Beruflich Dokumente
Kultur Dokumente
Metabolik Encelophaty
Hochgeladen von
fkiaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Metabolik Encelophaty
Hochgeladen von
fkiaCopyright:
Verfügbare Formate
See
discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/27199289
Metabolic Encephalopathies
Article December 2003
Source: OAI
CITATIONS READS
5 1,713
3 authors, including:
Visnja Supanc Vida Demarin
University Clinical Hospital Center "Sestre Milo International Institute for Brain Health, Zagreb,
28 PUBLICATIONS 187 CITATIONS 549 PUBLICATIONS 2,826 CITATIONS
SEE PROFILE SEE PROFILE
All content following this page was uploaded by Vida Demarin on 07 September 2017.
The user has requested enhancement of the downloaded file.
Supanc
Acta V. etCroat
Clin al. 2003; 42:351-357 Metabolic encephalopathies
Review
METABOLIC ENCEPHALOPATHIES
Vinja Supanc, Vesna Vargek-Solter and Vida Demarin
University Department of Neurology, Sestre milosrdnice University Hospital, Zagreb, Croatia
SUMMARY Metabolic encephalopathies may be important complications of many diseases in patients
treated at intensive care units. The term metabolic encephalopathies encompasses a large variety of differ-
ent conditions of the brain. Neurologic signs of metabolic encephalopathies, ancillary tests, differential
diagnosis, etiology, pathophysiology and treatment are discussed in this review. Metabolic encephalopa-
thies are usually multifactorial in origin and play an important role not only as diseases per se but also for
monitoring the severity of decompensating organ functions during deteriorating primary diseases.
Key words: Brain diseases metabolic, diagnosis; Brain diseases metabolic, physiopathology; Critical care; Shock septic,
diagnosis; Shock septic, physiopathology; Multiple organ failure, diagnosis
Introduction Etiology
Metabolic or secondary encephalopathies are disorders Metabolic encephalopathies are caused by hypoxic-is-
in which a disturbance of cerebral function (encephalop- chemic states, a variety of organ dysfunctions, systemic
athy) results from failure of some other organ system (e.g., diseases and toxic agents (Table 1). Alcohol is the single
heart and circulation, lungs and respiration, kidneys, liver, most frequent exogenous toxic agent1.
pancreas and the endocrine glands); in fact in many cases
they are multifactorial in origin. Encephalopathies can be Pathophysiology
defined as diffuse, multifocal and functional cerebral dis-
turbances, which are not caused by inflammation, in oth- Up to now, the pathophysiologic mechanism of meta-
er words, it is not encephalitis, and, at least in the begin- bolic encephalopathies has not been completely under-
ning, is not combined with morphologic changes. Primary stood. The basic precondition is probably a disturbance of
encephalopathies are caused by different, mostly geneti- blood brain barrier with changes in the amino acid and
cally defined disturbances of amino acid, carbohydrate and neurotransmitter profile. Evidence from clinical and exper-
lipid metabolism. imental research shows that vascular factors, infection and
Metabolic encephalopathies are most common compli- endotoxins have a distinctive role in the pathophysiology2.
cations of many diseases in patients treated at intensive Histopathologic studies found tissue hypoxia, edema and
care units and their clinical manifestation can be taken as necrosis in vascular and special types of hepatic encepha-
a warning of deterioration or beginning of organ dysfunc- lopathies. Morphologic changes of astrocytes including
tion. Reversibility of metabolic encephalopathy relates to hyperplasia of protoplasmic astrocytes that resembles
successful treatment of systemic dysfunction, subject of Alzheimer type II cells are found at the cellular level3,4.
progress in the field of internal medicine.
Clinical Featres
Correspondence to: Vinja Supanc, M.D., University Department of Neu-
Metabolic disturbances are frequent causes of impaired
rology, Sestre milosrdnice University Hospital, Vinogradska c. 29, HR- consciousness. Their presence must always be considered
10000 Zagreb, Croatia when there are no focal signs of cerebral disease and both
Received July 7, 2003, accepted in revised form October 3, 2003 the imaging studies and the cerebrospinal fluid are normal.
Acta Clin Croat, Vol. 42, No. 4, 2003 351
Supanc V. et al. Metabolic encephalopathies
Table 1. Major causes of metabolic encephalopathies Clinical signs in metabolic encephalopathies may be
divided into global cerebral signs and focal cerebral signs.
Hypoxia Global signs predominate and may be accompanied by
Anemia mostly less pronounced focal signs, depending on the se-
Pulmonary disease verity of encephalopathy. In early stages, global signs in-
Alveolar hypoventilation clude confusion and slight cognitive disturbances as well
as psychomotor hyperactivity (agitation, hallucination,
Ischemia delusions, delirium) and autonomic dysfunctions (Chey-
Cardiovascular disease (including cardiac arrest) ne-Stokes respiration, cardiac arrhythmias or arrest, verti-
Stokes-Adams syndrome, cardiac arrhythmias go, nausea, vomiting, vasomotor and sudomotor disturbanc-
Hypersensitive carotid sinus es). In more severe cases, seizures, global brainstem signs
Microvascular diseases with oral and facial automatisms, pathologic reflexes, trem-
Hyperviscosity syndrome or, asterixis, multifocal myoclonus and abnormalities of
Hypotension muscle tone (paratonia, decorticate and decerebrate pos-
Hypertension turing) are found. The expression of these signs is variable
even in the clinical course of the same patient.
