Beruflich Dokumente
Kultur Dokumente
Translate 2
Hochgeladen von
BaharuddinCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Translate 2
Hochgeladen von
BaharuddinCopyright:
Verfügbare Formate
The detection of sedentary lifestyle as a risk factor is, to our knowledge, a new finding and could
be as a consequence of a major lymph flow mechanism (the muscle pump) being inactive.
There are several factors to be considered before our risk-factor findings are used for risk-
stratification purposes. First, these risk factors alone do not accurately predict who will develop
arm lymphoedema and who will not. These specific factors represent six of 12 identified risk
factors in one, prospective, population-based cohort study, which together explained only 35% of
variation between those who did and those who did not develop lymphoedema.39 Furthermore,
women can and do present with arm lymphoedema despite having healthy bodyweight, regular
physical activity levels, and lumpectomy surgery. Finally, little is known about the potential
contribution of the cancer itself, or the possible importance of genetic predisposition, to
lymphoedema risk. Findings from animal models110 and one study in human beings111 provide
preliminary evidence for a contribution of genetic susceptibility to the development of secondary
lympho edema after breast cancer. Nonetheless, current understanding of risk factors can inform
lymphoedema prevention and management strategies. Although treatment-related risk factors are
largely not modifiable (because they are generally dictated by the type and stage of disease and
available treatment options), substantial scope exists for the modification of patients' physical
activity levels and bodyweight after breast cancer: most women with breast cancer are
insufficiently active at diagnosis112114 and more than 50% are overweight or obese.115
Further research is needed to improve our understanding of risk factors (including further
exploration of known risk factors, such as whether lymphedoema rates differ between those with
delayed axillary-lymph-node dissection after sentinel-node biopsy compared with axillary-
lymph-node dissection from the outset), as well as prevention and treatment strategies. Only with
. increased knowledge will we be in a position to improve further the lives of women with breast
cancer, and reduce the overall socioeconomic burden of this disabling, distressing disorder.
398 individual studies identified and screened
286 excluded after assessment of abstracts and titles
112 full-text articles for eligibility
33 articles excluded
7 duplicate or secondary analyses
3 recorded pre-operation incidence only
19 did not meet eligibility criteria
3 simply assessed lymphedema
1 was done more than 30 years ago
79 articles included in review (74 incidence
and 31 risk factors)
72 studies on incidence*
29 studies on risk factors
Figure 1: Flow diagram of study selection for inclusion in this review and meta-analysis *We
included 74 articles, which presented results of 72 studies (two studies were each presented in
two articles). We included 31 articles, which presented results of 29 studies (two studies were
each presented in two articles).
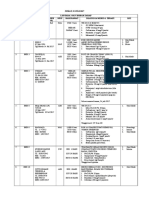
Included studies (n)
Incidence (%; 95% CI)
Pooled estimate
All studies 72 166 (136202)
Prospective cohort studies 30 214 (149298)
Randomized clinical trial 7 104 (79135)
Retrospective cohort 10 84 (54128)
Cross-sectional studies 25 177 (138224)
Location of study
Asia 4 180 (102298)
Australasia 7 215 (150298)
Europe 17 142 (109184)
Middle East 1 175 (139218)
North America 32 210 (151285)
South America 3 137 (81222)
UK 8 84 (51136)
Axillary surgery
SLNB 18 56 (6179)
ALND 18 199 (135282)
Measurement method*
Lymphoscintigraphy 1 50 (16144)
Bioelectrical impedance 3 159 (46426)
Self-reported clinical diagnosis 5 125 (62236)
Clinical diagnosis 7 126 (81193)
Circumference 38 148 (114190)
Perometry 17 164 (109241)
Self-reported swelling 19 204 (138290)
More than one measure 9 282 (118535)
Time since breast cancer diagnosis or surgery*
3 to <6 months 8 103 (62167)
6 to <12 months 15 138 (73245)
12 to <24 months 24 189 (142247)
2 to <5 years 30 186 (136248)
5 years 16 156 (100235)
More than one time category 6 76 (27195)
ALND=axillary-lymph-node dissection. SLNB=sentinel-lymph-node biopsy. *Numbers
(percentages) might not add to 72 (100%) because some studies measured lymphoedema with
more than one method or at more than one timepoint.
