Beruflich Dokumente
Kultur Dokumente
Amebiasis of The Penis
Hochgeladen von
ErtyWitalayaL.ToruanOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Amebiasis of The Penis
Hochgeladen von
ErtyWitalayaL.ToruanCopyright:
Verfügbare Formate
CASE R E P O R T
ELSEVIER
AMEBIASIS OF THE PENIS
MOHAMED J. HEJASE, RICHARD BIHRLE, GILBERTO CASTILLO, AND CHRISTOPHER L. COOGAN
ABSTRACT
Penile amebiasis is rarely a recognized entity because the penis is not the usual site of presentation for
amebiasis. Homosexual men have a higher risk of acquiring the lesion. Amebic ulcers resemble cutaneous
lesions arising from squamous cell carcinoma, chancroid, primary syphilis, granuloma inguinale, and many
other causes. An amebic ulcer should be suspected in a patient with balanoposthitis that resists antibiotic
therapy. Biopsy is fundamental to isolate the trophozoites to confirm the diagnosis. Metronidazole and hy-
drochloric emetine are still the treatment of choice. This diagnosis should especially be considered in cases
of lesions detected in patients who practice anogenital sex or who are immunocompromised. UROLOGY 48:
151-154, 1996.
mebiasis of the penis is a rare disease. About ulceration on the ventral surface of his foreskin
A 20 cases have been reported in the world lit-
erature to date. 1-11 However, many cases are still
(Fig. 1 ). On physical examination, a 2-cm irreg-
ular ulcer with a nonraised border covered by a
unpublished. Entamoeba histolytica is the etiologic serous exudate was evident. The patient also dem-
agent of h u m a n amebiasis. 8'12'13 Enteric infections, onstrated bilateral inguinal adenopathy. Serologic
which have traditionally been associated with con- testing for syphilis, h u m a n immunodeficiency vi-
taminated food or water, are now being found in rus (HIV), and hepatitis B surface antigen was
patients without such exposure. Transmission negative. Microscopic evaluation of the exudate
might be achieved by direct inoculation or revealed numerous E. histolytica trophozoites. Se-
through anal intercourse with a person suffering rologic titers were elevated, and examination of
from amebic dysentery. 8'9 It has been reported as stool samples revealed the presence of trophozo-
the result of coitus with a woman who had vul- ites. The treatment of the ulcer included local ap-
vovaginal amebiasis. 2'8 plication of nitrofurazone for 10 days with each
We present four cases of amebiasis, emphasizing dressing change. In addition to local care, a 10-day
the importance of a high index of suspicion for ac- course of oral metronidazole (800 mg three times
curate clinical diagnosis. The epidemiology, evalua- daily) was administered. Two-week follow-up ex-
tion, and treatment are all discussed. Urologists amination of the penis demonstrated complete
should consider amebiasis in the differential diagnosis healing of the ulcer.
of patients with penile lesions, especially those pa-
tients who are at high risk of acquiring such lesions. CASE 2
A 15-year-old uncircumcised man with a history
CASE REPORTS of active homosexuality presented with a 0.5-cm
necrotic ulceration on his distal foreskin. A mal-
CASE 1 odorous serous exudate was noted. Edema of the
A 39-year-old uncircumcised man presented foreskin prevented adequate retraction. Painless
with a history of foul-smelling exudate and tender bilateral inguinal adenopathy was found. Light mi-
croscopy in dark field for Treponema was negative,
From the Department of Urology, Hospital General de Zona as were serologic syphilis and gonorrhea tests. No
IMSS No. 33, Monterrey, Nuevo Leon, Mexico, and the Indiana HIV studies were performed at that time (1983).
