Beruflich Dokumente
Kultur Dokumente
Basal Ganglia Circuits As Targets For Neuromodulation in Parkinson Disease
Hochgeladen von
Sebastián GallegosOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Basal Ganglia Circuits As Targets For Neuromodulation in Parkinson Disease
Hochgeladen von
Sebastián GallegosCopyright:
Verfügbare Formate
Clinical Review & Education
Review | CIRCUITS AND CIRCUIT DISORDERS
Basal Ganglia Circuits as Targets for Neuromodulation
in Parkinson Disease
Mahlon R. DeLong, MD; Thomas Wichmann, MD
IMPORTANCE The revival of stereotactic surgery for Parkinson disease (PD) in the 1990s, with
pallidotomy and then with high-frequency deep brain stimulation (DBS), has led to a
renaissance in functional surgery for movement and other neuropsychiatric disorders.
OBJECTIVE To examine the scientific foundations and rationale for the use of ablation and
DBS for treatment of neurologic and psychiatric diseases, using PD as the primary example.
EVIDENCE REVIEW A summary of the large body of relevant literature is presented on
anatomy, physiology, pathophysiology, and functional surgery for PD and other basal ganglia
disorders.
FINDINGS The signs and symptoms of movement disorders appear to result largely from
signature abnormalities in one of several parallel and largely segregated basal ganglia
thalamocortical circuits (ie, the motor circuit). The available evidence suggests that the varied
movement disorders resulting from dysfunction of this circuit result from propagated
disruption of downstream network activity in the thalamus, cortex, and brainstem. Ablation
and DBS act to free downstream networks to function more normally. The basal ganglia
thalamocortical circuit may play a key role in the expression of disordered movement, and the
basal gangliabrainstem projections may play roles in akinesia and disturbances of gait.
Efforts are under way to target circuit dysfunction in brain areas outside of the traditionally
Author Affiliations: Department of
implicated basal ganglia thalamocortical system, in particular, the pedunculopontine nucleus, Neurology, School of Medicine,
to address gait disorders that respond poorly to levodopa and conventional DBS targets. Emory University, Atlanta, Georgia
(DeLong, Wichmann); Yerkes
National Primate Research Center,
CONCLUSIONS AND RELEVANCE Deep brain stimulation is now the treatment of choice for
Emory University, Atlanta, Georgia
many patients with advanced PD and other movement disorders. The success of DBS and (Wichmann).
other forms of neuromodulation for neuropsychiatric disorders is the result of the ability to Corresponding Author: Mahlon R.
modulate circuit activity in discrete functional domains within the basal ganglia circuitry with DeLong, MD, Department of
highly focused interventions, which spare uninvolved areas that are often disrupted with Neurology, School of Medicine,
Emory University, 101 Woodruff
drugs.
Circle, Ste 6000, Woodruff Memorial
Research Bldg, Atlanta, GA 30322
JAMA Neurol. doi:10.1001/jamaneurol.2015.2397 (medmrd@emory.edu).
Published online September 26, 2015. Section Editor: David E. Pleasure,
MD.
T
he 1950s and 1960s were a remarkable era for ablative ste- phenyl-1,2,3,6-tetrahydropyridine (MPTP) primate model of PD.1,2
reotactic surgery for movement disorders and followed the Although these results demonstrated the value of targeted surgi-
earlier development of the stereotactic frame and meth- cal interventions in the treatment of PD and identified the STN as a
ods of targeting of the basal ganglia and thalamus for treatment of potential new target, lesioning of the STN was initially believed to
Parkinson disease (PD), dystonia, and tremor. This era came to an be too risky for humans. Surgeons, also motivated by the report of
end in the early 1970s after the introduction of levodopa for the treat- Laitinen et al3 on the significant benefits of pallidotomy for both par-
ment of PD in the mid-1960s and the negative public response to kinsonism and levodopa motor compilations and using the postero-
the excesses of psychosurgery in that period. However, the use of ventral target of the internal pallidum (GPi) of Leksell, returned to
stereotactic surgery returned in the early 1990s. Functional sur- pallidotomy.
gery is once again a standard treatment for movement disorders. Toward the end of the 1980s, Benabid et al4 made the impor-
Critical for the revival of the procedure was the growing understand- tant discovery that electrical high-frequency stimulation (deep brain
ing of the functional organization of the basal ganglia circuitry and stimulation [DBS]) of the thalamus is as effective as thalamotomy
the pathophysiology of movement disorders (specifically parkin- for the treatment of essential tremor. Soon thereafter, the use of DBS
sonism), as well as the demonstration of the reversal of parkinson- at the newly identified STN target for PD was explored. Studies found
ism by lesioning the subthalamic nucleus (STN) in the 1-methyl-4- STN DBS to be a highly effective antiparkinsonian treatment, both
jamaneurology.com (Reprinted) JAMA Neurology Published online September 26, 2015 E1
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://archneur.jamanetwork.com/ by a Central Michigan University User on 09/27/2015
Clinical Review & Education Review Basal Ganglia Circuits as Targets for Neuromodulation in Parkinson Disease
in the primate model of PD5 and in humans with PD.6 Since that time,
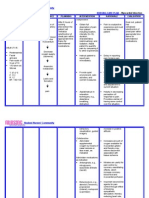
Figure 1. Anatomy of CortexBasal GangliaThalamocortical Circuits
the use of STN DBS has become the standard of care for patients with
advanced PD, in particular those who experience drug-induced com- Motor Oculomotor Prefrontal Limbic
plications or treatment-resistant tremor. Following the success of
STN DBS for PD, DBS has also been used successfully in patients with SMA, PMC FEF DLPFC MOFC
Cortex
CMA, M1 SEF LOFC ACA
dystonia as a primary disorder and with dystonia as a manifesta-
tion of PD, targeting primarily the GPi.7,8 Caudate
Deep brain stimulation has now virtually replaced ablative ap- Striatum Putamen Caudate Caudate (ventral)
VS
proaches because of its reversibility, adjustability, and less invasive
nature. The use of DBS to treat other neuropsychiatric disorders, such Pallidum SNr/GPi SNr/GPi SNr/GPi SNr/GPi
substantia (motor (oculomotor (associative (limbic
as Tourette syndrome, epilepsy, Alzheimer disease, and psychiatric nigra territory) territory) territory) territory)
disorders (eg, obsessive-compulsive disorder or treatment-
resistant depression), is remarkable. More than 40 brain sites have Thalamus
VLa, VLm MDpl, VLcr VApc, VAmc VAmc, VLm
VApc VApc VLcr, MDpl MD
been explored with DBS for 30 clinical disorders.9 Apart from its
therapeutic benefits, DBS proved to be a highly valuable tool for re-
search, providing a minimally invasive probe for stimulation and re-
ACA indicates anterior cingulate area; CMA, cingulate motor area; DLPFC,
cording of electrical signals from the implanted targets in patients dorsolateral prefrontal cortex; FEF, frontal eye fields; LOFC, lateral orbitofrontal
with a variety of diseases. This research has provided new insights cortex; M1, primary motor cortex; MD, mediodorsal; MDpl, mediodorsal nucleus
into brain network function and dysfunction in neurologic and psy- of thalamus, pars lateralis; MOFC, medial orbitofrontal cortex; PMC, premotor
cortex; SEF, supplementary eye field; SMA, supplementary motor area;
chiatric disorders. SNr, substantia nigra pars reticulata; VAmc, ventral anterior nucleus of
Ablation and DBS are different forms of neuromodulation that thalamus, pars magnocellularis; VApc, ventral anterior nucleus of thalamus,
address dysfunction in cortical and subcortical networks involving pars parvocellularis; VLa, anterior ventrolateral nucleus of the thalamus;
VLcr, ventrolateral nucleus of thalamus, pars caudalis, rostral division;
the basal ganglia, cerebellum, brainstem, thalamus, and cerebral cor-
VLm, ventrolateral nucleus of thalamus, pars medialis; and VS, ventral striatum.
