Beruflich Dokumente
Kultur Dokumente
Lecture 19 Bone Mechanics
Hochgeladen von
Henry Rodríguez GuzmánCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Lecture 19 Bone Mechanics
Hochgeladen von
Henry Rodríguez GuzmánCopyright:
Verfügbare Formate
Outline
! types and composition of bone
! adaptations of bone to imposed loads (Wolffs
Mechanics of Bone Law)
! effect on bone strength of load characteristics
(direction, rate of application, number of
Ozkaya and Nordin cycles)
Chapter 9, pages 206-211 ! effect of density and age on bone strength
! osteoporotic fractures
! tension band principle
! mechanics of fracture fixation
KIN 201 2007-1 Stephen Robinovitch, Ph.D. 1 2
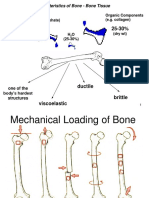
There are two primary types of Bone is a composite material
bone: cortical and trabecular ! Bone is a composite
! trabecular bone: interior material composed of
meshwork of trabeculae 66% hydroxyapatite
(thin struts); also known as (HA) crystals and 33%
cancellous or spongy bone; collagen fibrils (by dry
E ! 1 GPa; porosity ranges weight)
from 30% to 90% ! water makes up 25% of
! cortical bone: dense outer the wet weight of bone
shell of bone; also known ! HA crystals are strong
as compact bone; modulus and stiff but brittle;
E ! 18 GPa; porosity trabecular collagen prevents
ranges from 5% to 30% cortical brittle cracking
3 4
Skeletal structures are adapted to Optimal design theories: Wolffs Law
support musculoskeletal loads Wolff (1869): Wolffs Law:
bone adapts (remodels) in
! the structural
response to the mechanical
properties and
loads placed on it
failure force of
skeletal structures is Roux (1895): Principle of
well adapted to functional adaptation: bone
functional loads adapts to its function by
practicing the latter.
! does this reflect
Principle of maximum-
adaptation of human
minimum design: trajectorial
activity or
system of trabeculae
adaptation of
increasing increasing provides maximum strength
musculoskeletal
area load 5 with minimum material 6
anatomy?
Optimal design theories (cont) The strength and modulus of bone
(1) theory of uniform strength:
vary with the direction of loading
structure is designed so every ! bone is stronger in
bit of material is subjected to compression than tension
the same maximum stress ! bone is anisotropic: its
under a specific set of modulus and strength (in
loading conditions tension or compression)
(2) theory of trajectorial depend on the orientation
architecture: structure is of the tissue with respect
designed so material is to the load
located only in the paths of ! for cortical bone:
transmission of forces, Elong ! 17 GPa (! ult )tension
long
comp
" 135 MPa (! ult )long " #190 MPa
elsewhere there are voids Etrans ! 11 GPa (! ult )tension comp
(! ult )trans
trans " 50 MPa " #130 MPa
7 8
The modulus and strength of bone The strength of bone declines with
depends on rate of loading number of cycles during cyclic loading
Bone is viscoelastic - stress
FAST Like all materials, stress ultimate
its modulus and ! loading bone is susceptible to !
stress
strength increase with (N/m2) fatigue - when subject (N/m2)
SLOW
increasing rate of loading to repetitive or
loading fluctuating stress, it Fatigue (or
F will fail at a stress endurance) limit
strain " (m/m) level much lower than
damper (dashpot) with damping that required to cause 100 106
x, x constant b [N ! s m]. The force developed log (number of cycles
fracture on a single
k b by an ideal viscous damper is F = b ! x. to failure, N)
It' s presence in parallel with k adds a rate
application of load
dependance to the overall mechanical behavior.9 10
The strength and modulus of bone Osteoporosis: age-related decline in
vary with density (and microstructure) bone density and strength
! the strength and modulus of ! with age, bone becomes less
bone associate with density: dense (and therefore weaker)
! strength " (density)2 and more mineralized (and
! modulus " (density)3 therefore more brittle)
! density however can explain ! trabecular bone exhibits
only a small percent of the permanent microdamage and
variability between samples loss of connectivity healthy osteoporotic
in bone strength (R~0.4); adult
therefore microstructure
must also be important
11 12
Osteoporosis: age-related decline in Risk for injury depends on
bone density and strength (cont)
applied loads and failure loads
every decade after age 55: healthy
bone density declines by young applied load
10-20%, on average
stress ! = factor of risk =
modulus of elasticity
!
