Beruflich Dokumente
Kultur Dokumente
Chapter 53 Management of Mineral and Bone Disorders in Chronic Kidney Disease Patients 2015 Chronic Renal Disease
Hochgeladen von
Maria MihailovCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Chapter 53 Management of Mineral and Bone Disorders in Chronic Kidney Disease Patients 2015 Chronic Renal Disease
Hochgeladen von
Maria MihailovCopyright:
Verfügbare Formate
C H A P T E R
53
Management of Mineral and Bone
Disorders in Chronic Kidney Disease
Patients
Kristen L. Jablonski and Michel Chonchol
Division of Renal Diseases and Hypertension, University of Colorado Denver Anschutz
Medical Campus, Aurora, CO, USA
SCOPE OF THE PROBLEM AND PUBLIC However, much is still unknown, and there is an over-
HEALTH IMPLICATIONS all lack of large randomized controlled trials provid-
ing direction for clinical practice. The major basis of
With declining kidney function, mineral homeostasis the recommendations in this chapter are the KDIGO
becomes progressively deregulated, including alterations CKD-MBD guidelines released in 2009,1 with select
in serum concentrations of calcium, phosphorus, intact updates included in the 2013 KDIGO guideline on
parathyroid hormone (iPTH) and fibroblast growth fac- the Evaluation and Management of Chronic Kidney
tor-23 (FGF-23).1 These biochemical abnormalities are Disease.4 The recommendations of the National Kidney
tightly associated with cardiovascular mineralization Foundations Kidney Disease Outcomes Quality
and paradoxical skeletal demineralization (Figure 53.1).2 Initiative (KDOQI), released in 2010 to adapt the 2009
In 2005, Kidney Disease: Improving Global Outcomes KDIGO guidelines for use in the US,5 are consistent
(KDIGO), an international organization with the mission with the KDIGO guidelines, except where noted.
of developing clinical practice guidelines in CKD, for-
mally classified this clinical syndrome as Chronic Kidney
Disease-Mineral and Bone Disorder (CKD-MBD).3 This PATHOPHYSIOLOGY
terminology replaced renal osteodystrophy in order to
better describe the broader consequences of CKD com- Biochemical and hormonal abnormalities affect cal-
plications on mineral metabolism, bone and the cardio- cium, phosphorus, vitamin D, iPTH and FGF-23 metabo-
vascular system.1 The term renal osteodystrophy is now lism and handling, and bone and vascular calcification
restricted specifically to the alterations in bone morphol- alterations occur in patients with CKD-MBD.
ogy or pathology that can result from complications of
CKD, as CKD-MBD better reflects the systemic conse-
Calcium
quences of kidney disease, beyond bone alone.1
CKD-MBD is a common complication in CKD, CKD is characterized by moderate hypocalcemia,
occurs early in the disease, and both persists and pro- although calcium remains relatively stable in most
gresses across all stages of CKD.1 The interactions patients with non-dialysis-dependent CKD (Figure
between abnormal mineral metabolism, extraskel- 53.2).6,7 The mechanisms associated with the develop-
etal calcification and skeletal demineralization may ment of modest hypocalcemia in CKD patients are multi-
increase morbidity and mortality in patients with factorial, but include decreased intestinal absorption and
CKD.4 Thus, management of CKD-MBD may influence reduced 1,25 dihydroxyvitamin D3 (1,25(OH)2D3) levels
important clinical outcomes in this patient population. (Figure 53.3).8 An additional concern in patients with
P. Kimmel & M. Rosenberg (Eds): Chronic Renal Disease.
DOI: http://dx.doi.org/10.1016/B978-0-12-411602-3.00053-6 646 2015 Elsevier Inc. All rights reserved.
2012
Pathophysiology 647
Biochemical CKD, particularly those requiring dialysis, is increased
abnormalities S[Ca] resulting from pharmacological agents such as
calcium-based phosphate binders. However, there are
currently no data to support an increased risk of either
fracture or mortality with increasing S[Ca] in patients
with stage 3 to 5 CKD,1 although observational stud-
ies suggest that hypercalcemia may increase the relative
CKD-MBD risk of mortality in dialysis-dependent CKD.911 Based on
meta-analysis in the general population, calcium supple-
ments may increase the risk of cardiovascular events.12
Skeletal Cardiovascular Although the applicability to patients with CKD is
demineralization mineralization
unclear, this is biologically plausible.
FIGURE 53.1 Components of chronic kidney disease-mineral and
bone disorder (CKD-MBD). The clinical syndrome CKD-MBD was
formally classified by Kidney Disease: Improving Global Outcomes Phosphorus
(KDIGO) in 2005 to reflect the adverse consequences of CKD compli-
cations on mineral metabolism, skeletal demineralization and para-
In CKD stages 35, S[P] remains normal until eGFR
doxical extraskeletal cardiovascular mineralization. falls below 40mL/min/1.73m2 and is still relatively stable
until eGFR is <20mL/min/1.73m2 6,7 (Figure 53.2). S[P] is
(a) 100
90 Hyperphosphatemia, serum phosphate 4.6 mg/dl
80 Secondary hyperparathyroidism, PTH 65 pg/ml
70 FGF23 excess, FGF23 100 RU/ml
% of population
60
50
40
30
20
10
0
<20 2029 3039 4049 5059 6069 70
Estimated glomerular filtration rate, ml/min per 1.73 m2
(b) Median values of 1,25 dihydroxyvitamin D, (c) Median values of serum calcium, phosphorus,
25 hydroxyvitamin D, and intact PTH by GFR levels and intact PTH by GFR levels
50 1,25 Dihydroxyvitamin D3 (pg/ml) 150 45
Serum calcium (mg/dl) 150
45 25 Hydroxyvitamin D (ng/ml) 40 Serum phosphorus (mg/dl)
1,25 dihydroxyvitamin D (pg/ml),
Intact PTH (pg/ml) Intact PTH (mg/dl)
25 hydroxyvitamin D (ng/ml)
40 35
Serum calcium (mg/dl),
Intact PTH (pg/ml)
phosphorus (mg/dl)
35
Intact PTH (pg/ml)
100 30
100
30
25
25
20
20
50 15 50
15
10 10
5 5
0 0 0 0
>80 7970 6960 5950 4940 3930 2920 <20 >80 7970 6960 5950 4940 3930 2920 <20
GFR level (ml/min) GFR level (ml/min)
FIGURE 53.2 Alterations in biochemical and hormonal parameters with declining GFR in CKD. One of the earliest detectable changes in CKD-
MBD is rising fibroblast growth factor-23 (FGF-23) levels, which increases when GFR is approximately 70mL/min/1.73m2 and progressively rises
further as eGFR continues to decline (Panel A, right bars. Left bars indicate hyperphosphatemia; middle bars indicate secondary hyperparathyroid-
ism). Increasing FGF-23 contributes to a decline in calcitriol (1,25 dihydroxyvitamin D3) levels by inhibiting 1-hydroxylase activity and stimulating
24-hydroxylase, which is responsible for the degradation of calcitriol (Panel B). Intact parathyroid hormone (iPTH) also rises as GFR declines, although
not in a significant way until GFR falls below 45mL/min/1.73m2 (Panels B and C). In contrast, S[Ca] remains relatively stable in most patients with
non-dialysis-dependent CKD (Panel C). S[P] remains normal until GFR falls below 40mL/min/1.73m2 and is still relatively stable until GFR is
<20mL/min/1.73m2 (Panels A and C). Reprinted by permission from Macmillan Publishers Ltd: [Kidney International] (6), copyright (2011) [Panel A] and
Macmillan Publishers Ltd: [Kidney International] (13), copyright (2007) [Panels B and C].
VIII. THERAPEUTIC CONSIDERATIONS
648 53. Management of Mineral and Bone Disorders in Chronic Kidney Disease Patients
(Figure 53.2). Classic teaching was that the decline in
1,25(OH)2D3 was the result of loss of nephron mass.
PTH secretion
It is now known that increases in serum FGF-23 in
the early stages of kidney disease is also an important
contributor by inhibiting 1-hydroxylase activity and
stimulating 24-hydroxylase, which is responsible for the
Calcium FGF-23
absorption degradation of 1,25(OH)2D323 (Figure 53.3).
production
Several observational studies have shown inverse
associations between vitamin D metabolites and adverse
Phosphorus outcomes in patients with CKD, as well as in the general
retention
population. Low serum 25(OH)D3 level is independently
1,25(OH)2D
associated with all-cause mortality in both non-dialysis-
production and dialysis-dependent CKD patients,24,25 and in the
general population.26,27,28 1,25(OH)2D3 levels are also
FIGURE 53.3 Biochemical and hormonal abnormalities in CKD- inversely associated with mortality in non-dialysis-
MBD. In CKD-MBD, production of fibroblast growth factor-23 (FGF- dependent CKD patients. Low serum 25(OH)D3 and/or
23), the principal regulating hormone of phosphorus, is elevated
to counter a rise in S[P]. FGF-23 also inhibits synthesis of 1,25 dihy-
1,25(OH)2D3 are also independently associated with car-
droxyvitamin D3 (1,25(OH)2D3), by decreasing renal 1-hydroxyase diovascular events and mortality in individuals with24
expression and increasing 24-hydroxylase expression. FGF-23 also and without CKD.26,28,29 In addition, both 1,25(OH)2D330
initially suppresses parathyroid hormone (PTH) release and secre- and 25(OH)D327 levels are inversely associated with kid-
tion, although the parathyroid glands may become resistant and the ney disease progression, and low 25(OH)D3 is associated
relationship may change with advancing kidney disease. PTH release
and secretion also increase in response to hypocalcemia, hyperphos-
with increased risk of coronary artery disease progres-
phatemia and/or decreased 1,25(OH)2D3. Both decreased intestinal sion in the general population.31
absorption of calcium and reduced 1,25(OH)2D3 levels contribute to
the development of modest hypocalcemia.
