Beruflich Dokumente
Kultur Dokumente
Jurnal Zinc Hiperbilirubinemia
Hochgeladen von
Abdurrohman IzzuddinCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Jurnal Zinc Hiperbilirubinemia
Hochgeladen von
Abdurrohman IzzuddinCopyright:
Verfügbare Formate
Open Access Original Article
The Therapeutic Effect of Zinc Sulfate on Neonatal Hyper-
bilirubinemia
Somayyeh Hashemian1, Ashraf Mohammadzadeh2*, Ahmadshah Farhat2, Mohammad
Ramezani3, Seyed Javad Seyedi4
1. Department of Pediatric Endocrinology and Metabolism .Imam Reza Hospital , Faculty of Medicine, Mashhad University of Medical Sciences , Mashhad,
Iran
2. ween the 3rd and 7th days of life was also more significant among the zinc sulfate group Medical Sciences, Mashhad, Iran
3. Pharmaceutical and Biotechnology Research Center, School of Pharmacy, Mashhad University of Medical Sciences, Mashhad, Iran
4. Neonatal Research Center, Imam Reza Hospital, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
ABSTRACT
Background: Approximately 60% of term neonates and 80% of preterm ones suffer from hyperbilirubinemia in their
first week of life. This study sought to characterize the therapeutic effect of oral zinc sulfate on neonatal
hyperbilirubinemia.
Methods: In this randomized, double-blind, placebo-controlled clinical trial, 70 term neonates with total serum
bilirubin (TSB) level 20 mg/dl were enrolled. Thirty-four cases were treated with phototherapy and zinc (10 mg/day,
single dose) as case, while the remainder received phototherapy plus placebo. TSB level was measured at the onset of
the intervention, as well as 12, 24 and 48 h after the intervention and compared with each other.
Results: The mean TSB levels were significantly lower in the zinc group after 12, 24 and 48 h (P=0.038, 0.005, 0.001,
respectively). The mean durations of phototherapy in the case and control groups were 2.030.174 and 2.330.478
days, respectively, being significantly less in the case group (P=0.002).
Conclusion: This study revealed that oral zinc sulfate at a single dose of 10 mg/day diminished TSB level and duration
of phototherapy.
Keywords: Hyperbilirubinemia, Neonate, Treatment, Zinc sulfate
Introduction
In the recent years, a substantial body of sequel (1, 5). Such complications underscore the
research has been carried out to predict neonates importance of finding further treatments for this
who are most likely to develop hyperbilirubinemia. disease. As of yet, phototherapy and exchange
Reliable prediction can reduce hospital stay for transfusion were the treatment of choice in such
low-risk neonates and identify high-risk neonates cases; however, both of these approaches have
facilitating their closer follow-up (1). several disadvantages (4).
In general, 60% of term newborns and 80% of Exchange transfusion poses the risk of graft
preterm ones present with hyperbilirubinemia in versus host disease and a higher mortality rate
their first week of life (2, 3). The incidence of severe (2). Phototherapy induces parental anxiety due to
neonatal hyperbilirubinemia is the highest in hospitalization and cost of care. Furthermore, it
Asians (2), accounting for one-thirds of neonatal hinders mother-infant bonding. Drug therapy, on
admissions in Iran (3). Jaundice in such cases is the other hand, is more practical, acceptable and
mainly physiologic and diagnosed by ruling out cost-effective.
other causes of jaundice such as hemolysis, In several studies, the associations between
infection, or metabolic diseases, whereas 5-10% microneutrients and jaundice have been proposed.
require intervention (3, 4). The fundamental aim of Some of them, such as zinc sulfate, bind to bilirubin
detecting and treating severe neonatal jaundice is in the small intestine, reduce its absorption and
to prevent bilirubin encephalopathy and its chronic therefore prevent enterohepatic circulation, but
* Corresponding author: Ashraf Mohammadzadeh, Neonatal Research Center, Imam Reza Hospital, Faculty of Medicine, Mashhad
University of Medical Sciences, Mashhad, Iran. Tel: (+98)5118521121; Fax: (+98) 5118525316; Email: mohamadzadeha@mums.ac.ir
Please cite this paper as:
Hashemian S, Mohammadzadeh A, Farhat A, Ramezani M, Seyedi SJ. The Therapeutic Effect of Zinc Sulfate on Neonatal
Hyperbilirubinemia. 2017 Jun: 8(2). DOI: 10.22038/ijn.2016.7777
Hashemian S et al Effect of Zinc Sulfate on Hyperbilirubinemia
with inconsistent results (1, 6). nurses were explained to repeat the dose after 5-
Zinc is one of the essential elements in 10 min if the child vomited the drug.
neonatal growth, protein synthesis and regulation Total and direct serum bilirubin levels were
of inhibitory and stimulatory synapses of the measured at the outset of the intervention, as well
brain. It has been shown to lower bilirubin level as 12, 24 and 48 h after receiving the intervention
by inhibition of the normal enterohepatic cycling and in cases of extended hospitalization after 72 h.
of unconjugated bilirubin (7-9). Therefore, the A written informed consent was signed by the
anticipated role of zinc supplementation in parents of each infant prior to the study. The
neonatal jaundice seems to be an attractive issue. parents were assured that they could withdraw
This randomized clinical trial was conducted their neonates from the study at any time.
on term neonates to characterize the therapeutic The study protocol was approved by the
effect of oral zinc sulfate on neonatal jaundice. Ethics Committee of the Deputy of Research of
Mashhad University of Medical Sciences
Methods (IRCT201306031162N19).
