Beruflich Dokumente
Kultur Dokumente
Treating Skin Cancer With Topical Cream: Review
Hochgeladen von
vintaarnikeOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Treating Skin Cancer With Topical Cream: Review
Hochgeladen von
vintaarnikeCopyright:
Verfügbare Formate
Review
Treating skin cancer with topical
cream
Giuseppe Micali, Francesco Lacarrubba, Franco Dinotta,
Doriana Massimino & Maria Rita Nasca
1. Introduction University of Catania, Dermatology Clinic, Catania, Italy
2. Fluorouracil
Importance of the field: Topical pharmacotherapy is an approach to consider
3. Imiquimod
in selected skin cancers. Noninvasive, tissue-sparing, topical, self-administered
4. Diclofenac
treatments represent a highly desirable alternative option, both in aged and
5. Retinoids unhealthy patients who may be poor surgical candidates, as well as in rela-
Expert Opin. Pharmacother. Downloaded from informahealthcare.com by University of Aberdeen on 06/02/13
6. Conclusions tively young subjects with lesions located on cosmetically sensitive areas wish-
7. Expert opinion ing to avoid disfiguring scars. This paper reviews and discusses the use of
topical pharmacotherapy in the treatment of skin cancer.
Areas covered in this review: This paper examines the existing literature and
updates current knowledge of topical pharmacotherapy for skin cancer using
fluorouracil, imiquimod, diclofenac and retinoids.
What the reader will gain: There is a gap between current and best practice in
that the use of pharmacotherapy in the treatment of skin cancer is only par-
tially known. The purpose of this paper is to provide an in-depth knowledge
on this topic; consequently, the readers should be able to consider new
strategies in their practice.
For personal use only.
Take home message: Topical pharmacotherapy represents an option for treat-
ment of actinic keratoses and selected basal cell carcinomas. Moreover, prelim-
inary reports indicate imiquimod to be effective for skin or mucosal cancers
such as Bowens disease, erythroplasia of Queyrat and lentigo maligna.
Keywords: cancer, diclofenac, fluorouracil, imiquimod, pharmacotherapy, retinoids, skin
Expert Opin. Pharmacother. (2010) 11(9):1515-1527
1. Introduction
Treatment of skin cancer includes several options such as surgery (conventional
excisional and Mohs micrographic surgery), physical therapy (electrodesiccation/
curettage, cryosurgery, CO2 laser and radiation therapy) as well as photodynamic
therapy (PDT) and pharmacotherapy, both topical and systemic. Regardless of
the approach, removal of the tumor, preservation of function and good cosmetic
outcome represent treatment end points [1,2].
Topical pharmacotherapy represents an option for treatment of both actinic ker-
atoses and select basal cell carcinomas (BCCs). Moreover, some topical treatments
are reported as useful for skin or mucosal cancers such as Bowens disease, erythro-
plasia of Queyrat and lentigo maligna. Indications for topical pharmacotherapy
include extensive, multifocal, multiple tumors, indistinct lesion boundaries, locali-
zation in cosmetically sensitive areas (e.g., face), history of hypertrophic scarring
and/or keloids, surgical risk factors (age, associated diseases) and patient preference
to avoid invasive procedures.
In this review, evidence from the literature on topical pharmacotherapy of skin
cancer with fluorouracil, diclofenac, imiquimod and retinoids are analyzed. Their
proper use and indication are summarized and discussed.
10.1517/14656566.2010.481284 2010 Informa UK Ltd ISSN 1465-6566 1515
All rights reserved: reproduction in whole or in part not permitted
Treating skin cancer with topical cream
Article highlights.
efficacy compared with standard formulations is unclear [9].
In some studies, fluorouracil 0.5% formulation is as effective
. Topical pharmacotherapy offers effective alternative as fluorouracil 5% concentration, based on percentage reduc-
treatments for skin cancer, although careful patient
selection is required to achieve the desired goal of
tion and complete clearance of actinic keratoses from
complete tumour clearance. baseline [3,4,10-13]. Also, topical fluorouracil 0.5% achieves
. Topical pharmacotherapy deserves first-line treatment good patient compliance owing to reduced frequency of
status for actinic keratoses, especially in consideration of excessive skin reactions at application sites [10]. In a study of
the field cancerization phenomenon. 207 subjects, a microsphere formulation of fluorouracil
. Imiquimod 5% cream represents the more versatile
agent: although FDA-approved for only actinic keratoses
0.5% applied once daily for 1, 2 or 4 weeks was more effective
and superficial basal cell carcinomas (BCCs), its than vehicle in achieving actinic keratose clearance (15, 37,
off-label use supported by numerous studies includes 58 and 0%, respectively) [12]. In another similar double-blind,
nodular BCCs, Bowens disease, erythroplasia of Queyrat multicenter, parallel-group study, in which 177 participants
and lentigo maligna, with excellent outcome.
Expert Opin. Pharmacother. Downloaded from informahealthcare.com by University of Aberdeen on 06/02/13
were randomized to receive fluorouracil 0.5% once daily for
. An important issue that needs to be highlighted is the
frequent occurrence of moderate to severe application-
1, 2 or 4 weeks, patients achieved 100% clearance (26.3,
site irritation during imiquimod therapy; however, this 19.5 and 47.5%, respectively, vs 3.4% of controls) [14].
reaction is a good predictor of the therapeutic effect A recent systematic review including 13 RCTs, evaluated
and expert physicians can easily manage it without fluorouracil short- and long-term efficacy at different dosing
further complications. regimens and compared these results with other available treat-
. Fluorouracil has demonstrated in controlled studies to be
effective in actinic keratoses and superficial BCCs.
ments [5]. Fluorouracil 5% cream was effective in 49.0% of
. Diclofenac 3% gel in 2.5% hyaluronic acid (DHA), patients and achieved 100% clearance of lesions, compared
whose efficacy is at present limited to actinic keratoses, with 34.8% of the 0.5% formulation. Moreover, treatment
is considered a well-tolerated treatment by most with 5 and 0.5% resulted in an average reduction of 79.5
patients, with side effects at application sites and 86.1%, respectively, in the number of lesions.
considerably lower compared with other treatments.
One randomized study compared the efficacy rates of
For personal use only.
This box summarizes key points contained in the article.
fluorouracil 5% (twice daily for 4 weeks), imiquimod 5%
(3 times/weeks for 4 -- 8 weeks) and cryosurgery (1 -- 2 courses)
in patients affected by actinic keratoses. Complete clinical
clearance at the end of the treatment was achieved by 96,
2. Fluorouracil 85 and 68% of patients, respectively [15]. In a 12-month
follow-up, 33% of subjects sustained clearance for fluorouracil,
Topical fluorouracil is the most extensively studied topical 73% for imiquimod, and only 4% for cryosurgery [15]. This
chemotherapeutic agent. As an antimetabolite and structural study also evaluated cosmetic outcome, reporting no significant
analogue of thymidine, it hinders thymidylate synthetase difference between fluorouracil and imiquimod after 3 months
and interferes with DNA and RNA synthesis in dividing cells, of therapy; while at a 12-month follow-up, imiquimod
resulting in cell death [3-5]. reported a better cosmetic profile than both fluorouracil and
Topical fluorouracil 5% is FDA-approved for the treat- cryosurgery in terms of scarring, atrophy and induration [5,15].
ment of actinic keratoses and superficial BCCs. Efficacy in
the treatment of Bowens disease has been reported [3]. 2.2 Basal cell carcinoma
Topical fluorouracil 5% cream was the first FDA nonsurgical
2.1 Actinic keratoses treatment approved for superficial BCCs, though few con-
Topical effectiveness in the treatment of actinic keratoses was trolled studies are published [3]. A double-blind, randomized
first demonstrated in the 1960s [6], and subsequently con- trial evaluated the effectiveness of fluorouracil 5% cream in
firmed by several open trials, dose-ranging studies and treating BCCs using two different vehicles designed to enhance
randomized controlled trials (RCTs) [3-6]. penetration and efficacy [16]. In this study, 13 subjects with
Reduction in the number of actinic keratoses is achieved by 17 biopsy-proven BCCs were randomized to receive either fluo-
topical fluorouracil 5% twice daily for 2 -- 4 weeks, depending rouracil 5% in a phosphatidyl choline vehicle or fluorouracil
on the treatment site and patient sensitivity. In two random- 5% in a petrolatum-base. Treatments were applied twice a
ized trials, fluorouracil 5% cream applied twice daily for day for 4 weeks and resulted in a 90% cure rate (9/10), both
3 weeks on the dorsum of the hands [7] and on the face [8] clinical and histologic, for lesions treated with phosphatidyl
resulted in a mean reduction in actinic keratoses of 70 and choline formulation, compared with a 57% cure rate (4/7) in
78% respectively [7,8]. Less aggressive regimens are reported those treated with the petrolatum-based vehicle [16].
in order to enhance patient tolerance and compliance. Less In a more recent, single-arm evaluation of 31 superficial
frequent but more prolonged applications (only once or twice BCCs treated with fluorouracil 5% cream applied twice daily
a week for 6 -- 7 weeks), or lower potencies (1%, or dilution for up to 8 -- 12 weeks, 90% of lesions showed complete
to 0.5%), have been suggested as possible alternatives; but histologic clearance [17].
1516 Expert Opin. Pharmacother. (2010) 11(9)
Micali, Lacarrubba, Dinotta, Massimino & Nasca
2.3 Bowens disease studies have suggested an additional TLR-independent func-
Topical fluorouracil is successfully used for the treatment of tion, related to the suppression of adenylyl-cyclase, which is
Bowens disease, particularly in cases of multiple lesions or thought to be important for the control of viral infections and
where lesions are located in areas difficult to treat with con- tumors. Moreover, imiquimod may be involved in the produc-
ventional surgery. Twice-daily application of 5% fluorouracil tion of proapoptotic signalling in tumor cells via death receptor
formulation is recommended for up to 8 weeks or longer to pathways, including Fas receptor [30]. Several studies have
provide satisfactory results with low recurrence rates [18,19]. demonstrated imiquimod antiangiogenic property due to the
In an open-label study, 24 subjects with 26 biopsy- production of various cytokines and have provided evidence
confirmed lesions of Bowens disease were treated with topical for inhibition of pathological growth of new vessels [31].
fluorouracil 5% twice daily for up to 9 weeks. Complete clear- There are several studies evaluating the efficacy of imiqui-
ance was observed in 92% of subjects (24 of the 26 lesions), mod in the treatment of actinic keratoses, BCCs, Bowens
with an average duration of follow-up at 55 months. disease and lentigo maligna.
