm et al.34 )
frequently anaemic. Patients can have anaemia of chronic erythropoiesis and functional iron deficiency; such a state
disease (both unexplained and due to co-morbidities), or is the commonest cause of anaemia in patients undergo-
anaemia owing to nutritional deficiencies, blood loss or a ing cardiac surgery31 . In general surgical patients, chronic
combination of these. Iron deficiency is the most prevalent disease, inflammatory disease and malignancy are common
nutritional deficiency worldwide19 . A state of both absolute precipitants of functional iron deficiency32 . Functional iron
and functional iron deficiency can occur. Absolute iron deficiency is the most common cause of anaemia of chronic
deficiency is defined by the lack of stored iron. disease, and is present in around 50 per cent of anaemic
Functional iron deficiency is defined as the occurrence surgical patients.
of iron-restricted erythropoiesis in the presence of nor-
mal or even increased amounts of stored body iron30 . This
results from impaired iron transport, or chronic inflam- Treatment strategies
mation that prevents the uptake and transport of iron British Society of Gastroenterology guidelines33 for the
in situations where iron demand exceeds supply, such as management of iron deficiency anaemia state that all
haemoglobinopathy, chronic haemolytic anaemia or the patients should have iron supplementation to correct
use of erythropoiesis-stimulating agents (ESAs). Trans- anaemia and replenish body stores, and that parenteral
ferrin, a protein that binds and transports iron, can be iron can be used when oral preparations are ineffective
functionally blocked from carrying out its role owing to or not tolerated. A cut-off risk of bleeding of 10 per cent
increased levels of hepcidin, a hormone produced in the is useful in determining those patients in whom elective
liver that is regulated by iron stores and erythropoietic surgery should be postponed if anaemic (Fig. 2).
activity. Hepcidin levels are also increased in inflamma- Oral iron is a longstanding, low-cost treatment for
tory states. Hepcidin increases iron storage by inhibiting anaemia. Total body stores of iron are 34 g in healthy
the transport of iron into the plasma from hepatocytes and people. The bioavailability of ferrous iron is only 1015
macrophages, and from duodenal enterocytes after inges- per cent. This is reduced further by poor absorption
tion. Thus, hepcidin prevents the uptake of dietary iron resulting from the downregulation of duodenal absorp-
from the gastrointestinal tract, leading to iron-restricted tion by inflammation, infection and chronic disease. A
2015 BJS Society Ltd www.bjs.co.uk BJS 2015; 102: 13251337
Published by John Wiley & Sons Ltd
1330 B. Clevenger, S. V. Mallett, A. A. Klein and T. Richards
systematic review35 has demonstrated that oral iron may receiving allogeneic blood transfusions. A more recent
reduce the proportion of patients requiring blood transfu- meta-analysis41 showed a significant risk reduction in
sion. However, enteral iron is absorbed at a rate of 216 mg patients who received preoperative rEPO among patients
per day, and 36 months of treatment can be required undergoing cardiac surgery: RR 053 (95 per cent c.i. 032
to provide 10002000 mg to replenish the physiological to 088; P < 0010) without autologous blood donation
reserve of iron. Reduced uptake is one of the main rea- and 028 (018 to 044; P < 0001) with autologous blood
sons why oral iron often fails to ameliorate anaemia in donation.
surgical patients. Compliance can also be poor owing to The NATA guidelines28 for orthopaedic surgery recom-
the common side-effects of gastrointestinal disturbance, mend that ESAs be used for anaemic patients in whom
including abdominal pain, diarrhoea and constipation. nutritional deficiencies have been ruled out or corrected,
Meta-analysis36 has shown that oral iron has an OR of 232 or both. Use of intravenous iron together with an ESA has
(95 per cent c.i. 174 to 308; P < 0001) compared with been shown to improve the ESA response before surgery42 .
placebo for gastrointestinal side-effects. However, there are safety concerns regarding the use of
Intravenous iron, however, has been shown to be effec- perioperative ESAs43 . Potentially harmful effects include
tive in correcting anaemia in iron-deficient patients, with hypertension, and thrombotic and ischaemic events, pos-
significantly lower odds of gastrointestinal side-effects36 . sibly as a consequence of higher haemoglobin concentra-
Total-dose infusions of iron can now be administered in as tions, and possibly as secondary effects of the ESA on other
little as 15 min. There are several intravenous iron prepara- cells, including stimulation of tumour growth44 . Caution
tions available, including iron dextrans, iron polymaltose, should be exercised when considering the use of ESAs, and
ferumoxytol, ferric carboxymaltose, iron sucrose, ferric conservative dosing regimens are advised.
gluconate and iron isomaltoside37 . Historically, parenteral
iron preparations were associated with high rates of adverse Pillar 2: reduction in perioperative blood loss
events including anaphylaxis. Many reactions were related
to dextran-containing preparations, commonly because Multimodal approach to coagulopathy and
antibodies to dextran can be produced from exposure to haemorrhage
dental caries. Modern carbohydrate preparations have a Reducing perioperative blood loss requires a multimodal
significantly improved safety profile. There is good evi- approach, encompassing anaesthetic and surgical tech-
dence for their safety and efficacy in a range of conditions, nique, pharmacological interventions and cell salvage.
including the perioperative setting24 . A systematic review38 Antiplatelet and anticoagulant therapy is increasingly
demonstrated an increase in haemoglobin concentration being continued into the perioperative period to reduce
and reduced risk of RBC transfusion (relative risk (RR) perioperative cardiovascular risk, and this must be bal-
074, 95 per cent c.i. 062 to 088) with intravenous iron, anced against the risk of bleeding on an individual basis45 .
especially when used with ESAs or in patients with lower The haemostatic management of intraoperative bleeding
ferritin concentrations, but without significant difference requires careful monitoring of coagulation, including the
in mortality or serious adverse events. It must be noted use of point-of-care testing and protocols for the use
that this involved only a few trials in the perioperative set- of blood products and coagulation factor concentrates.
ting and further adequately powered studies with clinically A multimodal approach to coagulopathy and haemor-
meaningful endpoints are required. rhage must be employed, requiring liaison between the
surgical, anaesthetic and haematology teams as appro-
priate. A detailed review of perioperative coagulation
Erythropoiesis-stimulating agents
management is beyond the scope of this article, but recent
Recombinant erythropoietin (rEPO) has longstanding reviews46 48 have focused on this.