This randomized, double-blind, placebo-
controlled clinical trial was performed during Statistical analysis
July-December 2013. Seventy term neonates who The minimum sample size was calculated based
were admitted to neonatal intensive care unit of on Babaei et al. study (12). Data were analyzed
Imam Reza Hospital of Mashhad, Iran, were using SPSS, version 11.5. Quantitative variables are
selected for the study. The inclusion criteria presented as meanstandard deviation. The normal
comprised of gestational age 38 weeks, birth distribution of variables was proved by
weight 2500 gr and total serum bilirubin level Kolmogorov-Smirnov test. We used independent
20 mg/dl. All cases with hemolysis, glucose-6- samples t-test and Mann-Whitney U test for
phosphate dehydrogenase deficiency disease, comparison of the variables with and without
sepsis, severe respiratory disease requiring normal distribution, respectively. Pearson
mechanical ventilation, congenital anomalies and correlation coefficient and Chi-squared test were
a total serum bilirubin (TSB) of exchange level on used for comparison of qualitative variables.
admission were excluded. Among the 70 enrolled P-value less than 0.05 was considered statistically
neonates, four cases were excluded due to significant.
mechanical removal of bilirubin after exchange
blood transfusion (1 case and 3 controls). Serum Results
bilirubin level was measured using Unistar In the present study, 66 term newborns
Bilirubinometer (Reichert-Jung, Germany). Direct completed the study (n=33 for each group). There
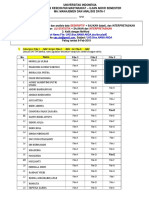
bilirubin was determined by the colorimetric were no significant differences between the two
method proposed by Lathe and Ruthven. groups regarding age, sex, date of jaundice onset,
Phototherapy initiation, duration and termi- mothers parity, route of delivery, birth weight
nation point were decided based on the American and weight at inclusion (Table 1).
Academy of Pediatrics guidelines (AAP 2004) Moreover, laboratory indices including
(10). Each phototherapy unit had four special blue reticulocyte count, hematocrit, as well as total and
lamps (Philips Co, Germany) and was adjusted to direct bilirubin were measured, showing no
25 cm above the infants cots. remarkable differences between the two groups
All the neonates received phototherapy during (Table 1).
the study period. In the study group, besides In the current study, at the first visit which was
phototherapy, 10 mg/day zinc sulfate was 12 h after receiving the medication, a significant
prescribed by the treating physician at a single difference was observed between the zinc and
dose in the form of syrup (based on Maamouri et placebo groups regarding total serum bilirubin
al. study) (11). level (P=0.038). This difference was also present
The control group received placebo with a 24 and 48 h after initiating the medication
similar color, taste, volume and package to the (P=0.005 and 0.001, respectively). Direct serum
zinc sulfate syrup for the same duration and at the bilirubin showed no significant differences
same dosage. The zinc and placebo syrups were between the two groups over time.
distributed by a single physician who was blinded Figure 1 depicts the changes in total serum
to the group allocations and the study protocol. bilirubin level (mg/dl) over time compared to
The pediatrician who visited the neonates was baseline in the two groups.
also blind to the type of intervention. The on-duty Changes in total and direct serum bilirubin
14 Iranian Journal of Neonatology 2017; 8(2)
Effect of Zinc Sulfate on Hyperbilirubinemia Hashemian S et al
Table 1. Demographic characteristics of the case and control groups
Zn Placebo P-value
Sex (%Female) 41.2 47.2 0.611
Age (day) 6.62.57 5.81.89 0.138
Date of jaundice onset (day) 3.31.35 3.00.95 0.300
Parity (Number) 1.40.65 1.60.75 0.326
Delivery route (%NVD) 75.0 52.0 0.095
Birth weight (gr) 3080.7564.60 3155.2458.17 0.592
Weight at inclusion (gr) 3159.6489.37 3173.0437.74 0.915
Hematocrit (%) 46.55.90 45.95.40 0.641
Reticulocyte count (%) 1.31.45 1.01.01 0.487
Total serum bilirubin (mg/dl) 22.52.31 21.51.61 0.052
Direct serum bilirubin (mg/dl) 0.620.218 0.670.224 0.718
with phototherapy can significantly reduce TSB
level. Moreover, we found a significant difference
in the mean TSB levels after 12, 24 and 48 h of
treatment between the zinc and placebo groups,
suggesting that zinc sulfate may play a certain role
in reducing neonatal hyperbilirubinemia.
Drug therapy is associated with high compliance
and low cost of care. Clofibrate, phenobarbtal, bile
salts, dipenycilamine, and zinc compounds were
found to act through different mechanisms such as
production inhibition, stimulation of hepatic
clearance and enzymatic inhibition (3, 13-16).
Figure 1. Changes in mean total serum bilirubin level over However, none of them has been proposed as a
time in the study and control groups common therapeutic method so far.