Expert Opin. Pharmacother. Downloaded from informahealthcare.com by University of Aberdeen on 06/02/13
Post-treatment biopsies were performed in 18/26 cases,
and 17 of the 18 histological specimens showed evidence of 3.1 Actinic keratoses
resolution [20]. Imiquimod is a topical FDA-approved treatment for face and
In a randomized trial comparing fluorouracil with PDT, scalp actinic keratoses in immunocompetent individuals. It is
fluorouracil 5% cream applied once daily for 1 week and used as a 5% cream three times a week for 4 weeks. Additional
twice daily for 2 -- 4 weeks resulted in a clearance rate of treatment may be required for those patients who do not
48 versus 82% for PDT at 12-month follow-up [21]. completely clear. The treatment site should not be cleansed
Interestingly, some authors have noted an increased effec- for at least 8 h after imiquimod application. Increasing the
tiveness of fluorouracil when used in combination with dosing frequency to more than three times a week has been
other therapeutic modalities (imiquimod, systemic retinoids, associated with a concomitant increase in the number of
cryotherapy and PDT) [18,19]. patients discontinuing the treatment because of excessive
application site irritation [32,33].
For personal use only.
2.4 Safety Multiple controlled studies have confirmed its short-
Topical fluorouracil cream has an acceptable safety profile term efficacy in reducing the number of actinic kerato-
based on RCT evidence. The most common adverse effects ses [32,34]. Overall clinical clearance rates from these studies
reported during treatment include erythema, irritation, burn- ranged from 45 to 57% in the imiquimod arm versus 2 to
ing, dryness, pain, pruritus and hypo- or hyperpigmenta- 15% in the placebo group, respectively [32].
tion [3]. These symptoms typically present at the application In a meta-analysis study [35] including five RCTs, imiqui-
site within 5 -- 10 days of treatment initiation and progres- mod 5% cream was found to achieve complete clearance in
sively improve as application frequency is reduced or treat- 50% of patients compared with 5% in the placebo group.
ment is discontinued. Allergic contact dermatitis has been In another meta-analysis study [36] consisting of four RCTs,
reported [4]. Systemic toxicity is rare since fluorouracil absorp- imiquimod 5% cream or vehicle was applied three times a
tion rate is low through fully keratinized skin. Fluorouracil week for up to 16 weeks in two studies and 12 weeks in one
should not be used in women who are or may become study, while the fourth study adopted a twice-weekly applica-
pregnant, since it is teratogenic and classified as pregnancy tion regimen for 16 weeks. The data showed complete clinical
category X. and histologic (only two studies) clearance of actinic keratoses
ranging from 45 to 84% in patients treated with imiquimod
3. Imiquimod compared with 0 -- 7% in the vehicle groups (p < 0.0001).
In a third meta-analysis study [37] comparing topical
Imiquimod is an immune response modifier with antiviral, imiquimod with topical fluorouracil, a relatively higher effi-
antitumor and antiangiogenic activity, first approved by cacy of imiquimod 5% than that of fluorouracil (0.5,
the FDA in 1997 for topical treatment of external genital 1 and 5%) has been demonstrated for actinic keratoses loca-
and perianal warts, and later for actinic keratoses and ted on face or scalp. The mean efficacy rate for each drug
superficial BCCs. was 70 12% for imiquimod compared with 52 18%
The mechanism of action of imiquimod is primarily related for fluorouracil.
to its activity upon toll-like receptors (TLR) 7 and 8 of antigen- Topical imiquimod long-term efficacy has been demon-
presenting cells, which are involved in the modulation of both strated in one study in which 36 subjects were randomized to
innate and acquired immunity pathways [2,22-27]. Imiquimod, receive either imiquimod or control vehicle (one application
by binding TLR-7, stimulates production and release of 3 times/week). Complete clinical and histologic clearance at
several endogenous cytokines and chemokines, which, in 12 weeks was observed in 84% of the treatment group. Twelve
turn, enhance and perpetuate cell-mediated immune response months after treatment, two subjects (8%) in the treatment
involving CD4+ and CD8+ T lymphocytes, resulting in group reported clinical recurrence. The imiquimod group
imiquimod antitumor and antiviral activity [22-24,28,29]. Recent was reviewed at a 2-year follow-up. Of these, 16% developed
Expert Opin. Pharmacother. (2010) 11(9) 1517
Treating skin cancer with topical cream
new actinic keratoses after 18 months and 20% reported new 6-week, randomized, open-label, dose-response study evaluat-
lesions after 24 months [38]. ing four dosing regimens; and a 12-week, randomized, vehi-
Recently, an RCT involving 20 subjects investigated cle-controlled, double-blind, dose-response study evaluating
imiquimod efficacy and safety of a lower dosing regimen four dosing regimens. Dosing once daily for 7 days/week
(once-weekly applications for 24 weeks). Although the resulted in the highest clinical and histologic clearance rate,
imiquimod-treated group improved compared with the pla- with 25 (71%) of 35 and 16 (76%) of 21 subjects showing
cebo arm, overall data showed a lower cure rate with placebo clearance of their tumor in the 6- and 12-week studies, respec-
(6.7%) compared with the active regimen [39]. tively [47]. In another Phase III randomized study, imiquimod
Interestingly, clinical and histologic clearance correlates as a monotherapy for nodular BCCs showed relatively poor
with irritation at the application site, indicating a major role efficacy since residual tumor was found in 36% of treated
of inflammation in imiquimods mechanism of action [36,38]. subjects [48].
Imiquimod has been combined with other therapeutic The long-term outcome of topical imiquimod in the treat-
Expert Opin. Pharmacother. Downloaded from informahealthcare.com by University of Aberdeen on 06/02/13
options (cryotherapy, fluorouracil), to increase efficacy [34]. ment of superficial, nodular and infiltrative BCCs has been
A recent clinical trial [40], concluded favorably on the use of evaluated in a 5-year follow-up, prospective, open-label study.
5% imiquimod combined with fluorouracil as it was found to Clearance rates (100% for superficial BCCs, 75% for nodular
increase clinical clearance and reduce recurrence rate of actinic BCCs and 60% for infiltrative BCCs) demonstrate long-
keratoses. Nevertheless, optimal frequency of application and term benefit, with only 2% recurrence, and confirm the previ-
duration of treatment need further elucidation. ously published RCT on short-term imiquimod [49]. Similar
findings have been reported in a second 5-year, long-term,
3.2 Basal cell carcinoma follow-up study carried out in Europe on 182 subjects with
Topical imiquimod 5% cream is licensed by the FDA for the BCCs [50], showing an overall clinical complete clearance
treatment of superficial BCCs. In a Cochrane Skin Group anal- rate at the end of the study of 77.9%.
ysis including seven RCTs, imiquimod was found to be effec- Two studies comparing the use of topical imiquimod 5%
tive and safe in the treatment of both superficial and nodular cream with and without occlusion in the treatment of superfi-
For personal use only.
BCCs, although response rates varied according to therapeutic cial and nodular BCCs showed no significant difference for
regimen and tumor type (superficial vs nodular) [41]. early treatment failure in the two regimens [51].
A European multicenter RCT [42] evaluating imiquimod The use of imiquimod has been evaluated in combination
(7 times/week for 6 weeks) clinical efficacy versus vehicle con- with other treatment modalities in order to improve its effec-
cluded that cure (based on both clinical and histologic clear- tiveness in the treatment of nodular BCCs [32]. A double-
ance) was achieved in 77 versus 6% of cases (p < 0.001) and blind, vehicle-controlled study on 20 patients with nodular
that histologic clearance occurred in 80 and 6% respectively BCCs evaluated the efficacy of curettage and electrodesicca-
(p < 0.001). tion followed by imiquimod in reducing the frequency of
Various imiquimod treatment regimens have been used residual tumor compared with curettage and electrodesicca-
with positive outcomes. A multicenter 6-week dose-response tion alone [52]. The subjects were randomized to an imiqui-
trial [43] evaluating different dosing schedules in 99 subjects mod (n = 10) or vehicle (n = 10) treatment group. After
treated with imiquimod 5% cream showed higher histologic 8 weeks of treatment, only one subject treated with imiqui-
clearance rates for twice-daily applications six times a week mod showed a residual tumor (10%) compared with four
(100%) compared with a less frequent dosing regimen (88, treated with vehicle (40%). Similarly, in an open-label study,
73 and 70% for once-daily, 6-times-weekly and 3-times- 17 subjects with a total of 34 nodular BCCs on the trunk
weekly regimens, respectively). Another RCT reported similar and limbs were treated with imiquimod following curettage
results showing decreasing histologic clearance rates (100, 87, (without electrodesiccation). After 3 months, 32 of 34 treated
81 and 52%) for less frequent applications (respectively twice- nodular BCCs (94%) showed no histologic evidence of resid-
daily, once-daily, 5 days/week and 3 days/week); clearance ual tumor [53]. Two previous clinical trials investigating the
rate for vehicle was 19% [44]. In one study designed to com- long-term histologic clearance obtained with postoperative
pare five to seven applications a week for a 6-week period, use of imiquimod 5% cream reported histologic clearance,
no statistical difference in clinical or histologic clearance was thus supporting imiquimod 5% as an adjunctive therapy after
noted between the two regimens [45]. Thus, five applications surgical removal of the primary BCCs [54,55]. In one of these
a week is preferred, as it provides a balance of efficacy and open-label studies, initial treatment with curettage was fol-
safety with minimal side effects. Similar results are supported lowed by once-daily application of imiquimod 5% cream
by a more recent, open-label clinical trial [46]. 5 times/week for 6 weeks: all 17 treated nodular BCCs
Topical imiquimod 5% in the treatment of nodular BCCs (100%) showed no histological evidence of residual tumor
has been investigated in several studies, showing poor efficacy on the post-treatment excision [54]. In the other study,
as a monotherapy compared with surgical excision, most a 36-month clinical experience on the use of imiquimod
likely due to skin barrier effect and deeper localization of 5% cream (applications once a day, 5 days/week for 6 weeks)
tumor cells [26]. Two Phase II studies were conducted: a following curettage of biopsy-confirmed nodular BCCs,
1518 Expert Opin. Pharmacother. (2010) 11(9)
Micali, Lacarrubba, Dinotta, Massimino & Nasca
reported a clearance rate of 96% along with a satisfactory the treatment [74], or the development of a more invasive mel-
cosmetic outcome [55]. anoma [71]. Interestingly, the use of topical imiquimod has
A recent RCT evaluating the preoperative effectiveness of also been suggested as a preoperative treatment to reduce the
imiquimod 5% cream applied nightly for 6 weeks with occlu- bulk of lentigo maligna before surgical removal, with
sion to nodular BCC on the nose, in reducing the level of the intent of improving cosmetic outcome of the surgical
Mohs stages, defect size, cost of Mohs surgery, and recon- excision [72].
