Beruflich Dokumente
Kultur Dokumente
RCT - Uplift
Hochgeladen von
bapimirab654Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
RCT - Uplift
Hochgeladen von
bapimirab654Copyright:
Verfügbare Formate
new england
The
journal of medicine
established in 1812 october 9, 2008 vol. 359 no. 15
A 4-Year Trial of Tiotropium in Chronic Obstructive
Pulmonary Disease
Donald P. Tashkin, M.D., Bartolome Celli, M.D., Stephen Senn, Ph.D., Deborah Burkhart, B.S.N., Steven Kesten, M.D.,
Shailendra Menjoge, Ph.D., and Marc Decramer, M.D., Ph.D., for the UPLIFT Study Investigators*
A bs t r ac t
Background
Previous studies showing that tiotropium improves multiple end points in patients From the David Geffen School of Medi-
with chronic obstructive pulmonary disease (COPD) led us to examine the long- cine at the University of California, Los
Angeles (D.P.T.); Caritas St. Elizabeths
term effects of tiotropium therapy. Medical Center, Boston (B.C.); Glasgow
University, Glasgow, Scotland (S.S.);
Methods Boehringer Ingelheim Pharmaceuticals,
In this randomized, double-blind trial, we compared 4 years of therapy with either Ridgefield, CT (D.B., S.K., S.M.); and the
University of Leuven, Leuven, Belgium
tiotropium or placebo in patients with COPD who were permitted to use all respira- (M.D.). Address reprint requests to Dr.
tory medications except inhaled anticholinergic drugs. The patients were at least 40 Tashkin at the David Geffen School of
years of age, with a forced expiratory volume in 1 second (FEV1) of 70% or less after Medicine, University of California, Los An-
geles, 10833 Le Conte Ave., Los Angeles,
bronchodilation and a ratio of FEV1 to forced vital capacity (FVC) of 70% or less. CA 90095-1690, or at dtashkin@mednet.
Coprimary end points were the rate of decline in the mean FEV1 before and after ucla.edu.
bronchodilation beginning on day 30. Secondary end points included measures of
*Investigators in the Understanding Po-
FVC, changes in response on St. Georges Respiratory Questionnaire (SGRQ), exac- tential Long-Term Impacts on Function
erbations of COPD, and mortality. with Tiotropium (UPLIFT) trial are listed
in Supplementary Appendix 1, available
Results with the full text of this article at www.
nejm.org.
Of a total of 5993 patients (mean age, 658 years) with a mean FEV1 of 1.320.44
liters after bronchodilation (48% of predicted value), we randomly assigned 2987 to This article (10.1056/NEJMoa0805800) was
the tiotropium group and 3006 to the placebo group. Mean absolute improvements published at www.nejm.org on October
5, 2008.
in FEV1 in the tiotropium group were maintained throughout the trial (ranging
from 87 to 103 ml before bronchodilation and from 47 to 65 ml after bronchodila- N Engl J Med 2008;359:1543-54.
tion), as compared with the placebo group (P<0.001). After day 30, the differences Copyright 2008 Massachusetts Medical Society.
between the two groups in the rate of decline in the mean FEV1 before and after
bronchodilation were not significant. The mean absolute total score on the SGRQ
was improved (lower) in the tiotropium group, as compared with the placebo group,
at each time point throughout the 4-year period (ranging from 2.3 to 3.3 units,
P<0.001). At 4 years and 30 days, tiotropium was associated with a reduction in the
risks of exacerbations, related hospitalizations, and respiratory failure.
Conclusions
In patients with COPD, therapy with tiotropium was associated with improvements
in lung function, quality of life, and exacerbations during a 4-year period but did
not significantly reduce the rate of decline in FEV1. (ClinicalTrials.gov number,
NCT00144339.)
n engl j med 359;15 www.nejm.org october 9, 2008 1543
The New England Journal of Medicine
Downloaded from nejm.org on January 22, 2013. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
P
rospective studies testing effects forced vital capacity (FVC) and slow vital capacity
on the progression of chronic obstructive (SVC); health-related quality of life, as measured
pulmonary disease (COPD) through the eval- by the total score on St. Georges Respiratory
uation of the slope of the forced expiratory volume Questionnaire (SGRQ), in which scores range
in 1 second (FEV1) have not shown that inhaled from 0 to 100, with lower scores indicating im-
short-acting anticholinergic drugs, inhaled corti- provement and a change of 4 units or more con-
costeroids, or N-acetylcysteine alter this marker sidered to be clinically meaningful; exacerbations
of disease progression.1-7 To date, only smoking of COPD (as defined below) and related hospital-
cessation has prospectively been shown to alter the izations; and the rate of death from any cause and
rate of decline of FEV1 in patients with COPD.2 from lower respiratory conditions. Details regard-
Tiotropium is a once-daily, inhaled anticho- ing secondary end points are provided in Supple-
linergic drug that provides at least 24-hour im- mentary Appendix 3.
provements in airflow and hyperinflation in pa- Patients received either 18 g of tiotropium
tients with COPD.8-10 Clinical trials lasting 6 weeks or a matching placebo once daily, delivered
to 12 months have shown improvements in exer- through the HandiHaler inhalation device (Boeh-
cise tolerance, health-related quality of life, and ringer Ingelheim). All respiratory medications,
rates of dyspnea and exacerbations.8-13 A retro- except other inhaled anticholinergic drugs, were
spective analysis of 1-year, placebo-controlled permitted during the trial. Smoking cessation
trials indicated that tiotropium had the potential programs were offered to all patients before ran-
to slow the rate of decline in FEV1.14 domization, and self-reported smoking behavior
Given previous favorable clinical outcomes, we was recorded at each visit. At the end of the
designed this trial to prospectively extend these study, all patients were provided with and asked
observations to 4 years.15 In the Understanding to take 40 g of ipratropium (two inhaler actua-
Potential Long-Term Impacts on Function with tions) four times daily and to return for a final
Tiotropium (UPLIFT) trial, we tested whether assessment 30 days later.
tiotropium would reduce the rate of decline in
FEV1 in patients with COPD who were permitted Patients
therapy other than other inhaled anticholinergic Patients were recruited at 490 investigational cen-
drugs, according to current COPD guidelines. ters in 37 countries. Criteria for participation in-
We evaluated the long-term effects of tiotropium cluded a diagnosis of COPD, an age of 40 years or
therapy on the clinically important outcomes of more, a smoking history of at least 10 pack-years,
health-related quality of life, exacerbations, re- a postbronchodilator FEV1 of 70% or less of the
lated hospitalizations, and mortality. predicted value, and an FEV1 of 70% or less of the
FVC (after supervised administration of 80 g of
Me thods ipratropium [four actuations], followed by 400 g
of albuterol [four actuations] 60 minutes later).16
Study Design Key exclusion criteria were a history of asthma, a
Details of the study design were reported previ- COPD exacerbation or respiratory infection with-
ously by Decramer et al.15 and are summarized in 4 weeks before screening, a history of pulmo-
below. The protocol is provided in Supplementary nary resection, use of supplemental oxygen for
Appendix 2, available with the full text of this more than 12 hours per day, and the presence of
article at www.nejm.org. a coexisting illness that could preclude participa-
The study was a 4-year, randomized, double- tion in the study or interfere with the study re-
blind, placebo-controlled, parallel-group trial in- sults. The protocol was approved by the ethics
volving patients with moderate-to-very-severe committee at each center, and all patients pro-
COPD.15 The two coprimary end points were the vided written informed consent.
yearly rate of decline in the mean FEV1 before the
use of a study drug and short-acting bronchodi- Procedures
lators in the morning (prebronchodilator) and af- After a screening period, eligible patients were
ter the use of a study drug (postbronchodilator) randomly assigned in a 1:1 ratio to receive either
from day 30 (steady state) until completion of tiotropium or placebo with the use of centralized
double-blind treatment. Secondary outcome mea- randomization in blocks of four, stratified accord-
sures included the rate of decline in the mean ing to site. After randomization, clinic visits oc-
1544 n engl j med 359;15 www.nejm.org october 9, 2008
The New England Journal of Medicine
Downloaded from nejm.org on January 22, 2013. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
Tiotropium in Chronic Obstructive Pulmonary Disease
curred at 1 month and 3 months and then every and a representative of Pfizer (see Supplementary
3 months throughout the 4-year study period. Appendix 4). The first draft of the manuscript
Spirometry was performed according to Amer- was written by an academic investigator, and the
ican Thoracic Society guidelines17 at randomiza- final content of the manuscript was developed
tion, at the 1-month visit, at visits every 6 months collaboratively by all authors. Statistical analyses
throughout the study period, and at a follow-up were performed by employees of Boehringer In-
visit approximately 30 days after the end of the gelheim. All authors had full access to the data
study. Before spirometry testing, respiratory med- and vouch for the accuracy and completeness of
ications were withheld according to the follow- the data and the analyses.