use to stimulate erythropoiesis in patients on dialysis. The choice of surgical technique can reduce intra-
Within 5 days of treatment an increase in RBC prolifera- operative blood loss; laparoscopic and minimally invasive
tion in bone marrow is evident. A Cochrane review39 of surgical techniques, such as robotic urological surgery,
rEPO in patients with colorectal cancer failed to show are associated with reduced bleeding. The position of the
any significant change in haemoglobin level with pre- patient during surgery can also influence bleeding. Venous
operative use of rEPO, or a decrease in the number of return can be obstructed, leading to vessel engorge-
patients receiving allogeneic blood. However, a systematic ment and increased venous pressure at the operative site,
review40 of patients undergoing orthopaedic and cardiac increasing bleeding. This is particularly true in lumbar
surgery showed a reduction in the proportion of patients spinal surgery where the patient is in the prone position,
2015 BJS Society Ltd www.bjs.co.uk BJS 2015; 102: 13251337
Published by John Wiley & Sons Ltd
Patient blood management 1331
increasing intra-abdominal compression and epidural Topical haemostatic agents
vessel engorgement. Efforts should be made to ensure that Fibrin sealants are composed of the clotting agents fibrino-
venous drainage is maintained by careful positioning. gen (with or without factor XIII) and thrombin (plus cal-
Neuraxial anaesthesia has been shown to reduce bleed- cium), which promote haemostasis when applied to wound
ing, probably owing to systemic hypotension and decreased surfaces, in a manner similar to the final common pathway
venous tone resulting from sympathetic blockade49 . Avoid- of the coagulation cascade. These can be sprayed or applied
ance of hypervolaemia and hypertension reduces surgical in liquid form. A Cochrane review57 of fibrin sealant use
bleeding, as well as improving operating conditions. reported a relative reduction in the rate of exposure to allo-
The triad of hypothermia, acidosis and hypocalcaemia geneic RBC transfusions by 37 per cent (RR 063, 95 per
must be avoided. Maintenance of normothermia, and cent c.i. 045 to 088). TXA is also used in topical form, in a
avoidance of acidosis and hypocalcaemia are priorities to saline solution or as a gel. A systematic review58 of a range
maintain haemostasis. Below 35 C, platelet function is of surgical specialties demonstrated a reliable reduction in
affected and the efficiency of enzymatic clotting factors surgical bleeding (RR 071, 95 per cent c.i. 069 to 072;
impaired. A decrease in temperature of 1 C increases P < 0001) and the risk of receiving a blood transfusion,
blood loss by approximately 16 per cent and increases the although noted that the effect on thromboembolic events
RR of transfusion by approximately 22 per cent50 . in this group was uncertain.
Pharmacological treatments
Autotransfusion
Antifibrinolytic drugs
Cell salvage
The antifibrinolytic drugs tranexamic acid (TXA) and
-aminocaproic acid are lysine analogues that reversibly RBCs are salvaged from the operative field using a
inhibit fibrinolysis by binding the lysine-binding sites on double-lumen suction device, with anticoagulants added
plasminogen, limiting the activation of plasmin, which to the aspirated blood. This is then stored in a reservoir,
cleaves fibrin strands. A Cochrane review51 of antifibri- before being centrifuged to separate out the components.
nolytic drugs found that TXA produced a RR of RBC The RBCs are washed and filtered, removing biochemical
transfusion of 061 (95 per cent c.i. 053 to 070) and con- debris, including free haemoglobin, white blood cells
cluded that the lysine analogues are effective in reduc- and plasma. These are suspended in normal saline for
ing blood loss during and after surgery, and appear to retransfusion, with a haematocrit of 5070 per cent. Some
be free of serious adverse effects. Prophylactic use of 200 ml of cell-salvaged RBCs equates to 1 unit of blood.
TXA has been shown to reduce perioperative blood loss in Cell salvage has been demonstrated to be cost-effective
cardiovascular, major orthopaedic and liver transplantation compared with transfusion59 . Cell salvage efficiency can be
surgery, urological, gynaecological and obstetric surgery52 . reduced by the concomitant use of antifibrinolytic agents
The dosing regimens vary, but a dose of 1 g is suffi- and haemostatic products. Modern systems allow the suc-
cient for most adults, with no evidence to support the tion device to be used independently, with the centrifuge
use of high doses53 . The CRASH-2 (Clinical Random- consumables used only if sufficient blood is aspirated for
ization of an Antifibrinolytic in Significant Haemorrhage) processing and return; this reduces cost while ensuring
trial54 showed that early (within 3 h of traumatic injury) that the capability to salvage shed RBCs is available.
administration of TXA (1 g followed by a 1-g infusion over Use of intraoperative cell salvage should be encouraged
8 h) significantly reduced the risk of death from haemor- to reduce the need for allogeneic blood transfusion and
rhage and all-cause mortality in traumatic bleeding. Impor- should be considered for operations with an anticipated
tantly, the mortality rate rose if the dose was given after blood loss greater than 1000 ml60 . However, if anticipated
3 h54 . blood loss is greater than 500 ml the authors recommend
Aprotinin reduces fibrinolysis by inhibiting plasmin. It consideration of cell salvage, because blood loss often
was withdrawn from clinical use following a multicentre exceeds this amount, and suctioning of blood with a com-
trial55 that showed an increase in mortality with its use. patible suction circuit, with the option to centrifuge and
However, this finding has been disputed in further analysis reinfuse if sufficient amounts are retrieved. A Cochrane
of that trial and its subsequent meta-analyses, leading to review61 found that the use of cell salvage reduced the
requests for relicensing of aprotinin in both Europe and relative rate of allogeneic RBC transfusion by 38 per cent
Canada, on the basis that its benefits in reducing blood loss (RR 062, 95 per cent c.i. 055 to 070), saving on aver-
and transfusion associated with cardiac surgery outweigh age 068 units of allogeneic RBCs per patient (weighted
its risks56 . mean difference 068; 95 per cent c.i. 088 to 049).