Systemic diseases
Focal cerebral signs may originate from the hemi-
Hepatic disease
spheres (visual disturbances, aphasia, apraxia, hemispas-
Renal disease
Pancreatic disease (gastrointestinal)
Malnutrition (vitamin deficiency) Table 2. Classification of the acquired metabolic disorders of
Endocrine dysfunction (hypoglycemia or the nervous system
hyperglycemia and hyperosmolar state)
Acid-base, electrolyte and fluid imbalances 1. Metabolic diseases presenting as a syndrome of
Vasculitis confusion, stupor or coma
Infections and sepsis Hypoxic-hypotensive encephalopathy
Malignancy (paraneoplastic syndromes) Hypercapnia
Hyperglycemia
Toxic agents Hypoglycemia
Alcohol, sedatives (barbiturates, narcotics, Hepatic failure
tranquilizers) Reyes syndrome
Psychiatric medications (tricyclic antidepressants, Uremia
anticholinergic drugs, phenothiazine, monoamine Disturbances of sodium, potassium, and
oxidase inhibitors) changes in osmolality
Heavy metals
Organic phosphates, solvents 2. Metabolic diseases presenting as a progressive
Other drugs (corticosteroids, penicillin, extrapyramidal syndrome
anticonvulsants) Acquired hepatocerebral degeneration
Hyperbilirubinemia, kernicterus
Hypoparathyroidism
The main feature of the reversible metabolic encephalo- 3. Metabolic diseases presenting as cerebellar ataxia
pathies is mental confusion with disorientation and inat- Hypothyroidism
tentiveness, accompanied in some instances by asterixis, Hyperthermia
tremor and myoclonus. This state may progress to stupor Celiac disease
and coma1,5. Slowing of the background rhythms in the
electroencephalogram parallels the severity of the meta- 4. Metabolic diseases causing psychosis or dementia
bolic disturbance6,7. Cushing disease and steroid encephalopathy
In Table 2, the acquired metabolic diseases of the ner- Thyroid psychosis and hypothyroidism
vous system are classified according to their most common Hyperparathyroidism
clinical presentation. Pancreatic encephalopathy
352 Acta Clin Croat, Vol. 42, No. 4, 2003
Supanc V. et al. Metabolic encephalopathies
tic, hemiatactic, hemisensory syndromes, reflex and mus- Clinical features depend on the degree of hypoxia as
cle tone changes) or/and from the brainstem (cranial nerve well as on the speed of the advancement of hypoxia. Mild
disturbances, e.g., oculovestibular, pupillomotor; nystag- degrees of hypoxia induce inattentiveness, poor judgement
mus, gaze deviations, brainstem reflex disturbances, dys- and motor incoordination. Profound anoxia may be well
arthria, dysphagia, respiratory disturbances, atactic, paretic, tolerated if arrived gradually; that could be seen in some
sensory syndromes hemi-, quadri-, alternating; reflex patients with advanced pulmonary disease who are fully
changes, myoclonus)8. awake even if their arterial oxygen pressure is in the range
The clinical course of encephalopathies is variable. of 4 to 5 kPa. This level, if occurring abruptly, causes coma9.
Coma may develop acutely or a fluctuating level of con- The most severe degrees of the lack of oxygen are usu-
sciousness may be present. This fluctuating individual ally caused by cardiac irregularities, especially by cardiac
course is a characteristic feature in the clinical assessment arrest. Consciousness is lost within seconds, but recovery
of different types of encephalopathies. will be complete if breathing, oxygenation of blood and
The history and clinical examination of consciousness, cardiac action are restored within 3 to 5 min. In case of
respiration, pupillary reactions and ocular movements, hypothermia or barbiturate coma recovery is complete if
spontaneous movements, muscle tone and posture must the restoration of cardiopulmonary functions is complet-
be carefully taken along with the battery of additional ed within 8 to 10 min. The outcome of cardiac arrest is gen-
erally poor in the majority of cases. Even when the rescus-
medical and laboratory examinations.
ciation is successful, patients have to overcome the sub-
Laboratory examinations provide reliable clues to most
sequent complication of anoxic/ischemic encephalopathy
of the causes of metabolic encephalopathies, and the fol-
during the next days or the next week. The reported re-
lowing determinations should be done: serum Na, K, Ca,
sults of recent studies suggest that therapeutic hypoter-
glucose, BUN, NH3, acid-base status and osmolality. It is
mia has a beneficial effect on the neurologic outcome in
important to remember that the brain may be damaged,
survivors10,11.
even irreversibly, by a disturbance of blood chemistry that
The main consequence of cardiac arrest is coma. If
is no longer present when the patient is first seen.
there is a state of complete unawareness and unresponsive-
On differential diagnosis it is necessary to consider
ness with abolition of all brainstem reflexes, and natural
vascular diseases of the brain including intracranial hem- respiration cannot be sustained, with no electrical activi-
orrhages, sinus venous thromboses, infectious or immuno- ty on electroencephalogram (EEG), but only cardiac ac-
logic diseases of the brain, brain tumors and other causes tion and blood pressure are maintained, the state is referred
of raised intracranial pressure, then malignant hyperther- to as brain death syndrome. Upon resuscitation patients
mia, malignant neuroleptic syndrome, acute adrenal fail- with stabilized breathing and cardiac activity may be pro-
ure and thyroid storm1,5. foundly comatose with the motionless and divergent eyes
but reactive pupils, the limbs inert and flaccid or rigid, and
Hypoxic/Anoxic and Ischemic Encephalopathy the tendon reflexes diminished. Generalized convulsions
and isolated or grouped myoclonic twitches may super-
The basic disorder is the lack of oxygen supply to the vene. If the damage is severe, coma persists, decerebrate
brain, which results from failure of the heart and circula- postures may be present or may occur in response to pain-
tion or of the lungs and respiration. The medical conditions ful stimuli, and there are bilateral Babinski signs and hy-
that most often lead to hypoxic/ischemic encephalopathy perthermia. Death may terminate this state or the indi-
are (1) myocardial infarction, ventricular arrhythmia, ex- vidual may survive for an indefinite period in persistent
ternal or internal hemorrhage, and septic or traumatic vegetative state12.
shock (in all of which cardiac function fails before that of Data derived from many large series show that six
respiration); (2) suffocation (from drowning, strangulation, months after cardiac arrest the estimated survival rate is
aspiration, compression of the trachea or tracheal obstruc- in the range between 11% and 22%. Sixty percent of pa-
tion); (3) carbon monoxide poisoning; (4) diseases that tients were found to have moderate to severe cognitive
paralyze the respiratory muscles (Guillain-Barr syndrome, deficits three months after cardiac arrest. One year later
myasthenia) or damage the central nervous system diffuse- about one half of the survivors still had moderate to severe
ly but the medulla specifically; and (5) general anesthe- neuropsychologic sequels that were thought to be perma-
sia, during which the patient is exposed to inspired gas that nent. These figures change with hypothermia applied af-
is oxygen-deficient. ter successful cardiac resuscitation in the field10,11.
