Beruflich Dokumente
Kultur Dokumente
Gastric Outlet Obstruction
Hochgeladen von
Femmy RuthCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Gastric Outlet Obstruction
Hochgeladen von
Femmy RuthCopyright:
Verfügbare Formate
International Surgery Journal
Clement SH et al. Int Surg J. 2017 Jan;4(1):264-269
http://www.ijsurgery.com pISSN 2349-3305 | eISSN 2349-2902
DOI: http://dx.doi.org/10.18203/2349-2902.isj20164453
Original Research Article
A clinical study of gastric outlet obstruction
Suresh Clement H.1*, Ram Prasad Cherukumalli2, Ch. Ravinder Rao3
1
Associate Professor, Department of General Surgery, Prathima Institute of Medical Sciences, Karimnagar, Telangana,
India
2
Senior Resident, Department of General Surgery, Gandhi Medical College, Secunderabad, Telangana, India
3
Professor, Department of General Surgery, Prathima Institute of Medical Sciences, Karimnagar, Telangana, India
Received: 20 September 2016
Accepted: 20 October 2016
*Correspondence:
Dr. Suresh Clement H,
E-mail: dr.sureshclement@gmail.com
Copyright: the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under
the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial
use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
Background: From the standpoint of pathology, the term pyloric stenosis is usually inaccurate at least in adult
patients, since the site of obstruction is rarely situated at the pylorus itself but, is more often placed immediately
proximal to the spinchter where the diagnosis of carcinoma is most probable or more distally in the duodenal bulb
where the cause is almost invariably a duodenal ulcer. The aim was to study infantile hypertrophic pyloric stenosis,
benign peptic ulcer and gastric carcinoma and evaluation of electrolyte abnormalities in gastric outlet obstruction, to
study various modalities of treatment and to assess pertaining to recovery from paralytic ileus.
Methods: This was a clinical observational study comprising of 40 cases of gastric outlet obstruction. The patients for
this study have been selected from Prathima Institute of Medical Sciences, Karimnagar, Telangana, India from
December 2013- November 2015. The cases were selected who were willing to undergo surgery.
Results: Congenital hypertrophic pyloric stenosis (CHPS) is more common among first born male infants. Parental
consanguinity is associated with increased incidence of congenital hypertrophic pyloric stenosis. CHPS is common in
the age group of first 3-6 weeks of life (average 4 weeks). Males are more commonly affected with gastric outlet
obstructions in adults. Cicatrized duodenal ulcer is more common in the age group of 30-40 years, while carcinoma
stomach is more common in age group of 50-60 years. Vomiting and visible gastric peristalsis are the most common
and constant symptom and sign of gastric outlet obstruction, more so in cases of cicatrized duodenal ulcers.
Conclusions: Ramstedts pyloromyotomy is the gold standard treatment for CHPS. Patients with gastric outlet
obstruction due to cicatrized duodenal ulcer require truncal vagotomy with posterior gastrojejunostomy. Vagotomy is
optional in view of better response with drugs for APD. Antral carcinoma cases require curative or palliative surgery
depending on the stage of the disease.
Keywords: Gastric outlet obstruction, Paralytic ileus, Recovery
INTRODUCTION duodenal bulb where the cause is almost invariably a
duodenal ulcer.
From the standpoint of pathology, the term pyloric
stenosis is usually inaccurate at least in adult patients, This study has been taken up to review the changes in
since the site of obstruction is rarely situated at the presentation of gastric outlet obstruction in infants,
pylorus itself but, is more often placed immediately adults, clinical features and investigations used to
proximal to the sphincter where the diagnosis of diagnose and to discuss treatment and postoperative
carcinoma is most probable or more distally in the recovery. One of the following can be used to diagnose
gastric outlet obstruction.1
International Surgery Journal | January 2017 | Vol 4 | Issue 1 Page 264
Clement SH et al. Int Surg J. 2017 Jan;4(1):264-269
Projectile vomiting of undigested food consumed The cases were selected who were willing to undergo
several days previously with absence of bile in surgery with following inclusion and exclusion criteria.
vomitus.