2015 BJS Society Ltd www.bjs.co.uk BJS 2015; 102: 13251337
Published by John Wiley & Sons Ltd
1332 B. Clevenger, S. V. Mallett, A. A. Klein and T. Richards
In orthopaedic surgery, the risk reduction was 55 per in a similar manner to that of functional iron deficiency
cent61 . of chronic disease. Patients who are either anaemic or
Retransfused blood can potentially be harmful owing to non-anaemic (who may nonetheless be iron-deficient)
the presence of other substances aspirated from the surgi- before surgery have been shown to respond well to intra-
cal field, including bacteria and malignant cells. However, venous iron in the postoperative period, with a reduction
studies62,63 have shown that, despite the aspiration of in the incidence of postoperative anaemia, compared with
microbiologically contaminated blood, there is no increase oral iron supplementation66 .
in positive cultures or postoperative infection, even though
the washing phase is unable to eliminate all bacteria. Euro-
Pillar 3: harnessing patient-specic
pean Society of Anaesthesiology guidelines29 suggest that
physiological reserve of anaemia
the decision to use salvaged blood potentially contam-
inated with bacteria or malignant cells should be made A patient-specific plan should be made before surgery to
on an individual basis. In a recent Cochrane review61 , predict the likely intraoperative blood loss. This should
mortality, reoperation for bleeding, infection, wound com- involve consideration of both transfusion thresholds and
plications, non-fatal myocardial infarction, thrombosis, tissue oxygenation, but also methods to minimize blood
stroke and length of hospital stay were not increased by loss and monitor haemostasis during surgery.
cell salvage; indeed, fewer patients who had undergone cell
salvage developed infection or wound complications.
Because retransfused washed RBCs from cell salvage Restrictive transfusion thresholds
provide no plasma, clotting factors or platelets, additional There is an increasing body of evidence demonstrating that
haemostatic therapies (such as platelets or fresh frozen restrictive transfusion thresholds are not inferior to liberal
plasma) may be required. transfusion thresholds and that the use of top-up transfu-
sions is ineffective in stable patients. The landmark TRICC
Acute normovolaemic haemodilution (Transfusion Requirements In Critical Care) study67 , pub-
Acute normovolaemic haemodilution involves the dona- lished in 1999, showed that a restrictive strategy (main-
tion of whole blood by the patient immediately before taining haemoglobin concentration in the range 7090 g/l,
surgery, and its simultaneous replacement with crystal- transfusing RBCs if it fell below 70 g/l) was at least as effec-
loid or colloid to maintain normovolaemia, aiming for a tive as a liberal strategy (maintaining haemoglobin con-
haematocrit of 2030 per cent. The aim is twofold: to centration at 100120 g/l, transfusing RBCs if it fell below
dilute circulating RBCs and plasma components, reducing 100 g/l) in critically ill patients, although those with acute
the amounts lost during surgical bleeding; and to provide myocardial infarction and unstable angina were excluded
fresh whole blood for retransfusion at the end of surgery, from the study.
providing RBCs, clotting factors and platelets to main- In the 15 years since that work, further studies have
tain haemostasis and oxygen delivery. A meta-analysis64 of supported these findings and clinical practice has moved
this technique concluded that there are only modest ben- inexorably towards a less liberal transfusion strategy. A
efits from this technique and did not support its adoption, restrictive threshold of less than 80 g/l after hip fracture
although it may be more cost-effective than cell salvage59 . surgery was compared with a liberal threshold of 100 g/l
in patients with a history or risk factors for cardiovascular
disease. The primary outcome was death or inability to
Postoperative measures
walk across a room without human assistance at 60-day
Efforts should continue to minimize blood loss in the post- follow-up. The liberal transfusion strategy did not reduce
operative period. The same basic measures to avoid coag- mortality rates or functional capacity in these patients68 .
ulopathy should be employed. Blood loss into drains is an In a long-term follow-up of this cohort, mortality did
area of interest. In orthopaedic surgery, the use of drains not differ significantly between the restrictive and liberal
has been shown to increase blood transfusion rates65 . In transfusion groups69 .
keeping with many enhanced recovery programmes, post- In a Cochrane review70 of over 6000 patients it was
operative surgical drain use is decreasing. Cell salvage can concluded that restrictive transfusion thresholds (where
also be used after operation60 , with retransfusion of blood the mean difference in postoperative haemoglobin con-
from drains, particularly in major orthopaedic surgery. centration was 148 (95 per cent c.i. 192 to 103) g/l
As well as blood lost during surgery, the inflammatory lower than in the liberal transfusion group) should be sup-
and stress response to surgery can reduce erythropoiesis ported for most patients, including those with pre-existing
2015 BJS Society Ltd www.bjs.co.uk BJS 2015; 102: 13251337
Published by John Wiley & Sons Ltd
Patient blood management 1333
Table 3 Important studies of transfusion thresholds
Haemoglobin (g/l)
Restrictive Liberal
Reference strategy strategy Population Outcome
Hbert et al.67 70 100 Critically ill patients Restrictive strategy as safe as a liberal
Transfusion Requirements In Critical Care strategy, except perhaps in patients
(TRICC) trial (1999) with ischaemic heart disease
Carson et al.68 80 100 Patients with high risk or history of Liberal transfusion strategy not
Functional Outcomes in Cardiovascular cardiovascular disease after hip superior in terms of morbidity or
Patients Undergoing Surgical Hip fracture surgery mortality
Fracture Repair (FOCUS) trial (2011)
Villanueva et al.71 70 90 Severe acute upper Significantly improved outcomes in
(2013) gastrointestinal bleeding restrictive group, including mortality
Holst et al.73 70 90 Patients with septic shock in Restrictive group had similar mortality
Transfusion Requirements In Septic intensive care and ischaemic event rates
Shock (TRISS) trial (2014)
Murphy et al.72 75 90 Non-emergency cardiac surgery Restrictive strategy not superior;
Transfusion Indication Threshold increased death rate in restrictive
Reduction (TITRe2) trial (2015) group
cardiovascular disease. Indeed, restrictive transfusion Thus, a transfusion threshold of 70 g/l can be recom-
strategies were associated with a statistically significant mended; however, a threshold of 90 g/l should be con-
reduction in hospital mortality (RR 077, 95 per cent c.i. sidered in patients with ischaemic heart disease or those
062 to 095), but not 30-day mortality (RR 085, 070 to undergoing cardiac surgery. It should be noted that both
103). The authors recommend that, in patients who do these thresholds are restrictive in comparison with histori-
not have acute coronary artery disease, blood transfusion cal practice (Table 3).