Acta Clin Croat, Vol. 42, No. 4, 2003 353
Supanc V. et al. Metabolic encephalopathies
The main prognostic variables for poor outcome are the lism, short and medium chain fatty acids, mercaptans,
absence of pupillary light reflexes and the absence of motor phenols) and altered neurotransmission including false
responses to pain on day 3, bilateral absence of early corti- neurotransmitters and benzodiazepine-like substances3.
cal SSEP within the first week, existence of biochemical Recent observations indicate that the increased GABA-
markers (serum neuron-specific enolase and S-100 pro- ergic neurotransmission is due to the increased concentra-
tein), myoclonic status, and on EEG burst suppression tions of substances like benzodiazepines. They are pro-
pattern or the development of alpha-coma in deeply co- duced from bacterial metabolism in the gut, bypass the
matose patients13,14. The permanent neurologic sequels or liver and bind benzodiazepine receptors in the brain17.
posthypoxic syndrome observed most frequently include While the practicality of using benzodiazepine receptor
persistent coma or stupor, with a lesser degree of cerebral antagonists (e.g., flumazenil: single doses of 0.2-0.3 mg
injury, dementia with or without extrapyramidal signs, vi- given every 1-3 min for a total dose of 2 mg, or infusion of
sual agnosia, extrapyramidal syndrome with cognitive im- 2 mg in 15 min, or in continuing infusion 2 mg/h) in the
pairment, choreoathetosis, cerebellar ataxia, intention or treatment of hepatic encephalopathy remains to be deter-
action myoclonus, Korsakoff amnesic state and seizures1. mined, there is evidence that the administration of these
A relatively uncommon phenomenon is delayed post- drugs does result in transient awakening in many pa-
anoxic encephalopathy, where an initial improvement over tients18. Important predisposing factors for developing
1 to 4 weeks is followed by a relapse characterized by ap- encephalopathy include an excess of protein derived from
athy, confusion, irritability or agitation and mania. Most the diet or gastrointestinal hemorrhage; hypoxia, hypokale-
patients survive this second episode, but some are left with mia, metabolic alkalosis, electrolyte depletion, excessive
serious mental and motor disturbances. In others there is diuresis, use of sedative or hypnotic drugs, and constipa-
progression with weakness, shuffling gait, diffuse rigidity tion.
and spasticity, incontinence, coma and death after 1 to 2 EEG is a sensitive and reliable indicator of impending
weeks. Postmortem examination showed widespread ce- coma. The usual abnormality consists of paroxysms of bi-
rebral demyelination5. laterally synchronous slow or triphasic waves in the delta
Treatment of hypoxic-ischemic encephalopathy is di- range, which predominate frontally6,7.
rected mainly to the prevention of a critical degree of hy- In most patients, the syndrome does not evolve beyond
poxic injury. Once cardiac and pulmonary functions have the stage of mild mental drowsiness and confusion, with
been restored, there is experimental evidence that reduc-
ing cerebral metabolism by hypothermia and barbiturates Table 3. Stages of hepatic encephalopathy
may prevent the delayed worsening, however, controlled
trials outside cardiac arrest have failed to show neurologic I Slight confusion, decreased psychomotor activity
benefit, furthermore, hypotension resulting from barbitu- (occasional hyperactivity), inverted sleep pattern,
rates is itself detrimental. Oxygen may be of value during hypo/hypersomnia, short attention span, low percep-
the first hours but is probably of little use after the blood tion, impaired calculation, mood changes, anxiety/
has been well oxygenated. Corticosteroids may theoreti- apathy, coordination and handwriting disturbances,
cally help reduce brain swelling, but their use has not been tremor.
corroborated by clinical trials. Seizures should be controlled
II Drowsiness, slow response, poor memory, disorien-
by antiepileptic drugs but after a few hours seizures are re-
tation for time, inappropriate behavior, asterixis,
placed by myoclonus and clonazepam may be useful in
ataxia, dysarthria.
their control2,15.
III Stupor, confusion, delirium, paranoia, disorientation,
Hepatic Encephalopathy amnesia, perseveration, hyperventilation, nystagmus,
hyperreflexia, Babinski sign, rigidity, muscle twitch-
Hepatic encephalopathy is a consequence of liver func- ing, incontinence, possibly epileptic seizures.
tion disturbance and/or portal-systemic shunts. It is grad-
ed from I (slight) to IV (coma, unresponsive)16, as shown IV Coma, abnormal flexion or extension responses, brisk
in Table 3. oculocephalic responses, dilated pupils and sluggish
The pathophysiology of this extensively investigated responses to light. In the early stages of coma reac-
encephalopathy refers to neurotoxins (ammonia metabo- tion to painful stimuli, later unresponsive.
354 Acta Clin Croat, Vol. 42, No. 4, 2003
Supanc V. et al. Metabolic encephalopathies
asterixis and EEG changes. Hepatic coma evolves over a toms such as fluctuating disturbance of consciousness and
period of days to weeks and often terminates fatally or the agitation, but also with additional signs such as hyperpnea,
symptoms may regress completely or partially and then hyperreflexia, multifocal myoclonus, tremor, asterixis, brain
fluctuate in severity for several weeks or months. There is stem signs with different types of nystagmus, and muscle
a group of patients (many of them experience repeated tone abnormalities. A variety of involuntary motor phenom-
attacks of hepatic coma) in whom irreversible mild demen- ena, such as twitches, convulsions, fasciculations, arrhyth-
tia and a disorder of posture and movement gradually ap- mic tremor, myoclonus, chorea and asterixis, form a con-
pear; the condition is referred to as chronic hepatocerebral dition known as the uremic twitch-convulsive syndrome.
degeneration1,5. Confusion, disturbances of sensory perception, hallucina-
Hepatic encephalopathy due to fulminant hepatic fail- tions and delusions sometimes assume the form of toxic
ure is in most cases caused by viral hepatitis and acetami- psychosis with paradoxical reactions to sedative drugs22.
nophen poisoning. The main complications of fulminant As in other acute encephalopathies, EEG shows stag-
hepatic failure is cerebral edema, which is one of the ma- es of generalized slowing with an excess of delta and the-
jor causes of mortality (80% to 90% of patients die). Oth- ta waves within 48 hours of the onset of renal failure. The
er severe complications are epileptic seizures (caused by grade of slowing increases with increased serum creati-
hypoglycemia), bleeding from the upper gastrointestinal nine6.
tract, combination with renal dysfunction (hepatorenal The pathophysiology of uremic encephalopathy re-
syndrome), and concomitant respiratory alkalosis and hy- mains uncertain. Animal experiments have shown bio-
potension19,20. chemical changes in the brain, such as elevated level of
Treatment of hepatic encephalopathy means treat- parathyroid hormone and concomitant calcium content.
