Beruflich Dokumente
Kultur Dokumente
Patient Comunication
Hochgeladen von
biozeusCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Patient Comunication
Hochgeladen von
biozeusCopyright:
Verfügbare Formate
Downloaded from www.ajronline.org by 79.169.193.56 on 07/19/15 from IP address 79.169.193.56. Copyright ARRS.
For personal use only; all rights reserved
Opinion
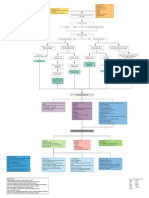
Patient Communication: What to Teach
Radiology Residents
Richard B. Gunderman 1
What weve got here is a failure to tion [2]. Most patients assume that they are re- communicatorstraits training programs
communicate. ceiving technically competent care; the quality should aim to fosterand a list of 10 practical
of the patientphysician relationship is the ma- techniques that radiology residents can be en-
Donn Pearce and Frank R. Pierson jor determinant of their satisfaction. Moreover, couraged to implement as they interact on a
Cool Hand Luke (screenplay) communication has been proven to affect pa- daily basis with patients.
tient outcomes [3]. For example, patients who
highly rate the quality of communication they
Traits of Effective Communicators
T
he standards by which residents will have with their physicians tend to require less
be evaluated in the future are chang- analgesia and enjoy higher functional status [4]. Sensitivity
ing. The American Board of Medi- Communication is also a major factor in medi- A resident was obtaining informed consent
cal Specialties has adopted six general cal malpractice suits: Low-quality communica- from a parent for a complex interventional pro-
competencies for all physicians [1]. These in- tion is a higher predictor of litigation than cedure her child was to undergo. After explain-
clude medical knowledge, patient care, interper- adverse outcomes [5], and 70% of depositions ing some of the more common complications,
sonal and communication skills, professionalism, show evidence of faulty communication [6]. Fi- the resident explicitly warned the mother that
practice-based learning and improvement, and nally, high-quality communication with patients one possible outcome could be death in the in-
systems-based practice. Radiology educators is associated with higher levels of career satis- terventional laboratory. After the resident left
need to take a close look at these competencies faction among physicians, indicating that efforts the room, the child burst into tears, terrified
and determine what their implications may be for to improve patientphysician communication that he was going to die during the procedure.
the future of radiology. To that end, this article fo- can benefit not only patients but also physicians It is imperative that all physicians interacting
cuses on the third of the six general competen- themselves [7]. with patients and families manifest a high de-
cies, interpersonal and communication skills. We Radiology residents must be given opportu- gree of sensitivity to their needs and vulnerabili-
spend huge amounts of time training residents to nities to improve their communication skills. ties. Radiologic tests and procedures are routine
detect lesions, offer appropriate differential diag- Physician develop habits or styles of interact- for the radiologist, but they are usually new ex-
noses, and perform procedures, but little or no ing with patients, and those habits can be posi- periences for patients and families and may pro-
time teaching them how to communicate with tively influenced by appropriate educational voke a considerable degree of anxiety. Patients
patients. How can we prepare residents to be experiences during their formative years. By often regard imaging examinations as potential
more effective communicators throughout their helping residents adopt effective habits of pa- threats, insofar as they may reveal life-threaten-
careers as practicing radiologists? tient communication early in their training, ing diseases or injuries. Moreover, providing
There are important reasons for all physi- residency programs can improve patient care, patients with the information they need to give
cians to be effective communicators. First, a enhance career satisfaction, and enrich the fu- informed consent brings to their attention addi-
clear correlation exists between the quality of ture of radiology itself. What follows is a dis- tional risks of the procedures themselves. Physi-
communication and the level of patient satisfac- cussion of six key characteristics of effective cians can not simply neglect to mention the
Received December 8, 2000; accepted after revision January 17, 2001.
1
Department of Radiology, Indiana University School of Medicine, 702 Barnhill Dr., RI 1053, Indianapolis, IN 46202-5200. Address correspondence to R. B. Gunderman.