ing schedule: study drug, 24 hours; morning dose
of inhaled corticosteroids, 12 hours; short-acting Statistical Analysis
beta-agonists, 8 hours; short-acting (twice-daily The number of patients needed for the study was
or four-times-daily) theophyllines and long-act- based on the assumption of a standard deviation
ing beta-agonists (including fixed combination of 90 ml in the rate of decline in the mean FEV1
with inhaled corticosteroids), 24 hours; and once- during the 4-year period2 to detect a difference of
daily theophyllines, 48 hours. Prebronchodilator 15 ml between the tiotropium group and the pla-
spirometry was performed initially, followed im- cebo group, with a power of more than 90% at
mediately by the blinded administration of a study a significance level of 5% with the use of a two-
drug. Immediately thereafter, all patients received sided test. The sample size was also based on an
80 g of ipratropium (four inhaler actuations), assumption that it would not be possible to per-
followed 60 minutes later by 400 g of albuterol form a complete evaluation of 35% of patients be-
(four inhaler actuations). Thirty minutes after the cause of early discontinuation. The sample size
administration of albuterol, spirometry was again was chosen to be sufficiently large to undertake
performed. Sites were provided with identical subgroup analyses of the primary end point in
spirometry equipment and study-specific software. smokers, who were assumed to comprise about
A centralized quality-assurance review of all spi 40% of enrolled patients. The other planned sub-
rometry data was performed during the study.15 group analyses included the variables of age, sex,
Health-related quality of life was measured with severity of COPD, region, reversibility, body-mass
the use of the SGRQ before prebronchodilator index, and concomitant use of medication. In ad-
spirometry testing at baseline and every 6 months.18 dition, we conducted a post hoc subgroup analy-
Reports of adverse events were collected at each sis comparing patients in each study group who
visit. were or were not receiving inhaled corticosteroids
Exacerbations were defined as an increase in or or long-acting beta-agonists at baseline.
the new onset of more than one respiratory symp- The two coprimary end points were analyzed
tom (cough, sputum, sputum purulence, wheez- with the use of a normal random-effects model
ing, or dyspnea) lasting 3 days or more and requir- in which the mean FEV1 changed linearly after
ing treatment with an antibiotic or a systemic day 30 for each patient, the intercepts and slopes
corticosteroid. Data regarding exacerbations and among patients were assumed to be random with
related hospitalizations were collected on study- an arbitrary covariance matrix, and the treatment
specific case-report forms at every visit. An inde- effect was fixed.19 The same model was used for
pendent data and safety monitoring committee the secondary end points of FVC and SVC (from
reviewed data throughout the trial (for details, day 30 until study completion) and the total
see Supplementary Appendixes 2 and 4). score on the SGRQ (from 6 months until study
completion). All patients who underwent ran-
Study Oversight domization and received a study drug and who
The design of the trial, the monitoring of the had at least three post-randomization data points
trial conduct, the approval of the statistical analy- (at least two for the SGRQ) were included in the
ses, the review and interpretation of the data, the analyses. We used likelihood-based methods to
writing of the manuscript, and the decision to handle missing data for the random coefficient
publish the manuscript involved a joint advisory regression analysis, and therefore no imputation
committee composed of four academic research- was deemed necessary. A sensitivity analysis was
ers (three investigators and a statistician), three conducted for the rate of decline in the mean
researchers employed by Boehringer Ingelheim, FEV1, with adjustment for baseline FEV1, smoking
n engl j med 359;15 www.nejm.org october 9, 2008 1545
The New England Journal of Medicine
Downloaded from nejm.org on January 22, 2013. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
status, age, sex, and height. Analyses of hetero- 1435 days in the placebo group. A higher propor-
geneity of subgroups were assessed by testing tion of patients did not complete at least 45
for interaction between study-group slope and months of treatment in the placebo group (44.6%)
each baseline factor. The yearly rates of decline than in the tiotropium group (36.2%, P<0.001)
from baseline to 30 days after the discontinuation (Fig. 2A). The majority of discontinuations were
of a study drug were analyzed using the Wilcoxon due to adverse events.
rank-sum test. The mean effects at various visits Baseline characteristics and concomitant use
were compared in the two study groups with the of respiratory medications were similar in the
use of repeated-measures analysis of covariance two study groups (Table 1). The mean age was
without imputation of missing values. SGRQ data 658 years among the patients, of whom 75%
from Turkey were excluded owing to incorrect were men and 30% were current smokers. The
validation of the questionnaire. mean prebronchodilator FEV1 was 1.100.40 liters
The times to the first exacerbation and asso- (39% of the predicted value), and the mean post-
ciated hospitalization in the two study groups bronchodilator FEV1 was 1.320.44 liters (48%
were compared with the use of log-rank tests and of the predicted value). The mean increase in FEV1
were prespecified as the key secondary analyses. after maximal bronchodilation was 2318%.21
Cox regression was used to derive hazard ratios. Patients whose disease was classified as stage II,
KaplanMeier curves of the probability of no III, or IV, according to criteria of the Global
exacerbation and related hospitalization were Initiative for Chronic Obstructive Lung Disease
calculated. The number of events and event days (GOLD), comprised 46%, 44%, and 9% of pa-
were compared between study groups with the tients, respectively.1 The mean baseline prebron-
use of Poisson regression with correction for chodilator FEV1 was lower in patients who discon-
treatment exposure and overdispersion.20 tinued a study drug than in those who completed
All patients who received a study drug were the study period (37% vs. 41% of the predicted
included in the analysis of safety and discontinu- value, P<0.001). More than 90% of patients were
ations. Incidence rates were computed as the receiving respiratory medications at baseline.
number of patients with events divided by the During the study period, 26% of patients
time at risk. Time-to-event analyses were per- changed their smoking behavior. On at least one
formed with the use of the log-rank test; hazard clinic visit, 74% of patients reported having re-
ratios were calculated with the use of Cox re- ceived inhaled corticosteroids, 72% long-acting
gression. beta-agonists, and 46% a fixed combination of
Analyses were performed with the use of SAS the two.
software, version 8.2 (SAS Institute). All reported
P values are two-sided and were not adjusted for Rate of Decline in Lung Function
multiple testing. The scientific steering commit- The rate of decline in the mean postbronchodila-
tee (Joint Advisory Committee) added a number tor FEV1 was greater in patients who prematurely
of secondary end points and updated the analy- discontinued a study drug (554 ml per year in
ses during the course of the trial while its mem- the tiotropium group and 574 ml per year in the
bers were unaware of study-group assignments. placebo group), as compared with those who
Details of the statistical analysis plan are pro- completed the study period (381 ml per year in
vided in Supplementary Appendix 3. the tiotropium group and 401 ml per year in the
placebo group).
R e sult s There were no significant differences between
study groups in the rate of decline in the mean
Study Population values for FEV1 and FVC either before or after
Patients were recruited from January 2003 through bronchodilation from day 30 to the end of study-
March 2004; the study ended in February 2008. drug treatment (Table 2; for SVC measures, see
Of the 8020 patients who were recruited, 5993 Supplementary Appendix 5). In the tiotropium
underwent randomization (Fig. 1). Of these pa- group, the mean values for FEV1 and FVC before
tients, 4383 (73%) completed 2 years, 3891 (65%) and after bronchodilation showed significant im-
completed 3 years, and 3569 (60%) completed at provements that were maintained at all time
least 45 months. The median duration of treat- points after randomization (Fig. 2B and 2C). Mean
ment was 1436 days in the tiotropium group and improvements in FEV1 in the tiotropium group,
1546 n engl j med 359;15 www.nejm.org october 9, 2008
The New England Journal of Medicine
Downloaded from nejm.org on January 22, 2013. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
Tiotropium in Chronic Obstructive Pulmonary Disease
8020 Patients were assessed
for eligibility
2027 Withdrew during
screening or did not meet
entry criteria
5993 Underwent randomization
(487 centers, 37 countries)
2987 Were assigned to receive 3006 Were assigned to receive
tiotropium placebo
1 Did not receive
0 Did not receive placebo
tiotropium
2986 Received tiotropium plus 3006 Received placebo plus
usual respiratory medication usual respiratory medication
1099 Discontinued tiotro-
1358 Discontinued placebo
pium
746 Had adverse event
627 Had adverse event
403 Withdrew consent
300 Withdrew consent
75 Had protocol non-
48 Had protocol non-
compliance
compliance
76 Were lost to follow-
64 Were lost to follow-
up
up
58 Had other reason
60 Had other reason
1887 Completed the study 1648 Completed the study
Tiotropium analysis sets Placebo analysis sets
2557 Prebronchodilator 2413 Prebronchodilator
spirometry spirometry
2554 Postbronchodilator 2410 Postbronchodilator
spirometry spirometry
Figure 1. Enrollment and Outcomes.
