Beruflich Dokumente
Kultur Dokumente
82-85 27.2 Amanatullah PDF
Hochgeladen von
Vetrivel TamizhOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
82-85 27.2 Amanatullah PDF
Hochgeladen von
Vetrivel TamizhCopyright:
Verfügbare Formate
4 ON THE WARDS
Your Practical Survival Guide to Surgical Internship
Derek F. Amanatullah, MD, PhD
Department of Orthopedic Surgery, University of California Davis Medical Center, Sacramento, California.
T
here is a lot of anxiety in medical school regarding his or her diet. Patients should be NPO (taking nothing
internship, especially surgical internship. Internship by mouth) post-surgery until they have bowel sounds;
is your introduction to medical responsibility. After then clear liquids may be started, and continued until
four years of developing your interview and examina- the patients pass flatus, when solids may be tried. Do not
tion skills, as well as increasing your fund of medical be afraid to go slowly or take a step back. If a patient
knowledge, you are ready for real patients. Internship is not taking food by mouth, note the nutritional route
is easy if you are diligent and reliable. The anxiety over or the reason for withholding oral nutrition; if he or she
internship results from translating theoretical knowl- is eating, know the type of diet (e.g., clear liquid, dys-
edge into practical skill, while doing no harm. Do not phagia ground, diabetic, low salt, regular). Know your
fear. It is not as hard as you think. Some sage words from patients urine output and if it is adequate (i.e., at least
my general surgery chief the day before internship sum 30 mL/hour; perhaps less for children and the elderly)
it up: Do what you are told; anticipate what you will be and the route (i.e., via catheter or naturally). If a patient
told; and, if you find yourself thinking independently, is off a patient-controlled analgesic (PCA) or other,
call someone. You know a lot as an intern! Use the more-invasive pain control (e.g., an epidural catheter) as
team and the hospital to your advantage and your tran- well as able to sit on a bedpan or use a urinal, get that
sition to responsibility will be easy. Maybe with these Foley catheter out. When removing a Foley catheter,
ten tips and tricks I found useful during my internship in be sure to write for bladder scan after six hours if the
your pocket, you can get some sleep as well. patient has not urinated, and to replace the Foley cath-
eter if the bladder scan is more than 350 mL. Assess the
number of days since the patients last bowel movement
GET TO KNOW YOUR SURROUNDINGS so you know how to adjust bowel care. Finally, under-
AND YOUR TEAM. stand the patients physical condition and progress with
physical, occupational, and speech therapy as well as all
Nothing will save you more time and effort than know- other consults required to aid in the management of the
ing where to go and whom to call. Spend a few hours patients case.
the day before your internship begins wandering the
hospital, trying to find the Emergency department, the
Radiology department (CT scanner, MRI, and X-Ray), TELL THE TRUTH.
the pharmacy, the telemetry floors, the cafeteria, the
call room, a shower, and several bathrooms near each. Nothing makes you look worse than reporting incor-
I would also recommend calling your Chiefand per- rect overnight events, physical examination findings, or
haps all of the senior residents on your teamto get to imaging and laboratory results. It is better to say I did
know how the chain of command should work and to not have time, I did not check, I forgot, or even I
whom you should address questions. Do not forget to do not know than to say you did or to make something
call the junior resident and get sign-outs on the patients up. You will get caught. It is better to be perceived as
you will be taking care of so you hit the ground running lazy and irresponsible than as deceptive and unreliable.
when you show up for prerounds that first day. The difference is that one is responsive to training, while
the other undermines every aspect of team communica-
tion and function. The latter violates your oath as a phy-
KNOW THE SEVEN Ps. sician and places patients in danger as a result of your
obfuscation. At the end of the day, you are building
Make sure you ask the patient, a nurse, or the post- respect as a physician and gaining trust in your decision-
call teamor read the chartand know the seven Ps making from your peers. Do not sacrifice respect for
for each of your patients: Problems, Progress, Pain, PO yourself, your team, or your patients by taking the easy
(oral intake), Pee-Pee, Poop, and Physical condition. road. Simply learn to be more efficient or spend more
Problems refers to the problem list you are address- time on the details; let your lack of information guide
ing for the patient (i.e., why and how the patient came you about where you need to make improvements and
to be under your care) and what you are doing for each become a better physician in the process.
