Beruflich Dokumente
Kultur Dokumente
Airway
Hochgeladen von
Nirma RahayuOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Airway
Hochgeladen von
Nirma RahayuCopyright:
Verfügbare Formate
Methods of Identifying and Managing the
Difficult Airway in the Pediatric Population
Joshua Belanger, CRNA
Mark Kossick, CRNA, DNSc
The goal of this literature review is to provide the ment techniques, normal pediatric airway anatomy,
anesthesia practitioner with the skill set to detect and and respiratory physiology. An emphasis is placed on
prepare for a difficult pediatric airway. The authors some common syndromes and their related anatomi-
have reviewed and compiled information on some cal abnormalities that can compromise the airway, as
of the most common conditions that can predis- well as anesthetic approaches recommended to suc-
pose pediatric patients to a difficulty airway, such as cessfully secure a potentially difficult airway.
macroglossia, mandibular hypoplasia, micrognathia,
cervical instability, limited cervical movement, maxil-
lary and midfacial hypoplasia, and cleft palate. This Keywords: Congenital, difficult airway, malformation,
article provides an overview of preoperative assess- pediatric.
A
irway management is a mainstay of anes- One primary objective of the authors assessment
thesia practice. Practitioners are required of the pediatric airway literature was to enhance the
to have a firm grasp on airway physiology, anesthetists ability to detect and prepare for a diffi-
assessment, and management, and regular cult pediatric airway, thereby improving overall airway
exposure to this aspect of anesthesia is vital management skills. For the purposes of this review, the
to maintaining these skills. Unfortunately, for many anes- authors have defined a DA as one in which adequate gas
thesia practitioners, only limited opportunities to manage exchange is not readily accomplished through mask ven-
the pediatric airway exist. tilation, airway adjuncts such as oral and nasal airways,
Statistics compiled in 1993 from the American Society or a combination of the two. A difficult intubation is
of Anesthesiologists Closed Claims Database have dem- said to occur when an experienced provider requires 3
onstrated that respiratory events were more common or more attempts to place an endotracheal (ET) tube,
in the pediatric population (ie, 5 years of age and with or without rescue adjuncts, such as retrograde
younger) than in the adult population. Specific respira- wires, light wands, video laryngoscopes, or gum elastic
tory events relative to this review (eg, airway obstruc- bougies.
tion, difficult intubation, inadequate ventilation) were
also shown to occur at a greater frequency in children Review of the Literature
(34%) vs adults (23%).1 The database also revealed that Using multiple online resources, such as EBSCOhost.
of 238 pediatric claims reviewed, 67 (28%) occurred in com, ScienceDirect.com, and PubMed.gov, the authors
children under the age of 1 year.1 Since then, the rate of searched for publications relevant to pediatric airway as-
these specific respiratory events for all pediatric patients sessment and management, pediatric genetic malforma-
has decreased to approximately 7%.2 This decline in tions with airway management implications, and acute
adverse respiratory events may be attributed to many or chronic injuries that may potentially alter the normal
factors, including better monitoring equipment, such as pediatric airway, thereby making it difficult to secure.
pulse oximetry and end-tidal gas analysis,1,2 as well as Search words used to locate relevant articles included
safer medication profiles.2 airway, pediatric, malformation, Down syndrome, cleft
Although most pediatric airways may be easily secured palate, difficult, management, and assessment.
by the experienced practitioner, the potential still exists Unfortunately, many journal articles reviewed by the
for discovering a difficult airway (DA) after induction, authors did not operationalize the term pediatric, making
possibly leading to a cannot-intubate-cannot-ventilate sit- assessment and critique of such literature difficult. For
uation. One retrospective study involving 8,434 patients the purposes of this article, the term pediatric is subcat-
under the age of 18 years demonstrated the overall inci- egorized as follows: premature, born less than 37 weeks
dence of a difficult laryngoscopy to be 1.35%.3 This study gestation; neonate, birth to 1 month; infant, 1 month
also noted that those under the age of 1 year (n = 1,759) to 1 year; toddler, 1 to 3 years; child, 3 to 12 years; and
had the greatest risk of presenting with a DA (4.7%).3 adolescent, 13 to 18 years.
www.aana.com/aanajournalonline AANA Journal February 2015 Vol. 83, No. 1 35
Normal Pediatric Airway Anatomy and airway is the diameter of the cricoid ring. In the adult,
Physiology the narrowest portion of the upper airway is the vocal
The pediatric patient is both anatomically and physiologi- cords, as opposed to the cricoid cartilage in the neonate,
cally different from the adult patient in many ways. These infant, and young child.9 This difference makes the
differences are most important under 2 years of age4,5 larynx funnel shaped, as opposed to the cylindrical shape
and decrease as the child matures, with most differences of the adult and adolescent larynx.9 This feature allows
disappearing around 6 to 8 years of age. One difference the uncuffed ET tube to create a relative subglottic seal;
that is readily noticeable on assessment of the infant and the narrowing of the airway below the vocal cords presses
toddler is the proportionately larger head, specifically against the sides of the tube.10
the occipital area. This difference is clinically significant There are several anatomical differences in the pediat-
in that the pediatric patient may potentially benefit from ric patient that are important to the anesthesia provider,
a pillow or roll being placed under the shoulders, as although they are not part of the airway. The costae are
opposed to the head, to assist with neck flexion.5,6 In more horizontal and contribute less to inspiratory and
contrast, other researchers have suggested that direct expiratory efforts, forcing the diaphragm to do most of
laryngoscopy is most effective when the shoulders and the work in neonates. The infants respiratory muscles
head are on a flat surface and the neck is fully extended.7 are primarily composed of type II (fast-twitch) fibers,
The anatomy of the pediatric airway is composed and have lower stores of glycogen and fat, allowing them
of the same anatomical components as seen in adults, to become easily fatigued after short periods of exertion
although the size and position of several structures are or labored breathing.5,11 This physiologic characteristic
noticeably different. The most notable differences can be further emphasizes the importance of rapidly establish-
seen when the adult upper airway is compared with that ing and securing the pediatric airway.