Zinc salts were demonstrated to be promising
in Table 2. both in-vitro and in-vivo (1). In other words, the
Moreover, one of the case and 11 of the control action of zinc in hyperbilirubinemia depends on
group subjects required treatment continuation its ability to reach the distal intestine where it is
up to 72 h. The other infants were all discharged once again absorbed into the blood, and therefore,
after 48 h of treatment. reduces the enterohepatic circulation.
The mean durations of phototherapy in the The first human study on this issue was carried
case and control groups were 2.030.174 and out by Mendez-Sanchez et al. on 20 adult patients
2.330.478 days, respectively, showing a of Gilbert syndrome. They reported that zinc sulfate
significantly shorter duration in the zinc sulfate significantly decreased serum unconjugated
group based on Mann-Whitney test (P=0.002). bilirubin level (9).
During the treatment period, no drug-related In another study, Rana et al. (1) investigated
side effects were observed in either group. the impact of oral zinc salt on the incidence of
hyperbilirubinemia and need for phototherapy in
Discussion term and late-preterm at-risk neonates between 25
This study revealed that zinc sulfate and 168 h of age. They concluded that twice-daily
supplementation at a dose of 10 mg/day along
Table 2. Changes in total and direct serum bilirubin levels after the intervention
Zn (n=33) Control (n=33)
Plasma bilirubin level (mg/dl) Mean (SD) Mean (SD) P-value
range range
22.5 (2.31) 21.5 (1.61)
Total serum bilirubin, baseline 0.052
20-26 20-26.5
17.3 (1.62) 18.2 (1.33)
Total serum bilirubin, after 12h 0.038
14.2-21.9 15.6-22.0
13.8 (1.98) 15.2 (1.72)
Total serum bilirubin, after 24h 0.005
7.1-17.4 12.3-18.0
10.3 (2.09) 11.9 (1.74)
Total serum bilirubin, after 48h 0.001
6.0-13.0 7.7-15.5
11.4 (1.17)
Total serum bilirubin, after 72h 8.6 0.045
9.8-12.6
15 Iranian Journal of Neonatology 2017; 8(2)
Hashemian S et al Effect of Zinc Sulfate on Hyperbilirubinemia
administration of oral zinc at a dose of 10 mg does Recommended Dietary Allowance recommend-
not reduce the incidence of hyperbilirubinemia in dations and the available literature, yet a different
such cases during the first week of life (1). dosage may have resulted differently. In addition,
Mosayebi et al. evaluated the serum zinc level starting the treatment sooner might have
alterations before and after phototherapy in influenced our findings and limited the impact of
hyperbilirubinemic newborns. They concluded other variables existing between birth and
that phototherapy increases serum zinc level by admission. Furthermore, we did not check the zinc
reducing bilirubin level, such that additional serum level before and after the intervention.
supplementation of this element can potentially
lead to zinc toxicity (17). Conclusion
Mafinejad et al. (2012) studied the prophylactic Administering oral zinc sulfate at a single dose
effects of zinc sulfate in neonatal hyperbilirubinemia. of 10 mg/day reduced the mean TSB level and
They showed that administration of zinc sulfate duration of phototherapy. Zinc, as a micronutrient,
neither affected hyperbilirubinemia nor delayed may be recommended as a safe and effective
jaundice manifestation. They observed that the medication in neonatal non-hemolytic jaundice
duration of phototherapy and hospitalization were besides phototherapy. Further studies with larger
less in zinc group. Weight gain between the 3rd and sample sizes, different dosages and formulations
7th days of life was also more significant among the of zinc, and more precise laboratory studies are
zinc sulfate group (11). recommended to confirm our findings.
In Vitek et al. study, the oral administration of
zinc salts efficiently decreased serum bilirubin Acknowledgments
level in hyperbilirubinemic rats, most probably The authors wish to thank Deputy of Research
due to the inhibition of enterohepatic circulation of Mashhad University of Medical Sciences for
of bilirubin. They suggested that this approach funding this project. We would also like to extend
might be useful for the treatment of severe our gratitude to Miss Mozhdeh Mahmoodi for data
unconjugated hyperbilirubinemia (8). capture and Miss Najmeh Saberi for her assistance
Nevertheless, Patton et al. studied the effect of with typing the article.
oral zinc on 60 neonates with hyperbilirubinemia.
The neonates received 5 mg oral zinc twice daily Conflicts of interests
for five days. They reported that bilirubin level None
measurement on day 5 of treatment showed no
significant difference between the two groups in References
terms of duration of hyperbilirubinemia (18). 1. Rana N, Mishra S, Bhatnagar S, Paul V, Deorari AK,
The present study also showed that although Agarwal R. Efficacy of zinc in reducing
zinc sulfate administration was not associated with hyperbilirubinemia among at-risk neonates: a
any reduction in the proportion of neonates randomized, double-blind, placebo-controlled trial.
requiring phototherapy, it did curtail phototherapy Indian J Pediatr. 2011; 78(9):1073-8.
