Beruflich Dokumente
Kultur Dokumente
Acute Respiratory Distress: Section I: Scenario Demographics
Hochgeladen von
harasthaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Acute Respiratory Distress: Section I: Scenario Demographics
Hochgeladen von
harasthaCopyright:
Verfügbare Formate
Acute Respiratory Distress 1
Section I: Scenario Demographics
Scenario Title: Respiratory Distress secondary to pulmonary edema
Date of Development: 10/06/2015
Target Learning Group: Juniors (PGY 1 2) Seniors (PGY 3) All Groups
Section II: Scenario Developers
Scenario Developer(s): Lindsey McMurray
Affiliations/Institution(s): University of Toronto
Contact E-mail (optional): mcmurray.lindsey@gmail.com
Section III: Curriculum Integration
Learning Goals & Objectives
Educational Goal: 1. To demonstrate basic management principles and consider differential of a
patient with undifferentiated dyspnea.
2. To review basic management principles of a patient with pulmonary edema.
CRM Objectives: 1. To prioritize management steps in an unstable patient.
2. To delegate tasks as necessary and communicate clearly with team members.
3. To recognize the need to call for help.
Medical Objectives: To demonstrate the emergent management of acute respiratory distress.
Case Summary: Brief Summary of Case Progression and Major Events
A 78 year old woman post-op from a TAH+ BSO for ovarian CA has just been transferred to the ward when
she develops acute shortness of breath. When the resident arrives, the patient is in significant respiratory
distress saturating 80% on RA. Oxygen and medical therapy will not adequately relieve the patients
distress. The resident will need to recognize that the patient has a Grade 3-4 LV and received 2L of fluid
intra-operatively. When BiPAP is called for, it will be unavailable. Ultimately, the patient will require
intubation.
References
Marx, J. A., Hockberger, R. S., Walls, R. M., & Adams, J. (2013). Rosen's emergency medicine: Concepts and clinical practice. St. Louis: Mosby.
2015 EMSIMCASES.COM Page 1
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Acute Respiratory Distress 2
Section IV: Scenario Script
A. Clinical Vignette: To Read Aloud at Beginning of Case
You are on the GYNE service and have been paged by the ward nurse to attend to a 78 year old woman
who is having trouble breathing. She is POD #0 from a 4 hour TAH+BSO operation for ovarian CA. She just
got to the ward about 1 hour ago. You enter the patients room she is hooked up to an IV with NS running
at 150cc/hr.
B. Scenario Cast & Realism
Patient: Computerized Mannequin Realism: Conceptual
Mannequin Physical
Standardized Patient Select most Emotional/Experiential
Hybrid important Other:
Task Trainer dimension(s) N/A
Confederates Brief Description of Role
Bedside nurse Provides additional information regarding clinical course, past medical history, chart
details, latest laboratory investigations
C. Required Monitors
EKG Leads/Wires Temperature Probe Central Venous Line
NIBP Cuff Defibrillator Pads Capnography
Pulse Oximeter Arterial Line Other:
D. Required Equipment
Gloves Nasal Prongs Scalpel
Stethoscope Venturi Mask Tube Thoracostomy Kit
Defibrillator Non-Rebreather Mask Cricothyroidotomy Kit
IV Bags/Lines Bag Valve Mask Thoracotomy Kit
IV Push Medications Laryngoscope Central Line Kit
PO Tabs Video Assisted Laryngoscope Arterial Line Kit
Blood Products ET Tubes Other:
Intraosseous Set-up LMA Other:
E. Moulage
Clean dressing to laparotomy scar, wound clean and dry. Diaphoresis on the forehead (spray bottle).
Mock chart with admission note (for resident to decipher past medical history).
F. Approximate Timing
Set-Up: 5 min Scenario: 10 min Debriefing: 5 min
2015 EMSIMCASES.COM Page 2
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Acute Respiratory Distress 3
Section V: Patient Data and Baseline State
A. Patient Profile and History
Patient Name: Grace Smith Age: 78 Weight: 80 kg
Gender: M F Code Status: Full
Chief Complaint: Shortness of breath.