of the neonate and infant upper airway. Compared with One of the most clinically significant physiologic
the adult, the neonate and infant nose is softer, with more factors unique to neonates, infants, and toddlers is their
mucous and lymphoid tissues present.8 Because of the elevated metabolic rate, leading to a rate of oxygen con-
smaller diameter of the nasal passages, it takes much less sumption more than double that of the adults5 (7-9 mL/
swelling or secretions to decrease total airflow, which kg/min compared with 3 mL/kg/min in adults). Another
can easily lead to obstruction5 since it has been suggested contributing factor to their more rapid rate of desatura-
that infants are obligate nasal breathers until they reach tion is their lower functional residual capacity,5 22 mL/
2 to 6 months of age.5 Being obligate nasal breathers is kg on average for toddlers12 vs 34 mL/kg for the adult.13
also important since an improperly placed face mask The newborn has just half the number of alveoli and only
can occlude the nares, creating an obstructed airway. 1/20th the surface area available for gas exchange com-
One airway structure that is proportionally larger in the pared with the adult, limiting oxygen absorption.14 The
pediatric patient than in the adult is the tongue. The pe- neonates and infants nervous system is predominantly
diatric tongue, especially during the neonatal and infant influenced by the parasympathetic system (because of
stages, is located closer to the palate by a more superiorly the incomplete maturation of the sympathetic nervous
located larynx, which potentiates airway obstructions. system), causing bradycardia in response to hypoxia and
Whereas the adult larynx is located at the junction of the further decreasing oxygen delivery.15 Because of these
fourth and fifth cervical vertebrae (C4-5), the neonate/ factors, when infants begin to experience an airway ob-
infant larynx is 1 level higher, typically located at C3-4,7 struction or become relatively tachypneic, they decom-
and may even be as high as C2-3.9 This superior position pensate more rapidly than do adults.
creates a more acutely angled view of the vocal cords
during direct laryngoscopy. Preoperative Assessment
Compared with the adult, the neonate and infant epi- Adult airway assessment systems are not always appli-
glottis tends to be longer, floppier, and omega shaped, cable to children. For example, the Mallampati classifi-
leading some authors to state that the straight laryngo- cation system and various measurements used to assess
scope blade may potentially be more effective in viewing the adult airway, such as thyromental and interincisor
the glottic opening.8 The epiglottis also sits at a greater distance, do not consistently correlate with the pediatric
angle to the anterior pharyngeal wall, making visualiza- patient population.5,16 However, the Mallampati classifi-
tion of the vocal cords more difficult.8 Like the epiglot- cation system has been shown to be applicable for use in
tis, most of the cartilaginous structures of the pediatric those 4 to 8 years of age.17 Because of this, the anesthesia
airway are softer (less ossified),9 and more pliable than provider will commonly rely on his or her physical as-
the adults, increasing the chances of compression and sessment and the surgeons history and physical exami-
obstruction of the airway when pressure is applied, such nation for predicting the DA in children.
as with the Sellick maneuver. As with all patients, the assessment process should
The last important anatomical difference of the upper begin with a thorough chart review, including the sur-
36 AANA Journal February 2015 Vol. 83, No. 1 www.aana.com/aanajournalonline
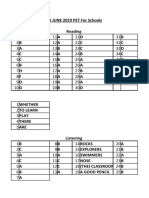
Incidence Potential related
Syndrome rate Common clinical features anatomical abnormalities
Down 11.8:10,000 Short stature, mental retardation, Macroglossia,21 cervical instability,22,23
live births20 hypotonia, epicanthal fold, mandibular hypoplasia/micrognathia,21,24
microcephaly, CHD maxillary/midfacial hypoplasia21,24,25
MPS (eg, 1:25,000 live Cognitive deficit, hearing/vision deficit, Macroglossia,27,28 cervical instability,27,28
Hurler, Hunter, births26 dwarfism, skeletal dysplasia, CHD, limited cervical movement27,28
Morquio) coarse facial features, myelopathy
Pierre Robin 1:8,500 live Respiratory compromise, feeding difficulty, Macroglossia (relative),30 mandibular
births29 glossoptosis, gastroesophageal reflux, CHD hypoplasia/micrognathia,30,31 cleft palate30,31
Treacher Collins 1:50,000 live Aplastic zygomas, microstomia, CHD Mandibular hypoplasia/micrognathia,33
births32 maxillary/midfacial hypoplasia,33 cleft palate32,34
Table. Congenital Syndromes and Their Related Anatomical Abnormalities
Abbreviations: CHD, congenital heart defect; MPS, mucopolysaccharidosis.
geons history and physical examination and any prior child breathes best.19 With pediatric patients, the physi-
anesthetic records, as well as the current airway physical cal examination may be incomplete because of a lack of
findings. Any mention of an abnormal birth or gestation- cooperation from the child. If the patient is cooperative,
al age, recent illnesses or surgeries, breathing problems, the tongue and airway should be assessed, as well as in-
or congenital abnormalities, should be further explored terincisor distance and the status of the teeth. Any loose
with the parent or caregiver. Studies have shown that the deciduous teeth should be documented on the chart; this
type of scheduled surgery may be a good indicator for a primarily affects the 5- to 10-year-old age group.