ment of liver disease. Few effective means of treating this Cerebral edema is notably absent. In fact computed to-
disorder include restriction of dietary protein, reducing mography (CT) scans and magnetic resonance imaging
bowel flora by oral administration of neomycin or kanamy- (MRI) often show cerebral shrinkage with chronic renal
cin, and the use of enemas (lactulose). The sustained use failure, likely due to hyperosmolality. Altered excretion of
of oral neomycin carries a risk of renal damage and ototox- drugs may lead to their accumulation and contribute to the
icity. Ultimately, in cases of intractable liver failure, trans- development of uremic encephalopathy. A state of twitch-
plantation becomes a treatment of last resort. Other meth- ing and convulsions in rats can be produced by the injec-
ods of treatment, the value of which still remains to be tion of urea alone. Uremia is frequently associated with
established, include the use of dopamine agonist (e.g., hypertension and a major problem arises in distinguishing
bromocriptine) and of keto-analogues of essential amino the cerebral effects of uremia per se from those of severe
acids. The keto-analogues should provide a nitrogen-free hypertension, a condition known as pseudouremia or hy-
source of essential amino acids and bromocriptin should pertensive encephalopathy22.
enhance dopaminergic transmission. The administration Complications of dialysis refer to dialysis disequilibri-
of branched-chain amino acids may result in considerable um syndrome, dialysis encephalopathy and Wernickes
improvement in mental status, but their effects have been encehalopathy. Dialysis disequilibrium syndrome is char-
variable and associated with an increased mortality1,5,21. acterized by headache, nausea, vomiting, blurred vision,
muscle twitching, hypertension, tremor, asterixis, multi-
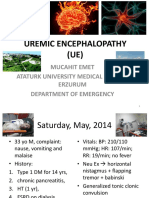
Renal Encephalopathies focal myoclonus, disorientation, and in severe cases psy-
chosis, stupor and coma. The symptoms tend to occur in
Diseases of the kidney such as glomerulonephritis, the third or fourth hour of dialysis and last for several hours.
pyelonephritis, interstitial nephropathies and arterioscle- Nowadays, it is believed that the symptoms should be
rotic diseases lead to uremia with the accumulation of toxic attributed to water intoxication due to inappropriate se-
substances causing encephalopathy. Clinical signs are quite cretion of antidiuretic hormone22. Progressive dialysis en-
clear, especially in acute renal failure which is mostly seen cephalopathy (dialysis dementia) is a subacute severe, fre-
in shock, by nephrotoxic agents, thrombotic thrombocyt- quently fatal neurologic disease characterized by speech
ic purpura, myoglobinuria and immunosuppressive treat- disturbances, involuntary motor phenomena, seizures and
ment. features of Alzheimers disease. The current view of its
Uremic encephalopathy presents like other encepha- pathogenesis is that it represents a form of aluminum in-
lopathies with changing expression of global cerebral symp- toxication. The aluminum may be derived from the dialy-
Acta Clin Croat, Vol. 42, No. 4, 2003 355
Supanc V. et al. Metabolic encephalopathies
sate or from orally administered aluminum gels. In recent to have diabetes, with current infection, enteritis, pancre-
years, the disorder has practically disappeared23,24. Wer- atitis or taking a drug known to upset diabetic control such
nicke-Korsakoff syndrome caused by thiamine depletion as thiazides, prednisone or phenytoin. Clinical features
has a classic triad of symptoms: mental symptoms (e.g., include seizures, focal neurologic deficits such as hemi-
global confusional state, disorientation in time and place, paresis or homonymous visual field defect. The mortality
Korsakoff amnesic state), ataxia and ocular abnormalities is high. Fluids should be replaced cautiously, using isotonic
(e.g., ophthalmoplegia with nystagmus and diplopia)25. saline and potassium, and correction of the markedly ele-
Treatment of uremic encephalopathy consists of dial- vated blood glucose requires relatively small amount of
ysis or renal transplantation. Improvement of symptoms insulin, since these patients often do not have insulin re-
may not be evident for a day or two after institution of sistance1,5.
dialysis. Convulsions often respond to relatively low dos-
es of anticonvulsants, but if there are associated metabol- Septic Encephalopathy
ic disturbances such as hyponatremia, the seizures may be
This encephalopathy has gained most interest in re-
difficult to control22.
cent years due to advances in the management of severe-
ly ill patients at intensive unit. Detection of its signs indi-
Encephalopathy with Hypoglycemia/ cates that the progressive basic disease has spread to the
Hyperglycemia nervous system. Multiorgan failure with and without sep-
When the level of blood glucose has declined to about sis is the leading cause of mortality in critical care account-
2.5 mmol/L, the initial symptoms occur, i.e. anxiety, hun- ing for 10% to 50% of deaths28. In sepsis, plasma and brain
amino acids are deranged with a decrease in branched chain
ger, sweating, headache, palpitation, vomiting, confusion,
amino acids and an increase in most neutral amino acids
drowsiness, and occasionally overactivity and bizarre be-
in the brain, similar to the findings in portasystemic en-
havior. In the next stage, motor restlessness, muscular
cephalopathy. Aromatic amino acid levels correlated with
spasms and decerebrate rigidity, convulsions and myoclo-
APACHE II scores and mortality. Scores and mortality rate
nus or focal neurologic deficits (e.g., hemiplegia) occur.
are higher in shock patients with higher levels of ammo-
Blood glucose levels of approximately 1.0 mmol/L are as-
nia and sulfur-containing amino acids29. This encephalop-
sociated with deep coma, dilatation of pupils, pale skin,
athy has become an important factor in surgery dealing
shallow respiration, slow pulse and hypotonia of limb
with sepsis. The principal clinical features are alterations
musculature. In this stage, injury to the brain may be ir-
in the level of consciousness and EEG changes. Since en-
reparable and recovery may be incomplete. The most com-
cephalogram is a sensitive index of brain function in sep-
mon causes of hypoglycemic encephalopathy are acciden-
tic encephalopathy, it would be useful to monitor suspect-
tal or deliberate overdose of insulin or an oral diabetic
ed patients with EEG as a predictor of the severity of en-
agent, insulin-secreting tumor of the pancreas, depletion
cephalopathy and associated mortality6,7.