History of Presenting Illness: I cant breathe. Patient is fully alert and conscious but in respiratory
distress. Nurse notes that patient received 2L of fluid in the OR.
Past Medical History: STEMI 2010 Medications: Atorvastatin, Ramipril
CHF with grade 3-4 LV Lasix
COPD Ventolin PRN
HTN ASA (on hold)
Allergies: None
Social History: 60 pack-year smoking, occasional alcohol, no illicit drugs
Family History: Non contributory
Review of Systems: CNS: No complaints.
HEENT: No complaints.
CVS: No chest pain.
RESP: Sudden onset shortness of breath upon transfer to ward.
GI: No complaints.
GU: No complaints.
MSK: No complaints. INT: Feels sweaty.
B. Baseline Simulator State and Physical Exam
No Monitor Display Monitor On, no data displayed Monitor on Standard Display
HR: 110/min BP: 150/95 RR: 34/min O2SAT: 80%
Rhythm: NSR T: 36.9oC Glucose: 6.2 mmol/L GCS: 15
General Status: Respiratory distress, diaphoretic, alert and following commands.
CNS: GCS 15.
HEENT: Normal
CVS: Pulse present, normal heart sounds.
RESP: Coarse crackles
ABDO: Dry dressing to abdomen
GU: Normal
MSK: Normal, no calf swelling. SKIN: Clammy, moist
2015 EMSIMCASES.COM Page 3
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Acute Respiratory Distress 4
Section VI: Scenario Progression
Scenario States, Modifiers and Triggers
Patient State Patient Status Learner Actions, Modifiers & Triggers to Move to Next State
1. Baseline State Respiratory Learner Actions Modifiers
Rhythm: NSR distress with - Monitors/Full vitals - NRB applied O2SAT to 88%
HR: 110/min significantly - Supplemental O2 - If BiPAP requested, RT says:
BP: 150/95 increased WOB - Call for crash cart itll be 10 minutes. Someone is
RR: 34/min but alert. - Call for RT, rapid response getting it.
O2SAT: 80% RA team
T: 36.9oC - Review patient history
- Focused physical exam
- Calls for portable CXR
- Trial ventolin+atrovent Triggers
- Send blood work (troponin, - 5 min 2. Patient Tires
VBG, BNP)
- Trial Nitro sprays +/- lasix
- EKG
- Consider trial of BiPAP
2. Patient Tires Respiratory Learner Actions Modifiers
HR 120/ min distress - Repeat physical exam - CXR available show to learner
RR 24 continues but - Consider nitro infusion as state begins
O2SAT 85% on patient begins - Prepare for intubation - If no move toward intubation
NRB to tire. Patient - Consider fentanyl pre-tx by 8 min O2SAT to 82% and
GCS Now drowsy becomes - Use vaso-neutral induction patient unresponsive
drowsy. - Adjuncts nearby - BVM assistance O2SAT to
- Call for help (anesthesia, 89%
ICU) - BVM with PEEP O2SAT to
- Intubates patient 92%
Triggers
- Intubation 3. Peri-
Intubation
- If BVM with PEEP and choose
to wait for help END CASE
3. Peri-Intubation Unchanged. Learner Actions
HR 90 - Start nitro infusion
BP 155/85 - Post-intubation CXR END CASE PRN
RR 12 (vent) - Place OG
O2SAT 82% with - Post-intubation sedation
intubation then to - Call ICU
94% after 45 sec - Reassess patient, consider
other diagnoses
2015 EMSIMCASES.COM Page 4
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Acute Respiratory Distress 5
Section VII: Supporting Documents, Laboratory Results, & Multimedia
Images (ECGs, CXRs, etc.)
ECG
https://thejarvik7.files.wordpress.com/2012/02/inferior-wall-stemi-2005-05-27-08.jpg
CXR
https://www.med-ed.virginia.edu/courses/rad/cxr/pathology2chest.html
2015 EMSIMCASES.COM Page 5
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Acute Respiratory Distress 6
Section VIII: Debriefing Guide
General Debriefing Plan
Individual Group With Video Without Video
Objectives
Educational Goal: 1. To demonstrate basic management principles and consider
differential of a patient with undifferentiated dyspnea.