University Medical Center, Indianapolis, Indiana Microscopic examination of the exudate showed
Reprint requests: Richard Bihrle, M.D., Department of Urol- abundant E. histolytica trophozoites. Biopsy of the
ogy, Indiana University Medical Center, University Hospital, lesion demonstrated a chronic inflammatory pro-
Suite 1725, 550 North University Blvd., Indianapolis, IN 46202-
5250 cess with infiltration of polymorphonucleated cells
Submitted: October 26, 1995, accepted (with revisions): Jan- and abundant eosinophils. Hydrochloric emetine
uary 4, 1996 (1 m g / k g / d a y intramuscularly) and ampicillin
COPYRIGHT 1996 BY ELSEVIER SCIENCE INC. 0090-4295/96/$15.00
ALL RIGHTS RESERVED PII S 0 0 9 0 - 4 2 9 5 ( 9 6 ) 0 0 1 0 8 - 2 1 S1
FIGURE 1. Penile amebiasis lesion shown on admis- FIGURE 2. Photomicrograph shows granular tissue,
sion. light epithelial hyperplasia, cytolysis, and the tropho-
zoites. Arrow marks trophozoite (hematoxglin and eosin
100).
(500 mg orally four times daily) for a total of 10
days were initiated. Because of incomplete reso-
lution of the lesion, the patient then received 10
days of oral metronidazole ( 1000 mg three times
a day). Two weeks following commencement of
therapy, the ulceration was completely healed. The
final scarring resulted in phimosis, which was later
treated by circumcision.
CASE 3
A 26-year-old man presented with a 15-day his-
tory of painful swelling of the penile foreskin and
a foul-smelling and blood-stained preputial dis-
charge. The foreskin could not be retracted. A bi-
opsy was obtained because a neoplasm was sus- FIGURE 3. Lesion detected upon admission prior to
pected. Within a week, the entire foreskin had treatment.
been destroyed by an ulcer. The entire penis was
edematous with no significant regional lymphad-
enopathy. Syphilis, gonorrhea, Chlamydia, and tered for 10 days. The patient was discharged
HIV tests were negative. Histologically, biopsy when he was asymptomatic. One month later, no
demonstrated a granuloma rich in trophozoites ulcers were detected on his penis.
(Fig. 2). Treatment consisted of hydrochloric em-
etine ( 1 m g / k g / d a y intramuscularly) and metron- COMMENT
idazole (1000 mg orally three times a day) for 2 Within the last two decades, the sexual trans-
weeks. He was examined 30 days later and found mission of protozoal pathogens generally acquired
to be completely asymptomatic with a normal by the fecal-oral route, such as Giardia lamblia
phallus.
and E. histolytica, has become apparent in the ur-
ban homosexual community. 14-16 E. histolytica is
CASE 4 endemic in Africa, South America, Mexico, and In-
A 52-year-old man was admitted with a 3-week dia. In the United States, the prevalence is lower,
history of a painful, exudative, and foul-smelling but several groups are at high risk of acquiring
ulceration on the ventral aspect of his foreskin that amebiasis. 8'17-19 Humans are the only known res-
grew rapidly, destroying his glans (Fig. 3 ). He had ervoir for E. histolytica.
already failed a 2-week course of oral tetracycline E. histolytica is a parasite that exists in two
(500 mg four times daily). Test results for syph- forms, cyst and trophozoite. The cyst is the infec-
ilis, gonorrhea, and HIV were negative. Biopsy of tious form and may yield up to eight trophozo-
the ulcer revealed the presence of trophozoites and ites. 2 It is estimated that as many as 10% of the
an inflammatory process. Oral metronidazole ( 750 world's population is infected with E. histolytica,
mg three times per day) and hydrochloric emetine and this organism is responsible for as many as
(1 m g / k g / d a y intramuscularly) were adminis- 100,000 deaths per year worldwide. 2 The incu-
1 52 UROLOGY 48 (1), 1996
bation period for amebiasis varies from a few days TABLE I. Classical presentation of
to several months, but it is usually 2 to 4 weeks, t6 genital ulcer
Penile amebiasis starts as pruriginous hyperemic
Classical Presentation Disease
zone on the foreskin that evolves into a vesicle.