(N/m2)
failure load
decreases by 2%, on elderly
average
! " 1 # failure
ultimate strain declines by
7% , on average strain " (m/m)
energy to failure declines
by 5%, on average
! < 1 # no failure
13
Osteoporotic fractures Tensile stress due to bending moments
vertebral fractures:
is reduced by a tension band
50,000/yr in Canada F
hip fractures: F
most are
23,000/yr in Canada
undiagnosed,
$1 billion in costs
asymptomatic
major cause of spring spring both springs
morbidity, death, under under
wrist fractures: under
need for skilled tension compression
most common fx compression
nursing
site
etiology related to
as common as hip
both bone strength
fractures for the
and falls
elderly tension band: a device located far
much less important from the neutral axis, that takes
in terms of $, up the tensile load, leaving the
morbidity, and death 15 bone entirely in compression 16
Muscles act as natural tension bands Area moment of inertia affects
to reduce tensile stress in bone stresses due to bending moments
Recall that the stress due to an internal bending moment
M "y
is ! b = b , where Mb is the bending moment, y is
Ia
the distance from the neutral axis, and I a is the area
moment of inertia of the structure Ia = # y 2 dA.
dA R Ro
y
h
dA
y
Ri
beam b solid rod hollow rod
1 3 ! !
17 I = bh
12
I = R4
4
I= (
4 o
)
R 4 " Ri418
Stability of fracture fixation devices:
compression plate versus
intramedulary rod.
9 mm 9 mm OD x 2.0 cm x 0.5 cm
Fp solid rod 6 mm ID plate
tubular rod
! ! 1
I= (. 45)4 I= [0. 454 " 0. 30 4 ] I= (0.5)(2. 0)3
4 4 12
F = 0.03cm 4 = 0.33cm 4
= 0.02cm 4
OR
Fd 1
I = (2. 0)(0.5)3
12
= 0.02cm 4
19
Plate orientation with respect to applied
I A! P =
1
(0.5)(2. 0)3
load affects stability of fracture fixation
L 12
= 0.33cm 4 Most-to-least stable:
A P A no
loading mode apposition
FA-P apposition
1
IM ! L = (2.0)(0. 5)3
0.5 cm 12 C, A, B C, B, A
= 0.021cm 4 B
2.0 cm
C, B, A C, B, A
FM-L
I A! P
= 16 C, B(=A) C, B(=A)
IM ! L C
22
Review questions
! What optimal design theories does bone appear to
satisfy?
! What evidence suggests that bone responds to
mechanical loads?
! How does bone strength and modulus vary with
density?
! What is meant by the statement that bone is
anisotropic? viscoelastic? susceptible to fatigue?
! That are the three most common sites for osteoporotic
fracture? Which type of fracture is most important?
! What is a tension band? How does it protect bone?
! How does the orientation of a plate used for fracture
fixation affect the rigidity of the fixation? 23
Das könnte Ihnen auch gefallen
- Chap 2.3 PDFDokument9 SeitenChap 2.3 PDFد.موسى التويتيNoch keine Bewertungen
- 083 Stock2018WolffsLawDokument3 Seiten083 Stock2018WolffsLawromariodreyerNoch keine Bewertungen
- Bone LectureDokument50 SeitenBone LectureHenry Rodríguez GuzmánNoch keine Bewertungen
- The Musculoskeletal SystemDokument27 SeitenThe Musculoskeletal SystemKinzhuy MotageNoch keine Bewertungen
- Biomech Ch2 2015Dokument147 SeitenBiomech Ch2 2015Guruprasad KancharlaNoch keine Bewertungen
- BiomechanicsDokument41 SeitenBiomechanicsRohith Jayasimha Rao100% (1)
- Porose Qualidade Ossea New England 2010Dokument12 SeitenPorose Qualidade Ossea New England 2010Ben-Hur AlbergariaNoch keine Bewertungen
- Analysis of Biological Design II: Stress Strain AnalysesDokument27 SeitenAnalysis of Biological Design II: Stress Strain AnalysesShimaNoch keine Bewertungen
- Bone Mechanical Properties in Healthy and Diseased StatesDokument31 SeitenBone Mechanical Properties in Healthy and Diseased StatesThauane MaiaNoch keine Bewertungen
- Biomechanical and Anatomical Concepts: Dr. Murtaza Najabat AliDokument28 SeitenBiomechanical and Anatomical Concepts: Dr. Murtaza Najabat AliPersonal growthNoch keine Bewertungen