can probably be withheld in the presence of haemoglobin
levels as low as 7080 g/l as long as there is no notable
bleeding70 . Similar findings were made in upper gastro-
Single-unit transfusions
intestinal bleeding where a restrictive transfusion strategy Single-unit transfusions are strongly recommended in
increased the 6-week survival probability (95 versus 91 per stable patients without bleeding, whereby each unit trans-
cent; HR for death with restrictive transfusion 055, 95 fused is an independent clinical decision, documented in the
per cent c.i. 033 to 092; P = 002)71 . In cardiac surgery, patient notes, with the patient reassessed after each trans-
however, the recently published TITRe2 (Transfusion fusion and the incremental haemoglobin concentration
Indication Threshold Reduction) trial72 demonstrated noted. Such policies encourage decision-making regarding
uncertainty of restrictive strategies in unstable cardiac the appropriateness of transfusion and haemoglobin tar-
patients, reporting a beneficial impact of liberal trans- get. A policy of transfusing RBCs in single-unit aliquots
fusion to a haemoglobin concentration of more than 90 g/l improves RBC utilization and decreases patient exposure
on mortality following cardiac surgery (42 versus 26 per to allogeneic blood74 . Adopting such a practice is good
cent in restrictive versus liberal group; HR 164, 95 per evidence-based medicine, but it will require significant
cent c.i. 100 to 267; P = 0045). Interestingly, in a similar educational programmes to overcome the provider and
study73 of critically ill patients with septic shock, a restric- system barriers to changing entrenched practice75 .
tive transfusion threshold of 70 compared with 90 g/l led
to similar numbers of ischaemic events, severe adverse
Maintaining tissue oxygen delivery
events and requirement for life support. The RR of death
in the lower-threshold group was 094 (95 per cent c.i. Tissue oxygen delivery is greatly influenced by haemo-
078 to 109; P = 044). In the TITRe2 study72 concurrent globin concentration. Physiologically the body responds
infection was common (more than 25 per cent in both to a reduced haemoglobin and blood oxygen content
groups). Based on these recent results, it would seem that by sensing oxygen levels at a cellular level, via vascular
the mechanism of the intervention by blood transfusion in chemoreceptors and in hypoxia-sensitive organs76 . The
these settings may be different and not related only to the body responds to anaemia by increasing cardiac out-
change in haemoglobin mass. put, vasodilatation, increasing minute ventilation, and
2015 BJS Society Ltd www.bjs.co.uk BJS 2015; 102: 13251337
Published by John Wiley & Sons Ltd
1334 B. Clevenger, S. V. Mallett, A. A. Klein and T. Richards
Table 4 Surgical patient blood management checklist
Sign in (before induction of anaesthesia)
Preoperative haemoglobin within normal range
Consideration of withholding antiplatelet and anticoagulant medication
Consideration of minimally invasive or laparoscopic technique
Point-of-care testing available
Time out (before surgical excision)
Careful patient positioning to maintain venous drainage
Patient warming > 36 C
Use cell salvage whenever blood loss > 500 ml is possible; set up collection reservoir and process if sufficient blood actually collected
Tranexamic acid 1 g to all patients undergoing surgery where blood loss is likely or possible
Availability of prothrombin complex concentrates and fibrinogen concentrates; use of topical haemostatic agents
Sign out (before patient leaves operating room)
Restrictive transfusion thresholds implemented (haemoglobin 7080 g/l depending on patient characteristics and haemodynamics)
Maintain oxygen delivery, targeting oxygen saturation levels > 95 per cent
Single-unit blood transfusion policy; reassessing haemoglobin level and clinical need between units
Postoperative drain or cell salvage
optimizing the oxygen saturation of haemoglobin in the and decisions relating to anaemia and blood transfusion,
lung and its extraction at the tissues. but more importantly represent a paradigm shift towards
Increasing oxygen delivery and reducing oxygen demand a more considered approach to blood transfusion, acknow-
can meet the balance needed to compensate for lower ledging its risks, preventatives and alternatives.
haemoglobin concentrations secondary to blood loss The arguments for making this change are broad. They
and dilution. This can be achieved by increasing the are both ethical and evidence-based. Failure to treat newly
arterial oxygen content of blood by increasing the frac- diagnosed anaemia is unacceptable, and clinicians must
tion of inspired oxygen, which increases the amount of recognize the risks of transfusion, and convey this to their
haemoglobin-bound oxygen and also the concentration patients. They are economic owing to the increasing cost
of oxygen dissolved in the blood. Cardiovascular function of transfusion and its related resource implications, and
can be optimized by the use of vasopressors such as nor- the scarcity of supply, as demand outstrips donation. The
adrenaline (norepinephrine) to maintain organ perfusion, ethics of using this precious resource in the most appro-
including coronary perfusion pressure, in the face of com- priate manner, as desired by donors, must be considered.
pensatory vasodilatation secondary to acute anaemia77 . The legal ramifications of adverse events, including
Consideration should be given to the adverse effects of transfusion-transmitted infection of pathogens, both
postoperative pain and infection on tissue oxygen deliv- known and unknown (such as variant CreutzfeldtJacob
ery and increased demand, with prevention and prompt disease), must also be considered.
treatment. PBM should become a routine part of surgical practice
to reduce risk and improve outcomes in the same way
as safer surgical checklists have been employed (Table 4).
Conclusion
Its implementation is likely to become a target of service
PBM presents an opportunity to ameliorate a recognized commissioners attempting to improve performance and
surgical risk and improve patient outcomes. Its imple- patient safety, while increasing efficiency and reducing
mentation within the NHS has now been recognized as costs.
necessary for patient and economic benefit, as demon-
strated by the introduction of new NHS-led national Acknowledgements
recommendations. Traditional practice has been to main-
tain a haemoglobin concentration or haematocrit based on T.R. is chief investigator for a National Institute for Health
arbitrary values (for example, less than 100 g/l or haema- Research Health Technology Assessment multicentre trial,
tocrit 30 per cent, the so-called 10/30 rule) established in PREVENTT (preoperative intravenous iron to treat
the 1940s. The decision to transfuse blood should not be anaemia in major surgery). University College London has
a reflex reaction to a defined haemoglobin concentration received educational grant funding from Vifor Pharma,
or haematocrit, as it often was in the past, but a consid- and also fees from Vifor Pharma and Pharmocosmos.
ered riskbenefit decision taken on an individual patient Papworth Hospital has received an educational grant from
basis. The pillars of PBM help structure the interventions CSL Behring and Brightwake.
