Beruflich Dokumente
Kultur Dokumente
Epidurals and Spinals - Apr16
Hochgeladen von
Sanj.etcOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Epidurals and Spinals - Apr16
Hochgeladen von
Sanj.etcCopyright:
Verfügbare Formate
Information for patients
Epidurals and spinals: information about their operation
for anyone who may benefit from an epidural or spinal
This leaflet has been made using information from the Royal College of
Anaesthetists information booklets, which were written by patients, patient
representatives and anaesthetists, working together.
What are epidurals and spinals?
The nerves from your spine to your lower body pass through an area in your back close to
your spine. Anaesthetists sometimes numb the nerves in this area by doing either a spinal
or epidural.
What is the difference between an epidural and a spinal anaesthetic?
A spinal is a single injection with a thin needle that puts the local anaesthetic close to the
nerves, within the fluid that surrounds the spinal cord. The numbing effect lasts for about 1
to 4 hours.
With an epidural, a fine plastic tube (an epidural catheter) is threaded through a needle and
the tube is left in the epidural space in the back. Local anaesthetic is injected down the tube
to cause numbness, which varies in extent according to the amount of local anaesthetic
injected. Local anaesthetic and other pain relieving drugs may be given to prolong the effect
of the numbness for more than 3-5 hours. An epidural usually stays in place for 2-3 days.
When is a spinal anaesthetic used?
A spinal anaesthetic may be used as an alternative to a general anaesthetic for some
operations below the waist. Depending on the type of operation and your own medical
condition, a spinal anaesthetic may sometimes be safer for you and suit you better than a
general anaesthetic.
In addition, spinals can be used to give pain relief for after the operation. Injecting morphine
and other painkillers into the spinal fluid directly means lower doses of medicine can be used
and they last longer. If the spinal is being used for pain relief after the operation, you will
have a general anaesthetic as well.
Operations a spinal is commonly/often used for:
Orthopaedic surgery any major operation on leg bones or joints.
Epidurals and spinals, April 2016 1
E
Epidurals and spinals
General surgery hernia repair, varicose veins, piles (haemorrhoids), or as pain relief for
major surgery such as a bowel resection.
Vascular surgery repairs to blood vessels of the legs.
Gynaecology vaginal repairs, hysterectomies or operations on the bladder outlet.
Urology prostate removal, bladder operations and genital surgery.
Will I be awake if I have a spinal anaesthetic?
You can normally choose:
To remain fully conscious.
To have some sedation during your operation. This makes you relaxed and drowsy
though you may remain conscious.
Or, occasionally, a spinal anaesthetic may be combined with a general anaesthetic.
You would definitely have a full general anaesthetic if your anaesthetist is unable to perform
the spinal, or it does not work satisfactorily or if the surgery is more complicated than
expected.
Will I feel anything during the operation?
Your anaesthetist will not permit surgery to begin until you are both convinced that the spinal is
working properly. You should not feel any pain during the operation but you may be aware of
other sensations, such as movement or pressure, as the surgical team carry out their work.
Should I tell the anaesthetist anything during the operation?
Yes, your anaesthetist will want to know about any sensations or other feelings you
experience during the operation. They will make adjustments to your care throughout the
operation and be able to explain things to you.
When is an epidural anaesthetic used?
An epidural is used when either the operation is expected to take longer than 3 hours or if it
is needed to provide you with pain relief for many hours to days after your operation.
Although an epidural provides numbness during the operation it is usually combined with a
full general anaesthetic.
Sometimes epidurals and spinals are done together: this is called a combined spinal and
epidural.
How is an epidural or spinal done?
Epidurals and spinals are usually put in when you are conscious. Sometimes sedation can
be used.
1. A needle will be used to put a thin plastic tube (a cannula) into a vein in your hand or
arm for giving fluids (a drip).
Epidurals and spinals, April 2016 2
E
Epidurals and spinals
2. You will either sit on the side of the bed with your feet on a low stool or lie on your side,
curled up with your knees tucked up towards your chest.
3. Local anaesthetic is injected into a small area of the skin of your back.
4. A special needle is pushed through this numb area.
If you are having a spinal then local anaesthetic is injected through the needle and the
needle removed.