2. Stoll BJ, Kliegman RM. Jaundice and hyper-
duration compared to controls. A shorter duration
bilirubinemia. In: Kliegman RM, Behrman RE, Jenson
by itself is highly beneficial as it can lead to earlier HB, Stanton BM, editors. Nelson textbook of
mother-infant bonding and impose lower costs on pediatric. 17th ed. Philadelphia: WB Saunders; 2011.
the medical system besides reducing possible side P. 592-8.
effects in the newborn. 3. Mohammadzadeh A, Farhat AS, Iranpour R. Effect of
Regarding several previous studies performed clofibrate in jaundiced term newborns. Indian J
on children with diarrhea, measles, pneumonia, Pediatr. 2005; 72(2):123-6.
common cold and malaria, we decided to use oral 4. Kaplan M, Wong RJ, Sibley E, Stevenson DK.
zinc as a safe agent at a single dose of 10 mg/day Neonatal jaundice and liver disease. In: Martin RJ,
(19-21). Accordingly, zinc sulfate syrup was well- Fanaroff A, Walsh MC, editors. Fanaroff and Martin's
Neonatal-Perinatal Medicine: diseases of the fetus
tolerated by the newborns and no side effects and infant. 9th ed. New York: Elsevier Health
were observed. It seems that zinc, as a Sciences; 2011. P. 1443-96.
micronutrient and a safe drug, can be beneficial in 5. Shapiro SM. Bilirubin toxicity in the developing
reducing bilirubin level in neonates through nervous system. Ped Neurol. 2003; 29(5):41021.
inhibition of enterohepatic circulation. 6. Odell GB, Gutchetr GR, Whitington PF, Yang G. Enteral
There were a few limitations in the current administration of agar as an effective adjunct to
study. The study had a small sample size and phototherapy of neonatal hyperbilirubinemia. Pediatr
although the dose of zinc was decided based on Res. 1983; 17(10):8104.
16 Iranian Journal of Neonatology 2017; 8(2)
Effect of Zinc Sulfate on Hyperbilirubinemia Hashemian S et al
7. Mendez-Sanchez N, Roldan-Valadez E, Flores MA, low birth weight neonates. J Hematol Oncol. 2009;
Cardenas-Vazquez R, Uribe M. Zinc salts precipitate 26(4):100-5.
unconjugated bilirubin in vitro and inhibit 15. Mohammadzadeh A, Farhat AS, Jafarzadeh M,
enterohepatic cycling of bilirubin in hamsters. Eur J Mirzarahimi M, Esmaeli H, Amiri R. Prophylactic
Clin Invest. 2001; 31(9):77380. effect of clofibrate in low birth weight neonate's
8. Vitek L, Munchova L, Zelenka J, Zadinova M, Malina J. hyperbilirobinemia. J Chinese Clin Med. 2008,
The effect of zinc salts on serum bilirubin levels in 3(3):140-4.
hyperbilirubinemic rats. J Pediatr Gastroenterol 16. Ashraf M, Ahmadshah F, Habibullah E, Niloofar J.
Nutr. 2005; 40(2):13540. Prophylactic effect of clofibrate on hyperbilirubinemia
9. Mendez-Sanchez N, Martinez M, Gonzalez V, Roldan- in verylow birth weight twins. Br J Pharmac Res. 2014;
Valadez E, Flores MA, Uriebe MA. Zinc Sulfate inhibits 4(7):818-25.
the enterohepatic circulation of unconjugated bilirubin 17. Mosayebi Z, Rahmani M, Behjati Ardakani S, Sheikh
in subjects with Gilbert syndrome. Ann Hepatol. 2002; M, Shariat M, Rezaeizadeh G. Evaluation of serum
1(1):403. zinc levels in hyperbilirubinemic neonates before
10. American Academy of Pediatrics Subcommittee on and after phototherapy. Iran J Pediatr. 2016;
Hyperbilirubinemia. Management of hyperbili- 26(3):e4146.
rubinemia in the newborn Infant 35 or more weeks of 18. Patton P, Rachmadi D, Sukadi A. Effect of oral zinc
gestation. Pediatrics. 2004; 114(1):297316. on hyperbilirubinemia in full term neonates.
11. Maamouri G, Boskabadi H, Mafinejad S, Bozorgnia Y, Paediatr Indonesian. 2011; 51(2):107-10.
Khakshur A. Efficacy of oral zinc sulfate intake in 19. Lamberti LM, Walker CL, Chan KY, Jian WY, Black
prevention of neonatal jaundice. Iran J Neonatol. RE. Oral zinc supplementation for the treatment of
2014; 4(4):116. acute diarrhea in children: a systematic review and
12. Babaei H, Hemmati M, Fallahi V, Rezaei M. Effect of meta-analysis. Nutrients. 2013; 5(11):4715-40.
oral zinc sulfate in prevention of jaundice in healthy 20. Bahl R, Bhandari N, Saksena M, Strand T, Kumar
term newborns. J Kermanshah Univ Med Sci. 2014; GT, Bhan MK, et al. Efficacy of zinc fortified oral
17(11):6806. rehydration solution in 6- to 35-month-old
13. Ebrahimimd S, Ashkani-Esfahani S, Poormahmudibs children with acute diarrhea. J Pediatr. 2002;
A. Investigating the efficacy of zizyphus jujuba on 141(5):67782.
neonatal jaundice. Iran J Pediatr. 2011; 21(3):320-4. 21. Fischer C, Harvey P. Low risk of adverse effects from
14. Mohammadzade A, Farhat AS, Amiri R, Esmaely H, zinc supplementation. New York: The USAID
Bagheri S. Treatment effect of clofibrate in jaundiced Micronutrient Program; 2006.