Several days later, this vesicle will evolve into a Painless superficial round Squamous cell carcinoma
painful, irregular ulcer with a viscous exudate that ulcer with elevated
is often foul smelling. The ulcer spreads rapidly base and mildly rolled
and may surround the entire penile shaft. If mis- edges
Grouped vesicles* Genital herpes
diagnosed and mistreated, this ulcerative process Traumatic ulcer
Onset during sexual
may cause significant penile deformity or even activity*
penile loss. 8-1 Previous studies in the United Recurrences associated Fixed drug reaction
States and elsewhere have demonstrated that a his- with the same systemic
tory of syphilis a n d / o r gonorrhea is highly corre- medicine*
lated with sexually transmitted amebiasis. 13'17-19 Painful deep ulcer with Chancroid
Genital primary l e s i o n s - - w h e t h e r papular, ve- undermined border
sicular; or p u s t u l a r - - q u i c k l y erode to an ulcera- Painless, firm, rolled, and Granuloma inguinale
tive phase. Ulcer characteristics can be valuable in elevated ulcer border
formulating a differential diagnosis (Table I).21 A Painless, firm, indurated Primary syphilis
deep genital ulcer suggests chancroid, whereas the ulcer
ulcers of syphilis, herpes, and lymphogranuloma * Pathognomonic.
venereum are more superficial. Primary penile
squamous cell carcinoma may occur at any ana-
tomic location of the penis. The fiat variety typi-
cally appears as a superficial round ulcer on a idly die after passage; therefore, stool samples
slightly elevated base, and it grows laterally and must be examined within 20 minutes of collection.
infiltrates deeply. A high index of suspicion for Serologic studies are also used in the diagnosis of
penile cancer and a low threshold for biopsy of all invasive amebiasis. Asymptomatic cyst passers will
penile lesions--including balanoposthitis--that usually have serologically low titers, but patients
do not respond to a short trial of conservative an- with invasive disease will have elevated titers. 2
timicrobial therapy are the primary requirements The necessity of treating asymptomatic cyst pass-
for early diagnosis and treatment of patients with ers is controversial. In a controlled study in To-
penile cancer. 22 The histologic picture confirms ronto, Canada, E. histolytica was isolated in stool
the acute and chronic inflammatory processes. It samples from 27% of the homosexual and 1% of
shows abundant granular tissue, light epithelial the heterosexual men, and G. lamblia was isolated
hyperplasia, and a superficial band of necrosis in from 13% of the homosexual and 3% of the het-
which trophozoites are encountered. These organ- erosexual men. 24 Most E. histolytica infections in
isms are n u m e r o u s and easy to identify by routine homosexual men are believed to be asympto-
staining procedures, s-n matic. 24
The clinical presentation of a penile ulcer shows Genital ulcer disease is a risk factor for the
great variability; a study by Chapel et al. 23 has transmission of h u m a n retroviral infection. An
demonstrated that even an experienced clinician u n d e r s t a n d i n g of this interaction is emerging
can misdiagnose 40% of genital ulcers. The differ- and will have an impact on the treatment and
ential diagnosis of an acute genital ulcer can be a control programs for the agents causing genital
difficult problem for physicians working in the ulcer disease. 25 The increased risk of contracting
sexually transmitted disease field. Although each acquired i m m u n o d e f i c i e n c y s y n d r o m e (AIDS)
etiology has its typical symptoms and signs, there with increasing age appears to be greater than
is tremendous overlap in clinical presentation. that associated with acquiring syphilis or ame-
What appears to be a classic picture may actually biasis, a finding that suggests a true increase in
be another infectious process. 22 As a result of the susceptibility. However, it is also possible that
nonspecificity of the clinical findings, the etiologic the apparent difference between the age distri-
diagnosis of genital ulcer disease requires labora- bution of reported cases of AIDS and reported
tory confirmation. cases of syphilis and amebiasis is the result of
The diagnosis of intestinal amebiasis is made by the long latency believed to be associated with
identifying E. histolytica cysts or trophozoites in AIDS. 26 Moreover, because the risk factors for
stool. A single stool specimen will usually detect a m e b i a s i s - - i n c l u d i n g multiple sexual partners,
one third of infected patients, and it is usually rec- poor hygiene, and anogenital s e x - - i s similar to
o m m e n d e d that three separate stool specimens be those for AIDS, declining sexual transmission of
examined to rule out amebiasis. Trophozoites rap- amebiasis might be used to predict decreasing
UROLOGY 48 (1), 1996 1 53
t r a n s m i s s i o n of HIV a n d l o w e r e d i n c i d e n c e of 11. Veliath AJ, Bansal R, Sankaran V, Rajaram P, and Par-
AIDS a m o n g h o m o s e x u a l a n d b i s e x u a l men. kash S: Genital amebiasis. IntJ Gynaecol Obstet 25: 249-256,
1987.