If you are having an epidural, a thin plastic catheter is passed through the needle into
your epidural space. The needle is then removed, leaving only the catheter in your back.
What will I feel while the epidural or spinal is being done?
Usually having a spinal or an epidural should not be too uncomfortable or take more than a
few minutes to perform.
The local anaesthetic stings briefly, but usually allows an almost painless procedure.
It is common to feel slight discomfort or ache in your back as the needle or catheter is
inserted.
Occasionally, an electric shock-like sensation or pain occurs during needle or catheter
insertion. If this happens, try to stay still and tell your anaesthetist immediately.
A sensation of warmth and numbness gradually develops, like the sensation after a
dental anaesthetic injection. You may still be able to feel touch, pressure and movement.
Your legs feel heavy and become increasingly difficult to move. This is a good sign as it
means the local anaesthetic is working well. With spinals this occurs within 5-10 minutes.
With epidurals this effect takes longer.
You may only notice these effects for the first time when you recover consciousness after
the operation if you are having sedation or a general anaesthetic as well as the spinal or
epidural.
If you are staying awake or having sedation you will probably be given extra oxygen to
breathe through a lightweight clear plastic mask. This is to improve oxygen levels in your
blood.
Overall, most people do not find these sensations to be unpleasant, just a bit strange.
The degree of numbness and weakness gradually decreases when the local anaesthetic
wears off.
Epidurals and spinals, April 2016 3
E
Epidurals and spinals
Advantages of an epidural or spinal:
There may be:
Less risk of chest infections after surgery.
Less effect on the heart and lungs.
Less chance of getting a blood clot in your leg after surgery.
Excellent pain relief immediately after surgery.
Less need for strong pain-relieving drugs.
Less sickness and vomiting.
Earlier return to drinking and eating after surgery.
Less confusion in older people after the operation.
Care after an operation with a spinal:
Your nurses will make sure that the numb area is protected from pressure and injury until
sensation returns.
It takes 1.5 4 hours for feeling to return to the area of your body that is numb. You
should tell the staff about any concerns or worries you may have.
As sensation returns, you may experience some tingling in the skin as the spinal wears
off. At this point you may become aware of some pain from the operation site and you
should ask for more pain relief before the pain becomes too severe.
As the spinal wears off, please ask for help when you first get out of bed.
You can normally drink fluids fairly soon after the operation and may also be able to eat a
light diet. The nurses will advise you when it is safe to do so.
Care when an epidural catheter has been left in place for pain relief.
At regular intervals, the nurses will take your pulse and blood pressure and ask you about
your pain and how you are feeling. They may check and adjust the epidural pump and
treat side effects.
You must not try to get out of bed without help until the epidural has fully worn off. The
nurses will advise you.
Side effects and complications of epidurals and spinals
Side effects are secondary effects of a treatment. They occur commonly and may be
unavoidable. Although they may be unpleasant (for example, feeling sick), they are not
usually dangerous. Complications are unwanted and unexpected events that are known to
occur occasionally due to a treatment. Serious complications are rare or very rare.
The risk of complications should be balanced against the benefits and compared with
alternative methods of pain relief. Your anaesthetist can help you do this.
Epidurals and spinals, April 2016 4
E
Epidurals and spinals
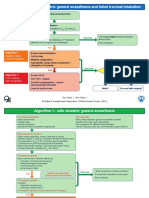
The following diagram may help you decide how you feel about a risk:
Very common or common side effects and complications
- Inability to pass urine. The epidural or spinal affects the nerves that supply the bladder,
so a catheter (tube) may be inserted to drain the urine away. Bladder function returns to
normal after the epidural wears off. Problems passing urine may occur after operations
whether you do or do not have an epidural or spinal.
- Low blood pressure. The local anaesthetic affects the nerves going to your blood vessels,
so blood pressure always drops a little.
- Itching. This can occur as a side effect of pain-relieving drugs that may be mixed with the
local anaesthetic in your epidural or spinal.
