Beruflich Dokumente
Kultur Dokumente
17
Hochgeladen von
HendroMaleCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
17
Hochgeladen von
HendroMaleCopyright:
Verfügbare Formate
254 Anterior MI and AV BlockKay Woon Ho et al
Case Series
Complete Atrioventricular Block Complicating Acute Anterior Myocardial
Infarction can be Reversed with Acute Coronary Angioplasty
Kay Woon Ho,1MBBS, MRCP, MMed, Tian Hai Koh,1MBBS, M Med (Int Med), Philip Wong,2FRCP, FACC, FAMS, Sung Lung Wong,1MBBS, MRCP,
Yen Teak Lim,1MB ChB (Glas), MRCP (UK), FAMS, Soo Teik Lim,1MBBS, MRCP (UK), FAMS, Li Fern Hsu,1MBBS, MRCP (UK), FAMS
Abstract
Introduction: A retrospective case series of acute anterior myocardial infarction (MI) pa-
tients complicated by complete atrioventricular block (AVB) treated with acute percutaneous
transluminal coronary angioplasty (PTCA). Clinical Picture: Eight patients with anterior MI
and complete AVB underwent acute PTCA between 2000 and 2005. Mean onset of complete
AVB was 16.6 16.9 hours from chest pain onset. Treatment: All patients underwent successful
PTCA to the left anterior descending artery. Outcome: Complete AVB resolved with PTCA in
88%; mean time of resolution was 89 144 minutes after revascularisation. One patient had
permanent pacemaker implanted at Day 12 after developing an 8-second ventricular standstill
during hospitalisation but not pacing-dependent on follow-up. The rhythm on discharge for
the other surviving patients was normal sinus rhythm. Conclusion: This case series suggests
that complete AVB complicating anterior MI is reversible with acute PTCA and survivors are
not at increased risk of recurrent AVB. Nevertheless, this condition is associated with extensive
myocardial damage and high mortality during the acute hospitalisation was not improved with
correction of AVB with temporary pacing.
Ann Acad Med Singapore 2010;39:254-7
Key words: Acute percutaneous transluminal coronary angioplasty
Introduction Only patients with anterior MI and complete AVB were
Complete atrioventricular block (AVB) develops in included, an example of which is shown in Figure 1. The
more than 5% of patients with myocardial infarction diagnoses of anterior MI and complete AVB were made using
(MI).1-7 These patients have poorer outcomes compared standard clinical definitions. Complete AVB was defined as
to those without complete AVB.1-4 Thrombolysis has been complete interruption of AV conduction with dissociation
demonstrated to improve the prognosis of such patients, of P waves and QRS complexes as well as existence of
especially those with inferior MI.1-3,6-9 Patients with anterior junctional or ventricular escape rhythm with a rate slower
MI, however, remained at high risk of mortality and most than the atrial rate. Complete AVB was considered present
required pacemaker implantation.3 With the increasingly if it occurred during the index hospitalisation. Anterior MI
widespread availability of acute percutaneous transluminal was defined as acute onset of chest pain associated with
coronary angioplasty (PTCA) for MI, the prognosis of these presence of new or presumably new ST-elevation >0.2
high-risk patients would be expected to improve, although mV in 2 or more contiguous anterior ECG leads (V1-V4)
limited data have been available to date. We report on a associated with elevated cardiac enzymes within 24 hours
retrospective case series of 8 patients with acute anterior of the onset of ischaemic discomfort.
MI complicated by complete AVB who were treated with The clinical details for the patients were obtained from
acute PTCA. our acute MI database and the index hospitalisation records,
while follow-up and mortality information were obtained
Case Series through outpatient and hospitalisation records. The study
The records of all patients with MI treated with acute was approved by the institutional review board. The
PTCA at our centre between 2000 and 2005 were examined. patients are presented as a case series with their pertinent
1
Department of Cardiology, National Heart Centre Singapore
2
Department of Cardiology, National Heart Centre Singapore and Duke-NUS Graduate Medical School Singapore
Address for Correspondence: Dr Hsu Li Fern, National Heart Centre, Mistri Wing, 17 Third Hospital Avenue, Singapore 168752.
Email: hsulifern@novenaheartcentre.com.sg
Annals Academy of Medicine
Anterior MI and AV BlockKay Woon Ho et al 255
Fig. 1. ECG of anterior AMI
complicated by CAVB.