- Biomechanics of Bone and Skeletal SystemDokument11 SeitenBiomechanics of Bone and Skeletal SystemArun KumarNoch keine Bewertungen
- Physical Propertes of Bone, Cartilage and Their Function Adaptation in Various ConditionsDokument15 SeitenPhysical Propertes of Bone, Cartilage and Their Function Adaptation in Various ConditionsSwasti PandeyNoch keine Bewertungen
- Eckstein - Et - Al-2006 - The Effect of Exercise On Human Articular CartilageDokument22 SeitenEckstein - Et - Al-2006 - The Effect of Exercise On Human Articular CartilageStavros LitsosNoch keine Bewertungen
- Bone Remodeling Wolff's LawDokument4 SeitenBone Remodeling Wolff's LawThe Penitent OneNoch keine Bewertungen
- Ebacher2007 Dynamic Cimp TractDokument11 SeitenEbacher2007 Dynamic Cimp Tractimen mehriNoch keine Bewertungen
- Bone Biomechanics: Rabab Kaur MPT (M) 2 Year Isic-IrsDokument55 SeitenBone Biomechanics: Rabab Kaur MPT (M) 2 Year Isic-Irssakshi bansal100% (1)
- Biomechanics of Bones: Warsaw University of TechnologyDokument31 SeitenBiomechanics of Bones: Warsaw University of Technology1balamanianNoch keine Bewertungen
- World's Largest Science, Technology & Medicine Open Access Book PublisherDokument28 SeitenWorld's Largest Science, Technology & Medicine Open Access Book PublisherAndaPintilieNoch keine Bewertungen
- Structural and Functional Analysis of Human MovementDokument29 SeitenStructural and Functional Analysis of Human MovementMani KandanNoch keine Bewertungen
- Bone PDFDokument27 SeitenBone PDFAndreea HateganNoch keine Bewertungen
- CH Turner - Bone StrengthDokument18 SeitenCH Turner - Bone Strengthsharathr22Noch keine Bewertungen
- What Do You Think When You Hear The Word Biomechanics?Dokument102 SeitenWhat Do You Think When You Hear The Word Biomechanics?jvwestNoch keine Bewertungen
- L6 - Fascia - MechanicsDokument30 SeitenL6 - Fascia - MechanicsAmanda BorowczykNoch keine Bewertungen
- Mechanics of Musculoskeletal Components: EnergyDokument7 SeitenMechanics of Musculoskeletal Components: EnergyMay Myat MonNoch keine Bewertungen
- Experimental Determination of Material PropertiesDokument8 SeitenExperimental Determination of Material PropertiesCristina BancilaNoch keine Bewertungen
- Contribution of Elastic Tissues To The Mechanics and Energetics of Muscle Function During MovementDokument10 SeitenContribution of Elastic Tissues To The Mechanics and Energetics of Muscle Function During MovementEsin CoşkunerNoch keine Bewertungen
- Bone and Its Adaptation To Mechanical Loading: A Review: S. J. Mellon and K. E. TannerDokument21 SeitenBone and Its Adaptation To Mechanical Loading: A Review: S. J. Mellon and K. E. TannerJhony RodriguezNoch keine Bewertungen
- Material and Nanomechanical Properties of Bone Structural Units of - 2022 - BoneDokument12 SeitenMaterial and Nanomechanical Properties of Bone Structural Units of - 2022 - BoneGeorgiana BunghiuzNoch keine Bewertungen
- Bone BiomechanicsDokument36 SeitenBone BiomechanicsAliNoch keine Bewertungen
- Age-Related Changes in The Plasticity and ToughnessDokument7 SeitenAge-Related Changes in The Plasticity and ToughnessleonidNoch keine Bewertungen
- Donald T. Reilly 75Dokument16 SeitenDonald T. Reilly 75Salman SolehuddinNoch keine Bewertungen
- Lecture 2 BoneDokument22 SeitenLecture 2 BoneiamkpvemuriNoch keine Bewertungen
- 2 Bone Growth and DevelopmentDokument76 Seiten2 Bone Growth and DevelopmentEman AhmadNoch keine Bewertungen
- Bioinspired Actuators With Intrinsic Muscle-Like Mechanical PropertiesDokument20 SeitenBioinspired Actuators With Intrinsic Muscle-Like Mechanical PropertiesPedro Javier Garcia RamirezNoch keine Bewertungen