2015 BJS Society Ltd www.bjs.co.uk BJS 2015; 102: 13251337
Published by John Wiley & Sons Ltd
Patient blood management 1335
Disclosure: The authors declare no other conflict of interest. http://www.transfusionguidelines.org.uk/transfusion-
handbook [accessed 1 October 2014].
14 Lacroix J, Hbert PC, Fergusson DA, Tinmouth A, Cook
References
DJ, Marshall JC et al. Age of transfused blood in critically ill
1 Musallam KM, Tamim HM, Richards T, Spahn DR, adults. N Engl J Med 2015; 372: 14101418.
Rosendaal FR, Habbal A et al. Preoperative anaemia and 15 Kaukonen KM, Bailey M, Ady B, Aubron C, French C,
postoperative outcomes in non-cardiac surgery: a Gantner D et al. A randomised controlled trial of standard
retrospective cohort study. Lancet 2011; 378: 13961407. transfusion versus fresher red blood cell use in intensive care
2 Ferraris VA, Davenport DL, Saha SP, Austin PC, (TRANSFUSE): protocol and statistical analysis plan. Crit
Zwischenberger JB. Surgical outcomes and transfusion of Care Resusc 2014; 16: 255261.
minimal amounts of blood in the operating room. Arch Surg 16 Acheson AG, Brookes MJ, Spahn DR. Effects of allogeneic
2012; 147: 4955. red blood cell transfusions on clinical outcomes in patients
3 Hofmann A, Farmer S, Shander A. Five drivers shifting the undergoing colorectal cancer surgery. Ann Surg 2012; 256:
paradigm from product-focused transfusion practice to 235244.
patient blood management. Oncologist 2011; 16: 311. 17 Bolton-Maggs PHB (ed.), Poles D, Watt A, Thomas D,
4 Spahn DR, Theusinger OM, Hofmann A. Patient blood Cohen H; Serious Hazards of Transfusion (SHOT) Steering
management is a winwin: a wake-up call. Br J Anaesth Group. Annual SHOT Report 2012; 2013. http://www.shotuk.
2012; 108: 889892. org/wp-content/uploads/2013/08/SHOT-Annual-Report-
5 Tobler LH, Busch MP. History of posttransfusion hepatitis. 2012.pdf [accessed 1 October 2014].
Clin Chem 1997; 43: 14871493. 18 Shander A, Knight K, Thurer R, Adamson J, Spence R.
6 World Health Organization. Availability, safety and quality Prevalence and outcomes of anemia in surgery: a systematic
of blood products. Report by the Secretariat. Agenda item review of the literature. Am J Med 2004; 116: 58S69S.
11.17. Sixty-third World Health Assembly WHA63/20. WHO: 19 Geisel T, Martin J, Schulze B, Schaefer R, Bach M, Virgin
Geneva, 2010; 25. G et al. An etiologic profile of anemia in 405 geriatric
7 Shander A, Van Aken H, Colomina MJ, Gombotz H, patients. Anemia 2014; 2014: 932486.
Hofmann A, Krauspe R et al. Patient blood management in 20 Hung M, Besser M, Sharples LD, Nair SK, Klein AA. The
Europe. Br J Anaesth 2012; 109: 5568. prevalence and association with transfusion, intensive care
8 JPAC Joint United Kingdom (UK) Blood Transfusion and unit stay and mortality of pre-operative anaemia in a cohort
Tissue Transplantation Services Professional Advisory of cardiac surgery patients. Anaesthesia 2011; 66: 812818.
Committee. Patient Blood Management; 2014. http://www. 21 Murphy GJ, Reeves BC, Rogers CA, Rizvi SI, Culliford L,
transfusionguidelines.org.uk/uk-transfusion-committees/ Angelini GD. Increased mortality, postoperative morbidity,
national-blood-transfusion-committee/patient-blood- and cost after red blood cell transfusion in patients having
management [accessed 1 October 2014]. cardiac surgery. Circulation 2007; 116: 25442552.
9 Hofmann A, Ozawa S, Farrugia A, Farmer SL, Shander A. 22 Dunne JR, Malone D, Tracy JK, Gannon C, Napolitano
Economic considerations on transfusion medicine and LM. Perioperative anemia: an independent risk factor for
patient blood management. Best Pract Res Clin Anaesthesiol infection, mortality, and resource utilization in surgery.
2013; 27: 5968. J Surg Res 2002; 102: 237244.
10 Lasocki S, Krauspe R, von Heymann C, Mezzacasa A, 23 Beattie WS, Karkouti K, Wijeysundera DN, Tait G. Risk
Chainey S, Spahn DR. PREPARE: the prevalence of associated with preoperative anemia in noncardiac surgery: a
perioperative anaemia and need for patient blood single-center cohort study. Anesthesiology 2009; 110:
management in elective orthopaedic surgery. A multicentre 574581.
observational study. Eur J Anaesthesiol 2015; 32: 160167. 24 Lin DM, Lin ES, Tran MH. Efficacy and safety of
11 Glance LG, Dick AW, Mukamel DB, Fleming FJ, Zollo RA, erythropoietin and intravenous iron in perioperative blood
Wissler R et al. Association between intraoperative blood management: a systematic review. Transfus Med Rev 2013;
transfusion and mortality and morbidity in patients 27: 221234.
undergoing noncardiac surgery. Anesthesiology 2011; 114: 25 Wu WC, Schifftner TL, Henderson WG, Eaton CB, Poses
283292. RM, Uttley G et al. Preoperative hematocrit levels and
12 Bernard AC, Davenport DL, Chang PK, Vaughan TB, postoperative outcomes in older patients undergoing
Zwischenberger JB. Intraoperative transfusion of 1 U to 2 U noncardiac surgery. JAMA 2007; 297: 24812488.
packed red blood cells is associated with increased 30-day 26 Leichtle SW, Mouawad NJ, Lampman R, Singal B, Cleary
mortality, surgical-site infection, pneumonia, and sepsis in RK. Does preoperative anemia adversely affect colon and
general surgery patients. J Am Coll Surg 2009; 208: rectal surgery outcomes? J Am Coll Surg 2011; 212:
931937. 187194.