G i v e n the l o n g i n c u b a t i o n of AIDS, s u c h a de- 12. Sorvillo F, Lieb L, Mascola L, and Waterman SH: De-
cline in i n c i d e n c e s h o u l d follow the initial de- clining rates of amebiasis in Los Angeles County: a sentinel
crease in amebiasis rates b y several years.12 This for decreasing acquired immunodeficiency syndrome (AIDS)
is p r o b a b l y d u e to the i n c r e a s i n g use of c o n d o m s incidence? Am J Public Health 79:1563-1564, 1989.
a n d i m p r o v e d s e x u a l e d u c a t i o n in the p o p u l a - 13. Takeuchi T, Kobayashi S, Asami K, and Yamaguchi N:
Correlation of positive syphilis serology with invasive ame-
tion. biasis in Japan. AmJ Trop Med Hyg 36: 321-324, 1987.
Patients presenting with a penile ulcer of enteric 14. Burnham WR, Reeve RS, and Finch RG: Entamoeba his-
etiology, w i t h o u t a history of the classic m e a n s of tolytica infection in male homosexuals. Gut 21: 1097-1099,
transmission, have m o s t likely been infected sex- 1980.
ually. These patients s h o u l d be advised that their 15. McMillan A, Gilmour HM, McNeillage G, and Scott
GR: Amoebiasis in homosexual men. Gut 25: 356-360, 1984.
sexual contacts are p r o b a b l y infected as well. All 16. Felman YM, and Ricciardi NB: Sexually transmitted en-
sexually active individuals w h o p e r f o r m anilingus teric diseases. Bull NY Acad Med 55: 533-539, 1979.
and fellatio, especially male h o m o s e x u a l s a n d their 17. Phillips SC, Mildvan MC, William DC, Gelb AM, and
contacts, are at high risk for their infections. 16'27 White MC: Sexual transmission of enteric protozoa and hel-
In the evaluation of patients with a genital ulcer, minths in a venereal-disease-clinic population. N Engl J Med
305: 605-606, 1981.
one s h o u l d suspect an amebic ulcer w h e n e v e r a 18. Quinn TC, Stamm WE, Goodell SE, Mkritichian E, Be-
patient presents with balanoposthitis or a penile nedettiJ, Corey L, Schuffler MD, and Holmes KK: The polym-
ulcer that resists antibiotics. Biopsy or scrapings icrobial origin of intestinal infections in homosexual men. N
from freshly collected necrotic exudate are fun- EnglJ Med 309: 576-582, 1983.
d a m e n t a l in isolating the t r o p h o z o i t e s to confirm 19. Markell EK, Havens RF, Kuritsubo RA, and WingerdJ:
Intestinal protozoa in homosexual men of the San Francisco
the diagnosis. Metronidazole and h y d r o c h l o r i c Bay area: prevalence and correlates of infection. Am J Trop
emetine offer an excellent regression and fast-heal- Med Hyg 33: 239-245, 1984.
ing process of these ulcers. 20. Schain D, Ravdin JI: Entamoeba histolytica and other
intestinal amoeba, in Gorbach SL, Bartlett JG, and Blacklow
NR (Eds): Infectious Diseases, Philadelphia, Saunders, 1992,
REFERENCES pp 1953-1959.
