Beruflich Dokumente
Kultur Dokumente
Midpoint Reflection
Hochgeladen von
api-350193110Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Midpoint Reflection
Hochgeladen von
api-350193110Copyright:
Verfügbare Formate
Jenna Richard
NUR 4143
March 4, 2017
Midterm Reflection
Throughout my time spent in the NICU at St Francis Medical Center, I have experienced
many moments that were challenging and allowed me to grow as a nurse and as a person. One
patient comes to mind when I think of the most challenging moment so far in my clinical
immersion. It was not that the patient himself was challenging or required complex care, but
rather the social aspect was difficult to wrap my head around. The baby was withdrawing
because his mother had been using heroin, smoking cigarettes, and drinking alcohol throughout
her pregnancy. On top of that, he was born with a congenital heart defect- tetralogy of fallot.
After a long stay in the NICU receiving morphine and then being weaned from it, it was time to
go home. However, it was not such a happy time as it usually is seeing a baby go home. We were
worried about this babys future and whether he would receive the proper care he needed.
We were sure to do everything in our power to make sure the baby had the best life
possible after leaving the hospital. We taught the parents and the babys older sister over and
over about proper care and precautions for caring for a newborn. Child protective services chose
not to take the child from the parents, even though the father of the child was also a registered
sex offender and had not one, but two ankle monitors on. This is one thing that I wish would
have gone differently- that CPS would have taken measures to ensure the safety of the child
rather than just turning the other cheek. But this was out of our hands, and the child eventually
did go home with his parents.
The clinical judgment that we made was based on the history of the mothers drug abuse
and the fathers criminal record. We did our best to take this as an opportunity to educate the
family and hope that they could change in order to provide the best life possible for their new
baby. We also worked to promote bonding between the parents and child and encouraged the
family to visit as often as possible to help with the babys recovery.
After talking with the mother for some time, we learned that she had been on an
extremely high dose of methadone near the end of her pregnancy and was still taking it daily. She
was told by the staff at the methadone clinic that most babies never even experienced withdrawal
symptoms. This is completely untrue, in fact, an article from BMJ Case Reports says that 48-
94% of infants exposed to methadone or heroin in utero experienced Neonatal Abstinence
Syndrome (NAS). The article also mentions the difficulty of determining the prevalence of
heroin use in pregnancy due to the mothers feelings of guilt, fear of social services involvement,
and denial. Many times, we do not know that the mother has been using until the babies starts
showing signs of withdrawal.
Babies suffering from NAS are commonly seen in the NICU at St Francis and I have
already cared for five of these babies in my short time on the unit. It is incredibly sad and
frustrating to see these innocent babies suffer and it is even harder to see them go to a broken
home. The most important thing that we can do as nurses to prevent future occurrences like this
is to educate and make sure that the mothers are receiving proper prenatal care. With the
growing heroin epidemic, it is more important than ever to be sure that pregnant women are
aware of the dangers of opioid use in pregnancy.
References
Namboodiri, V., George, S., Boulay, S., & Fair, M. (2010). Pregnant heroin addict: what about
the baby? BMJ Case Reports, 2010, bcr09.2009.2246.