- Feeling sick and vomiting. These can be treated with anti-sickness drugs. These
problems are less frequent with an epidural or spinal than with most other methods of
pain relief.
- Backache. This is common after surgery whether you have an epidural or spinal or not. It
is not related to having an epidural. It may be caused by lying on a firm flat operating
table.
- Inadequate pain relief. It may be impossible to place the epidural or spinal, the local
anaesthetic may not spread adequately to cover the whole surgical area, or the catheter
can fall out with an epidurals. Other methods of pain relief are available if your epidural or
spinal fails.
- Headaches. Minor headaches are common after surgery, with or without an epidural.
Occasionally a severe headache occurs after an epidural or spinal because the lining of
the fluid filled space surrounding the spinal cord has been inadvertently punctured (a
dural tap). The fluid leaks out and causes low pressure in the brain, particularly when
you sit up. If this happens, it may be necessary to inject a small amount of your own
blood into your epidural space. This is called an epidural blood patch. The blood clots
and plugs the hole in the epidural lining. This will cure the headache in the majority of
cases.
Epidurals and spinals, April 2016 5
E
Epidurals and spinals
Uncommon complications
- Slow breathing. Some drugs used in the epidural or spinal can cause slow breathing
and/or drowsiness requiring treatment.
- Catheter infection. An epidural catheter can become infected and may have to be
removed. Antibiotics may be necessary. It is very rare for the infection to spread any
further than the insertion site in the skin.
Rare or very rare complications
Other complications, such as convulsions (fits), breathing difficulty and damage to nerves are
rare. Permanent disabling nerve damage, epidural abscess (infection), epidural haematoma
(blood clot) and cardiac arrest (stopping of the heart) are very rare indeed.
In comparison, you are more likely to die from an accident on the roads or in your own home
every year than suffer permanent damage from an epidural or spinal. These risks can be
discussed further with your anaesthetist.
Not everyone is able to have a spinal or epidural as occasionally the risks of complications
are too high. For example, some people still taking blood thinning medication may not be
able to have an epidural / spinal if the medicine has not been stopped in time. Your
anaesthetist will discuss this with you.
Although spinals and epidurals may be a very good anaesthetic for your operation and
provide better pain relief after your surgery, it is not compulsory. This information is to help
you make an informed choice. There are good alternative methods.
You will be seen by the anaesthetist before your operation when you will be given the
chance to ask any questions. Together you and the anaesthetist will decide the best
anaesthetic for you for your operation.
The information in this leaflet can also be made available in other languages and in large
print upon request. Please contact the Patient Relations Team on 0118 322 8338, or email
talktous@royalberkshire.nhs.uk
SURG-A_923
RBFT Anaesthetics/ Preoperative Assessment Clinic: April 2016
Review due: April 2018
Epidurals and spinals, April 2016 6
Das könnte Ihnen auch gefallen
- GUIDELINE For IMPROVING OUTCOME After Anaesthesia and Critical Care - 2017 - College of AnaesthesiologistsDokument83 SeitenGUIDELINE For IMPROVING OUTCOME After Anaesthesia and Critical Care - 2017 - College of AnaesthesiologistsSanj.etcNoch keine Bewertungen