Parathyroid Hormone
maintained within the normal laboratory range until later
Under physiological circumstances, PTH maintains
stages of CKD mainly by FGF-23, which increases phos-
S[Ca], increases phosphate excretion, and stimulates pro-
phate excretion to maintain normal S[P].13 Increased S[P]
duction of 1,25(OH)2D3. Production increases in response
is a stimulus for secondary hyperparathyroidism1 and a
to hypocalcemia, hyperphosphatemia and/or decreased
mediator of vascular calcification.14
1,25(OH)2D3 (Figure 53.3).1 FGF-23 can also suppress
Observational studies support that even in the nor-
PTH, although the parathyroid glands may become resis-
mal range, increased S[P] is associated with increased
tant and the relationship may change with advancing
risk of all-cause mortality in patients without CKD,15,16
kidney disease.23,32
non-dialysis-dependent CKD,17,18 as well as consistently
iPTH rises as GFR declines, although not in a signifi-
in patients treated with chronic dialysis.18,19 In addition,
cant way until eGFR falls below 45mL/min/1.73m2 6
increased S[P] that is still in the normal range is also
(Figure 53.2). This is initially an adaptive response to
associated with increased prevalence of vascular and val-
maintain calcium, phosphorus, and 1,25(OH)2D3 homeo-
vular calcification in patients with CKD.20
stasis.1 Decreased S[Ca] was once thought to be central in
the development of secondary hyperparathyroidism. It is
now accepted that FGF-23 is a key player in this process,
Vitamin D
initially inhibiting PTH, although this is compromised as
25-hydroxyvitamin D (25(OH)D3; calcidiol) is con- CKD progresses.13
sidered the best measure of vitamin D nutritional status Most observational evidence on the relationship
because of its long half-life in the circulation of approxi- between PTH and clinical outcomes was generated from
mately 3 weeks. 25(OH)D3 is converted in the kidney chronic HD patients. When iPTH is elevated beyond an
by 1-hydroxylase to 1,25(OH)2D3 (calcitriol), the active inflection point ranging from 480 to 600pg/mL,10,33,34
form of vitamin D, although extrarenal conversion can there is an increased mortality risk, but this finding is
also occur.1 1,25(OH)2D3 is an important regulator of not consistent and the relationship may be U-shaped,
mineral homeostasis and musculoskeletal function, in inverse, or non-significant.35,36,37 Increased iPTH may
addition to having pleiotropic extracellular effects. also be associated with risk of cardiovascular events in
Most patients with CKD have low levels of this population.1 In general, iPTH fails to correlate with
1,25(OH)2D3.1,21 This decline occurs early in the dis- fracture risk, and the relationship of PTH levels with
ease, and the severity increases as CKD progresses6,22 bone formation rates vary greatly.1
VIII. THERAPEUTIC CONSIDERATIONS
Diagnosis 649
FGF-23 A systematic review of bone biopsies in patients
with CKD stages 3 to 5 showed 32% had osteitis fibrosa
FGF-23 was first identified in 2000,38 and the dis- (increased turnover and normal mineralization), 18%
covery has led to a re-consideration of the mechanisms adynamic (decreased turnover and acellularity), 16%
driving secondary hyperparathyroidism.13 FGF-23 is were normal, 8% had osteomalacia (decreased turnover
secreted by skeletal osteocytes in response to changes and abnormal mineralization), and 20% had mixed dis-
in bone formation and S[P] (Figure 53.3). However, the ease (increased turnover with abnormal mineralization).1
mechanisms underlying the direct regulation of FGF-23 Alterations in bone are important, as this can lead
production are largely unknown.39 FGF-23 is the princi- to increased bone fragility and fracture. Hip fractures
pal regulating hormone of phosphorus, and also inhibits are 2 to 3 times more common in elderly patients with
synthesis of 1,25(OH)2D3 and suppresses PTH, at least stage 3 to 4 CKD.1 Although the risk in early stage CKD
initially.23,32 These functions are accomplished by reduc- is unclear, chronic dialysis patients with adynamic bone
ing the activity and/or expression of sodium-phosphate disease and/or osteomalacia have an increased risk of
co-transporters, possibly reducing intestinal phosphate fracture.50,51
absorption, decreasing renal 1-hydroxyase expres-
sion, and increasing 24-hydroxylase expression absorp-
tion.23,32 FGF-23 acts by binding to receptors that are Vascular Calcification
part of the tyrosine kinase superfamily40 in the presence
Extraskeletal calcification of the vasculature increases
of the membrane-bound co-receptor klotho,32 but animal
progressively with declining eGFR, and is more preva-
studies support that FGF-23 can also act independently
lent, severe, and accelerated in CKD compared to the
of klotho, at least in the heart.41
general population.14 Calcification can occur in both the
Increasing FGF-23 levels may be one of the earli-
intimal and medial layers of the vasculature, but medial
est detectable changes in CKD-MBD. FGF-23 levels
calcification is considered the more common and major
begin to increase when eGFR is approximately 70mL/
form of calcification in CKD.52 Medial calcification is
min/1.73m2, and progressively rise as eGFR declines
characterized by diffuse mineral deposition through-
further (Figure 53.2).13,42 Small elevations in FGF-23
out the vascular tree53 and is associated with increased
are initially required, as this increases renal phosphate
large-elastic artery stiffness. This promotes increased
excretion, thus maintaining S[P] within normal limits.
systolic blood pressure, reduced diastolic blood pressure,
With CKD progression, circulating FGF-23 levels con-
increased cardiac afterload, compromised perfusion of
tinue to rise, the phosphaturic response declines, and
the coronary arteries and left ventricular remodeling.54,55
eventually S[P] is increased. It is presently unknown
Accordingly, vascular calcification is a major contributor
why FGF-23 rises early in CKD, before a rise in S[P].
to CVD in CKD patients, and observational data indicate
In non-dialysis-dependent CKD patients, FGF-23 lev-
vascular calcification predicts of cardiovascular events
els are independently associated with mortality,43,44 car-
and mortality.14,52 However, it is presently unclear if
diovascular events,43,44,45 and CKD progression.43,44,46
intervening to slow progression of vascular calcification
Very large hazard ratios support the contention
alters outcomes in CKD patients.1
that FGF-23 is a key outcome predictor. FGF-23 lev-
els are also independently associated with left ven-
tricular hypertrophy in non-dialysis-dependent CKD DIAGNOSIS
patients,41,47 chronic HD patients,48 and in the general
population.49 Evidence in animals indicates that block- The basis of these recommendations are primarily
ing FGF-23 can prevent the development of left ven- the KDIGO guidelines,1,4 mentioning differences from
tricular hypertrophy.41 One of the strongest working KDOQI5 when applicable. Traditionally, biochemical
hypotheses regarding why FGF-23 predicts of cardiovas- parameters have been the primary indicators for the
cular events and mortality is its causal effect on left ven- basis of diagnosis, identifying therapeutic targets, and
tricular hypertrophy. managing CKD-MBD. When considering biochemical
values, it is recommended that all therapeutic decisions
are based on trends rather than a single value.
Bone Clinically significant biochemical manifestations of
Traditionally, renal osteodystophy has been charac- CKD-MBD may begin in stage 3 (a GFR of approxi-
terized based on bone turnover and mineralization. In mately 40 to 50 mL/min/1.73 m2),6 but the rate and
CKD-MBD, alterations in these parameters vary greatly. degree of changes are highly variable. Therefore the
The spectrum of bone turnover ranges from abnormally frequency of assessment must consider the individual
low to very high, and mineralization may or may not be patient.1 The most recent KDIGO guidelines recom-
present. mend measuring S[Ca], S[P], iPTH, as well as alkaline
VIII. THERAPEUTIC CONSIDERATIONS
650 53. Management of Mineral and Bone Disorders in Chronic Kidney Disease Patients
phosphatase (ALP), at least once in all adults with an in CKD stages 3 to 5, with repeat testing intervals com-
eGFR less than 45mL/min/1.73m2 in order to establish mensurate with both baseline levels and current treat-
a baseline.4 At least one of these biochemical abnormali- ment (Table 53.1).1 KDOQI also recommends periodic
ties must be present for the diagnosis of CKD-MBD.1 testing of 25(OH)D3 and initiating treatment if levels are
Most observational data on these parameters were gen- low.5 However, there is still some debate in the nephrol-
erated in a HD population. Much less is known about ogy community regarding whether 25(OH)D3 levels
stage 3 to 5 CKD. This makes establishing diagnostic cri- should be measured and monitored, as there is a lack
teria as well as treatment recommendations challenging. of evidence that vitamin D supplementation indeed
Furthermore, there are no clear data available supporting improves clinical outcomes. The assays used to measure
that routine measurement improves outcomes, but these 25(OH)D3 are not well standardized, with the DiaSorin
are the best recommendations based on the currently assay being most commonly used in clinical practice.1
available data.1
PTH
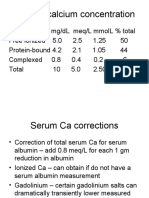
Calcium KDIGO recommends monitoring serum iPTH lev-
KDIGO recommends monitoring S[Ca] beginning in els beginning in stage 3 and considering these levels
stage 3 CKD. While the frequency of monitoring should and progression in determining repeat testing inter-
consider the individual patient, a reasonable monitor- vals. A reasonable monitoring schedule in stages 4
ing schedule is every 6 to 12 months in stage 3, every 3 and 5 is every 6 to 12 and 3 to 6 months, respectively
to 6 months in stage 4, and every 1 to 3 months in stage (Table 53.1). An optimal level of iPTH in stages 3 to 5
5 (Table 53.1).1 Ideally, ionized calcium should be used, CKD is currently unknown and difficult to establish
as this is the physiologically active form. However, this because the range of values widens as CKD progresses.
is not a routinely available, practical or cost effective In addition, there are methodological challenges to
option, thus total calcium is most frequently measured. measurement associated with assay type, sample type,
methodology, and variability. The second generation
assay (iPTH) is most commonly used in clinical prac-
Phosphorus tice. There are also normally minute to minute oscilla-
tions in levels, although this is blunted in CKD. Thus,
Recommendations for monitoring S[P] parallel those KDIGO does not provide a specific target recommen-
for S[Ca] (Table 53.1).1 S[P] varies diurnally, although dation, but instead recommends interpretation on the
this variation is less in patients with CKD.56 basis of the specifics of each individual laboratory.
Guidance of therapy should be based on a persistent
rise in levels, rather than an absolute value.1
Vitamin D
25(OH)D3 is considered the best measure of vitamin
FGF-23
D nutritional status, as it has a long half-life (approxi-
mately 3 weeks). 1,25(OH)2D3 has a much shorter half- FGF-23 is not currently considered in the diagno-
life (approximately 4 to 6 hours).1 Epidemiological sis of CKD-MBD, as it is still a relatively new, but very
studies have found both 25(OH)D3 and 1,25(OH)2D3 important, component of CKD-MBD. Thus, FGF-23
to be independent predictors of all-cause and cardio- is not discussed in the KDIGO or KDOQI guidelines,
vascular mortality in both patients with CKD and in and FGF-23 is currently more commonly assessed
the general population.2428 Vitamin D status refers to in research. There are two enzyme-linked immuno-
whether or not circulating levels of 25(OH)D3 are con- asays that are used to measure FGF-23: the intact FGF-
sidered adequate. While there is no consensus on what 23 assay (primarily serum) and the C-terminal FGF-23
is considered adequate levels, the most recent 2013 assay (primarily plasma). Initial studies showed a good
update from KDIGO recommended using the interna- correlation between the two, although this has been
tional definition of <20ng/mL as a cut-off for vitamin D questioned in more recent work.61,62 Values for FGF-23
deficiency.4 Serum 25(OH)D3 levels are inversely associ- are skewed to the right, therefore median levels are typ-
ated with serum PTH levels in CKD57 and non-CKD58,59 ically reported in research. Using the C-terminal assay,
patients, until 25(OH)D3 increases to 30 to 40ng/mL, at typical levels in healthy adults are 17.8197.0 RU/mL
which point PTH level plateaus at its nadir.60 Such data (median 76.5 RU/mL) (Table 53.1).63 In non-dialysis-
provide the basis for the term vitamin D status, which dependent CKD patients, the typical elevation is 25-
refers generally to whether an individual has deficient, fold higher (63.65592 RU/mL; median 188 RU/mL),
insufficient or sufficient serum levels of 25(OH)D3. and in dialysis patients, levels can reach an exponential
KDIGO recommends considering monitoring 25(OH)D3 1000-fold increase (150115,000 RU/mL; median 4175
VIII. THERAPEUTIC CONSIDERATIONS
Diagnosis 651
TABLE 53.1 Biochemical Diagnosis of CKD-MBD*
Physiological Triggers and KDIGO Monitoring
Parameter Normal Range (serum) Consequences Changes in CKD Recommendations
Calcium* 8.510.5mg/dL# Low 1,25(OH)2D3, decreased Most often moderate Stage 3: every 6 to 12
intestinal absorption and hypocalcemia, although months
phosphate retention hypercalcemia can occur (rare)
Stage 4: every 3 to 6 months
Favors the development of Remains normal until eGFR Stage 5: every 1 to 3 months
SHP <40mL/min/1.73m and stays
2
relatively stable until eGFR
<20mL/min/1.73m2
Phosphorus* 2.54.5mg/dL Impaired phosphate excretion Remains normal until eGFR Stage 3: every 6 to 12
promotes a rise in S[P] <40mL/min/1.73m2 and stays months
relatively stable until eGFR
Stage 4: every 3 to 6 months
<20mL/min/1.73m2
Increased levels stimulate SHP, Stage 5: every 1 to 3 months
Does not rise until later stages
promote vascular calcification
because FGF-23 initially
maintains the normal range
by increasing renal phosphate
excretion
Vitamin D* Deficient = 25(OH)D3 <20ng/ 1,25(OH)2D3 synthesis in the Insufficiency and deficiency Baseline testing in stages 3
mL kidney is compromised are highly prevalent, possibly to 5, with repeat intervals
approximately 50% of CKD commensurate with baseline
Insufficient = 2030ng/mL May be an underlying cause of patients levels and treatment
Sufficient >30ng/mL elevated PTH
PTH* Abnormal if eGFR is <45mL/ Increases in response Approximately 60% of Stage 3: based on baseline
min/1.73m2 and iPTH is to hypocalcemia, patients with eGFR <60mL/ levels and CKD progression
persistently above upper limit of hyperphosphatemia and/or min/1.73m2 have elevated
Stage 4: every 6 to 12
normal for the given assay and decreased 1,25(OH)2D3 iPTH levels
months
progressively rising
Hypercalcemia, high Stage 5: every 3 to 6 months
1,25(OH)2D3 and FGF-23 can
suppress
FGF-23 In one small study: healthy Secreted by skeletal Increases very early in CKD No recommendation given
adults: 17.8197.0 RU/mL osteocytes in response to (eGFR approximately 70mL/
(median 76.5 RU/mL) changes in bone formation min/1.73m2) and progressively
Non-dialysis-dependent CKD: and S[P], principal increases as GFR declines
63.65592.0 RU/mL (median regulating hormone of
188.0 RU/mL) phosphorus
Maintenance HD: 150115,000 High FGF-23 inhibits
RU/mL (median 4715.0 RU/ 1,25(OH)2D3 and favors
mL) increased PTH
All therapeutic decisions should be based on trends rather than a single laboratory value. 1,25(OH)2D3: 1,25D dihydroxyvitamin D3, SHP: secondary hyperparathyroidism, eGFR:
estimated glomerular filtration rate, S[P]: serum phosphorus concentration, 25(OH)D3: 25 hydroxyvitamin D3, iPTH: intact parathyroid hormone, FGF-23: fibroblast growth factor-23.