http://doi.org/10.1136/bcr.09.2009.2246
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
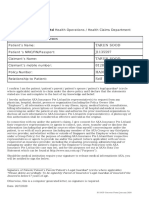
- To: AXA Insurance Pte LTD Health Operations / Health Claims DepartmentDokument1 SeiteTo: AXA Insurance Pte LTD Health Operations / Health Claims DepartmentT SooNoch keine Bewertungen
- Mental Health Assessment?: What Is ADokument2 SeitenMental Health Assessment?: What Is AMarwa Kazi MohammedNoch keine Bewertungen
- Ophthalmology ODOS - EMRDokument8 SeitenOphthalmology ODOS - EMRLinda O'HaraNoch keine Bewertungen
- Pay-for-Performance / Quality Incentives: Discussion Paper For The MMA 623e Advisory BoardDokument10 SeitenPay-for-Performance / Quality Incentives: Discussion Paper For The MMA 623e Advisory BoardAnurag PaliwalNoch keine Bewertungen
- Bhandara MTPDokument2 SeitenBhandara MTPAbhishek Motiram JagtapNoch keine Bewertungen
- q5 Nursery SchoolDokument4 Seitenq5 Nursery SchoolPK CheahNoch keine Bewertungen
- Labor Standards Midterms Digests 2014Dokument268 SeitenLabor Standards Midterms Digests 2014Leo Joselito Estoque BonoNoch keine Bewertungen
- Patient's Medical Chart PDFDokument2 SeitenPatient's Medical Chart PDFHydieNoch keine Bewertungen
- Easy Health Insurance Claim Form Apollo Munich 1 2Dokument2 SeitenEasy Health Insurance Claim Form Apollo Munich 1 2Mohit GuptaNoch keine Bewertungen
- Electronic Child Health Network (Echn) : Hospitals in OntarioDokument7 SeitenElectronic Child Health Network (Echn) : Hospitals in OntariobevNoch keine Bewertungen
- Selecting Automation For The Clinical Chemistry LaboratoryDokument7 SeitenSelecting Automation For The Clinical Chemistry LaboratoryFathul WiandaruNoch keine Bewertungen
- Anita Eulogy FinalDokument5 SeitenAnita Eulogy Finalapi-355635505Noch keine Bewertungen
- Patient Safety IngDokument6 SeitenPatient Safety IngUlfani DewiNoch keine Bewertungen
- Harry Hoxsey Cancer CureDokument10 SeitenHarry Hoxsey Cancer CureFashji100% (1)
- Inspector Wade V North Coast Area Health Service (2005) NSWIRComm 349 (5 October 2005)Dokument121 SeitenInspector Wade V North Coast Area Health Service (2005) NSWIRComm 349 (5 October 2005)api-377007350% (2)
- Seha Ar11 enDokument83 SeitenSeha Ar11 enKhaled AlObaidliNoch keine Bewertungen
- Training Code (GE.008) - CQMRDokument11 SeitenTraining Code (GE.008) - CQMRBung HerryNoch keine Bewertungen
- Daradia Pain Hospital, The Exclusive Pain Management Hospital, Not Only Treats Pain, But Also Organizes Pain Management Courses To Train PhysiciansDokument2 SeitenDaradia Pain Hospital, The Exclusive Pain Management Hospital, Not Only Treats Pain, But Also Organizes Pain Management Courses To Train PhysiciansPR.comNoch keine Bewertungen
- The Economic Burden of ObesityDokument13 SeitenThe Economic Burden of ObesityNasir Ali100% (1)
- Transition Care ModelDokument2 SeitenTransition Care ModelErhyqck De GuzmanNoch keine Bewertungen
- 620 BPG Childhood ObesityDokument91 Seiten620 BPG Childhood Obesityzenagit123456Noch keine Bewertungen
- Puericulture Centers PDFDokument3 SeitenPuericulture Centers PDFraul_bsuNoch keine Bewertungen
- 2 Pioneers and Milestones in The Field of Orthodontics and Orthognathic Surgery 2014 Orthognathic SurgeryDokument43 Seiten2 Pioneers and Milestones in The Field of Orthodontics and Orthognathic Surgery 2014 Orthognathic SurgeryiweourvgiuNoch keine Bewertungen
- Hemingway A Very Short StoryDokument1 SeiteHemingway A Very Short StoryDaniel DiazNoch keine Bewertungen
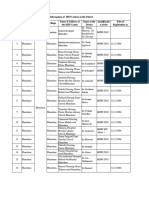
- Provider List PH PDFDokument20 SeitenProvider List PH PDFAl Polen Jr SingcayNoch keine Bewertungen
- Nur 2100 Reflection - Catholic Healthcare MinistriesDokument3 SeitenNur 2100 Reflection - Catholic Healthcare Ministriesapi-485309887Noch keine Bewertungen
- MOLA's Osteology BooksDokument1 SeiteMOLA's Osteology BooksMOLA (Museum of London Archaeology)Noch keine Bewertungen
- List of State Nursing Council Recognised Institutions Offering B.SC (N) Programme Inspected Under Section 13 and 14 of INC Act For The Academic Year 2020-2021Dokument168 SeitenList of State Nursing Council Recognised Institutions Offering B.SC (N) Programme Inspected Under Section 13 and 14 of INC Act For The Academic Year 2020-2021principal MCONNoch keine Bewertungen
- Code of Ethics PhilDokument3 SeitenCode of Ethics PhilAlleyan Hannah DenumNoch keine Bewertungen
- Caribbean Application Document - ASCE 7-05Dokument39 SeitenCaribbean Application Document - ASCE 7-05Jayant LakhlaniNoch keine Bewertungen