with respect to either diagnosis or treatment. Progress
refers to the events in the past twenty-four hours that
have happened positively or negatively to your patient. WHEN ON CALL, AVOID DISASTER,
Progress is what the team will want to hear about every AND THEN WORK IT UP.
day. Assess your patients pain and adjust medications so
the patient is reasonably comfortable. Know how your You are going to get called about everything. Do not
patient is getting nutrition and how far you can advance blow off even the simplest matter, or act out of reflex;
82 EJBM, Copyright 2012
4 ON THE WARDS
Your Practical Survival Guide to Surgical Internship
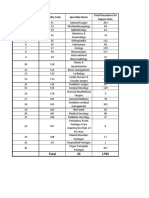
TABLE 1. REGULAR INSULIN SLIDING SCALE without contrast, CT of the pulmonary artery, and elec-
trocardiogram. With those tests, you will be ready to call
Finger-Stick Glucose Units of Regular Insulin SQ
the appropriate consulting service (neurology, cardiol-
Measurement x1 or Order
ogy, or psychiatry), to tell the team your findings in the
060 Give amp D50 and call HO morning, and to begin the necessary intervention. You
61120 0 Units; do nothing get the idea. I have one attending who says, The enemy
121150 2 Units
is everywhere, even within. Resist the temptation to
react, and instead, think. On a similar note, I must rein-
151200 4 Units force the value of advanced cardiac life support. Read it
201250 6 Units and know it. Do not blow it off, as I know many interns
251300 8 Units do. Do not plan on the code team just being there. These
are your patients and you should know how to manage
301350 10 Units
bradyarrhythmias and tachyarrhythmias as well as pulse-
>351 12 Units and call HO lessness until the code team gets there to help. I carry a
Abbreviations: SQ, subcutaneous; amp, ampoule; D50, 50% dextrose solu- cheat sheet in my pocket for each of these, because they
tion; HO, house officer are things you cannot just look up or think about when
they come up, unlike almost every other call you will get.
instead, try to think. Investigate and, when in doubt, Trust me!
see the patient. Say you get a call regarding a patient
with a fever on postoperative day one and you know
this is probably atelectasis, because you remember the REPLACE THE ELECTROLYTES.
six Ws (wind atelectasis day one; water urinary tract
infection day three; walk deep venous thrombosis Avoiding arrhythmias is worth it. Use the 2349 rule
day five; wound day seven; where abscess day ten; to remember the desired levels of magnesium, phospho-
weird drugs day ten). You could reflexively recommend rous, potassium, and calcium, respectively. Keep potas-
encouraging incentive spirometry every hour and indi- sium over 4.0 mEq/L. Add 20 mEq/L to intravenous (IV)
cate that you will see the patient in the morning, but if fluids unless the patient has renal issues; then reconsider
you did, you would miss a rare and devastating presen- fluids altogether. Remember that PO potassium works
tation of Clostridium wound infection, which presents faster that IV potassium, so use PO if possible, and if you
with cloudy discharge from the wound and fever. So must use IV add lidocaine unless the patient has a central
look at the wound on postoperative day one and order line, because potassium chloride burns. Use potassium
blood cultures times three, line cultures, a urine analysis chloride 1060 mEq PO once or potassium chloride 10
with culture, a chest X-ray, and a duplex ultrasound of mEq IV one to six times with or without 1 mL of lidocaine,
bilateral lower extremities if the fever is after postopera- and remember that every 10 mEq PO/IV increases the
tive day one. potassium by 0.1 mEq/L, so calculate accordingly. Keep
magnesium over 2.0 mg/dL. Giving magnesium oxide
Say you get a call regarding a patient with hypotension 400 mg PO once or magnesium sulfate 1 g IV once each
immediately postoperatively in the post-anesthesia care will raise the magnesium level by 0.2 mg/dL. Keep phos-
unit; you think it must be hypovolemia. You reflexively phorous above 3.0 mg/dL. Give Neutra-Phos 2 packets
order a liter of normal saline bolus without asking about PO q8h (every eight hours) (8 mmol per packet) or Kphos
the heart rate or urine output, and thus miss a myocar- 2 tablets PO q8h (8 mmol per tablet). Sodium or potas-
dial infarction. Hypotension can be due to a failure in sium phosphate 1530 mmol IV once every six hours can
preload, the pump, or afterload, and you must consider be used for faster repletion. Keep calcium above 9.0 mg/
each possibility each time. Do not just assume hypovo- dL. Give calcium carbonate 1,250 mg PO BID (twice a
lemia (i.e., failure of adequate preload). Or consider a day) or calcium chloride 1 g IV once for faster repletion.