Patients with three or more measurements of pulmonary function after day 30 were included in the analysis of lung
AUTHOR: Tashkins RETAKE 1st
function. Patients in the study wereICM
permitted to use all respiratory medications except
2nd other inhaled anticholinergic
FIGURE: 1 of 3
drugs. After the initial assessment,REG F patient
one underwent randomization twice. 3rd
CASE Revised
EMail Line 4-C SIZE
ARTIST: ts H/T H/T
as compared with the placebo Enon group, ranged served
Combo in favor of tiotropium,
33p9 as compared with
from 87 to 103 ml before bronchodilation and placebo
AUTHOR, PLEASE NOTE: (403 ml in the tiotropium group and
from 47 to 65 ml after bronchodilation (P<0.001).
Figure has been redrawn 473
and typeinhasthe placebo
been reset. group, P=0.046) in the sub-
Please check carefully.
Adjustments for baseline FEV1, smoking status, group of 1554 patients who were not receiving
age, sex, and height had similar results.
JOB: 35915 either inhaledISSUE:corticosteroids
10-09 -08 or long-acting beta-
The prespecified subgroup analyses revealed agonists at baseline.
no significant heterogeneity in the effect of tio Among 3421 patients from baseline until 30
tropium according to the baseline variables exam- days after treatment discontinuation, the median
ined (Supplementary Appendix 6). In a post hoc rate of decline in prebronchodilator FEV1 did not
analysis, between-group differences in the rate differ significantly between the tiotropium group
of decline in postbronchodilator FEV1 were ob- (15 ml per year) and the placebo group (17 ml per
n engl j med 359;15 www.nejm.org october 9, 2008 1547
The New England Journal of Medicine
Downloaded from nejm.org on January 22, 2013. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
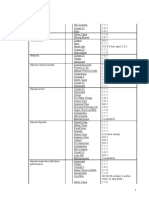
Table 1. Baseline Characteristics of the Patients.*
Characteristic Tiotropium (N=2986) Placebo (N=3006)
Male sex (%) 75.4 73.9
Age (yr) 64.58.4 64.58.5
Body-mass index 26.05.1 25.95.1
Smoking status
Current smoker (%) 29.3 29.9
Smoking history (pack-yr) 49.028.0 48.427.9
Duration of COPD (yr) 9.97.6 9.77.4
Baseline spirometry
Before bronchodilation
FEV1 (liters) 1.100.40 1.090.40
FEV1 (% of predicted value) 39.512.0 39.311.9
FVC (liters) 2.630.81 2.630.83
Ratio of FEV1 to FVC 42.410.5 42.110.5
After bronchodilation
FEV1 (liters) 1.330.44 1.320.44
FEV1 (% of predicted value) 47.712.7 47.412.6
FVC (liters) 3.090.86 3.090.90
Ratio of FEV1 to FVC 43.610.8 43.310.7
GOLD stage (%)
II 46 45
III 44 44
IV 8 9
SGRQ total score (units) 45.717.0 46.017.2
Respiratory medication (%)
Any 93.4 93.1
Inhaled anticholinergic
Short-acting 44.9 44.1
Long-acting 2.0 1.6
Inhaled 2-agonist
Short-acting 68.5 68.1
Long-acting 60.1 60.1
Corticosteroid
Inhaled 61.6 61.9
Oral 8.4 8.3
Theophylline compound 28.4 28.5
Mucolytic agent 7.4 6.9
Leukotriene-receptor antagonist 3.3 3.1
Supplemental oxygen 2.3 1.9
* Plusminus values are means SD. The body-mass index is the weight in kilograms divided by the square of the height
in meters. FEV1 denotes forced expiratory volume in 1 second, FVC forced vital capacity, and SGRQ St. Georges
Respiratory Questionnaire.
Data were missing in this category for 2% of patients. The enrollment of three patients with stage I disease, according
to criteria of the Global Initiative for Chronic Obstructive Lung Disease (GOLD), represented a protocol violation, but
data from these patients were included in the study.
Data are for 2888 patients in the tiotropium group and 2909 patients in the placebo group. Scores on the SGRQ range from
0 to 100, with lower scores indicating improvement; a change of 4 units or more is considered to be clinically meaningful.
This medication was used either alone or as a fixed combination.
1548 n engl j med 359;15 www.nejm.org october 9, 2008
The New England Journal of Medicine
Downloaded from nejm.org on January 22, 2013. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
Tiotropium in Chronic Obstructive Pulmonary Disease
A Probability of Discontinuation B FEV1
50 1.50
Placebo
Probability of Discontinuation (%)
*
After Bronchodilation
*
40 1.40 *
*
* Tiotropium
*
* (N=2516)
30 1.30 *
Tiotropium *
FEV1 (liters)
* * *
20 1.20 * * Placebo
* * (N=2374)
* *
10 1.10 Tiotropium
Hazard ratio, 0.89 (95% CI, 0.850.94) (N=2494)
P<0.001 Before Bronchodilation
0 1.00 Placebo
0 6 12 18 24 30 36 42 48 (N=2363)
0.00
Month 01 6 12 18 24 30 36 42 48
No. at Risk Month
Tiotropium 2986 2726 2565 2432 2293 2177 2060 1970 Day 30
Placebo 3006 2618 2418 2249 2090 1947 1831 1723
C FVC D SGRQ Total Score
3.30 50
* After Bronchodilation
* Placebo
*
* Tiotropium (N=2337)
SGRQ Total Score (units)
3.10 *
* * (N=2516)
Improvement 45
FVC (liters)
2.90 * * Placebo *
* * * Tiotropium
* (N=2374) * *
* * 40 * (N=2478)
* * *
2.70 * *
Tiotropium
(N=2494)
2.50 Before Bronchodilation 35
Placebo
(N=2363)
0.00 0
01 6 12 18 24 30 36 42 48 0 6 12 18 24 30 36 42 48
Month Month
Day 30
Figure 2. Probability of Treatment Discontinuation, Mean FEV1 and FVC before and after Bronchodilation, and Scores for Health-Related
Quality of Life.
Panel A shows the probability of treatment discontinuation
ICM
AUTHOR:inTashkin
the tiotropium groupRETAKE
and the placebo
1st group. Panel B shows the estimated
mean forced expiratory volume in 1 second (FEV REG F1) before
FIGURE:and 3 bronchodilation from day2nd
2 ofafter 30 to the end of the study. Before broncho-
3rd
dilation, the annual rates of decline were the CASE
same in the tiotropium group and the placebo Revised
group: 301 ml per year. After bronchodila-
tion, the annual rate of decline was 401 ml per year in the tiotropium group,
Line as
4-C compared with 421 ml per year in the placebo group.
EMail SIZE
Panel C shows the mean forced vital capacity (FVC)ARTIST:
before andts after H/Tbronchodilation
H/T from
36p6day 30 to the end of the study. Before bron-
Enon
Combo group and 393 in the placebo group. After bronchodila-
chodilation, the annual rate of decline was 433 ml per year in the tiotropium
tion, the annual rates of decline were the same in the tiotropium
AUTHOR, group and the
PLEASE placebo group: 613 ml per year. Panel D shows the health-
NOTE:
related quality-of-life score from month 6 to the Figure
end ofhasthebeen redrawn
study, and type has
as measured onbeen reset.
St. Georges Respiratory Questionnaire (SGRQ), which
Please check carefully.
ranges from 0 to 100, with lower scores indicating improvement. The annual rate of change was 1.250.09 units per year in the tiotropi-
um group, as compared with 1.210.09 units in the placebo group. Repeated-measure analysis of variance was used to estimate means.