17 Iranian Journal of Neonatology 2017; 8(2)
Das könnte Ihnen auch gefallen
- Contract of Lease (711) - AguilarDokument7 SeitenContract of Lease (711) - AguilarCoy Resurreccion Camarse100% (2)
- IIT JEE Physics Preparation BooksDokument3 SeitenIIT JEE Physics Preparation Booksgaurav2011999Noch keine Bewertungen
- Food Combining PDFDokument16 SeitenFood Combining PDFJudas FK TadeoNoch keine Bewertungen
- 4-Page 7 Ways TM 20Dokument4 Seiten4-Page 7 Ways TM 20Jose EstradaNoch keine Bewertungen
- Apley's System of Orthopaedics and Fractures 9th Edition PDFDokument993 SeitenApley's System of Orthopaedics and Fractures 9th Edition PDFInggriht Senny Bondang96% (53)
- ANSI-ISA-S5.4-1991 - Instrument Loop DiagramsDokument22 SeitenANSI-ISA-S5.4-1991 - Instrument Loop DiagramsCarlos Poveda100% (2)
- HyperbilirubinemiaDokument4 SeitenHyperbilirubinemiaJuan Carlos Andrade SalumNoch keine Bewertungen
- PhototherapyDokument6 SeitenPhototherapyMultazam ZulfikarNoch keine Bewertungen
- Jurnal 3Dokument8 SeitenJurnal 3Siska YunitaNoch keine Bewertungen
- Phototherapy Induced Hypocalcemia in Neonates: A Case-Control Prospective StudyDokument5 SeitenPhototherapy Induced Hypocalcemia in Neonates: A Case-Control Prospective Studyrandomized1234Noch keine Bewertungen
- Pharmacokinetics of anti-TB Drugs in Malawian Children: Reconsidering The Role of EthambutolDokument6 SeitenPharmacokinetics of anti-TB Drugs in Malawian Children: Reconsidering The Role of EthambutolIsmi Azisa Chaeria SaputriNoch keine Bewertungen
- Synopsis Phototherapy in JaunicDokument5 SeitenSynopsis Phototherapy in JaunicEngr Saeed Ur RehmanNoch keine Bewertungen
- Ijcp-5538 oDokument5 SeitenIjcp-5538 oDrkaleembrimsNoch keine Bewertungen
- Jemc V5i2 23384Dokument6 SeitenJemc V5i2 23384Students CBUNoch keine Bewertungen
- The Effect of Human Recombinant Erythropoietin On Prevention of Anemia of PrematurityDokument6 SeitenThe Effect of Human Recombinant Erythropoietin On Prevention of Anemia of PrematuritySri Nowo MinartiNoch keine Bewertungen
- HealthDokument3 SeitenHealthsri309Noch keine Bewertungen
- Jurnal AnakDokument5 SeitenJurnal Anakariani khikmatul mazidahNoch keine Bewertungen
- IJP - Volume 8 - Issue 9 - Pages 11939-11944Dokument6 SeitenIJP - Volume 8 - Issue 9 - Pages 11939-11944A'la Nur RoyanNoch keine Bewertungen
- Jurnal Reading AiDokument14 SeitenJurnal Reading AiMohammad AlmuhaiminNoch keine Bewertungen
- Effect of Foot Reflexology On Neonatal JaundiceDokument7 SeitenEffect of Foot Reflexology On Neonatal JaundiceSarini Suryadi100% (1)
- Jurnal Anak 1Dokument7 SeitenJurnal Anak 1Luciana LorenzaNoch keine Bewertungen
- Knowledge Level and Determinants of Neonatal Jaundice A Cross-Sectional Study in The Effutu Municipality of GhanaDokument10 SeitenKnowledge Level and Determinants of Neonatal Jaundice A Cross-Sectional Study in The Effutu Municipality of GhananicloverNoch keine Bewertungen
- Evaluation of Gastric Aspirate Shake Test in Predicting Surfactant Need in Preterm Infants With Neonatal Respiratory Distress Syndrome A Cross-Sectional StudyDokument9 SeitenEvaluation of Gastric Aspirate Shake Test in Predicting Surfactant Need in Preterm Infants With Neonatal Respiratory Distress Syndrome A Cross-Sectional StudyVita DesriantiNoch keine Bewertungen
- JaundiceDokument4 SeitenJaundiceAndhitNoch keine Bewertungen
- 2006-Intravenous Immunoglobulin in ABO and RH Hemolytic Diseases of NewbornDokument4 Seiten2006-Intravenous Immunoglobulin in ABO and RH Hemolytic Diseases of Newborn蔡黑面Noch keine Bewertungen
- A Randomized, Controlled Trial of Liraglutide For Adolescents With ObesityDokument12 SeitenA Randomized, Controlled Trial of Liraglutide For Adolescents With ObesityWarun KumarNoch keine Bewertungen
- Navodaya College of Nursing: Proforma For Registration of Subjects ForDokument18 SeitenNavodaya College of Nursing: Proforma For Registration of Subjects ForStephy SojanNoch keine Bewertungen