tex. Disturbances propagated throughout specific basal ganglia cir- Reprinted with permission from Elsevier Limited.10
cuits result in movement disorders, such as PD, dystonia, and cho-
rea, as well as psychiatric disorders, such as obsessive-compulsive
disorder and depression, which we now recognize as circuit disor-
ders. It is surprising that, in most cases, ablation and DBS achieve resulting tighter arrangement of functional subdivisions, the pres-
similar results. Also surprising is the fact that these procedures, al- ence of broad dendritic fields, and the apparent overlap between
though remarkably effective in relieving the signs and symptoms of neighboring terminal fields of corticosubthalamic projections.13
movement disorders, do not seem to significantly impair voluntary The signs and symptoms of movement disorders result from dys-
movement, a phenomenon referred to as the paradox of stereo- function within the motor circuit (Figure 2A).14 The motor circuit
tactic surgery. In the present review, we focus on aspects of basal originates and terminates in cortical precentral and postcentral mo-
ganglia circuit dysfunction in movement disorders, using PD as the tor areas, including the motor cortex, premotor cortex, cingulate mo-
example, that provide the understanding and rationale for use of tor area, and supplementary motor area. The cortical areas of ori-
functional neurosurgery in the treatment of these conditions. We gin project in a highly topographic manner to the motor portion of
also comment on the possible functions of the basal ganglia and their the striatum, putamen, and postcommissural caudate nucleus, as
relationship to the paradox. well as to the motor area of the STN.11 The preserved somatotopy
and specificity of neuronal responses found at each node of the mo-
tor circuit reflects the topographic and parallel organization of con-
nections within the motor circuit from the cortex through the basal
Functional Organization of Basal Ganglia Circuits ganglia and thalamus.
The basal ganglia are components of a family of parallel and largely As the first leg of the motor circuit, corticostriatal projections
closed circuits (Figure 1)10 that originate in the cerebral cortex, tra- terminate on dendrites of striatal medium spiny projection neu-
verse the basal ganglia and thalamus, and return to their individual rons. Separate families of -aminobutyric acidergic (GABAergic)
sites of origin in the frontal lobe.11,12 The circuits have been grouped topographic projections link the striatal motor areas to the exter-
and designated as motor, oculomotor, prefrontal, and limbic, reflect- nal segment of the globus pallidus and to GPi and substantia nigra
ing the perceived functions of the cortical areas from which they origi- pars reticulate (SNr). The GPi and SNr are the major output nuclei
nate. The segregated organization of the circuits provides for par- of the basal ganglia and project to the thalamus and brainstem. The
allel processing of cortical inputs through the networks, presumably striatal projections to the GPi and SNr are divided into direct and
by processes that are similar across the different circuits. The spa- indirect pathways. The direct pathway arises from medium spiny
tial separation of these circuits provides an explanation for the re- neurons that project monosynaptically to the GPi and SNr. These me-
markable fact that it is possible to surgically target network com- dium spiny neurons preferentially express dopamine D1-like recep-
ponents to treat specific signs and symptoms of these diseases tors. The indirect pathway arises from medium spiny neurons that
without disturbing other functions. The separation of functional do- project to the external segment of the globus pallidus and express
mains is particularly obvious in the case of GPi and allows DBS to be dopamine D2-like receptors. The indirect pathway encompasses sub-
domain specific in this nucleus. Interventions targeting the STN are sequent projections from the external segment of the globus palli-
perhaps less specific because of the smaller size of the nucleus, the dus to the GPi, both directly and via the STN.
E2 JAMA Neurology Published online September 26, 2015 (Reprinted) jamaneurology.com
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://archneur.jamanetwork.com/ by a Central Michigan University User on 09/27/2015
Basal Ganglia Circuits as Targets for Neuromodulation in Parkinson Disease Review Clinical Review & Education
Figure 2. Parkinsonism-Related Activity Changes in the Basal GangliaThalamocortical Motor Circuit and Targets of Medical and Surgical
and Interventions
A Circuit dysfunction
Normal Parkinsonism
Cortex Cortex
(M1, PMC, SMA, CMA) (M1, PMC, SMA, CMA)
Putamen Putamen
D2 D1
CM VA/VL CM VA/VL
Indirect Direct
SNc SNc
GPe GPe
STN GPi/SNr STN GPi/SNr
Brain stem/ PPN Brain stem/ PPN
Spinal cord Spinal cord
B Treatment targets
Cortex
(M1, PMC, SMA, CMA)
DBS
Tremor
Dopaminergic drugs Dyskinesias
Tremor
Rigidity Putamen
Akinesia/bradykinesia CM VA/VL
Anticholinergic drugs
Tremor DBS
SNc Dyskinesias
Dystonia
GPe
DBS
Tremor STN GPi
Rigidity
Akinesia/bradykinesia
DBS
Dyskinesias
Tremor
Dystonia
Brain stem/ PPN Rigidity
Spinal cord Akinesia/bradykinesia
Dyskinesias
Dystonia
DBS
Gait instability
Freezing of gait
Falls
A, Parkinsonism-related changes in overall activity in the basal nucleus (STN), internal pallidal segment (GPi), and nucleus ventralis intermedius
gangliathalamocortical motor circuit. Black arrows indicate inhibitory targets for the treatment of Parkinson disease. CM indicates centromedian
connections; gray arrows, excitatory connections. The thickness of the arrows nucleus; D1 and D2, dopamine receptor subtypes; GPe, external segment of the
corresponds to their presumed activity. B, Potential and actual targets of globus pallidus; PPN, pedunculopontine nucleus; SNc, substantia nigra pars
antiparkinsonian therapeutic interventions and signs and symptoms addressed compacta; VA, ventral anterior nucleus of the thalamus; and VL, ventrolateral
with each target (arrows with open arrowheads). Deep brain stimulation (DBS) nucleus of the thalamus. For other abbreviations, see the legend to Figure 1.
is approved by the US Food and Drug Administration only at the subthalamic Reprinted with permission from Elsevier Limited.14
Another cortical input to the basal ganglia, the hyperdirect path- latencies than via the striatum. Similar to the other basal ganglia nu-
way, links frontal cortical areas to the STN.15 It remains unclear clei, the STN is divided into motor, oculomotor, associative, and lim-
whether the corticosubthalamic projection consists of collaterals of bic domains based on anatomical and physiologic studies. As men-
corticobulbar and corticospinal pathways or arises from separate cor- tioned above, cortical inputs to the STN may converge and be
tical neurons. The corticosubthalamic pathway, together with the integrated to some extent.13
STN GPi connection (which is presumably shared with the indirect Projections from the motor circuit portions of the GPi termi-
pathway) constitutes the hyperdirect pathway. This pathway may nate in portions of the anterior ventrolateral thalamic nucleus,
allow cortical inputs to reach the GPi and SNr with relatively shorter whereas projections from the associative circuit (mostly from the
jamaneurology.com (Reprinted) JAMA Neurology Published online September 26, 2015 E3
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://archneur.jamanetwork.com/ by a Central Michigan University User on 09/27/2015
Clinical Review & Education Review Basal Ganglia Circuits as Targets for Neuromodulation in Parkinson Disease
SNr) terminate in the ventral anterior thalamic nucleus. The pri- Activity over the hyperdirect pathway is proposed to play a role
mary projections to the different frontal cortical motor fields arise in preventing a premature, reflexive response by increasing inhibi-
from thalamic neurons in the anterior ventrolateral thalamic nucleus tory output to the thalamocortical targets, thus allowing time for the
and the ventral anterior thalamic nucleus and close the motor cir- selection of the most appropriate response. This mechanism may
cuit. Considerable evidence indicates that the motor circuit is com- be relevant in behavioral situations in which a switch from auto-
posed of multiple nonoverlapping parallel subcircuits centered on matic or habitual control to voluntary control is desirable.25
these separate motor fields.16 The modulatory effect of dopamine on basal ganglia transmis-
Collaterals from the main pallidofugal and nigrofugal projections sion (particularly in the striatum) is fundamental to basal ganglia
to the ventral lateral thalamus are directed to the intralaminar nuclei physiology. Dopamine release facilitates corticostriatal transmis-
of the thalamus: the centromedian and parafascicular nuclei. In pri- sion over the direct pathway while inhibiting corticostriatal trans-
mates, the centromedian nucleus receives input from motor areas in mission over the indirect pathway.26 Given the proposed functions
the GPi and SNr and projects to the motor portions of the putamen and of the direct and indirect pathways, the net effect of striatal dopa-
STN,whereasparafascicularnucleusinputandoutputarecomponents mine release therefore appears to be a reduction of basal ganglia out-
of the associative and limbic circuits.17 Unlike the cortical projections put. Applied to the function of the motor circuit, this reduction would
of the ventral anterior thalamic nucleus and the anterior ventrolateral translate into a release of movement inhibition. In addition to its ac-
thalamicnucleussystem,projectionsfromthecentromedianandpara- tions in the striatum, dopamine acts directly on receptors in the STN,
fascicular nuclei to the cerebral cortex are sparse. pallidum thalamus, and cortex to influence discharge patterns and
Another target of GPi and SNr axon collaterals is the brainstem, rates in these structures.27 The behavioral effects of dopamine re-
in particular, the pedunculopontine nucleus18 and the superior col- lease at these sites are not well understood.