Visible gastric peristalsis (VGP) on empty stomach Inclusion criteria
Gastric succession splash 3-4 hours after the last
meal. Peptic ulcer disease
Palpable hypertrophied stomach Carcinoma pyloric antrum
Delayed emptying of stomach on barium meal Infantile hypertrophic pyloric stenosis.
studies.
A gastric residue containing undigested food on Exclusion criteria
upper GI endoscopy
An aspirate of more than 400 ml on saline load test. Among pediatric age group
Demonstration at operation or autopsy of grossly
narrowed gastric outlet. Pyloric or prepyloric atresia, mucosal diaphragm
Duodenal atresia and stenosis
Aetiology varies in infants and adults. Common causes Foreign bodies, bezoars and worms.
being, congenital hypertrophic pyloric stenosis in infants
and chronic cicatrized duodenal ulcers and antral In adults
carcinoma in adults. Gastric outlet obstruction is
described by Sir James Walton as The stomach you can Hypertrophic pyloric stenosis of adults
hear, the stomach you can feel and the stomach you can Gastroduodenal tuberculosis
see.1 Cicatrised DU was the most common cause of Benign neoplasm of the stomach
gastric outlet obstruction but, due to wider usage of H 2 Carcinoma stomach with liver metastasis, ascites,
blockers and PPIs better health care facilities with new peritoneal implantation.
investigations in the armamentorium, its incidence is on
decline and is replaced by carcinoma stomach. An elaborate study of these cases with regard to the
Carcinoma stomach is detected early nowadays because history, clinical features, routine and special
of early investigatory interventions and in some countries investigations, pre-operative treatment, operative
as a part of screening programme. findings, post-operative management and complications
in post-operative period is done.
In managing gastric outlet obstruction, measures
employed are designed to In history, details were noted about presenting
Improve the local condition of stomach complaints, duration, history of acid peptic disease
Correct fluid and electrolyte imbalance features of metabolic disturbances, occupation and
Correct anemia, hypoproteinemia and vitamin personal history including diet, bowel and bladder habits,
deficiency smoking and alcoholism.
Treatment of etiological conditions by surgery
which is selected to suit individual patient, Thorough analysis of the findings of physical
depending upon age, general condition and examination was done which included hydration status,
associated condition as each surgery is deficient in VGP, mass, succussion splash, hepatomegaly and ascites.
some respect. Associated conditions like anemia, hypertension and
diabetes were managed appropriately before surgery.
In this study 40 cases have been selected to include
variety of cases of gastric outlet obstruction, both in Haemoglobin level, bleeding time, clotting time, routine
paediatric and adult age groups to study gastric outlet urine examination, chest screening, ECG, blood
obstruction cases with respect to infantile hypertrophic grouping, blood urea, serum creatinine, fasting and post-
pyloric stenosis, benign peptic ulcer and gastric prandial blood sugar were estimated as a part of general
carcinoma and evaluation of electrolyte abnormalities in work-up for surgery. Special investigations like serum
gastric outlet obstruction, to study various modalities of electrolytes, barium meal study, upper GI endoscopy and
treatment and to assess pertaining to recovery from ultrasonography of the abdomen and pelvis were done.
paralytic ileus.
Management of cases
METHODS
In infants, dehydration was primarily corrected by using
This was a clinical observational study comprising of 40 intravenous normal saline or half strength normal saline
cases of gastric outlet obstruction. The patients for this according to the body weight. Surgery was performed as
study have been selected from Prathima Institute of elective as emergency, after improving the infants
Medical Sciences, Karimnagar, Telangana, India from general condition. In adults pre-operative treatment
December 2013 - November 2015. included correction of dehydration, metabolic status,
anaemia, IV H2 blockers; liquid diet and antacids were
International Surgery Journal | January 2017 | Vol 4 | Issue 1 Page 265
Clement SH et al. Int Surg J. 2017 Jan;4(1):264-269
given along with twice a day stomach wash for a IV fluids were given according to the requirement
minimum of three days. According to the investigation that is depending upon body weight
reports and operative findings, definitive surgery was In infants oral feeds were started 24hrs after the
undertaken. surgery
Adults were kept nil orally for 4-5 days and oral sips
Anaesthesia were allowed after the removal of Ryles tube and
gradually shifted to solids from semi-solids
General anaesthesia was given for all cases.