struction, indicated that imiquimod was not effective as a
neoadjuvant treatment in nodular BCCs [56]. 3.5 Safety
Finally, some case reports have claimed positive responses Topical imiquimod is generally well tolerated. However,
to topical imiquimod 5% in large superficial BCCs [57,58] patients may experience moderate to severe application-site irri-
and multiple BCCs as observed in Gorlin syndrome [59,60]. tation, which may occasionally extend beyond the application
site. Such reactions include burning, pruritus, pain, tenderness,
Expert Opin. Pharmacother. Downloaded from informahealthcare.com by University of Aberdeen on 06/02/13
3.3 Bowens disease erythema, edema, vesicles, erosions, ulcerations, excoriations,
Some RCTs have assessed imiquimod 5% cream efficacy and exudation and crusting (Figures 1, 2 and 3) [32]. Acute,
safety in the topical treatment of Bowens disease. In a double- severe reactions require temporary discontinuation (generally
blind, placebo-controlled trial, 31 subjects with biopsy- 1 -- 2 weeks). Also, superficial scarring, pigmentary changes,
proven Bowens disease were randomized to receive either and, rarely, onset of other dermatoses (psoriasis, pemphigus
imiquimod 5% cream or vehicle, as a daily application for foliaceus, aphthosis, vitiligo, angioedema, eruptive epidermoid
16 weeks [61]. At the end of the study, 75% of treated subjects cysts) have been reported [75-81]. Although systemic absorption
showed both clinical and histologic resolution, with no relapse is low, influenza-like, gastrointestinal symptoms (fatigue, fever
during a 9-month follow-up period. By contrast, no improve- and chills, arthralgias, myalgias, nausea, diarrhea) or induction
ment was recorded in the placebo group. The presence of 25% of nondermatologic disorders (chronic neuropathic pain, auto-
non-responders in the imiquimod-treated group was attrib- immune spondyloarthropathy) have also, though rarely, been
uted to the presence of thick, hyperkeratotic lesions. Similar reported [26,82,83].
For personal use only.
results were reported by several nonrandomized clinical trials Sunlight exposure to the application site should be avoided
and case reports [19,62-64]. or minimized because imiquimod heightens sunburn suscepti-
Finally, some studies show favorable evidence for the bility; similarly, the concurrent use of sunscreen should be
use of topical 5% imiquimod in the treatment of erythro- encouraged. Safety of topical imiquimod during pregnancy
plasia of Queyrat [19,64,65]. Despite the absence of RCTs, is not established and thus its use is not recommended. Ani-
topical imiquimod is accepted as alternative therapy by mal studies have not shown clear evidence of teratogenicity
some practitioners. As such, imiquimod 5% has been success- or fetotoxicity, but with FDA pregnancy category, contracep-
fully used 3 times a week for 4 weeks, followed by progres- tion is generally recommended for women of childbearing age
sive reduction in dosing to complete clinic resolution (at while using topical imiquimod [84].
8 weeks) [64,65].
4. Diclofenac
3.4 Lentigo maligna
Imiquimod has been suggested as a possible alternative treat- The upregulation of arachidonic acid metabolism, due
ment for lentigo maligna, although no RCTs establishing to overexpression of cyclooxygenase enzymes (primarily
its long-term efficacy, treatment schedule and regimen are COX-2), may promote carcinogenic effects [85]. Thus, arach-
clearly defined. idonic acid metabolites have been shown to play a possible
The first reported case proposing the therapeutic role of role in promoting epithelial tumor growth by stimulating
imiquimod in lentigo maligna dates back to 2000 [66]. Since angiogenesis, inhibiting apoptosis and increasing invasiveness
then, several uncontrolled studies and case reports have of tumor cells [86-89]. Several studies have shown NSAIDs to
favorably described the possible role of imiquimod 5% in be safe and effective for the treatment of precancerous lesions,
treating lentigo maligna and with clinical, dermatoscopic including actinic keratoses, apparently via COX-2 inhibition.
and histologic resolution [67-73]. Also, they may play a role in preventing the development of
Naylor et al. reported a high rate of complete clinical and nonmelanoma skin cancers [3,85,87,88,90].
histologic clearance and no relapses at 1-year follow-up in Diclofenac is a potent NSAID that acts as an inhibi-
80% of 28 patients, using daily topical imiquimod 5% cream tor of COX-2. Recently, additional mechanisms of action
for 3 months [67]. Similar results are confirmed by a more recent have explained its therapeutic benefit by induction of
study of 48 subjects (37 complete responders, 11 no or partial apoptosis, alteration of cell proliferation and inhibition of
response) with a mean follow-up duration of 49 months [70]. angiogenesis [91].
However, despite these results, some authors have reported Diclofenac 3% gel in 2.5% hyaluronic acid (DHA) is FDA-
discordance between clinical and histological clearance rates, approved for actinic keratoses and has also been demonstrated
together with possible recurrence of the disease at the end of to be effective in the treatment of Bowens disease.
Expert Opin. Pharmacother. (2010) 11(9) 1519
Treating skin cancer with topical cream
4.1 Actinic keratoses 5. Retinoids
Several studies suggest DHA is a safe and effective topi-
cal therapy for actinic keratoses [3,9,33,91-97]. The FDA- Retinoids are vitamin A derivatives that act by binding
approved regimen consists of twice-daily applications for up nuclear receptors involved in gene transcription. As a conse-
to 12 weeks. quence, retinoids control cell proliferation and differentiation
Two vehicle-controlled studies have evaluated the effi- and might potentially interfere with the tumor-promotion
cacy of twice-daily applications of DHA in actinic kera- phase of carcinogenesis by inducing apoptosis [4].
toses [93,96]. In one study of 48 subjects, DHA provided Among topical retinoids, tretinoin cream 0.05 -- 0.1% and
total resolution in 33% of subjects (vs 10% of those treated adapalene gel 0.1 -- 0.3% have been used in the treatment of
with vehicle) after 60 days of treatment [96]. In another study actinic keratoses.
of 120 subjects, DHA totally cleared target lesions in 50%
of subjects (vs 20% of those treated with vehicle) after 5.1 Actinic keratoses
Expert Opin. Pharmacother. Downloaded from informahealthcare.com by University of Aberdeen on 06/02/13
90 days [93]. Topical tretinoin, approved by the FDA for the treatment
In another Phase IV, open-label study, subjects were treated of the cutaneous manifestations of photo-aging, has been
twice daily with DHA for a period of 90 days with a follow- used at varying concentrations as a single or combination
up assessment at 30 days post-treatment. The rate of respond- treatment for facial actinic keratoses, showing some efficacy
ers demonstrating actinic keratose clearance 75% were in reducing the number of lesions [4,9]. Different treatment
78 and 85% after 90 and 120 days respectively [92]. regimens have been proposed. In a comparative study, a
As regards comparator studies, a randomized, open- higher dose response, in terms of cure rate, has been
label, 12-week study of 49 subjects with actinic kera- obtained with the 0.3% formulation (55%) compared
toses showed a complete response in 12% of subjects treated with the 0.1% formulation (35%) [9,99]. A multicenter study
with once-daily applications of DHA (vs 22% of subjects on 1265 patients treated with tretinoin 0.05% or 0.1% or
treated with imiquimod 5% cream 3 times a week) [95]. In vehicle for about 15 months indicated tretinoin 0.1% twice
another study, DHA (applied twice daily for 90 days) led daily to be the most effective treatment (p < 0.001). Over-
For personal use only.
to clearance of 89% of actinic keratose lesions (vs 98% of all, 73% of tretinoin-treated patients showed a reduction in
those treated with 5-fluorouracil applied twice daily for the total number of lesions, compared with 40% of the
28 days) [97]. vehicle group [4,100,101].
Because follow-up is limited to 30 days in these studies, The efficacy and tolerability of isotretinoin 0.1% cream in
data on long-term efficacy of DHA for actinic keratose the treatment of actinic keratoses were evaluated in a double-
progression and regression are still lacking and need to be blind, parallel-group study on 100 subjects randomly assigned
investigated more [9]. to treatment with 0.1% cream or vehicle twice daily for
24 weeks to the face, the scalp and the upper extremities [102].
4.2 Bowens disease On the face, 66% of subjects treated with isotretinoin
So far, no RCTs have been reported on the evaluation of the achieved a > 30% reduction in lesion count compared with
effectiveness of in the treatment of Bowens disease. Anedoc- 45% of subjects treated with vehicle [102].
tal reports include two cases treated with DHA twice daily Interestingly, retinoids may enhance the effectiveness of
for about 3 months with clinical and histological clearance fluorouracil by improving its percutaneous absorption [4,101].
at the end of the treatment [98]. More recent reports on A double-blind, controlled study on 19 subjects applying fluo-
five patients with histology-proven Bowens disease, showed rouracil 5% cream to actinic keratoses on each arm twice daily,
similar results with once-daily application for 8 weeks [61]. followed by nightly application of tretinoin 0.05% cream to
These preliminary findings support the use of DHA for one arm, and a control cream to the other, revealed after
selected cases. However, additional investigations to define 3 months of treatment that the tretinoin-treated cohort had a
optimum dosage regimens and long-term follow-up are meaningful statistical improvement (p < 0.04) compared
needed [19]. with the control cohort [103].