1. Herman HB, and Berman LS: Penile ulcer caused by 21. Krauss SJ: Evaluation and management of acute genital
Entamoeba histolytica. JAMA 120: 827-830, 1942. ulcers in sexually active patients. Urol Clin North Am 11:
2. Mylius RE, Ten Seldam RE: Venereal infection by En- 155-162, 1984.
tamoeba histolytica in a New Guinea native couple. Trop 22. Burgers JK, Badalament RA, and Drago JR: Penile can-
Geogr Med 14: 20-26, 1962. cer: clinical presentation, diagnosis and staging. Urol Clin
3. Quevedo MA, and Elias-Dib J: A case of amebiasis of North Am 19: 247-256, 1992.
the penis. Medicina (Mexico) 43: 240-243, 1963. 23. Chapel TA, Brown WJ, Jeffres C, and Stewart JA: How
4. Shih HE, Wu GK, and Lieu VT: The dysenteric disor- reliable is the morphological diagnosis of penile ulcerations?
ders, in Manson-Bahr P (Ed): Synopsis of Tropical Medicine, Sex Transm Dis 4: 150-152, 1977.
2nd ed. London, Cassell, 1943, pp 249-260. 24. Keystone JS, Keystone DL, and Proctor EM: Intestinal
5. Sosa-Camacho B, and Beirana L: Amibiasis cutanea parasitic infections in homosexual men: prevalence, symp-
genital. Dermatologia 3: 127-129, 1959. toms and factors in transmission. Can Med AssocJ 123: 512-
6. Straub M: Geneesk. tijdschr, v Nederl Indie 64: 989, 514, 1980.
1924. 25. Jessamine PG, and Ronald AR: Chancroid and the role
7. Talwalkar GV: Amebiasis of the penis. J Indian Med of genital ulcer disease in the spread of human retroviruses.
Assoc 39: 103-104, 1962. Med Clin North Am 74: 1417-1431, 1990.
8. Purpon I, Jimenez D, and Lopez R: Amebiasis of the 26. Moss AR, Bacchetti P, Osmond D, Dritz S, Abrams D,
penis. J Urol 98: 372-374, 1967. Conant M, Volberding P, and Ziegler J: Incidence of the ac-
9. Parkash S, Ramakrishnan K, Ananthakrishnan N, quired immunodeficiency syndrome in San Francisco, 1980-
Topno M, and Aurora AL: Amoebic ulcer of the penis. Post- 1983. J Infect Dis 152: 152-161, 1985.
grad Med J 58: 375-377, 1982. 27. Mildvan D, Gelb AM, and William DC: Venereal trans-
10. Castillo CG, Decanini LH, Yanez AE, and Rizzi HH: mission of enteric pathogens in male homosexuals: two case
Amebiasis del pene. Rev Mex Urol 31: 401-407, 1971. reports. JAMA 238: 1387-1389, 1977.