DA. Pediatric patients undergoing cardiac surgery or oral
and maxillofacial surgery have the highest prevalence of Anatomical Abnormalities of Congenital,
difficult intubations (40%),3 and half of these patients Genetic, and Acquired Malformations
presenting as a difficult intubation also have some form One prominent reason for a DA in the pediatric patient is
of malformation.3 an anatomical malformation. Although many congenital,
Once the chart has been reviewed, a physical as- genetic, and acquired malformations and abnormali-
sessment should be performed. Some general observa- ties may present as a cluster, many may also present in
tions should be made, starting with the head and face. isolation (eg, cleft palate). Malformations presenting as
When viewed from the side, the chin and location of a group may also define a syndrome (eg, Pierre Robin).
the lower teeth in relation to the upper teeth should be Although most anesthesia practitioners may never en-
evaluated. A hypoplastic chin, or micrognathia, as seen counter a rare malformation, other abnormalities may be
in many genetic malformations, is a good indicator of a seen infrequently depending on the providers practice
DA.8 Flexion and extension of the neck can also be as- setting; for example, Down syndrome has a reported inci-
sessed from the side, potentially revealing limitations, dence of 11.8 cases per 10,000 live births.20 Although it is
instabilities, tumors, or goiters. Some additional items outside the scope of this article to cover all acquired and
to assess are head size and symmetry, patients activity congenital malformations, as well as all types of airway
level, breathing pattern and sounds, posture, and color. devices, some of the more familiar anatomical abnormali-
It would also be prudent to ask the caregiver about any ties known to affect the pediatric airway are listed in the
recent upper respiratory tract infections, which could Table.20-34
predispose the patient to a hyperreactive airway. A child Macroglossia. Macroglossia, defined as a propor-
who is resting in the sniffing position or tripod position tionately large tongue, has the potential to create a DA
could indicate respiratory distress, as could unexplained through posterior migration of the tongue, either during
restlessness or agitation. The use of accessory muscles or after induction. This can cause an airway obstruction
for breathing should also be assessed. Noisy breathing, and make it difficult to mask ventilate and obtain an
snoring, nasal congestion, or an impaired sense of smell adequate view of the vocal cords during laryngoscopy.
without a runny nose could indicate adenoid or tonsillar One congenital defect that commonly presents with
enlargement.18 Excessive daytime somnolence, morning macroglossia is mucopolysaccharidosis (MPS).27 This ly-
headaches, loud and abnormal mouth breathing, snoring, sosomal storage disease consists of 7 different syndromes
attention problems, hyperactivity, or a history of apnea (Hurler, Hunter, Sanfilippo, Morquio, Maroteaux-Lamy,
could indicate an airway obstruction or obstructive sleep Sly, and Natowicz); with Hurler syndrome being associ-
apnea (OSA), which could worsen after induction of the ated with the highest incidence of difficult intubation
anesthetic.19 Asking the caregiver or caregivers how the (27.6%-54%).27,35
child prefers to sleep will give an indication as to how the Although macroglossia typically presents as a result of
www.aana.com/aanajournalonline AANA Journal February 2015 Vol. 83, No. 1 37
a congenital malformation,27 it may also occur second- Mandibular Hypoplasia and Micrognathia. Mandibular
ary to acute trauma or an allergic response. This could hypoplasia and micrognathia are considered by some
include angioedema of the tongue; angiotensin-converting authors as synonyms for an undersized mandible. One
enzyme inhibitors, which are regularly prescribed to pedi- syndrome commonly associated with this condition is
atric patients with congenital heart defects (CHDs), have Pierre Robin syndrome. The clinical triad of this syndrome
been known to produce lingual subcutaneous edema. consists of micrognathia, cleft palate, and glossoptosis, or
Macroglossia is one of the more easily treated malfor- a downward displacement of the tongue.31,36 When this
mations, potentially requiring an oral airway while per- clinical triad is accompanied by additional malformations
forming mask ventilation and use of video laryngoscopy or syndromes, it is referred to as Pierre Robin sequence.