- QBase Anaesthesia 1Dokument209 SeitenQBase Anaesthesia 1Sanj.etcNoch keine Bewertungen
- Secondary Transport - PactDokument4 SeitenSecondary Transport - PactSanj.etcNoch keine Bewertungen
- Opioid and Non-Opioid Analgesics in The ICUDokument2 SeitenOpioid and Non-Opioid Analgesics in The ICUSanj.etcNoch keine Bewertungen
- SLCoP Sinhala5405694062132472021Dokument1 SeiteSLCoP Sinhala5405694062132472021Sanj.etcNoch keine Bewertungen
- Transfer of The Critically Ill Patient - PACTDokument3 SeitenTransfer of The Critically Ill Patient - PACTSanj.etcNoch keine Bewertungen
- 6 - Glossary - PactDokument7 Seiten6 - Glossary - PactSanj.etcNoch keine Bewertungen
- 500 SBA Gen Systemic Pathology PDFDokument27 Seiten500 SBA Gen Systemic Pathology PDFSanj.etcNoch keine Bewertungen
- Rhabdomyolysis - PACTDokument2 SeitenRhabdomyolysis - PACTSanj.etcNoch keine Bewertungen
- Foetal AutopsyDokument17 SeitenFoetal AutopsySanj.etcNoch keine Bewertungen
- Med Oncology MCQDokument109 SeitenMed Oncology MCQdrzika100% (8)
- BMI 8 Selection ExamDokument4 SeitenBMI 8 Selection ExamSanj.etcNoch keine Bewertungen
- Endgames: Acute EpiglottitisDokument3 SeitenEndgames: Acute EpiglottitisSanj.etcNoch keine Bewertungen
- Delirium in critically ill patients: Should we worryDokument37 SeitenDelirium in critically ill patients: Should we worrySanj.etcNoch keine Bewertungen
- Peripartum Collapse 4.0Dokument14 SeitenPeripartum Collapse 4.0Sanj.etcNoch keine Bewertungen
- Anaesthesia For Major Abdominal SurgeryDokument1 SeiteAnaesthesia For Major Abdominal SurgerySanj.etcNoch keine Bewertungen
- Intravenous FluidsDokument37 SeitenIntravenous FluidsStella UmehNoch keine Bewertungen
- J Coll Physicians Surg Pak 2014 24 8 603 605Dokument3 SeitenJ Coll Physicians Surg Pak 2014 24 8 603 605Sanj.etcNoch keine Bewertungen
- 01 15 DAS Algorithms Web PRINT20092015Dokument6 Seiten01 15 DAS Algorithms Web PRINT20092015Sanj.etcNoch keine Bewertungen
- 128 Diabetic KetoacidosisDokument9 Seiten128 Diabetic KetoacidosisDite Bayu NugrohoNoch keine Bewertungen
- Gas CylindersDokument9 SeitenGas CylindersSanj.etcNoch keine Bewertungen
- Management of Safe AnaesthesiaDokument38 SeitenManagement of Safe AnaesthesiaSanj.etcNoch keine Bewertungen
- A Non-Fatal Self-Poisoning Attempt With Sildenafil: by Guest On 11 November 2017Dokument5 SeitenA Non-Fatal Self-Poisoning Attempt With Sildenafil: by Guest On 11 November 2017Sanj.etcNoch keine Bewertungen
- Saline IV Fluid ComparisonDokument2 SeitenSaline IV Fluid ComparisonSanj.etcNoch keine Bewertungen
- Ain ShamsJAnaesthesiol73336 7108132 - 015828Dokument4 SeitenAin ShamsJAnaesthesiol73336 7108132 - 015828Sanj.etcNoch keine Bewertungen
- SSCBundleCard PrintDokument2 SeitenSSCBundleCard PrintSanj.etcNoch keine Bewertungen
- Antimicrobial Stewardship Systems and Processes For Effective Antimicrobial Medicine Use PDF 1837273110469Dokument52 SeitenAntimicrobial Stewardship Systems and Processes For Effective Antimicrobial Medicine Use PDF 1837273110469Sanj.etcNoch keine Bewertungen
- IV Fluid ChartDokument2 SeitenIV Fluid Charthady920Noch keine Bewertungen
- Emergency Laparotomy: Patient Information FactsheetDokument4 SeitenEmergency Laparotomy: Patient Information FactsheetMuhammad RizqiNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- V60 Ventilator Specifications PDFDokument4 SeitenV60 Ventilator Specifications PDFJonathan Issac Dominguez RamirezNoch keine Bewertungen
