Beruflich Dokumente
Kultur Dokumente
165 Real World Introduction of Tobramycin Inhalation P 2015 Journal of Cys
Hochgeladen von
Emad Tawfik AhmadOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
165 Real World Introduction of Tobramycin Inhalation P 2015 Journal of Cys
Hochgeladen von
Emad Tawfik AhmadCopyright:
Verfügbare Formate
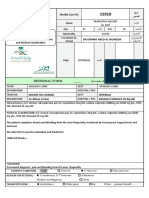
S100 7.
Physiotherapy Posters
163 Phoniatric voice rehabilitation in cystic brosis 165 Real world introduction of tobramycin inhalation powder TIP in
adults with cystic brosis
L. Graziano1 , M. Tornaghi2 , B. Giacomodonato1 , M. Curzi1 , T. Perelli1 ,
S. De Sanctis1 , M. Varchetta1 , F. Alatri1 . 1 Sapienza University of Rome, H.B. Langman1 , A.L. Brennan1 , R.J. Bright-Thomas1 , A.M. Jones1 , D.W. Riley1 ,
Pediatrics, Rome, Italy; 2 Sapienza University of Rome, Medical Administration S.C. Johnson1 . 1 Manchester Adult Cystic Fibrosis Centre, Manchester, United
Kingdom
Ofce, Rome, Italy
Objectives: To evaluate the introduction of TIP in adult patients attending Manchester
Objectives: Patients with cystic brosis (CF) may present a progressive quality Adult Cystic Fibrosis Centre.
alteration of voice which appears with increased fatigue and relational discomfort. Methods: In December 2012 TIP was introduced in line with NICE recommendations.
To describe our experience in treating voice disorders in seven patients with CF. Tolerance prior to prescription was assessed at test dose followed by 1 month trial
Methods: 7 patient with CF (3F) age 2046 years had otolaryngological visit, of treatment. Outcome measures included spirometry, 7 day symptom score (Bennett
rhinolaryngoscopic examination and functional assessment of the voice. Three dif- et al, 2010 JCF) and perceived treatment burden (110 scale, 10 = overwhelming).
ferent conditions were found: 3 double lung transplantation patients with unilateral IV antibiotic days were calculated for patients who completed 12 months of treatment.
vocal cord paralysis due to surgery and with timbre of voice blown; 1 patient with 12 month follow up is ongoing.
gastroesophageal reux with bilateral vocal cord edema and with timbre of voice Results: Values are median (range)unless stated otherwise. 92 patients received a test
veiled; 3 patients with bilateral hypotonia of the true vocal chords and with timbre dose of TIP, mean age 28 years (1750), baseline FEV1 1.55 (0.584.3), baseline
FEV1 % predicted 43 (21112). 68 patients completed 1 month trial. 60/68 patients
of voice hoarse. Patients started a six months phoniatric voice rehabilitation
who completed trial continued treatment. 36/60 (60%) continued for >12 months.
program. Exercises consisted in breathing exercises to relax thoracic outlet and 23/36 have received 12 month clinical follow up.
to increase vocal cord rmness and phonation time.
Table 1. Comparison of baseline and 1 month data
Results: All patients achivied their physiological timbre of voice, a detension of
the thoracic outlet, an increased phonation time, an effective compensation by the Baseline (n = 60) 1 month follow up (n = 60)
contralateral vocal fold on that in paralysis, a regression of vocal cord edema FEV1 (litres) 1.625 (0.5753.69) 1.875 (0.624.15)
(laryngoscopy). FEV1 % predicted 46 (21112) 48.5 (21116)
Conclusion: A multidisciplinary program of phoniatric voice rehabilitation allowed Symptom score 5 (016) 4 (08)
the resolution of a functional disturbance and the relational discomfort in our
Treatment burden 5 (010) 2 (08)
patients with dysphonia.
Values are median (range).
Table 2. 12 month follow up data (n = 23)
pre post
FEV1 1.7 (0.5753.65) 1.71 (0.553.73)
FEV1 % predicted 48 (2180) 46 (2085)
IV days 26 (071) 15 (056)
Conclusion: In real world use TIP appears to be associated with reduction in
perceived symptom scores and treatment burden; improvement in spirometry and
reduction in IV days. Only 60% patients continued TIP for >12 months. Reasons
for this need further evaluation.