In a prospective randomized, controlled study, 90 subjects
4.3 Safety with actinic keratoses and photodamage were randomized
DHA is considered a well-tolerated treatment by most to either adapalene gel (0.1 or 0.3%) or vehicle, once daily
patients, with mild irritant side effects at application sites for 4 weeks, followed by twice-daily application up to
(considerably lower compared with other treatments, such as 9 months [104]. Participants receiving adapalene gel 0.1 or
fluorouracil and imiquimod) and a satisfactory cosmetic out- 0.3% achieved a dose-dependent reduction in the number
come. However, pruritus and rash may occur [9]. Of note, its of actinic keratoses. Overall, 62 and 66% of subjects in the
use should be carefully considered in certain conditions, such adapalene gel 0.1 and 0.3% groups, respectively, were consid-
as in the case of positive history for bleeding diathesis, hepatic ered to have shown clear, marked or moderate improvement
dysfunction or known hypersensitivity to any component of in actinic keratoses compared with 34% of those treated
the medication [3,91,94]. with vehicle [104].
1520 Expert Opin. Pharmacother. (2010) 11(9)
Micali, Lacarrubba, Dinotta, Massimino & Nasca
5.2 Basal cell carcinoma keratoses in consideration of the field cancerization phenom-
Some studies have supported the efficacy of tazarotene, a enon. This finding -- for example the presence of histologically
selective retinoic acid receptor (RAR) ligand, in reducing the abnormal tissue surrounding an invasive squamous cell
expression of retinoid-induced tumor suppressor and inhibit- carcinoma -- was first described in tumors of the upper gastro-
ing tumor cell formation in mouse models [105,106]. In one intestinal system in 1953 [109]. As actinic keratoses represent
clinical study including 30 subjects, topical tazarotene 0.1% the earliest, clinically detectable cutaneous lesions of multi-
gel was applied once daily up for 20 weeks to treat multi- focal, preneoplastic areas of dysplastic keratinocytes that
ple superficial BCCs. Complete cure rate was achieved can extend beyond visible lesions, or that might appear years
in 58.5% of lesions after a mean 11-week duration of later, the use of topical agents to promote reversal of neo-
treatment [107]. plastic transformation in surrounding tissue may provide a
field effect on subclinical disease and contribute to the
5.3 Lentigo maligna prevention of further tumor development in adjacent
Expert Opin. Pharmacother. Downloaded from informahealthcare.com by University of Aberdeen on 06/02/13
In one study, two elderly subjects with facial lentigo maligna areas [110,111].
showed complete regression, both clinical and histopa- Fluorouracil, the first topical medication approved for
thologic, after once-daily topical treatment with tazarotene actinic keratoses, is also effective in treating BCCs and
0.1% gel for 6 -- 8 months. After a follow-up period of Bowens disease. However, it provides cytotoxic action that
18 and 30 months, no recurrence was observed [108]. can also destroy adjacent tissues. Efficacy of fluorouracil is
dose-related and depends on skin-barrier penetration of the
5.4 Safety applied formulation. Thicker, hypertrophic lesions may need
Topical retinoids may be responsible for mild to moderate to be pretreated with keratolytic agents or gentle curettage.
local side effects consisting of erythema, peeling, dryness, Generally, patients who develop an intense inflammatory
burning and pruritus [101,104] that may lead to patient dis- reaction obtain a greater clinical response. The use of topical
continuation or noncompliance. Retinoids may also induce fluorouracil without close clinical follow-up or histologic
sun hypersensitivity, thus sun exposure to application site confirmation of cure may lead to the persistence of invasive
For personal use only.
should be minimized, and the use of concurrent appropriate tumors and their occult progression.
sunscreens recommended. At this point in time, imiquimod 5% cream represents a
more versatile agent. Although FDA-approved only for actinic
6. Conclusions keratoses and superficial BCCs, its off-label use includes
Bowens disease, erythroplasia of Queyrat and lentigo maligna,
Several studies have demonstrated the usefulness of topical with excellent outcome. Although there is an RCT for Bowens
pharmacotherapy in the treatment of cutaneous malignancies. disease, optimal dosage and duration of therapy for each off-
Noninvasive, tissue-sparing, topical, self-administered treat- label use, as well as long-term efficacy, should be assessed
ments represent a highly desirable alternative option, both through additional RCTs. An important issue that needs to
in aged and unhealthy patients who may be poor surgical can- be highlighted is the frequent occurrence of irritation during
didates, as well as in relatively young subjects with lesions imiquimod therapy, including burning, pruritus, pain, tender-
located on cosmetically sensitive areas wishing to avoid ness, erythema, edema, vesicles, erosions, ulcerations, excoria-
disfiguring scars. tions, exudation and crusting. As for fluorouracil treatment,
the ability to develop an inflammatory reaction to imiquimod
7. Expert opinion is a good predictor of the therapeutic effect, and expert
physicians can easily manage it without further complications.
Topical pharmacotherapy offers effective alternative treat- DHAs efficacy is at present limited to actinic keratoses, in
ments for skin cancer, although careful patient selection is which the overall clearance rate slightly lower than that of
required to achieve the desired goal of complete tumor clear- fluorouracil and imiquimod. However, DHA, with better tol-
ance. Therapeutic response is related both to tumor type, erability, may represent an alternative for those patients who
extension and localization, as well as to the ability of the are not willing to tolerate the typical side effects associated
patient to be compliant. The advantages and disadvantages with fluorouracil and imiquimod. So far, no RCTs have
for topical treatment available for skin cancers are summarized been carried out to evaluate DHA efficacy in other cutaneous
in Table 1. malignancies. However, some studies seem to support its use
Undoubtedly, noninvasive topical pharmacotherapy in Bowens disease for selected cases and further investigation
deserves first-line treatment status for actinic keratoses. Topi- is needed.
cal compounds containing fluorouracil 5 or 0.5%, imiquimod The cure rate of actinic keratoses seems to be lower for ret-
5%, DHA 3% or tretinoin 0.1% have all demonstrated inoids compared with other topical treatments. Moreover, a
efficacy in randomized trials with variable outcome rates. prolonged treatment (up to 15 months) is usually required.
Moreover, topical therapy may often be preferred to more Therefore, this treatment does not compare favorably with
destructive or invasive treatments in the treatment of actinic more rapidly effective treatments for actinic keratoses.
Expert Opin. Pharmacother. (2010) 11(9) 1521
Treating skin cancer with topical cream
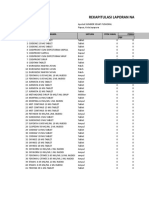
Table 1. Topical treatments for skin cancers: advantages and disadvantages.
Indication Therapeutic options Advantages Disadvantages
Actinic keratoses Imiquimod 5% Short and long-term efficacy Mild to severe side effects
with high RR at application site
Several recent RCTs available High cost
Fluorouracil 0.5 -- 5% Short and long-term efficacy Few recent RCTs available
with high RR Mild to severe side effects
at application site
Diclofenac 3% in 2.5% Short-term efficacy with high RR Lack of data on long-term efficacy
hyaluronic acid Recent RCTs available
Mild side effects
Retinoids Short-term efficacy with moderate RR Lack of data on long-term efficacy
Expert Opin. Pharmacother. Downloaded from informahealthcare.com by University of Aberdeen on 06/02/13
Mild side effects
Basal cell carcinoma Imiquimod 5% Short- and long-term efficacy with Mild to severe side effects
high RR for superficial BCC at application site
Short and long-term efficacy with High cost
moderate RR for nodular BCC
Several recent RCTs available
Fluorouracil 5% Short and long-term efficacy Limited RCTs available
with high RR Mild to severe side effects
at application site
Retinoids Some data of short-term efficacy with Lack of RCTs
moderate RR
Mild side effects
Bowens disease Imiquimod 5% Short-term efficacy with high RR Limited data on long-term efficacy
Recent RCTs available Mild to severe side effects
at application site
For personal use only.
High cost
Fluorouracil 5% Short- and long-term efficacy Lack of RCTs
with high RR Mild to severe side effects
at application site
Diclofenac 3% in 2.5% Some data on short-term efficacy Lack of RCTs
hyaluronic acid with high RR
Mild side effects
Erythroplasia of Queyrat Imiquimod 5% Some data on short-term efficacy Lack of RCTs
with high RR Mild to severe side effects
at application site
High cost
Lentigo maligna Imiquimod 5% Some data on short-term efficacy Lack of RCTs
with high RR Mild to severe side effects
at application site
High cost
Retinoids Few data on short-term efficacy Lack of RCTs
High RR: 70%.
Moderate RR: 40 -- 69%.
BCC: Basal cell carcinoma; RCTs: Randomized controlled trials; RR: Resolution rate.
Of note, the preliminary results in treating BCCs and lentigo agents (e.g., fluorouracil and retinoids) standardized optimal
maligna with retinoids have not been confirmed by concentrations have not necessarily been assessed for each
other studies. possible indication or clinical use.
Some of these treatments carry an individual response that As the ultimate goal is to treat patients successfully with the
could be essential for achievement of clinical and histologic best risk-to-benefit treatment options, more controlled clinical
cure. For example, both the inflammatory reaction and trials are necessary, as well as the development of new molecules
therapeutic effects of imiquimod are not always dose-related, with enhanced efficacy and reduced side effects. The potential
and may vary among patients depending on an un- of new applications is that they may be applied to a wide vari-
predictable individual response. This implies that close ety of cutaneous malignancies. Certainly, treatment of skin
clinical supervision and clinical experience are essential for tumors with immunomodulators is an important advance,
accurate interpretation of outcome. In addition, for some and industry and scientists are focusing on this and related
1522 Expert Opin. Pharmacother. (2010) 11(9)
Micali, Lacarrubba, Dinotta, Massimino & Nasca
A. B.
Expert Opin. Pharmacother. Downloaded from informahealthcare.com by University of Aberdeen on 06/02/13
Figure 1. A. Small superficial BCC. B. Mild application-site reaction during IQ treatment: erythema, vesicles and erosions.