2. To review basic management principles of a patient with pulmonary
edema.
CRM Objectives: 1. To prioritize management steps in an unstable patient.
2. To delegate tasks as necessary and communicate clearly with team
members.
3. To recognize the need to call for help.
Medical Objectives: To demonstrate the emergent management of acute respiratory distress.
Sample Questions for Debriefing
1. What do you think your team did really well with this critically ill patient?
2. What were some communication difficulties the team experienced?
3. What are your top priorities on arriving to assess a patient in respiratory distress?
4. What are your immediate options to improve patients state?
5. Who can you call for help?
6. What else is on the differential for respiratory distress?
7. When do you need to intubate?
8. How is CHF management different in a hypotensive patient?
9. How would you approach an intubation like this on the ward? What are options to buy time until help is
available? Why is this airway so tenuous?
Key Moments
Recognition of acute respiratory distress and need to intervene.
Recognition of further deterioration and need to intubate.
2015 EMSIMCASES.COM Page 6
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Das könnte Ihnen auch gefallen
- I.C.U. Chest Radiology: Principles and Case StudiesVon EverandI.C.U. Chest Radiology: Principles and Case StudiesNoch keine Bewertungen
- Anaphylaxis With Angioedema: Section I: Scenario DemographicsDokument7 SeitenAnaphylaxis With Angioedema: Section I: Scenario DemographicsharasthaNoch keine Bewertungen
- ICU Scoring Systems A Complete Guide - 2020 EditionVon EverandICU Scoring Systems A Complete Guide - 2020 EditionNoch keine Bewertungen
- BradycardiaDokument8 SeitenBradycardialetonierNoch keine Bewertungen
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsVon EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNoch keine Bewertungen
- ATLS (Advanced Trauma Life Support) Teaching Protocol Pretest (30 Min) Context of Tutorial (2 Hours)Dokument16 SeitenATLS (Advanced Trauma Life Support) Teaching Protocol Pretest (30 Min) Context of Tutorial (2 Hours)anon_778118144Noch keine Bewertungen
- Critical Care SedationVon EverandCritical Care SedationAngelo Raffaele De GaudioNoch keine Bewertungen
- Early Emergency Care ProceduresDokument53 SeitenEarly Emergency Care ProceduresDwi ayu oktaveni100% (1)
- Initial Assessment and Management: Presented by Fayez Abillama, MDDokument53 SeitenInitial Assessment and Management: Presented by Fayez Abillama, MDDaniel GhosseinNoch keine Bewertungen
- Emt Skill SheetsDokument39 SeitenEmt Skill SheetsPatriciaChRistiani100% (1)
- Pediatric FirstAid CPR AEDDokument12 SeitenPediatric FirstAid CPR AEDVirtuepearlsNoch keine Bewertungen
- 2melnyk Ebp The Seven StepsDokument3 Seiten2melnyk Ebp The Seven Stepsapi-272725467100% (1)
- Initial Assessment and Management of Multiply Injured PatientsDokument30 SeitenInitial Assessment and Management of Multiply Injured PatientsSikaNoch keine Bewertungen
- A3 - ABCDE Algorithms PDFDokument63 SeitenA3 - ABCDE Algorithms PDFteguhNoch keine Bewertungen
- Normal Ranges Vital Signs 2017Dokument2 SeitenNormal Ranges Vital Signs 2017Elvis Nguyen100% (1)
- Trauma NurseDokument11 SeitenTrauma Nurseapi-247119922Noch keine Bewertungen