164 Autogenic drainage and assisted autogenic drainage in children 166 Improvements in inhalational treatment amongst children using
with cystic brosis: A systematic review the Philips I-neb insight online software
L. Corten1 , J. Jelsma2 , B.M. Morrow3 . 1 University of Cape Town, Health and C. Yonge1 , V. Keenan1 , S. Payne1 , G. Connett1 . 1 Southampton University
Rehabilitation Sciences (Physiotherapy), Observatory, Cape Town, South Africa; Hospitals NHS Trust, Regional Paediatric CF Unit, Southampton, United Kingdom
2 University of Cape Town, Health and Rehabilitation Sciences, Cape Town, South
Objectives: The Philips I-neb Adaptive Aerosol Delivery system is a portable drug
Africa; 3 University of Cape Town, Paediatrics and Child Health, Cape Town,
delivery device using vibrating mesh technology. I-neb insight on-line software
South Africa
collects detailed data about I-neb usage. These data have previously assessed
Chest physiotherapy is considered an essential part of symptomatic, multidisci- adherence. In this study we have utilised data to identify individuals with poor
plinary management in cystic brosis (CF), as it facilitates clearance of viscous inhalation techniques to assess the effectiveness of an active intervention.
pulmonary secretions. Methods: Data for nebuliser use over a recent two month period from 13 I-nebs
Objectives: To determine the effect of autogenic drainage (AD) and assisted auto- in children age 516 yrs were analysed to identify individuals with poor and/or de-
genic drainage (AAD) compared to no; sham; or other types of chest physiotherapy clining inhalational techniques according to examination of total I-neb nebulisation
in children with CF. time, inhalation time/breath and rest time. All patients had been previously assessed
Methods: Six databases, clinicaltrials.gov and pactr.org were searched. We included in their use of a TIM mouthpiece to achieve >2 s inhalation. Those identied with
randomized controlled trials, quasi-randomized controlled trials and randomized poor and/or declining inhalation techniques received tailored interventions. Further
cross-over trials on AD and AAD in children younger than 18 years, diagnosed data were obtained over the following month. Parameters for the most recent two
with CF. One author conducted the database search. Titles, abstracts and data weeks were compared with those obtained in the two weeks prior to intervention.
were evaluated by two independent reviewers with agreement by discussion and Results: Six children were identied with poor inhalation techniques. In most, short
consensus. comings occurred for all parameters. Median total nebulisation time decreased from
Results: A total of 126 titles were screened, of which seven were eligible. However, 3 min 25 s to 2 min 38 s. Median inhalation time/breath increased from 3.45 s to
only two studies made a clear distinction between pediatric (ntotal = 47; n1 = 36 & 3.65 s. Rest time as a % of total treatment time decreased from 39% to 31%.
n2 = 9) and adult data, and were therefore analyzed. We were unable to perform a Conclusion: This study indicates how software generated data about routine
meta-analysis, as only one study clearly indicated separate results for the different nebuliser inhalation techniques can be used to optimise patient performance and
periods of the cross-over. Based on the pediatric data of this one study, participants decrease burden of care using patient specic feedback and education. Further
who received AD had a signicant improvement in Huang scores; a tendency to have studies might usefully determine how inhalational techniques are maintained in the
fewer hospital admissions during one year when compared to postural drainage; and long term.
a clear preference for AD by participants. One other study reported pediatric data,
however no signicance levels were provided.
Conclusion: Due to the lack of pediatric-specic randomized controlled trials, small
sample sizes and unclear risk of bias of most studies, we were unable to determine
the efcacy and/or safety of AD and AAD in children with CF.
