Beruflich Dokumente
Kultur Dokumente
Spums Position Statement On Pfo and Diving
Hochgeladen von
tonylee24Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Spums Position Statement On Pfo and Diving
Hochgeladen von
tonylee24Copyright:
Verfügbare Formate
Diving and Hyperbaric Medicine Volume 45 No.
2 June 2015 129
Joint position statement on persistent foramen ovale (PFO) and diving
South Pacific Underwater Medicine Society (SPUMS) and the United Kingdom Sports Diving
Medical Committee (UKSDMC)
David Smart, Simon Mitchell, Peter Wilmshurst, Mark Turner and Neil Banham
Abstract
(Smart D, Mitchell S, Wilmshurst P, Turner M, Banham N. Joint position statement on persistent foramen ovale (PFO) and
diving. South Pacific Underwater Medicine Society (SPUMS) and the United Kingdom Sports Diving Medical Committee
(UKSDMC). Diving and Hyperbaric Medicine. 2015 June;45(2):129-131.)
This consensus statement is the result of a workshop at the SPUMS Annual Scientific Meeting 2014 with representatives of
the UK Sports Diving Medical Committee (UKSDMC) present, and subsequent discussions including the entire UKSDMC.
Right-to-left shunt across a persistent or patent foramen ovale (PFO) is a risk factor for some types of decompression
illness. It was agreed that routine screening for PFO is not currently justifiable, but certain high risk sub-groups can be
identified. Divers with a history of cerebral, spinal, inner-ear or cutaneous decompression illness, migraine with aura, a
family history of PFO or atrial septal defect and those with other forms of congenital heart disease are considered to be
at higher risk. For these individuals, screening should be considered. If screening is undertaken it should be by bubble
contrast transthoracic echocardiography with provocative manoeuvres, including Valsalva release and sniffing. Appropriate
quality control is important. If a shunt is present, advice should be provided by an experienced diving physician taking into
account the clinical context and the size of shunt. Reduction in gas load by limiting depth, repetitive dives and avoiding
lifting and straining may all be appropriate. Divers may consider transcatheter device closure of the PFO in order to return
to normal diving. If transcatheter PFO closure is undertaken, repeat bubble contrast echocardiography must be performed
to confirm adequate reduction or abolition of the right-to-left shunt, and the diver should have stopped taking potent anti-
platelet therapy (aspirin is acceptable).
Key words
Patent foramen ovale (PFO); persistent foramen ovale; fitness to dive; decompression illness; transcatheter closure;
cardiovascular; health surveillance; medical society
Introduction Each statement is followed by identification of the level
of evidence in the literature for that statement and the
This statement was produced from a workshop held at supporting references.
the 43rd Annual Scientific Meeting of the South Pacific
Underwater Medicine Society (SPUMS) on 23 May 2014, Statement 1
and following consultation with the United Kingdom Sport
Diving Medical Committee (UKSDMC), two members of Routine screening for persistent foramen ovale (PFO) (also
which attended the meeting (PW and MT). The statement referred to as patent foramen ovale) at the time of dive
must be interpreted in consultation with a medical medical fitness assessment (either initial or periodic) is not
practitioner experienced in diving medicine and will be indicated (IV consensus of SPUMS/UKSDMC).
subject to review based on new evidence becoming available.