JOB: 35915 ISSUE: 10-09-08
Means are adjusted for baseline measurements. For FEV1 and FVC, patients with three or more acceptable pulmonary-function tests
after day 30 and no missing baseline values were included in the analysis. For the SGRQ total score, patients with two or more accept-
able scores after month 6 and no missing baseline values were included in the analysis. The I bars represent standard errors, and the
horizontal dashed lines represent baseline levels. Asterisks denote P<0.001, the dagger P=0.002, and the double dagger P=0.04.
n engl j med 359;15 www.nejm.org october 9, 2008 1549
The New England Journal of Medicine
Downloaded from nejm.org on January 22, 2013. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Table 2. Annual Rates of Decline in FEV1 and FVC before and after Bronchodilation and Scores on Health-Related Quality of Life.*
Difference between Tiotropium P
Variable Tiotropium Placebo and Placebo (95% CI) Value
Patients Mean Decline Patients Mean Decline
no. ml/yr no. ml/yr
FEV1
Before bronchodilation 2557 301 2413 301 02 (4 to 4) 0.95
After bronchodilation 2554 401 2410 421 22 (6 to 2) 0.21
FVC
Before bronchodilation 2557 433 2413 393 44 (4 to 12) 0.30
After bronchodilation 2554 613 2410 613 14 (7 to 9) 0.84
Total SGRQ score 2505 1.250.09 2362 1.210.09 0.040.13 (0.2 to 0.3) 0.78
* Plusminus values are means SE. Values for the rate of decline in forced expiratory volume in 1 second (FEV1) and forced vital capacity
(FVC) are expressed as milliliters per year. Values were measured from day 30 until the end of the study (including 30 days after the discon-
tinuation of treatment). Patients with three or more measurements after day 30 were included in the analysis of lung function.
P values are unadjusted.
Values for the health-related quality-of-life score on St. Georges Respiratory Questionnaire (SGRQ) are expressed in units per year. Scores on
the SGRQ range from 0 to 100, with an increase in the score indicating a decline in quality of life; a change of 4 units or more is considered to
be clinically meaningful. Patients with two or more measurements after month 6 were included in the analysis of the SGRQ.
year) (P=0.25). However, among 3418 patients median of 16.7 months (95% CI, 14.9 to 17.9) in
who had technically acceptable postbronchodila- the tiotropium group and 12.5 months (95% CI,
tor spirometry, there was a significant difference 11.5 to 13.8) in the placebo group. Tiotropium
in favor of tiotropium in the median rate of de- was also associated with a significant delay in
cline in postbronchodilator FEV1 (27 ml per year the time to the first hospitalization for an exac-
in the tiotropium group, as compared with 32 ml erbation. Since hospitalizations for exacerbations
per year in the placebo group; P=0.01). occurred in less than 50% of patients, a median
time to the first event cannot be calculated. In the
Health-Related Quality of Life tiotropium group, the associated hazard ratios
Significant differences in favor of tiotropium were were 0.86 (95% CI, 0.81 to 0.91) and 0.86 (95% CI,
observed at all time points for the mean absolute 0.78 to 0.95), respectively. Tiotropium was also
change in the SGRQ total score (ranging from 2.3 associated with a reduction in the mean number
to 3.3 units, P<0.001), although the differences on of exacerbations of 14% (P<0.001) (Fig. 3A and
average were below what is considered to have Supplementary Appendix 7). The mean numbers
clinical significance (Fig. 2D). The overall mean of exacerbations leading to hospitalizations were
between-group difference in the SGRQ total infrequent and did not differ significantly be-
score at any time point was 2.7 (95% confidence tween the two study groups (Table 3).
interval [CI], 2.0 to 3.3) in favor of tiotropium
(P<0.001). A higher proportion of patients in the Mortality
tiotropium group than in the placebo group had Data regarding vital status were systematically
an improvement of 4 units or more in the SGRQ requested for patients who prematurely discon-
tinued study participation on a recorded date de-
total scores from baseline at 1 year (49% vs. 41%),
2 years (48% vs. 39%), 3 years (46% vs. 37%), and termined as 4 years from the first day of admin-
4 years (45% vs. 36%) (P<0.001 for all compari- istration of a study drug. Data regarding deaths
sons). There were no significant between-group extending beyond 4 years (up to and beyond 1470
differences in the rate of decline in SGRQ scores days) were not systematically collected but were
from 6 months to the end of the study (Table 2). occasionally received. Every effort was made to en-
sure that vital-status data were full and complete
Exacerbations up to 4 years, as described. Vital-status informa-
Tiotropium was associated with a significant de- tion (at least 45 months of follow-up, including
lay in the time to the first exacerbation, with a patients who discontinued treatment) was known
1550 n engl j med 359;15 www.nejm.org october 9, 2008
The New England Journal of Medicine
Downloaded from nejm.org on January 22, 2013. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
Tiotropium in Chronic Obstructive Pulmonary Disease
for 98% of patients in the tiotropium group and
A COPD Exacerbation
97% in the placebo group. During a period of
80
4 years plus 30 days (1470 days) included in the
intention-to-treat analysis, 941 patients died: Placebo Tiotropium
Probability of Exacerbation (%)
14.9% in the tiotropium group and 16.5% in the 60
placebo group (hazard ratio, 0.89; 95% CI, 0.79
to 1.02) (Fig. 3B). For the 4-year, protocol-defined
study period up to day 1440, among patients for 40
whom vital-status information was available, 921
patients died: 14.4% in the tiotropium group and
16.3% in the placebo group (hazard ratio, 0.87; 20 Hazard ratio, 0.86
(95% CI, 0.810.91)
95% CI, 0.76 to 0.99). P<0.001
0
Adverse Events 0 6 12 18 24 30 36 42 48
Safety was monitored through the collection of Month
reports of adverse events, serious adverse events, No. at Risk
and fatal events while patients were receiving a Tiotropium 2986 1996 1496 1223 983 838 709 610 26
study drug (including the last day of a study drug Placebo 3006 1815 1284 1010 776 634 545 460 21
plus 30 days). Adverse events were reported by
B Death from Any Cause
92.6% of the tiotropium group and 92.3% of the 20
placebo group. The proportions of serious ad-
verse events were 51.6% in the tiotropium group Probability of Death from Any Cause (%)
and 50.2% in the placebo group. Fatal events oc- 15
Placebo
curred in 381 patients (12.8%) in the tiotropium
group and 411 (13.7%) in the placebo group
Tiotropium
(hazard ratio, 0.84; 95% CI, 0.73 to 0.97). 10
In the tiotropium group, as compared with
the placebo group, the most common adverse
5
events were due to lower respiratory causes, in- Hazard ratio, 0.89
(95% CI, 0.791.02)
cluding COPD exacerbations (64.8% and 66.1%, P=0.09
respectively; relative risk, 0.84; 95% CI, 0.79 to 0
0.89), pneumonia (14.5% and 13.9%; relative risk, 0 6 12 18 24 30 36 42 48
0.96; 95% CI, 0.84 to 1.10), and dyspnea (12.2% Month
and 14.7%; relative risk, 0.75; 95% CI, 0.65 to No. at Risk
0.86). Respiratory failure developed in 88 patients Tiotropium 2986 2948 2899 2851 2785 2721 2646 2574 2306
Placebo 3006 2961 2903 2836 2772 2696 2624 2523 2249
in the tiotropium group and in 120 in the pla-
cebo group (relative risk, 0.67; 95% CI, 0.51 to Figure 3. KaplanMeier Estimates of the Probability of COPD Exacerbation
0.89). Myocardial infarction developed in 67 pa- and Death from Any Cause.
tients in the tiotropium group and 85 in the KaplanMeierICM curvesAUTHOR:
show theTashkin
cumulative incidenceRETAKEestimate 1stof the proba-
2nd
bility of COPDREG F FIGURE:(Panel
exacerbation 3 of 3 A) and of death from any cause at day
placebo group (relative risk, 0.73; 95% CI, 0.53 3rd
1470 for all patients
CASE for whom data were available regarding Revised vital status
to 1.00), and stroke developed in 82 in the (Panel B). TheEMail
numbers of patients who Line 4-C to receive
continued SIZE a study drug
tiotropium group and 80 in the placebo group (including those
ARTIST: ts H/T
at 30 days after the last
Enon
H/Tlisted for
dose) are each time point,
22p3
Combo
(relative risk, 0.95; 95% CI, 0.70 to 1.29). Adverse with the study period truncated at 48 months. All patients who received at
AUTHOR, PLEASE NOTE:
events consistent with the known safety profile least one dose of a study drug were included in the analysis. P values were
Figure has been redrawn and type has been reset.
calculated with use of the log-rank test.
of tiotropium, such as dry mouth and constipa- Please check carefully.
tion, were observed.22,23
JOB: 35915 ISSUE: 10-09-08
Serious adverse events reported by more than tive heart failure, COPD exacerbation, dyspnea,
1% of patients in either study group were either or respiratory failure. Serious adverse events ac-
cardiac or respiratory in nature (Table 4). The cording to organ system and adverse events that
incidence of such serious adverse events was were reported by more than 3% of patients in
lower in the tiotropium group than in the pla- either of the study groups are provided in Sup-
cebo group, including a reduced risk of conges- plementary Appendix 8.
n engl j med 359;15 www.nejm.org october 9, 2008 1551
The New England Journal of Medicine
Downloaded from nejm.org on January 22, 2013. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Table 3. Exacerbations of COPD and Related Hospitalizations.*
Relative Risk for Tiotropium
Variable Tiotropium Placebo vs. Placebo (95% CI) P Value
Exacerbation
Per patient-year no. 0.730.02 0.850.02 0.86 (0.810.91) <0.001
Leading to hospitalization no. per 0.150.01 0.160.01 0.94 (0.821.07) 0.34
patient-year
Days per patient-year 12.110.32 13.640.35 0.89 (0.830.95) 0.001
Hospitalization days per patient-year 3.170.17 3.130.17 1.01 (0.871.18) 0.86
Patients with exacerbation no. (%)
Total 2001 (67.0) 2049 (68.2) NA 0.35
Leading to hospitalization 759 (25.4) 811 (27.0) NA 0.18
* Plusminus values are means SE. NA denotes not applicable.