AJR 2001;177:4143 0361803X/01/177141 American Roentgen Ray Society
AJR:177, July 2001 41
Gunderman
unpleasant aspects of imaging, nor should they each patient, but nearly every patient encounter pecuniary self-interest but out of a commitment
sugar coat the risks in an effort to make things is an important opportunity for education. Tak- to their welfare, and that their doctor will be
easier for patients. On the other hand, such dis- ing a minute or two to educate patients relieves a there for them in times of need. When a patient
cussions can be handled in a gentle and com- good bit of their anxiety about the unknown. perceives that a physician has acted dishonestly,
passionate way, and residents should endeavor Moreover, administering even minidoses of word of mouth can damage the regard of many
to interact with families with the same degree of teaching automatically invites the physician to friends and family members for the whole pro-
Downloaded from www.ajronline.org by 79.169.193.56 on 07/19/15 from IP address 79.169.193.56. Copyright ARRS. For personal use only; all rights reserved
sensitivity they would hope other physicians look at the health care encounter from the pa- fession of medicine. The career of every physi-
would show their family members. tients point of view (Does he or she understand cian has been enriched by the high standard of
what I am doing and saying?), and gives the pa- conduct observed by professional forebears,
Courtesy tient the sense of being treated as a person. and it is incumbent on each physician to pre-
A busy attending radiologist and a resident serve that trust for generations of physicians yet
entered a patient examination room. Without a Appropriateness to come. If something unfortunate has hap-
word to the patient, they began to discuss the Because of time constraints, a team of medi- pened, it is better to acknowledge and express
patients condition and the appropriate tech- cal students came into the radiology department regret about it than to attempt to cover it up.
nique for the examination. A minute later, they to interview a father awaiting the completion of
both left the room, without ever saying hello to his sons imaging examination. He later com- Openness
her or introducing themselves. The patient plained, They were rude and asked the most ri- A patient sat silently as two radiologists
later reported that she wasnt sure they realized diculous questions they could think of: whether discussed his case. After they left the room,
that she had been in the room. I am married to the childs mother, and whether the patient commented, They never let me
Patients are human beings too, and deserve to I have ever been arrested for child abuse. For in on what they were thinking. I would have
be treated with an appropriate level of respect Gods sake, my son had a heart murmur picked liked to know why they were saying all those
and civility. It can be extremely disconcerting up at a routine check-up. things, but instead I just felt like an idiot.
and even humiliating to be talked to or about No template for the patientphysician en- Patients should be regarded not as passive re-
without having first been introduced. The health counter works well in all cases. Radiologists cipients of medical ministrations, but as active
care enterprise is a complex one, especially from must be attuned to the situation at hand and participants in their own care. Keeping the pa-
the patients point of view, and patients may adapt their approach accordingly. Even a single tient in the dark merely breeds uncertainty
come into contact with a bewildering variety of inappropriate comment or question can seri- and anxiety, as well as a sense of impotence that
health care workers during a single visit. A phy- ously undermine the relationship between a pa- is antithetical to a strong patientphysician alli-
sician would never start an examination on a pa- tient and a physician. Everything the radiologist ance. By getting patients actively involved in
tient without first verifying the patients identity, says to the patient is an opportunity to assess the their own care, physicians can improve both the
and patients have the same interest in knowing patients response and to adapt the discussion technical outcomes of care, through improved
who is caring for them. No matter how pressed accordingly, not simply a one-way transfer of patient compliance, and patients overall satis-
for time or overworked residents may be, even information. A key to effective communication faction with the care they have received [9].
forgiving patients are likely to perceive the resi- is good listening, including the ability to tune in Moreover, keeping patients informed and in-
dents as rude if they fail to introduce themselves. to nonverbal clues to the patients state of mind. volved bespeaks a high level of physician re-
spect that helps to preserve and promote
Compassion Honesty patients sense of their own vigor and dignity.