Statement 2
The levels of evidence defined for the position statement are
those promulgated in the 2015 ACCF/AHA Clinical Practice Consideration should be given to investigating for PFO under
Guideline Methodology Summit Report:1 any of the following circumstances:
A history of decompression illness (DCI) with cerebral,
Ia Evidence from meta-analysis of randomized controlled spinal, vestibulocochlear or cutaneous manifestations
trials; (IIa);28
Ib Evidence from at least one randomized controlled trial; A current or past history of migraine with aura (IIa);915
IIa Evidence from at least one well designed controlled A history of cryptogenic stroke (IIa); 16,17
trial which is not randomized; A history of PFO or atrial septal defect (ASD) in a first
IIb Evidence from at least one well designed experimental degree relative (IIa). 18,19
trial;
III Evidence from case, correlation, and comparative Statement 3
studies;
IV Evidence from a panel of experts. If screening for PFO is performed, then the following is
recommended:
130 Diving and Hyperbaric Medicine Volume 45 No. 2 June 2015
That testing is undertaken by centres well practiced in Statement 7
the technique (IV consensus of SPUMS/UKSDMC);
The screening must include bubble contrast, ideally Following closure of a PFO and before returning to diving,
combined with trans-thoracic echocardiogram (TTE) the diver requires a repeat bubble contrast echocardiogram
because this best facilitates cooperation with provocation demonstrating shunt closure, a minimum of three months
manoeuvres. Use of two-dimensional and colour-flow after the closure (III).11,21,22,24
echocardiography without bubble contrast is not
adequate (IIa);6,7,20 Statement 8
The screening must include the use of provocation
manoeuvres to promote right-to-left shunt including Diving should not be resumed until satisfactory closure
Valsalva release and sniffing as described in the of the PFO is confirmed, and the diver has ceased potent
supporting references (both undertaken when the right antiplatelet medication (aspirin is acceptable) (III).11,21,22,24
atrium is densely opacified by bubble contrast) (IIa).6,7
References
Statement 4
This list is restricted to the original case control studies and
Interpreting a positive PFO screening result: main reports. There have been many subsequent reports of
A spontaneous shunt without provocation or a large, the association of PFO and cryptogenic stroke.
provoked shunt is recognized as an unequivocal risk
factor for those forms of DCI listed in statement 2 1 Jacobs AK, Kushner FG, Ettinger SM, Guyton RA, Anderson
(IIa);68 JL, Ohman EM, et al. ACCF/AHA clinical practice guideline
Smaller shunts are associated with a lower but poorly methodology summit report: a report of the American College
of Cardiology Foundation/American Heart Association Task
defined risk of DCI. The significance of minor degrees
Force on Practice Guidelines. J Am Coll Cardiol. 2013;61:213-
of shunting needs to be interpreted in the clinical setting 65. [Available from: http://www.cardiosource.org].
that led to testing (IIa).68 2 Moon RE, Camporesi EM, Kisslo JA. Patent foramen ovale and
decompression sickness in divers. Lancet. 1989;333:513-4.
Statement 5 3 Wilmshurst PT, Byrne JC, Webb-Peploe MM. Relation
between interatrial shunts and decompression sickness in
Following diagnosis of a PFO considered likely to be divers. Lancet. 1989;334:1302-6.
associated with increased DCI risk, the diver may consider 4 Wilmshurst P, Davidson C, OConnell G, Byrne C. Role
the following options in consultation with a diving physician: of cardiorespiratory abnormalities, smoking and dive
characteristics in the manifestations of neurological
Stop diving (IV consensus of SPUMS/UKSDMC);
decompression illness. Clin Sci. 1994;86:297-303.
Dive more conservatively: There are various strategies 5 Germonpr P, Dendale P, Unger P, Balestra C. Patent foramen
that might be employed to reduce the risk of significant ovale and decompression sickness in sports divers. J Appl
venous bubble formation after diving, or the subsequent Physiol. 1998;84:1622-6.
right-to-left shunting of such bubbles across a PFO. 6 Wilmshurst P, Bryson P. Relationship between the clinical
The appropriateness of this approach, and the strategies features of neurological decompression illness and its causes.
chosen, need to be considered on an individual basis, Clin Sci 2000;99:65-75.
and in discussion with a diving medicine expert. 7 Wilmshurst PT, Pearson MJ, Walsh KP, Morrison WL, Bryson
Examples include: reducing dive times to well inside P. Relationship between right-to-left shunts and cutaneous
decompression illness. Clin Sci. 2001;100:539-42.
accepted no-decompression limits; restricting dive
8 Cantais E, Louge P, Suppini A, Foster P, Palmier B.
depths to less than 15 metres; performing only one Right-to-left shunt and risk of decompression illness with
dive per day; use of nitrox with air dive planning tools; cochleovestibular and cerebral symptoms in divers: case
intentional lengthening of a safety stop or decompression control study in 101 consecutive dive accidents. Crit Care
time at shallow stops; avoidance of heavy exercise and Med. 2003;31:84-8.
unnecessary lifting or straining for at least three hours 9 Del Sette M, Angeli S, Leandri M, Ferriero G, Bruzzone GL,
after diving (IV consensus of SPUMS/UKSDMC). Finocchi C, et al. Migraine with aura and right-to-left shunt
Close the PFO (III).7,11,2124 on transcranial Doppler; a case control study. Cerebrovasc
Dis. 1998;8:327-30.