call about a confused, bedridden, elderly woman who Remember always to recheck a basic metabolic panel
is trying to get out of bed. Sure, you can put her in a with calcium, magnesium, and phosphorous after elec-
posy and physically or chemically restrain her, but the trolyte repletion to reassess and adjust therapy.
major issue is why she is acting like this. Take a second to
think about the differential, including delirium, demen-
tia, stroke, myocardial infarction, pulmonary embolism, THE REGULAR INSULIN SLIDING
infection, electrolyte abnormality, psychosis, or toxicity. SCALE IS YOUR BEST FRIEND.
Now it is easy, instead of overwhelming. Simply order
oxygen and pulse oximetry; collect a basic metabolic Every diabetic patient should have such a scale to moni-
panel, calcium, magnesium, phosphorous, arterial blood tor his or her glucose control. This way you can report the
gas, cardiac markers, vitamin B12, folate, urine analysis patients use of regular insulin, so the team can adjust
with culture, blood cultures times three, line cultures, NPH qAC (with each meal) or daily Lantus. Memorize
and urine toxicity screen; give a full dose of aspirin Table 1; enough said. Every diabetic patient needs fin-
(unless contraindicated); and get a chest X-ray, head CT ger-stick measurements qAC and qHS (nightly) if eating
The Einstein Journal of Biology and Medicine 83
4 ON THE WARDS
Your Practical Survival Guide to Surgical Internship
and q6h (every six hours) if NPO. Also, remember to hold sure also to order other PRN medications, such as bowel
or halve any scheduled insulin if the patient is not eating care, Benadryl, and Zofran, to cover narcotic side effects.
prior to surgery. By the way, since we are on the topic of Nonsteroidal anti-inflammatory drugs such as Motrin
the operating room (OR), be sure to check the consent 600 mg PO q8h around the clock and Toradol 30 mg IV
or get the patients consent yourself; hold anticoagula- once followed by 15mg IV q8h for 48 hours can also be
tion if appropriate; order preoperative antibiotics (e.g., great adjuvant analgesics if your patient does not have
Kefzol 1 g IV on call to the OR), and make your patient bleeding or renal issues. Finally, some pain is caused by
NPO at midnight except for medication if he or she is are muscle spasms, so watch for intermittent achy, cramplike
on call to the OR (OCTOR) the next day. pains in the extremities or back, with poor relief from
narcotic medicationsValium 5 mg PO q8h PRN spasm
will usually do the trick.
GIVE THE PATIENT THEIR VITAMINS.
Everyone should get a multivitamin PO daily, but there BOWEL CARE IS KING.
are special patients-alcoholics and poor wound healers-
who need a bit more help. Every alcoholic should get Especially since almost everyone is on narcotics for pain
folic acid 1 mg PO daily and thiamine 100 mg PO daily control. Colace 100 mg PO BID and Senna 2 tabs PO
as well as Ativan 2 mg IM (intramuscular) or IV q2h qHS are essential. Be sure to add a HOLD order for loose
(every two hours) PRN (as needed), for agitation. Poor stools as well. The problem arises when Colace and
healers need zinc sulfate 220 mg PO daily, vitamin C 500 Senna are not doing the trick; this is where PRN bowel
mg PO BID, and vitamin A 20,000 units PO daily to facili- care will help you and the nursing staff out. I always
tate the synthesis of collagen. dose with milk of magnesia 30 cc PO PRN constipation.