of liver glycogen in prolonged alcoholic binge, starvation
or acute liver disease, and chronic renal insufficiency. Treat-
Conclusion
ment of all forms of hypoglycemia consists of immediate
correction of the hypoglycemia26,27. Metabolic encephalopathies represent a crucial prob-
Clinical features of diabetic acidosis consist of dehy- lem in severely ill patients. They may develop in the clin-
dration, fatigue, headache, abdominal pain, stupor, coma, ical course of deteriorating systemic disease as well as com-
Kussmaul type of breathing and often positive Babinski plications during treatment at critical care unit. Signs of
sign. Usually the condition has developed over a period of metabolic encephalopathy may be an early indication of
days in young diabetics with current infection and/or in- developing complications.
adequate insulin therapy. Treatment consists of prompt
administration of insulin and repletion of intravascular References
volume. In hyperosmolar nonketotic hyperglycemia the 1. WIJDICKS EFM. Neurology of critical illness. Philadelphia: F.A.
blood glucose is extremely high, over 40 mmol/L but ke- Davis, 1995.
toacidosis does not develop or is mild. There is also hemo- 2. MORRIS JC, FERENDELLI JA. Metabolic encephalopathy. In:
concentration and prerenal azotemia. Most of the patients PEARLMAN AL, COLLINS RC, eds. Neurobiology of disease.
are elderly diabetics, but some were not previously known New York: Oxford University Press, 1990;496-527.
356 Acta Clin Croat, Vol. 42, No. 4, 2003
Supanc V. et al. Metabolic encephalopathies
3. JONES EA. Pathogenesis of hepatic encephalopathy. Clin Liver Dis 17. MULLEN KD. Benzodiazepine compounds and hepatic encepha-
2000;4:467-85. lopathy. N Engl J Med 1991;325:509.
4. NORENBERG MD. The role of astrocytes in hepatic encephalop- 18. ALS-NIELSEN B, KJAERGARD LL, GLUND C. Benzodiazepine
athy. Neurochem Pathol 1987;6:13. receptor antagonists for acute and chronic hepatic encephalopathy.
5. HACKE W, ed. Neurocritical care. Berlin, Heidelberg, New York: Review. Cochrane Database Syst Rev 2001;4:CD002798. Review.
Springer, 1994. 19. BERNSTEIN D, TRIPODI J. Fulminant hepatic failure. Crit Care
6. MARKAND ON. Electroencephalogram in metabolic encephalopa- Clin 1998;14:181-97.
thies. Electroencephalogr Clin Neurophysiol Suppl 1999;50:301-10. 20. BASILE AS, HUGHES RD, HARRISON PM, et al. Elevated brain
7. YOUNG GB, McLACHLAN RS, KREEFT JH, DEMELO JD. An concentrations of 1,4-benzodiazepines in fulminant hepatic failure.
electroencephalographic classification for coma. Can J Neurol Sci N Engl J Med 1991;325:473.
1997;24:320-5. 21. NAYLOR CD, OROURKE K, DETSKY AS, BAKER, JP. Parenter-
8. KUNZE K. Metabolic encephalopathies. J Neurol 2002;249:1150-9. al nutrition with branched-chain amino acids in hepatic encephal-
opathy: a meta analysis. Gastroenterology 1989;97:1033.
9. MIYAMOTO O, AUER RN. Hypoxia, hyperoxia, ischemia and brain
necrosis. Neurology 2000;54:362-71. 22. FRASER CL, ARIEFF AJ. Metabolic encephalopathy as a compli-
cation of renal failure: mechanisms and mediators. New Horizons
10. BERNARD SA, GRAY TW, BUIST MD, JONES BM, SILVESTER
1994;2:518-26.
W, GUTTERIDGE G, SMITH K, et al. Treatment of comatose sur-
vivors of out-of hospital cardiac arrest with induced hypothermia. 23. ALFREY AC, LeGENDRE GR, KAEHNY WD. The dialysis en-
N Engl J Med 2002;346:557-63. cephalopathy syndrome. Possible aluminum intoxication. N Engl J
Med 1976;294:184-8.
11. The Hypothermia after Cardiac Arrest Study Group. Mild therapeu-
tic hypothermia to improve the neurologic outcome after cardiac 24. ROZAS VV, PORT FK. Progressive dialysis encephalopathy: preven-
arrest. N Engl J Med 2002;346:549-56. tion through control of aluminium levels in water. Ann Neurol
1979;6:88.
12. ROINE RO, KAJASTE S, KASTE M. Neuropsychologic sequelae
of cardiac arrest. JAMA 1993;269:237-42. 25. IHARA M, ITO T, YANAGIHARA C, NISHIMURA Y. Wernickes
encephalopathy associated with hemodialysis. Clin Neurol Neuro-
13. FOGEL W, KRIEGER D, VEITH M, et al. Serum neuron-specific
surg 1999;101:118-21.
enolase as early predictor of outcome after cardiac arrest. Crit Care
Med 1997;25:1133-8. 26. AUER RN. Progress review: hypoglycemic brain damage. Stroke
1986;17:699.
14. ROSEN H, ROSENGREN L, HERLITZ J, et al. Increased serum
levels of the S-100 protein are associated with hypoxic brain dam- 27. MALOUF R, BRUST JCM. Hypoglycemia: causes, neurological
age after cardiac arrest. Stroke 1988;29:473-477. manifestations, and outcome. Ann Neurol 1985;17:421.
15. WIJDICKS EFM, PARISI JE, SHARBROUGH FW. Prognostic val- 28. ZAUNER Ch, GENDO A, KRAMER L, et al. Metabolic encephal-
ue of myoclonus status in comatose survivors of cardiac arrest. Ann opathy in critical ill patients suffering from septic or nonseptic
Neurol 1994;35:239-43. multiple organ failure. Crit care Med 2000;28:1310-5.
16. WEISSENBORN K, MARSANO S, DIEHL AM, KUNZE K. He- 29. SPRUNG ChL, CERRA FB, FREUND HR, et al. Amino acid alter-
patic coma. In: HACKE W, ed. Neurocritical care. Berlin, Heidel- ations and encephalopathy in the sepsis syndrome. Crit Care Med
berg, New York: Springer, 1994;253-6. 1991;19:753-7.