10 Anzola GP, Magoni M, Guindani M, Rozzini L, Dalla Volta G.
Statement 6
Potential sources of cerebral embolism in migraine with aura.
A transcranial Doppler study. Neurology. 1999;52:1622-5.
The options outlined in statement 5 require careful 11 Wilmshurst PT, Nightingale S, Walsh KP, Morrison WL.
consideration of the risks and benefits and the clinical Effect on migraine of closure of cardiac right-to-left shunts
setting that led to screening (IV consensus of SPUMS/ to prevent recurrence of decompression illness or stroke or for
UKSDMC).24 haemodynamic reasons. Lancet. 2000;356:1648-51.
12 Wilmshurst P, Nightingale S. Relationship between migraine
Diving and Hyperbaric Medicine Volume 45 No.2 June 2015 131
and cardiac and pulmonary right-to-left shunts. Clin Sci. patent foramen ovale for the secondary prevention of recurrent
2001;100:215-20. paradoxical embolism in divers (IPG371 December 2010).
13 Schwerzmann M, Nedeltchev K, Lagger F, Mattle HP, [cited 2015 April 26]. Available from: http://www.nice.org.uk/
Windecker S, Meier B, et al. Prevalence and size of directly guidance/ipg371/documents/percutaneous-closure-of-patent-
detected patent foramen ovale in migraine with aura. foramen-ovale-for-the-secondary-prevention-of-recurrent-
Neurology. 2005;65:1415-8. paradoxical-embolism-in-divers-consultation-document
14 Wilmshurst PT, Pearson MJ, Nightingale S. Re-evaluation
of the relationship between migraine and persistent foramen Submitted: 31 October 2014
ovale and other right-to-left shunts. Clin Sci. 2005;108:365-7. Accepted: 30 April 2015
15 Wilmshurst P, Nightingale S, Pearson M, Morrison L,
Walsh K. Relation of atrial shunts to migraine in patients Acknowledgements
with ischaemic stroke and peripheral emboli. Am J Cardiol.
2006;98:831-3. We are grateful for the contribution of the participants at the
16 Lechat P, Mas JL, Lascault G, Loron P, Theard M, Klimczac workshop held at the 43rd Annual Scientific Meeting of the SPUMS
M, et al. Prevalence of patent foramen ovale in patients with and of the other members of the UKSDMC.
stroke. New Engl J Med. 1988;318:1148-52.
17 Webster MWI, Chancellor AM, Smith HJ, Swift DL, Sharpe Conflicts of interest
DN, Bass NM, et al. Patent foramen ovale in young stroke
patients. Lancet. 1988;332:11-12. MT acts as a consultant and proctor for St Jude Medical, Medtronic
18 Wilmshurst PT, Pearson MJ, Nightingale S, Walsh KP, and Edwards Lifesciences, as a consultant and lecturer for Gore
Morrison WL. Inheritance of persistent foramen ovale and Medical and performs PFO closures on private patients. The other
atrial septal defects and the relationship to familial migraine authors declare that they have no conflicts of interest.
with aura. Heart. 2004;90:1315-20.
19 Wilmshurst P, Panikkar J, Pearson M, Nightingale S. Relation David Smart1, Simon Mitchell2, Peter Wilmshurst3, Mark Turner4,
between inheritance of cyanotic congenital heart disease and Neil Banham5
persistent foramen ovale. Am J Cardiol. 2009;104:148-9.