Table 1. Baseline Characteristics of Patients Admitted for Anterior AMI Complicated by CAVB
Patient Age Sex Risk factor Prior IHD Prior CCF
no. (y) Smoking DM HTN HLD FHX
1 71 F N Y Y Y Y N N
2 69 M Y N N Y N N N
3 62 F N N Y Y N N N
4 44 M Y N Y Y N Y N
5 67 M Y N Y N N N N
6 51 M N Y N Y N N N
7 65 M Y Y Y Y N N N
8 69 M Y N N Y N N N
AMI: acute myocardial infarction; CAVB: complete atrioventricular block; CCF: congestive
heart failure; DM: diabetes mellitus; FHX: family history of ischemic heart disease; HLD:
hyperlipidaemia; HTN: hypertension; IHD: ischaemic heart disease
details tabulated for reference and comparison. Continuous alternating LBBB/RBBB in 1. Mean onset of complete AVB
variables are presented as means ( standard deviation) was 16.6 16.9 hours from chest pain onset. Peak cardiac
while categorical variables are presented as frequencies enzyme measurements were: creatine kinase (CK) 4375
and percentages. 2667 U/L, CKMB 459 303 U/L, troponin-T 16.1 5.0
g/L. Echocardiography showed a mean left ventricular
Results ejection fraction (LVEF) of 31% 10%.
Eight patients with anterior AMI and complete AVB Mean door-to-balloon time was 239 220 minutes.
who underwent acute PTCA were found. Their baseline Angiography showed triple vessel disease in 3 (38%),
characteristics are shown in Table 1. Almost all patients double vessel disease in 1 (12%) and single vessel disease
were male, with a mean age of 62.3 9.7 years. All had in 4 (50%). The infarct-related artery was the left anterior
more than 1 standard risk factor, but only 1 patient had descending artery (LAD) in all cases, with the occlusion
documented pre-existing coronary artery disease prior to at the proximal portion in 7 of the 8 patients. All patients
the MI. underwent successful acute PTCA to LAD.
The clinical characteristics of the patients at presentation Seven patients required temporary transvenous pacing
are shown in Table 2. The patients were highly unstable, as due to haemodynamic instability. The complete AVB was
indicated by their high Killip classification (mean 3.0 1.4) transient in 7 (88%), resolving with acute PTCA. Mean time
and the presence of cardiogenic shock at presentation or of resolution was 89 144 minutes after revascularisation.
during hospitalisation in 50%. Three patients had complete The last patient was listed for implantation of a permanent
AVB at presentation and the rest developed it shortly after pacemaker (PPM) after developing an 8-second ventricular
hospitalisation. The initial electrocardiogram (ECG) of the standstill during hospitalisation. The PPM was inserted
5 patients with delayed onset of AVB showed left bundle on Day 12 of admission. Subsequently, his complete AVB
branch block (LBBB) in 2 patients, right bundle branch resolved on Day 18, and his discharge rhythm was first
block (RBBB)/left anterior fascicular block (LAFB) in 2, degree AVB. During follow-up, the patient was not pacing-
March 2010, Vol. 39 No. 3
256 Anterior MI and AV BlockKay Woon Ho et al
Table 2. Clinical Data of Patients Admitted for Anterior AMI Complicated by CAVB
Patient Killip class Cardiogenic Onset of Bundle LVEF TPW Time to Peak Peak Peak Death
no. on admission shock CAVB branch (%) insertion CAVB CK CKMB troponin during
during from chest block on resolution (U/L) (U/L) T hospital-
hospitalisation pain (h) ECG from (g/L) isation
PTCA (h)
1 3 N 13 Left BBB 30 Y 48 1037 94 7.43 Y
2 4 Y 24 Right BBB/ 20 Y 24 7356 843 22.37 Y
LAFB
3 1 N 48 Right BBB/ 35 Y 432 6385 626 17.35 N
Left BBB
4 1 N 0 No BBB 22 Y 6 446 51 16.12 N
5 4 Y 24 Left BBB 35 Y 96 3260 317 11.10 N
6 1 N 0 No BBB 50 N 7 4375 459 16.24 N
7 4 Y 0 Left BBB 35 Y 0 4787 443 16.00 Y
8 2 Y 48 Right BBB/ 20 Y 96 7356 843 22.37 Y
LAFB
AMI: acute myocardial infarction; BBB: bundle branch block; CAVB: complete atrioventricular block; CK: creatinine kinase; LAFB: left anterior fascicular
block; LVEF: left ventricular ejection fraction; PTCA: percutaneous transluminal coronary angioplasty; TPW: temporary pacing wire
dependent. The rhythm on discharge for the other surviving of LV function. However, information regarding acute
patients was normal sinus rhythm. revascularisation and outcome in this group of patients is
Four patients died during the index hospitalisation (50% very limited, possibly due to the small numbers of such
mortality). The cause of death was myocardial pump failure/ patients compared to those in the setting of inferior MI.