- The New Rapid ResponderDokument3 SeitenThe New Rapid RespondersarahNoch keine Bewertungen
- Outcomes of Ebp Process 2017Dokument3 SeitenOutcomes of Ebp Process 2017api-272725467100% (1)
- Min Min Min Min: Most Urgent Very Urgent Urgent Less Urgent Not UrgentDokument1 SeiteMin Min Min Min: Most Urgent Very Urgent Urgent Less Urgent Not UrgentAlma Alnajjar0% (1)
- Nursing Care of Clients in Emergency Situation 2Dokument52 SeitenNursing Care of Clients in Emergency Situation 2Danica FrancoNoch keine Bewertungen
- Malignant Hyperthermia Fact SheetDokument2 SeitenMalignant Hyperthermia Fact Sheetapi-301819201Noch keine Bewertungen
- Nsg241 Study Guide Exam 5Dokument76 SeitenNsg241 Study Guide Exam 5NatalieAndersonNoch keine Bewertungen
- Trauma OverviewDokument48 SeitenTrauma OverviewFrancescoBarbero100% (1)
- A&E Triage SystemDokument5 SeitenA&E Triage SystemArnel AlmutiahNoch keine Bewertungen
- Algorithm-ACLS CA in Pregnancy In-Hospital 200612Dokument1 SeiteAlgorithm-ACLS CA in Pregnancy In-Hospital 200612Hyunsoo EllisNoch keine Bewertungen
- AbbreviationDokument19 SeitenAbbreviationJayson NatividadNoch keine Bewertungen
- Identify, Prepare, and Pass Instruments: Team Member Type of Role TimingDokument47 SeitenIdentify, Prepare, and Pass Instruments: Team Member Type of Role TimingMuhammad Ihsan100% (1)
- Emergency NursingDokument46 SeitenEmergency NursingJoshua P AloveroNoch keine Bewertungen
- RSI For Nurses ICUDokument107 SeitenRSI For Nurses ICUAshraf HusseinNoch keine Bewertungen
- NURSING GUIDELINE - Version 1.0Dokument35 SeitenNURSING GUIDELINE - Version 1.0hidayatNoch keine Bewertungen
- Basic Life SupportDokument34 SeitenBasic Life SupportEveline FebrinaNoch keine Bewertungen
- ECG Basics 1Dokument24 SeitenECG Basics 1Dr.U.P.Rathnakar.MD.DIH.PGDHMNoch keine Bewertungen
- Neurologic Assessment RationaleDokument16 SeitenNeurologic Assessment RationaleflorenzoNoch keine Bewertungen
- Basic Life SupportDokument5 SeitenBasic Life SupportbuenoevelynNoch keine Bewertungen
- Initial Assessment and Management of Trauma PatientsDokument8 SeitenInitial Assessment and Management of Trauma PatientsAlvin De LunaNoch keine Bewertungen
- Ed Assessment Tool SampleDokument28 SeitenEd Assessment Tool SampleAnonymous ibmeej9Noch keine Bewertungen
- Mock ScenarioDokument35 SeitenMock ScenarioCarla Catrina EstradaNoch keine Bewertungen
- Student Refresher CourseDokument87 SeitenStudent Refresher CourseRaisa S. MariscalNoch keine Bewertungen
- Early Warning Score & Rapid Response TeamDokument26 SeitenEarly Warning Score & Rapid Response TeamAsim IdreesNoch keine Bewertungen
- Adult CPR flow chartDokument1 SeiteAdult CPR flow chartLia IshakNoch keine Bewertungen
- Vital Signs and Early Warning ScoresDokument47 SeitenVital Signs and Early Warning Scoresdr_nadheem100% (1)
- ILS Case Studies COMP 2020.ppsxDokument39 SeitenILS Case Studies COMP 2020.ppsxKim Orven KhoNoch keine Bewertungen
- Operating Room Preparation: Philipp Acaso Ralph ArcoDokument158 SeitenOperating Room Preparation: Philipp Acaso Ralph ArcoTiffany Luv Adrias100% (1)
- Typhon Case LogDokument3 SeitenTyphon Case LogJeremy HallNoch keine Bewertungen
- Basic Concept of BLS: Muhammad SaleemDokument27 SeitenBasic Concept of BLS: Muhammad Saleemms khanNoch keine Bewertungen