- A Randomized, Controlled Trial of Liraglutide For Adolescents With ObesityDokument12 SeitenA Randomized, Controlled Trial of Liraglutide For Adolescents With ObesityJosé Luis ChavesNoch keine Bewertungen
- Zinc As An Adjunct Therapy in The Management of Severe Pneumonia Among Gambian Children: Randomized Controlled TrialDokument19 SeitenZinc As An Adjunct Therapy in The Management of Severe Pneumonia Among Gambian Children: Randomized Controlled TrialDicky rahadianNoch keine Bewertungen
- BMC Pediatrics: Management of Neonatal Hyperbilirubinemia: Pediatricians' Practices and Educational NeedsDokument7 SeitenBMC Pediatrics: Management of Neonatal Hyperbilirubinemia: Pediatricians' Practices and Educational Needsmaya maeNoch keine Bewertungen
- Tatalaksana PJBDokument5 SeitenTatalaksana PJBmayaNoch keine Bewertungen
- Journal Club: Surfactant Therapy in Premature InfantsDokument44 SeitenJournal Club: Surfactant Therapy in Premature InfantsSubash PaudealNoch keine Bewertungen
- 1607 4536 1 PBDokument7 Seiten1607 4536 1 PBdianNoch keine Bewertungen
- Pengaruh Pemberian Modifikasi Posisi Bayi Pada Pasien Fototerapi Terhadap Derajat Ikterik Pada Bayi Baru Lahir Di RSU Mitra DelimaDokument6 SeitenPengaruh Pemberian Modifikasi Posisi Bayi Pada Pasien Fototerapi Terhadap Derajat Ikterik Pada Bayi Baru Lahir Di RSU Mitra DelimaerlitaNoch keine Bewertungen
- Journal Club PDADokument30 SeitenJournal Club PDASnehal PatilNoch keine Bewertungen
- Therapeutic Effects of Oral Zinc Supplementation On Acute Watery Diarrhea With Moderate Dehydration: A Double-Blind Randomized Clinical TrialDokument7 SeitenTherapeutic Effects of Oral Zinc Supplementation On Acute Watery Diarrhea With Moderate Dehydration: A Double-Blind Randomized Clinical TrialRizqulloh Taufiqul Hakim BarsahNoch keine Bewertungen
- Jurnal 2 AnakDokument5 SeitenJurnal 2 AnakHafich ErnandaNoch keine Bewertungen
- JN 212308Dokument8 SeitenJN 212308Ivhajannatannisa KhalifatulkhusnulkhatimahNoch keine Bewertungen
- A Nurse-Initiated Jaundice Management Protocol Improves Quality of Care in The Paediatric Emergency DepartmentDokument5 SeitenA Nurse-Initiated Jaundice Management Protocol Improves Quality of Care in The Paediatric Emergency DepartmentDr-Dalya ShakirNoch keine Bewertungen
- High-Intensity Phototherapy For The Treatment of Severe Nonhaemolytic Neonatal HyperbilirubinemiaDokument4 SeitenHigh-Intensity Phototherapy For The Treatment of Severe Nonhaemolytic Neonatal HyperbilirubinemiamoyretnowulanNoch keine Bewertungen
- Avaluació I TractamentDokument10 SeitenAvaluació I Tractamentanollaru38Noch keine Bewertungen
- Hyperbilirubinemia, Phototherapy, and Childhood Asthma: ObjectivesDokument11 SeitenHyperbilirubinemia, Phototherapy, and Childhood Asthma: ObjectivesrizaniaNoch keine Bewertungen
- Proca 3Dokument10 SeitenProca 3alejandro1122Noch keine Bewertungen
- Iatrogenic Severe Hyperglycemia Due To Parenteral Administration of Glucose in Children - A Case Series PDFDokument7 SeitenIatrogenic Severe Hyperglycemia Due To Parenteral Administration of Glucose in Children - A Case Series PDFSultan Rahmat SeptianNoch keine Bewertungen
- Jaundice EatingDokument15 SeitenJaundice Eatingraja yasminNoch keine Bewertungen
- A Randomised Dose-Ranging Study of Tiotropium Respimat® in Children With Symptomatic Asthma Despite Inhaled CorticosteroidsDokument10 SeitenA Randomised Dose-Ranging Study of Tiotropium Respimat® in Children With Symptomatic Asthma Despite Inhaled CorticosteroidsabdmaliknasNoch keine Bewertungen
- 1008-Main Article Text (Blinded Article File) - 2118-3-10-20200715Dokument3 Seiten1008-Main Article Text (Blinded Article File) - 2118-3-10-20200715putrinrainiNoch keine Bewertungen
- Diagnostic Value of Gastric Shake Test For Hyaline Membrane Disease in Preterm InfantDokument7 SeitenDiagnostic Value of Gastric Shake Test For Hyaline Membrane Disease in Preterm InfantJonathan JonesNoch keine Bewertungen