cardiogenic shock. Death occurred in 1/3 (33%) patients with To date, published information regarding PTCA in anterior
AVB at presentation and 3/5 (60%) patients who developed MI and complete AVB has been confined to case reports.9
AVB later during hospitalisation. During follow-up of 22.4 Acute mortality in our series of patients was high despite
8.7 months, there was only 1 readmission for congestive temporary transvenous pacing, with cardiogenic shock being
cardiac failure. No death, acute coronary syndrome or other the main cause of mortality. The lack of mortality reduction
events were observed among the other surviving patients. with temporary pacing in patients with anterior AMI and
complete AVB has also been reported in other studies.10,11
Discussion This finding suggests that the high mortality is related to
Large community-based studies have demonstrated a the extensive myocardial injury and myocardial pump
reduced incidence of complete AVB complicating acute failure rather than the deleterious effects of complete AVB.
MI in the thrombolytic era compared to pre-thrombolysis, The resolution of complete AVB after acute PTCA in
suggesting the beneficial role of reperfusion on prevention our patients suggests that the conduction block could
and resolution of complete AVB in acute MI.3,4 However, be attributable to ischaemia rather than necrosis of the
the development of complete AVB is still associated with intracardiac conduction system.9,12,13 Electrophysiological
a higher risk of short- and long-term mortality compared studies in patients who had suffered an anterior MI with
to patients without AVB.1-3,6 complete AVB have demonstrated no permanent AV
The distinction between inferior and anterior MI is conduction abnormalities in the majority of them, 4 to 40
important in the setting of complete AVB. AV conduction months after MI.14
abnormalities, including complete AVB, commonly Prophylactic PPM implantations in such patients have
complicate inferior MI. This is due to involvement of failed to reduce the subsequent risk of sudden cardiac
the blood supply to the AV node, as the AV nodal artery death.13 The cause of late sudden cardiac death relates
arises from the right coronary artery in most people. The to the occurrence of ventricular tachyarrhythmias rather
AVB in inferior MI usually resolves promptly with acute than the recurrence of AV block. In our case series, AVB
revascularisation in most cases, and PPM implantation is resolved completely in the surviving patients within 18 days
usually not required. In contrast, development of complete of MI. Therefore, the decision to implant a PPM should be
AVB in anterior MI suggests extensive myocardial damage.7 delayed in such patients who have undergone successful
This is reflected in our case series by a high Killip class revascularisation to allow time for complete resolution of
on admission, high incidence of cardiogenic shock, high the AVB. The decision regarding implantation of cardiac
peak cardiac enzyme levels, and marked impairment defibrillators (ICDs) to reduce sudden cardiac death should
Annals Academy of Medicine
Anterior MI and AV BlockKay Woon Ho et al 257
be taken on an individual basis. Survivors do well after block (the Worcester Heart Attack Study). Am J Cardiol 1992;69:1135-41.
discharge with no mortality documented during follow-up, 5. Dubois C, Pierard LA, Smeets JP, Foidart G, Legrand V, Kulbertus HE.
consistent with published data that such patients were not at Short- and long-term prognostic importance of complete bundle-branch
block complicating acute myocardial infarction. Clin Cardiol 1988;11:
increased risk of dying after discharge compared to similar 292-6.
patients with anterior AMI patients without.3 6. Harpaz D, Behar S, Gottlieb S, Boyko V, Kishon Y, Eldar M, for the
SPRINT Study Group and the Israeli Thrombolytic Survey Group.
Conclusion Complete atrioventricular block complicating acute myocardial infarction
Our case series suggests that complete AVB complicating in the thrombolytic era. J Am Coll Cardiol 1999;34:1721-8.
anterior MI is reversible with acute PTCA and survivors are 7. Archbold RA, Sayer JW, Ray S, Wilkinson P, Ranjadayalan K, Timmis
AD. Frequency and prognostic implications of conduction defects in acute
not at increased risk of recurrent AVB. Nevertheless, this myocardial infarction since the introduction of thrombolytic therapy. Eur
condition is associated with extensive myocardial damage Heart J 1998;19:893-8.
and high mortality during the acute hospitalisation which 8. Sgarbossa EB, Pinski SL, Topo, EJ, Califf RM, Barbagelata A, Goodman
was not significantly improved with correction of AVB SG, et al. Acute myocardial infarction and complete bundle branch
with temporary pacing. block at hospital admission: clinical characteristics and outcome in the
thrombolytic era. J Am Coll Cardiol 1998;31:105-10.