during ET tube placement.36 Pulling the tongue forward Although the jaw in the patient with Pierre Robin syn-
with padded forceps can aid in visualization of the vocal drome is hypoplastic, it is also retrognathic, meaning the
cords. The straight blade, such as the Wisconsin or Miller attachment location of the mandibular condyle to the skull
blade, has been recommended by many authors as being is in a more posterior position, further increasing the dif-
the ideal blade of choice in neonates and infants with ficulty of intubation.31
macroglossia.37,38 Micrognathia causes the proportionately large tongue
Cervical Spine Abnormalities. Cervical spine abnor- to be forced to a more posterior position in the oro-
malities fall into 2 categories: those that cause instability pharynx, making it difficult to obtain an adequate view
and those that limit mobility. Cervical spine instabil- of the vocal cords with direct laryngoscopy. Because of
ity is a hallmark finding in some of the more common this, the posterior portion of the tongue and glottis is
congenital malformations, with Down syndrome being more acutely angled. The GlideScope, Airtraq optical
the most widely known.22 Cervical spine instability also laryngoscope (Prodol Meditec), DCI video laryngoscope
can have an acute presentation, such as in patients with (Karl Storz), Truview PCD, and flexible fiberoptic bron-
injuries sustained from a motor vehicle accident or other choscope are well suited for attempting to intubate the
trauma. Patients with cervical instability are at risk of patient with a DA.42 Manual external tracheal manipula-
compression of the cervical spinal cord, especially due to tion is also helpful in decreasing the angle of the base of
manipulation of the cervical vertebrae during laryngos- the tongue and glottis, aiding in the visualization of the
copy.28 Depending on the severity of the malformation vocal cords. The proportionately large tongue is also a
or trauma, preoperative lateral flexion and extension hindrance during direct laryngoscopy because there is no
images of the cervical spine may be beneficial.28 In-line room to sweep the tongue when attempting to align the
stabilization (not traction) is of utmost importance, and axes of the head and neck.
the neck and head should remain in as neutral a position Maxillary/Midfacial Hypoplasia. Maxillary hypo-
as possible throughout the entire procedure.28 plasia, which is a primary component of midfacial
The fiberoptic bronchoscope, Bullard laryngoscope, hypoplasia, is seen with several congenital malforma-
bougie, and light wand, may be useful in patients with tions (see the Table), and intubating conditions may be
limited or unstable cervical vertebrae since these devices similar to those with micrognathia. Midfacial hypoplasia
do not require the neck to be mobilized during at- typically consists of a hypoplastic nasal bone, maxilla,
tempted visualization of airway structures.39 The Bullard and zygomas. One common problem encountered with
laryngoscope has been shown in one prospective study midfacial hypoplasia is OSA.25 The underdeveloped facial
involving 18 fresh cadavers intubated by one anesthe- bones force the tongue to a more posterior position,
siologist, to provide the best view of the vocal cords with making airway obstruction a common problem. Airway
the least amount of cervical manipulation compared with management modalities are similar to those used for mi-
the GlideScope (Verathon) video laryngoscope, and the crognathia.25,36
Viewmax (Rusch) or Macintosh laryngoscope blades.39 Cleft Palate. One anatomical malformation that may
The GlideScope also has been shown to improve the laryn- complicate the management of the pediatric airway is the
goscopic view in the pediatric patient with a DA.40 In con- cleft palate. The incidence of cleft palate, with or without
trast, in normal pediatric airways, one prospective random- cleft lip, is reported to be between 9.1 and 15.6 cases
ized study involving 134 patients (birth to age 10 years) per 10,000 live births worldwide, which makes it one of
found the GlideScope and Truview PCD (Truphatek) video the most common birth defects.43 Epidemiologic studies
laryngoscopes were inferior to direct laryngoscopy.41 In have shown that clefts are an isolated malformation in
patients not at risk of aspiration, a laryngeal mask airway 71% of occurrences, and 29% to 33% of cases are as-
(LMA) is an excellent choice for airway management. It is sociated with a syndrome, chromosomal abnormality, or
also recognized as being a rescue airway device for failed in- multiple congenital anomalies of unknown etiology.43,44
tubations. Contraindications to the use of an LMA include Patients with Pierre Robin syndrome have a 50% to 80%
a full stomach, recent trauma, and the need for high (> chance of presenting with cleft palate. Male occurrence is
20-25 cm H2O) positive pressure ventilation. also greater, with an odds ratio of 1.7.43,44
38 AANA Journal February 2015 Vol. 83, No. 1 www.aana.com/aanajournalonline
During assessment of a patient with a cleft palate, there risks associated with an emergent intubation.
are several other closely related maladies that should be For many of the acute airway alterations listed above,
considered. Up to 29% of patients presenting with cleft inflammation of some part of the airway is a large contrib-
palate (with or without cleft lip) will have some form of uting factor to the problem. One method of minimizing
CHD, such as patent foramen ovale, patent ductus arterio- this inflammation is with oral or intravenous (IV) dexa-
sus, or coarctation of aorta.43-45 Depending on the severity methasone (0.2-0.5 mg/kg orally or IV). Dexamethasone
of the cleft palate, a complete airway obstruction may occur is also useful in reducing inflammation from surgery and
if the tongue enters the cleft, effectively occluding both airway manipulation during direct laryngoscopy. Airway
the oral and nasal cavities simultaneously.46 Although the management methods of acute presentations are similar
general pediatric population has OSA at an occurrence of to those used to treat congenital ones, as described previ-
2% to 3%, patients with cleft palate experience OSA at a ously and in the following section.