Inj. Ciprofloxacin 200 mg bid was given in adults.
Surgeries performed In paediatric cases inj. Taxim was given according
to body weight
Infantile hypertrophic pyloric stenosis Analgesics: Inj. Paracetamol, 1gm mg, IV, bid
H2 blockers: Inj. Ranitidine, 50 mg, IV, bid
Ramstedts pyloromyotomy In paediatric cases subcuticular sutures were put. In
adults sutures were removed by 8-10 days after
Peptic ulcer disease operation
The follow-up period ranged from three months to
Truncal vagotomy (TV) with posterior six months.
gastrojejunostomy.
Gastric carcinoma RESULTS
Partial gastrectomy with Billroth II reconstruction. Or Table 1: Causes of gastric outlet obstruction.
anterior gastrojejunostomy alone
Causes Number Percentage
Infantile hypertrophic
Post-operative management 10 25
pyloric stenosis
Half hourly temperature, pulse and respiratory chart Cicatrised duodenal ulcer 21 52.5
for first six hours and fourth hourly chart thereafter Carcinoma pyloric antrum 09 22.5
Fourth hourly blood pressure chart Total 40 100
Ryles tube aspiration every hourly for first 24
hours. Then once in 2-4 hours Ryles tube was Cicatrized duodenal ulcer was the most common cause of
removed after appearance of bowel sounds and gastric outlet obstruction.
minimal Ryles tube output on aspiration
Table 2: Distribution according to symptoms.
Cicatrised duodenal ulcer Carcinoma antrum Total
Symptoms
Number Percentage Number Percentage Number Percentage
Pain 21 100 08 88.8 29 96.6
Vomiting 21 100 09 100 30 100
Anorexia 15 71.42 09 100 24 80
Weight loss 13 61.9 09 100 22 73.3
Hematemesis 04 19.04 05 55.5 09 30
Malena 11 52.38 04 44.44 15 50
Table 3: Distribution as per the signs
Duodenal ulcer Carcinoma pyloric regions Total
Signs
Number Percentage Number Percentage Number Percentage
Pallor 18 85.7 09 100 27 90
VGP 21 100 09 88.8 29 96.6
Succession splash 18 85.7 06 66.6 24 80
Palpable mass 08 88.8 03 26.6 11 36.6
Dehydration 15 71.42 06 66.6 21 70
International Surgery Journal | January 2017 | Vol 4 | Issue 1 Page 266
Clement SH et al. Int Surg J. 2017 Jan;4(1):264-269
In cases of carcinoma the pain was constant dull aching posterior gastro-jejunostomy. Five patients (55.5%) had
or gripping in nature used to get aggravated by food and operable disease underwent Billroth II resection and in 4
vomiting used to give relief from the pain. patients (44.4%) growth was fixed and they underwent
anterior gastro-jejunostomy alone.
The duration of pain was from 3 months to 6 months with
a median of 4 months. 17 cases gave history of APD and Table 4: Types of surgical procedures adopted in the
2 of them were malignant cases suggesting malignancy study.
developing from gastric ulcer.
Cases type Procedure Number Percentage
Pallor was present in 27 (90%) cases and more so in Truncal
carcinoma of pyloric region. VGP present in 29 (96.6%) vagotomy
Duodenal
cases, 8 of which were malignant. Succussion splash was with posterior 21 100
ulcer
present in 24 (80%) cases of which 6 were malignant gastro-
cases. jejunostomy
Carcinoma Billroth II
05 55.5
Palpable mass was present in 8 cases of carcinoma of antrum gastrectomy
pyloric region and nil in duodenal ulcer cases. Succussion Anterior
splash and VGP were less prominent in carcinoma cases. gastro- 04 44.4
21 patients (100%) underwent truncal vagotomy with jejunostomy
Table 5: Start of oral feeds.