*
To make a diagnosis of CKD-MBD, one of more of these laboratory abnormalities must be present.
#
May vary by laboratory.
Frequency of monitoring should consider the presence and magnitude of abnormalities.
RU/mL).13,61,63 It is also important to consider the frac- component of CKD-MBD, as it provides information
tional excretion of phosphate in the interpretation of regarding bone turnover, mineralization and volume.1
these values, as FGF-23 is the principal regulating hor- KDIGO asserts than bone biopsy is reasonable for cer-
mone of phosphorus. tain settings in stage 3 to 5 CKD, including patients
with unexplained fractures, persistent bone pain, unex-
plained hypercalcemia or hyphophatemia, and before
Bone starting therapy with biophosphonates in those with
Bone biopsy-based histology is considered the known CKD-MBD.1 Routine bone mineral density
gold standard technique for the diagnosis of the bone (BMD) testing using dual energy X-ray absorptiometry
VIII. THERAPEUTIC CONSIDERATIONS
652 53. Management of Mineral and Bone Disorders in Chronic Kidney Disease Patients
(DXA) scans is not recommended in patients with an known hypercalcemia is recommended.1 Figure 53.4
eGFR <45mL/min/1.73m2. BMD does not predict frac- provides an algorithmic approach to the treatment
ture risk in these patients as in the general population, of hypercalcemia and other abnormalities of mineral
and results may be either unhelpful or misleading.4,5 metabolites in patients with CKD-MBD.
Recommendations suggest treatment for hypocal-
cemia should be initiated only when patients with
Vascular Calcification CKD present with symptoms of hypocalcemia, such as
While extraskeletal calcification is a component of numbness and tingling. In some cases, hypocalcemia
diagnosis of CKD-MBD, KDIGO does not recommend (defined as S[Ca] less than 7.5mg/dL) should war-
indiscriminate screening of all patients with CKD-MBD rant treatment. The initial treatment should include
for vascular calcification, as it is unclear if intervention oral calcium supplementation and/or active vitamin D
will alter outcomes.1 KDOQI also does not recommend analogues to correct hypocalcemia. However, vitamin
screening asymptomatic patients with CKD for calcifica- D analogues should mainly be used only if the symp-
tion.5 At this time, there is consensus among the nephrol- tomatic hypocalcemia is present with an elevated PTH.
ogy community that screening for vascular calcification In those patients who have hypocalcemia in the setting
will increase the costbenefit ratio, as there is a lack of of hyperphosphatemia, the high S[P] should be treated
potential therapeutic interventions to reverse vascular with a phosphate binder before initiating any other
calcification. However, when vascular calcification is therapy for hypocalcemia.
detected, the patient should be considered to have high
cardiovascular risk. Phosphorus
The data on normalizing S[P] in those patients with
TREATMENT CKD not requiring chronic dialysis are conflicting.65 The
recommendation in chronic dialysis patients is to achieve
To date, the focus in the literature has been on the asso- at least a S[P] <5.5mg/dL. Figure 53.4 provides a sug-
ciation between disordered mineral metabolism in CKD gested approach to correcting S[P] abnormalities in non-
and adverse outcomes, including mortality, cardiovascu- dialysis-dependent CKD patients.
lar disease, and fractures. This has led to targeting these Observational data suggest that phosphate binders
parameters in clinical practice to potentially improve of any type may reduce mortality in both dialysis-66
these outcomes, but large RCTs supporting clinical prac- and non-dialysis-dependent CKD patients.67 Most RCTs
tice are presently very limited.1 Most of the available have been completed in chronic HD populations, with
literature consists of observational data or surrogate out- only one trial available in patients with stage 3 to 5
comes, rather than therapeutic options associated with CKD.68 The phosphate binder sevelamer slowed vascu-
hard outcomes. In general, therapy has typically focused lar calcification in this study, which is largely consistent
on correcting biochemical and hormonal abnormalities in with studies in dialysis patients,19,69 although not all
order to limit their potentially adverse consequences. This trials have been positive.70,71 The efficacy of phosphate
section focuses largely on treatments targeting correction binders for reducing cardiovascular events or mortality
of biochemical and hormonal abnormalities. in non-dialysis-dependent CKD is currently unknown.
In dialysis patients, both a RCT72 and secondary anal-
ysis of an open label study73 showed no difference in
Calcium mortality based on allocation to sevelamer compared to
There is little observational or interventional evi- calcium-based binders. A third study performed in inci-
dence that targeting S[Ca] alters clinical outcomes in dent HD patients found increased mortality in calcium-
CKD, although calcium supplementation may increase based binder compared to sevelamer group, although
risk of CVD in the general population.64 KDIGO recom- the KDIGO work group1 raised a concern of a possibly
mends maintaining S[Ca] in the normal range in stage unsuccessful randomization.19 RCTs using phosphate
3 to 5 CKD patients (Table 53.2).1 KDOQI agrees with binders with cardiovascular end-points are also lack-
this recommendation, with a preference towards the ing in the chronic dialysis population. The effects of
lower end of the reference range in stage 5 patients (8.4 calcium-based binders compared to either sevelamer
to 9.6mg/dL).5 However, most of the data supporting or lanthanum on bone histology are unclear, with some
this recommendation are observational, and there does studies in chronic dialysis patients showing improve-
not appear to be any detriment to clinical outcomes to ments and some showing worsening.71,74,75
maintaining S[Ca] within the normal laboratory range. Sevelamer and calcium-based binders appear to be
To achieve this goal, limiting the use of calcium-based equally effective at lowering S[P] in RCTs with stage 3 to
binders, calcitriol and/or its analogs in patients with 5 CKD patients.68 Lanthanum also appears to be effective
VIII. THERAPEUTIC CONSIDERATIONS
Treatment 653
TABLE 53.2 Treatment of Biochemical Abnormalities in CKD-MBD
Parameter KDIGO/KDOQI Treatment Recommendations Therapeutic Options
Calcium Stage 3 to 4: maintain corrected S[Ca] in the Limit calcium-based binders and/or 1,25(OH)2D3 or active vitamin D
normal range treatment if known hypercalcemia
Stage 5: same as above, with a preference towards
the lower end of the reference range (8.49.6mg/dL)
Phosphorus If GFR <45mL/min/1.73m2, maintain S[P] in the Dietary phosphate restriction
normal range
Phosphate binders
Choice of binder should consider other
Aluminum hydroxide (not recommended)
components of CKD-MBD, other therapies and
Calcium carbonate and calcium acetate
Magnesium hydroxide and magnesium carbonate
side-effects
Sevelamer hydrochloride and sevelamer carbonate
Maintain S[P] in the target range in stage 3 to 4, Lanthanum carbonate
lower in stage 5
Vitamin D Only indicated to correct 25(OH)D3 deficiency, Nutritional vitamin D
follow recommendations for general population Ergocalciferol (D2)
(10002000 IU/d cholecalciferol [D3]) Cholecalciferol (D3)
Recommend using 50,000 IU/week or per month
ergocalciferol (D2) to correct deficiency to >30ng/mL
PTH Stages 3 to 5: optimal levels unknown First evaluate for hyperphosphatemia, hypocalcemia and vitamin D deficiency
Suggest lowering PTH threshold in CKD stages 4 Initial options
to 5 to prompt evaluation and possible treatment Limit dietary phosphate
Phosphate binders
Calcium supplements
Nutritional vitamin D (only if 25(OH)D3 deficient)
If PTH continues to rise and remains above upper limit of normal and the
patient is 25(OH)D3 deficient: calcitriol or vitamin D analogs
Cinacalcet not recommended by KDIGO in non-dialysis CKD patients
Severe HPT without response to other therapy: parathyriodectomy
FGF-23 Optimal levels unknown. KDIGO and KDOQI do KDIGO does not make a recommendation
not make recommendations
Only therapeutic option at this time is dietary phosphate reduction
Sevelamer and lanthanum carbonate may lower FGF-23
S[Ca]: serum calcium concentration, 1,25(OH)2D3: 1,25D dihydroxyvitamin D, eGFR: estimated glomerular filtration rate, 25(OH)D3: 25 hydroxyvitamin D, S[P]: serum
phosphorus concentration, PTH: parathyroid hormone, HPT: hyperparathyroidism, FGF-23: fibroblast growth factor-23. See Figure 53.4 for an approach to treating biochemical
abnormalities in patients with CKD-MBD.
in chronic dialysis patients.76,77 A recent meta-analysis on clinical outcomes. Overall, a phosphate-restricted
concluded that all currently available phosphate bind- diet combined with oral phosphate binders is a well-
ers effectively lower S[P] compared to placebo.78 Trials established recommendation for controlling hyper-
have shown no difference in S[Ca] in stage 3 to 5 CKD phosphatemia in patients with stage 3 to 5 CKD.1,5
patients randomized to sevelamer or a calcium-based The choice of phosphate binder should consider other
phosphate binder,68 but lower S[Ca] in chronic dialysis components of CKD-MBD, concomitant therapies, and
patients treated with sevelamer compared to calcium- side-effects. There is currently insufficient evidence on
based binders.19,69,71,72 comparative clinical efficacy to recommend a specific
The most recent KDIGO guidelines recommend binder for all patients.1
maintaining S[P] in the normal range if eGFR <45mL/ Dietary phosphate restriction is important in the
min/1.73m2.4 KDOQI recommends lower than the treatment of CKD-MBD because 6070% of ingested
target range in stage 5 (Table 53.2).5 This is one of phosphate is absorbed.79 However, there are numer-
the recommendations most widely accepted by the ous challenges to achieving treatment goals, includ-
nephrology community. Prospective RCTs, however, are ing patient compliance, issues with food labels, and
needed to prove that lowering S[P] below the recom- the presence of abundant food additives (Table 53.3).79
mended target range indeed has any significant affect Consequently, there are not enough data on dietary
VIII. THERAPEUTIC CONSIDERATIONS
654 53. Management of Mineral and Bone Disorders in Chronic Kidney Disease Patients
Hypercalcemia Hyperphosphatemia 25(OH)D deficiency
(>10.2 mg/dl) (>4.5 mg/dl) (<20 ng/ml)
Oral calcium-based Dietary phosphorus 10002000 IU/d
phosphate binders? restriction cholecalciferol (D3)
yes
no
Discontinue
Active vitamin D or Persistent Re-check at
vitamin D analogs? hyperphosphatemia? 6 months
yes no
yes
no
Maintain
Discontinue Consider phosphate change Persistent
Check for other binders* 25(OH)D deficiency?
causes (e.g.