- Nifedipine Versus Terbutaline, Tocolytic Effectiveness and Maternal and Neonatal Adverse Effects: A Randomized, Controlled Pilot TrialDokument7 SeitenNifedipine Versus Terbutaline, Tocolytic Effectiveness and Maternal and Neonatal Adverse Effects: A Randomized, Controlled Pilot TrialkennydimitraNoch keine Bewertungen
- Clinical Study: Safety and Efficacy of Misoprostol Versus Oxytocin For The Prevention of Postpartum HemorrhageDokument5 SeitenClinical Study: Safety and Efficacy of Misoprostol Versus Oxytocin For The Prevention of Postpartum HemorrhageTasya Arsy LiyanaNoch keine Bewertungen
- Clinical Study: Safety and Efficacy of Misoprostol Versus Oxytocin For The Prevention of Postpartum HemorrhageDokument5 SeitenClinical Study: Safety and Efficacy of Misoprostol Versus Oxytocin For The Prevention of Postpartum HemorrhageMuhammad Ghifari RifanshaNoch keine Bewertungen
- Srep08219 PDFDokument8 SeitenSrep08219 PDFLinda JajauuooNoch keine Bewertungen
- 113 JMSCRDokument12 Seiten113 JMSCRRiki AntoNoch keine Bewertungen
- Am J Clin Nutr 2013 Wadhwa 1387 94Dokument8 SeitenAm J Clin Nutr 2013 Wadhwa 1387 94annisanadyapNoch keine Bewertungen
- Jurnal Pendukung 1.Dokument9 SeitenJurnal Pendukung 1.Risky PerdanaNoch keine Bewertungen
- The Effects of Betamethasone On Clinical Outcome of The Late Preterm Neonates Born Between 34 and 36 Weeks of GestationDokument17 SeitenThe Effects of Betamethasone On Clinical Outcome of The Late Preterm Neonates Born Between 34 and 36 Weeks of GestationjeffyNoch keine Bewertungen
- Prevention of TB Using Rifampicin Plus Isoniazid Reduces Nevirapine Concentrations in HIV-exposed InfantsDokument7 SeitenPrevention of TB Using Rifampicin Plus Isoniazid Reduces Nevirapine Concentrations in HIV-exposed InfantsSorina ElenaNoch keine Bewertungen
- Jurnal Berpikir KritisDokument9 SeitenJurnal Berpikir KritisNindita IllahiNoch keine Bewertungen
- 2020 Article 2459Dokument9 Seiten2020 Article 2459Chong ArthinantNoch keine Bewertungen
- 10.1007@s12098 020 03454 1Dokument6 Seiten10.1007@s12098 020 03454 1rayhantaswinNoch keine Bewertungen
- The Effect of Phototherapy (24 Hours) Towards Jaundice Degrees of The Newborn in Hospital Nicu West Nusa Tenggara ProvinceDokument9 SeitenThe Effect of Phototherapy (24 Hours) Towards Jaundice Degrees of The Newborn in Hospital Nicu West Nusa Tenggara ProvinceAnonymous nGCyG4nqhNoch keine Bewertungen
- Impact of Oligohydramnios On Maternal and PerinataDokument6 SeitenImpact of Oligohydramnios On Maternal and PerinataDiana SchlittlerNoch keine Bewertungen
- Neonatal Jaundice Literature ReviewDokument6 SeitenNeonatal Jaundice Literature Reviewaflsmawld100% (1)
- Infantile Hypertrophic Pyloric Stenosis at A TertiDokument7 SeitenInfantile Hypertrophic Pyloric Stenosis at A TertiVașadi Razvan CristianNoch keine Bewertungen
- TugasDokument12 SeitenTugasLola SantiaNoch keine Bewertungen
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalVon EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalNoch keine Bewertungen
- EngDokument48 SeitenEngnina nurhayatiNoch keine Bewertungen
- Jurnal InvaginasiDokument3 SeitenJurnal InvaginasiAbdurrohman IzzuddinNoch keine Bewertungen
- HFSA Focused Update of The Management of Heart Failure UCM - 493384Dokument33 SeitenHFSA Focused Update of The Management of Heart Failure UCM - 493384Monica SunataNoch keine Bewertungen
- BiosDokument6 SeitenBiosDevinaNoch keine Bewertungen
- Algoritma CHFDokument1 SeiteAlgoritma CHFdiany astutiNoch keine Bewertungen
- Psqi Sleep QuestionnaireDokument1 SeitePsqi Sleep QuestionnaireOverSkyLordNoch keine Bewertungen
- The Ocular Surface: SciencedirectDokument8 SeitenThe Ocular Surface: SciencedirectMakmur SejatiNoch keine Bewertungen
- Galor, 2013Dokument3 SeitenGalor, 2013Abdurrohman IzzuddinNoch keine Bewertungen
- Sexual Fetishism in A Quail (Coturnix Japonica) Model System: Test of Reproductive SuccessDokument6 SeitenSexual Fetishism in A Quail (Coturnix Japonica) Model System: Test of Reproductive SuccessAbdurrohman IzzuddinNoch keine Bewertungen