- Valentine Gifting - Accessories EditionDokument25 SeitenValentine Gifting - Accessories EditionPriyanath PaulNoch keine Bewertungen
- Laboratory SafetyDokument4 SeitenLaboratory SafetyLey DoydoraNoch keine Bewertungen
- Introduction To The Philosophy of The Human Person Quarter I - Module 2Dokument26 SeitenIntroduction To The Philosophy of The Human Person Quarter I - Module 2Katrina TulaliNoch keine Bewertungen
- Motor Electrico Bojin J4103 - B User ManualDokument6 SeitenMotor Electrico Bojin J4103 - B User ManualJordan BonnettNoch keine Bewertungen
- Generate Ideas with TechniquesDokument19 SeitenGenerate Ideas with TechniquesketulNoch keine Bewertungen
- SpringDokument4 SeitenSpringarun123123Noch keine Bewertungen
- Independence Day Resurgence ScriptDokument60 SeitenIndependence Day Resurgence ScriptdavidNoch keine Bewertungen
- Effectiveness of Using High Gas Pressure in A Blast Furnace As A Means of Intensifying The Smelting OperationDokument10 SeitenEffectiveness of Using High Gas Pressure in A Blast Furnace As A Means of Intensifying The Smelting Operationchandan kumar100% (1)
- LP IV Lab Zdvzmanual Sem II fbsccAY 2019-20z 20-ConvxvzzertedDokument96 SeitenLP IV Lab Zdvzmanual Sem II fbsccAY 2019-20z 20-ConvxvzzertedVikas GuptaNoch keine Bewertungen
- Cambridge International General Certificate of Secondary EducationDokument16 SeitenCambridge International General Certificate of Secondary EducationAdaaan AfzalNoch keine Bewertungen
- Why Leaders Should Look in the “MirrorDokument4 SeitenWhy Leaders Should Look in the “MirrorCaryl Baylon EstreraNoch keine Bewertungen
- Types of Ego?Dokument2 SeitenTypes of Ego?S.UdhayakumarNoch keine Bewertungen
- WP1019 CharterDokument5 SeitenWP1019 CharternocnexNoch keine Bewertungen
- Johnson 1999Dokument20 SeitenJohnson 1999Linh Hoàng PhươngNoch keine Bewertungen
- Project Cost ForecastDokument11 SeitenProject Cost ForecastJames MendesNoch keine Bewertungen
- EDUC 5 - QuestionairesDokument7 SeitenEDUC 5 - QuestionairesWilliam RanaraNoch keine Bewertungen
- Double Burden of Malnutrition 2017Dokument31 SeitenDouble Burden of Malnutrition 2017Gîrneţ AlinaNoch keine Bewertungen
- Pembahasan Soal UN Bahasa Inggris SMP 2012 (Paket Soal C29) PDFDokument15 SeitenPembahasan Soal UN Bahasa Inggris SMP 2012 (Paket Soal C29) PDFArdi Ansyah YusufNoch keine Bewertungen
- Lorain Schools CEO Finalist Lloyd MartinDokument14 SeitenLorain Schools CEO Finalist Lloyd MartinThe Morning JournalNoch keine Bewertungen
- Larong Lahi Week 15 18Dokument7 SeitenLarong Lahi Week 15 18CJAY SOTELONoch keine Bewertungen
- HYBT Series: Assembling Terminal BlockDokument8 SeitenHYBT Series: Assembling Terminal Blockanon_670965762Noch keine Bewertungen
- PrognosisDokument7 SeitenPrognosisprabadayoeNoch keine Bewertungen
- Painter CardDokument1 SeitePainter CardPraveen RANANoch keine Bewertungen
- Assignment No.7Dokument2 SeitenAssignment No.7queen estevesNoch keine Bewertungen
- Lake Isle of Innisfree Lesson Plan BV ZGDokument4 SeitenLake Isle of Innisfree Lesson Plan BV ZGapi-266111651100% (1)
- Helmholtz DecompositionDokument4 SeitenHelmholtz DecompositionSebastián Felipe Mantilla SerranoNoch keine Bewertungen
- All Types of Switch CommandsDokument11 SeitenAll Types of Switch CommandsKunal SahooNoch keine Bewertungen
- EPM Mid Lecture 03 Chapt 1Dokument17 SeitenEPM Mid Lecture 03 Chapt 1Partho Protim MondolNoch keine Bewertungen
- How To Use Hyper-V Snapshot Revert, Apply, and Delete OptionsDokument15 SeitenHow To Use Hyper-V Snapshot Revert, Apply, and Delete OptionsKaran MishraNoch keine Bewertungen