no
malignancy)
yes
Discontinue
Continue D3 or
increase dose
FIGURE 53.4 Algorithmic approach to treating biochemical and hormonal abnormalities in CKD-MBD. The first step in the treatment of
hypercalcemia is to check if the patient is taking oral calcium-based phosphate binders. If so, the binder should be discontinued. The same ques-
tion should be asked regarding therapy with active vitamin D or vitamin D analogs. If neither is a potential cause of hypercalcemia, other poten-
tial causes should be evaluated, such as malignancy. To treat hyperphosphatemia, dietary phosphorus restriction should first be attempted. If
hyperphosphatemia persists, phosphate binders should be considered. However, phosphate binders are not FDA-approved for the treatment of
hyperphosphatemia in non-dialysis-dependent CKD (indicated by *). Consistent with KDIGO recommendations, we recommend treatment of
25(OH)D3 deficiency with 10002000 IU/day of cholecalciferol (D3). Serum 25(OH)D3 should be re-checked after 6 months, with supplementa-
tion continued or increased according to repeat test levels.
modifications to strongly endorse phosphate restriction doses that could induce hypermagnesemia in CKD
alone as the primary or sole therapy to control hyper- patients.79
phosphatemia in patients with CKD-MBD.1 Sevelamer hydrochloride is a non-calcium, non-metal,
Phosphate binders available for the treatment of non-absorbable phosphate binder. Sevelamer carbonate
CKD-MBD have particular advantages and disad- is similar to sevelamer hydrochloride, and is assumed
vantages (Table 53.3). Aluminum hydroxide is not to have equal efficacy and potentially improved acid
recommended for use as there is a risk of serious hema- base balance and lower risk of acidosis.1,80 Both have the
tological, neurological and skeletal adverse events as a advantages of avoiding calcium overload, metal expo-
consequence of aluminum toxicity.79 Calcium carbonate sure and absorption, and have also been shown to lower
and calcium acetate are both calcium-based phosphate LDL cholesterol.79 Sevelamer also has potential benefits
binders that are inexpensive and effective at lowering on vascular calcification and mortality,68,72 and treat-
S[P], but increase risk of calcium overload, which may ment can lower FGF-23.81 Disadvantages of sevelamer
promote vascular calcification or adynamic bone dis- include high cost, gastrointestinal side-effects, a high pill
ease (although there is less calcium exposure with cal- burden, and the risk of decreased bicarbonate levels with
cium acetate than calcium carbonate).79 Accordingly, sevelamer hydrochloride.79
KDIGO does not recommend using calcium-based Lanthanum carbonate is a non-calcium, naturally
phosphate binders in patients with known low bone occurring metal-based binder first approved for use
turnover, vascular calcification or hypercalcemia.1 in 2004.82 Advantages include effective phosphate
Magnesium-based binders include magnesium hydrox- lowering, avoidance of calcium overload, lesser pill
ide and magnesium carbonate. Both magnesium-based requirement than sevelamer, and chewable deliv-
binders are associated with a lower calcium load than ery. Lanthanum is eliminated by the liver, and there-
pure calcium-based phosphate binders. However, they fore its handling is not dependent on renal function.79
have gastrointestinal side-effects, are not well studied, Lanthanum may also have benefits beyond lowering
and have lower efficacy, which may necessitate higher S[P], such as improving bone remodeling or lowering
VIII. THERAPEUTIC CONSIDERATIONS
Treatment 655
TABLE 53.3 Advantages and Disadvantages of Available Therapies to Treat CKD-MBD-associated Biochemical Abnormalities
Therapeutic Options Pro Con
Dietary phosphate Important modulator of S[P] because 60 to 70% of all ingested Challenging to adhere to (food choices, food labeling,
restriction dietary phosphate is absorbed additives, etc.)
Not enough data available to strongly endorse as the sole
therapy for treatment hyperphosphatemia
Aluminum Very effective phosphate binding Not recommended due to risk of serious hematological,
hydroxide neurological and skeletal adverse events resulting from
aluminum toxicity
Calcium carbonate Inexpensive, effective and readily available Potential of hypercalcemia-associated risks (e.g. vascular
calcification, adynamic bone disease)
KDIGO does not recommend using in patients with
known low bone turnover, vascular calcification or
hypercalcemia
Calcium acetate Potentially less calcium exposure and better phosphate- Risk of hypercalcemia
binding capacity than calcium carbonate
More costly than calcium carbonate
KDIGO does not recommend using in patients with
known low bone turnover, vascular calcification or
hypercalcemia
Magnesium Potentially less calcium exposure than calcium-based binders Gastrointestinal side-effects
hydroxide and
Lower efficacy, which may necessitate higher doses and
magnesium
potentially hypermagnesemia
carbonate
Not well studied
Sevelamer Effective High cost
hydrochloride
Avoids calcium overload Gastrointestinal side-effects
Avoids metal exposure High pill burden
Not absorbed Potential for decreased serum bicarbonate levels
(acidosis)
May have benefits beyond lowering S[P] (such as lowering
LDL, slowing vascular calcification, and lowering FGF-23)
Sevelamer carbonate Assumed to have similar advantages to sevelamer High cost
hydrochloride with improved acidbase balance
Gastrointestinal side-effects
High pill burden
Lanthanum Effective High cost
carbonate
Avoids calcium overload Gastrointestinal side-effects
Chewable Long-term clinical consequences unknown
Eliminated by the liver thus metabolism not dependent on
renal function
May have benefits beyond lowering S[P] (such as improving
bone remodeling, lowering FGF-23 levels)
Nutritional vitamin Effective at raising 25(OH)D3 and 1,25(OH)2D3 levels Lack of RCTs in CKD patients
D (D2 and D3)
Extra-renal conversion to 1,25(OH)2D3 may confer extra-renal Less studied in CKD patients
benefits
Can also suppress PTH Some question as to whether it is adequate to raise
25(OH)D3 to sufficient levels in all CKD patients
Inexpensive
Incidence of hypercalcemia and hyperphosphatemia is low
(Continued)
VIII. THERAPEUTIC CONSIDERATIONS
656 53. Management of Mineral and Bone Disorders in Chronic Kidney Disease Patients
TABLE 53.3 Advantages and Disadvantages of Available Therapies to Treat CKD-MBD-Associated
CKD-MBD-associated Biochemical
BiochemicalAbnormalities
Abnormalities (Continued)
Therapeutic Options Pro Con
Calcitriol (1,25D3) Effective at raising 1,25(OH)2D3 levels May promote hypercalcemia (risk of adynamic bone
disease, vascular calcification) and/or raise S[P]
Decreases PTH production by the parathyroid glands
Vitamin D Effective at raising 1,25(OH)2D3 May promote hypercalcemia (risk of adynamic bone
receptor activators disease, vascular calcification) and/or raise S[P]
Decreases PTH production by the parathyroid glands
(1,25(OH)2D3
analogs: e.g. Newer analogs are more selective for PTH suppression with
paricalcitol, fewer effects on S[Ca] and S[P]
doxercalciferol)
Cinacalcet Effectively lowers PTH Did not reduce mortality in EVOLVE trial
May also lower S[P] Gastrointestinal side-effects
Risk of hypocalcemia
Not FDA approved for use in patients with CKD not
requiring dialysis
Parathyroidectomy Generally reduces PTH, S[Ca] and S[P] Last choice therapy
Lack of RCTs on the benefits and risks
S[P]: serum phosphorus concentration, FGF-23: fibroblast growth factor-23, 1,25(OH)2D3: 1,25D dihydroxyvitamin D, 25(OH)D3: 25 hydroxvitamin D, PTH: parathyroid
hormone, S[Ca]: serum calcium concentration, RCT: randomized-controlled trial.
FGF-23.76,83 However, the cost of lanthanum carbonate reduced risk of progression to ESRD.88 In a meta-anal-
is high, gastrointestinal side-effects are common, and ysis of trials in non-CKD patients, nutritional vitamin
the long-term clinical consequences of its use are still D supplementation was shown to decrease mortality.89
largely unknown.1,79,84 One small observational study in chronic HD patients
showed an association between cholecalciferol use and
reduced left ventricular mass index.90
Vitamin D There are currently no published large RCTs on the
KDIGO recommends treating CKD patients with effects of either active or nutritional vitamin D therapy
low circulating levels of 25(OH)D3, with supplementa- on mortality or cardiovascular events in patients with
tion with 10002000 IU/d of cholecalciferol, consistent CKD,1 or in the general population. The ongoing NIH-
with repletion recommendations for the general popula- funded Vitamin D and Omega-3 Trial (VITAL) will
tion.4 KDOQI recommends using ergocalciferol (50,000 provide insight into the effects of nutritional vitamin D
IU weekly or monthly) to correct 25(OH)D3 deficiency supplementation on hard outcomes in the general pop-
if levels are lower than 30ng/mL.85 Both forms of vita- ulation. The PRIMO (Paricalcitol Capsule Benefits in
min D supplementation have been shown to increase Renal Failure-Induced Cardiac Morbidity) trial showed
serum 25(OH)D3 levels. However, there is a lack of data no change in left ventricular mass index in stage 3 to 4
regarding the impact of these nutritional vitamin D sup- CKD patients treated with 2 g/day paricalcitol for 48
plements on clinical management issues, including pill weeks.91 This finding was in contrast to earlier evidence
burden and the cost related to treatment and monitoring. that vitamin D analogs reduce LVH in rats.92 Studies
1,25(OH)2D3 levels are usually not monitored through- on vascular calcification are inconclusive, and mouse
out the course of CKD. Therefore, treatment should not models of CKD suggest that there is a balance needed
be administered in response to low 1,25(OH)2D3. Figure between high and low levels of 1,25(OH)2D3 to protect
53.4 provides an algorithmic approach to treating CKD against versus induce vascular calcification.93 It is cur-
patients with low circulating levels of 25(OH)D3, with rently unknown if vitamin D treatment reduces fracture
the available evidence supporting this overall approach. risk in patients with CKD, and the effects on bone are
Observational data in chronic dialysis patients sup- inconclusive. Randomized trials have shown possible
port increased survival with treatment with 1,25(OH)2D3 improvements in osteitis fibrosa and mineralization, but
analogs,11,24 but this finding is likely confounded by indi- also reduced bone turnover, which could increase the
cation and results are not consistent.86,87 Data are limited risk of developing adynamic bone disease.94,95
in non-dialysis-dependent CKD patients, as well as for In stage 35 CKD patients, RCTs support that cal-
nutritional vitamin D therapy. Observational data sug- citriol and vitamin D analogs both lower serum iPTH
gest that active vitamin D therapy is also associated with compared to placebo,9698 may increase S[Ca]9799 or
VIII. THERAPEUTIC CONSIDERATIONS
Treatment 657
S[P],99 or may not change either.96 Additionally, vitamin (1,25(OH)D2) are analogs of 1,25(OH)2D3 that activate
D analogs may reduce proteinuria100102 and lower the the vitamin D receptor. Vitamin D analogs are also effec-
inflammatory acute phase protein C-reactive protein.100 tive at raising serum 1,25(OH)2D3 levels, and newer ana-
Nutritional vitamin D treatment may also lower iPTH in logs are more selective for PTH suppression with less
this population, and the associated incidence of hyper- effect on S[Ca] and S[P].96,112 Observational evidence sug-
calcemia and hyperphosphatemia is low.103 gests that vitamin D analog use may improve survival
KDIGO currently recommends correcting 25(OH) in dialysis patients11,24 and slow progression to ESRD in
D3 deficiency to >30ng/mL using treatment strategies earlier stages.88 However, negative results of the recent
similar to those used in the general population (Table PRIMO study on left ventricular mass index called the
53.2).1,4 Use of calcitriol and vitamin D analogs should utility of vitamin D analogs for treating CVD in CKD
be limited in the presence of hypercalcemia. KDIGO into question.91
acknowledges that the efficacy of this overall approach
is not well studied, but given that treatment is safe with
minimal risk of toxicity across all stages of CKD, this
Parathyroid Hormone
strategy is recommended. KDOQI recommends using The EVOLVE (Evaluation of Cinacalcet Hydrochloride