- Advanced Airway Management: Leaugeay Webre, BS, CCEMT-P, Nremt-PDokument35 SeitenAdvanced Airway Management: Leaugeay Webre, BS, CCEMT-P, Nremt-Pbasic100% (4)
- Antrim ED Handbook 2019Dokument238 SeitenAntrim ED Handbook 2019Chris Jardine LiNoch keine Bewertungen
- Oral Station ScenarioDokument3 SeitenOral Station ScenariojrworthingtonNoch keine Bewertungen
- Department of Nursing Initial Competency Validation Checklist: Orientation: RNDokument4 SeitenDepartment of Nursing Initial Competency Validation Checklist: Orientation: RNAmeng GosimNoch keine Bewertungen
- PEDIATRIC ASSESSMENT OVERVIEWDokument2 SeitenPEDIATRIC ASSESSMENT OVERVIEWAghnia Nafila100% (1)
- Neurological Examination PDFDokument6 SeitenNeurological Examination PDFArif K BashaNoch keine Bewertungen
- Care of Chest Tubes Closed Chest Drainage SystemDokument21 SeitenCare of Chest Tubes Closed Chest Drainage Systemhady920100% (1)
- Rapid Sequence Intubation: BackgroundDokument8 SeitenRapid Sequence Intubation: Backgroundmarsh86Noch keine Bewertungen
- Triage PDFDokument59 SeitenTriage PDFagungNoch keine Bewertungen
- Blood Transfusion Single Use PathwayDokument6 SeitenBlood Transfusion Single Use PathwayropusanNoch keine Bewertungen
- Saudi CPR Guidlines in EnglishDokument16 SeitenSaudi CPR Guidlines in EnglishpiyushbamsNoch keine Bewertungen
- Guideline of ExtravasationDokument35 SeitenGuideline of ExtravasationAura Lorena Rivas Zambrano100% (1)
- Blood Transfusion ReactionDokument9 SeitenBlood Transfusion ReactionReema Akberali nooraniNoch keine Bewertungen
- Bio 235 Midterm 1 NotesDokument53 SeitenBio 235 Midterm 1 NotesNita JosephNoch keine Bewertungen
- Periop Power PointDokument97 SeitenPeriop Power PointAldrine Albor Anyayahan INoch keine Bewertungen
- No.6 Tzellos2008Dokument8 SeitenNo.6 Tzellos2008harasthaNoch keine Bewertungen
- Medicina 57 00312 v3Dokument16 SeitenMedicina 57 00312 v3harasthaNoch keine Bewertungen
- Paravetebral EpiduralDokument7 SeitenParavetebral EpiduralharasthaNoch keine Bewertungen
- Dialysis in Critically IllDokument48 SeitenDialysis in Critically IllFate ChanNoch keine Bewertungen
- Opioid-Induced Tolerance and HyperalgesiaDokument70 SeitenOpioid-Induced Tolerance and HyperalgesiaharasthaNoch keine Bewertungen
- LectureDokument4 SeitenLectureharasthaNoch keine Bewertungen
- Jurnal Anastesi - The Role of Continous Peripheral Nerve BlocksDokument20 SeitenJurnal Anastesi - The Role of Continous Peripheral Nerve BlocksMichele JohnsonNoch keine Bewertungen
- JPR 8 009Dokument13 SeitenJPR 8 009harasthaNoch keine Bewertungen
- Regional Anaesthesia To Prevent Chronic Pain After Surgery: A Cochrane Systematic Review and Meta-AnalysisDokument10 SeitenRegional Anaesthesia To Prevent Chronic Pain After Surgery: A Cochrane Systematic Review and Meta-AnalysisharasthaNoch keine Bewertungen
- Postmastectomy and Postthoracotomy Pain: Anne M. Wallace, MD, and Mark S. Wallace, MDDokument18 SeitenPostmastectomy and Postthoracotomy Pain: Anne M. Wallace, MD, and Mark S. Wallace, MDharasthaNoch keine Bewertungen
- Peripheral Chemical Mediators of Pain and HyperalgesiaDokument1 SeitePeripheral Chemical Mediators of Pain and HyperalgesiaharasthaNoch keine Bewertungen
- HOW TO Assess For Pain Sensitisation in The Clinic HANDOUTDokument12 SeitenHOW TO Assess For Pain Sensitisation in The Clinic HANDOUTharasthaNoch keine Bewertungen