1
20 Ha JW, Shin MS, Kang S. Enhanced detection of right-to-left School of Medicine, University of Tasmania and Department of
shunt through patent foramen ovale by transthoracic contrast Diving and Hyperbaric Medicine, Royal Hobart Hospital, Hobart,
echocardiography using harmonic imaging. Am J Cardiol. Tasmania, Australia
2
2001;87:669-71. Department of Anaesthesiology, University of Auckland and
21 Wilmshurst P, Walsh K, Morrison L. Transcatheter occlusion Auckland City Hospital, Auckland, New Zealand
3
of foramen ovale with a button device after neurological Cardiology Department, Royal Stoke University Hospital, Stoke-
decompression illness in professional divers. Lancet. on-Trent, Staffordshire, UK
4
1996;348:752-3. Bristol Heart Institute, Bristol, UK
5
22 Walsh KP, Wilmshurst PT, Morrison WL. Transcatheter Department of Hyperbaric Medicine, Fiona Stanley Hospital,
closure of patent foramen ovale using the Amplatzer septal Perth, Western Australia
occluder to prevent recurrence of neurological decompression
illness in divers. Heart. 1999;81:257-61. Address for correspondence:
23 Billinger M, Zbinden R, Mordasini R, Windecker S, Associate Professor David Smart
Schwerzmann M, Meier B, et al. Patent foramen ovale closure Department of Diving and Hyperbaric Medicine
in recreational divers: effect on decompression illness and Royal Hobart Hospital
ischaemic brain lesions during long-term follow-up. Heart. Hobart, Tasmania 7000
2011;97:1932-7. Australia
24 National Institute for Health and Care Excellence. NICE Phone: +61-(03)-6222-8193
interventional procedure guidance percutaneous closure of E-mail: <david.smart@dhhs.tas.gov.au>
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Short Cases Article 2014Dokument2 SeitenShort Cases Article 2014DrSajid BuzdarNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Prinsip Penyusunan Gigi Artifisial Kelompok 7Dokument53 SeitenPrinsip Penyusunan Gigi Artifisial Kelompok 7gilangNoch keine Bewertungen
- Lazarus Final Report 2011Dokument7 SeitenLazarus Final Report 2011ratzzuscaNoch keine Bewertungen
- BAby It's Cold Outside (Duet)Dokument4 SeitenBAby It's Cold Outside (Duet)tonylee24Noch keine Bewertungen
- IBS-Q For HCPDokument2 SeitenIBS-Q For HCPtonylee24Noch keine Bewertungen
- Jingle Bell Rock - SATBDokument6 SeitenJingle Bell Rock - SATBtonylee24100% (1)
- HBO2 For FlapsDokument8 SeitenHBO2 For Flapstonylee24Noch keine Bewertungen
- Hyperbaric Oxygen For Post Concussive SyndromeDokument28 SeitenHyperbaric Oxygen For Post Concussive Syndrometonylee24Noch keine Bewertungen
- Tone-Deafness - A New Disconnection Syndrome?Dokument14 SeitenTone-Deafness - A New Disconnection Syndrome?tonylee24Noch keine Bewertungen
- The Linked Dual Representation Model of Vocal Perception and ProductionDokument12 SeitenThe Linked Dual Representation Model of Vocal Perception and Productiontonylee24Noch keine Bewertungen
- Absolute Pitch: Prevalence, Ethnic Variation, and Estimation of The Genetic ComponentDokument18 SeitenAbsolute Pitch: Prevalence, Ethnic Variation, and Estimation of The Genetic Componenttonylee24Noch keine Bewertungen
- Action-Perception Mismatch in Tone-DeafnessDokument5 SeitenAction-Perception Mismatch in Tone-Deafnesstonylee24Noch keine Bewertungen
- Widespread Auditory Deficits in Tune DeafnessDokument29 SeitenWidespread Auditory Deficits in Tune Deafnesstonylee24Noch keine Bewertungen
- Left Hemisphere Diffusivity of The Arcuate Fasciculus: Influences of Autism Spectrum Disorder and Language ImpairmentDokument14 SeitenLeft Hemisphere Diffusivity of The Arcuate Fasciculus: Influences of Autism Spectrum Disorder and Language Impairmenttonylee24Noch keine Bewertungen
- Oxytocin Enhances Brain Function in Children With AutismDokument6 SeitenOxytocin Enhances Brain Function in Children With Autismtonylee24Noch keine Bewertungen