5th day 6th day 7th day
Cases
Number Percentage Number Percentage Number Percentage
Cicatrised duodenal ulcer 09 42.8 09 42.8 03 14.28
Antral carcinoma 03 33.3 05 55.5 01 11.1
All the patients were kept nil orally and on Ryles tube which was treated by chest physiotherapy and review of
aspiration for duration varying from 4 to 7days. Oral sips antibiotics.
were allowed after removal of Ryles tube and
appearance of bowel sounds. One patient of carcinoma pyloric region died because of
anastomotic leak on 10th post-operative day. Rest of the
Table 6: Postoperative complications. patients had an uneventful postoperative period.
Postoperative hospitalization was in the range from 8 to
Postoperative 12 days with average of 10 days.
Number
complication
Wound infection 04 Follow up for a period of 3 months to 6 months was
Respiratory tract infection 03 done. Three patients of antral carcinoma were treated
Died 01 postoperatively by chemotherapy with 5-fluorouracil. 5
cases (23.95%) of cicatrized duodenal ulcer and 4 cases
Total 08
(44.4%) of carcinoma antrum were lost for follow up.
One patient with antral carcinoma developed multiple
Wound infection developed in four patients, who were
secondaries and expired one month after surgery on
treated by repeated dressing and appropriate antibiotics.
follow up.
In three patients, respiratory tract infection developed
Table 7: Duration of follow up.
Follow up
Cases Average duration Mortality
Number Percentage
Cicatrised duodenal ulcer 16 76.1 4 months 00
Antral carcinoma 05 55.5 2.6 months 01 (11.1%)
International Surgery Journal | January 2017 | Vol 4 | Issue 1 Page 267
Clement SH et al. Int Surg J. 2017 Jan;4(1):264-269
DISCUSSION cancer.6 The commonest cause of gastric outlet
obstruction is cicatrized duodenal ulcer. The next
This study included 10 cases of gastric outlet obstruction commonest cause is carcinoma of pyloric antrum. The
in paediatric age group. All cases are of congenital values are close to the values observed by H. Ellis 1
hypertrophic pyloric stenosis. series.
Male infants accounted for 80% of the cases, which is in In this study most patients were in the fifth and sixth
comparison with the results of Swenson.2 decade of life. In chronic duodenal ulcer cases the
maximum incidence seen in the age group of 30-39 years
There is preponderance of the disease in 1st born infants (38.09%). The average age being 42.5 years with a span
(80%) in this study which is similar to the observations as from 21 to 67 years. Men outnumbered women by 6:1. In
shown by Swenson and as per Gibba MK et al there is the series of Fisher et al.7
increased incidence among first born infants (44%).2,3
The average age was 54 with a span from 20-89 and men
In the present series of cases history of consanguineous outnumbered women by 2:1. In antral carcinoma cases,
marriage between parents was noted in 4 cases showing a the maximum incidence was seen in the age group of 50-
hereditary tendency. As the stomach becomes dilated and 59 years (44.4%). The youngest age of presentation was
muscle becomes flaccid in a neglected infant due to 38 years and the oldest was 67 years with the average age
decompensatory stage, the vomitus becomes regurgitant being 53 years. Men outnumbered women by 3.5:1 as
in type. The vomitus is never bile stained. The infant does compared to 5.5:1 observed by Yogiram and
not appear to be in any discomfort but feels hungry and Chowdhary.8 This higher incidence in males, worldwide
readily accepts feeds immediately after vomiting. All the can be explained as because of more consumption of
10 infants in the present series presented with the gastric irritants by males compared to females.
complaints of vomiting which is similar to the study of
Clifford D Benson.4 43% of the patients were manual labourers who gave a
history of irregular diet habits, which seemed to
In all the cases (100%), vomiting was nonbilious. The contribute to disease process. The series of Donald D.
average age at the onset of vomiting was 30 days i.e. 4 Kozoll and Karl A. Meyer also showed the same pattern
weeks after birth which is in comparison with the study with the non-skilled day labourer group listed most
by Spicer and Benson CD who reported the average as 3 frequently with obstruction.9
weeks.4
The duration of pain was from 3 months to 6 months with
Visible gastric peristalsis and palpable pyloric mass was a median of 4 months 17 cases gave history of APD and 2
observed in 100% of the cases which can be compared of them were malignant cases suggesting malignancy
with report of spicer.5 developing from gastric ulcer. Anorexia was present in 9
(100%) cases of carcinoma of antrum and in 15 (71.42%)
In the present series, 6 infants with prolonged vomiting of duodenal ulcer patients. Loss of weight was seen in 22
presented with serum electrolyte abnormalities. (73.3%) cases. 9 (100%) cases of carcinoma and 13
Ramstedts Pyloromyotomy was performed under general (61.9%) cases of duodenal ulcer gave history of weight
anaesthesia in all 10 cases (100%) using a supra loss. In duodenal ulcer cases the loss of weight was
umbilical transverse muscle cutting incision. Intra gradual but in cases with carcinoma, the loss was rapid.