vitamin D2 (ergocalciferol) to correct serum 25(OH)D3 Therapy to Lower Cardiovascular Events) study raises
levels that are <30ng/mL.5 Overall, there is no consen- questions regarding the utility of lowering PTH for
sus regarding the optimal treatment type, dose, or tar- improving cardiovascular outcomes in patients with
get levels of 25(OH)D3. More research is needed to help CKD.113 Prior to EVOLVE, observational data supported
answer these questions. notions that lowering PTH with cinacalcet is associated
Nutritional options to treat 25(OH)D3 deficiency are with decreased all-cause and cardiovascular mortality
ergocalciferol (D2) and cholecalciferol (D3) (Table 53.3), in chronic HD patients.9 RCTs with therapeutic agents
which must undergo conversion in the liver to 25(OH) to lower PTH (testing calcium supplementation, phos-
D3. Nutritional vitamin D is effective at raising both phate binders, nutritional vitamin D, 1,25(OH)2D3 ana-
serum 25(OH)D3 and 1,25(OH)2D3 levels in CKD patients logs and calcimimetics) were mostly limited to the effects
in both observational studies104,105 and RCTs.106,107 There on biochemical parameters and surrogate outcomes. In a
is currently debate regarding whether ergocalciferol single trial in stage 3 to 5 CKD, calcium-binders did not
or cholecalciferol is better at raising and maintaining lower iPTH, but increased coronary calcification score.68
serum 25(OH)D3 levels.108,109 There is overall a lack of Treatment with active vitamin D and its analogs low-
large observational cohort studies and RCTs using nutri- ers serum iPTH, but may also increase S[Ca] or S[P].9698
tional vitamin D in CKD patients. However, there has Active vitamin D and vitamin D analogs have also been
been greater interest in its use in addition to or instead shown to improve histological indices of bone turn-
of active vitamin D in CKD patients more recently. There over.98 No RCTs have prospectively aimed to evaluate
is still some question regarding whether nutritional vita- the efficacy of phosphate binders for lowering iPTH,68
min D can adequately raise 25(OH)D3 to sufficient levels though one study in stage 3 to 5 CKD patients showed a
in all CKD patients.104,105 Nutritional vitamin D is also decrease in iPTH with 8 weeks of treatment with lantha-
effective at lowering PTH,106,107 although the evidence is num.114 While most studies have been in chronic dialy-
not as strong as for active vitamin D therapy.110 An addi- sis populations,115,116 calcimimetics did lower iPTH in
tional advantage of ergocalciferol and cholecalciferol is prospective trials of stage 3 to 5 CKD patients, as well as
that they are relatively inexpensive. induce an asymptomatic decrease in S[Ca] and S[P].117,118
Active (1,25(OH)2D3) vitamin D and 1,25(OH)2D3 In the ADVANCE study, a randomized trial to evalu-
analogs have been more traditionally used as therapeu- ate the effects of cinacalcet plus low-dose vitamin D on
tic options in patients with CKD. Normalization of S[P] vascular calcification in HD patients, cinacalcet, a calci-
should occur before initiation of active vitamin D or mimetic, plus low-dose paricalcitol did not significantly
vitamin D analogs. Calcitriol (1,25(OH)2D3) is effective change the primary end-point, the Agatston coronary
at raising serum 1,25(OH)2D3 levels, as well as decreas- calcification score.119
ing PTH production by the parathyroid glands. Calcitriol The EVOLVE study was a randomized, double-
also increases S[Ca], which further suppresses PTH blinded, placebo controlled study in 3883 chronic HD
secretion.111 Observational evidence supports that cal- patients with moderate to severe secondary hyperpara-
citriol use may be associated with reduced risk of death thyroidism.113 In the unadjusted intent to treat analysis,
or dialysis in patients with secondary hyperparathyroid- there was no significant change in mortality or cardio-
ism.88 However, there are concerns that calcitriol use may vascular events with cinacalcet, despite effective lower-
lead to adynamic bone disease, hypercalcemia and/or ing of iPTH.
hyperphosphatemia, as well as vascular calcification.79,111 Optimal levels of iPTH for patients with stage 3 to 5
Paricalcitol (19-nor-1,25(OH)2D2) and doxercalciferol CKD are unknown, thus KDIGO does not recommend
VIII. THERAPEUTIC CONSIDERATIONS
658 53. Management of Mineral and Bone Disorders in Chronic Kidney Disease Patients
targeting a specific range (Table 53.2).1 KDOQI suggests FGF-23
lowering the iPTH threshold in stage 4 to 5 CKD for
prompting evaluation and possible treatment of hyper- The discovery of FGF-23 is relatively recent, and
parathyroidism.5 This is one of the most debated recom- thus its role in the treatment of CKD-MBD is not yet
mendations, as there is a lack of studies relating serum well understood or targeted. There are some small diet
iPTH levels to bone disease. There is some consensus, manipulation studies and observational evidence that
however, that trends in iPTH levels should be consid- suggest that manipulating dietary phosphate intake can
ered before initiating a therapeutic intervention. KDIGO alter FGF-23 levels.56,120,121 Several small studies have
considers any of the following to be reasonable first- also shown that phosphate lowering with the binders
line therapies for the treatment of hyperparathyroidism: sevelamer81,122 and lanthanum (plus a low phosphate
reduced phosphate intake, phosphate binders, calcium diet)83 can also reduce levels of FGF-23 in patients with
supplements, and if the patient is also 25(OH)D3 defi- stage 3 to 4 CKD. However, the degree of change in FGF-
cient, nutritional vitamin D.1,4 If these options are not 23 in response to phosphate binders or dietary phos-
effective, iPTH is progressively rising and remains above phate restriction is minimal compared to the magnitude
the upper limit of normal, and 25(OH)D3 deficiency is of change seen with progression of CKD. Thus manipu-
present, then treatment with 1,25(OH)2D3 or 1,25(OH)2D3 lating phosphorus alone, either through dietary intake or
analogs should be considered. with phosphate binders, may not be enough to modify
Calcimimetics are not currently recommended for FGF-23 levels in a meaningful way.
treatment of hyperparathyroidism in non-dialysis- FGF-23 receptor blockers are currently being tested
dependent CKD, as the work group felt more data were in animal models to suppress FGF receptor signaling.123
still needed, nor are they approved by the FDA in this There are also ongoing phase I/II oncology clinical trials
population. In circumstances of severe hyperparathy- using FGF receptor (14) tyrosine kinase inhibitors. This
roidism that fails to respond to other therapy, parathy- may represent a potential pharmacological target in the
roidectomy is recommended. treatment of CKD-MBD. However, there are potential
There are advantages and disadvantages associated concerns of negative or unknown consequences of low-
with calcimimetics compared to parathyroidectomy ering FGF-23 that will need to be carefully considered.
for treatment of hyperparathyroidism in CKD patients
(Table 53.3). By mimicking an increase in extracellular cal-
cium, calcimimetics increase intracellular calcium, which
Bone
decreases PTH release.1 Cinacalcet, which acts as a posi- KDIGO recommends that in patients with stage 1 to
tive allosteric modulator by inducing a conformational 2 CKD and osteoporosis or a high risk of fracture, and
change in the calcium sensing receptor to increase sensi- patients with stage 3 CKD with osteoporosis or a high
tivity to extracellular calcium,79 is the only type II calcimi- risk of fracture and iPTH in the normal range, manage-
metic currently available for clinical use. While cinacalcet ment should be the same as in the general population. In
is effective at lowering iPTH in both chronic dialysis patients with stage 3 CKD and low bone mineral density
patients115,116 and non-dialysis CKD patients,117,118 its use and/or fragility fractures, treatment should consider the
is associated with gastrointestinal side-effects.113 In the magnitude and reversibility of biochemical abnormali-
EVOLVE study, there was also an increased occurrence of ties, as well as CKD progression, and performance of
hypocalcemia with use of cinacalcet, without any reduc- bone biopsy should be considered. In patients with stage
tion in cardiovascular events or mortality.113 45 CKD and low bone mineral density and/or fragil-
There is a lack of randomized controlled trials to ity fractures, additional investigation with bone biopsy
show either the benefits or risks associated with para- is recommended prior to beginning an antiresorptive
thyroidectomy to treat secondary or autonomous agent, as they are likely only effective in patients with
hyperparathyroidism, as well as studies specifically increased bone resorption and could promote adynamic
comparing surgical to medical therapy for treatment of bone disease. It is also recommended that secondary
secondary hyperparathroidism. However, it is gener- hyperparathyroidism be corrected first.1
ally accepted that a well-performed parathyroidectomy Biphosphonates are effective at decreasing fractures in
reduces serum iPTH concentrations, S[Ca] and S[P] in non-CKD patients with osteoporosis, and post-hoc anal-
CKD patients with secondary or autonomous hyper- ysis of RCTs supports they may be as effective in stage 3
parathyroidism. In addition to a last resort therapy CKD patients. While in theory therapy with bisphospho-
when patients fail to respond to medical therapy, para- nates could benefit patients with stage 4 to 5 CKD and
thyroidectomy could also be considered if the medical low bone density and high turnover, KDIGO does not
management of hyperparathyroidism leads to an unac- recommend the use of bisphosphonates in patients with
ceptable rise in S[Ca] and/or S[P], or if there are other an eGFR <30mL/min/1.73m2 unless there is a strong
intolerable adverse events.1 clinical rationale.4 Teriparatide is an anabolic drug that
VIII. THERAPEUTIC CONSIDERATIONS
REFERENCES 659
increases the formation of new bone. It is a recombinant 2. Demer L, Tintut Y. The bone-vascular axis in chronic kidney dis-
human 1-34 PTH, and therefore is contraindicated in ease. Curr Opin Nephrol Hypertens 2010;19(4):34953.
3. Moe S, Drueke T, Cunningham J, Goodman W, Martin K,
patients with hyperparathyroidism.1 Teriparatide does Olgaard K, et al. Definition, evaluation, and classification
not appear to be contraindicated in women with stage 2 of renal osteodystrophy: a position statement from Kidney
to 3 CKD and normal biochemistry, based on a post-hoc Disease: Improving Global Outcomes (KDIGO). Kidney Int
analysis.124 2006;69(11):194553.
Raloxifene is a selective estrogen receptor modulator 4. Kidney Disease: Improving Global Outcomes (KDIGO) CKD
Work Group KDIGO 2012 Clinical Practice Guideline for the
approved for the treatment of post-menopausal osteo- Evaluation and Management of Chronic Kidney Disease. Kidney
porosis. Raloxifene reduces vertebral fracture risk in Int Suppl 2013;3:1962.
this population, although there are concerns common to 5. National Kidney Foundation. K/DOQI clinical practice guide-
estrogen therapy, including increased risk of fatal stroke.1 lines for bone metabolism and disease in chronic kidney disease.
A post-hoc analysis including participants from a trial Am J Kidney Dis 2003;42(4 Suppl. 3):S1201.
6. Levin A, Bakris GL, Molitch M, Smulders M, Tian J, Williams
who had mild to moderate CKD and normal biochem- LA, et al. Prevalence of abnormal serum vitamin D, PTH, cal-
istry suggests raloxifene may be as safe and effective for cium, and phosphorus in patients with chronic kidney disease:
these patients as the general population, although this results of the study to evaluate early kidney disease. Kidney Int
cohort in not likely representative of the typical CKD 2007;71(1):318.
population.125 7. Gal-Moscovici A, Sprague SM. Use of vitamin D in chronic kid-
ney disease patients. Kidney Int 2010;78(2):14651.
8. Hruska KA, Levi M, Slatopolsky E. Disorders of phospho-
rus, calcium and magnesium metabolism. In: Schrier RW,
Vascular Calcification editor. Diseases of the kidney and urinary tract 8th ed.
There is no clear evidence-based protocol established Philadelphia: Lippincott Williams and Wilkins; 2007.