- 9d18 PDFDokument22 Seiten9d18 PDFharasthaNoch keine Bewertungen
- Education and Laboratory Testing for COVID-19Dokument61 SeitenEducation and Laboratory Testing for COVID-19mulyadi diningrum100% (1)
- International Journal of Anesthetics and Anesthesiology Ijaa 3 052Dokument9 SeitenInternational Journal of Anesthetics and Anesthesiology Ijaa 3 052harasthaNoch keine Bewertungen
- Endothelial Glycocalyx: Role in Body Fluid Homeostasis and Fluid ManagementDokument9 SeitenEndothelial Glycocalyx: Role in Body Fluid Homeostasis and Fluid ManagementharasthaNoch keine Bewertungen
- Craniocervical Dystonia Blepharospasm. Spasmodic Contraction of TheDokument3 SeitenCraniocervical Dystonia Blepharospasm. Spasmodic Contraction of TheharasthaNoch keine Bewertungen
- Acog AccretaDokument17 SeitenAcog AccretaharasthaNoch keine Bewertungen
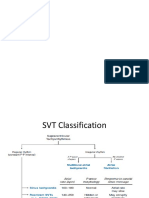
- SVTDokument21 SeitenSVTharasthaNoch keine Bewertungen
- Managing Advanced Parkinson's CareDokument29 SeitenManaging Advanced Parkinson's CareharasthaNoch keine Bewertungen
- Caesarean Section1846Dokument12 SeitenCaesarean Section1846harasthaNoch keine Bewertungen
- 1 PBDokument6 Seiten1 PBAustine OsaweNoch keine Bewertungen
- MorphineDokument16 SeitenMorphineharasthaNoch keine Bewertungen
- 4.5 THE TREATMENT OF CONGENITAL HYDROCEPHALUS. M.J. Joubert PDFDokument3 Seiten4.5 THE TREATMENT OF CONGENITAL HYDROCEPHALUS. M.J. Joubert PDFharasthaNoch keine Bewertungen
- Mortality Predictors in SepsisDokument5 SeitenMortality Predictors in SepsisharasthaNoch keine Bewertungen
- Breech NRPDokument8 SeitenBreech NRPharasthaNoch keine Bewertungen
- Pengaruh Anestesi Regional Dan General Pada Sectio Cesaria Pada Ibu Dengan Pre Eklampsia Berat Terhadap Apgar ScoreDokument12 SeitenPengaruh Anestesi Regional Dan General Pada Sectio Cesaria Pada Ibu Dengan Pre Eklampsia Berat Terhadap Apgar ScoreMuhamad Ongky NRahardiNoch keine Bewertungen
- Brusselle - Immunology of COPD - Review - Lancet 2011 PDFDokument12 SeitenBrusselle - Immunology of COPD - Review - Lancet 2011 PDFharasthaNoch keine Bewertungen
- Mortality Predictors in SepsisDokument5 SeitenMortality Predictors in SepsisharasthaNoch keine Bewertungen
- MorphineDokument16 SeitenMorphineharasthaNoch keine Bewertungen
- Medical Reimbursement PDFDokument3 SeitenMedical Reimbursement PDFOrlando WilliamsNoch keine Bewertungen
- Module 9 BIOETHICAL PRINCIPLEDokument10 SeitenModule 9 BIOETHICAL PRINCIPLEColeen TanNoch keine Bewertungen
- Nursing Core Competency Standards 2012Dokument27 SeitenNursing Core Competency Standards 2012JustinP.DelaCruz100% (1)
- Normal Ranges Vital Signs 2017Dokument2 SeitenNormal Ranges Vital Signs 2017Elvis Nguyen100% (1)
- Scope and Delimitation of The StudyDokument7 SeitenScope and Delimitation of The StudyMarebel ManabatNoch keine Bewertungen
- ORDBMS ExerciseDokument2 SeitenORDBMS Exerciseramesh kumar.aNoch keine Bewertungen
- E-mail Your CV in Microsoft Word Format to Apply for Medical Jobs in Saudi ArabiaDokument7 SeitenE-mail Your CV in Microsoft Word Format to Apply for Medical Jobs in Saudi ArabiaashfaqzteNoch keine Bewertungen
- HR 1701 - Commending Medical and Nursing Board TopnotchersDokument2 SeitenHR 1701 - Commending Medical and Nursing Board TopnotchersBayan Muna Party-listNoch keine Bewertungen