operative and post-operative periods were uneventful in Haemetemesis was present in 9 (30%) cases and malena
all cases (100%) and no incidence of burst abdomen was was present in 15 (50%) cases. These findings are similar
noticed in the present study though Ramstedts operation to other studies.8,10
had a particular tendency to predispose for burst abdomen
according to several authors. Oral feeds were started In the present series 29 cases were subjected to serum
within 24-48 hours after surgery. 8 out 10 cases operated electrolyte estimation. Out of them 15 cases (50%)
(80%) were followed up. Average period of follow up showed electrolyte imbalance. In the series of Maichel L
was 6 months and they were asymptomatic with Schwartz electrolyte imbalance was present in 30%.
significant weight gain. 2 cases (20%) were lost to follow Upper GI endoscopy was done in 30 cases (100%).10 9
up cases (30%) had pyloric antral carcinoma and 21 (70%)
had cicatrized duodenal ulcer.
The total number of adult cases of gastric outlet
obstruction in this study was 30. This consisted of Gastric In the present series, 100% of cicatrized duodenal ulcer
outlet obstruction secondary to cicatrised duodenal ulcer patients underwent truncal vagotomy with posterior
(21) and gastric outlet obstruction secondary to gastrojejunostomy. In carcinoma of pyloric antrum cases,
malignancy (9). 55.5% patients underwent Billroth II polya gastrectomy
and 44.4% patients underwent anterior
Gastric outlet obstruction due to carcinoma stomach is a gastrojejunostomy. In this series four patients had wound
leading cause of cancer deaths second only to lung infection which was treated by repeated dressings and
International Surgery Journal | January 2017 | Vol 4 | Issue 1 Page 268
Clement SH et al. Int Surg J. 2017 Jan;4(1):264-269
appropriate antibiotics. Three patients had respiratory Funding: No funding sources
tract infections that were treated by review of antibiotics Conflict of interest: None declared
and chest physiotherapy. One patient with carcinoma Ethical approval: The study was approved by the
pyloric region developed anastomotic leak and expired on institutional ethics committee
the tenth post-operative day.
REFERENCES
The overall mortality rate was 6.66% (22.2% for
malignant cases). Mortality rate was zero in case of 1. Ellis H, Pyloric stenosis In: Nyhus LM, Wastell C,
cicatrised duodenal ulcer. Three patients of antral editors. Surgery of the stomach and duodenum, 4th
carcinoima were treated postoperativelv by chemotherapy Ed. Little Brown Publications, Boston, 1986:475.
with 5 FU. Most of the patients with cicatrized duodenal 2. Swenson. Pyloric stenosis In: Raffenssperger GJ,
ulcer (76.1%) and antral carcinoma (55.55%) were Ed. Swensons Paediatric Surgery 5th ed. 1990;211-
followed up. There has been no recurrence of symptoms 9.
in any of the cases that turned up for follow up one 3. Gibba MK, Herden V. Mayo clinic proc-
patient with antral carcinoma case which presented with 50:312,1971.
multiple secondaries postoperatively and expired one 4. Benson CD, Mustard WT, Ravich MM. Congenital
month after surgery. pyloric Stenosis. Paediatr Surg. 1962;2:670-4.