If that does not work, I move on to Dulcolax 10 mg PO/
PR (per rectum) daily PRN no bowel movement. The last
ADDRESS YOUR PATIENTS PAIN BEFORE IT STARTS. resort, to my mind, is lactulose 30 mL PO q4h until bowel
movement, or a pink lady enema once; these will usu-
This topic is complicated, but some basics are critical. ally get things moving.
Every patient needs to have a baseline medication, pref-
erably PO. I prefer Percocet 5/325 mg 1-2 tabs PO q4h
(every four hours) PRN pain or Vicodin 5/500 mg 1-2 tabs PRN MEDICATIONS HELP YOU SLEEP.
PO q6h PRN pain. (Be careful with Vicodin, as it has 500
mg of Tylenol and can lead to Tylenol toxicity if more They help your patients sleep, too. Most are designed to
than 4 g of Tylenol is consumed daily.) If your patient control the side effects of narcotics (e.g., itching, nau-
has a nasogastric tube or cannot take solid food, Lortab sea/vomiting) and of the hospital itself (e.g., insomnia).
elixir 7.5 mg per 15 mL PO q4h PRN pain is the way to go. Use Benadryl 50 mg PO/IV q6h PRN itching/insomnia,
After a basal medication is on board, add an IV medica- and you can add Ambien 10 mg PO qHS PRN insomnia
tion for breakthrough pain (BTP), such as morphine 1-4 if that is not sufficient. Use Zofran 4 mg IV q12h (every
mg IV q2h PRN BTP or Dilaudid 0.2 0.8 mg IV q2h PRN 12 hours) PRN nausea/vomiting, and you can add Reglan
BTP. You can increase the dose range for BTP pain medi- 10 mg IV q6h PRN nausea/vomiting if that is not suffi-
cations, but it is probably better to address the patients cient, but always give antiemetic IV as patients may not
baseline pain needs. Do not be afraid to ask for help be able to take PO medications with nausea/vomiting.
here from the team or a pain consult. Another way to Hypertension control can be difficult, but metoprolol
address basal pain is to offer patient-controlled anesthe- 12.5 mg PO BID HOLD for systolic blood pressure less
sia (PCA). This will allow the patient to determine the than 100 or heart rate less than 60 and hydralazine 10
dose of his or her own medication. It is ordered using mg IV q4h PRN SBP greater than 160 is a good start, and
either morphine or Dilaudid (or, rarely, Fentanyl), and can be titrated by the team or cardiology as appropri-
given as an incremental dose every 6, 10, or 25 minutes. ate. Flomax 0.4 mg PO daily is useful for patients with
The patient can dose himself or herself by using a but- elevated postvoid residual volumes. Pepcid 20 mg PO/IV
ton without having to ask for nurse assistance. Beware BID or Nexium 40 mg PO/IV daily are staples for inten-
the basal rate of administration with a PCA; do not sive-care-unit patients and great for daily dyspepsia con-
use this as an intern without asking the team, as this trol for floor patients as well. Others that are useful in a
is how patients die using a PCA: they stop breathing. pinch are Maalox 30 ml PO q6h PRN dyspepsia, Imodium
Remember the side effects of narcotics, including respi- 2mg PO q6h PRN diarrhea, Robitussin 400 mg PO q4h
ratory depression, constipation, itching, and nausea. PRN cough and congestion or Hycodan 3 ml PO q6h
Therefore, every IV narcotic must be accompanied by an PRN cough, Thorazine 25 mg PO q8h PRN hiccups, and
order to HOLD narcotics if the patient is unresponsive Cepacol 1 tab PO q2h PRN sore throat or Chloraseptic
or somnolent, or has a respiratory rate less than six. Be 12 spray q2h PRN sore throat.