A. B.
For personal use only.
Figure 2. A. Nodular BCC. B. Moderate application-site reaction during IQ treatment: erythema, oedema, vesicles and
exudation.
A. B.
Figure 3. A. Large superficial BCC. B. Severe application-site reaction during IQ treatment: erythema, oedema, ulcerations,
exudation and crusting.
Expert Opin. Pharmacother. (2010) 11(9) 1523
Treating skin cancer with topical cream
fields. In our opinion, future development should include other Declaration of interest
immune response modifiers such as resiquimod, an analogue of
imiquimod that shows encouraging preliminary results for The authors state no conflict of interest and have received no
actinic keratoses [112]. payment in preparation of this manuscript.
Bibliography
1. McGuire JF, Ge NN, Dyson S. fluorouracil cream applied to each side of treatment options. Ther Clin
Nonmelanoma skin cancer of the head the face in patients with actinic keratosis. Risk Manag 2008;4:1085-95
and neck I: histopathology and clinical Clin Ther 2002;24:990-1000 20. Bargman H, Hochman J.
behaviour. Am J Otolaryngol 11. McIntyre WJ, Downs MR, Bedwell SA. Topical treatment of Bowens disease
2009;30:121-33 Treatment options for actinic keratoses. with 5-fluorouracil. J Cutan Med Surg
2. Lacarrubba F, Nasca MR, Micali G. Am Fam Physician 2007;76:667-71 2003;7:101-5
Expert Opin. Pharmacother. Downloaded from informahealthcare.com by University of Aberdeen on 06/02/13
Advances in the use of topical 12. Jorizzo J, Stewart D, Bucko A, et al. 21. Salim A, Leman JA, McColl JH, et al.
imiquimod to treat dermatologic Randomized trial evaluating a new 0.5% Randomized comparison of
disorders. Ther Clin Risk Manag fluorouracil formulation demonstrates photodynamic therapy with topical
2008;4:87-97 efficacy after 1-, 2-, or 4-week treatment 5-fluorouracil in Bowens disease.
3. McGillis ST, Fein H. Topical treatment in patients with actinic keratosis. Cutis Br J Dermatol 2003;148:539-43
strategies for non-melanoma skin cancer 2002;70:335-9 22. Garland SM. Imiquimod. Curr Opin
and precursor lesions. Semin Cutan 13. Yentzer B, Hick J, Williams L, et al. Infect Dis 2003;16:85-9
Med Surg 2004;23:174-83 Adherence to a topical regimen of 23. Schon M, Schon MP. The antitumoral
4. Weinberg JM. Topical therapy for actinic 5-fluorouracil, 0.5%, cream for the mode of action of imiquimod and other
keratoses: current and evolving therapies. treatment of actinic keratoses. imidazoquinolines. Curr Med Chem
Rev Recent Clin Trials 2006;1:53-60 Arch Dermatol 2009;145:203-5 2007;14:681-7
5. Askew DA, Mickan SM, Soyer HP, 14. Weiss J, Menter A, Hevia O, et al. 24. Schon MP, Schon M. Imiquimod: mode
For personal use only.
Wilkinson D. Effectiveness of Effective treatment of actinic keratosis of action. Br J Dermatol
5-fluorouracil treatment for actinic with 0.5% fluorouracil cream for 1, 2, or 2007;157(Suppl 2):8-13
keratosis -- a systematic review of 4 weeks. Cutis 2002;70:22-9
25. Ceilley RI, Del Rosso JQ.
randomized controlled trials. 15. Krawtchenko N, Roewert-Huber J, Current modalities and new advances in
Int J Dermatol 2009;48:453-63 Ulrich M, et al. A randomised study of the treatment of basal cell carcinoma.
6. Dillaha CJ, Jansen GT, Honeycutt WM, topical 5% imiquimod vs. topical Int J Dermatol 2006;45:489-9
Holt GA. Further studies with topical 5-fluorouracil vs. cryosurgery in
26. Chang YC, Madkan V, Cook-Norris R,
5-fluorouracil. Arch Dermatol immunocompetent patients with actinic
et al. Current and potential uses of
1965;92:410-17 keratoses: a comparison of clinical and
imiquimod. South Med J
7. Kurwa HA, Yong Gee SA, Seed P, et al. histological outcomes including 1-year
2005;98:914-20
A randomized paired comparison of follow-up. Br J Dermatol
2007;157(Suppl 2):34-40 27. Patel GK, Goodwin R, Chawla M, et al.
photodynamic therapy and topical
Imiquimod 5% cream monotherapy for
5-fluorouracil in the treatment of actinic 16. Romagosa R, Saap L, Givens M, et al.
cutaneous squamous cell carcinoma
keratoses. J Am Acad Dermatol A pilot study to evaluate the treatment of
in situ (Bowens disease): a randomized,
1999;41:414-18 basal cell carcinoma with 5-fluorouracil
double blind, placebo-controlled trial.
8. Witheiler DD, Lawrence N, Cox SE, using phosphatidyl choline as a
J Am Acad Dermatol 2006;54:1025-32
et al. Long-term efficacy and safety of transepidermal carrier. Dermatol Surg
2000; 26:338-40 28. Sauder DN. Imiquimod: modes of
Jessners solution and 35% trichloroacetic
action. Br J Dermatol
acid vs 5% fluorouracil in the treatment 17. Gross K, Kircik L, Kricorian G.
2003;149(Suppl 66):5-8
of widespread facial actinic keratoses. 5% 5-Fluorouracil cream for the
Dermatol Surg 1997;23:191-6 treatment of small superficial Basal cell 29. Schiller M, Metze D, Luger TA, et al.
carcinoma: efficacy, tolerability, cosmetic Immune response modifiers-mode of
9. de Berker D, McGregor JM,
outcome, and patient satisfaction. action. Exp Dermatol 2006;15:331-41
Hughes BR; British Association of
Dermatologists Therapy Guidelines and Dermatol Surg 30. Berman B, Sullivan T, De Araujo T,
Audit Subcommittee. Guidelines for the 2007;33:433-9;discussion 440 et al. Expression of Fas-receptor on basal
management of actinic keratoses. 18. Moreno G, Chia AL, Lim A, cell carcinomas after treatment with
Br J Dermatol Shumack S. Therapeutic options for imiquimod 5% cream or vehicle.
2007;156:222-30, Erratum in: Br J Bowens disease. Australas J Dermatol Br J Dermatol
Dermatol 2008;158:873 2007;48:1-8, Erratum in: Australas J 2003;149(Suppl 66):59-61
10. Loven K, Stein L, Furst K, Levy S. Dermatol 2007;48:142 31. Li VW, Li WW, Talcott KE, Zhai AW.
Evaluation of the efficacy and tolerability 19. Neubert T, Lehmann P. Imiquimod as an antiangiogenic agent.
of 0.5% fluorouracil cream and 5% Bowens disease -- a review of newer J Drugs Dermatol 2005;4:708-17
1524 Expert Opin. Pharmacother. (2010) 11(9)
Micali, Lacarrubba, Dinotta, Massimino & Nasca
32. Gaspari A, Tyring SK, Rosen T. from a randomized vehicle-controlled comparing low-frequency dosing with
Beyond a decade of 5% imiquimod phase III study in Europe. Br J Dermatol and without occlusion. Br J Dermatol
topical therapy. J Drugs Dermatol 2005;152:939-47 2002;147:1227-36
2009;8:467-74 43. Marks R, Gebauer K, Shumack S, et al.; 52. Spencer JM. Pilot study of imiquimod
33. Gebauer K, Shumack S, Cowen PS. Australasian Multicentre Trial Group. 5% cream as adjunctive therapy to
Effect of dosing frequency on the safety Imiquimod 5% cream in the treatment curettage and electrodesiccation for
and efficacy of imiquimod 5% cream for of superficial basal cell carcinoma: results nodular basal cell carcinoma.
treatment of actinic keratosis on the of a multicenter 6-week dose-response Dermatol Surg 2006;32:63-9
forearms and hands: a phase II, trial. J Am Acad Dermatol 53. Wu JK, Oh C, Strutton G, Siller G.
randomized placebo-controlled trial. 2001;44:807-13 An open-label, pilot study examining the
Br J Dermatol 2009;161:897-903 44. Geisse JK, Rich P, Pandya A, et al. efficacy of curettage followed by
34. Stockfleth E, Ulrich C, Imiquimod 5% cream for the treatment imiquimod 5% cream for the treatment
Lange-Asschenfeldt B, et al. Treatment of of superficial basal cell carcinoma: of primary nodular basal cell carcinoma.
Expert Opin. Pharmacother. Downloaded from informahealthcare.com by University of Aberdeen on 06/02/13
multiple, multiform actinic keratoses on a double-blind, randomized Australas J Dermatol 2006;47:46-8
the head with imiquimod 5% cream. vehicle-controlled study. J Am 54. Neville JA, Williford PM, Jorizzo JL.
Eur J Dermatol 2009;19:355-9 Acad Dermatol 2002;47:390-8 Pilot study using topical imiquimod 5%
35. Hadley G, Derry S, Moore RA. 45. Geisse J, Caro I, Lindholm J, et al. cream in the treatment of nodular basal
Imiquimod for actinic keratoses: Imiquimod 5% cream for the treatment cell carcinoma after initial treatment with
systematic review and meta-analysis. of superficial basal cell carcinoma: results curettage. J Drugs Dermatol
J Invest Dermatol 2006;126:1251-5 from two phase III, randomized, 2007;6:910-14
36. Falagas ME, Angelousi AG, Peppas G. vehicle-controlled studies. J Am 55. Tillman DK Jr, Carroll MT.
Imiquimod in the treatment of actinic Acad Dermatol 2004;50:722-33 A 36-month clinical experience of the
keratosis. A meta-analysis of randomized 46. Schiessl C, Wolber C, Tauber M, et al. effectiveness of curettage and imiquimod
controlled trials. J Am Acad Dermatol Treatment of all basal cell carcinoma 5% cream in the treatment of basal cell
2006;55:537-8 variants including large and high-risk carcinoma. J Drugs Dermatol
lesions with 5% imiquimod cream: 2008;7(1 Suppl 1):7-14
For personal use only.