liculus.Thepedunculopontinenucleusisaheterogeneousnucleusthat Phasic activation of dopamine receptors on medium spiny neu-
gives rise to cholinergic projections to the thalamus, cerebellum, and rons also shapes the strength of glutamatergic (corticostriatal) trans-
other areas; noncholinergic projections to the substantia nigra pars mission in the striatum, likely through modulation of long-term po-
compacta, STN, and globus pallidus; and descending projections to tentiation and depression, and may play a prominent role in
the pons, medulla, and spinal cord.18 The pedunculopontine nucleus reinforcement learning.28 Based on inactivation and neuroimaging
is a component of the brainstem locomotor region,19 but it may also studies, the associative (prefrontal) circuit plays a prominent role in
have other functions. For instance, lesions of the pedunculopontine the initial learning of a motor task, and the motor circuit may con-
nucleus in primates lead to a general reduction of movement.20 tribute more to the execution of learned motor sequences.29 It is
There is also growing evidence21 for subcortical anatomical not clear whether dopamine release in other basal ganglia loca-
connections and physiologic interactions between the basal gan- tions and the cerebral cortex has similar functions in learning and
glia and the cerebellum across multiple functional domains. Thus, plasticity. It also remains unclear how the apparent role of dopa-
dysfunction in either cerebellar or basal ganglia networks may be mine in the shaping of basal ganglia activity patterns intersects with
directly propagated to the other. In movement disorders, there is the more concrete concepts of the regulation of basal ganglia out-
evidence22 that rest tremor in PD and some types of dystonia put through the direct, indirect, or hyperdirect pathways.
involve such subcortical circuit interactions. In light of these sub-
cortical interactions between the cerebellar and basal ganglia net-
works, it is likely that pure basal ganglia or cerebellar disorders
Pathophysiology of Parkinsonism
may not exist.
The defining features of parkinsonism (ie, akinesia and bradykine-
sia, tremor at rest, and muscular rigidity) are the clinically most
Interactions Between Direct, Indirect, troublesome initial aspects for patients with PD. Parkinsonism is be-
lieved to result from decreased dopaminergic transmission in the mo-
and Hyperdirect Pathways in the Motor Circuit
tor portions of the basal ganglia, in particular, in the motor territory
A fundamental fact and starting point for all models of basal gan- of the striatum (ie, the putamen), owing to progressive loss of in-
glia circuitry and function is that the output from the GPi and SNr nervation from dopaminergic neurons in the dorsolateral substan-
consists of highly active GABAergic (inhibitory) neurons that con- tia nigra pars compacta. Parkinsonism is readily reversed by admin-
tinuously inhibit thalamic and brainstem targets. It is widely istration of levodopa, the precursor of dopamine. Unfortunately, the
believed that activity in the motor circuit over the direct and indi- gradual emergence of levodopa-induced dyskinesias and motor fluc-
rect pathways facilitates or inhibits movements, respectively, and tuations, as well as the development of dopamine-unresponsive fea-
that this involves a modulation of GPi and SNr activity. Cortical tures of gait and balance difficulties and freezing of gait, lead to in-
phasic activation of medium spiny neurons of the direct pathway creasing incapacitation, falls, and decreased quality of life.
act to eventually reduce basal ganglia output with subsequent dis-
inhibition of related thalamocortical neurons and facilitation of Neuronal Activity Changes in Parkinsonism
intended movement.23,24 By contrast, activation of medium spiny Selective dopamine depletion can be achieved through exposure of
neurons of the indirect pathway may lead to increased basal gan- the animals to toxins, such as 6-hydroxy-dopamine or MPTP. Stud-
glia output and to suppression or prevention of movement. The ies in these models, as well as more recent studies in optogenetic
balance between direct and indirect pathway activity may regu- models, have strengthened the view that firing rate changes in the
late the amplitude or speed or limit the extent or duration of ongo- direct and indirect pathways may contribute to parkinsonism (the
ing movements.22,23 so-called rate model of parkinsonism).30 These studies showed a re-
E4 JAMA Neurology Published online September 26, 2015 (Reprinted) jamaneurology.com
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://archneur.jamanetwork.com/ by a Central Michigan University User on 09/27/2015
Basal Ganglia Circuits as Targets for Neuromodulation in Parkinson Disease Review Clinical Review & Education
duction of neuronal discharge in the external segment of the glo- ameliorates parkinsonism.20 Furthermore, several studies37 have
bus pallidus and increased activity in the STN, GPi, and SNr. These shown that the cholinergic neurons of the pedunculopontine nucleus
changes may be a consequence of striatal dopamine depletion and degenerate in PD, indicating that this degeneration may be crucial in
may lead to increased inhibition of the external segment of the glo- the development of gait and balance disorders.
bus pallidus neurons via striatal output neurons of the indirect path- Many reports38 have indicated parkinsonism-associated mor-
way, which, in turn, results in disinhibition of the STN, GPi, and SNr. phologic and functional plasticity of glutamatergic synapses and re-
The increased inhibitory basal ganglia output from the GPi and SNr cipient dendritic spines in the striatum in dopamine-depleted ani-
to the thalamus may excessively inhibit thalamocortical interac- mals and in patients with PD. Several studies have demonstrated that
tions, which may then lead to slowness or absence of movement. morphologic and functional changes also occur in the glutamater-
Changes in discharge patterns in the basal ganglia, thalamus, and gic pathways terminating in the STN (including those from the cor-
cortex are now considered to be of equal or greater importance in tex, thalamus, and pedunculopontine nucleus). Thus, N-methyl-D-
the pathophysiology of parkinsonism than are the aforementioned aspartate glutamate receptor antagonists are known to ameliorate
rate changes.30 One of the most discussed changes in the electrical experimental parkinsonism, presumably by blocking transmission
activity of the basal ganglia of individuals with parkinsonian symp- at terminals of the projections from cortex, thalamus or pedunctu-
toms is the development of oscillatory fluctuations of neuronal spik- lopontine nucleus to the STN.39,40 In addition evidence is emerg-
ing (particularly at frequencies <30 Hz) in the GPi, SNr, and STN as ing that the parkinsonian state is associated with profound plastic-
well as in brain areas that receive basal ganglia output, including the ity at glutamatergic synapses in the STN,41 which may secondarily
thalamus, pyramidal tract neurons of the motor cortex, and possi- affect GABAergic transmission at this site.42 Similar to the findings
bly also brain stem areas, such as the pedunculopontine nucleus. in the striatum, it is not clear whether these changes are causative
Other parkinsonism-related abnormalities are the emergence of ab- or maladaptive.