- The Cervical & Thoracic Spine - Mechanical Diagnosis & Therapy - Vol 2Dokument288 SeitenThe Cervical & Thoracic Spine - Mechanical Diagnosis & Therapy - Vol 2booksbearreading100% (6)
- Library GenesisDokument10 SeitenLibrary Genesismusic cisumNoch keine Bewertungen
- 4.BST GIM Post Summary Form - DermatologyDokument3 Seiten4.BST GIM Post Summary Form - Dermatologyjosiah masukaNoch keine Bewertungen
- Dermatomycological Profile of Patients in A Tertiary Care Hospital of Western MaharashtraDokument2 SeitenDermatomycological Profile of Patients in A Tertiary Care Hospital of Western MaharashtraApple IdeaNoch keine Bewertungen
- Nursing Care Plan Ineffective Breathing Pattern Hepatic MassDokument2 SeitenNursing Care Plan Ineffective Breathing Pattern Hepatic MassRheegell Ellar-Fuertes100% (3)
- Cirrus How To Read en OUS en 31 011 0002II Final3Dokument28 SeitenCirrus How To Read en OUS en 31 011 0002II Final3Alondra Verdugo GómezNoch keine Bewertungen
- MD Development PaediatrcsDokument102 SeitenMD Development PaediatrcsMuhammad Farooq SaeedNoch keine Bewertungen
- OP - Department Frequently Asked Question PDFDokument29 SeitenOP - Department Frequently Asked Question PDFMSA AvGeekNoch keine Bewertungen
- A Review On Peppermint OilDokument7 SeitenA Review On Peppermint OilElok Faiqotul UmmaNoch keine Bewertungen
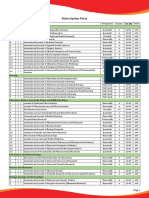
- Journal Subscription FormDokument3 SeitenJournal Subscription FormAkiNik Publications100% (1)
- Brachial Plexus Injuries in Adults PrefaceDokument2 SeitenBrachial Plexus Injuries in Adults PrefaceSatrio Bangun NegoroNoch keine Bewertungen
- Oral IrrigatorDokument30 SeitenOral IrrigatorNorman Tri Kusumo100% (1)
- Development Behaviour PediatricsDokument1.057 SeitenDevelopment Behaviour PediatricsoktisaripuniNoch keine Bewertungen
- MD Pediatrics Thesis TopicsDokument4 SeitenMD Pediatrics Thesis Topicslisadiazsouthbend100% (2)
- The Weber Collection. Vol. I: Greek Coins: Auriol Find Class, Hispania, Gallia, Britannia, Italy and Sicily / by L. ForrerDokument535 SeitenThe Weber Collection. Vol. I: Greek Coins: Auriol Find Class, Hispania, Gallia, Britannia, Italy and Sicily / by L. ForrerDigital Library Numis (DLN)Noch keine Bewertungen
- Clinical Standing DocumentDokument15 SeitenClinical Standing DocumentPrivat EtavirpNoch keine Bewertungen
- Updated For 75 BDSDokument55 SeitenUpdated For 75 BDSArfanNoch keine Bewertungen
- Review of Orthopaedic Trauma 2e 2013 PDF Unitedvrg PDFDokument568 SeitenReview of Orthopaedic Trauma 2e 2013 PDF Unitedvrg PDFWahyu Alamsyah DasopangNoch keine Bewertungen
- The POWER of WHEY & MCT For Critically Ill PatientsDokument46 SeitenThe POWER of WHEY & MCT For Critically Ill PatientsBayu Residewanto PutroNoch keine Bewertungen
- 2022 Springer Nature Fully Open Access JournalsDokument36 Seiten2022 Springer Nature Fully Open Access JournalsEntertainment HubNoch keine Bewertungen
- Oncology Scope of ServicesDokument2 SeitenOncology Scope of ServicesJaisurya SharmaNoch keine Bewertungen
- Strolling Match PDFDokument100 SeitenStrolling Match PDFHK15100% (1)
- Articulo . - El Autocuidado de Los Medicos en Formacion y Las Instituciones de SaludDokument10 SeitenArticulo . - El Autocuidado de Los Medicos en Formacion y Las Instituciones de SaludMIGUEL ANGEL RAMOS BORJANoch keine Bewertungen
- Hospital CEO COO Healthcare in New York City Resume Patrick SullivanDokument3 SeitenHospital CEO COO Healthcare in New York City Resume Patrick SullivanPatrickSullivan2Noch keine Bewertungen
- Playground Safety Fact SheetDokument4 SeitenPlayground Safety Fact Sheetapi-129796121Noch keine Bewertungen
- Hospital List in SADokument26 SeitenHospital List in SASudhakar KuppireddyNoch keine Bewertungen
- Airways. DR HUSNIDokument89 SeitenAirways. DR HUSNIFarah Fauziah RachmawatieNoch keine Bewertungen