84 EJBM, Copyright 2012
4 ON THE WARDS
Your Practical Survival Guide to Surgical Internship
A NOTE TO REMEMBER
Corresponding Author: Derek F. Amanatullah, MD, PhD (derek.amanatullah@
ucdavis.ucdmc.edu).
Remember, Interns do not die on start day, patients
do! Communicate with your team, pay attention to Conflict of Interest Disclosures: The author has completed and submitted the
ICMJE Form for Disclosure of Potential Conflicts of Interest. No conflicts were
detail, and know your patients. You will do fine. Always reported.
remember to check and double-check allergies when
writing prescriptions for medications and adjust accord-
ingly. You will have to be resourceful, be thoughtful,
and read the published literature. This, I hope, is enough
to make you a bit more relaxed and comfortable on that
fateful day when the theory of medical school becomes
very real. Good luck!
The Einstein Journal of Biology and Medicine 85
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Basics of Pharmacology: Speaker - DR - SantoshDokument76 SeitenBasics of Pharmacology: Speaker - DR - SantoshRamya ChallaNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Oregano: The Top 5 Health Benefits of OreganoDokument4 SeitenOregano: The Top 5 Health Benefits of OreganoKrishnamurthiNageswari100% (1)
- Roles and Responsibilities of ASHADokument3 SeitenRoles and Responsibilities of ASHAmohanpskohli8310Noch keine Bewertungen
- CataractDokument3 SeitenCataractVetrivel Tamizh100% (1)
- Notice No. 152 - 2022 INICET Tentative Seat PositionDokument9 SeitenNotice No. 152 - 2022 INICET Tentative Seat PositionVetrivel TamizhNoch keine Bewertungen
- Rhinoplasty Basic Approaches and Techniques in Nasal Tip SurgeryDokument10 SeitenRhinoplasty Basic Approaches and Techniques in Nasal Tip SurgeryVetrivel TamizhNoch keine Bewertungen
- Electrode Portfolio Sell SheetDokument2 SeitenElectrode Portfolio Sell SheetVetrivel TamizhNoch keine Bewertungen
- AIIMS Madurai - MBBS Prospectus 2022-2023 Academic SessionDokument16 SeitenAIIMS Madurai - MBBS Prospectus 2022-2023 Academic SessionVetrivel TamizhNoch keine Bewertungen
- Basic Reg AiimsDokument1 SeiteBasic Reg AiimsVetrivel TamizhNoch keine Bewertungen
- Aiims FinalDokument1 SeiteAiims FinalVetrivel TamizhNoch keine Bewertungen
- All India Institute of Medical Sciences: ImportantDokument1 SeiteAll India Institute of Medical Sciences: ImportantVetrivel TamizhNoch keine Bewertungen
- Signs in OtorhinolaryngologyDokument5 SeitenSigns in OtorhinolaryngologyVetrivel TamizhNoch keine Bewertungen
- 40001239F PDFDokument88 Seiten40001239F PDFVetrivel TamizhNoch keine Bewertungen
- Q.P. Code: 222240Dokument7 SeitenQ.P. Code: 222240Vetrivel TamizhNoch keine Bewertungen
- Worker 5 1 PDFDokument83 SeitenWorker 5 1 PDFVetrivel TamizhNoch keine Bewertungen
- Buy Indian Products From Now - List PDFDokument7 SeitenBuy Indian Products From Now - List PDFVetrivel TamizhNoch keine Bewertungen
- Buy Indian Products From Now - List PDFDokument7 SeitenBuy Indian Products From Now - List PDFVetrivel TamizhNoch keine Bewertungen