normal synchrony between neurons and a tendency of neurons in Changes in cerebellar circuits and in interactions between the
the STN, GPi, SNr, and motor thalamus to discharge in oscillatory or cerebellum and basal ganglia may also be important in the patho-
nonoscillatory bursts. Oscillatory burst discharge patterns can oc- physiology of PD. Cerebellar involvement is most clearly recog-
cur with or without concomitant tremor. nized as contributing to parkinsonian tremor. Parkinsonian tremor
appears to be strongly related to abnormal oscillatory activity in the
Changes in Local Field Potentials cerebellar-receiving territory of the thalamus (nucleus ventralis in-
Oscillations can also be identified with local field potentials re- termedius), and DBS or lesions of this area are among the most ef-
corded from DBS electrodes in the basal ganglia. Such oscillations fective treatments of isolated parkinsonian tremor. Tremor also
reflect synchronous membrane potential fluctuations in neuronal clearly responds in many patients to dopaminergic therapy, al-
assemblies. Recordings demonstrate31 the presence of oscillations though often only to high doses of these treatments, and it is not
in the 10- to 25-Hz range in the STN, GPi, and cortex in the unmedi- clear how dopamine loss is linked to tremor.22 The degree of stria-
cated parkinsonian state and in the 60- to 80-Hz range when pa- tal dopamine loss does not correlate with the severity of tremor al-
tients receive levodopa. More recently, abnormal coupling of the am- though the amount of dopamine loss in the GPi and the retrorubral
plitude of -band oscillations and the phase of -band oscillations area does correlate with tremor.22
have been described in cortical local field potentials.32 Because the
amplitude of local field potential oscillations correlates to some ex-
tent with the severity of aspects of parkinsonism, efforts are under
way to use these signals in a closed-loop manner to control the de- Targeting Neurologic Signs and Symptoms
livery of DBS.33
Through Neuromodulation
Other Changes Contributing to Motor Disturbances in PD The fact that virtually all movement disorders of basal ganglia ori-
Most of the extrastriatal portions of the basal ganglia, as well as the gin appear to result from motor circuit dysfunction allows for selec-
thalamus and cerebral cortex, receive dopaminergic innervation, and tive interventions with ablation or DBS (Figure 2B), specifically in the
parkinsonism is associated with substantial loss of input in all of these STN and the GPi, which is highly effective for the cardinal features
areas. Local dopamine loss in the STN, GPi, and SNr has been shown27 of PD as well as dystonia and drug-induced motor fluctuations and
to lead to abnormal firing patterns in these nuclei and may be in- dyskinesias. Although the external segment of the globus pallidus
volved in the beneficial effects and adverse effects of dopaminer- is not currently targeted, it has been shown43 that DBS of this re-
gic medications. gion may also be effective for PD.
Other structures and feedback loops, such as those involving the Unfortunately, interventions at the conventional surgical tar-
pedunculopontinenucleusandcentromediannucleusofthethalamus, gets (STN or GPi) are generally not effective against levodopa-
likely also contribute to parkinsonism. Several studies34 have shown unresponsive gait and balance disturbances and freezing of gait. As
that DBS of the centromedian nucleus of the thalamus area can ame- mentioned above, degeneration of cholinergic pedunculopontine
liorate tremor and transiently reduce akinesia and bradykinesia. The nucleus neurons is implicated in the gait and balance disturbances.
projection from the centromedian nucleus of the thalamus to the stria- In fact, low-frequency stimulation in this area, presumably by acti-
tum is also known to degenerate in patients with PD as well as in ex- vating remaining neurons and their axons, may improve parkinso-
perimental animals with parkinsonism.35,36 Reduced activity in the pe- nian gait problems.44
dunculopontine nucleus has been linked to poverty of movement, and Thalamic targets have also been used for DBS or ablative pro-
increasing pedunculopontine nucleus activity in parkinsonian animals cedures in the treatment of PD. Ablation or DBS of the cerebellar re-
jamaneurology.com (Reprinted) JAMA Neurology Published online September 26, 2015 E5
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://archneur.jamanetwork.com/ by a Central Michigan University User on 09/27/2015
Clinical Review & Education Review Basal Ganglia Circuits as Targets for Neuromodulation in Parkinson Disease
cipient portions of the thalamus is effective for treatment of tremor, tributed motor system which can operate, albeit imperfectly, in the
including the rest tremor in PD,45 but has little effect on akinesia and absence of striato-pallido-thalamo-cortical feedback. There may,
bradykinesia. Ablation or DBS of the pallidal-receiving area of the however, be subtle defects in motor performance after thalamic and
thalamus has been found46 to be effective for drug-induced dyski- pallidal lesions which have escaped attention.48(p877)
nesias and some forms of dystonia but seems to have little effect As mentioned above, numerous proposals for the general
on bradykinesia or akinesia, suggesting that the basal ganglia thala- function of the basal ganglia have been advanced, but, as argued
mocortical pathway may be more involved in the expression of ab- elsewhere,49 these functions are not solidly established and are
normal movements rather than akinesia and bradykinesia. Abnor- difficult to reconcile with the outcomes of both animal studies and
mal and excessive GPi output to the pedunculopontine nucleus may stereotactic surgery. The dramatic and immediate effects of abla-
disrupt and inhibit activity in this nucleus and may play a greater role tion and DBS and the absence of intervention-related motor
in akinesia than is usually assumed.20 impairments in patients with PD argue against an essential role of
Targeting of the motor circuit portions of the STN, GPi, and thala- the basal ganglia in the basic control of movement (through pro-
mus for ablative or stimulation approaches is surprisingly effective cesses such as response inhibition or action selection) and favor
for a diverse group of movement disorders, suggesting that the sur- the view that the basal ganglia motor circuit primarily serves
gical interventions do not target specific pathophysiologic abnor- higher-order functions, such as reinforcement learning and the
malities. Instead, they appear to eliminate disruptive basal ganglia regulation of global movement vigor.50 Even if deficits exist, it
output regardless of its specific character. This finding is most eas- may be very difficult to detect those resulting from interference
ily understood in the case of pallidotomy or subthalamotomy, which with such functions in patients who have preexisting significant,
directly interrupts abnormal outflow from the basal ganglia. Al- widespread disturbances.
though the actions of DBS are complex and controversial, they may
be viewed in part as acting in a fashion similar to ablation. In this case,
an informational lesion may be achieved by overriding and block-
Conclusions
ing transmission of abnormal activity.47 Ablative or functional le-
sions of basal ganglia output may subsequently allow the relatively During the past 2 decades, there has been remarkable progress in
intact portions of the motor system downstream from the basal gan- understanding the pathophysiologic basis of movement disorders
glia to resume more normal functions. It would thus appear that the such as PD, clarifying the effects of, and rationale for, current surgi-
signs and symptoms of movement disorders that result from disor- cal procedures and developing novel surgical targets. Deep brain
dered basal ganglia activity simply reflect the disturbance induced stimulation has also proved to be a useful tool for exploring and
by the altered activity in brain networks that are targeted by the ab- studying function and dysfunction in movement disorders as well
normality and do not represent or reflect the absence of the nor- as other neuropsychiatric disorders.
mal functions of the basal ganglia. To progress further and to develop more effective treatment
strategies for patients with movement disorders, we need a clearer
understanding of the network structure and function and of the na-
ture of the signature network disturbances in neurologic and psy-
The Paradox of Stereotactic Surgery
chiatric disorders, in particular regarding the contribution of dis-
An important aspect and major element of the rationale for surgi- turbed interactions between the hyperdirect, direct, and indirect
cal ablation and DBS is the fact that the interventions are highly suc- circuits as well as the contribution of interactions between the basal
cessful in ameliorating the signs and symptoms of these disorders ganglia, cerebellar, and brainstem networks. Also much needed is a
but do not cause obvious or significant impairment of voluntary clearer understanding of the mechanisms of action of DBS and the
movement. This is the paradox of stereotactic surgery discussed in development of novel targets and stimulation paradigms. Finally,
a well-known article by Marsden and Obeso.48 These authors specu- there remains a need to identify better ways of addressing both drug-
lated that the motor circuits of the basal ganglia are part of a dis- resistant motor and nonmotor symptoms of PD.