During a prolonged interventional procedure During an imaging procedure, the radiology Many of the procedures through which we put
performed under local anesthesia, the radiolo- nurse recommended that the resident use a par- patients can seem awkward and even dehuman-
gists present discussed the similarities and differ- ticular piece of equipment. The resident in- izing, but explanations of what will happen and
ences between this patients condition and others formed the nurse that her suggestion was why go a long way toward putting them at ease.
they had seen in the recent past. In part because inappropriate. Later, when the attending radiol- One of the best ways to make the experience
they never took time to explain to the patient ogist entered to room to observe, he asked the less discomfiting is to give patients opportuni-
what they were doing or why, the patient later resident why he hadnt used that piece of equip- ties to pose questions and take the time to an-
complained that the experience left her feeling ment. To the patients surprise, the resident took swer them appropriately. Many experiences in
like a piece of meat under a microscope. no responsibility and instead blamed the nurse, the health care arena are so new that patients
Patients need to know that those caring for who had since left the room. may have difficulty formulating questions. In
them view them not merely as an assemblage of Few things are more corrosive to the trust on such cases, it can be helpful for the physician to
organs or tissues, but as persons. This principle is which good patientphysician relationships de- offer, Some of the patients undergoing this
succinctly embodied in the comment of another pend than dishonesty. Even apparently innocu- procedure wonder about. Such openness
patient, who complained, I am a human being, ous instances of deception, the white lies a helps patients feel that the radiologist under-
not a laboratory rat. Because the radiologists physician might be tempted to tell in order to stands where they are and cares enough to help
expertise is based so thoroughly on images, re- provide reassurance to a patient, ultimately do them understand what is going on.
stricting the professional gaze to the anatomic more harm than good by undermining trust [8].
interior of the patient is an ever-present occupa- Because patients need to be able to entrust phy- Practical Tips
tional liability. Yet from the patients point of sicians with their lives, physicians have a duty These traits of effective communicators pro-
view, what the radiologist says is every bit as sig- to deal honestly with patients at all times. Pa- vide a theoretical underpinning for the develop-
nificant as what the radiologist does. Radiolo- tients need to know that they can confide in their ment of daily habits of effective communication.
gists need not take time out to give a lecture to doctor, that their doctor is operating not from However, the translation of theory into practice
42 AJR:177, July 2001
Teaching Patient Communication
is not always a straightforward matter. To show Ask if the patient has any questions. Take diology residents must not be left with the im-
how these traits manifest themselves practically time to answer them, including, when appro- pression that the techniques of effective
in interactions between radiologists and patients, priate, the admission, We dont know. communication deserve attention merely be-
I list 10 simple habits of communication that all Listen, giving the patient your undivided at- cause they provide a means of manipulating pa-
physicians can make use of in the first few min- tention. It is acceptable to jot down notes as the tients to achieve more important goals, such as
utes of every patient encounter. It is important patient talks, but those notes should pertain to higher customer satisfaction ratings or reduced
Downloaded from www.ajronline.org by 79.169.193.56 on 07/19/15 from IP address 79.169.193.56. Copyright ARRS. For personal use only; all rights reserved
that radiologists not view the first minute or two what the patient is actually saying. medicallegal liability. Rather, effective com-
of a patient encounter as a mere formality, an es- Look for opportunities to express respect munication and the enrichment of the pa-
sentially meaningless exchange of pleasantries, and admiration. Telling patients and families tientphysician relationship are worthy ends
but that they treat it as a crucial stage in building that they are doing a good job frequently in themselves and deserve to be pursued for
a healthy patientphysician relationship. means more to them than physicians would their own sake, regardless what other benefits
Introduce yourself, shake hands with the pa- ever suppose and enhances their ability to cope they produce. They lie at the core of what it
tient and every family member or friend in the with bad news, should the need arise. means to be a good doctor, something to which
room, and find out their names and relation- all good radiologists intrinsically aspire.