The relative risks in this category were calculated with the use of Poisson regression corrected for treatment exposure
and overdispersion.
The comparisons in this category were calculated with the use of Fishers exact test.
Discussion are also smaller than those observed in the post
hoc analysis of lung function in the Towards
In our study, we showed that in the presence of a Revolution in COPD Health (TORCH) trial
freely prescribed respiratory medications (i.e., in- (ClinicalTrials.gov number, NCT00268216).24
haled long-acting beta-agonists, inhaled cortico There are several potential explanations for the
steroids, and theophyllines) other than another in- discrepancies in the rate of decline in our study,
haled anticholinergic agent, tiotropium (at a dose as compared with those in previous studies. First,
of 18 g once daily) did not alter the rate of de- our study design allowed for prescription of all
cline in the mean FEV1 in patients with COPD. respiratory therapies at the discretion of physi-
However, lung function was significantly better cians, with the exception of another inhaled anti-
than in the placebo group throughout the trial, cholinergic agent. It is therefore possible that the
and there were improvements in health-related medical care that patients received during our
quality of life and the rate of exacerbations. study, including both short-acting and long-acting
As compared with results of previous long- inhaled respiratory medications and aggressive
term, prospective studies, the yearly rate of de- treatment of exacerbations, differed from that in
cline in FEV1 that we observed was numerically earlier trials and, as a whole, contributed to the
lower than the rates of decline reported previ generally lower rates of decline. However, such
ously.2-6 Prospective interventional studies that factors have not been definitively shown. Second,
were designed to examine the decline in FEV1 in our study, a higher proportion of patients with
such as the European Respiratory Society sustained abstinence from smoking tobacco may
Study on Chronic Obstructive Pulmonary Disease have resulted in a lower mean rate of decline. In
(EUROSCOP), the Inhaled Steroids in Obstructive our study, self-reports of smoking behavior indi-
Lung Disease in Europe (ISOLDE) trial, the Lung cated that only 30% of patients were current
Health Study II, and the Bronchitis Randomized smokers at baseline, as compared with 38 to 90%
on NAC [N-acetylcysteine] CostUtility Study in other studies.3-6 Third, other factors, such as
(BRONCUS) showed a decline in postbroncho- differences in study design, selection of patients,
dilator rates ranging from 44 to 57 ml per year and regional factors, could also account for dis-
in the active-treatment groups and 47 to 69 ml crepancies. In interpreting the results of our
per year in the placebo groups.3-6 In our study, study, one should consider that the rates of de-
the decline in lung function averaged 30 ml per cline in our study are similar to those reported
year before bronchodilation and 41 ml per year for healthy nonsmokers and sustained quitters
after bronchodilation in the two study groups, with mild-to-moderate COPD.2
a change that is less than that in any of the pre- Similar, low rates of decline in lung function
vious studies. The values for the decline in FEV1 were seen in the two study groups. A possible
1552 n engl j med 359;15 www.nejm.org october 9, 2008
The New England Journal of Medicine
Downloaded from nejm.org on January 22, 2013. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
Tiotropium in Chronic Obstructive Pulmonary Disease
Table 4. Incidence Rate of Serious Adverse Events per 100 Patient-Years.*
Relative Risk for Tiotropium
Adverse Event Tiotropium (N=2986) Placebo (N=3006) vs. Placebo (95% CI)
Cardiac 3.56 4.21 0.84 (0.730.98)
Angina 0.51 0.36 1.44 (0.912.26)
Atrial fibrillation 0.74 0.77 0.95 (0.681.33)
Cardiac failure 0.61 0.48 1.25 (0.841.87)
Congestive heart failure 0.29 0.48 0.59 (0.370.96)
Coronary artery disease 0.21 0.37 0.58 (0.331.01)
Myocardial infarction 0.69 0.97 0.71 (0.520.99)
Lower respiratory 11.32 13.47 0.84 (0.770.92)
Bronchitis 0.37 0.31 1.20 (0.731.98)
COPD exacerbation 8.19 9.70 0.84 (0.760.94)
Dyspnea 0.38 0.62 0.61 (0.400.94)
Pneumonia 3.28 3.46 0.95 (0.811.11)
Respiratory failure 0.90 1.31 0.69 (0.520.92)
* Listed are the incidence rates of serious adverse events (excluding lung cancer) that were reported by more than 1% of
patients in either study group, according to organ class during the study period (from the first day of administration of
a study drug until the last day plus 30 days).
P<0.05.
explanation for this finding is that tiotropium during the 4-year study period. Tiotropium also
does not influence the decline in lung function improved lung function, as compared with pla-
over time. There are other potential explanations. cebo, beyond the improvement resulting from
Current management of COPD could affect the serial administration of maximal doses of salbu-
decline in lung function so that a ceiling effect tamol and ipratropium. These improvements in
occurs and further improvements are not seen in lung function were accompanied by improve-
the absence of an intervention that repairs or ments in some of the clinical outcomes mea-
regenerates lung tissue. This possibility is sup- sured. Scores regarding health-related quality of
ported by the high rate of prescriptions for con- life improved relative to placebo during the entire
comitant respiratory medications in our study 4-year study period. In the tiotropium group,
and by the differences between tiotropium and there were significant delays in the onset of ex-
placebo in the rate of decline in postbronchodi- acerbations and associated hospitalizations. These
lator FEV1 in patients who did not use inhaled outcomes appeared in the presence of substan-
corticosteroids or long-acting beta-agonists. An- tial use of concomitant COPD therapies.
other potential reason is the higher rate of dis- The results of our study are consistent with
continuation in the placebo group. Data from our the published pooled safety analysis23 and indi-
study and other trials suggest that patients who cate a reduction in cardiac adverse events associ-
discontinue treatment have a more rapid decline ated with tiotropium. The reduced risk of respi-
in lung function than those who do not discon- ratory failure was also observed in the previous
tinue treatment.25 Since patients who discontin- pooled safety analysis of tiotropium, in which
ued treatment had, on average, significantly more the relative risk of respiratory failure in the tiotro-
severe airflow obstruction at baseline, those in pium group, as compared with the placebo group,
the placebo group who completed the trial prob- was 0.59 (95% CI, 0.26 to 1.34).23 However, our
ably represent healthy survivors. The possibil- study had significantly more power to detect such
ity of a healthy-survivor effect may not be ade- differential event reporting because of a larger
quately addressed with the prespecified analysis and longer exposure to tiotropium.
presented here.25,26 Our data show that among patients with
Tiotropium improved measures of airflow ob- COPD who were receiving other classes of respi-
struction and vital capacity that were performed ratory medications during the study period, the
24 hours after daily study-drug administration addition of 18 g of tiotropium once daily for up
n engl j med 359;15 www.nejm.org october 9, 2008 1553
The New England Journal of Medicine
Downloaded from nejm.org on January 22, 2013. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
Tiotropium in Chronic Obstructive Pulmonary Disease
to 4 years did not result in changes in the rate AstraZeneca, Boehringer Ingelheim, and GlaxoSmithKline, lec-
ture fees from Almirall, AstraZeneca, Boehringer Ingelheim,
of decline in lung function. However, there were and GlaxoSmithKline, and grant support from Boehringer In-
important lung-function benefits associated with gelheim, Forrest, and GlaxoSmithKline; Dr. Senn, receiving
tiotropium that were maintained during the consulting fees from Bayer, Boehringer Ingelheim, Chiesi, Eisai,
GlaxoSmithKline, INOT, Novartis, Pfizer, Servier, and Takeda,
4 years, as well as positive effects on health-relat- lecture fees from Amgen, Alcon, and Unilever, and grant sup-
ed quality of life and a reduced risk of exacerba- port from Boehringer Ingelheim, Chiesi, GlaxoSmithKline, and
tions and exacerbation-related hospitalizations Novartis, having an equity interest in Novartis, and serving as an
expert witness for GlaxoSmithKline; Ms. Burkhart, Dr. Kesten,
consistent with a relevant effect on the clinical and Dr. Menjoge, being employees of Boehringer Ingelheim; and
course of COPD. Finally, tiotropium reduced re- Dr. Decramer, receiving consulting fees from Boehringer Ingel
heim, Pfizer, GlaxoSmithKline, and Nycomed, lecture fees from
spiratory morbidity (including a decreased risk of Boehringer Ingelheim and Pfizer, and grant support from Astra-
respiratory failure) and reduced cardiac morbidity. Zeneca. No other potential conflict of interest relevant to this
Supported by Boehringer Ingelheim and Pfizer. article was reported.