- Jurnal Shah 2010Dokument24 SeitenJurnal Shah 2010Abdurrohman IzzuddinNoch keine Bewertungen
- Psqi Sleep QuestionnaireDokument1 SeitePsqi Sleep QuestionnaireOverSkyLordNoch keine Bewertungen
- Jurnal ACSDokument39 SeitenJurnal ACSNovia AristantiaNoch keine Bewertungen
- Psqi Sleep QuestionnaireDokument1 SeitePsqi Sleep QuestionnaireOverSkyLordNoch keine Bewertungen
- Psqi Sleep QuestionnaireDokument1 SeitePsqi Sleep QuestionnaireOverSkyLordNoch keine Bewertungen
- Jurnal Cognitive FrailtyDokument9 SeitenJurnal Cognitive FrailtyAbdurrohman IzzuddinNoch keine Bewertungen
- Early Roentgen Observations in Acute Osteomyelitis: by Marie A. Capitanio, M.D., and John A. Kirkpatrick, M.DDokument9 SeitenEarly Roentgen Observations in Acute Osteomyelitis: by Marie A. Capitanio, M.D., and John A. Kirkpatrick, M.DAbdurrohman IzzuddinNoch keine Bewertungen
- NonalcoholicFattyLiverDisease2012 25762 FTPDokument19 SeitenNonalcoholicFattyLiverDisease2012 25762 FTPbudi_26690Noch keine Bewertungen
- Jurnal Hipertiroid KehamilanDokument5 SeitenJurnal Hipertiroid KehamilanAbdurrohman IzzuddinNoch keine Bewertungen
- Linkedin Job Invite MessageDokument4 SeitenLinkedin Job Invite MessageAxiom IntNoch keine Bewertungen
- Chemical BondingDokument7 SeitenChemical BondingSanaa SamkoNoch keine Bewertungen
- Rid and Clean Safety DataDokument1 SeiteRid and Clean Safety DataElizabeth GraceNoch keine Bewertungen
- Cat Hydo 10wDokument4 SeitenCat Hydo 10wWilbort Encomenderos RuizNoch keine Bewertungen
- Prof. Monzer KahfDokument15 SeitenProf. Monzer KahfAbdulNoch keine Bewertungen
- ANNAPURNA Sanitary Work 3 FinalDokument34 SeitenANNAPURNA Sanitary Work 3 FinalLaxu KhanalNoch keine Bewertungen
- Aqualab ClinicDokument12 SeitenAqualab ClinichonyarnamiqNoch keine Bewertungen
- Intro To Law CasesDokument23 SeitenIntro To Law Casesharuhime08Noch keine Bewertungen
- 4Q 4 Embedded SystemsDokument3 Seiten4Q 4 Embedded SystemsJoyce HechanovaNoch keine Bewertungen
- The Eaglet - Vol. 31, No. 3 - September 2019Dokument8 SeitenThe Eaglet - Vol. 31, No. 3 - September 2019Rebecca LovettNoch keine Bewertungen
- Pharmaniaga Paracetamol Tablet: What Is in This LeafletDokument2 SeitenPharmaniaga Paracetamol Tablet: What Is in This LeafletWei HangNoch keine Bewertungen
- 5Dokument3 Seiten5Carlo ParasNoch keine Bewertungen
- Catalogue 2021Dokument12 SeitenCatalogue 2021vatsala36743Noch keine Bewertungen
- A List of Run Commands For Wind - Sem AutorDokument6 SeitenA List of Run Commands For Wind - Sem AutorJoão José SantosNoch keine Bewertungen
- PSIG EscalatorDokument31 SeitenPSIG EscalatorNaseer KhanNoch keine Bewertungen
- Allen F. y D. Gale. Comparative Financial SystemsDokument80 SeitenAllen F. y D. Gale. Comparative Financial SystemsCliffordTorresNoch keine Bewertungen
- Zoonotic Diseases From HorsesDokument12 SeitenZoonotic Diseases From HorsesSandra Ximena Herreño MikánNoch keine Bewertungen
- ch-1 NewDokument11 Seitench-1 NewSAKIB MD SHAFIUDDINNoch keine Bewertungen
- 2 Lista Total de Soportados 14-12-2022Dokument758 Seiten2 Lista Total de Soportados 14-12-2022Emanuel EspindolaNoch keine Bewertungen
- Literatures of The World: Readings For Week 4 in LIT 121Dokument11 SeitenLiteratures of The World: Readings For Week 4 in LIT 121April AcompaniadoNoch keine Bewertungen
- New Kanban System DesignDokument4 SeitenNew Kanban System DesignJebin GeorgeNoch keine Bewertungen
- A Practical Guide To Transfer Pricing Policy Design and ImplementationDokument11 SeitenA Practical Guide To Transfer Pricing Policy Design and ImplementationQiujun LiNoch keine Bewertungen
- Ikramul (Electrical)Dokument3 SeitenIkramul (Electrical)Ikramu HaqueNoch keine Bewertungen
- Lifelong Learning: Undergraduate Programs YouDokument8 SeitenLifelong Learning: Undergraduate Programs YouJavier Pereira StraubeNoch keine Bewertungen
- Taxation: Presented By: Gaurav Yadav Rishabh Sharma Sandeep SinghDokument32 SeitenTaxation: Presented By: Gaurav Yadav Rishabh Sharma Sandeep SinghjurdaNoch keine Bewertungen