significantly higher rate (31%),19 and patients with Down
syndrome are at an even greater risk of OSA (45%).25 Considerations for Management of the
Airway management of patients with an isolated cleft Difficult Airway
palate (ie, cleft palate with no cleft lip) is usually accom- There are several recommendations the authors would
plished with minimal difficulty.41,47 One retrospective like to make that may assist anesthesia providers in man-
study involving infants and toddlers (1 month to 3 years aging the difficult pediatric airway. For example, during
of age) reported 4.77% of cases being classified as a dif- transport of patients with obstructive abnormalities to
ficult laryngoscopy and 1.93% as a difficult intubation.47 the OR, the prone position may help to prevent airway
In that study, 985 subjects were scheduled for repair obstruction.36 This would include patients with macro-
of cleft lip and palate. The researchers also found that glossia, acute airway masses, or epiglottitis.37,42,46 Once
the incidence of difficult laryngoscopy in infants (1-6 the patient is in the OR, preoxygenation should begin
months of age) with cleft lip/palate was 7.06%. as soon as possible. An awake flexible fiberoptic intuba-
For patients with bilateral cleft palates, the premax- tion can be highly effective in securing a documented
illa (the most anterior portion of the maxilla) is angled and compromised DA. This may be accomplished with
forward, causing the upper incisors to hamper blade prudent administration of sedation (midazolam, 0.3-0.5
movement and obstruct the line of sight during direct mg/kg orally or per rectal, or ketamine, 1-2 mg/kg in-
laryngoscopy. During a direct laryngoscopy in a patient tramuscularly [IM] or IV), antisialagogues (atropine,
with a unilateral left or bilateral cleft palate, the laryngo- 0.02 mg/kg IM, or glycopyrrolate, 0.01 mg/kg IM), and
scope blade tends to drop into the left cleft palate, further subsequent local anesthesia of the airway (lidocaine,
obstructing the view.47 This can be remedied by gently maximum of 4 mg/kg), administered either by aerosoliza-
packing the cleft palate with gauze before intubation or tion or local injection. Maintenance of adequate sponta-
by using a plastic tooth guard to span the cleft.8 An oral neous ventilation and effectively maintenance of normal
airway placed immediately after induction typically pre- airway tone are essential components of this technique.
vents the tongue from obstructing the oropharyngeal and The use of IV medications at times may also be a
nasal cavities, allowing for easy mask ventilation.8 desired method of induction, although preserving spon-
taneous respirations may be difficult without judicious
The Acutely Altered Airway titration. Propofol can be an ideal drug for this technique
There are numerous conditions that may cause the pedi- because of its short time of onset and duration of action.
atric airway to become acutely difficult to secure. Some One caveat to an IV induction is that a peripheral IV
examples include acute epiglottitis, hemangiomas, papil- catheter is needed, which may be difficult to obtain in an
lomatosis, venous lymphatic malformations, burns, la- uncooperative child. It is important to note that airway
ryngoceles, angioedema, or arteriovenous malformations; obstruction may occur with all forms of induction, and
fortunately, most of these are rare. methods of achieving effective ventilation, such as with
One potential alteration with an infectious etiology is oral and nasal airways, LMAs, and jet ventilation, should
acute epiglottitis. In 1989, acute epiglottitis had an oc- be readily available.
currence of 15 cases per 100,000 live births, but after the Following induction of general anesthesia for a surgi-
development and subsequent mass administration of the cal procedure requiring a protected airway, the anesthe-
Haemophilus influenzae type B vaccination in 1990, the tist may at his or her discretion intubate with or without
rate dropped 73% to 4 cases per 100,000 live births.48 paralytics. Any concerns for substantial airway inflam-
Epiglottitis occurs rapidly within 24 hours, is supraglot- mation due to a difficult intubation should be managed
tic, and typically affects 2- to 7-year-olds, although it may before extubation.36 Extubation criteria for a child who
occur in adults. Elective early intubation in the operating had a difficult intubation should include full reversal of
room (OR) is recommended for every patient presenting paralytics, evidence of an adequate spontaneous minute
with confirmed acute epiglottitis, effectively avoiding the volume, and being completely awake. If the patients
www.aana.com/aanajournalonline AANA Journal February 2015 Vol. 83, No. 1 39
postoperative pain is predicted to require the use of 8. Dickison AE. The normal and abnormal pediatric upper airway:
recognition and management of obstruction. Clin Chest Med.
high-dose narcotics, a prolonged intubation should be 1987;8(4):583-596.
considered because of the respiratory depressant effects 9. Hudgins PA, Siegel J, Jacobs I, Abramowsky CR. The normal pediatric
of opioids. After the patient has been extubated and larynx on CT and MR. Am J Neuroradiol. 1997;18(2):239-245.
transferred to the postanesthesia care unit, all healthcare 10. Rasche RF, Kuhns LR. Histopathologic changes in airway mucosa of
infants after endotracheal intubation. Pediatrics. 1972;50(4):733-738.
providers and parents should be informed of any difficul-
11. Keens TG, Bryan AC, Levison H, Ianuzzo CD. Developmental pattern
ties with perioperative airway management. of muscle fiber types in human ventilatory muscles. J Appl Physiol
Respir Environ Exer Physiol. 1978;44(6):909-913.