9. Block GA, Zaun D, Smits G, Persky M, Brillhart S, Nieman K,
for treatment given a positive calcification test. In gen-
etal. Cinacalcet hydrochloride treatment significantly improves
eral, the KDIGO recommendations focus on strategies all-cause and cardiovascular survival in a large cohort of hemo-
to minimize the progression of vascular calcification in dialysis patients. Kidney Int 2010;78(6):57889.
patients with known calcification.1 Non-calcium-based 10. Kimata N, Albert JM, Akiba T, Yamazaki S, Kawaguchi T,
binders are recommended for the treatment of hyper- Fukuhara S, et al. Association of mineral metabolism factors
with all-cause and cardiovascular mortality in hemodialysis
phosphatemia in CKD patients with known vascular
patients: the Japan Dialysis Outcomes and Practice Patterns
calcification. There is currently a lack of intervention study. Hemodialysis Int 2007;11(3):3408.
data on the effects of calcimimetics, nutritional or active 11. Kalantar-Zadeh K, Kuwae N, Regidor DL, Kovesdy CP,
vitamin D/analogs, or parathyroidectomy on vascular Kilpatrick RD, Shinaberger CS, et al. Survival predictability of
calcification progression. time-varying indicators of bone disease in maintenance hemodi-
alysis patients. Kidney Int 2006;70(4):77180.
12. Bolland MJ, Avenell A, Baron JA, Grey A, MacLennan GS,
Gamble GD, etal. Effect of calcium supplements on risk of myo-
CONCLUSION cardial infarction and cardiovascular events: meta-analysis. BMJ
2010;341:c3691.
The pathophysiology of CKD-MBD, a common clini- 13. Isakova T, Wahl P, Vargas GS, Gutierrez OM, Scialla J, Xie H,
cal syndrome in patients with CKD with consequences etal. Fibroblast growth factor 23 is elevated before parathyroid
hormone and phosphate in chronic kidney disease. Kidney Int
affecting mineral metabolism, bone mineralization and
2011;79(12):13708.
extracellular calcification, is complex. Treatment of CKD- 14. Kendrick J, Chonchol M. The role of phosphorus in the develop-
MBD, especially in early stages of disease, with a focus on ment and progression of vascular calcification. Am J Kidney Dis
the biochemical and hormonal factors, and calcium, phos- 2011;58(5):82634.
phorus, vitamin D, iPTH and FGF-23 metabolism, as well 15. Tonelli M, Sacks F, Pfeffer M, Gao Z, Curhan G. Relation
between serum phosphate level and cardiovascular event rate in
as consideration of bone and vascular calcification, is often
people with coronary disease. Circulation 2005;112(17):262733.
not evidence-based, because of the lack of information 16. Chonchol M, Dale R, Schrier RW, Estacio R. Serum phospho-
from observational studies as well as RCTs performed in rus and cardiovascular mortality in type 2 diabetes. Am J Med
specific patient populations. There is great need for well- 2009;122(4):3806.
designed RCTs to further guide the diagnosis and com- 17. Eddington H, Hoefield R, Sinha S, Chrysochou C, Lane B, Foley
RN, et al. Serum phosphate and mortality in patients with
plex management of patients with CKD-MBD.
chronic kidney disease. Clin J Am Soc Nephrol 2010;5(12):22517.
18. Kestenbaum B, Sampson JN, Rudser KD, Patterson DJ, Seliger
References SL, Young B, et al. Serum phosphate levels and mortality risk
among people with chronic kidney disease. J Am Soc Nephrol
1. Kidney Disease: Improving Global Outcomes (KDIGO) CKD- 2005;16(2):5208.
MBD Work Group. KDIGO clinical practice guideline for the diag- 19. Block GA, Spiegel DM, Ehrlich J, Mehta R, Lindbergh J,
nosis, evaluation, prevention, and treatment of Chronic Kidney Dreisbach A, etal. Effects of sevelamer and calcium on coronary
Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int Suppl artery calcification in patients new to hemodialysis. Kidney Int
2009(113):S1130. 2005;68(4):181524.
VIII. THERAPEUTIC CONSIDERATIONS
660 53. Management of Mineral and Bone Disorders in Chronic Kidney Disease Patients
20. Adeney KL, Siscovick DS, Ix JH, Seliger SL, Shlipak MG, Jenny NS, 39. Ohkido I, Yokoyama K, Kagami S, Hosoya T. The hypoth-
et al. Association of serum phosphate with vascular and valvular esis that bone turnover influences FGF23 secretion. Kidney Int
calcification in moderate CKD. J Am Soc Nephrol 2009;20(2):3817. 2010;77(8):7434.
21. Chonchol M, Kendrick J, Targher G. Extra-skeletal effects 40. Faul C. Fibroblast growth factor 23 and the heart. Curr Opin
of vitamin D deficiency in chronic kidney disease. Ann Med Nephrol Hypertens 2012;21(4):36975.
2011;43(4):27382. 41. Faul C, Amaral AP, Oskouei B, Hu MC, Sloan A, Isakova T,
22. Levin A, Le Barbier M, Er L, Andress D, Sigrist MK, Djurdjev et al. FGF23 induces left ventricular hypertrophy. J Clin Invest
O. Incident isolated 1,25(OH)(2)D(3) deficiency is more common 2011;121(11):4393408.
than 25(OH)D deficiency in CKD. J Nephrol 2012;25(2):20410. 42. Gutierrez O, Isakova T, Rhee E, Shah A, Holmes J, Collerone G,
23. Shimada T, Hasegawa H, Yamazaki Y, Muto T, Hino R, Takeuchi et al. Fibroblast growth factor-23 mitigates hyperphosphatemia
Y, et al. FGF-23 is a potent regulator of vitamin D metabolism but accentuates calcitriol deficiency in chronic kidney disease.
and phosphate homeostasis. J Bone Min Res 2004;19(3):42935. J Am Soc Nephrol 2005;16(7):220515.
24. Wolf M, Shah A, Gutierrez O, Ankers E, Monroy M, Tamez H, 43. Kendrick J, Cheung AK, Kaufman JS, Greene T, Roberts WL, Smits
et al. Vitamin D levels and early mortality among incident G, etal. FGF-23 associates with death, cardiovascular events, and
hemodialysis patients. Kidney Int 2007;72(8):100413. initiation of chronic dialysis. J Am Soc Nephrol 2011;22(10):191322.
25. Navaneethan SD, Schold JD, Arrigain S, Jolly SE, Jain A, 44. Isakova T, Xie H, Yang W, Xie D, Anderson AH, Scialla J, etal.
Schreiber Jr MJ, et al. Low 25-hydroxyvitamin D levels and Fibroblast growth factor 23 and risks of mortality and end-stage
mortality in non-dialysis-dependent CKD. Am J Kidney Dis renal disease in patients with chronic kidney disease. JAMA
2011;58(4):53643. 2011;305(23):24329.
26. Ginde AA, Scragg R, Schwartz RS, Camargo Jr CA. Prospective 45. Seiler S, Reichart B, Roth D, Seibert E, Fliser D, Heine GH. FGF-
study of serum 25-hydroxyvitamin D level, cardiovascular dis- 23 and future cardiovascular events in patients with chronic
ease mortality, and all-cause mortality in older U.S. adults. J Am kidney disease before initiation of dialysis treatment. Nephrol
Geriatr Soc 2009;57(9):1595603. Dial Transplant 2010;25(12):39839.
27. Melamed ML, Michos ED, Post W, Astor B. 25-hydroxyvitamin 46. Fliser D, Kollerits B, Neyer U, Ankerst DP, Lhotta K, Lingenhel
D levels and the risk of mortality in the general population. Arch A, et al. Fibroblast growth factor 23 (FGF23) predicts progres-
Intern Med 2008;168(15):162937. sion of chronic kidney disease: the Mild to Moderate Kidney
28. Dobnig H, Pilz S, Scharnagl H, Renner W, Seelhorst U, Wellnitz Disease (MMKD) Study. J Am Soc Nephrol 2007;18(9):26008.
B, et al. Independent association of low serum 25-hydroxyvita- 47. Gutierrez OM, Januzzi JL, Isakova T, Laliberte K, Smith K,
min D and 1,25-dihydroxyvitamin D levels with all-cause and Collerone G, et al. Fibroblast growth factor 23 and left ven-
cardiovascular mortality. Arch Intern Med 2008;168(12):13409. tricular hypertrophy in chronic kidney disease. Circulation
29. Kendrick J, Targher G, Smits G, Chonchol M. 2009;119(19):254552.
25-Hydroxyvitamin D deficiency is independently associated 48. Kirkpantur A, Balci M, Gurbuz OA, Afsar B, Canbakan B,
with cardiovascular disease in the Third National Health and Akdemir R, et al. Serum fibroblast growth factor-23 (FGF-23)
Nutrition Examination Survey. Atherosclerosis 2009;205(1):25560. levels are independently associated with left ventricular mass
30. Kendall JM, Thomas SE, Spurlock G, Mir MA. An active sodium and myocardial performance index in maintenance haemodialy-
transport inhibitor released from spontaneously hypertensive sis patients. Nephrol Dial Transplant 2011;26(4):134654.
and normotensive rat fetal hypothalamic cells in culture. Am J 49. Mirza MA, Larsson A, Melhus H, Lind L, Larsson TE. Serum intact
Hypertens 1988;1(3 Pt 3):83S7S. FGF23 associate with left ventricular mass, hypertrophy and geom-
31. Dawson-Hughes B. Serum 25-hydroxyvitamin D and functional etry in an elderly population. Atherosclerosis 2009;207(2):54651.
outcomes in the elderly. Am J Clin Nutr 2008;88(2):537S540S. 50. Piraino B, Chen T, Cooperstein L, Segre G, Puschett J. Fractures
32. Heine GH, Seiler S, Fliser D. FGF-23: the rise of a novel car- and vertebral bone mineral density in patients with renal osteo-
diovascular risk marker in CKD. Nephrol Dial Transplant dystrophy. Clin Nephrol 1988;30(2):5762.
2012;27(8):307281. 51. Gerakis A, Hadjidakis D, Kokkinakis E, Apostolou T, Raptis S,
33. Block GA, Klassen PS, Lazarus JM, Ofsthun N, Lowrie EG, Billis A. Correlation of bone mineral density with the histologi-
Chertow GM. Mineral metabolism, mortality, and morbidity in cal findings of renal osteodystrophy in patients on hemodialy-
maintenance hemodialysis. J Am Soc Nephrol 2004;15(8):220818. sis. J Nephrol 2000;13(6):43743.
34. Floege J, Kim J, Ireland E, Chazot C, Drueke T, de Francisco A, 52. Giachelli CM. The emerging role of phosphate in vascular calci-
etal. Serum iPTH, calcium and phosphate, and the risk of mor- fication. Kidney Int 2009;75(9):8907.
tality in a European haemodialysis population. Nephrol Dial 53. Covic A, Kanbay M, Voroneanu L, Turgut F, Serban DN, Serban
Transplant 2011;26(6):194855. IL, etal. Vascular calcification in chronic kidney disease. Clin Sci
35. Avram MM, Mittman N, Myint MM, Fein P. Importance of low 2010;119(3):11121.
serum intact parathyroid hormone as a predictor of mortality in 54. Guerin AP, Blacher J, Pannier B, Marchais SJ, Safar ME, London
hemodialysis and peritoneal dialysis patients: 14 years of pro- GM. Impact of aortic stiffness attenuation on survival of
spective observation. Am J Kidney Dis 2001;38(6):13517. patients in end-stage renal failure. Circulation 2001;103(7):98792.