5. Spicer RD. Infantile hypertrophic pyloric stenosis:a
All the patients were subjected to a standard pre- review. Br J Surg. 1982;69:128-35.
operative treatment, which included stomach wash twice 6. Alexander HR, Kelsun DP, Tepper JE. Cancer of
a day for three days prior to surgery. Preoperatively the Stomach, In: Vincent T. Devita Jr, Hellman S,
stomach was dilated in majority of the cases. Post- Rosenberg SA, Ed(s), Cancer: Principles and
operatively Ryles tube aspiration continued till bowel practice of oncology, 6th Ed. Lippincott Williams
movements established by noting bowel sounds, passing and Wilkins, Philadelphia, 2001:1092.
of flatus and gross reduction in quantity of Ryles tube 7. Fisher DR, Ebert PA, Zenidena GD. Obstructing
aspiration. peptic ulcers results of treatment. Arch Surg.
1967;94:724-9.
Later on majority of patients were allowed to take oral 8. Yogiram B, Choudhary NVS. Duodenal (ulcer)
fluids on 6th day followed by semisolid and solid diet. stenosis in Andhra Pradesh: a ten year study. Indian
The average hospital stay in this series was 10 days. This J Surg. 1983;12:3.
is almost similar when compared to the series of Ralph A. 9. Kozoll DD, Meyer KA. Obstructing gastroduodenal
Matteis and Robert E. Hermann where the average ulcers: Symptoms and signs. Arch Surg.
hospital stay was 8.3 days and of Fisher et al where it was 1964;89:491.
6.8 days.7,11,12 10. Schwartz ML, Humphry WE, Dunn HD, Weiland
Douglas. Gastric outlet obstruction in peptic ulcer
CONCLUSION disease, an indication for surgery. Am J Surg.
1982:143:90.
Ramstedts pyloromyotomy is the gold srandard 11. Ralph A. Vagotomy and drainage for obstructing
treatment for CHPS. Patients with gastric outlet duodenal ulcers. Am J Surg. 1974;127:237.
obstruction due to cicatrized duodenal ulcer require 12. Bailey RW. Laparoscopic management of peptic
truncal vagotomy with posterior gastrojejunostomy. ulcer disease. Surgical Laparoscopy Update, Quality
Vagotomy is optional in view of better response with Medical Publishing, Missouri, 1993:241.
drugs for APD. Antral carcinoma cases require curative
or palliative surgery depending on the stage of the Cite this article as: Clement SH, Cherukumalli RP,
disease. Rao CR. A clinical study of gastric outlet obstruction.
Int Surg J 2017;4:264-9.
International Surgery Journal | January 2017 | Vol 4 | Issue 1 Page 269
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- DR ErinaDokument14 SeitenDR ErinaFemmy RuthNoch keine Bewertungen
- Application LetterDokument1 SeiteApplication LetterFemmy RuthNoch keine Bewertungen
- Ebram Assigment (Ma'Am Sondang)Dokument7 SeitenEbram Assigment (Ma'Am Sondang)Femmy RuthNoch keine Bewertungen
- Biogrpy of William BlakeDokument7 SeitenBiogrpy of William BlakeFemmy RuthNoch keine Bewertungen
- Biogrpy of William BlakeDokument7 SeitenBiogrpy of William BlakeFemmy RuthNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Nursing Care Plan Placenta PreviaDokument2 SeitenNursing Care Plan Placenta PreviaApril Ann HortilanoNoch keine Bewertungen
- Dr. Khairiyadi, M.Kes., Sp.A Departemen Ilmu Kesehatan Anak RSUD Ulin BanjarmasinDokument78 SeitenDr. Khairiyadi, M.Kes., Sp.A Departemen Ilmu Kesehatan Anak RSUD Ulin BanjarmasinEldhaNoch keine Bewertungen
- 0199975744Dokument305 Seiten0199975744nicoletaelenaNoch keine Bewertungen
- Slides From McCullough 10-27-2021 PresentationDokument83 SeitenSlides From McCullough 10-27-2021 PresentationAssociation of American Physicians and Surgeons100% (10)