Conclusion 12. Regli A, Habre W, Saudan S, Mamie C, Erb TO, von Ungern-Sternberg
BS; Swiss Paediatric Respiratory Research Group. Impact of Trendelen-
Although many pediatric patients commonly present burg positioning on functional residual capacity and ventilation homo-
with an unremarkable airway, it is prudent for the anes- geneity in anaesthetised children. Anaesthesia. 2007;62(5):451-455.
thetist to be vigilant for the occult challenging airway. 13. Lumb AB, Nunn JF. Respiratory function and ribcage contribution
Being cognizant of clinical markers and diagnoses that to ventilation in body positions commonly used during anesthesia.
Anesth Analg. 1991;73(4):422-426.
are associated with difficulties in securing an airway is
14. Hislop AA, Wigglesworth JA, Desai R. Alveolar development in the
of value. This would include having a cardinal under- human fetus and infant. Early Hum Dev. 1986;13(1):1-11.
standing of the anatomical and physiologic differences 15. Keenan RL, Shapiro JH, Kane FR, Simpson PM. Bradycardia during
between a pediatric and adult patients airway. anesthesia in infants: an epidemiologic study. Anesthesiology. 1994;80
(5):976-982.
Furthermore, a working knowledge of how the airway
16. Lee A, Fan LT, Gin T, Karmakar MK, Ngan WD. A systematic review
of neonates, infants, toddlers, children, and adolescents (meta-analysis) of the accuracy of the Mallampati tests to predict the
may become altered because of congenital or acquired difficult airway. Anesth Analg. 2006;102(6):1867-1878.
malformations will allow the anesthetist to establish a 17. Santos AP, Mathias LA, Gozzani JL, Watanabe M. Difficult intubation
patent airway before or during induction of anesthesia. in children: applicability of the Mallampati index. Revi Bras Anestesiol.
2011;61(2):156-162.
For example, children born with Down syndrome are 18. Adewale L. Anatomy and assessment of the pediatric airway. Paediatr
known to have anatomical abnormalities such as macro- Anaesth. 2009;19(suppl 1):1-8.
glossia, cervical instability, and mandibular and/or maxil- 19. Maclean JE, Waters K, Fitzsimons D, Hayward P, Fitzgerald DA.
lary hypoplasia. Screening for obstructive sleep apnea in preschool children with cleft
palate. Cleft Palate Craniofac J. 2009;46(2):117-123.
Because of the existence of many diverse congenital 20. Shin M, Besser LM, Kucik JE, Lu C, Siffel C, Correa A; Congenital
and acquired malformations that can afflict pediatric Anomaly Multistate Prevalence and Survival Collaborative. Prevalence
patients, it is difficult to establish recommendations for of Down syndrome among children and adolescents in 10 regions of
the United States. Pediatrics. 2009;124(6):1565-1571.
airway management that would be universally applicable
21. Fink GB, Madaus WK, Walker GF. A quantitative study of the face in
to each abnormality. Thus, the authors intent with this Downs syndrome. Am J Orthod. 1975;67(5):540-553.
review was to compile the more prevalent syndromes that 22. Semine AA, Ertel AN, Goldberg MJ, Bull MJ. Cervical-spine instability
anesthetists may encounter and their common clinical in children with Down syndrome (trisomy 21). J Bone Joint Surg Am.
features that can impose problems with ventilation, in ad- 1978;60(5):649-652.
23. Pueschel SM, Scola FH. Atlantoaxial instability in individuals with
dition to describing airway management techniques and Down syndrome: epidemiologic, radiographic, and clinical studies.
strategies that may minimize airway mishaps. Pediatrics. 1987;80(4):555-560.
24. Frostad WA, Cleall JF, Melosky LC. Craniofacial complex in the trisomy
REFERENCES 21 syndrome (Downs syndrome). Arch Oral Biol. 1971;16(7):707-722.
1. Morray JP, Geiduschek JM, Caplan RA, Posner KL, Gild WM, Cheney 25. Marcus CL, Keens TG, Bautista DB, von Pechmann WS, Ward SL.
FW. A comparison of pediatric and adult anesthesia closed malprac- Obstructive sleep apnea in children with Down syndrome. Pediatrics.
tice claims. Anesthesiology. 1993;78(3):461-467. 1991;88(1):132-139.
2. Jimenez N, Posner KL, Cheney FW, Caplan RA, Lee LA, Domino KB. 26. National Institute of Neurological Disorders and Stroke. Mucopoly-
An update on pediatric anesthesia liability: a closed claims analysis. saccharidoses [fact sheet]. April 29, 2013. Updated April 16, 2014.
Anesth Analg. 2007;104(1):147-53. http://www.ninds.nih.gov/disorders/mucopolysaccharidoses/muco
3. Heinrich S, Birkholz T, Ihmsen H, Irouschek A, Ackermann A, Schmidt polysaccharidoses.htm. Accessed December 2, 2014.
J. Incidence and predictors of difficult laryngoscopy in 11,219 pediat- 27. Frawley G, Fuenzalida D, Donath S, Yaplito-Lee J, Peters H. A retro-
ric anesthesia procedures. Paediatr Anaesth. 2012;22(8):729-736. spective audit of anesthetic techniques and complications in children
4. Krauss BS, Harakal T, Fleisher GR. The spectrum and frequency of with mucopolysaccharidoses. Paediatr Anaesth. 2012;22(8):737-744.
pediatric illnesses presenting to a pediatric emergency department. 28. Muenzer J, Wraith JE, Clarke LA; International Consensus Panel on
Pediatr Emerg Care. 1991;7(2):67-71. Management and Treatment of Mucopolysaccharidosis I. Mucopoly-
5. Luten C, Kissoon N. Approach to the pediatric airway. In: Walls RM, saccharidosis I: management and treatment guidelines. Pediatrics.
ed. Manual of Emergency Airway Management. 2nd ed. Philadelphia, 2009;123(1):19-29.