1 54 UROLOGY 48 (1), 1996
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Essentials of MicrobiologyDokument647 SeitenEssentials of MicrobiologyMarsidi SaidNoch keine Bewertungen
- YersiniaDokument16 SeitenYersiniaAlexandra Ançã PiresNoch keine Bewertungen
- Bachelor of Science Degree in Food - Nutrition and DieteticsDokument42 SeitenBachelor of Science Degree in Food - Nutrition and Dieteticspaul machariaNoch keine Bewertungen
- Annual Infection Control Report Für 2021Dokument26 SeitenAnnual Infection Control Report Für 2021Ruby Joyce AguilarNoch keine Bewertungen
- RetrovirusDokument23 SeitenRetrovirusali haidarNoch keine Bewertungen
- Han Dog 2017Dokument10 SeitenHan Dog 2017ErtyWitalayaL.ToruanNoch keine Bewertungen
- Paranasal Sinus Opacification-To-Pneumatization Ratio Applied As A Rapid and Validated Clinician AssessmentDokument6 SeitenParanasal Sinus Opacification-To-Pneumatization Ratio Applied As A Rapid and Validated Clinician AssessmentErtyWitalayaL.ToruanNoch keine Bewertungen
- Advanced Basal Cell Carcinoma, The Hedgehog Pathway, and Treatment Options - Role of Smoothened InhibitorsDokument12 SeitenAdvanced Basal Cell Carcinoma, The Hedgehog Pathway, and Treatment Options - Role of Smoothened InhibitorsErtyWitalayaL.ToruanNoch keine Bewertungen
- Srep 30353Dokument7 SeitenSrep 30353ErtyWitalayaL.ToruanNoch keine Bewertungen
- (Doi 10.1007/978!3!319-62061-9 - 27) Scarfe, William C. Angelopoulos, Christos - Maxillofacial Cone Beam Computed Tomography - CBCT-Based Image Guidance For Sinus and Skull Base SurgeryDokument14 Seiten(Doi 10.1007/978!3!319-62061-9 - 27) Scarfe, William C. Angelopoulos, Christos - Maxillofacial Cone Beam Computed Tomography - CBCT-Based Image Guidance For Sinus and Skull Base SurgeryErtyWitalayaL.ToruanNoch keine Bewertungen
- 4 106 1 PB PDFDokument4 Seiten4 106 1 PB PDFErtyWitalayaL.ToruanNoch keine Bewertungen
- Changing Pattern of Cutaneous Tuberculosis: A Prospective StudyDokument7 SeitenChanging Pattern of Cutaneous Tuberculosis: A Prospective StudyErtyWitalayaL.ToruanNoch keine Bewertungen
- Treatment of Chromoblastomycosis: Brooklyn, New YorkDokument5 SeitenTreatment of Chromoblastomycosis: Brooklyn, New YorkErtyWitalayaL.ToruanNoch keine Bewertungen
- Granuloma Inguinale: RquchDokument9 SeitenGranuloma Inguinale: RquchErtyWitalayaL.ToruanNoch keine Bewertungen
- Microchimica Acta Volume 181 Issue 15-16 2014 (Doi 10.1007/s00604-014-1297-3) Seok, Youngung Byun, Ju-Young Mun, Hyoyoung Kim, Min-Gon - Colorimetric Detection of PCR Products of DNA From PathogDokument7 SeitenMicrochimica Acta Volume 181 Issue 15-16 2014 (Doi 10.1007/s00604-014-1297-3) Seok, Youngung Byun, Ju-Young Mun, Hyoyoung Kim, Min-Gon - Colorimetric Detection of PCR Products of DNA From PathogErtyWitalayaL.ToruanNoch keine Bewertungen
- Harrison 1501Dokument1 SeiteHarrison 1501ErtyWitalayaL.ToruanNoch keine Bewertungen
- Chapter Quiz For Antimicrobial AgentsDokument1 SeiteChapter Quiz For Antimicrobial AgentsIrwan M. IskoberNoch keine Bewertungen
- Riesgo MicrobiologicoDokument47 SeitenRiesgo MicrobiologicocarbouNoch keine Bewertungen