- Liu 2017Dokument7 SeitenLiu 2017Hieu DangNoch keine Bewertungen
- Nihms 743965Dokument25 SeitenNihms 743965registrepremsaNoch keine Bewertungen
- Functional and Clinical Significance of Skeletal Muscle ArchitectureDokument20 SeitenFunctional and Clinical Significance of Skeletal Muscle Architectureapi-3702726Noch keine Bewertungen
- Paper58 Mechanical Properties Hierarchical Structure Bone Med Eng Phys 20 (2) Rho Et Al 1998Dokument11 SeitenPaper58 Mechanical Properties Hierarchical Structure Bone Med Eng Phys 20 (2) Rho Et Al 1998leksremeshNoch keine Bewertungen
- L1 - Biophysics - ViscoelasticityDokument8 SeitenL1 - Biophysics - ViscoelasticityalllexissssNoch keine Bewertungen
- Finite-Element Analysis To Determine Effect of MonDokument20 SeitenFinite-Element Analysis To Determine Effect of MonRufaida HussainNoch keine Bewertungen
- Vật Liệu & Kỹ Thuật Y Sinh: Biomedical Materials and EngineeringDokument57 SeitenVật Liệu & Kỹ Thuật Y Sinh: Biomedical Materials and EngineeringkhuongdaihuynhNoch keine Bewertungen
- Implant Protective Occlusion A ReviewDokument7 SeitenImplant Protective Occlusion A Reviewlayla.adham94Noch keine Bewertungen
- Anatomical Reference Planes: Human Bone Growth and DevelopmentDokument12 SeitenAnatomical Reference Planes: Human Bone Growth and Developmentapi-3825389Noch keine Bewertungen
- 06 KnightDokument5 Seiten06 Knightcristina ArraisNoch keine Bewertungen
- Bone PhysicsToday 2009Dokument8 SeitenBone PhysicsToday 2009meriemarkounNoch keine Bewertungen
- Elastic Properties of Woven Bone: Effect of Mineral Content and Collagen Fibrils OrientationDokument14 SeitenElastic Properties of Woven Bone: Effect of Mineral Content and Collagen Fibrils OrientationAlvaraso MarmolNoch keine Bewertungen
- 2000 - Effect of Plate Position Relative To Bending Direction On The Rigidity of A Plate Osteosynthesis. A Theoretical AnalysisDokument15 Seiten2000 - Effect of Plate Position Relative To Bending Direction On The Rigidity of A Plate Osteosynthesis. A Theoretical AnalysisJimena BetancurNoch keine Bewertungen
- Massoud Biomechanics CollectionDokument66 SeitenMassoud Biomechanics CollectionAhmed Abul-MagdNoch keine Bewertungen
- Bone Composite AnalysisDokument10 SeitenBone Composite AnalysiskritiNoch keine Bewertungen
- Tsubota 2009Dokument7 SeitenTsubota 2009Catherine NocuaNoch keine Bewertungen
- Experimental Flatfoot Model The Contribution of Dynamic LoadingDokument6 SeitenExperimental Flatfoot Model The Contribution of Dynamic LoadingGeorge FernandoNoch keine Bewertungen
- Poro-Micromechanics of BoneDokument1 SeitePoro-Micromechanics of Boneagrawal29071989Noch keine Bewertungen
- Kim, Chang, Jung - 2010 - The Finite Element Analysis of A Fractured Tibia Applied by Composite Bone Plates Considering Contact ConditioDokument10 SeitenKim, Chang, Jung - 2010 - The Finite Element Analysis of A Fractured Tibia Applied by Composite Bone Plates Considering Contact ConditioMorteza AtaeiNoch keine Bewertungen
- Rho 1998Dokument11 SeitenRho 1998Catherine NocuaNoch keine Bewertungen
- Forms of Variable Resistance Training.10Dokument15 SeitenForms of Variable Resistance Training.10Juan LamaNoch keine Bewertungen
- Cartilage in The Normal Human Knee: in Vivo Characterization of Indentation Stiffness of ArticularDokument6 SeitenCartilage in The Normal Human Knee: in Vivo Characterization of Indentation Stiffness of ArticularantonioopNoch keine Bewertungen
- Length Dependence of Active Force Production in Skeletal MuscleDokument13 SeitenLength Dependence of Active Force Production in Skeletal Muscleleal thiagoNoch keine Bewertungen
- Stability of The Lumbar SpineDokument55 SeitenStability of The Lumbar SpineBryan HuaritaNoch keine Bewertungen