9. Wilber D, Walton J, ONeill W, Laufer N, Pitt B. Effects of reperfusion
on complete heart block complicating anterior myocardial infarction. J
Am Coll Cardiol 1984;4:1315-21.
REFERENCES 10. Ginks WR, Sutton R, Oh W, Leatham A. Long-term prognosis after acute
1. Spencer FA, Jabbour S, Lessard D, Yarzebski J, Ravid S, Zaleskas V, et al. anterior infarction with atrioventricular block. Br Heart J 1977;39:186-9.
Two-decade-long trends (1975-1997) in the incidence, hospitalization, and 11. Kuo CT, Liu CY, Lee YS. Immediate prognostic significance of complete
long-term death rates associated with complete heart block complicating atrioventricular block in acute myocardial infarction. Taiwan Yi Xue Hui
acute myocardial infarction: a community-wide perspective. Am Heart Za Zhi 1989;88:712-7.
J 2003;145:500-7. 12. Hackel DB, Sevilla MD, Mikat EM, Reimer KA, Ideker RE, Turi ZG.
2. Meine TJ, Al-Khatib SM, Alexander JH, Granger CB, White HD, Kilaru R, Comparison of patients with acute anterior or posterior myocardial
et al. Incidence, predictors, and outcomes of high-degree atrioventricular infarcts with and without complete heart block. Am J Cardiovasc Pathol
block complicating acute myocardial infarction treated with thrombolytic 1988;2:105-26.
therapy. Am Heart J 2005;149:670-4. 13. Grigg L, Kertes P, Hunt D, Goble A, Pitt A, Boxall J, Hale G. The role
3. Aplin M, Engstrom T, Vejlstrup NG, Clemmensen P, Torp-Pedersen of permanent pacing after anterior myocardial infarction complicated by
C, Kober L. Prognostic importance of complete atrioventricular block transient complete atrioventricular block. Aust N Z J Med 1988;18:685-8.
complicating acute myocardial infarction (TRACE Study Group). Am 14. Orlandi M, Raimondi W, Oddone A, Berra R, Tommasini G, Birolli
J Cardiol 2003;92:853-6. M, et al. Long term electrophysiological study on patients with acute
4. Goldberg RJ, Zevallos JC, Yarzebski J, Alpert JS, Gore JM, Chen Z, et al. myocardial infarction and complete heart block. Is cardiac pacing always
Prognosis of acute myocardial infarction complicated by complete heart necessary? G Ital Cardiol 1978;8Suppl 1:223-7.
March 2010, Vol. 39 No. 3
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- ATI Comprehensive & MentalDokument998 SeitenATI Comprehensive & MentalYolanda Stark96% (45)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- D-5450-1-B HS60G80GL SM EngDokument84 SeitenD-5450-1-B HS60G80GL SM EngRuslan Valiakhmetov100% (2)
- Business Plan MriDokument17 SeitenBusiness Plan Mriapi-298975236100% (1)
- Advanced EKG RefresherDokument181 SeitenAdvanced EKG RefresherIoana Antonesi100% (3)
- ECG Mastery Blue Belt Workbook PDFDokument135 SeitenECG Mastery Blue Belt Workbook PDFPadma Priya Duvvuri100% (5)
- FLASHCARD CardiovascularDokument40 SeitenFLASHCARD CardiovascularsnehaNoch keine Bewertungen
- J Oftalmologi Vol 7 No 2 (Gilbert WS Simanjuntak)Dokument5 SeitenJ Oftalmologi Vol 7 No 2 (Gilbert WS Simanjuntak)Riska AprilianaNoch keine Bewertungen
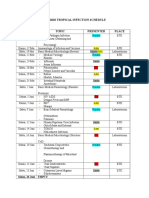
- Imo Tropical Infection ScheduleDokument3 SeitenImo Tropical Infection ScheduleHendroMaleNoch keine Bewertungen
- Imo Tropical Infection ScheduleDokument3 SeitenImo Tropical Infection ScheduleHendroMaleNoch keine Bewertungen
- Hand Foot Mouth - DiseaseDokument24 SeitenHand Foot Mouth - DiseaseHendroMaleNoch keine Bewertungen
- Hand Foot Mouth - DiseaseDokument24 SeitenHand Foot Mouth - DiseaseHendroMaleNoch keine Bewertungen
- Chemotherapy: Dr. Rajendra Nath ProfessorDokument135 SeitenChemotherapy: Dr. Rajendra Nath ProfessorHendroMaleNoch keine Bewertungen