36. Melamed ML, Eustace JA, Plantinga L, Jaar BG, Fink NE, Coresh 55. London GM. Alterations of arterial function in end-stage renal
J, etal. Changes in serum calcium, phosphate, and PTH and the disease. Nephron 2000;84(2):1118.
risk of death in incident dialysis patients: a longitudinal study. 56. Moe SM, Zidehsarai MP, Chambers MA, Jackman LA, Radcliffe
Kidney Int 2006;70(2):3517. JS, Trevino LL, et al. Vegetarian compared with meat dietary
37. Drechsler C, Krane V, Grootendorst DC, Ritz E, Winkler K, Marz protein source and phosphorus homeostasis in chronic kidney
W, et al. The association between parathyroid hormone and disease. Clin J Am Soc Nephrol 2011;6(2):25764.
mortality in dialysis patients is modified by wasting. Nephrol 57. Gonzalez EA, Sachdeva A, Oliver DA, Martin KJ. Vitamin D
Dial Transplant 2009;24(10):31517. insufficiency and deficiency in chronic kidney disease. A single
38. Yamashita T, Yoshioka M, Itoh N. Identification of a novel fibro- center observational study. Am J Nephrol 2004;24(5):50310.
blast growth factor, FGF-23, preferentially expressed in the 58. Chapuy MC, Preziosi P, Maamer M, Arnaud S, Galan P,
ventrolateral thalamic nucleus of the brain. Biochem Biophys Res Hercberg S, et al. Prevalence of vitamin D insufficiency in an
Commun 2000;277(2):4948. adult normal population. Osteoporos Int 1997;7(5):43943.
VIII. THERAPEUTIC CONSIDERATIONS
REFERENCES 661
59. Thomas MK, Lloyd-Jones DM, Thadhani RI, Shaw AC, Deraska 77. Finn WF. Lanthanum carbonate versus standard therapy
DJ, Kitch BT, et al. Hypovitaminosis D in medical inpatients. for the treatment of hyperphosphatemia: safety and efficacy
N Engl J Med 1998;338(12):77783. in chronic maintenance hemodialysis patients. Clin Nephrol
60. Dawson-Hughes B, Harris SS, Dallal GE. Plasma calcidiol, sea- 2006;65(3):191202.
son, and serum parathyroid hormone concentrations in healthy 78. Navaneethan SD, Palmer SC, Vecchio M, Craig JC, Elder GJ,
elderly men and women. Am J Clin Nutr 1997;65(1):6771. Strippoli GF. Phosphate binders for preventing and treat-
61. Shimada T, Urakawa I, Isakova T, Yamazaki Y, Epstein M, ing bone disease in chronic kidney disease patients. Cochrane
Wesseling-Perry K, etal. Circulating fibroblast growth factor 23 Database Syst Rev 2011;(2):CD006023
in patients with end-stage renal disease treated by peritoneal 79. Barreto FC, de Oliveira RA, Oliveira RB, Jorgetti V.
dialysis is intact and biologically active. J Clin Endocrinol Metab Pharmacotherapy of chronic kidney disease and mineral bone
2010;95(2):57885. disorder. Expert Opin Pharmacother 2011;12(17):262740.
62. Smith ER, Cai MM, McMahon LP, Holt SG. Biological variabil- 80. Pai AB, Shepler BM. Comparison of sevelamer hydrochloride
ity of plasma intact and C-terminal FGF23 measurements. J Clin and sevelamer carbonate: risk of metabolic acidosis and clinical
Endocrinol Metab 2012;97(9):335765. implications. Pharmacotherapy 2009;29(5):55461.
63. Imanishi Y, Inaba M, Nakatsuka K, Nagasue K, Okuno S, 81. Oliveira RB, Cancela AL, Graciolli FG, Dos Reis LM, Draibe SA,
Yoshihara A, etal. FGF-23 in patients with end-stage renal dis- Cuppari L, etal. Early control of PTH and FGF23 in normophos-
ease on hemodialysis. Kidney Int 2004;65(5):19436. phatemic CKD patients: a new target in CKD-MBD therapy?
64. Bolland MJ, Grey A, Avenell A, Gamble GD, Reid IR. Calcium Clin J Am Soc Nephrol 2010;5(2):28691.
supplements with or without vitamin D and risk of cardiovas- 82. Koizumi M, Komaba H, Nakanishi S, Fujimori A, Fukagawa M.
cular events: reanalysis of the Womens Health Initiative limited Cinacalcet treatment and serum FGF23 levels in haemodialy-
access dataset and meta-analysis. BMJ 2011;342:d2040. sis patients with secondary hyperparathyroidism. Nephrol Dial
65. Block GA, Wheeler DC, Persky MS, Kestenbaum B, Ketteler Transplant 2012;27(2):78490.
M, Spiegel DM, etal. Effects of phosphate binders in moderate 83. Gonzalez-Parra E, Gonzalez-Casaus ML, Galan A, Martinez-
CKD. J Am Soc Nephrol 2012;23(8):140715. Calero A, Navas V, Rodriguez M, et al. Lanthanum carbon-
66. Isakova T, Gutierrez OM, Chang Y, Shah A, Tamez H, Smith K, ate reduces FGF23 in chronic kidney disease Stage 3 patients.
et al. Phosphorus binders and survival on hemodialysis. J Am Nephrol Dial Transplant 2011;26(8):256771.
Soc Nephrol 2009;20(2):38896. 84. Drueke TB. Lanthanum carbonate as a first-line phosphate
67. Kovesdy CP, Kuchmak O, Lu JL, Kalantar-Zadeh K. Outcomes binder: the cons. Semin Dial 2007;20(4):32932.
associated with phosphorus binders in men with non-dialysis- 85. Uhlig K, Berns JS, Kestenbaum B, Kumar R, Leonard MB,
dependent CKD. Am J Kidney Dis 2010;56(5):84251. Martin KJ, et al. KDOQI US commentary on the 2009 KDIGO
68. Russo D, Miranda I, Ruocco C, Battaglia Y, Buonanno E, Manzi Clinical Practice Guideline for the Diagnosis, Evaluation, and
S, et al. The progression of coronary artery calcification in pre- Treatment of CKD-Mineral and Bone Disorder (CKD-MBD). Am
dialysis patients on calcium carbonate or sevelamer. Kidney Int J Kidney Dis 2010;55(5):77399.
2007;72(10):125561. 86. Tentori F, Albert JM, Young EW, Blayney MJ, Robinson BM, Pisoni
69. Chertow GM, Burke SK, Raggi P. Sevelamer attenuates the pro- RL, etal. The survival advantage for haemodialysis patients taking
gression of coronary and aortic calcification in hemodialysis vitamin D is questioned: findings from the Dialysis Outcomes and
patients. Kidney Int 2002;62(1):24552. Practice Patterns Study. Nephrol Dial Transplant 2009;24(3):96372.
70. Qunibi W, Moustafa M, Muenz LR, He DY, Kessler PD, Diaz- 87. St Peter WL, Li S, Liu J, Gilbertson DT, Arneson TJ, Collins
Buxo JA, et al. A 1-year randomized trial of calcium acetate AJ. Effects of monthly dose and regular dosing of intravenous
versus sevelamer on progression of coronary artery calcifica- active vitamin D use on mortality among patients undergoing
tion in hemodialysis patients with comparable lipid control: the hemodialysis. Pharmacotherapy 2009;29(2):15464.
Calcium Acetate Renagel Evaluation-2 (CARE-2) study. Am J 88. Shoben AB, Rudser KD, de Boer IH, Young B, Kestenbaum B.
Kidney Dis 2008;51(6):95265. Association of oral calcitriol with improved survival in nondia-
71. Barreto DV, Barreto Fde C, de Carvalho AB, Cuppari L, Draibe lyzed CKD. J Am Soc Nephrol 2008;19(8):16139.
SA, Dalboni MA, et al. Phosphate binder impact on bone 89. Autier P, Gandini S. Vitamin D supplementation and total mor-
remodeling and coronary calcification results from the BRiC tality: a meta-analysis of randomized controlled trials. Arch
study. Nephron Clin Pract 2008;110(4):c27383. Intern Med 2007;167(16):17307.
72. Suki WN, Zabaneh R, Cangiano JL, Reed J, Fischer D, Garrett L, 90. Matias PJ, Jorge C, Ferreira C, Borges M, Aires I, Amaral T,
et al. Effects of sevelamer and calcium-based phosphate binders etal. Cholecalciferol supplementation in hemodialysis patients:
on mortality in hemodialysis patients. Kidney Int 2007;72(9):11307. effects on mineral metabolism, inflammation, and cardiac
73. St Peter WL, Liu J, Weinhandl E, Fan Q. A comparison of dimension parameters. Clin J Am Soc Nephrol 2010;5(5):90511.
sevelamer and calcium-based phosphate binders on mortality, 91. Thadhani R, Appelbaum E, Pritchett Y, Chang Y, Wenger J,
hospitalization, and morbidity in hemodialysis: a secondary anal- Tamez H, et al. Vitamin D therapy and cardiac structure and
ysis of the Dialysis Clinical Outcomes Revisited (DCOR) random- function in patients with chronic kidney disease: the PRIMO
ized trial using claims data. Am J Kidney Dis 2008;51(3):44554. randomized controlled trial. JAMA 2012;307(7):67484.
74. D'Haese PC, Spasovski GB, Sikole A, Hutchison A, Freemont TJ, 92. Kong J, Kim GH, Wei M, Sun T, Li G, Liu SQ, etal. Therapeutic
Sulkova S, etal. A multicenter study on the effects of lanthanum effects of vitamin D analogs on cardiac hypertrophy in sponta-
carbonate (Fosrenol) and calcium carbonate on renal bone dis- neously hypertensive rats. Am J Pathol 2010;177(2):62231.
ease in dialysis patients. Kidney Int Suppl 2003;85:S738. 93. Mathew S, Lund RJ, Chaudhary LR, Geurs T, Hruska KA.
75. Ferreira A, Frazao JM, Monier-Faugere MC, Gil C, Galvao J, Vitamin D receptor activators can protect against vascular calci-
Oliveira C, etal. Effects of sevelamer hydrochloride and calcium fication. J Am Soc Nephrol 2008;19(8):150919.
carbonate on renal osteodystrophy in hemodialysis patients. 94. Baker LR, Muir JW, Sharman VL, Abrams SM, Greenwood RN,
J Am Soc Nephrol 2008;19(2):40512. Cattell WR, et al. Controlled trial of calcitriol in hemodialysis
76. Freemont AJ, Hoyland JA, Denton J. The effects of lanthanum car- patients. Clin Nephrol 1986;26(4):18591.
bonate and calcium carbonate on bone abnormalities in patients 95. Salusky IB, Kuizon BD, Belin TR, Ramirez JA, Gales B,
with end-stage renal disease. Clin Nephrol 2005;64(6):42837. Segre GV, et al. Intermittent calcitriol therapy in secondary
VIII. THERAPEUTIC CONSIDERATIONS
662 53. Management of Mineral and Bone Disorders in Chronic Kidney Disease Patients
hyperparathyroidism: a comparison between oral and intraperi- 112. Martin KJ, Gonzalez EA, Gellens M, Hamm LL, Abboud
toneal administration. Kidney Int 1998;54(3):90714. H, Lindberg J. 19-Nor-1-alpha-25-dihydroxyvitamin D2
96. Coburn JW, Maung HM, Elangovan L, Germain MJ, Lindberg (Paricalcitol) safely and effectively reduces the levels of intact
JS, Sprague SM, et al. Doxercalciferol safely suppresses PTH parathyroid hormone in patients on hemodialysis. J Am Soc
levels in patients with secondary hyperparathyroidism associ- Nephrol 1998;9(8):142732.
ated with chronic kidney disease stages 3 and 4. Am J Kidney Dis 113. Chertow GM, Block GA, Correa-Rotter R, Drueke TB, Floege
2004;43(5):87790. J, Goodman WG, et al. Effect of cinacalcet on cardiovascu-
97. Coyne D, Acharya M, Qiu P, Abboud H, Batlle D, Rosansky S, etal. lar disease in patients undergoing dialysis. N Engl J Med
Paricalcitol capsule for the treatment of secondary hyperparathy- 2012;367(26):248294.
roidism in stages 3 and 4 CKD. Am J Kidney Dis 2006;47(2):26376. 114. Sprague SM, Abboud H, Qiu P, Dauphin M, Zhang P, Finn W.
98. Nordal KP, Dahl E. Low dose calcitriol versus placebo in Lanthanum carbonate reduces phosphorus burden in patients
patients with predialysis chronic renal failure. J Clin Endocrinol with CKD stages 3 and 4: a randomized trial. Clin J Am Soc Nephrol
Metab 1988;67(5):92936. 2009;4(1):17885.