ARTICLE INFORMATION Funding/Support: The writing of this article was REFERENCES
Accepted for Publication: July 28, 2015. supported by grant P50-NS071669 from the 1. Bergman H, Wichmann T, DeLong MR. Reversal
National Institutes of Health/National Institute of of experimental parkinsonism by lesions of the
Published Online: September 26, 2015. Neurological Disorders and Stroke and grant
doi:10.1001/jamaneurol.2015.2397. subthalamic nucleus. Science. 1990;249(4975):
P51-OD011132 from the National Institutes of 1436-1438.
Author Contributions: Drs DeLong and Wichmann Health/Office of Research Infrastructure Programs
had full access to all the data in the study and take to the Yerkes Center. 2. Wichmann T, DeLong MR, Guridi J, Obeso JA.
responsibility for the integrity of the data and the Milestones in research on the pathophysiology of
Role of the Funder/Sponsor: The funding sources Parkinsons disease. Mov Disord. 2011;26(6):
accuracy of the data analysis. had no role in the design and conduct of the study;
Study concept and design: All authors. 1032-1041.
collection, management, analysis, and
Acquisition, analysis, or interpretation of data: All interpretation of the data; preparation, review, or 3. Laitinen LV, Bergenheim AT, Hariz MI. Leksells
authors. approval of the manuscript; and decision to submit posteroventral pallidotomy in the treatment of
Drafting of the manuscript: All authors. the manuscript for publication. Parkinsons disease. J Neurosurg. 1992;76(1):53-61.
Critical revision of the manuscript for important 4. Benabid AL, Pollak P, Louveau A, Henry S,
intellectual content: All authors. de Rougemont J. Combined (thalamotomy and
Administrative, technical, or material support: All stimulation) stereotactic surgery of the VIM
authors. thalamic nucleus for bilateral Parkinson disease.
Conflict of Interest Disclosures: None reported. Appl Neurophysiol. 1987;50(1-6):344-346.
E6 JAMA Neurology Published online September 26, 2015 (Reprinted) jamaneurology.com
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://archneur.jamanetwork.com/ by a Central Michigan University User on 09/27/2015
Basal Ganglia Circuits as Targets for Neuromodulation in Parkinson Disease Review Clinical Review & Education
5. Benazzouz A, Gross C, Fger J, Boraud T, 21. Bostan AC, Dum RP, Strick PL. Cerebellar pedunculopontine nucleus lesions: a tale of two
Bioulac B. Reversal of rigidity and improvement in networks with the cerebral cortex and basal systems. J Neurosci. 2013;33(29):11986-11993.
motor performance by subthalamic high-frequency ganglia. Trends Cogn Sci. 2013;17(5):241-254. 38. Villalba RM, Smith Y. Differential structural
stimulation in MPTP-treated monkeys. Eur J Neurosci. 22. Hallett M. Tremor: pathophysiology. plasticity of corticostriatal and thalamostriatal
1993;5(4):382-389. Parkinsonism Relat Disord. 2014;20(suppl 1): axo-spinous synapses in MPTP-treated
6. Pollak P, Benabid AL, Gross C, et al. Effects of the S118-S122. parkinsonian monkeys. J Comp Neurol. 2011;519(5):
stimulation of the subthalamic nucleus in Parkinson 23. Albin RL, Young AB, Penney JB. The functional 989-1005.
disease. (in French). Rev Neurol (Paris). 1993;149(3): anatomy of basal ganglia disorders. Trends Neurosci. 39. Klockgether T, Turski L. NMDA antagonists
175-176. 1989;12(10):366-375. potentiate antiparkinsonian actions of L-dopa in
7. Fox MD, Alterman RL. Brain stimulation for 24. DeLong MR. Primate models of movement monoamine-depleted rats. Ann Neurol. 1990;28(4):
torsion dystonia. JAMA Neurol. 2015;72(6):713-719. disorders of basal ganglia origin. Trends Neurosci. 539-546.
8. Mills KA, Starr PA, Ostrem JL. Neuromodulation 1990;13(7):281-285. 40. Pan MK, Tai CH, Liu WC, Pei JC, Lai WS, Kuo CC.
for dystonia: target and patient selection. 25. Jahanshahi M. Effects of deep brain stimulation Deranged NMDAergic cortico-subthalamic
Neurosurg Clin N Am. 2014;25(1):59-75. of the subthalamic nucleus on inhibitory and transmission underlies parkinsonian motor deficits.
9. Hariz M, Blomstedt P, Zrinzo L. Future of brain executive control over prepotent responses in J Clin Invest. 2014;124(10):4629-4641.
stimulation: new targets, new indications, new Parkinsons disease. Front Syst Neurosci. 2013;7:118. 41. Mathai A, Ma Y, Par JF, Villalba RM,
technology. Mov Disord. 2013;28(13):1784-1792. 26. Wichmann T. Functional aspects of the basal Wichmann T, Smith Y. Reduced cortical innervation
10. Wichmann T, Delong MR. Deep brain ganglia. In: Burn D, ed. Oxford Textbook of of the subthalamic nucleus in MPTP-treated
stimulation for neurologic and neuropsychiatric Movement Disorders. Oxford, England: Oxford parkinsonian monkeys. Brain. 2015;138(pt 4):
disorders. Neuron. 2006;52(1):197-204. University Press; 2013:21-32. 946-962.
11. Alexander GE, DeLong MR, Strick PL. Parallel 27. Rommelfanger KS, Wichmann T. Extrastriatal 42. Chu HY, Atherton JF, Wokosin D, Surmeier DJ,
organization of functionally segregated circuits dopaminergic circuits of the basal ganglia. Front Bevan MD. Heterosynaptic regulation of external
linking basal ganglia and cortex. Annu Rev Neurosci. Neuroanat. 2010;4:139. globus pallidus inputs to the subthalamic nucleus
1986;9:357-381. by the motor cortex. Neuron. 2015;85(2):364-376.
28. Hikosaka O, Kim HF, Yasuda M, Yamamoto S.
12. Middleton FA, Strick PL. Basal ganglia and Basal ganglia circuits for reward value-guided 43. Vitek JL, Zhang J, Hashimoto T, Russo GS,
cerebellar loops: motor and cognitive circuits. Brain behavior. Annu Rev Neurosci. 2014;37:289-306. Baker KB. External pallidal stimulation improves
Res Brain Res Rev. 2000;31(2-3):236-250. parkinsonian motor signs and modulates neuronal
29. Miyachi S, Hikosaka O, Miyashita K, Krdi Z, activity throughout the basal ganglia thalamic
13. Haynes WI, Haber SN. The organization of Rand MK. Differential roles of monkey striatum in network. Exp Neurol. 2012;233(1):581-586.
prefrontal-subthalamic inputs in primates provides learning of sequential hand movement. Exp Brain Res.
an anatomical substrate for both functional 1997;115(1):1-5. 44. Garcia-Rill E, Hyde J, Kezunovic N,
specificity and integration: implications for basal Urbano FJ, Petersen E. The physiology of the
30. Galvan A, Devergnas A, Wichmann T. pedunculopontine nucleus: implications for deep
ganglia models and deep brain stimulation. J Neurosci. Alterations in neuronal activity in basal
2013;33(11):4804-4814. brain stimulation. J Neural Transm. 2015;122(2):
ganglia-thalamocortical circuits in the parkinsonian 225-235.