13 JPAC Joint United Kingdom (UK) Blood Transfusion and 27 Baron DM, Hochrieser H, Posch M, Metnitz B, Rhodes A,
Tissue Transplantation Services Professional Advisory Moreno RP et al.; European Surgical Outcomes Study
Committee. Transfusion Handbook 5th Edition: January 2014. (EuSOS) group for Trials Groups of European Society of
2015 BJS Society Ltd www.bjs.co.uk BJS 2015; 102: 13251337
Published by John Wiley & Sons Ltd
1336 B. Clevenger, S. V. Mallett, A. A. Klein and T. Richards
Intensive Care Medicine; European Society of Peri-Operative Transfusion (ISPOT) Investigators. Transfus
Anaesthesiology. Preoperative anaemia is associated with Med 1998; 8: 309317.
poor clinical outcome in non-cardiac surgery patients. Br J 41 Alghamdi AA, Albanna MJ, Guru V, Brister SJ. Does the use
Anaesth 2014; 113: 416423. of erythropoietin reduce the risk of exposure to allogeneic
28 Goodnough LT, Maniatis A, Earnshaw P, Benoni G, Beris blood transfusion in cardiac surgery? A systematic review
P, Bisbe E et al. Detection, evaluation, and management of and meta-analysis. J Cardiac Surgery 2006; 21: 320326.
preoperative anaemia in the elective orthopaedic surgical 42 Rineau E, Chaudet A, Carlier L, Bizot P, Lasocki S. Ferric
patient: NATA guidelines. Br J Anaesth 2010; 106: 1322. carboxymaltose increases epoetin- response and prevents
29 Kozek-Langenecker SA, Afshari A, Albaladejo P, Santullano iron deficiency before elective orthopaedic surgery. Br J
CA, De Robertis E, Filipescu DC et al. Management of Anaesth 2014; 113: 296298.
severe perioperative bleeding: guidelines from the European 43 Unger EF, Thompson AM, Blank MJ, Temple R.
Society of Anaesthesiology. Eur J Anaesthesiol 2013; 30: Erythropoiesis-stimulating agents time for a reevaluation.
270382. N Engl J Med 2010; 362: 189192.
30 Busti F, Campostrini N, Martinelli N, Girelli D. Iron 44 Pascual M, Bohle B, Alonso S, Mayol X, Salvans S, Grande
deficiency in the elderly population, revisited in the hepcidin L et al. Preoperative administration of erythropoietin
era. Front Pharmacol 2014; 5: 83. stimulates tumor recurrence after surgical excision of colon
31 Hung M, Ortmann E, Besser M, Martin-Cabrera P, cancer in mice by a vascular endothelial growth factor.
Richards T, Ghosh M et al. A prospective observational J Surg Res 2013; 183: 270277.
cohort study to identify the causes of anaemia and 45 Kasivisvanathan R, Abbassi-Ghadi N, Kumar S, Mackenzie
association with outcome in cardiac surgical patients. Heart H, Thompson K, James K et al. Risk of bleeding and adverse
2015; 101: 107112. outcomes predicted by thromboelastography platelet
mapping in patients taking clopidogrel within 7 days of
32 Clevenger B, Richards T. Preoperative anaemia. Anaesthesia
non-cardiac surgery. Br J Surg 2014; 101: 13831390.
2015; 70(Suppl 1): 2028, e6e8.
46 Gill R. Practical management of major blood loss.
33 Goddard AF, James MW, McIntyre AS, Scott BB; British
Anaesthesia 2015; 70(Suppl 1): 5457, e19e20.
Society of Gastroenterology. Guidelines for the
47 Mallett SV, Armstrong M. Point-of-care monitoring of
management of iron deficiency anaemia. Gut 2011; 60:
haemostasis. Anaesthesia 2015; 70(Suppl 1): 7377, e25e26.
13091316.
48 Schchl H, Voelckel W, Schlimp CJ. Management of
34 Meybohm P, Fischer DP, Geisen C, Mller MM, Weber
traumatic haemorrhage the European perspective.
CF, Herrmann E et al. German PBM Study Core Group.
Anaesthesia 2015; 70(Suppl 1): 102107, e35e37.
Safety and effectiveness of a patient blood management
49 Richman JM, Rowlingson AJ, Maine DN, Courpas GE,
(PBM) program in surgical patients the study design for a
Weller JF, Wu CL. Does neuraxial anesthesia reduce
multi-centre prospective epidemiologic non-inferiority trial.
intraoperative blood loss? A meta-analysis. J Clin Anesth
BMC Health Serv Res 2014; 14: 576.
2006; 18: 427435.
35 Gurusamy KS, Nagendran M, Broadhurst JF, Anker SD, 50 Rajagopalan S, Mascha E, Na J, Sessler DI. The effects of
Richards T. Iron therapy in anaemic adults without chronic mild perioperative hypothermia on blood loss and
kidney disease. Cochrane Database Syst Rev 2014; transfusion requirement. Anesthesiology 2008; 108: 7177.
(12)CD010640. 51 Henry DA, Carless PA, Moxey AJ, OConnell D, Stokes BJ,
36 Tolkien Z, Stecher L, Mander AP, Pereira DIA, Powell JJ. Fergusson DA et al. Anti-fibrinolytic use for minimising
Ferrous sulfate supplementation causes significant perioperative allogeneic blood transfusion. Cochrane Database
gastrointestinal side-effects in adults: a systematic review Syst Rev 2011; (3)CD001886.
and meta-analysis. PLoS One 2015; 10: e0117383. 52 Ortmann E, Besser MW, Klein AA. Antifibrinolytic agents
37 Auerbach M, Goodnough LT, Shander A. Iron: the new in current anaesthetic practice. Br J Anaesth 2013; 111:
advances in therapy. Best Pract Res Clin Anaesthesiol 2013; 27: 549563.