ship. You do not want to mistakenly refer to the
Conclusion
patients mother as grandma during the ex-
amination. Having considered what radiology residents
Whenever addressing the patient and fam- need to know about effective patient commu- References
ily members, refer to them by name, generally nication, how can we teach such skills? One 1. Hattery RR. The presidents message. ABR Ex-
aminer 2000;5:13
using Mr., Mrs., or Ms. Make sure you have starting point is to make use of the vignettes
2. Brody DS, Miller SM, Lerman CE, et al. The rela-
understood everyones name correctly; if nec- described, asking a group of residents to dis- tionship between patients satisfaction with their
essary, ask them to spell it. cuss opportunities to improve the quality of physicians and perception about intervention they
Make eye contact with the person to whom communication in each case. In the course of devised and received. Med Care 1989;27:10271035
you are speaking. It is disconcerting to be critiquing instances of poor communication, 3. Greenfield S, Kaplan S, Ware JE. Expanding pa-
spoken to by someone who never looks you residents become more attentive to their own tient involvement in care: effects on patient out-
in the eye, because it creates the impression approaches. Second, staff radiologists should comes. Ann Intern Med 1985;102:520528
4. Stewart MA. Effective physician-patient commu-
that they are avoiding something. make an effort to observe residents interac-
nication and health outcomes: a review. Can Med
Touch the patient. No words can substitute. tions with patients and to provide structured, Assoc J 1995;152:14231433
Find out routinely how long the patient has constructive feedback. Communication de- 5. Levinson W, Roter DL, Mullooly J, Dull VT,
been waiting, and acknowledge it. When the serves every bit as much one-on-one attention Frankel RM. Physician-patient communication:
wait has been especially long, consider offer- as differential diagnosis and catheter tech- the relationship with malpractice claims among
ing some explanation. It is possible to express nique. Finally, programs can provide addi- primary care physicians and surgeons. JAMA
1997;277:553559
regret without accepting unwarranted blame. tional resources for effective communication,
6. Beckman HB, Markakis KM, Suchman AL,
Convey an understanding of the patients his- including information on verbal, nonverbal, Frankel RM. The doctor-patient relationship and
tory. Such a demonstration provides reassurance and image-mediated approaches as well as malpractice: lessons from plaintiff depositions.
that the radiologist has done his homework, tools for assessing patients level of under- Arch Intern Med 1994;154:13651370
and gives the patient a chance to expand or clar- standing, conversing with patients who speak a 7. Chuck JM, Nesbitt TS, Kwan J, Kam SM. Is being
ify any important points. different language, and interacting with dis- a doctor still fun? West J Med 1993;159:665669
8. Thom DH, Ribisl KM, Stewart AL, Luke DA. Fur-
Briefly explain any tests or procedures in abled patients.
ther validation and reliability testing of the trust in
language that the patient and family can un- In discussing useful techniques of communi- physicians scale. Med Care 1999;37:510517
derstand. A key part of any explanation is the cation, the teaching physician should stress that 9. Safran DG, Taira DA, Rogers WH, et al. Linking
rationale, why the examination is being per- high-quality patientphysician interaction is not primary care performance to outcomes of care. J
formed in the first place. merely a tool to be used for some other end. Ra- Family Practice 1998;47:213220
AJR:177, July 2001 43