- Obs-13 240122 184549Dokument51 SeitenObs-13 240122 184549Edison MesacheNoch keine Bewertungen
- gp30mpc 150Dokument27 Seitengp30mpc 150locomotoras.slpNoch keine Bewertungen
- Matrix APDDokument1 SeiteMatrix APDQHSE BTGNoch keine Bewertungen
- Rashid Ch10 ImagesDokument47 SeitenRashid Ch10 ImagesAtiq Ur RehmanNoch keine Bewertungen
- Kočnice Shimano BR-M422Dokument1 SeiteKočnice Shimano BR-M422salecello2113Noch keine Bewertungen
- 20v4000enDokument266 Seiten20v4000enMario MartinezNoch keine Bewertungen
- AR15.40-P-5032TA Remove/install Alternator 4.2.09 Engine 648.961 in MODEL 211.023 /223 /026 /226Dokument2 SeitenAR15.40-P-5032TA Remove/install Alternator 4.2.09 Engine 648.961 in MODEL 211.023 /223 /026 /226Stefan AdrianNoch keine Bewertungen
- Physical Mechanical and Flexural Properties of 3 Orthodontic Wires An in Vitro Study. DANIELA DLICANDokument8 SeitenPhysical Mechanical and Flexural Properties of 3 Orthodontic Wires An in Vitro Study. DANIELA DLICANAlvaro ChacónNoch keine Bewertungen
- Review B4C Jace4865 Boron Carbide Structure Properties and Stability Under StressDokument24 SeitenReview B4C Jace4865 Boron Carbide Structure Properties and Stability Under StressAlexandru PrisecaruNoch keine Bewertungen
- PPTDokument22 SeitenPPTMuhamMad TaufikNoch keine Bewertungen
- Saes T 629Dokument10 SeitenSaes T 629Azhar Saqlain.Noch keine Bewertungen
- Gas Technology Institute PresentationDokument14 SeitenGas Technology Institute PresentationAris KancilNoch keine Bewertungen
- Base Plate and Anchor Rod DesignDokument2 SeitenBase Plate and Anchor Rod DesignKannan MurugesanNoch keine Bewertungen
- West Virginia Transporter 2017Dokument16 SeitenWest Virginia Transporter 2017Kyle LangsleyNoch keine Bewertungen
- Bucher LRV Hydraulic ValveDokument90 SeitenBucher LRV Hydraulic Valvedean_lockey0% (1)
- Delphi Informant Magazine Issue 3 Volume 6 2000Dokument36 SeitenDelphi Informant Magazine Issue 3 Volume 6 2000Raimo JankaNoch keine Bewertungen
- Table StructureDokument180 SeitenTable StructureVictor PathakNoch keine Bewertungen
- TXL 025 12s Datasheet 1 en PDFDokument11 SeitenTXL 025 12s Datasheet 1 en PDFJulianCitoNoch keine Bewertungen
- Andreki, P. (2016) - Exploring Critical Success Factors of Construction Projects.Dokument12 SeitenAndreki, P. (2016) - Exploring Critical Success Factors of Construction Projects.beast mickeyNoch keine Bewertungen
- Scania Jenerator DC1372A - 438-487kW PDFDokument2 SeitenScania Jenerator DC1372A - 438-487kW PDFMehmet ErenNoch keine Bewertungen
- Panduit Electrical CatalogDokument1.040 SeitenPanduit Electrical CatalognumnummoNoch keine Bewertungen
- Simulasi Pengendalian Level Steam DrumDokument15 SeitenSimulasi Pengendalian Level Steam DrumSatria dinusaNoch keine Bewertungen
- PayrollBatchLoader v4Dokument158 SeitenPayrollBatchLoader v4MaheshNoch keine Bewertungen
- Company ProfileDokument6 SeitenCompany ProfileFaidzil ChabibNoch keine Bewertungen
- PRO-II Thermodynamic Model SelectionDokument79 SeitenPRO-II Thermodynamic Model Selectionchemsac2100% (1)
- Pre Accion PDFDokument8 SeitenPre Accion PDFjhoger2012Noch keine Bewertungen
- Free Gear Calculator - KHK GearsDokument5 SeitenFree Gear Calculator - KHK GearslawlawNoch keine Bewertungen
- Urethane UB-7 Catalog 2013Dokument32 SeitenUrethane UB-7 Catalog 2013yfontalvNoch keine Bewertungen
- SEC StdsDokument65 SeitenSEC Stdserson1981Noch keine Bewertungen
- Deep Bar and Double Cage 010223Dokument20 SeitenDeep Bar and Double Cage 010223Debankan ChatterjeeNoch keine Bewertungen
- VVP Engineering College: Assignment 2Dokument12 SeitenVVP Engineering College: Assignment 2Fake 1Noch keine Bewertungen