Saetak
METABOLIKE ENCEFALOPATIJE
V. Supanc, V. Vargek-Solter i V. Demarin
Metabolike encefalopatije su znaajne komplikacije koje se javljaju u mnogih bolesnika lijeenih u jedinicima intenzivnog
lijeenja. Termin metabolike encefalopatije odnosi se na irok spektar poremeaja funkcije mozga za vrijeme teke, kritine
bolesti. U ovom lanku prikazani su neuroloki simptomi, mogunosti dijagnostikih metoda, kao i etiologija, patofiziologija te
terapija metabolikih encefalopatija. Metabolike encefalopatije su u svojoj osnovi multifaktorijalne, a prepoznavanje njihovih
simptoma ima vanu ulogu u ranom otkrivanju zatajivanja organskih sustava za vrijeme pogoravanja osnovne bolesti.
Kljune rijei: Bolesti mozga metabolike, dijagnostika; Bolesti mozga metabolike, fiziopatologija; Kritina skrb; ok septiki, dijagnostika;
ok septiki, fiziopatologija; Vieorgansko zatajenje, dijagnostika
Acta Clin Croat, Vol. 42, No. 4, 2003 357
View publication stats
Das könnte Ihnen auch gefallen
- Neurology Multiple Choice Questions With Explanations: Volume IVon EverandNeurology Multiple Choice Questions With Explanations: Volume IBewertung: 4 von 5 Sternen4/5 (7)
- Metabolic Encephalopathies: Ens Teaching ReviewDokument12 SeitenMetabolic Encephalopathies: Ens Teaching ReviewSiska AnjelinaNoch keine Bewertungen
- Neurology Multiple Choice Questions With Explanations: Volume IIIVon EverandNeurology Multiple Choice Questions With Explanations: Volume IIIBewertung: 4.5 von 5 Sternen4.5/5 (6)
- Metabolic Encephalopathy and Metabolic ComaDokument14 SeitenMetabolic Encephalopathy and Metabolic ComaqlinlynNoch keine Bewertungen
- Topics in Behavioral Neurology and Neuropsychology: With Key ReferencesVon EverandTopics in Behavioral Neurology and Neuropsychology: With Key ReferencesNoch keine Bewertungen
- Metabolic Encephalopathy: Behind The Name: TerminologyDokument3 SeitenMetabolic Encephalopathy: Behind The Name: TerminologyKARINA ORMACHEANoch keine Bewertungen
- Hypocalcemia - Diagnosis and Treatment - Endotext - NCBI BookshelfDokument31 SeitenHypocalcemia - Diagnosis and Treatment - Endotext - NCBI Bookshelfgalnaresdaniela7Noch keine Bewertungen
- Uremic EnchepalopathyDokument5 SeitenUremic Enchepalopathyafdhalul mahfudNoch keine Bewertungen
- Discoveries 08 110Dokument19 SeitenDiscoveries 08 110Riki AntoNoch keine Bewertungen
- Uremic Encephalopathy and Other Brain Disorders Associated With Renal FailureDokument5 SeitenUremic Encephalopathy and Other Brain Disorders Associated With Renal FailuresrikandhihasanNoch keine Bewertungen
- MR 6 ComaDokument8 SeitenMR 6 ComaShruti JestineNoch keine Bewertungen
- Uremic EncephalophatyDokument48 SeitenUremic EncephalophatySindi LadayaNoch keine Bewertungen
- Spektro Uv VisDokument7 SeitenSpektro Uv VisNadaNoch keine Bewertungen
- Special Neurology - Second Edition RevisedDokument115 SeitenSpecial Neurology - Second Edition RevisedAimee100% (1)
- Special NeurologyDokument115 SeitenSpecial NeurologyUbaidillah Romadlon AlfairuziNoch keine Bewertungen
- Convulsion Febril PediatricsDokument11 SeitenConvulsion Febril PediatricsOrlando HernandezNoch keine Bewertungen
- Neurologic Diseases of RuminantsDokument6 SeitenNeurologic Diseases of Ruminantsh8tcsfmmndNoch keine Bewertungen
- Pathophysiology and Treatment of MyoclonusDokument21 SeitenPathophysiology and Treatment of MyoclonusVincentius Michael WilliantoNoch keine Bewertungen
- Mahoney 1982Dokument13 SeitenMahoney 1982Aji DwijayantoNoch keine Bewertungen
- Metabolic EncephalopathiesDokument10 SeitenMetabolic EncephalopathiesSrinath M VNoch keine Bewertungen
- Epilepsy in Mitochondrial DisordersDokument6 SeitenEpilepsy in Mitochondrial Disordersana maria ruizNoch keine Bewertungen
- Toxic and Metabolic Encephalopathies: Chapter OutlineDokument18 SeitenToxic and Metabolic Encephalopathies: Chapter OutlinekhusnulNoch keine Bewertungen
- Seifter 2010Dokument5 SeitenSeifter 2010vidianka rembulanNoch keine Bewertungen
- 2 - Debilidad AgudaDokument15 Seiten2 - Debilidad AgudaMarian ZeaNoch keine Bewertungen
- Degenerative DiseasesDokument29 SeitenDegenerative DiseasesAwang WibisonoNoch keine Bewertungen
- Wernicke Korsakoff SyndromeDokument19 SeitenWernicke Korsakoff Syndrometerry2wa100% (4)
- II-E Altered PerceptionDokument16 SeitenII-E Altered PerceptionDharylle CariñoNoch keine Bewertungen
- CNS ST 6 CDokument13 SeitenCNS ST 6 CEuiJinMoonNoch keine Bewertungen
- 2-WS Geriatri-Dr Rensa2Dokument44 Seiten2-WS Geriatri-Dr Rensa2Yuni RochyaningsihNoch keine Bewertungen
- Epilepsy: Head TraumaDokument17 SeitenEpilepsy: Head TraumaAimanRiddleNoch keine Bewertungen
- B5W1L9.Peripheral Neuropathy - Lecture Notes 12Dokument4 SeitenB5W1L9.Peripheral Neuropathy - Lecture Notes 12mihalcea alinNoch keine Bewertungen
- Cerebrovascular AccidentDokument59 SeitenCerebrovascular AccidentSiwani raiNoch keine Bewertungen
- Clinical and Neuropathological Criteria For Frontotemporal DementiaDokument3 SeitenClinical and Neuropathological Criteria For Frontotemporal DementiaSandra MilenaNoch keine Bewertungen
- Indicator of Dyscirculatory Encephalopathy in HypothyroidismDokument4 SeitenIndicator of Dyscirculatory Encephalopathy in HypothyroidismresearchparksNoch keine Bewertungen
- Neuromusculo Skeletal: Dr. Jumraini Tammasse, SpsDokument46 SeitenNeuromusculo Skeletal: Dr. Jumraini Tammasse, SpsFareez HairiNoch keine Bewertungen