Table 1: Incidence of breast cancer-related lymphoedema
Contributors TD, BN, and SH participated in the conception and design of the review. TD and
SR participated in the extraction and analysis of data. TD, SR, BN, and SH participated in the
interpretation of data and writing of the paper. All authors approved the final version.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Steps For Applying For The DHCA Prometric ExaminationDokument1 SeiteThe Steps For Applying For The DHCA Prometric ExaminationLentoOt EksDiiNoch keine Bewertungen
- National Acupuncture Foundation - Clean Needle Technique Ver PDFDokument73 SeitenNational Acupuncture Foundation - Clean Needle Technique Ver PDFJessé de AndradeNoch keine Bewertungen
- Harvest Moon Hero of ValleyDokument72 SeitenHarvest Moon Hero of ValleyBaharuddinNoch keine Bewertungen
- Denah RuanganDokument30 SeitenDenah RuanganBaharuddinNoch keine Bewertungen
- Ugd 28Dokument2 SeitenUgd 28BaharuddinNoch keine Bewertungen
- Koran 28 Juli 2017Dokument10 SeitenKoran 28 Juli 2017BaharuddinNoch keine Bewertungen
- Extremely Preterm Infants Small For Gestational Age Are at Risk For Motor Impairment at 3 Years Corrected AgeDokument3 SeitenExtremely Preterm Infants Small For Gestational Age Are at Risk For Motor Impairment at 3 Years Corrected AgeBaharuddinNoch keine Bewertungen
- Koran 28 Juli 2017Dokument10 SeitenKoran 28 Juli 2017BaharuddinNoch keine Bewertungen
- Daftar Pustaka (Ubah Page Number)Dokument1 SeiteDaftar Pustaka (Ubah Page Number)BaharuddinNoch keine Bewertungen
- Outline ICON JournalDokument3 SeitenOutline ICON JournalBaharuddinNoch keine Bewertungen
- Hypothermia in TraumaDokument37 SeitenHypothermia in TraumaBaharuddinNoch keine Bewertungen
- Disaster Victim Identification (Dvi) : ( (GB) Version 2008)Dokument21 SeitenDisaster Victim Identification (Dvi) : ( (GB) Version 2008)Shanty ManekNoch keine Bewertungen
- Reflective Practice A Systematic ReviewDokument27 SeitenReflective Practice A Systematic ReviewBogdanRadu100% (1)
- Referat ObsgynDokument21 SeitenReferat ObsgynRoberto HutapeaNoch keine Bewertungen
- 7.ipc Yemen Food Security Nutrition 2022june Report EnglishDokument41 Seiten7.ipc Yemen Food Security Nutrition 2022june Report EnglishSirajNoch keine Bewertungen
- Interventional Procedure in NeurosurgeryDokument2 SeitenInterventional Procedure in NeurosurgeryAbhinav GuptaNoch keine Bewertungen
- I Great Medi Care Pds enDokument6 SeitenI Great Medi Care Pds enainafaqeeraNoch keine Bewertungen
- MPH Curriculum ExampleDokument3 SeitenMPH Curriculum ExampleMark EbrahimNoch keine Bewertungen
- Journal Club Template: For Randomized Controlled TrialsDokument19 SeitenJournal Club Template: For Randomized Controlled TrialsAndrew DavidsonNoch keine Bewertungen
- Peptic Ulcers: H.pylori Infection Is Usually Contracted in Childhood, Perhaps ThroughDokument2 SeitenPeptic Ulcers: H.pylori Infection Is Usually Contracted in Childhood, Perhaps ThroughMike PalmaNoch keine Bewertungen
- Prosto 1Dokument11 SeitenProsto 1saliamaharaniNoch keine Bewertungen
- Tiara Puspita Dan Zahara Ilmiah SafitriDokument17 SeitenTiara Puspita Dan Zahara Ilmiah SafitriTiara Puspita keperawatanNoch keine Bewertungen
- Lec 5 New Castle DiseaseDokument38 SeitenLec 5 New Castle Diseasebasit abdulNoch keine Bewertungen
- Pyogenic GranulomaDokument13 SeitenPyogenic GranulomaPiyusha SharmaNoch keine Bewertungen
- Effects of Mental Health On Physical WellDokument3 SeitenEffects of Mental Health On Physical WellYash RaiNoch keine Bewertungen
- Making Medical Decision For Someone ElseDokument23 SeitenMaking Medical Decision For Someone Elseapi-274729393100% (1)
- Ncpfdardrug Study NotesDokument3 SeitenNcpfdardrug Study NotesLuigi GeduqueNoch keine Bewertungen
- Bronchiectasis (Obstructive) Cheat Sheet: by ViaDokument1 SeiteBronchiectasis (Obstructive) Cheat Sheet: by ViaKat KatNoch keine Bewertungen
- Prosthodontics Q&a (CDD)Dokument121 SeitenProsthodontics Q&a (CDD)Tara Lingating100% (1)
- Your Life Your Choice Death BookDokument53 SeitenYour Life Your Choice Death BookJeffersonLuvrNoch keine Bewertungen
- Management of Adolescent GynecomastiaDokument11 SeitenManagement of Adolescent GynecomastiaChon ChiNoch keine Bewertungen
- Review Jurnal Kva Nasiona Dan InternasionalDokument4 SeitenReview Jurnal Kva Nasiona Dan Internasionalbnanx milkNoch keine Bewertungen
- Covid 19 Faqs Hospitals Hospital Laboratory Acute Care Facility Data ReportingDokument52 SeitenCovid 19 Faqs Hospitals Hospital Laboratory Acute Care Facility Data ReportingRajesh SharmaNoch keine Bewertungen
- Mental Health in IndiaDokument6 SeitenMental Health in IndiaStarlin MythriNoch keine Bewertungen
- Mast Cell Activation DiseaseDokument8 SeitenMast Cell Activation DiseaseJesse FrontierlandNoch keine Bewertungen
- Research Study On Knowledge of Interns Regarding Wound CareDokument41 SeitenResearch Study On Knowledge of Interns Regarding Wound CareBritten Norman Santiago100% (1)
- SAJS Vol543 2112 HIG SA Guidelines For The Management of Ventral HerniasDokument29 SeitenSAJS Vol543 2112 HIG SA Guidelines For The Management of Ventral HerniasMonika Diaz KristyanindaNoch keine Bewertungen
- Jadwal OktoberDokument48 SeitenJadwal OktoberFerbian FakhmiNoch keine Bewertungen
- A Literature Review of Midwifery-Led Care in Reducing Labor and Birth InterventionsDokument14 SeitenA Literature Review of Midwifery-Led Care in Reducing Labor and Birth Interventionsradilla syafitriNoch keine Bewertungen
- I Sometimes Worry About My Short Attention SpanDokument1 SeiteI Sometimes Worry About My Short Attention SpanAmmer Yaser MehetanNoch keine Bewertungen
- Clinical Oral Implants Res - 2022 - Jung - Effect of Peri Implant Mucosal Thickness On Esthetic Outcomes and The EfficacyDokument9 SeitenClinical Oral Implants Res - 2022 - Jung - Effect of Peri Implant Mucosal Thickness On Esthetic Outcomes and The EfficacyGustavo BerrioNoch keine Bewertungen