131140. 53 Ker K, Prieto-Merino D, Roberts I. Systematic review,
38 Litton E, Xiao J, Ho KM. Safety and efficacy of intravenous meta-analysis and meta-regression of the effect of
iron therapy in reducing requirement for allogeneic blood tranexamic acid on surgical blood loss. Br J Surg 2013; 100:
transfusion: systematic review and meta-analysis of 12711279.
randomised clinical trials. BMJ 2013; 347: f4822. 54 CRASH-2 trial collaborators, Shakur H, Roberts I, Bautista
39 Devon KM, McLeod RS. Pre and peri-operative R, Caballero J, Coats T et al. Effects of tranexamic acid on
erythropoietin for reducing allogeneic blood transfusions in death, vascular occlusive events, and blood transfusion in
colorectal cancer surgery. Cochrane Database Syst Rev 2009; trauma patients with significant haemorrhage (CRASH-2): a
(1)CD007148. randomised, placebo-controlled trial. Lancet 2010; 376:
40 Laupacis A, Fergusson D. Erythropoietin to minimize 2332.
perioperative blood transfusion: a systematic review of 55 Fergusson DA, Hbert PC, Mazer CD, Fremes S,
randomized trials. The International Study of MacAdams C, Murkin JM et al.; BART Investigators. A
2015 BJS Society Ltd www.bjs.co.uk BJS 2015; 102: 13251337
Published by John Wiley & Sons Ltd
Patient blood management 1337
comparison of aprotinin and lysine analogues in high-risk Transfusion Requirements in Critical Care Investigators,
cardiac surgery. N Engl J Med 2008; 358: 23192331. Canadian Critical Care Trials Group. N Engl J Med 1999;
56 McMullan V, Alston RP III. Aprotinin and cardiac surgery: 340: 409417.
a sorry tale of evidence misused. Br J Anaesth 2013; 110: 68 Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman
675678. BR, Rhoads GG et al. Liberal or restrictive transfusion in
57 Carless PA, Henry DA, Anthony DM. Fibrin sealant use for high-risk patients after hip surgery. N Engl J Med 2011; 365:
minimising peri-operative allogeneic blood transfusion. 24532462.
Cochrane Database Syst Rev 2013; (2)CD004171. 69 Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman
58 Ker K, Beecher D, Roberts I. Topical application of BR, Rhoads GG et al. Liberal versus restrictive blood
tranexamic acid for the reduction of bleeding. Cochrane transfusion strategy: 3-year survival and cause of death
Database Syst Rev 2013; (7)CD010562. results from the FOCUS randomised controlled trial. Lancet
59 Davies L, Brown TJ, Haynes S, Payne K, Elliott RA, 2015; 385: 11831189.
McCollum C. Cost-effectiveness of cell salvage and 70 Carson JL, Carless PA, Hbert PC. Transfusion
alternative methods of minimising perioperative allogeneic thresholds and other strategies for guiding allogeneic red
blood transfusion: a systematic review and economic model. blood cell transfusion. Cochrane Database Syst Rev 2012;
Health Technol Assess 2006; 10: 1210. (4)CD002042.
60 Ashworth A, Klein AA. Cell salvage as part of a blood 71 Villanueva C, Colomo A, Bosch A, Concepcin M,
conservation strategy in anaesthesia. Br J Anaesth 2010; 105: Hernandez-Gea V, Aracil C et al. Transfusion strategies for
401416. acute upper gastrointestinal bleeding. N Engl J Med 2013;
61 Carless PA, Henry DA, Moxey AJ, OConnell D, Brown T, 368: 1121.
Fergusson DA. Cell salvage for minimising perioperative 72 Murphy GJ, Pike K, Rogers CA, Wordsworth S, Stokes EA,
allogeneic blood transfusion. Cochrane Database Syst Rev Angelini GD et al.; TITRe2 Investigators. Liberal or
2010; (4)CD001888. restrictive transfusion after cardiac surgery. N Engl J Med
62 Feltracco P, Michieletto E, Barbieri S, Serra E, Rizzi S, 2015; 372: 9971008.
Salvaterra F et al. Microbiologic contamination of 73 Holst LB, Haase N, Wetterslev J, Wernerman J,
intraoperative blood salvaged during liver transplantation. Guttormsen AB, Karlsson S et al.; TRISS Trial Group;
Transplant Proc 2007; 39: 18891891. Scandinavian Critical Care Trials Group. Lower versus
63 Bowley DM, Barker P, Boffard KD. Intraoperative blood higher hemoglobin threshold for transfusion in septic shock.
salvage in penetrating abdominal trauma: a randomized, N Engl J Med 2014; 371: 13811391.
controlled trial. World J Surg 2006; 30: 10741080. 74 Ma M, Eckert K, Ralley F, Chin-Yee I. A retrospective study
64 Segal JB, Blasco Colmenares E, Norris EJ, evaluating single-unit red blood cell transfusions in reducing
Guallar E. Preoperative acute normovolemic allogeneic blood exposure. Transfusion Med 2005; 15:
hemodilution: a meta-analysis. Transfusion 2004; 44: 307312.
632644. 75 Murphy DJ, Pronovost PJ, Lehmann CU, Gurses AP,
65 Parker MJ, Roberts CP, Hay D. Closed suction drainage for Whitman GJR, Needham DM et al. Red blood cell
hip and knee arthroplasty. A meta-analysis. J Bone Joint Surg transfusion practices in two surgical intensive care units: a
Am 2004; 86-A: 11461152. mixed methods assessment of barriers to evidence-based
66 Bisbe E, Molt L, Arroyo R, Muniesa JM, Tejero M. practice. Transfusion 2014; 54: 26582667.
Randomized trial comparing ferric carboxymaltose 76 Hare GMT, Tsui AK, Ozawa S, Shander A. Anaemia: can
versus oral ferrous glycine sulphate for postoperative we define haemoglobin thresholds for impaired oxygen
anaemia after total knee arthroplasty. Br J Anaesth 2014; homeostasis and suggest new strategies for treatment? Best
113: 402409. Pract Res Clin Anaesthesiol 2013; 27: 8598.