- PR mbbs3022017 10012017Dokument4 SeitenPR mbbs3022017 10012017Vetrivel TamizhNoch keine Bewertungen
- Faculty 363 Histotechnique Lectures - 2Dokument27 SeitenFaculty 363 Histotechnique Lectures - 2einsteinspy100% (1)
- Basic Safety TrainingDokument1 SeiteBasic Safety TrainingMade HartawanNoch keine Bewertungen
- TRIKATUDokument5 SeitenTRIKATUAngshuman DuttaNoch keine Bewertungen
- EYE MCQ Uploaded by Hafiz BilalDokument2 SeitenEYE MCQ Uploaded by Hafiz BilalMohammad Jamal NasirNoch keine Bewertungen
- Jurnal DBDDokument10 SeitenJurnal DBDFirman FajriNoch keine Bewertungen
- Laporan Stock OpnameDokument138 SeitenLaporan Stock OpnameAnggunia DeaNoch keine Bewertungen
- Dr. Syed Shakeel Ahmad: ObjectiveDokument3 SeitenDr. Syed Shakeel Ahmad: ObjectiveSyed Shakeel AhmadNoch keine Bewertungen
- QUIZ Classification of Surgery in TableDokument1 SeiteQUIZ Classification of Surgery in TableMaria Sheila BelzaNoch keine Bewertungen
- Meditation Its EffectDokument11 SeitenMeditation Its Effectmanisami7036Noch keine Bewertungen
- Percakapan BHS Ingg 1-5 - OciDokument30 SeitenPercakapan BHS Ingg 1-5 - OciYetty LasmiNoch keine Bewertungen
- Daftar Obat Apotek MutiaraDokument7 SeitenDaftar Obat Apotek Mutiarafany hertinNoch keine Bewertungen
- Act 1 Urinary SystemDokument20 SeitenAct 1 Urinary Systemisabellamarie.castillo.crsNoch keine Bewertungen
- Eac MsdsDokument2 SeitenEac Msdsteguh30Noch keine Bewertungen
- Pharma CompaniesDokument14 SeitenPharma CompaniesAmit SaunNoch keine Bewertungen
- Research Forms 2Dokument35 SeitenResearch Forms 2api-343437101Noch keine Bewertungen
- Chapter 16 BLOODDokument2 SeitenChapter 16 BLOODJennyNoch keine Bewertungen
- 수산부산물에 대한 해양바이오산업 활용 의향 조사 연구Dokument15 Seiten수산부산물에 대한 해양바이오산업 활용 의향 조사 연구이수하1118Noch keine Bewertungen
- All PackageRates (ABPMJAY) PDFDokument300 SeitenAll PackageRates (ABPMJAY) PDFSumit Soni0% (1)
- Actalyke Mini Op Man D6500091JDokument29 SeitenActalyke Mini Op Man D6500091Jjyoti ranjanNoch keine Bewertungen
- End-Stage Heart DiseaseDokument44 SeitenEnd-Stage Heart DiseaseCyrille AgnesNoch keine Bewertungen
- Day Scholar Application2007-08Dokument13 SeitenDay Scholar Application2007-08Bild Andhra PradeshNoch keine Bewertungen
- Orthotic/Prosthetic Referral Form: Dispensing RX: Please Evaluate and Treat Patient With The Following DeviceDokument1 SeiteOrthotic/Prosthetic Referral Form: Dispensing RX: Please Evaluate and Treat Patient With The Following DeviceKelly Roberts WiggenNoch keine Bewertungen
- ProliaDokument17 SeitenProliamktantumNoch keine Bewertungen
- Art. ENFit Enteral Nutrition ConnectionsDokument4 SeitenArt. ENFit Enteral Nutrition Connectionscarlos enriqueNoch keine Bewertungen
- World Service Office PO Box 9999 Van Nuys, CA 91409 USADokument2 SeitenWorld Service Office PO Box 9999 Van Nuys, CA 91409 USAmustafa hezamNoch keine Bewertungen
- Quality Management in The Imaging Sciences 5th Edition Papp Test BankDokument35 SeitenQuality Management in The Imaging Sciences 5th Edition Papp Test Bankmisdateholinessaubzt6100% (22)
- Eye Test For Alp Post Imp PDFDokument1 SeiteEye Test For Alp Post Imp PDFGyg GtgNoch keine Bewertungen