- Sepsis and CellulitisDokument2 SeitenSepsis and Cellulitisryan_weldon_3Noch keine Bewertungen
- Disorders of Coagulation FactorsDokument35 SeitenDisorders of Coagulation FactorsMelesNoch keine Bewertungen
- Case Study On Nephrotic SyndromeDokument7 SeitenCase Study On Nephrotic SyndromeArchana VermaNoch keine Bewertungen
- ICD-10 TK Pedsos 2013Dokument10 SeitenICD-10 TK Pedsos 2013Ludi Dhyani RahmartaniNoch keine Bewertungen
- Diabetis 2Dokument33 SeitenDiabetis 2Fercho MedNoch keine Bewertungen
- Metformin, Glucophage, Glucophage XR, Glumetza, Fortamet, RiometDokument5 SeitenMetformin, Glucophage, Glucophage XR, Glumetza, Fortamet, RiometAgronaSlaughterNoch keine Bewertungen
- Drug Name Gemcitabine: Synonym (S) : Common Trade Name (S) : ClassificationDokument8 SeitenDrug Name Gemcitabine: Synonym (S) : Common Trade Name (S) : ClassificationOka Robi MuhammadNoch keine Bewertungen
- Buttaravoli, Philip - Minor Emergencies - Blunt Scrotal Trauma (2007)Dokument3 SeitenButtaravoli, Philip - Minor Emergencies - Blunt Scrotal Trauma (2007)Vivian ChanNoch keine Bewertungen
- Broiler Breeder DiseasesDokument12 SeitenBroiler Breeder DiseasesvetbcasNoch keine Bewertungen
- Kaposi SarcomaDokument11 SeitenKaposi Sarcomaedgar mandengNoch keine Bewertungen
- Neck Pain: Simple ExercisesDokument2 SeitenNeck Pain: Simple ExercisesVijaya Krishna DevarapalliNoch keine Bewertungen
- Aches and Pains in The ElderlyDokument34 SeitenAches and Pains in The ElderlyAna CampeanuNoch keine Bewertungen
- em Exam - 1-AnswersDokument3 Seitenem Exam - 1-AnswersAzra MuzafarNoch keine Bewertungen
- A Case Study of Bronchial Asthma in Acute Exacerbation (Baiae)Dokument13 SeitenA Case Study of Bronchial Asthma in Acute Exacerbation (Baiae)Samantha BolanteNoch keine Bewertungen
- Jabeen & TahirDokument12 SeitenJabeen & TahirSanaNoch keine Bewertungen
- Using Sugar To Treat Those Nasty Wounds: American Farriers Journal Special Management Report #1..Dokument3 SeitenUsing Sugar To Treat Those Nasty Wounds: American Farriers Journal Special Management Report #1..alfirafresdiNoch keine Bewertungen
- Therapy of Acute Respiratory Infections in Children: NoveltiesDokument11 SeitenTherapy of Acute Respiratory Infections in Children: NoveltiesrizkaNoch keine Bewertungen
- TB in Special SituationsDokument49 SeitenTB in Special SituationsVipul KumarNoch keine Bewertungen
- Berikut Ini Macam Macam Penyakit Dan Istilah MedisDokument24 SeitenBerikut Ini Macam Macam Penyakit Dan Istilah MedisIis Izy IssooNoch keine Bewertungen
- HealthMeans Lets Talk About AutoimmunityDokument37 SeitenHealthMeans Lets Talk About AutoimmunityvaleriabostanNoch keine Bewertungen
- THC AspergerDokument168 SeitenTHC AspergerMICHAELNoch keine Bewertungen
- MetoprololDokument3 SeitenMetoprololapi-3797941100% (3)
- Endocrine NCLEX PN Pract & ANS Questions IIDokument13 SeitenEndocrine NCLEX PN Pract & ANS Questions IIYA HONoch keine Bewertungen
- AZ Heart Angioscreen - Biltmore Lifestyles Dec 2022Dokument1 SeiteAZ Heart Angioscreen - Biltmore Lifestyles Dec 2022Brittany LudwigNoch keine Bewertungen
- Kode Kombinasi Icd 10 Dan Icd 9 Indonesia Update 2018Dokument10 SeitenKode Kombinasi Icd 10 Dan Icd 9 Indonesia Update 2018Dini AzizahNoch keine Bewertungen
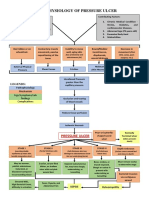
- Pathophysiology of Pressure UlcerDokument1 SeitePathophysiology of Pressure UlcerSTORAGE FILENoch keine Bewertungen