- SW Chapter 21 KeyDokument9 SeitenSW Chapter 21 KeykylevNoch keine Bewertungen
- ACTINOMYCESDokument47 SeitenACTINOMYCESSushant KumarNoch keine Bewertungen
- 4 ISOLATION AND IDENTIFICATION OF Escherichia Coli ISOLATED FROM LAYER CHICKEN IN CHICKEN VILLAGE NORTH LOMBOKDokument3 Seiten4 ISOLATION AND IDENTIFICATION OF Escherichia Coli ISOLATED FROM LAYER CHICKEN IN CHICKEN VILLAGE NORTH LOMBOKCatur DewantoroNoch keine Bewertungen
- Principles of Aseptic Technique in An Operating Room1Dokument2 SeitenPrinciples of Aseptic Technique in An Operating Room1Joezerk Jhon Biel100% (1)
- Cervical Cancer Awareness MonthDokument16 SeitenCervical Cancer Awareness MonthParpar IparNoch keine Bewertungen
- Norfloxillin 200 Sol.: Bi D VW WJB 200 MJDokument2 SeitenNorfloxillin 200 Sol.: Bi D VW WJB 200 MJSharfina Akter BithiNoch keine Bewertungen
- All About TonsillitisDokument4 SeitenAll About TonsillitisJennifer AsistidoNoch keine Bewertungen
- MK CoryzaDokument3 SeitenMK CoryzaMoses Jr KazevuNoch keine Bewertungen
- Bacterial Pathogens in Chicken Meat-444Dokument7 SeitenBacterial Pathogens in Chicken Meat-444bhawana bhattNoch keine Bewertungen
- UntitledDokument30 SeitenUntitledLEE JIA XINNoch keine Bewertungen
- Comparison Chart of Gram +ve & - VeDokument2 SeitenComparison Chart of Gram +ve & - Veسيفل إسلامNoch keine Bewertungen
- Home Remedies For UtiDokument5 SeitenHome Remedies For UtiShiro KiryuuNoch keine Bewertungen
- Chiron & NAT Introduction KL 29APR08Dokument35 SeitenChiron & NAT Introduction KL 29APR08api-3750327100% (1)
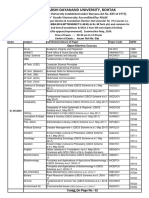
- 4 - 04!24!2024!15!07-09 - Open Elective & Foundation Elective Courses 2nd Semester Date Sheet May 2024Dokument2 Seiten4 - 04!24!2024!15!07-09 - Open Elective & Foundation Elective Courses 2nd Semester Date Sheet May 2024ujjwaltiwari319Noch keine Bewertungen
- Essential Oil Composition and Antimicrobial Interactions of Understudied Tea Tree SpeciesDokument8 SeitenEssential Oil Composition and Antimicrobial Interactions of Understudied Tea Tree SpeciesxiuhtlaltzinNoch keine Bewertungen
- CIA Patho 1Dokument23 SeitenCIA Patho 1Suhas H GNoch keine Bewertungen
- Writting Discussion TextDokument2 SeitenWritting Discussion TextAditya Diyan100% (1)
- Stool AssessmentDokument2 SeitenStool AssessmentAlex MendozaNoch keine Bewertungen
- Astm 2315Dokument5 SeitenAstm 2315yuanlupeNoch keine Bewertungen
- Establishing MIC Breakpoints and Interpretation of in Vitro Susceptibility TestsDokument13 SeitenEstablishing MIC Breakpoints and Interpretation of in Vitro Susceptibility TestsakshayajainaNoch keine Bewertungen
- Form P (Weekly Reporting Format - IDSP) : Oriana Hospital PVT - LTDDokument2 SeitenForm P (Weekly Reporting Format - IDSP) : Oriana Hospital PVT - LTDRavi ParmarNoch keine Bewertungen
- Pharmacology Obat Lepra Dan TBC Kutis: Dharma Permana, PHD, AptDokument33 SeitenPharmacology Obat Lepra Dan TBC Kutis: Dharma Permana, PHD, AptanggiNoch keine Bewertungen
- Teesside Covid Testing: WWW - Recovery4life - Co.ukDokument2 SeitenTeesside Covid Testing: WWW - Recovery4life - Co.ukjames gNoch keine Bewertungen