14. Galvan A, Wichmann T. Pathophysiology of state. Front Neuroanat. 2015;9:5.
parkinsonism. Clin Neurophysiol. 2008;119(7): 45. OSullivan D, Pell M. Long-term follow-up of
31. Brown P, Oliviero A, Mazzone P, Insola A, DBS of thalamus for tremor and STN for Parkinsons
1459-1474. Tonali P, Di Lazzaro V. Dopamine dependency of disease. Brain Res Bull. 2009;78(2-3):119-121.
15. Nambu A, Takada M, Inase M, Tokuno H. Dual oscillations between subthalamic nucleus and
somatotopical representations in the primate pallidum in Parkinsons disease. J Neurosci. 2001;21 46. Duval C, Panisset M, Strafella AP, Sadikot AF.
subthalamic nucleus: evidence for ordered but (3):1033-1038. The impact of ventrolateral thalamotomy on tremor
reversed body-map transformations from the and voluntary motor behavior in patients with
32. de Hemptinne C, Ryapolova-Webb ES, Air EL, Parkinsons disease. Exp Brain Res. 2006;170(2):
primary motor cortex and the supplementary et al. Exaggerated phase-amplitude coupling in the
motor area. J Neurosci. 1996;16(8):2671-2683. 160-171.
primary motor cortex in Parkinson disease. Proc
16. Hoover JE, Strick PL. Multiple output channels Natl Acad Sci U S A. 2013;110(12):4780-4785. 47. Agnesi F, Connolly AT, Baker KB, Vitek JL,
in the basal ganglia. Science. 1993;259(5096): Johnson MD. Deep brain stimulation imposes
33. Little S, Pogosyan A, Neal S, et al. Adaptive complex informational lesions. PLoS One. 2013;8
819-821. deep brain stimulation in advanced Parkinson (8):e74462.
17. Smith Y, Raju DV, Pare JF, Sidibe M. The disease. Ann Neurol. 2013;74(3):449-457.
thalamostriatal system: a highly specific network of 48. Marsden CD, Obeso JA. The functions of the
34. Peppe A, Gasbarra A, Stefani A, et al. Deep basal ganglia and the paradox of stereotaxic surgery
the basal ganglia circuitry. Trends Neurosci. 2004; brain stimulation of CM/PF of thalamus could be
27(9):520-527. in Parkinsons disease. Brain. 1994;117(pt 4):877-897.
the new elective target for tremor in advanced
18. Mena-Segovia J, Bolam JP, Magill PJ. Parkinsons disease? Parkinsonism Relat Disord. 49. Wichmann T, DeLong MR. Rationale for surgical
Pedunculopontine nucleus and basal ganglia: 2008;14(6):501-504. interventions in movement disorders. In: Winn RH,
distant relatives or part of the same family? Trends ed. Youmans & Winn Neurological Surgery. 7th ed.
35. Villalba RM, Wichmann T, Smith Y. Neuronal Philadelphia, PA: Saunders/Elsevier; 2015. In press.
Neurosci. 2004;27(10):585-588. loss in the caudal intralaminar thalamic nuclei in a
19. Alam M, Schwabe K, Krauss JK. The primate model of Parkinsons disease. Brain Struct 50. Mazzoni P, Hristova A, Krakauer JW. Why dont
pedunculopontine nucleus area: critical evaluation Funct. 2014;219(1):381-394. we move faster? Parkinsons disease, movement
of interspecies differences relevant for its use as a vigor, and implicit motivation. J Neurosci. 2007;27
36. Halliday GM. Thalamic changes in Parkinsons (27):7105-7116.
target for deep brain stimulation. Brain. 2011; disease. Parkinsonism Relat Disord. 2009;
134(pt 1):11-23. 15(suppl 3):S152-S155.
20. Stein JF. Akinesia, motor oscillations and the 37. Grabli D, Karachi C, Folgoas E, et al. Gait
pedunculopontine nucleus in rats and men. Exp disorders in parkinsonian monkeys with
Neurol. 2009;215(1):1-4.
jamaneurology.com (Reprinted) JAMA Neurology Published online September 26, 2015 E7
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://archneur.jamanetwork.com/ by a Central Michigan University User on 09/27/2015
Das könnte Ihnen auch gefallen
- Budwig Cancer GuideDokument101 SeitenBudwig Cancer Guidedora.oreiro9920Noch keine Bewertungen
- Free Aromatherapy E-Course Denise Whichello BrownDokument51 SeitenFree Aromatherapy E-Course Denise Whichello BrownDaniela BerbeceNoch keine Bewertungen
- 1908 Character and Anal ErotismDokument4 Seiten1908 Character and Anal ErotismFutile Hurling100% (1)
- Electromyography in CNS Disorders: Central EMGVon EverandElectromyography in CNS Disorders: Central EMGBhagwan T. ShahaniNoch keine Bewertungen
- 1358453842.3856hematology Question BankDokument182 Seiten1358453842.3856hematology Question BankKay BristolNoch keine Bewertungen
- Drug Education NotesDokument75 SeitenDrug Education NotesJoshua D None-NoneNoch keine Bewertungen
- Surgical Therapies For Parkinson DiseaseDokument13 SeitenSurgical Therapies For Parkinson DiseaseAnali Durán CorderoNoch keine Bewertungen
- Neuromodulation PDFDokument18 SeitenNeuromodulation PDFSureshNoch keine Bewertungen
- CH 11 Admission, Discharge, Transfers & ReferralsDokument14 SeitenCH 11 Admission, Discharge, Transfers & ReferralsNilakshi Barik Mandal100% (1)
- The Right Choice: Smith&nephewDokument4 SeitenThe Right Choice: Smith&nephewapi-19808945Noch keine Bewertungen
- Johns Hopkins Dean - Reflections On Medical School AdmissionsDokument4 SeitenJohns Hopkins Dean - Reflections On Medical School AdmissionstheintrepiddodgerNoch keine Bewertungen
- TheraSuit BrochureDokument8 SeitenTheraSuit BrochureMhmd IrakyNoch keine Bewertungen
- França (2018) Brain StimulationDokument12 SeitenFrança (2018) Brain StimulationAna paula CamargoNoch keine Bewertungen
- Neurosurgery For Parkinson - S DiseaseDokument12 SeitenNeurosurgery For Parkinson - S DiseaseJesus German Loya ValladolidNoch keine Bewertungen
- Anatomia y Fisiologia de GB MDSDokument9 SeitenAnatomia y Fisiologia de GB MDSMauricioNoch keine Bewertungen
- Improving Working Memory Exploring The Effect of Transcranial RandomDokument6 SeitenImproving Working Memory Exploring The Effect of Transcranial RandomDanish MujibNoch keine Bewertungen
- Invasive Recordings From The BrainDokument13 SeitenInvasive Recordings From The BrainMaria Isabel BowieNoch keine Bewertungen
- Current Surgical Treatments For Parkinson's Disease and Potential Therapeutic TargetsDokument4 SeitenCurrent Surgical Treatments For Parkinson's Disease and Potential Therapeutic TargetsRudolph MuliawanNoch keine Bewertungen
- Schulz Gerloff Hummel 2013 Non Invasive Brain Stimulation in Neurological DiseasesDokument9 SeitenSchulz Gerloff Hummel 2013 Non Invasive Brain Stimulation in Neurological DiseasesandreapalmapNoch keine Bewertungen
- Fnins 14 558532Dokument16 SeitenFnins 14 558532anita putri effendiNoch keine Bewertungen
- Brain Structure Alterations in Depression Psychoradiological EvidenceDokument10 SeitenBrain Structure Alterations in Depression Psychoradiological EvidenceMoo GeeNoch keine Bewertungen