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Motor Stimulation With Interferential Cu 1985 Australian Journal of PhysiothDokument6 SeitenMotor Stimulation With Interferential Cu 1985 Australian Journal of PhysiothEmad Tawfik AhmadNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- 151 Effects of Physiotherapy Treatment On Knee Oa Gai 2009 Osteoarthritis AnDokument2 Seiten151 Effects of Physiotherapy Treatment On Knee Oa Gai 2009 Osteoarthritis AnEmad Tawfik AhmadNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- 1 19 Osteoarthritis Year in Review Rehabilitatio 2011 Osteoarthritis and CADokument1 Seite1 19 Osteoarthritis Year in Review Rehabilitatio 2011 Osteoarthritis and CAEmad Tawfik AhmadNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Journey To The Centre of The EarthDokument43 SeitenJourney To The Centre of The EarthEmad Tawfik Ahmad100% (4)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Risk-Prone Health BehaviorDokument2 SeitenRisk-Prone Health Behaviordragon3466100% (1)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Cool Azul Sports GelDokument1 SeiteCool Azul Sports GelroslizamhNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Unit 3 & Unit 4Dokument8 SeitenUnit 3 & Unit 4Melania Arliana MeoNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Referral FormDokument2 SeitenReferral Formraad_alghamdi_1Noch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Comfort Measures: A Concept Analysis: Irene Oliveira, RN, BSCNDokument21 SeitenComfort Measures: A Concept Analysis: Irene Oliveira, RN, BSCNLina Mahayaty SembiringNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- March 2013 Board of Nursing NoticesDokument528 SeitenMarch 2013 Board of Nursing NoticesJames LindonNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- What Works in Therapy?Dokument12 SeitenWhat Works in Therapy?Ariel PollakNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Trial of ScarDokument12 SeitenTrial of Scarnyangara50% (2)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Section 12Dokument7 SeitenSection 12Saravanan ThangarajanNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- 5.teori Personaliti TEORI AARON BECKDokument35 Seiten5.teori Personaliti TEORI AARON BECKJinn Ting TanNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Art 1 - Frequency Evaluation of Different Extraction Protocols in Orthodotic Treatment During 35 YearsDokument7 SeitenArt 1 - Frequency Evaluation of Different Extraction Protocols in Orthodotic Treatment During 35 YearsAlejandro Aranzábal NavarreteNoch keine Bewertungen
- General AnaesthesiaDokument10 SeitenGeneral AnaesthesiaAlfiatuz ZahroNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Form of Application For Claiming Reimbursement of Medical Expenses of Government Servants and Their FamiliesDokument5 SeitenForm of Application For Claiming Reimbursement of Medical Expenses of Government Servants and Their FamiliesAmit GautamNoch keine Bewertungen
- Askep Demensia GerontikDokument8 SeitenAskep Demensia Gerontikjoveny meining tyas0% (1)
- Emergency Obstetric and Newborn CareDokument4 SeitenEmergency Obstetric and Newborn CaremnmrznNoch keine Bewertungen
- Difficult Airway 2011 Power Point PresentationDokument54 SeitenDifficult Airway 2011 Power Point PresentationBalaji Mallela100% (1)
- Health Insurance Summit - ProceedingsDokument43 SeitenHealth Insurance Summit - ProceedingsanuiscoolNoch keine Bewertungen
- 1mg BillDokument1 Seite1mg BillkgagansinghNoch keine Bewertungen
- The FIM Instrument Background Structure and UsefulnessDokument31 SeitenThe FIM Instrument Background Structure and UsefulnessAni Fran SolarNoch keine Bewertungen
- Case Presentation Format 3Dokument1 SeiteCase Presentation Format 3Priya Sharma Sabarad100% (3)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Quality Assurance in NursingDokument7 SeitenQuality Assurance in NursingSimran Chauhan100% (1)
- Patient Safety and Clinical RiskDokument5 SeitenPatient Safety and Clinical Riskshylajathomas33Noch keine Bewertungen
- Crisis Prevention Intervention Plan TrainingDokument8 SeitenCrisis Prevention Intervention Plan TrainingSheila OdorNoch keine Bewertungen
- Cac Ethiopia - Istanbul Tours 2022Dokument6 SeitenCac Ethiopia - Istanbul Tours 2022Awol AminNoch keine Bewertungen
- Research Paper (Plastic Surgery)Dokument7 SeitenResearch Paper (Plastic Surgery)Won-joon Jung100% (7)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Health Center IPCR RN Ver 1.1 (With Program Management)Dokument7 SeitenHealth Center IPCR RN Ver 1.1 (With Program Management)RvBombeta50% (2)
- Teaching Plan: Objectives Identified Problems/Concerns Activities Evaluation Student Nurse Client/Family MemberDokument5 SeitenTeaching Plan: Objectives Identified Problems/Concerns Activities Evaluation Student Nurse Client/Family MemberRaine SarmientoNoch keine Bewertungen
- BlindnessDokument26 SeitenBlindnessdrmeenaxiNoch keine Bewertungen
- Textbook of Medical Parasitology Protozoology HelmDokument2 SeitenTextbook of Medical Parasitology Protozoology HelmramyadevidurairajNoch keine Bewertungen
- Key Skills in Integrated Dental Care: Peter Mossey, Gareth Holsgrove, Elizabeth Davenport and David StirrupsDokument12 SeitenKey Skills in Integrated Dental Care: Peter Mossey, Gareth Holsgrove, Elizabeth Davenport and David Stirrupsdruzair007Noch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)