37. Gupta AK, Davey V, Mcphail H.
Evaluation of the effectiveness of histological and clinical changes, 56. Butler DF, Parekh PK, Lenis A.
imiquimod and 5-fluorouracil for the outcome, and follow-up. Imiquimod 5% cream as adjunctive
treatment of actinic keratosis: critical J Drugs Dermatol 2007;6:507-13 therapy for primary, solitary, nodular
review and meta-analysis of efficacy 47. Shumack S, Robinson J, Kossard S, et al. nasal basal cell carcinomas before Mohs
studies. J Cutan Med Surg Efficacy of topical 5% imiquimod cream micrographic surgery: a randomized,
2005;9:209-14 for the treatment of nodular basal cell double blind, vehicle-controlled study.
38. Stockfleth E, Christophers E, carcinoma: comparison of dosing Dermatol Surg 2009;35:24-9
Benninghoff B, Sterry W. Low incidence regimens. Arch Dermatol 57. Shumack S, Gebaeuer K, Quirk C, et al.
of new actinic keratoses after topical 5% 2002;138:1165-71 5% imiquimod cream for the treatment
imiquimod cream treatment: a long-term 48. Eigentler TK, Kamin A, Weide BM, of a large superficial basal cell carcinoma.
follow-up study. Arch Dermatol et al. A phase III, randomized, open label Arch Dermatol 2004;140:1286-7
2004;140(12):1542 study to evaluate the safety and efficacy 58. Micali M, Nasca MR, Musumeci ML.
39. Zeichner JA, Stern DW, Uliasz A, et al. of imiquimod 5% cream applied thrice Treatment of an extensive superficial
Placebo-controlled, double-blind, weekly for 8 and 12 weeks in the basal cell carcinoma of the face with
randomized pilot study of imiquimod treatment of low-risk nodular basal cell imiquimod 5% cream. Int J Tissue React
5% cream applied once per week for carcinoma. J Am Acad Dermatol 2005;27:111-14
6 months for the treatment of actinic 2007;57:616-21
59. Micali G, Lacarrubba F, Nasca MR,
keratoses. J Am Acad Dermatol 49. Vidal D, Matas-Guiu X, Alomar A. et al. The use of imiquimod 5% cream
2009;60:59-62 Fifty-five basal cell carcinomas treated for the treatment of basal cell carcinoma
40. Price NM. The treatment of actinic with topical imiquimod: outcome at as observed in Gorlins syndrome.
keratoses with a combination of 5-year follow-up. Arch Dermatol Clin Exp Dermatol
5-fluorouracil and imiquimod creams. 2007;143:266-8 2003;28(Suppl 1):19-23
J Drugs Dermatol 2007;6:778-81 50. Gollnick H, Barona CG, Frank RG, 60. Kagy MK, Amonette R. The use of
41. Bath-Hextall FJ, Bong J, Perkins W, et al. Recurrence rate of superficial basal imiquimod 5% cream for the treatment
et al. Interventions for basal cell cell carcinoma following treatment with of superficial basal cell carcinomas in a
carcinoma of the skin (Cochrane review). imiquimod 5% cream: conclusion of a basal cell nevus syndrome patient.
Cochrane Database Syst Rev 5-year long-term follow-up study in Dermatol Surg 2000;26:577-8
2007;1:CD003412 Europe. Eur J Dermatol 2008;18:677-82
61. Patel MJ, Stockfleth E. Does progression
42. Schulze HJ, Cribier B, Requena L, et al. 51. Sterry W, Ruzicka T, Herrera E, et al. from actinic keratosis and Bowens
Imiquimod 5% cream for the treatment Imiquimod 5% cream for the treatment disease end with treatment: diclofenac
of superficial basal cell carcinoma: results of superficial and nodular basal cell 3% gel, an old drug in a new
carcinoma: randomized studies
Expert Opin. Pharmacother. (2010) 11(9) 1525
Treating skin cancer with topical cream
environment? Br J Dermatol treatment of lentigo maligna with 87. Eberle J, Fecker LF, Forschner T, et al.
2007;156(Suppl 3):53-6 imiquimod. Dermatol Surg Apoptosis pathways as promising targets
62. Smith SR, Morhenn VB, Piacquadio DJ. 2009;35:1286-9 for skin cancer therapy. Br J Dermatol
Bilateral comparison of the efficacy and 75. Brown T, Zirvi M, Cotsarelis G, et al. 2007;156(Suppl 3):18-24
tolerability of 3% diclofenac sodium gel Vitiligo-like hypopigmentation associated 88. Fecker LF, Stockfleth E, Nindl I, et al.
and 5% 5-fluorouracil cream in the with imiquimod treatment of genital The role of apoptosis in therapy and
treatment of actinic keratoses of the face warts. J Am Acad Dermatol prophylaxis of epithelial tumours by
and scalp. J Drugs Dermatol 2005;52:715-16 nonsteroidal anti-inflammatory drugs
2006;5:156-9 76. Gilliet M, Conrad C, Geiges M, et al. (NSAIDs). Br J Dermatol
63. Mackenzie-Wood A, Kossard S, Psoriasis triggered by toll-like receptor 2007;156(Suppl 3):25-33
de Launey J, et al. Imiquimod 5% cream 7 agonist imiquimod in the presence of 89. Zhan H, Zheng H. The role of topical
in the treatment of Bowens disease. dermal plasmacytoid dendritic cell cyclo-oxygenase-2 inhibitors in skin
J Am Acad Dermatol 2001;44:462-70 precursors. Arch Dermatol cancer: treatment and prevention. Am J
Expert Opin. Pharmacother. Downloaded from informahealthcare.com by University of Aberdeen on 06/02/13
64. Alessi SS, Sanches JA, de Oliveira WR, 2004;140:1490-5 Clin Dermatol 2007;8:195-200
et al. Treatment of cutaneous tumors 77. Mashiah J, Brenner S. 90. Subbaramaiah K, Zakim D, Weksler BB,
with topical 5% imiquimod cream. Possible mechanisms in the induction of Dannenberg AJ. Inhibition of
Clinics 2009;64:961-6 pemphigus foliaceus by topical cyclooxygenase: a novel approach to
65. Micali G, Nasca MR, De Pasquale R. imiquimod treatment. Arch Dermatol cancer prevention. Proc Soc Exp
Erythroplasia of Queyrat treated with 2005;141:908-9 Biol Med 1997;216:201-10
imiquimod 5% cream. J Am 78. Zalaudek I, Petrillo G, Argenziano G. 91. Merk HF. Topical diclofenac in the
Acad Dermatol 2006;55:901-3 Aphthous ulcers and imiquimod. J Am treatment of actinic keratoses.
66. Ahmed I, Berth-Jones J. Imiquimod: Acad Dermatol 2005;53:360-1 Int J Dermatol 2007;46:12-8
a novel treatment for lentigo maligna. 79. Barton JC. Angioedema associated with 92. Nelson C, Rigel D, Smith S, et al.
Br J Dermatol 2000;143:843-5 imiquimod. J Am Acad Dermatol Phase IV, open-label assessment of the
67. Naylor MF, Crowson N, Kuwahara R, 2004;51:477-8 treatment of actinic keratosis with 3.0%
For personal use only.
et al. Treatment of lentigo maligna with 80. Marty CL, Randle HW, Walsh JS. diclofenac sodium topical gel (Solaraze).
topical imiquimod. Br J Dermatol Eruptive epidermoid cysts resulting from J Drugs Dermatol 2004;3:401-7
2003;149(Suppl 66):66-70 treatment with imiquimod. 93. Wolf JE Jr, Taylor JR, Tschen E,
68. Rajpar SF, Marsden JR. Imiquimod in Dermatol Surg 2005;31:780-2 Kang S. Topical 3.0% diclofenac in
the treatment of lentigo maligna. 81. Sriprakash K, Godbolt A. Vitiligo-like 2.5% hyaluronan gel in the treatment of
Br J Dermatol 2006;155:653-6 depigmentation induced by imiquimod actinic keratoses. Int J Dermatol
treatment of superficial basal cell 2001;40:709-13
69. Micali G, Lacarrubba F, Nardone B,
Nasca MR. Videodermatoscopy of carcinoma. Australas J Dermatol 94. Dirschka T, Bierhoff E, Pflugfelder A,
lentigo maligna treated with imiquimod. 2009;50:211-13 Garbe C. Topical 3.0% diclofenac in
J Drugs Dermatol 2008;7:1077-80 82. Yi BA, Nirenberg MJ, Goldstein SM, 2.5% hyaluronic acid gel induces
et al. Chronic neuropathic pain regression of cancerous transformation in
70. Powell AM, Robson AM,
associated with imiquimod: report of actinic keratoses. J Eur Acad
Russell-Jones R, Barlow RJ. Imiquimod
2 cases. J Am Acad Dermatol Dermatol Venereol 2010;24:258-63
and lentigo maligna: a search for
prognostic features in a 2005;52:57-8 95. Kose O, Koc E, Erbil AH, et al.
clinicopathological study with long-term 83. Benson E. Imiquimod: potential Comparison of the efficacy and
follow-up. Br J Dermatol risk of an immunostimulant. tolerability of 3% diclofenac sodium gel
2009;160:994-8 Australas J Dermatol 2004;45:123-4 and 5% imiquimod cream in the
treatment of actinic keratosis.
71. Junkins-Hopkins JM. Imiquimod use in 84. Scheinfeld N, Lehman DS.
J Dermatolog Treat 2008;19:159-63
the treatment of lentigo maligna. J Am An evidence-based review of medical and
Acad Dermatol 2009;61:865-7 surgical treatments of genital warts. 96. Rivers JK, Arlette J, Shear N, et al.
Dermatol Online J 2006;12(3):5 Topical treatment of actinic keratoses
72. Walling HW. Lentigo maligna: current
with 3.0% diclofenac in 2.5%
concepts in diagnosis and management. 85. Buckman SY, Gresham A, Hale P, et al.
hyaluronan gel. Br J Dermatol
G Ital Dermatol Venereol COX-2 expression is induced by UVB
2002;146:94-100
2009;144:149-55 exposure in human skin: implications for
the development of skin cancer. 97. Smith SR, Morhenn VB, Piacquadio DJ.