Dr. Tashkin reports receiving consulting fees from AstraZen- We thank the UPLIFT trial team and clinical monitors; Dr.
eca, Boehringer Ingelheim, Dey Laboratories, and Schering, Dacheng Liu and Dr. Inge Leimer of Boehringer Ingelheim for
lecture fees from AstraZeneca, Boehringer Ingelheim, and Dey their statistical support; Terry Keyser (funded by Boehringer In-
Laboratories, and grant support from Almirall, AstraZeneca, gelheim) for editorial and technical support in the preparation
Boehringer Ingelheim, Dey Laboratories, GlaxoSmithKline, of this manuscript; and Dr. Romain Pauwels, who contributed to
Ivax, MediciNova, Nabi Biopharmaceuticals, Novartis, Pfizer, the design of the study and was a key member of the UPLIFT
and Sepracor; Dr. Celli, receiving consulting fees from Almirall, Joint Advisory Committee before his death in 2005.
References
1. Global Initiative for Chronic Obstruc- 8. Casaburi R, Mahler DA, Jones PW, et munity for Coal and Steel. Bull Eur Phys-
tive Lung Disease. Global strategy for the al. A long-term evaluation of once-daily iopathol Respir 1983;19:Suppl:7-28.
diagnosis, management and prevention of inhaled tiotropium in chronic obstructive 17. American Thoracic Society. Standard-
chronic obstructive pulmonary disease. pulmonary disease. Eur Respir J 2002;19: ization of spirometry: 1994 update. Am J
Bethesda, MD: National Heart, Lung, and 217-24. Respir Crit Care Med 1995;152:1107-36.
Blood Institute, April 2001 (revised 2007). 9. ODonnell DE, Flge T, Gerken F, et al. 18. Jones PW, Quirk FH, Baveystock CM,
(Accessed September 16, 2008, at http:// Effects of tiotropium on lung hyperinfla- Littlejohns P. A self-complete measure of
www.goldcopd.org.) tion, dyspnoea and exercise tolerance in health status for chronic airflow limita-
2. Anthonisen NR, Connett JE, Kiley JP, COPD. Eur Respir J 2004;23:832-40. tion: the St. Georges Respiratory Ques-
et al. Effects of smoking intervention and 10. Maltais F, Hamilton A, Marciniuk D, tionnaire. Am Rev Respir Dis 1992;145:
the use of an inhaled anticholinergic et al. Improvements in symptom-limited 1321-7.
bronchodilator on the rate of decline of exercise performance over 8 h with once- 19. Laird NM, Ware JH. Random-effects
FEV1: the Lung Health Study. JAMA 1994; daily tiotropium in patients with COPD. models for longitudinal data. Biometrics
272:1497-505. Chest 2005;128:1168-78. 1982;38:963-74.
3. The Lung Health Study Research 11. Vincken W, van Noord JA, Greefhorst 20. Suissa S. Statistical treatment of exac-
Group. Effect of inhaled triamcinolone APM, et al. Improved health outcomes in erbations in therapeutic trials of chronic
on the decline in pulmonary function in patients with COPD during 1 yrs treat- obstructive pulmonary disease. Am J Res
chronic obstructive pulmonary disease. ment with tiotropium. Eur Respir J 2002; pir Crit Care Med 2006;173:842-6.
N Engl J Med 2000;343:1902-9. 19:209-16. 21. Tashkin DP, Celli B, Decramer M, et al.
4. Pauwels RA, Lfdahl CG, Laitinen LA, 12. Brusasco V, Hodder R, Miravitlles M, Bronchodilator responsiveness in patients
et al. Long-term treatment with inhaled Korducki L, Towse L, Kesten S. Health out- with COPD. Eur Respir J 2008;31:742-50.
budesonide in persons with mild chronic comes following treatment for six months 22. Spiriva HandiHaler. Ingelheim, Ger-
obstructive pulmonary disease who con- with once daily tiotropium compared with many: Boehringer Ingelheim Pharma
tinue smoking. N Engl J Med 1999;340: twice daily salmeterol in patients with GmbH, 2008 (package insert).
1948-53. COPD. Thorax 2003;58:399-404. [Erratum, 23. Kesten S, Jara M, Wentworth C, Lanes
5. Burge PS, Calverley PM, Jones PW, Thorax 2005;60:105.] S. Pooled clinical trial analysis of the
Spencer S, Anderson JA, Maslen TK. Ran- 13. Niewoehner DE, Rice K, Cote C, et al. safet y of tiotropium. Chest 2006;130:
domised, double blind placebo controlled Prevention of exacerbations of chronic 1695-703.
study of fluticasone propionate in patients obstructive pulmonary disease with tiotro- 24. Celli BR, Thomas NE, Anderson JA, et
with moderate to severe chronic obstruc- pium, a once-daily inhaled anticholinergic al. Effect of pharmacotherapy on rate of
tive pulmonary disease: the ISOLDE trial. bronchodilator. Ann Intern Med 2005;143: decline of lung function in chronic ob-
BMJ 2000;320:1297-303. 317-26. structive pulmonary disease: results from
6. Decramer M. Rutten-van Mlken M, 14. Anzueto A, Tashkin D, Menjoge S, the TORCH study. Am J Respir Crit Care
Dekhuijzen PN, et al. Effects of N-acetyl- Kesten S. One-year analysis of longitudi- Med 2008;178:332-8.
cysteine on outcomes in chronic obstruc- nal changes in spirometry in patients with 25. Calverley PM, Spencer S, Willits L,
tive pulmonary disease (Bronchitis Ran- COPD receiving tiotropium. Pulm Pharma- Burge PS, Jones PW. Withdrawal from
domized on NAC Cost-Utility Study, col Ther 2005;18:75-81. treatment as an outcome in the ISOLDE
BRONCUS): a randomised placebo-con- 15. Decramer M, Celli B, Tashkin DP, et study of COPD. Chest 2003;124:1350-6.
trolled trial. Lancet 2005;365:1552-60. al. Clinical trial design considerations in 26. Kesten S, Plautz M, Piquette CA, Habib
[Erratum, Lancet 2005;366:984.] assessing long-term functional impacts of MP, Niewoehner DE. Premature discon-
7. Soriano JB, Sin DD, Zhang X, et al. tiotropium in COPD: the UPLIFT trial. tinuation of patients: a potential bias in
A pooled analysis of FEV1 decline in COPD COPD 2004;1:303-12. COPD clinical trials. Eur Respir J 2007;30:
patients randomized to inhaled cortico 16. Quanjer PH. Standardised lung func- 898-906.
steroids or placebo. Chest 2007;131:682-9. tion testing: report of the European Com- Copyright 2008 Massachusetts Medical Society.