67 Hbert PC, Wells G, Blajchman MA, Marshall J, Martin C, 77 Meier J, Gombotz H. Pillar III optimisation of
Pagliarello G et al. A multicenter, randomized, controlled anaemia tolerance. Best Pract Res Clin Anaesthesiol 2013; 27:
clinical trial of transfusion requirements in critical care. 111119.
2015 BJS Society Ltd www.bjs.co.uk BJS 2015; 102: 13251337
Published by John Wiley & Sons Ltd
Das könnte Ihnen auch gefallen
- Risk Factors of Osteoarthritis Knee - A Cross-Sectional StudyDokument3 SeitenRisk Factors of Osteoarthritis Knee - A Cross-Sectional StudyElias Oktovianus HaulussyNoch keine Bewertungen
- The Annals of Otology, Rhinology & Laryngology Jan 2002 111, 1Dokument1 SeiteThe Annals of Otology, Rhinology & Laryngology Jan 2002 111, 1Elias Oktovianus HaulussyNoch keine Bewertungen
- AIS Learning Hearing AidsDokument2 SeitenAIS Learning Hearing AidsElias Oktovianus HaulussyNoch keine Bewertungen
- Unusual Cause of Shoulder PainDokument3 SeitenUnusual Cause of Shoulder PainElias Oktovianus HaulussyNoch keine Bewertungen
- The Different Types of Human Prion Disease (Including CJD)Dokument4 SeitenThe Different Types of Human Prion Disease (Including CJD)Elias Oktovianus HaulussyNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Detail Design Drawings: OCTOBER., 2017 Date Span Carriage WayDokument26 SeitenDetail Design Drawings: OCTOBER., 2017 Date Span Carriage WayManvendra NigamNoch keine Bewertungen
- Diogenes Laertius-Book 10 - Epicurus - Tomado de Lives of The Eminent Philosophers (Oxford, 2018) PDFDokument54 SeitenDiogenes Laertius-Book 10 - Epicurus - Tomado de Lives of The Eminent Philosophers (Oxford, 2018) PDFAndres Felipe Pineda JaimesNoch keine Bewertungen
- Nutridiet-Enteral and Parenteral FeedingDokument3 SeitenNutridiet-Enteral and Parenteral FeedingBSN 1-N CASTRO, RicciNoch keine Bewertungen
- A Content Analysis of SeabankDokument13 SeitenA Content Analysis of SeabankMarielet Dela PazNoch keine Bewertungen
- Dry Compressing Vacuum PumpsDokument62 SeitenDry Compressing Vacuum PumpsAnonymous zwSP5gvNoch keine Bewertungen
- Applying For A Job: Pre-ReadingDokument5 SeitenApplying For A Job: Pre-ReadingDianitta MaciasNoch keine Bewertungen
- 19 Dark PPT TemplateDokument15 Seiten19 Dark PPT TemplateKurt W. DelleraNoch keine Bewertungen
- NHD Process PaperDokument2 SeitenNHD Process Paperapi-203024952100% (1)
- Yetta Company ProfileDokument6 SeitenYetta Company ProfileAfizi GhazaliNoch keine Bewertungen
- SDSSSSDDokument1 SeiteSDSSSSDmirfanjpcgmailcomNoch keine Bewertungen
- Common Core Content and Training Objectives For Basic AIS Training - Phase 2 - SpecialistDokument82 SeitenCommon Core Content and Training Objectives For Basic AIS Training - Phase 2 - SpecialistjlferreiraNoch keine Bewertungen
- RCA LCD26V6SY Service Manual 1.0 PDFDokument33 SeitenRCA LCD26V6SY Service Manual 1.0 PDFPocho Pochito100% (1)
- PD3 - Strategic Supply Chain Management: Exam Exemplar QuestionsDokument20 SeitenPD3 - Strategic Supply Chain Management: Exam Exemplar QuestionsHazel Jael HernandezNoch keine Bewertungen
- CATaclysm Preview ReleaseDokument52 SeitenCATaclysm Preview ReleaseGhaderalNoch keine Bewertungen
- Img 20150510 0001Dokument2 SeitenImg 20150510 0001api-284663984Noch keine Bewertungen
- HUMSS - Introduction To World Religions & Belief Systems CGDokument13 SeitenHUMSS - Introduction To World Religions & Belief Systems CGAliuqus SirJasper89% (18)
- Biotech NewsDokument116 SeitenBiotech NewsRahul KapoorNoch keine Bewertungen
- 2201 IntGCSE (9-1) Subject Grade Boundaries V1Dokument4 Seiten2201 IntGCSE (9-1) Subject Grade Boundaries V1Fariha RahmanNoch keine Bewertungen
- Lady in The House, Her Responsibilities & Ambitions: Amrita DuhanDokument7 SeitenLady in The House, Her Responsibilities & Ambitions: Amrita DuhanFitness FableNoch keine Bewertungen
- Maths Formulas For IGCSEDokument2 SeitenMaths Formulas For IGCSEHikma100% (1)
- Perdarahan Uterus AbnormalDokument15 SeitenPerdarahan Uterus Abnormalarfiah100% (1)
- Hele Grade4Dokument56 SeitenHele Grade4Chard Gonzales100% (3)
- MFE Module 1 .Dokument15 SeitenMFE Module 1 .Adarsh KNoch keine Bewertungen
- Dating Apps MDokument2 SeitenDating Apps Mtuanhmt040604Noch keine Bewertungen
- OM CommandCenter OI SEP09 enDokument30 SeitenOM CommandCenter OI SEP09 enGabriely MuriloNoch keine Bewertungen
- RARE Manual For Training Local Nature GuidesDokument91 SeitenRARE Manual For Training Local Nature GuidesenoshaugustineNoch keine Bewertungen
- Manuel SYL233 700 EDokument2 SeitenManuel SYL233 700 ESiddiqui SarfarazNoch keine Bewertungen
- VimDokument258 SeitenVimMichael BarsonNoch keine Bewertungen
- Lightning Arrester Lightningcontroller MC 125-B/Npe: Operation and Fields of ApplicationDokument2 SeitenLightning Arrester Lightningcontroller MC 125-B/Npe: Operation and Fields of ApplicationAnas BasarahNoch keine Bewertungen
- Design of Reinforced Cement Concrete ElementsDokument14 SeitenDesign of Reinforced Cement Concrete ElementsSudeesh M SNoch keine Bewertungen