- Overview of The Hereditary Ataxias - UpToDateDokument15 SeitenOverview of The Hereditary Ataxias - UpToDatericanoy191Noch keine Bewertungen
- Dyscirculatory Encephalopathy: Principles of Treatment: P.F. BoymamatovaDokument5 SeitenDyscirculatory Encephalopathy: Principles of Treatment: P.F. Boymamatovasrushtideokar0537Noch keine Bewertungen
- Hypoxia Ischemic Encephalopathy and Congenital AnomaliesDokument36 SeitenHypoxia Ischemic Encephalopathy and Congenital AnomaliesVarna MohanNoch keine Bewertungen
- Hepatic EncephalopathyDokument9 SeitenHepatic EncephalopathyMelchor Alcántara BarreraNoch keine Bewertungen
- Peripheral Neuropathy: By: R'Syah ESI NeurologistDokument39 SeitenPeripheral Neuropathy: By: R'Syah ESI Neurologistraynhard b. fandres100% (2)
- Inbornerrorsofmetabolism Withmovementdisorders: Defects in Metal Transport and Neurotransmitter MetabolismDokument15 SeitenInbornerrorsofmetabolism Withmovementdisorders: Defects in Metal Transport and Neurotransmitter MetabolismVadiga Ramana KumarNoch keine Bewertungen
- Metabolic Encephalopaty PDFDokument46 SeitenMetabolic Encephalopaty PDFRez QNoch keine Bewertungen
- Keywords: Encephalopathy, Intensive Care, Metabolic Disorders Key MessageDokument6 SeitenKeywords: Encephalopathy, Intensive Care, Metabolic Disorders Key MessageElena DocNoch keine Bewertungen
- Neurology & Systemic DiseaseDokument313 SeitenNeurology & Systemic DiseaseAlphaNoch keine Bewertungen
- Hie 200213194802Dokument63 SeitenHie 200213194802Thea DinoNoch keine Bewertungen
- 28sici 291096 9136 28199802 2915 3A2 3C97 3A 3aaid Dia523 3e3.0.co 3B2 5 PDFDokument16 Seiten28sici 291096 9136 28199802 2915 3A2 3C97 3A 3aaid Dia523 3e3.0.co 3B2 5 PDFHesbon MomanyiNoch keine Bewertungen
- Epileptic Seizures As The First Manifestation of Fahr's SyndromeDokument5 SeitenEpileptic Seizures As The First Manifestation of Fahr's Syndromejanfk2000Noch keine Bewertungen
- What Is NeurodegenerationDokument8 SeitenWhat Is NeurodegenerationJuan Castaño CastroNoch keine Bewertungen
- VEM5384 Clincial Neurology DisordersDokument62 SeitenVEM5384 Clincial Neurology DisordersdeadnarwhalNoch keine Bewertungen
- Evaluation and Management of Autonomic Nervous System DisordersDokument10 SeitenEvaluation and Management of Autonomic Nervous System DisordersbpppbbNoch keine Bewertungen
- ATAXIAS PTDokument13 SeitenATAXIAS PTKarunya VkNoch keine Bewertungen
- Card EncephDokument6 SeitenCard EncephKota AnuroopNoch keine Bewertungen
- Cognitive Disorders: P.Tembo Mental HealthDokument17 SeitenCognitive Disorders: P.Tembo Mental HealthGift MwapeNoch keine Bewertungen
- 10.1007@s42399 021 01027 7Dokument9 Seiten10.1007@s42399 021 01027 7firstia anugerah1Noch keine Bewertungen
- PRES (Posterior Reversible Encephalopathy Syndrome) and Eclampsia-ReviewDokument5 SeitenPRES (Posterior Reversible Encephalopathy Syndrome) and Eclampsia-ReviewAvicena M IqbalNoch keine Bewertungen
- Chapter 426 - Seizures and Epilepsy: Susan S. SpencerDokument35 SeitenChapter 426 - Seizures and Epilepsy: Susan S. Spencerenriquelima19Noch keine Bewertungen
- PG 15 40720Dokument5 SeitenPG 15 40720fani rudiyantiNoch keine Bewertungen
- Algoritmo Diagnostico de La Ceguera Monocular en Una Paciente Con NeurosarcoidosisDokument8 SeitenAlgoritmo Diagnostico de La Ceguera Monocular en Una Paciente Con NeurosarcoidosisFarid Santiago Abedrabbo LombeydaNoch keine Bewertungen
- Ensefalopati Uremikum Bu YantiDokument16 SeitenEnsefalopati Uremikum Bu YantiAnggi SetyariniNoch keine Bewertungen
- Guarin, Consuelito Danzelle G. PHARM 1-C 0994 Pathophysiology of Nervous SystemDokument9 SeitenGuarin, Consuelito Danzelle G. PHARM 1-C 0994 Pathophysiology of Nervous SystemChelito GuarinNoch keine Bewertungen
- Ciritical Appraisal Therapy StudyDokument3 SeitenCiritical Appraisal Therapy StudyDiana AstriaNoch keine Bewertungen
- Transnasal Approach: A Case Report. Journal of Medical Case Report. 3: 7317Dokument2 SeitenTransnasal Approach: A Case Report. Journal of Medical Case Report. 3: 7317fkiaNoch keine Bewertungen
- Cover LetterDokument2 SeitenCover LetterfkiaNoch keine Bewertungen
- NO Medrec Nama Pasien TGL Keluar Pasien: Rupi SaroniDokument1 SeiteNO Medrec Nama Pasien TGL Keluar Pasien: Rupi SaronifkiaNoch keine Bewertungen
- Daftar PustakaDokument2 SeitenDaftar PustakafkiaNoch keine Bewertungen
- The Prevention and Management of Pressure UlcerDokument5 SeitenThe Prevention and Management of Pressure UlcerrantiNoch keine Bewertungen
- LogbookDokument9 SeitenLogbookforriskyguyNoch keine Bewertungen
- Neonatal Ventilation - Neocon 2017-2Dokument156 SeitenNeonatal Ventilation - Neocon 2017-2RAM SOFTWARE100% (2)
- Zinc and Copper Levels in Preeclampsia: A Study From Coastal South IndiaDokument4 SeitenZinc and Copper Levels in Preeclampsia: A Study From Coastal South IndiaIriawan Indra PutraNoch keine Bewertungen
- Lecture-25 Cesarean SectionDokument21 SeitenLecture-25 Cesarean SectionMadhu Sudhan PandeyaNoch keine Bewertungen
- Farmacist Desk Reference ReviewDokument1 SeiteFarmacist Desk Reference ReviewThinh DoNoch keine Bewertungen
- The Cost Conundrum in HealthcareDokument8 SeitenThe Cost Conundrum in HealthcarePaul SchumannNoch keine Bewertungen
- Discharge Planning PaperDokument4 SeitenDischarge Planning Paperapi-338998736Noch keine Bewertungen
- Dengue Hemorrhagic FeverDokument12 SeitenDengue Hemorrhagic FeverzeeNoch keine Bewertungen
- A SphygmomanometerDokument3 SeitenA Sphygmomanometerdeepesh288Noch keine Bewertungen