- 2Dokument79 Seiten2HendroMaleNoch keine Bewertungen
- Imo Tropical Infection ScheduleDokument3 SeitenImo Tropical Infection ScheduleHendroMaleNoch keine Bewertungen
- VirologyDokument7 SeitenVirologySuman GangerNoch keine Bewertungen
- 16 The Predictors of Pacemaker Dependency of Post Myocardial Infarction Patients Who Have Heart BlockDokument1 Seite16 The Predictors of Pacemaker Dependency of Post Myocardial Infarction Patients Who Have Heart BlockHendroMaleNoch keine Bewertungen
- Bio Module-02Dokument40 SeitenBio Module-02XdxdNoch keine Bewertungen
- The Boys Fourth Book of Radio and Electronics MorganDokument120 SeitenThe Boys Fourth Book of Radio and Electronics MorganJames MarovichNoch keine Bewertungen
- C1-Human HeartDokument3 SeitenC1-Human HeartNursuzela Abd MalekNoch keine Bewertungen
- Share With The World: Defibrillator MonitorDokument4 SeitenShare With The World: Defibrillator MonitorJuan Esteban F.Noch keine Bewertungen
- Hardware Pace Using Slope DetectionDokument18 SeitenHardware Pace Using Slope DetectionGabriel GarcíaNoch keine Bewertungen
- 2023-Transfemoral Tricuspid Valve Replacement and One-Year Outcomes The TRISCEND StudyDokument12 Seiten2023-Transfemoral Tricuspid Valve Replacement and One-Year Outcomes The TRISCEND StudyNeison DuarteNoch keine Bewertungen
- TechPatient CARDIO V3 BrochureDokument4 SeitenTechPatient CARDIO V3 BrochureMaría Beatríz LNoch keine Bewertungen
- iKA Reocor S en 371305-D 2011-11-28 PDFDokument8 SeiteniKA Reocor S en 371305-D 2011-11-28 PDFAlexNoch keine Bewertungen
- Tabel Severitas BPJS Tindakan JantungDokument9 SeitenTabel Severitas BPJS Tindakan JantungTeduh ParamadinaNoch keine Bewertungen
- Venus Viva Operation Manual For IRB Rev.02 23.04.14Dokument52 SeitenVenus Viva Operation Manual For IRB Rev.02 23.04.14andres2013bioNoch keine Bewertungen
- Medtronic HBP Basics ELearnDokument77 SeitenMedtronic HBP Basics ELearnRichiNoch keine Bewertungen
- Day 3 - APPEC 2021Dokument413 SeitenDay 3 - APPEC 2021GaurieNoch keine Bewertungen
- Guia Seleccion Productos AffinityDokument4 SeitenGuia Seleccion Productos AffinityFrank MariniNoch keine Bewertungen
- ds2278 QSG en PDFDokument22 Seitends2278 QSG en PDFjose jimenezNoch keine Bewertungen
- Samsung Safety - InstructionsDokument16 SeitenSamsung Safety - InstructionsЮрий ОгаревNoch keine Bewertungen
- Implantable DefibrillatorDokument8 SeitenImplantable Defibrillatornikkitha parkerNoch keine Bewertungen
- Rate Control in Atrial Fi BrillationDokument11 SeitenRate Control in Atrial Fi BrillationNaty PradoNoch keine Bewertungen
- KKH Baby Bear Book 3rd EditionDokument672 SeitenKKH Baby Bear Book 3rd EditionJonathan TayNoch keine Bewertungen
- Anaesthetic Management of Emergency LSCS, An Unusual Case of Complete Heart Block With Permanent Pace MakerDokument2 SeitenAnaesthetic Management of Emergency LSCS, An Unusual Case of Complete Heart Block With Permanent Pace MakerIOSRjournalNoch keine Bewertungen
- SA Exit Block (Andrea Romandini)Dokument10 SeitenSA Exit Block (Andrea Romandini)Swempi Melchiadi AbollaNoch keine Bewertungen
- CRM Tendril Sts Pacing Lead CatalogDokument2 SeitenCRM Tendril Sts Pacing Lead CatalogsleonNoch keine Bewertungen
- 1 Florendo Vs Philam PlansDokument6 Seiten1 Florendo Vs Philam PlansRon GamboaNoch keine Bewertungen
- Practice ECGStripsDokument300 SeitenPractice ECGStripsrobby zayendraNoch keine Bewertungen
- Manual EN SG 40000 46000Dokument78 SeitenManual EN SG 40000 46000aleksandarNoch keine Bewertungen