1554 n engl j med 359;15 www.nejm.org october 9, 2008
The New England Journal of Medicine
Downloaded from nejm.org on January 22, 2013. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
Das könnte Ihnen auch gefallen
- Medical-Surgical Nursing ReviewDokument90 SeitenMedical-Surgical Nursing Reviewɹǝʍdןnos99% (312)
- NAPLEX NoteDokument58 SeitenNAPLEX Notebapimirab654Noch keine Bewertungen
- NCLEX Cheat SheetDokument3 SeitenNCLEX Cheat SheetRichard Allen Seman80% (10)
- Transfer Case Electrical RMDokument51 SeitenTransfer Case Electrical RMDaniel Canales75% (4)
- Drug Study - ParacetamolDokument8 SeitenDrug Study - Paracetamoldamtere71% (7)
- EB-300 310 Service ManualDokument32 SeitenEB-300 310 Service ManualVictor ArizagaNoch keine Bewertungen
- Calculation of The Current Transformer Accuracy Limit FactorDokument14 SeitenCalculation of The Current Transformer Accuracy Limit FactorWeiKiat Goh67% (3)
- Fergie 2Dokument8 SeitenFergie 2RambuNoch keine Bewertungen
- Adverse Health Consequences in COPD Patients With Rapid Decline in FEV - Evidence From The UPLIFT TrialDokument9 SeitenAdverse Health Consequences in COPD Patients With Rapid Decline in FEV - Evidence From The UPLIFT TrialCarolina MachadoNoch keine Bewertungen
- Acute Bronchodilator Responsiveness and Health Outcomes in COPD Patients in The UPLIFT TrialDokument11 SeitenAcute Bronchodilator Responsiveness and Health Outcomes in COPD Patients in The UPLIFT TrialcarinasheliapNoch keine Bewertungen
- TORCH Salmeterol Fluticasona en EpocDokument15 SeitenTORCH Salmeterol Fluticasona en EpocAgustina AndradeNoch keine Bewertungen
- Full ArticleDokument8 SeitenFull Articlekbrown733Noch keine Bewertungen
- ArticleDokument12 SeitenArticleRia DeviNoch keine Bewertungen
- Therapy Asthma DiseaseDokument4 SeitenTherapy Asthma DiseaseRatna S PutriNoch keine Bewertungen
- Jurnal Respirology ASPRDokument55 SeitenJurnal Respirology ASPRyosukexxNoch keine Bewertungen
- Indacaterol Provides 24-Hour Bronchodilation in COPD: A Placebo-Controlled Blinded Comparison With TiotropiumDokument8 SeitenIndacaterol Provides 24-Hour Bronchodilation in COPD: A Placebo-Controlled Blinded Comparison With TiotropiumCalca NeusNoch keine Bewertungen
- Spirometric Changes During Exacerbations of COPD: A Post Hoc Analysis of The WISDOM TrialDokument7 SeitenSpirometric Changes During Exacerbations of COPD: A Post Hoc Analysis of The WISDOM Trialluongminhnhat108Noch keine Bewertungen
- 2015 Article 218Dokument14 Seiten2015 Article 218Fi NoNoch keine Bewertungen
- AsmathDokument6 SeitenAsmathRido SaputraNoch keine Bewertungen
- Extrafine Triple Therapy Delays Copd Clinically Important Deterioration Vs Ics/Laba, Lama, or Laba/LamaDokument16 SeitenExtrafine Triple Therapy Delays Copd Clinically Important Deterioration Vs Ics/Laba, Lama, or Laba/LamatriNoch keine Bewertungen
- Azitromicyn COPDDokument10 SeitenAzitromicyn COPDLucrécia BórgiaNoch keine Bewertungen
- New England Journal Medicine: The ofDokument11 SeitenNew England Journal Medicine: The ofsufaNoch keine Bewertungen
- Once-Daily Indacaterol Versus TiotropiumDokument10 SeitenOnce-Daily Indacaterol Versus TiotropiumAnonymous p52JDZOdNoch keine Bewertungen
- Ajrccm 157 5 9709032Dokument5 SeitenAjrccm 157 5 9709032AlexandraGeorgeNoch keine Bewertungen
- Oxberry, 2011Dokument7 SeitenOxberry, 2011Maoi28Noch keine Bewertungen
- Print 1Dokument8 SeitenPrint 1Zaura Meliana MulyadiNoch keine Bewertungen
- 1 s2.0 S2531043718301107 MainDokument8 Seiten1 s2.0 S2531043718301107 MainCraniolyne RefianNoch keine Bewertungen
- Tiotropium Vs SalmeterolDokument20 SeitenTiotropium Vs Salmeteroldicky wahyudiNoch keine Bewertungen
- Simvastatin For The Prevention of Exacerbations in Moderate-to-Severe COPDDokument10 SeitenSimvastatin For The Prevention of Exacerbations in Moderate-to-Severe COPDdhamaraNoch keine Bewertungen
- TRD 70 323 1Dokument7 SeitenTRD 70 323 1Nurul Ummah NuNoch keine Bewertungen
- Withdrawal of Inhaled GlucocorticoidsDokument10 SeitenWithdrawal of Inhaled GlucocorticoidsAndi MarwansyahNoch keine Bewertungen
- Azithromycin For Prevention of Exacerbations of COPDDokument10 SeitenAzithromycin For Prevention of Exacerbations of COPDAJNoch keine Bewertungen
- Indacaterol-Glycopyrronium Versus Salmeterol-Fluticasone For COPDDokument13 SeitenIndacaterol-Glycopyrronium Versus Salmeterol-Fluticasone For COPDAbby OliivasNoch keine Bewertungen
- Effect of Inhaled Tiotropium On Intraocular Pressure in Patients of Chronic Obstructive Pulmonary DiseaseDokument7 SeitenEffect of Inhaled Tiotropium On Intraocular Pressure in Patients of Chronic Obstructive Pulmonary DiseaseIJAR JOURNALNoch keine Bewertungen
- Jurnal TuberkulosisDokument12 SeitenJurnal TuberkulosisviviavisaNoch keine Bewertungen
- Jurnal AsmaDokument12 SeitenJurnal AsmaaulNoch keine Bewertungen
- 01.stoller - Long-Term Oxygen Treatment - 2010Dokument9 Seiten01.stoller - Long-Term Oxygen Treatment - 2010guidepNoch keine Bewertungen
- Impact of Self-Reported Gastroesophageal Reflux Disease in Subjects From Copdgene CohortDokument9 SeitenImpact of Self-Reported Gastroesophageal Reflux Disease in Subjects From Copdgene CohortkasabeNoch keine Bewertungen
- The Effect of Acebrophylline Vs Sustained Release Theophylline in Pati...Dokument4 SeitenThe Effect of Acebrophylline Vs Sustained Release Theophylline in Pati...Agencia FaroNoch keine Bewertungen
- Title Sputum Bacteriology in Patients With Severe Chronic Lung DiseasesDokument47 SeitenTitle Sputum Bacteriology in Patients With Severe Chronic Lung DiseasesHam FGNoch keine Bewertungen
- Effects of Oral Doxofylline On InflammatoryDokument6 SeitenEffects of Oral Doxofylline On InflammatoryJanna Peñamora-DestrizaNoch keine Bewertungen
- Anti in Ammatory Effects of Statin in COPD: Egyptian Journal of Chest Diseases and TuberculosisDokument5 SeitenAnti in Ammatory Effects of Statin in COPD: Egyptian Journal of Chest Diseases and TuberculosiszzakieNoch keine Bewertungen
- Jur Nal Reading 1Dokument11 SeitenJur Nal Reading 1Lalu Ryan NovariNoch keine Bewertungen
- Long-Term Oxygen Therapy in COPD: Evidences and Open Questions of Current IndicationsDokument10 SeitenLong-Term Oxygen Therapy in COPD: Evidences and Open Questions of Current Indicationsnurharyanti darmaningtyasNoch keine Bewertungen
- CCRPM 2011 001 PDFDokument5 SeitenCCRPM 2011 001 PDFAlexandria Firdaus Al-farisyNoch keine Bewertungen
- 2.5.17 Jurnal TTP, OLD Vs MonoterapiDokument25 Seiten2.5.17 Jurnal TTP, OLD Vs Monoterapimuhammad syahir tajuddinNoch keine Bewertungen
- Copd 10 1787Dokument14 SeitenCopd 10 1787YOBEL NATHANIELNoch keine Bewertungen
- Estudio POST HOC Increase TreprostinilDokument10 SeitenEstudio POST HOC Increase TreprostinilMaria Jose Contreras SilvaNoch keine Bewertungen
- CNAF Post ExtubacionDokument10 SeitenCNAF Post ExtubacionpelaojaegerNoch keine Bewertungen
- Jurnal Biokim 7Dokument8 SeitenJurnal Biokim 7Friska ApriantiNoch keine Bewertungen
- ETHOS Symptoms & Quality of LifeDokument9 SeitenETHOS Symptoms & Quality of Lifeluongminhnhat108Noch keine Bewertungen
- 717 FullDokument8 Seiten717 FullRin4lNoch keine Bewertungen
- Factors Influencing Decline in Quality of Life inDokument6 SeitenFactors Influencing Decline in Quality of Life inlalopotNoch keine Bewertungen