- Final Exam Assignment PERIODokument4 SeitenFinal Exam Assignment PERIOيارا حسينNoch keine Bewertungen
- Use of Alternative Medicine To Manage Pain: (CITATION Har16 /L 1033)Dokument6 SeitenUse of Alternative Medicine To Manage Pain: (CITATION Har16 /L 1033)Syed Muhammad Baqir RazaNoch keine Bewertungen
- Gonorrhea Case StudyDokument2 SeitenGonorrhea Case StudyDonna LLerandi100% (1)
- Denpasar Festival 2021Dokument4 SeitenDenpasar Festival 2021Ery CorniawatiNoch keine Bewertungen
- Carcinoma of Breast Case SheetDokument7 SeitenCarcinoma of Breast Case SheetHanisha VasireddyNoch keine Bewertungen
- CIA Principles of Management: Responsibilities and Responsiveness of An Organization (Serum Institute of India)Dokument20 SeitenCIA Principles of Management: Responsibilities and Responsiveness of An Organization (Serum Institute of India)Tanmay JainNoch keine Bewertungen
- Penjagaan Pensiun Dan RealisasinyaDokument11 SeitenPenjagaan Pensiun Dan RealisasinyasidoharjoNoch keine Bewertungen
- Catheterisation - Suprapubic Catheter ProcedureNewDokument12 SeitenCatheterisation - Suprapubic Catheter ProcedureNewAmit KapuriaNoch keine Bewertungen
- BONE Level 2-BDokument60 SeitenBONE Level 2-Bjefri banjarnahorNoch keine Bewertungen
- Value of A Community-Based Medication ManagementDokument12 SeitenValue of A Community-Based Medication ManagementGetrudeNoch keine Bewertungen
- Introduction RHDDokument5 SeitenIntroduction RHDapriellejoyjovenaNoch keine Bewertungen
- RCP OnpatroDokument14 SeitenRCP OnpatroMihaela BerindeieNoch keine Bewertungen
- NSTP Act2 Suan, Allyna ChantalDokument8 SeitenNSTP Act2 Suan, Allyna ChantalChan TalNoch keine Bewertungen
- Tesis StuntingDokument2 SeitenTesis StuntingLentri Fitri MulyaniNoch keine Bewertungen
- Communication Interaction in ICU-Patient and Staff Experiences and Perceptions.Dokument5 SeitenCommunication Interaction in ICU-Patient and Staff Experiences and Perceptions.osondoarNoch keine Bewertungen
- Hypertension in Pregnancy PDFDokument397 SeitenHypertension in Pregnancy PDFMary PrietoNoch keine Bewertungen
- Skilled Birth Attendant PostersDokument16 SeitenSkilled Birth Attendant PostersPrabir Kumar Chatterjee100% (1)
- Median Rhomboid GlossitisDokument4 SeitenMedian Rhomboid GlossitisYeltserNoch keine Bewertungen
- HMOLEDokument12 SeitenHMOLEHermie Joy MaglaquiNoch keine Bewertungen
- MED 251 Block 9 PHL Brochure and TarpDokument6 SeitenMED 251 Block 9 PHL Brochure and TarpFerdinand Sta Ana Jr.Noch keine Bewertungen
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (404)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDVon EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDBewertung: 5 von 5 Sternen5/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (29)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBewertung: 2 von 5 Sternen2/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossVon EverandThe Obesity Code: Unlocking the Secrets of Weight LossBewertung: 4 von 5 Sternen4/5 (6)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Von EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Bewertung: 3 von 5 Sternen3/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisVon EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 5 von 5 Sternen5/5 (81)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- The Comfort of Crows: A Backyard YearVon EverandThe Comfort of Crows: A Backyard YearBewertung: 4.5 von 5 Sternen4.5/5 (23)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Von EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Bewertung: 4.5 von 5 Sternen4.5/5 (110)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsVon EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsBewertung: 5 von 5 Sternen5/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessVon EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessBewertung: 4.5 von 5 Sternen4.5/5 (328)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaVon EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- To Explain the World: The Discovery of Modern ScienceVon EverandTo Explain the World: The Discovery of Modern ScienceBewertung: 3.5 von 5 Sternen3.5/5 (51)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 4 von 5 Sternen4/5 (5)
- Troubled: A Memoir of Foster Care, Family, and Social ClassVon EverandTroubled: A Memoir of Foster Care, Family, and Social ClassBewertung: 4.5 von 5 Sternen4.5/5 (27)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeVon EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeBewertung: 4.5 von 5 Sternen4.5/5 (253)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisVon EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisBewertung: 4 von 5 Sternen4/5 (1)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisVon EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisBewertung: 3.5 von 5 Sternen3.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsVon EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsBewertung: 4 von 5 Sternen4/5 (4)
- The Marshmallow Test: Mastering Self-ControlVon EverandThe Marshmallow Test: Mastering Self-ControlBewertung: 4.5 von 5 Sternen4.5/5 (59)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsVon EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsBewertung: 4.5 von 5 Sternen4.5/5 (170)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryVon EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryBewertung: 4 von 5 Sternen4/5 (45)