PA: Lippincott Williams & Wilkins; 2004. 29. Bush PG, Williams AJ. Incidence of the Robin anomalad (Pierre Robin
6. Vialet R, Nau A, Chaumotre K, Martin C. Effects of head posture syndrome). Br J Plast Surg. 1983;36(4):434-437.
on the oral, pharyngeal and laryngeal axis alignment in infants and 30. Evans AK, Rahbar R, Rogers GF, Mulliken JB, Volk MS. Robin
young children by magnetic resonance imaging. Pediatr Anaesth. sequence: a retrospective review of 115 patients. Int J Pediatr Otorhi-
2008;18(6):525-531. nolaryngol. 2006;70(6):973-980.
7. Westhorpe RN. The position of the larynx in children and its relationship 31. Arteau-Gauthier I, Leclerc JE, Godbout A. Can we predict a difficult
to the ease of intubation. Anaesth Intensive Care. 1987;15(4):384-388. intubation in cleft lip/palate patients? J Otolaryngol Head Neck Surg.
40 AANA Journal February 2015 Vol. 83, No. 1 www.aana.com/aanajournalonline
2011;40(5):413-419. devices for indirect laryngoscopy in children younger than two years
32. Rovin S, Dachi SF, Borenstein DB, Cotter WB. Mandibulofacial dysostosis, of age. Paediatr Anaesth. 2011;21(2):98-103.
a familial study of five generations. J Pediatr. 1964 Aug;65:215-221. 43. Calzolari E, Pierini A, Astolfi G, Bianchi F, Neville AJ, Rivieri F. Asso-
33. Mehrotra D, Hasan M, Pandey R, Kumar S. Clinical spectrum of ciated anomalies in multi-malformed infants with cleft lip and palate:
Treacher Collins syndrome. J Oral Biol Craniofac Res. 2011;1(1):36-40. an epidemiologic study of nearly 6 million births in 23 EUROCAT
34. Sinkueakunkit A, Chowchuen B, Sriraj W, et al. Outcome of anes- registries. Am J Med Genet A. 2007;143A(6):528-537.
thetic management for children with craniofacial deformities. Pediatr 44. Milerad J, Larson O, Hagberg C, Ideberg M. Associated malformations
Int. 2013;55(3):360-365. in infants with cleft lip and palate: a prospective, population-based
35. Walker RW, Darowski M, Morris P, Wraith JE. Anaesthesia and study. Pediatrics. 1997;100(2):180-186.
mucopolysaccharidoses: a review of airway problems in children. 45. Shah CV, Pruzansky S, Harris WS. Cardiac malformations with facial
Anaesthesia. 1994;49(12):1078-1084. clefts; with observations on the Pierre Robin syndrome. Am J Dis
36. Infosino A. Pediatric upper airway and congenital anomalies. Anesthe- Child. 1970;119(3):238-244.
siol Clin North Am. 2002;20(4):747-766. 46 Sher AE. Mechanisms of airway obstruction in Robin sequence: impli-
37. McNiece WL, Dierdorf SF. The pediatric airway. Semin Pediatr Surg. cations for treatment. Cleft Palate Craniofac J. 1992;29(3):224-231.
2004;13(3):152-165. 47. Xue FS, Zhang GH, Li P, et al. The clinical observation of difficult
38. Walker R. Management of the difficult airway in children. J Roy Soc laryngoscopy and difficult intubation in infants with cleft lip and pal-
Med. 2001;94(40)(suppl;):341-344. ate. Paediatr Anaesth. 2006;16(3):283-289.
39. Zamora JE, Nolan RL, Sharan S, Day AG. Evaluation of the Bullard, 48. Adams WG, Deaver KA, Cochi SL, et al. Decline of childhood Hae-
GlideScope, Viewmax, and Macintosh laryngoscopes using a cadaver mophilus influenzae type b (Hib) disease in the Hib vaccine era.
model to simulate the difficult airway. J Clin Anesth. 2011;23(1):27-34. JAMA. 1993;269(2):221-226.
40. Lee JH, Park YH, Byon HJ, et al. A comparative trial of the GlideScope
video laryngoscope and direct laryngoscope in children with difficult AUTHORS
direct laryngoscopy and an evaluation of the effect of blade size. Joshua Belanger, CRNA, is a staff nurse anesthetist at Park Ridge Health,
Anesth Analg. 2013;117(1):176-181. Hendersonville, North Carolina. Email: belanger.josh@gmail.com.