73. Navi D, Huntley A.
Carcinogenesis 1998;19:723-9 Bilateral comparison of the efficacy and
Imiquimod 5 percent cream and the
tolerability of 3% diclofenac sodium gel
treatment of cutaneous malignancy. 86. Masferrer JL, Leahy KM, Koki AT, et al.
and 5% 5-fluorouracil cream in the
Dermatol Online J 2004;10(1):4 Antiangiogenic and antitumor activities
treatment of actinic keratoses of the face
74. Woodmansee CS, McCall MW. of cyclooxygenase-2 inhibitors.
and scalp. J Drugs Dermatol
Recurrence of lentigo maligna and Cancer Res 2000;60:1306-11
2006;5:156-9
development of invasive melanoma after
1526 Expert Opin. Pharmacother. (2010) 11(9)
Micali, Lacarrubba, Dinotta, Massimino & Nasca
98. Dawe SA, Salisbury JR, Higgins E. 104. Kang S, Goldfarb MT, Weiss JS, et al. 110. Ulrich C. Topical treatment of field
Two cases of Bowens disease successfully Assessment of adapalene gel for the cancerization. Cancer Treat Res
treated topically with 3% diclofenac in treatment of actinic keratoses and 2009;146:439-46
2.5% hyaluronan gel. Clin Exp Dermatol lentigines: a randomized trial. J Am 111. Vatve M, Ortonne JP,
2005;30:712-13 Acad Dermatol 2003;49:83-90 Birch-Machin MA, Gupta G.
99. Bollag W, Ott F. Retinoic acid: topical 105. Lee S, Selva D, Huilgol SC, et al. Management of field change in actinic
treatment of senile or actinic keratoses Pharmacological treatments for basal cell keratosis. Br J Dermatol
and basal cell carcinomas. Agents Actions carcinoma. Drugs 2007;67:915-34 2007;157(Suppl 2):21-4
1970;1:172-5 106. So PL, Fujimoto MA, Epstein EH Jr. 112. Szeimies RM, Bichel J, Ortonne JP,
100. Kligman AL, Thorne EG. Pharmacologic retinoid signaling and et al. A phase II dose-ranging study of
Topical therapy of actinic keratoses with physiologic retinoic acid receptor topical resiquimod to treat actinic
tretinoin. In: Marks R, editor, Retinoids signaling inhibit basal cell carcinoma keratosis. Br J Dermatol
in Cutaneous Malignancy. Blackwell tumorigenesis. Mol Cancer Ther 2008;159:205-10
Expert Opin. Pharmacother. Downloaded from informahealthcare.com by University of Aberdeen on 06/02/13
Scientific Publications, Oxford; 2008;7:1275-84
1991. p. 66-73 107. Peris K, Ferrari A, Fargnoli MC, et al. Affiliation
101. Odom R. Managing actinic keratoses Dermoscopic monitoring of tazarotene Giuseppe Micali MD,
with retinoids. J Am Acad Dermatol treatment of superficial basal cell Francesco Lacarrubba MD, Franco Dinotta MD,
1998;39:S74-8 carcinoma. Dermatol Surg Doriana Massimino MD &
2005;31:217-20 Maria Rita Nasca MD PhD
102. Alirezai M, Dupuy P, Amblard P, et al.
Clinical evaluation of topical isotretinoin 108. Chimenti S, Carrozzo AM, Citarella L, Author for correspondence
in the treatment of actinic keratoses. et al. Treatment of lentigo maligna with University of Catania,
Dermatology Clinic,
J Am Acad Dermatol 1994;30:447-51 tazarotene 0.1% gel. J Am
Acad Dermatol 2004;50:101-3 A.O.U. Policlinico -- Vittorio Emanuele,
103. Bercovitch L. Topical chemotherapy of Via Santa Sofia, 78 95123 Catania, Italy
actinic keratoses of the upper extremity 109. Slaughter DP, Southwick HW, Tel: +39 095 321705; Fax: +39 095 3782425;
with tretinoin and 5-fluorouracil: Smejkal W. Field cancerization in oral
E-mail: cldermct@nti.it
For personal use only.
a double-blind controlled study. stratified squamous epithelium; clinical
Br J Dermatol 1987;116:549-52 implications of multicentric origin.
Cancer 1953;6:963-8
Expert Opin. Pharmacother. (2010) 11(9) 1527
Das könnte Ihnen auch gefallen
- 2019 Melasma - A Critical Analysis of Clinical Trials Investigating Treatment Modalities Published in The Past 10 YearsDokument6 Seiten2019 Melasma - A Critical Analysis of Clinical Trials Investigating Treatment Modalities Published in The Past 10 Yearsyezafig4001Noch keine Bewertungen
- Lasers e HiperpigmentaçãoDokument6 SeitenLasers e HiperpigmentaçãoRafael PioltineNoch keine Bewertungen
- JCutanAesthetSurg114211-3112943 083849Dokument6 SeitenJCutanAesthetSurg114211-3112943 083849Elaine Medeiros100% (1)
- Ali 2019Dokument8 SeitenAli 2019Ana Claudia Kordelos DinizNoch keine Bewertungen
- Kulichova2014 002Dokument12 SeitenKulichova2014 002JAVIYAROSNoch keine Bewertungen
- AnestesicoDokument9 SeitenAnestesicoTeo BurgosNoch keine Bewertungen
- Research Microneedling in DermatologyDokument10 SeitenResearch Microneedling in DermatologyErik BrooksNoch keine Bewertungen
- A Guide To Topical Vehicle FormulationsDokument6 SeitenA Guide To Topical Vehicle FormulationsPipim BayasariNoch keine Bewertungen
- JCutanAesthetSurg114211-2961181 081331Dokument6 SeitenJCutanAesthetSurg114211-2961181 081331Albert EdoNoch keine Bewertungen
- Dermatologia 2Dokument7 SeitenDermatologia 2Lilian S F BlumerNoch keine Bewertungen
- Jurnal AccDokument4 SeitenJurnal AccOlivia Chandra DeviNoch keine Bewertungen
- Corneal Opacity ManagementDokument5 SeitenCorneal Opacity ManagementAgWan Finger BillNoch keine Bewertungen
- Intra NasalDokument13 SeitenIntra NasalpetriliaNoch keine Bewertungen
- Cp201011 Practice Tools-363Dokument4 SeitenCp201011 Practice Tools-363Shawn BNoch keine Bewertungen
- A Novel at Home Procedure Providing Marked Improvements - 2014 - Journal of The PDFDokument1 SeiteA Novel at Home Procedure Providing Marked Improvements - 2014 - Journal of The PDFNachi MontianarrtNoch keine Bewertungen
- Microneedling Tratamiento en CicatricesDokument7 SeitenMicroneedling Tratamiento en CicatricesRocio VinderolaNoch keine Bewertungen
- Efecto de La Mesoterapia Con Nano ChipDokument7 SeitenEfecto de La Mesoterapia Con Nano ChipEdimarKatherineQuinteroGarcíaNoch keine Bewertungen
- Efficacy and Safety of 1927 NM Fractional Thulium Fiber Laser For The Treatment of Melasma: A Retrospective Study of 100 PatientsDokument5 SeitenEfficacy and Safety of 1927 NM Fractional Thulium Fiber Laser For The Treatment of Melasma: A Retrospective Study of 100 Patientsdl qiuNoch keine Bewertungen
- Ijn 183342 Enhancement of Wound Healing by Single Wall Multi Wall Carbo 110718Dokument12 SeitenIjn 183342 Enhancement of Wound Healing by Single Wall Multi Wall Carbo 110718Mustafa IdaisNoch keine Bewertungen
- 2019 - Comparasion NdYag Picosecond Laser and Fractional 1550 NM Erbium in Facial Acne Scar TreatmentDokument6 Seiten2019 - Comparasion NdYag Picosecond Laser and Fractional 1550 NM Erbium in Facial Acne Scar TreatmentnancyerlenNoch keine Bewertungen
- Dermatological Pharmacology Topical AgentsDokument5 SeitenDermatological Pharmacology Topical AgentsYilianeth Mena DazaNoch keine Bewertungen
- Treatment of Xanthelasma Palpebrarum Using PulsedDokument3 SeitenTreatment of Xanthelasma Palpebrarum Using PulsedАркадий ЖивицаNoch keine Bewertungen
- Acne Vulgaris and Light-Based TherapiesDokument17 SeitenAcne Vulgaris and Light-Based TherapiesANA CATARINA PESTANA BELCHIORNoch keine Bewertungen
- A Practical Approach To Chemical PeelsDokument8 SeitenA Practical Approach To Chemical Peelsleenatalia93100% (2)
- Mesotherapy: A Bibliographical Review: Mesoterapia: Uma Revisão BibliográficaDokument6 SeitenMesotherapy: A Bibliographical Review: Mesoterapia: Uma Revisão BibliográficaSofieNoch keine Bewertungen
- Actinic Cheratosis - A ReviewDokument4 SeitenActinic Cheratosis - A ReviewMARIUS-MIRCEA POPESCU-MICLOSANUNoch keine Bewertungen
- Oral Minoxidil 2023Dokument10 SeitenOral Minoxidil 2023maat1Noch keine Bewertungen
- Principle of Topical Agent-FzpDokument16 SeitenPrinciple of Topical Agent-FzpMurwani LatifahNoch keine Bewertungen
- Transdermal Drug Delivery System A ReviewDokument6 SeitenTransdermal Drug Delivery System A ReviewEditor IJTSRDNoch keine Bewertungen
- Nanoemulsions and Dermatological Diseases: Contributions and Therapeutic AdvancesDokument7 SeitenNanoemulsions and Dermatological Diseases: Contributions and Therapeutic AdvancesliliNoch keine Bewertungen
- Banana Leaves An Alternative Wound Dressing MaterialDokument3 SeitenBanana Leaves An Alternative Wound Dressing MaterialEsther Lois Santiago AlvaradeNoch keine Bewertungen