- Pedunculopontine Nucleus Microelectrode Recordings in Movement Disorder PatientsDokument10 SeitenPedunculopontine Nucleus Microelectrode Recordings in Movement Disorder PatientsT.U. Pai João da Caridade & Caboclo FlechasNoch keine Bewertungen
- Treatment of Parkinson Disease With Motor Fluctuations and DyskinesiaDokument15 SeitenTreatment of Parkinson Disease With Motor Fluctuations and DyskinesiaSalvador FigueroaNoch keine Bewertungen
- DBS2008Dokument48 SeitenDBS2008Carol Artigas Gómez100% (1)
- Therapeutic Developments in Spinal Muscular Atrophy: Douglas M. Sproule and Petra KaufmannDokument13 SeitenTherapeutic Developments in Spinal Muscular Atrophy: Douglas M. Sproule and Petra KaufmannNoniqTobingNoch keine Bewertungen
- Noninvasive Spinal Cord Stimulation Tech PDFDokument11 SeitenNoninvasive Spinal Cord Stimulation Tech PDFmustakNoch keine Bewertungen
- Deep Brain Stimulation For Parkinson's Disease - Patient SelectionDokument9 SeitenDeep Brain Stimulation For Parkinson's Disease - Patient SelectionAtul JainNoch keine Bewertungen
- An Evaluation of Neuroplasticity and Behavior After Deep Brain Stimulation of The Nucleus Accumbens in An Animal Model of DepressionDokument10 SeitenAn Evaluation of Neuroplasticity and Behavior After Deep Brain Stimulation of The Nucleus Accumbens in An Animal Model of DepressionFrontiersNoch keine Bewertungen
- Fphys 06 00240Dokument14 SeitenFphys 06 00240elbueno21Noch keine Bewertungen
- Art. L Zrinzo - MRI-guided STN DBS in Parkinson's Disease Without Microelectrode Recording Efficacy and SafetyDokument7 SeitenArt. L Zrinzo - MRI-guided STN DBS in Parkinson's Disease Without Microelectrode Recording Efficacy and SafetyEstereotaxia BrasilNoch keine Bewertungen
- Fluorescent False NTsDokument5 SeitenFluorescent False NTsMae PNoch keine Bewertungen
- Surgical Management of Spinal Dysraphism: Five - Year Experience in A Central HospitalDokument5 SeitenSurgical Management of Spinal Dysraphism: Five - Year Experience in A Central HospitalBhayu RizallinoorNoch keine Bewertungen
- Artículo15 - ParkinsonDokument15 SeitenArtículo15 - ParkinsonRicardo FernandezNoch keine Bewertungen
- Vagus Nerve Stimulation A New Tool For Brain ResearchDokument9 SeitenVagus Nerve Stimulation A New Tool For Brain ResearchErnesto Ochoa MonroyNoch keine Bewertungen
- Manual Therapy: Annina B. Schmid, Robert J. Nee, Michel W. CoppietersDokument9 SeitenManual Therapy: Annina B. Schmid, Robert J. Nee, Michel W. CoppietersJose PerezNoch keine Bewertungen
- Art. PA Star - Microelectrode-Guided Implantation of Deep Brain Stimulators Into The Globus Pallidus Internus For Dystonia Techniques, Electrode Locations, and OutcomesDokument14 SeitenArt. PA Star - Microelectrode-Guided Implantation of Deep Brain Stimulators Into The Globus Pallidus Internus For Dystonia Techniques, Electrode Locations, and OutcomesPaul RodrigoNoch keine Bewertungen
- Movementdisordersand Proxysmaldisorders: Carola - TammingaDokument2 SeitenMovementdisordersand Proxysmaldisorders: Carola - Tammingastein godoy pachecoNoch keine Bewertungen
- Jurnal NeuropsikiatriDokument10 SeitenJurnal NeuropsikiatriPosterilmiah Majestynas2019Noch keine Bewertungen
- Imaging in Movement Disorders.11Dokument25 SeitenImaging in Movement Disorders.11BALEWNoch keine Bewertungen
- Parkinson's Disease: Mechanisms, Translational Models and Management StrategiesDokument14 SeitenParkinson's Disease: Mechanisms, Translational Models and Management StrategiesGleyce CabralNoch keine Bewertungen
- Clinical Efficacy and Potential Mechanisms of NeurofeedbackDokument11 SeitenClinical Efficacy and Potential Mechanisms of NeurofeedbackFelix NogueiraNoch keine Bewertungen
- Review: Dopaminergic Neurons and Brain Reward Pathways From Neurogenesis To Circuit AssemblyDokument11 SeitenReview: Dopaminergic Neurons and Brain Reward Pathways From Neurogenesis To Circuit AssemblyNazihan Safitri AlkatiriNoch keine Bewertungen
- Advances in Understanding and Treating Mental Illness: Proceedings of The 40th Canadian College of Neuropsychopharmacology Annual Meeting SymposiaDokument6 SeitenAdvances in Understanding and Treating Mental Illness: Proceedings of The 40th Canadian College of Neuropsychopharmacology Annual Meeting Symposiareynolds.lauNoch keine Bewertungen
- Translational Principles of Deep Brain Stimulation: ReviewsDokument13 SeitenTranslational Principles of Deep Brain Stimulation: ReviewsbleaurosenNoch keine Bewertungen
- Neuroimage: Clinical: Cyril Atkinson-Clement, Serge Pinto, Alexandre Eusebio, Olivier CoulonDokument13 SeitenNeuroimage: Clinical: Cyril Atkinson-Clement, Serge Pinto, Alexandre Eusebio, Olivier CoulonKanagaraj SubramaniNoch keine Bewertungen
- Applications of Transcranial Magnetic Stimulation TMS in Child and Adolescent PsychiatryDokument10 SeitenApplications of Transcranial Magnetic Stimulation TMS in Child and Adolescent Psychiatryssky worthNoch keine Bewertungen
- Parkinson19 PDFDokument6 SeitenParkinson19 PDFLorenaNoch keine Bewertungen
- Contents NCLDokument3 SeitenContents NCLdewi najiraNoch keine Bewertungen
- J Clinph 2013 03 031Dokument7 SeitenJ Clinph 2013 03 031Andres Rojas JerezNoch keine Bewertungen
- Science:, 819 (2003) Ted M. Dawson and Valina L. DawsonDokument5 SeitenScience:, 819 (2003) Ted M. Dawson and Valina L. DawsonSomanshu BanerjeeNoch keine Bewertungen
- Schizophrenia ResearchDokument7 SeitenSchizophrenia ResearchCarol Ximena Vargas CastroNoch keine Bewertungen
- JR 5Dokument9 SeitenJR 5rahmat feryadiNoch keine Bewertungen
- Luig Jes 2013Dokument12 SeitenLuig Jes 2013ximena sanchezNoch keine Bewertungen
- Fnhum 17 1006744Dokument14 SeitenFnhum 17 1006744Peggy WangNoch keine Bewertungen
- Personality and Individual Differences: Sharon NivDokument11 SeitenPersonality and Individual Differences: Sharon NivAndrea ReisNoch keine Bewertungen
- Role of Preclinical Data in PDDokument23 SeitenRole of Preclinical Data in PDIrving ParraNoch keine Bewertungen
- 668 FullDokument10 Seiten668 FullfranciscoNoch keine Bewertungen
- Parkinson's: A Syndrome Rather Than A Disease?: BackgroundDokument8 SeitenParkinson's: A Syndrome Rather Than A Disease?: BackgroundEduardo Santana SuárezNoch keine Bewertungen
- Fnana 12 00025Dokument11 SeitenFnana 12 00025Mohamed TahaNoch keine Bewertungen
- Biology ProjectDokument14 SeitenBiology ProjectVittal Rao LNoch keine Bewertungen