41. Riveros R, Sung W, Sessler DI, et al. Comparison of the Truview PCD and Mark Kossick, CRNA, DNSc, is a tenured professor and graduate anes-
the GlideScope video laryngoscopes with direct laryngoscopy in pediatric thesia simulation education coordinator at Western Carolina Universitys
patients: a randomized trial. Can J Anaesth. 2013;60(5):450-457. Graduate Program of Nurse Anesthesia, Asheville, North Carolina. Email:
42. Holm-Knudsen R. The difficult pediatric airwaya review of new makossick@wcu.edu.
www.aana.com/aanajournalonline AANA Journal February 2015 Vol. 83, No. 1 41
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Collective Nouns (TES)Dokument34 SeitenCollective Nouns (TES)Micah PraiseNoch keine Bewertungen
- Facts About Owls: Horned Owl (Bubo Virginianus, Fig. 1) Is The Most Widely Distributed Owl inDokument6 SeitenFacts About Owls: Horned Owl (Bubo Virginianus, Fig. 1) Is The Most Widely Distributed Owl insprite2lNoch keine Bewertungen
- Rhymes For Class I IIDokument19 SeitenRhymes For Class I IIBala MuruganNoch keine Bewertungen
- 2013 BCF Stallion Auction CatalogDokument31 Seiten2013 BCF Stallion Auction Catalogapi-85716849Noch keine Bewertungen
- EarthAndLifeScience (SHS) Q2 Mod23 PerpetuationOfLife V1Dokument23 SeitenEarthAndLifeScience (SHS) Q2 Mod23 PerpetuationOfLife V1Roseman TumaliuanNoch keine Bewertungen
- WREB QuestionsDokument12 SeitenWREB QuestionsEvan BlackwellNoch keine Bewertungen
- Cells Are The Basic Unit of Life. The Cell Theory States ThatDokument4 SeitenCells Are The Basic Unit of Life. The Cell Theory States ThatMet XiiNoch keine Bewertungen
- Noun Worksheet For Class 4 With Answers 1Dokument10 SeitenNoun Worksheet For Class 4 With Answers 1Kamini jain100% (3)
- Traction and Orthopedic ApliancesDokument321 SeitenTraction and Orthopedic ApliancesAravinda Pravita Ichsantiarini100% (4)
- Foam Rolling Programme PDFDokument20 SeitenFoam Rolling Programme PDFGerardClarke100% (2)
- Guía 7 de Ingles Pasado SimpleDokument6 SeitenGuía 7 de Ingles Pasado SimpleDocentes Arkos Mosquera100% (2)
- MSH Regulated Sexual ConductsDokument3 SeitenMSH Regulated Sexual ConductsthekarlpazNoch keine Bewertungen
- Fleming Et Al. 2009 - The Evolution of Bat Pollination - A Phylogenetic PerspectiveDokument27 SeitenFleming Et Al. 2009 - The Evolution of Bat Pollination - A Phylogenetic PerspectiveMarcelo MorettoNoch keine Bewertungen
- The Gatekeepers of DuatDokument1 SeiteThe Gatekeepers of DuatMarcus LibertatesNoch keine Bewertungen
- D&D Fishing MinigameDokument2 SeitenD&D Fishing MinigameLucas MarquesNoch keine Bewertungen
- Asian Hornet (Vespa Velutina) Response PlanDokument11 SeitenAsian Hornet (Vespa Velutina) Response PlanPeter Anthony MartinsNoch keine Bewertungen
- Plants and Animals of The Book of MormonDokument42 SeitenPlants and Animals of The Book of MormonMosiah221100% (3)
- The Buffoon and The Countryman: Desree Gale R. de Guzman X-ZaraDokument3 SeitenThe Buffoon and The Countryman: Desree Gale R. de Guzman X-ZaraDesree GaleNoch keine Bewertungen
- Best Dog Grooming Near Me 0121Dokument3 SeitenBest Dog Grooming Near Me 0121Arch. ZionNoch keine Bewertungen
- LC4082Dokument3 SeitenLC4082Rene NyilNoch keine Bewertungen
- Tiger 3 FlashcardsDokument191 SeitenTiger 3 FlashcardsEdyta SałekNoch keine Bewertungen
- Keys For Pet Exam PackDokument34 SeitenKeys For Pet Exam PackEleftheria AggeleaNoch keine Bewertungen
- Fritz NotesDokument4 SeitenFritz NotesSnehasish Bar50% (2)
- Pathophysiology Exam 4 - ReviewDokument18 SeitenPathophysiology Exam 4 - ReviewWaqas GillNoch keine Bewertungen
- Olivia The Big GiraffeDokument13 SeitenOlivia The Big GiraffeGraciela Acuña100% (4)
- Animal Instinct 990 Passage and QuestionsDokument4 SeitenAnimal Instinct 990 Passage and QuestionsCosta Sam0% (1)
- GA HuntingDokument72 SeitenGA HuntingEnrique HernandezNoch keine Bewertungen
- Frequently Asked Questions: Why Are These Companies Included On The "Do Test" List?Dokument15 SeitenFrequently Asked Questions: Why Are These Companies Included On The "Do Test" List?XnateriverXNoch keine Bewertungen
- Nov 25, Pennywise - Castlegar, Slocan ValleyDokument48 SeitenNov 25, Pennywise - Castlegar, Slocan ValleyPennywise PublishingNoch keine Bewertungen
- Atlas of Obstetrics and GynaecologyDokument426 SeitenAtlas of Obstetrics and GynaecologyBooksToLearn88% (8)