99. Coyle EF, Coggan AR, Hopper MK, Walters TJ. Determinants of 115. Lindberg JS, Moe SM, Goodman WG, Coburn JW, Sprague SM,
endurance in well-trained cyclists. J Appl Physiol 1988;64(6):262230. Liu W, et al. The calcimimetic AMG 073 reduces parathyroid
100. Alborzi P, Patel NA, Peterson C, Bills JE, Bekele DM, Bunaye hormone and calcium x phosphorus in secondary hyperpara-
Z, et al. Paricalcitol reduces albuminuria and inflammation in thyroidism. Kidney Int 2003;63(1):24854.
chronic kidney disease: a randomized double-blind pilot trial. 116. Messa P, Macario F, Yaqoob M, Bouman K, Braun J, von
Hypertension 2008;52(2):24955. Albertini B, etal. The OPTIMA study: assessing a new cinacalcet
101. Fishbane S, Chittineni H, Packman M, Dutka P, Ali N, Durie N. (Sensipar/Mimpara) treatment algorithm for secondary hyper-
Oral paricalcitol in the treatment of patients with CKD and pro- parathyroidism. Clin J Am Soc Nephrol 2008;3(1):3645.
teinuria: a randomized trial. Am J Kidney Dis 2009;54(4):64752. 117. Chonchol M, Locatelli F, Abboud HE, Charytan C, de Francisco
102. de Zeeuw D, Agarwal R, Amdahl M, Audhya P, Coyne D, AL, Jolly S, et al. A randomized, double-blind, placebo-
Garimella T, et al. Selective vitamin D receptor activation with controlled study to assess the efficacy and safety of cinacal-
paricalcitol for reduction of albuminuria in patients with type cet HCl in participants with CKD not receiving dialysis. Am J
2 diabetes (VITAL study): a randomised controlled trial. Lancet Kidney Dis 2009;53(2):197207.
2010;376(9752):154351. 118. Charytan C, Coburn JW, Chonchol M, Herman J, Lien YH, Liu
103. Kandula P, Dobre M, Schold JD, Schreiber Jr MJ, Mehrotra R, W, et al. Cinacalcet hydrochloride is an effective treatment for
Navaneethan SD. Vitamin D supplementation in chronic kidney secondary hyperparathyroidism in patients with CKD not
disease: a systematic review and meta-analysis of observational receiving dialysis. Am J Kidney Dis 2005;46(1):5867.
studies and randomized controlled trials. Clin J Am Soc Nephrol 119. Raggi P, Chertow GM, Torres PU, Csiky B, Naso A, Nossuli K,
2011;6(1):5062. et al. The ADVANCE study: a randomized study to evaluate
104. Al-Aly Z, Qazi RA, Gonzalez EA, Zeringue A, Martin KJ. the effects of cinacalcet plus low-dose vitamin D on vascular cal-
Changes in serum 25-hydroxyvitamin D and plasma intact PTH cification in patients on hemodialysis. Nephrol Dial Transplant
levels following treatment with ergocalciferol in patients with 2011;26(4):132739.
CKD. Am J Kidney Dis 2007;50(1):5968. 120. Burnett SM, Gunawardene SC, Bringhurst FR, Juppner H, Lee
105. Zisman AL, Hristova M, Ho LT, Sprague SM. Impact of ergocal- H, Finkelstein JS. Regulation of C-terminal and intact FGF-
ciferol treatment of vitamin D deficiency on serum parathyroid 23 by dietary phosphate in men and women. J Bone Miner Res
hormone concentrations in chronic kidney disease. Am J Nephrol 2006;21(8):118796.
2007;27(1):3643. 121. Gutierrez OM, Wolf M, Taylor EN. Fibroblast growth factor 23,
106. Dogan E, Erkoc R, Sayarlioglu H, Soyoral Y, Dulger H. Effect of cardiovascular disease risk factors, and phosphorus intake in
depot oral cholecalciferol treatment on secondary hyperparathy- the Health Professionals Follow-up Study. Clin J Am Soc Nephrol
roidism in stage 3 and stage 4 chronic kidney diseases patients. 2011;6(12):28718.
Ren Fail 2008;30(4):40710. 122. Yilmaz MI, Sonmez A, Saglam M, Yaman H, Kilic S, Eyileten T,
107. Moe SM, Saifullah A, LaClair RE, Usman SA, Yu Z. A random- etal. Comparison of calcium acetate and sevelamer on vascular
ized trial of cholecalciferol versus doxercalciferol for lowering function and fibroblast growth factor 23 in CKD patients: a ran-
parathyroid hormone in chronic kidney disease. Clin J Am Soc domized clinical trial. Am J Kidney Dis 2012;59(2):17785.
Nephrol 2010;5(2):299306. 123. Gavine PR, Mooney L, Kilgour E, Thomas AP, Al-Kadhimi K,
108. Holick MF, Biancuzzo RM, Chen TC, Klein EK, Young A, Bibuld Beck S, etal. AZD4547: an orally bioavailable, potent, and selec-
D, et al. Vitamin D2 is as effective as vitamin D3 in maintain- tive inhibitor of the fibroblast growth factor receptor tyrosine
ing circulating concentrations of 25-hydroxyvitamin D. J Clin kinase family. Cancer Res 2012;72(8):204556.
Endocrinol Metab 2008;93(3):67781. 124. Miller PD, Roux C, Boonen S, Barton IP, Dunlap LE, Burgio DE.
109. Nigwekar SU, Bhan I, Thadhani R. Ergocalciferol and cholecal- Safety and efficacy of risedronate in patients with age-related
ciferol in CKD. Am J Kidney Dis 2012;60(1):13956. reduced renal function as estimated by the Cockcroft and Gault
110. Melamed ML, Thadhani RI. Vitamin D therapy in chronic kid- method: a pooled analysis of nine clinical trials. J Bone Miner Res
ney disease and end stage renal disease. Clin J Am Soc Nephrol 2005;20(12):210515.
2012;7(2):35865. 125. Ishani A, Blackwell T, Jamal SA, Cummings SR, Ensrud KE. The
111. Palmer SC, McGregor DO, Craig JC, Elder G, Macaskill P, effect of raloxifene treatment in postmenopausal women with
Strippoli GF. Vitamin D compounds for people with chronic kid- CKD. J Am Soc Nephrol 2008;19(7):14308.
ney disease not requiring dialysis. Cochrane Database Syst Rev
2009;(4):CD008175.
VIII. THERAPEUTIC CONSIDERATIONS
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Pentagon NLE Review NotesDokument33 SeitenPentagon NLE Review NotesChieChay Dub93% (123)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Fluid & ElectrolyteDokument26 SeitenFluid & Electrolytesanjana bhatia100% (1)
- Qatar Prometric ReviewerDokument7 SeitenQatar Prometric ReviewerValerieOchavoNoch keine Bewertungen
- Kdigo 2012 CKD GLDokument163 SeitenKdigo 2012 CKD GLOkky Sari Rahayu100% (1)
- Association Between Sodium Intakes With The Risk ofDokument7 SeitenAssociation Between Sodium Intakes With The Risk ofMaria MihailovNoch keine Bewertungen
- Biochemical Consequences of Chronic Renal FailureDokument14 SeitenBiochemical Consequences of Chronic Renal FailureMaria MihailovNoch keine Bewertungen
- 1349 7235 55 2759Dokument6 Seiten1349 7235 55 2759Maria MihailovNoch keine Bewertungen
- Journal of Epidemiology: Original ArticleDokument9 SeitenJournal of Epidemiology: Original ArticleMaria MihailovNoch keine Bewertungen
- JMedLife 09 449Dokument6 SeitenJMedLife 09 449Maria MihailovNoch keine Bewertungen
- JMedLife 09 449Dokument6 SeitenJMedLife 09 449Maria MihailovNoch keine Bewertungen
- Vitamine HidrosolubileDokument2 SeitenVitamine HidrosolubileMaria MihailovNoch keine Bewertungen
- DR - Aadi KHAN MOH EXAM 23 MAY 2017Dokument10 SeitenDR - Aadi KHAN MOH EXAM 23 MAY 2017FA KhanNoch keine Bewertungen
- Mineral MetabolismDokument12 SeitenMineral MetabolismPavan Kumar RNoch keine Bewertungen
- Chronic Kidney Disease: PathophysiologyDokument19 SeitenChronic Kidney Disease: PathophysiologyAnastasia Gaudensia Wewe WNoch keine Bewertungen
- Buchta 2003Dokument7 SeitenBuchta 2003lbNoch keine Bewertungen
- Clinical Chemistry Recall QuestionsDokument27 SeitenClinical Chemistry Recall QuestionschippaiqweqweNoch keine Bewertungen
- TumsDokument2 SeitenTumsAdrianne BazoNoch keine Bewertungen
- Neonatal HypocalcemiaDokument8 SeitenNeonatal HypocalcemiaCristina Fernández ValenciaNoch keine Bewertungen
- HypocalcemiaDokument2 SeitenHypocalcemiaRachel Frances SorillaNoch keine Bewertungen
- Nursing Care Plan Medical Surgical C: Student Name: Vi TranDokument18 SeitenNursing Care Plan Medical Surgical C: Student Name: Vi Tranapi-301819201Noch keine Bewertungen
- ZometaDokument6 SeitenZometaMisgi Candra DasaNoch keine Bewertungen
- Small Animal Clinical NutritionDokument14 SeitenSmall Animal Clinical NutritionJairo Pereira100% (1)
- Disorders of Calcium, Magnesium, and Phosphate BalanceDokument20 SeitenDisorders of Calcium, Magnesium, and Phosphate BalanceMarcela HincapiéNoch keine Bewertungen
- SERUM MINERAL LEVELSDokument8 SeitenSERUM MINERAL LEVELSprajakta kuralkarNoch keine Bewertungen
- Hypocalcemia Is Associated With Disease Severity in Patients With DengueDokument5 SeitenHypocalcemia Is Associated With Disease Severity in Patients With DengueDwitari Novalia HaraziNoch keine Bewertungen
- 0815 Skugor HyperAndHypocalcemiaDokument79 Seiten0815 Skugor HyperAndHypocalcemiaSirNorman BalinoNoch keine Bewertungen
- HypocalcemiaDokument34 SeitenHypocalcemiaClaudia IrimieNoch keine Bewertungen
- 3dr year Common Biochemistry MCQsDokument8 Seiten3dr year Common Biochemistry MCQsYasmin Amr NounouNoch keine Bewertungen
- Vaka TustimeDokument887 SeitenVaka TustimeMohamed AbbasNoch keine Bewertungen
- Neonatal HypocalcemiaDokument5 SeitenNeonatal HypocalcemiaLekshmi ManuNoch keine Bewertungen
- Causes, Symptoms and Treatments of HypocalcaemiaDokument2 SeitenCauses, Symptoms and Treatments of HypocalcaemiaPris AtarashiiNoch keine Bewertungen
- Calcium Gluconate Drug Classification, Dosage and Side EffectsDokument4 SeitenCalcium Gluconate Drug Classification, Dosage and Side EffectsStacy MC PelitoNoch keine Bewertungen
- HYPOCALCEMIADokument27 SeitenHYPOCALCEMIAJeffri SetiawanNoch keine Bewertungen
- A Safe and Effective'' Protocol For Management of Post-Thyroidectomy HypocalcemiaDokument8 SeitenA Safe and Effective'' Protocol For Management of Post-Thyroidectomy HypocalcemiaAsep HrNoch keine Bewertungen
- Parathyroid HormoneDokument120 SeitenParathyroid HormoneLaura TapiaNoch keine Bewertungen
- Fluids and ElectrolytesDokument19 SeitenFluids and Electrolytesderic100% (5)
- Calcium ImbalancesDokument3 SeitenCalcium ImbalancesAna Dominique EspiaNoch keine Bewertungen
- Pedoman Obat High AlertDokument6 SeitenPedoman Obat High AlertErvinaOctavianiNoch keine Bewertungen