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Dr. Horowitz Continues To Expose True Origins of HIV and EbolaDokument3 SeitenDr. Horowitz Continues To Expose True Origins of HIV and Eboladinh son my100% (2)
- Banco de Preguntas ReabilitacionDokument19 SeitenBanco de Preguntas ReabilitacionVanessa AlcantaraNoch keine Bewertungen
- ICMR Award 2017-18 Citation Booklet PDFDokument30 SeitenICMR Award 2017-18 Citation Booklet PDFHarshendra GuduruNoch keine Bewertungen
- Post Stroke Scalp AcupunctureDokument64 SeitenPost Stroke Scalp AcupunctureJosé Mário91% (11)
- 2021.10.27 Letter To NIHDokument14 Seiten2021.10.27 Letter To NIHZerohedge Janitor100% (1)
- Mental Health Studyguide Part 1Dokument39 SeitenMental Health Studyguide Part 1Ngoc TB VoNoch keine Bewertungen
- Incident vs. Prevalent Cases and Measures of OccurrenceDokument3 SeitenIncident vs. Prevalent Cases and Measures of OccurrenceRenzo FernandezNoch keine Bewertungen
- Embase OnlyDokument138 SeitenEmbase OnlyAnastasiaKurtiNoch keine Bewertungen
- Tomczyk Dominika Resume 0812-2020Dokument1 SeiteTomczyk Dominika Resume 0812-2020api-535602662Noch keine Bewertungen
- 1.1.2 OSH Foundations and Its Benefits - CEC 003-CEC32S6 - Construction Occupational Safety and Health (COSH)Dokument4 Seiten1.1.2 OSH Foundations and Its Benefits - CEC 003-CEC32S6 - Construction Occupational Safety and Health (COSH)RYAN JOSEPH QUIMONoch keine Bewertungen
- SerratiopeptidaseDokument4 SeitenSerratiopeptidaseMo KhanNoch keine Bewertungen
- Psychiatrist in Pune - Dr. Niket KasarDokument8 SeitenPsychiatrist in Pune - Dr. Niket KasarDr. Niket KasarNoch keine Bewertungen
- Indian AdministrationDokument52 SeitenIndian Administrationcitidotnet100% (1)
- Kasus 1 RKG 5 Euginia YosephineDokument5 SeitenKasus 1 RKG 5 Euginia YosephineEuginia YosephineNoch keine Bewertungen
- Patient Safety Full ReportDokument40 SeitenPatient Safety Full ReportYudi Ariesta Chandra100% (1)
- Cardiology BrochureDokument2 SeitenCardiology Brochureong251183Noch keine Bewertungen
- Teenage Pregnancy Position PaperDokument1 SeiteTeenage Pregnancy Position PaperBryll Bryan Mantatao PonNoch keine Bewertungen
- Medical Marijuana BrochureDokument2 SeitenMedical Marijuana BrochureMPP100% (1)
- Philippine Practice Standards For PharmacistsDokument8 SeitenPhilippine Practice Standards For PharmacistsAgatha Rose100% (1)
- Pre Authorization FormDokument1 SeitePre Authorization FormKhuda BukshNoch keine Bewertungen
- Sample of MRCOG Assessment 2021 - Saeed HasanDokument28 SeitenSample of MRCOG Assessment 2021 - Saeed HasanIslam AwniNoch keine Bewertungen
- Metronidazole Drug StudyDokument2 SeitenMetronidazole Drug StudyA.Noch keine Bewertungen
- Myocardial Infarction With CABG Concept MapDokument1 SeiteMyocardial Infarction With CABG Concept MapMaria Therese100% (1)
- RN Circulator FlyerDokument1 SeiteRN Circulator FlyerLucas JelmarNoch keine Bewertungen
- Ourse Yllabus Section I - College and University Catalog DataDokument5 SeitenOurse Yllabus Section I - College and University Catalog DatabagusNoch keine Bewertungen
- Electronic Patient Report FormDokument6 SeitenElectronic Patient Report FormDS Systems0% (1)
- Case Study 2Dokument3 SeitenCase Study 2XilcaNoch keine Bewertungen
- Shah - Cancer of The Head and Neck PDFDokument12 SeitenShah - Cancer of The Head and Neck PDFElizabetha SalzcenNoch keine Bewertungen
- EthnolecrepooooorttpdfDokument61 SeitenEthnolecrepooooorttpdfNoelle Grace Ulep BaromanNoch keine Bewertungen
- Patients ' Views of Wearable Devices and Ai in Healthcare: Findings From The Compare E-CohortDokument8 SeitenPatients ' Views of Wearable Devices and Ai in Healthcare: Findings From The Compare E-CohortPratush RajpurohitNoch keine Bewertungen