- Fimmu 13 856254Dokument15 SeitenFimmu 13 856254Maria Vitória GomesNoch keine Bewertungen
- Cerebral Palsy: Causes and Treatment Alternatives, Based On The Evidence Provided by Gait Analysis - Rupcich M, Bravo RDokument2 SeitenCerebral Palsy: Causes and Treatment Alternatives, Based On The Evidence Provided by Gait Analysis - Rupcich M, Bravo RRicardo BravoNoch keine Bewertungen
- Deep Brain Stimulation For The Treatment of Uncommon Tremor SyndromesDokument15 SeitenDeep Brain Stimulation For The Treatment of Uncommon Tremor SyndromesAnonymous b6clzcSJNoch keine Bewertungen
- 2014 PD Rehabil NeurolSciDokument9 Seiten2014 PD Rehabil NeurolScimsa_imegNoch keine Bewertungen
- Neuroanatomic Connectivity of The Human Ascending ArousalDokument16 SeitenNeuroanatomic Connectivity of The Human Ascending ArousalBritany SantanaNoch keine Bewertungen
- Review: New Horizons in Diabetic Neuropathy: Mechanisms, Bioenergetics, and PainDokument18 SeitenReview: New Horizons in Diabetic Neuropathy: Mechanisms, Bioenergetics, and PainDIBA TRIULANDARI KUSNADINoch keine Bewertungen
- Pi Is 1094715921064345Dokument7 SeitenPi Is 1094715921064345syarifaNoch keine Bewertungen
- Paper Frontiers TOC-DBS Varjao21Dokument12 SeitenPaper Frontiers TOC-DBS Varjao21TatianeDanielNoch keine Bewertungen
- Sexuality and Spinal Cord InjuryDokument10 SeitenSexuality and Spinal Cord InjurySebastián GallegosNoch keine Bewertungen
- Cognitive Impairment and Dementia in Parkinson's Disease - Clinical Features, Diagnosis, and ManagementDokument15 SeitenCognitive Impairment and Dementia in Parkinson's Disease - Clinical Features, Diagnosis, and ManagementSebastián GallegosNoch keine Bewertungen
- Neuromuscular Manifestations of Critical Illness: Invited ReviewDokument24 SeitenNeuromuscular Manifestations of Critical Illness: Invited ReviewSebastián GallegosNoch keine Bewertungen
- Direct and Indirect Pathways of Basal Ganglia A Critical ReppraisalDokument9 SeitenDirect and Indirect Pathways of Basal Ganglia A Critical ReppraisalSebastián Gallegos0% (1)
- Osteogenesis Imperfecta: Epidemiology and Pathophysiology: Elizabeth Martin, MHS, and Jay R. Shapiro, MDDokument7 SeitenOsteogenesis Imperfecta: Epidemiology and Pathophysiology: Elizabeth Martin, MHS, and Jay R. Shapiro, MDSebastián GallegosNoch keine Bewertungen
- Brain: Altering Spinal Cord Excitability Enables Voluntary Movements After Chronic Complete Paralysis in HumansDokument16 SeitenBrain: Altering Spinal Cord Excitability Enables Voluntary Movements After Chronic Complete Paralysis in HumansSebastián GallegosNoch keine Bewertungen
- Biochemical and Biophysical Research CommunicationsDokument6 SeitenBiochemical and Biophysical Research CommunicationsSebastián GallegosNoch keine Bewertungen
- Thomson 2007 Functional Maps of Neocortical CircuitryDokument24 SeitenThomson 2007 Functional Maps of Neocortical CircuitrySebastián GallegosNoch keine Bewertungen
- Annurev - Castillo PDokument27 SeitenAnnurev - Castillo PSebastián GallegosNoch keine Bewertungen
- The Structure of Multi-Neuron Firing Patterns in Primate RetinaDokument13 SeitenThe Structure of Multi-Neuron Firing Patterns in Primate RetinaSebastián GallegosNoch keine Bewertungen
- Katz 2002 VisualPlasticity HW 4Dokument9 SeitenKatz 2002 VisualPlasticity HW 4Sebastián GallegosNoch keine Bewertungen
- Mount Castle 1957Dokument27 SeitenMount Castle 1957Sebastián GallegosNoch keine Bewertungen
- 599 FullDokument4 Seiten599 FullSebastián GallegosNoch keine Bewertungen
- Neuroscience PDFDokument4 SeitenNeuroscience PDFSebastián GallegosNoch keine Bewertungen
- Nursing Care Plan Myocardia InfarctionDokument3 SeitenNursing Care Plan Myocardia Infarctionaldrin1920Noch keine Bewertungen
- Daftar Harga Pengujian Dan Kalibrasi Alat KesehatanDokument3 SeitenDaftar Harga Pengujian Dan Kalibrasi Alat KesehatanVIDYA VIRA PAKSYA PUTRANoch keine Bewertungen
- Prospectus PDFDokument68 SeitenProspectus PDFPrince Digital ComputersNoch keine Bewertungen
- 2019 Fall RNSG 2263 Clinical Mental Health CIDDokument102 Seiten2019 Fall RNSG 2263 Clinical Mental Health CIDadam50% (2)
- AbortionDokument39 SeitenAbortionMerielLouiseAnneVillamilNoch keine Bewertungen
- Athos Dosys enDokument6 SeitenAthos Dosys enzakaria tahoriNoch keine Bewertungen
- GHA-Hospital List As of March 2019Dokument1 SeiteGHA-Hospital List As of March 2019JULIUS TIBERIONoch keine Bewertungen
- Egyptian Hospital Accreditation Program: Standards: Sixth Edition May 2005Dokument71 SeitenEgyptian Hospital Accreditation Program: Standards: Sixth Edition May 2005khayisamNoch keine Bewertungen
- RXN For DR - SagamlaDokument2 SeitenRXN For DR - Sagamlayeng botzNoch keine Bewertungen
- Imperforate Anus PDFDokument2 SeitenImperforate Anus PDFGlyneth FranciaNoch keine Bewertungen
- Current Issues in Postoperative Pain Management PDFDokument12 SeitenCurrent Issues in Postoperative Pain Management PDFikm fkunissulaNoch keine Bewertungen
- Human Biology Laboratory 4: Body Tissues and Organization List The 4 Tissue Types and Give A General Function: Pg. 40Dokument4 SeitenHuman Biology Laboratory 4: Body Tissues and Organization List The 4 Tissue Types and Give A General Function: Pg. 40bugyourselfNoch keine Bewertungen
- 01 WB - CC - Management - of - PADIS - and - NMB - in - Adult - Intensive - Care - Unit - PatientsDokument49 Seiten01 WB - CC - Management - of - PADIS - and - NMB - in - Adult - Intensive - Care - Unit - PatientskushishaNoch keine Bewertungen
- Carcinoma StomachDokument54 SeitenCarcinoma StomachDn Ezrinah Dn EshamNoch keine Bewertungen
- Neck Pain and Lower Back Pain. Med Clin N Am. 2019.Dokument14 SeitenNeck Pain and Lower Back Pain. Med Clin N Am. 2019.Jose Fernando Diez100% (1)
- Virtual Long Bone DissectionDokument2 SeitenVirtual Long Bone Dissectionapi-438665079Noch keine Bewertungen
- Chapter - 014 Student HandoutsDokument16 SeitenChapter - 014 Student Handoutsebiniyam2021Noch keine Bewertungen
- FREMEC FormsDokument1 SeiteFREMEC FormsAviation MedicineNoch keine Bewertungen
- Real - VITAL-SIGNS ChecklistDokument2 SeitenReal - VITAL-SIGNS ChecklistLoraine SandovalNoch keine Bewertungen
- Physical Capabilities of Instructors at The End of Hot Fire Training (0305) (158529)Dokument42 SeitenPhysical Capabilities of Instructors at The End of Hot Fire Training (0305) (158529)Onion PapaNoch keine Bewertungen
- Farm ChemicalsDokument16 SeitenFarm ChemicalsHasrul RosliNoch keine Bewertungen