- Magbanua MK CasesDokument5 SeitenMagbanua MK Casesapi-26570979Noch keine Bewertungen
- Gail Luskin ResumeDokument3 SeitenGail Luskin Resumeapi-260548731Noch keine Bewertungen
- Dispensing Medications During Off-Hours StrategiesDokument14 SeitenDispensing Medications During Off-Hours StrategiesHamza Ali100% (2)
- Moot Proposition Purc LudhianaDokument4 SeitenMoot Proposition Purc LudhianaRaj RawlNoch keine Bewertungen
- ICL-Coding Operative ReportDokument33 SeitenICL-Coding Operative ReportHIMOfficial100% (2)
- Department of Education: Republic of The PhilippinesDokument11 SeitenDepartment of Education: Republic of The PhilippinesRogen VigilNoch keine Bewertungen
- Monthly Free Acupuncture Treatment Camp HighlightsDokument21 SeitenMonthly Free Acupuncture Treatment Camp HighlightsShripadNoch keine Bewertungen
- ACSMs Exercise Testing Prescription PDFDokument6 SeitenACSMs Exercise Testing Prescription PDFHARIZNoch keine Bewertungen
- Historical Development of Community HealthDokument11 SeitenHistorical Development of Community HealthMuhamad YusufNoch keine Bewertungen
- Entrepreneurial Nursing Skills for Addressing Philippine Health ConcernsDokument8 SeitenEntrepreneurial Nursing Skills for Addressing Philippine Health ConcernsTeanu Jose Gabrillo TamayoNoch keine Bewertungen
- Ulster County Recovery and Resilience Working Group Spending PlanDokument18 SeitenUlster County Recovery and Resilience Working Group Spending PlanDaily FreemanNoch keine Bewertungen
- Fluoroscopy-Guided Shoulder Injections Relieve Hemiplegic Shoulder PainDokument8 SeitenFluoroscopy-Guided Shoulder Injections Relieve Hemiplegic Shoulder PainDiego Pinto PatroniNoch keine Bewertungen
- Application of Wellness in Physical TherapyDokument26 SeitenApplication of Wellness in Physical TherapyZgama AbdulrahmanNoch keine Bewertungen
- Bair Paws Patient Satisfaction Case StudyDokument3 SeitenBair Paws Patient Satisfaction Case StudymochkurniawanNoch keine Bewertungen
- DBOIDokument325 SeitenDBOIVibin AntonyNoch keine Bewertungen
- Philhealth List of Assigned Members in Lala Rural Health UnitDokument299 SeitenPhilhealth List of Assigned Members in Lala Rural Health UnitJhonrie PakiwagNoch keine Bewertungen
- Planning and Designing An Isolation Facility in Hospitals Need of The Hour PDFDokument9 SeitenPlanning and Designing An Isolation Facility in Hospitals Need of The Hour PDFdzakyzahidNoch keine Bewertungen
- Chapter 13Dokument15 SeitenChapter 13Jessica nonye100% (1)
- Immediate Dental Implant Placement Into Infected vs. Non-Infected Sockets: A Meta-AnalysisDokument7 SeitenImmediate Dental Implant Placement Into Infected vs. Non-Infected Sockets: A Meta-Analysismarlene tamayoNoch keine Bewertungen
- Summer Eval IDokument4 SeitenSummer Eval Iapi-632827798Noch keine Bewertungen
- OPD Schedule of Faculty of Dental Sciences BHUDokument1 SeiteOPD Schedule of Faculty of Dental Sciences BHUG HhNoch keine Bewertungen
- Pengetahuan Ibu Tentang Mobilisasi Dini Pasca Persalinan Normal Pervaginam Di Wilayah Kerja Puskesmas Labuhan Rasoki Kecamatan Padangsidimpuan Tenggara Tahun 2018Dokument6 SeitenPengetahuan Ibu Tentang Mobilisasi Dini Pasca Persalinan Normal Pervaginam Di Wilayah Kerja Puskesmas Labuhan Rasoki Kecamatan Padangsidimpuan Tenggara Tahun 2018Geuman ChajgoNoch keine Bewertungen