- Farshi, 2019Dokument6 SeitenFarshi, 2019Thalita HerekNoch keine Bewertungen
- Efektivitas Dan Keamanan Kojic DipalmitatDokument6 SeitenEfektivitas Dan Keamanan Kojic DipalmitatmurjonocrbNoch keine Bewertungen
- Recent Nanotechnological Aspects in Cosmetics and Dermatological PreparationsDokument11 SeitenRecent Nanotechnological Aspects in Cosmetics and Dermatological PreparationsAmalia AfifahNoch keine Bewertungen
- 2%MSH美白Dokument10 Seiten2%MSH美白jiying huangNoch keine Bewertungen
- Jurnal Kulit AcneDokument7 SeitenJurnal Kulit AcnePsyhlaNoch keine Bewertungen
- Jcad 4 11 20Dokument2 SeitenJcad 4 11 20Gabriel Balbino NogueiraNoch keine Bewertungen
- Nanoparticles For Dermal and Transdermal Drug Delivery IntechOpenDokument5 SeitenNanoparticles For Dermal and Transdermal Drug Delivery IntechOpenAditya WijayaNoch keine Bewertungen
- Skin Toxicity During Breast Irradiation: Pathophysiology and ManagementDokument5 SeitenSkin Toxicity During Breast Irradiation: Pathophysiology and Managementalejandromfunes1749Noch keine Bewertungen
- Patches PDFDokument20 SeitenPatches PDFMadalina CalcanNoch keine Bewertungen
- Diagnosis and Management of Conjunctivitis For The DermatologistDokument7 SeitenDiagnosis and Management of Conjunctivitis For The DermatologistRhevyNoch keine Bewertungen
- 03.transdermal Drug Delivery SystemsDokument56 Seiten03.transdermal Drug Delivery SystemsMoganaa LakshmiNoch keine Bewertungen
- Acne Treatments: Future Trajectories: Review ArticleDokument7 SeitenAcne Treatments: Future Trajectories: Review ArticleIsabel Zamora AuzaNoch keine Bewertungen
- Review On Novel Drug Delivery System of Microsphere Type, Material, Method of Preparation and EvaluationDokument7 SeitenReview On Novel Drug Delivery System of Microsphere Type, Material, Method of Preparation and EvaluationEditor IJTSRDNoch keine Bewertungen
- Choosing A Wound Dressing Based On Common Wound CharacteristicsDokument11 SeitenChoosing A Wound Dressing Based On Common Wound CharacteristicsYolis MirandaNoch keine Bewertungen
- Dermatological Pharmacology: Topical Agents: Key PointsDokument3 SeitenDermatological Pharmacology: Topical Agents: Key PointsIsmail IbrahimNoch keine Bewertungen
- Tinea Incognito 1Dokument3 SeitenTinea Incognito 1samuelNoch keine Bewertungen
- Transdermal Drug Delivery System A RevieDokument12 SeitenTransdermal Drug Delivery System A RevieMrunali Porete CSE-11Noch keine Bewertungen
- 88Dokument8 Seiten88merinapingNoch keine Bewertungen
- Microneedling in Skin of ColorDokument8 SeitenMicroneedling in Skin of ColorDiva Natasya KrismanitaNoch keine Bewertungen
- Webinar Argano Melasma and Januluma DR Seraj Nonpharmacologic ManagementDokument22 SeitenWebinar Argano Melasma and Januluma DR Seraj Nonpharmacologic Managementmohammad kazem HajianiNoch keine Bewertungen
- Acta Biomaterialia: Full Length ArticleDokument15 SeitenActa Biomaterialia: Full Length Articledavin otooleNoch keine Bewertungen
- DERMATOTERAPIDokument55 SeitenDERMATOTERAPIPutri Windiani Haryono HNoch keine Bewertungen
- Azithromycin in Durasite For The Treatment of Blepharitis: Clinical Ophthalmology DoveDokument8 SeitenAzithromycin in Durasite For The Treatment of Blepharitis: Clinical Ophthalmology Dovemelon segerNoch keine Bewertungen
- Microneedles A Transdermal Drug Delivery SystemDokument12 SeitenMicroneedles A Transdermal Drug Delivery Systemchristin stanley100% (1)
- 2020ENDOCARE Zoe-Draelos Skin-Health-Beauty-Pyramid Paper ENDokument5 Seiten2020ENDOCARE Zoe-Draelos Skin-Health-Beauty-Pyramid Paper ENNazera SalejeeNoch keine Bewertungen
- Management of Aging SkinDokument19 SeitenManagement of Aging SkinmonitamiftahNoch keine Bewertungen
- Formulation and Evaluation of Transdermal PatchDokument4 SeitenFormulation and Evaluation of Transdermal PatchMelissa STanNoch keine Bewertungen
- Nanomedicine Unlocks Potential: Applying Nanotechnology to Detect, Deliver, and Defeat CancerVon EverandNanomedicine Unlocks Potential: Applying Nanotechnology to Detect, Deliver, and Defeat CancerNoch keine Bewertungen
- Pharmaceutical and Cosmetic Products for Topical Administration: Pharmaceutical MonographsVon EverandPharmaceutical and Cosmetic Products for Topical Administration: Pharmaceutical MonographsBewertung: 5 von 5 Sternen5/5 (1)
- ObatDokument9 SeitenObatmarsenNoch keine Bewertungen
- Neo Fax 2011Dokument409 SeitenNeo Fax 2011Lourdes M. RodriguezNoch keine Bewertungen
- Mult AEREL AEACNDokument7 SeitenMult AEREL AEACNBart RoofthooftNoch keine Bewertungen
- Drug Study RifampicinDokument2 SeitenDrug Study RifampicinJamil Lorca100% (5)
- Antimikroba Anti Jamur Antiparasit Antibiotik Antiviral Antimico-Bacterium Antimikosis Antihelmintik Antiamuba AntimalariaDokument22 SeitenAntimikroba Anti Jamur Antiparasit Antibiotik Antiviral Antimico-Bacterium Antimikosis Antihelmintik Antiamuba AntimalariaHaris GaulNoch keine Bewertungen
- Drug Utilization Pattern of Anti-Diabetic Drugs Among Diabetic Outpatients in A Tertiary Care HospitalDokument3 SeitenDrug Utilization Pattern of Anti-Diabetic Drugs Among Diabetic Outpatients in A Tertiary Care HospitalTazkiyatan IsriaNoch keine Bewertungen
- Drug-Induced Memory DisordersDokument1 SeiteDrug-Induced Memory DisordersNeeru KaulNoch keine Bewertungen
- Role of Chemotherapy in Malignant Ovarian TumorsDokument36 SeitenRole of Chemotherapy in Malignant Ovarian TumorsUsha AnengaNoch keine Bewertungen
- Reviewing Depot Injection Efficacy in The Treatment of SchizophreniaDokument10 SeitenReviewing Depot Injection Efficacy in The Treatment of SchizophreniaAnonymous raLgWVyqNoch keine Bewertungen
- Drug Senna Drug CardDokument1 SeiteDrug Senna Drug CardSrkocher100% (2)
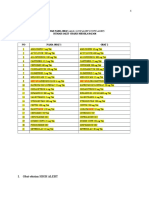
- Rekapitulasi Laporan Narkotika: NO Nama Satuan Stok Awal Pemasukan PBFDokument11 SeitenRekapitulasi Laporan Narkotika: NO Nama Satuan Stok Awal Pemasukan PBFBang23 ManikNoch keine Bewertungen
- Sodium Picosulfate For ConstipationDokument2 SeitenSodium Picosulfate For Constipationshoukat aliNoch keine Bewertungen
- ReferensiDokument4 SeitenReferensiBayuAjiWicaksonoNoch keine Bewertungen
- Status AsthamaticusDokument40 SeitenStatus AsthamaticusNazia ShamimNoch keine Bewertungen
- Pharma Drug SufficesDokument3 SeitenPharma Drug SufficesJillian GayleNoch keine Bewertungen
- DCO SyllabusDokument2 SeitenDCO SyllabusMrunal DixitNoch keine Bewertungen
- Isi Tas EmergencyDokument2 SeitenIsi Tas EmergencyyeniNoch keine Bewertungen
- Dosage Chapter 1 PDFDokument4 SeitenDosage Chapter 1 PDFLena EmataNoch keine Bewertungen
- Ikon New CatelogueDokument32 SeitenIkon New CatelogueShlokeasundNoch keine Bewertungen
- The Role of The Pharmacist in The Control of Acute PoisoningDokument6 SeitenThe Role of The Pharmacist in The Control of Acute PoisoningJayrine MonteroNoch keine Bewertungen
- Drug DiscoveryDokument6 SeitenDrug DiscoveryGaurav DarochNoch keine Bewertungen
- IFU Hydro Deluxe - LFT03 Rev.02Dokument9 SeitenIFU Hydro Deluxe - LFT03 Rev.02Ana ČolovićNoch keine Bewertungen
- Calc Practice Problems - SSD Electron 1Dokument1 SeiteCalc Practice Problems - SSD Electron 1api-630484455Noch keine Bewertungen
- Unofficial Translation of The German Package LeafletDokument5 SeitenUnofficial Translation of The German Package LeafletMAHMOUD DRIDINoch keine Bewertungen
- Effect MetforminDokument9 SeitenEffect MetforminAsep Cloud OvernightNoch keine Bewertungen
- Pulseless Arrest Algorithm For Managing VF and Pulseless VTDokument3 SeitenPulseless Arrest Algorithm For Managing VF and Pulseless VTLaili CinthiaNoch keine Bewertungen
- SBFR Weekly Forum 43Dokument55 SeitenSBFR Weekly Forum 43Miraf MesfinNoch keine Bewertungen
- Non-Hodgkin Lymphoma (NHL)Dokument11 SeitenNon-Hodgkin Lymphoma (NHL)archanaNoch keine Bewertungen
- Data Ba RangDokument180 SeitenData Ba Rangsherly damayantiNoch keine Bewertungen
- Types of Parenteral ProductsDokument7 SeitenTypes of Parenteral ProductsJoginder KumarNoch keine Bewertungen