- 143 Full PDFDokument5 Seiten143 Full PDFVanshika GuptaNoch keine Bewertungen
- Management of Acute Exacerbation of Copd: Dr. Fanny WS KoDokument3 SeitenManagement of Acute Exacerbation of Copd: Dr. Fanny WS KoCalca NeusNoch keine Bewertungen
- 136 Full CopdDokument7 Seiten136 Full CopdAnty FftNoch keine Bewertungen
- Thoraxjnl 2015 207194Dokument9 SeitenThoraxjnl 2015 207194Fi NoNoch keine Bewertungen
- ZGQMV F63 PZ SQT Pkps DZ QR DSDokument5 SeitenZGQMV F63 PZ SQT Pkps DZ QR DSfannysanastasyaNoch keine Bewertungen
- Comparison of Tiotropium Once Daily, Formoterol Twice Daily and Both Combined Once Daily in Patients With COPDDokument9 SeitenComparison of Tiotropium Once Daily, Formoterol Twice Daily and Both Combined Once Daily in Patients With COPDArezoo JamNoch keine Bewertungen
- TiotropiumDokument2 SeitenTiotropiumElaine SombranoNoch keine Bewertungen
- Medi 99 E23646Dokument8 SeitenMedi 99 E23646panumatkhamphiranonNoch keine Bewertungen
- Chatham 2004Dokument5 SeitenChatham 2004raul huertaNoch keine Bewertungen
- Serum Surfactant Protein D Is Steroid Sensitive and Associated With Exacerbations of COPDDokument8 SeitenSerum Surfactant Protein D Is Steroid Sensitive and Associated With Exacerbations of COPDPatrick RamosNoch keine Bewertungen
- Copd 10 1703Dokument7 SeitenCopd 10 1703brikitabelaNoch keine Bewertungen
- Exhaled 8-Isoprostane As An Biomarker of Lung Oxidative Stress in Patients With COPD and Healthy SmokersDokument3 SeitenExhaled 8-Isoprostane As An Biomarker of Lung Oxidative Stress in Patients With COPD and Healthy SmokersAnthonyJohanNoch keine Bewertungen
- Essentials in Lung TransplantationVon EverandEssentials in Lung TransplantationAllan R. GlanvilleNoch keine Bewertungen
- Lung Transplantation: Evolving Knowledge and New HorizonsVon EverandLung Transplantation: Evolving Knowledge and New HorizonsGanesh RaghuNoch keine Bewertungen
- Drug List, Pharmaceutics II: Clofibrate (Atromid-S) - Soft Gelatin CapsuleDokument6 SeitenDrug List, Pharmaceutics II: Clofibrate (Atromid-S) - Soft Gelatin Capsulebapimirab654Noch keine Bewertungen
- Med Surg V1 2015 AnswersDokument2 SeitenMed Surg V1 2015 Answersbapimirab654Noch keine Bewertungen
- Med Surg v1 2015 AnswersDokument2 SeitenMed Surg v1 2015 Answersbapimirab654Noch keine Bewertungen
- Review For PKDokument3 SeitenReview For PKbapimirab654Noch keine Bewertungen
- Quiz 4Dokument1 SeiteQuiz 4bapimirab654Noch keine Bewertungen
- Brand Generic Class Other: NAPLEX ReviewDokument72 SeitenBrand Generic Class Other: NAPLEX Reviewbapimirab654Noch keine Bewertungen
- Quiz 5Dokument1 SeiteQuiz 5bapimirab654Noch keine Bewertungen
- Drug Information II Study Guide - StudentDokument6 SeitenDrug Information II Study Guide - Studentbapimirab654Noch keine Bewertungen
- Glossary of TermsDokument3 SeitenGlossary of Termsbapimirab654Noch keine Bewertungen
- HAI Prevention The Power Is in Your Hands.1Dokument8 SeitenHAI Prevention The Power Is in Your Hands.1kencheenNoch keine Bewertungen
- Patient Is Alert and Oriented To Person Place and TimeDokument1 SeitePatient Is Alert and Oriented To Person Place and Timebapimirab654Noch keine Bewertungen
- OxygenationDokument7 SeitenOxygenationMarcus, RN100% (11)
- M7 Practice Problem KeyDokument14 SeitenM7 Practice Problem Keybapimirab654Noch keine Bewertungen
- MedicationDokument1 SeiteMedicationbapimirab654Noch keine Bewertungen
- References: NCSBN's Review For The NCLEX-PN ExaminationDokument5 SeitenReferences: NCSBN's Review For The NCLEX-PN Examinationbapimirab6540% (1)
- Isbar Clear CommunicationDokument1 SeiteIsbar Clear Communicationbapimirab654Noch keine Bewertungen
- Mercedes (DTC) 976990001963 20220615144147Dokument3 SeitenMercedes (DTC) 976990001963 20220615144147YB MOTOR Nissan - Datsun SpecialistNoch keine Bewertungen
- Double-Outlet Right Ventricle With An An Intact Interventricular Septum and Concurrent Hypoplastic Left Ventricle in A CalfDokument6 SeitenDouble-Outlet Right Ventricle With An An Intact Interventricular Septum and Concurrent Hypoplastic Left Ventricle in A CalfYoga RivaldiNoch keine Bewertungen
- Feature Writing EnglishDokument2 SeitenFeature Writing EnglishAldren BababooeyNoch keine Bewertungen
- Eoi QAMDokument6 SeitenEoi QAMPeeyush SachanNoch keine Bewertungen
- Electric Bike Monitoring and Controlling System Based On Internet of ThingsDokument8 SeitenElectric Bike Monitoring and Controlling System Based On Internet of ThingsEarl PhamtonhiveNoch keine Bewertungen
- With EU Stage V Engine Installed: 200 HP (149 KW) / 2,200 RPMDokument4 SeitenWith EU Stage V Engine Installed: 200 HP (149 KW) / 2,200 RPMSara Sarmiento EcheverryNoch keine Bewertungen
- K&J Magnetics - Demagnetization CurvesDokument4 SeitenK&J Magnetics - Demagnetization CurvessubbannachrsNoch keine Bewertungen
- M1-Safety StandardsDokument9 SeitenM1-Safety StandardscarlNoch keine Bewertungen
- Visedo FPC-2016Dokument13 SeitenVisedo FPC-2016Probonogoya Erawan SastroredjoNoch keine Bewertungen
- Ultimate GuideDokument33 SeitenUltimate GuidemrosamusicNoch keine Bewertungen
- English 8 - B TR Và Nâng CaoDokument150 SeitenEnglish 8 - B TR Và Nâng CaohhNoch keine Bewertungen
- EXP1POSTLABDokument13 SeitenEXP1POSTLABGiane MagimotNoch keine Bewertungen
- Streamline SWR (S) - Rev - 00-04-2019 PDFDokument2 SeitenStreamline SWR (S) - Rev - 00-04-2019 PDFarjun 11Noch keine Bewertungen
- 1mrk513011-Ben en Auxiliary Current Transformer For Radss 1-Phase and 3-Phase Slce 12 Slce 16 Slxe 4Dokument4 Seiten1mrk513011-Ben en Auxiliary Current Transformer For Radss 1-Phase and 3-Phase Slce 12 Slce 16 Slxe 4GustavoForsterNoch keine Bewertungen
- Movimiento Circular, Momentun Lineal y EnergíaDokument92 SeitenMovimiento Circular, Momentun Lineal y EnergíaJulio César Macías ZamoraNoch keine Bewertungen
- Adminstration of Intramusclar InjectionDokument3 SeitenAdminstration of Intramusclar InjectionDenise CastroNoch keine Bewertungen
- Mechanical Advantage HomeworkDokument8 SeitenMechanical Advantage Homeworkafeurbmvo100% (1)
- Ansible Automation SA Technical Deck Q2FY19Dokument43 SeitenAnsible Automation SA Technical Deck Q2FY19daniel_vp21Noch keine Bewertungen
- Your Heart: Build Arms Like ThisDokument157 SeitenYour Heart: Build Arms Like ThisNightNoch keine Bewertungen
- Organic Chemistry (Some Basic Principles and TechniquesDokument30 SeitenOrganic Chemistry (Some Basic Principles and TechniquesNaveen SharmaNoch keine Bewertungen
- Afectiuni Si SimptomeDokument22 SeitenAfectiuni Si SimptomeIOANA_ROX_DRNoch keine Bewertungen
- Master of Business Administration in Aviation Management MbaamDokument10 SeitenMaster of Business Administration in Aviation Management MbaamAdebayo KehindeNoch keine Bewertungen
- Fluid Solids Operations: High HighDokument20 SeitenFluid Solids Operations: High HighPriscilaPrzNoch keine Bewertungen
- Good Stuff Courage, Resilience, Gratitude, Generosity, Forgiveness, and Sacrifice (Akhtar, Salman)Dokument221 SeitenGood Stuff Courage, Resilience, Gratitude, Generosity, Forgiveness, and Sacrifice (Akhtar, Salman)madhugaggar999Noch keine Bewertungen
- Pi 0614 Hiblack f890b en WebDokument2 SeitenPi 0614 Hiblack f890b en Web王偉仲Noch keine Bewertungen
- Wic ReflectionDokument3 SeitenWic Reflectionapi-307029735Noch keine Bewertungen