Beruflich Dokumente
Kultur Dokumente
Early Physical Therapy Vs Usual Care in Patients With Recent-Onset LowBack Pain
Hochgeladen von
GiovanniOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Early Physical Therapy Vs Usual Care in Patients With Recent-Onset LowBack Pain
Hochgeladen von
GiovanniCopyright:
Verfügbare Formate
Research
Original Investigation
Early Physical Therapy vs Usual Care in Patients
With Recent-Onset Low Back Pain
A Randomized Clinical Trial
Julie M. Fritz, PhD, PT; John S. Magel, PhD, PT; Molly McFadden, MS; Carl Asche, PhD; Anne Thackeray, PhD, PT;
Whitney Meier, DPT; Gerard Brennan, PhD, PT
Supplemental content at
IMPORTANCE Low back pain (LBP) is common in primary care. Guidelines recommend jama.com
delaying referrals for physical therapy. CME Quiz at
jamanetworkcme.com and
OBJECTIVE To evaluate whether early physical therapy (manipulation and exercise) is more CME Questions page 1511
effective than usual care in improving disability for patients with LBP fitting a decision rule.
DESIGN, SETTING, AND PARTICIPANTS Randomized clinical trial with 220 participants recruited
between March 2011 and November 2013. Participants with no LBP treatment in the past 6
months, aged 18 through 60 years (mean age, 37.4 years [SD, 10.3]), an Oswestry Disability
Index (ODI) score of 20 or higher, symptom duration less than 16 days, and no symptoms
distal to the knee in the past 72 hours were enrolled following a primary care visit.
INTERVENTIONS All participants received education. Early physical therapy (n = 108)
consisted of 4 physical therapy sessions. Usual care (n = 112) involved no additional
interventions during the first 4 weeks.
MAIN OUTCOMES AND MEASURES Primary outcome was change in the ODI score (range:
0-100; higher scores indicate greater disability; minimum clinically important difference, 6
points) at 3 months. Secondary outcomes included changes in the ODI score at 4-week and
1-year follow-up, and change in pain intensity, Pain Catastrophizing Scale (PCS) score,
fear-avoidance beliefs, quality of life, patient-reported success, and health care utilization at
4-week, 3-month, and 1-year follow-up.
RESULTS One-year follow-up was completed by 207 participants (94.1%). Using analysis of
covariance, early physical therapy showed improvement relative to usual care in disability
after 3 months (mean ODI score: early physical therapy group, 41.3 [95% CI, 38.7 to 44.0] at
baseline to 6.6 [95% CI, 4.7 to 8.5] at 3 months; usual care group, 40.9 [95% CI, 38.6 to 43.1]
at baseline to 9.8 [95% CI, 7.9 to 11.7] at 3 months; between-group difference, 3.2 [95% CI,
5.9 to 0.47], P = .02). A significant difference was found between groups for the ODI score
after 4 weeks (between-group difference, 3.5 [95% CI, 6.8 to 0.08], P = .045]), but not at
1-year follow-up (between-group difference, 2.0 [95% CI, 5.0 to 1.0], P = .19). There was no
improvement in pain intensity at 4-week, 3-month, or 1-year follow-up (between-group
difference, 0.42 [95% CI, 0.90 to 0.02] at 4-week follow-up; 0.38 [95% CI, 0.84 to
0.09] at 3-month follow-up; and 0.17 [95% CI, 0.62 to 0.27] at 1-year follow-up). The PCS Author Affiliations: Department of
scores improved at 4 weeks and 3 months but not at 1-year follow-up (between-group Physical Therapy, University of Utah,
Salt Lake City (Fritz, Magel,
difference, 2.7 [95% CI, 4.6 to 0.85] at 4-week follow-up; 2.2 [95% CI, 3.9 to 0.49] at McFadden, Thackeray, Meier);
3-month follow-up; and 0.92 [95% CI, 2.7 to 0.61] at 1-year follow-up). There were no Department of Physical Therapy,
differences in health care utilization at any point. Intermountain Healthcare, Salt Lake
City, Utah (Magel, Thackeray,
Brennan); Department of Internal
CONCLUSIONS AND RELEVANCE Among adults with recent-onset LBP, early physical therapy Medicine, University of Illinois College
resulted in statistically significant improvement in disability, but the improvement was modest of Medicine at Peoria, Peoria, Illinois
and did not achieve the minimum clinically important difference compared with usual care. (Asche).
Corresponding Author: Julie M.
Fritz, PhD, PT, Department of Physical
TRIAL REGISTRATION clinicaltrials.gov Identifier: NCT01726803
Therapy, University of Utah, 520
Wakara Way, Salt Lake City, UT 84108
JAMA. 2015;314(14):1459-1467. doi:10.1001/jama.2015.11648 (julie.fritz@utah.edu).
(Reprinted) 1459
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by a Azienda Ospedaliero- Universitaria User on 01/11/2016
Research Original Investigation Early Physical Therapy vs Usual Care for Recent-Onset Low Back Pain
L
ifetime prevalence of low back pain (LBP) is about 70%, records to identify primary care visits with an International
and 25% of adults report LBP lasting at least 1 day in the Classification of Diseases, Ninth Revision, LBP diagnosis
past 3 months.1 Back pain accounts for 2% to 5% of all (diagnosis codes: 719.55, 721.3, 722.1, 722.52, 722.73, 722.83,
physician visits.1,2 Health care costs for LBP in the United States 722.93, 724, 729.2, 737.3, 756.11, 756.12, 846, 847.2, 847.3,
were approximately $86 billion in 2005,3 and have been in- or 847.9). A letter describing the study was mailed with an
creasing faster than overall health care spending.3,4 Despite in- opt-out option, followed by telephone contact. Interested
creasing resource use, rates of poor outcomes for LBP are individuals were scheduled for evaluation. After providing
increasing.5,6 written informed consent participants underwent a baseline
Most patients with LBP who seek care begin in primary evaluation followed by random assignment to an interven-
care.7 Initial management decisions in this setting may be tion group.
highly influential on outcomes. Early use of magnetic reso- Eligibility requirements were aged 18 through 60 years
nance imaging or opioids, which contradicts current practice with LBP (defined as pain between the 12th rib and buttocks), 1
guidelines,8 is associated with higher rates of prolonged dis- ODI score of 20 or higher, current symptoms duration of less
ability and invasive procedures.9-11 The effect of early physi- than 16 days, and no pain or numbness distal to the knee(s) in
cal therapy is unclear. Guidelines advise delaying referral to the past 72 hours. These criteria identified a subgroup of
physical therapy or other specialists for a few weeks to per- patients likely to respond to the physical therapy protocol in
mit spontaneous recovery.12 Recent observational studies this study.14 Exclusion criteria were prior lumbar surgery,
report early physical therapy is associated with lower costs pregnancy, any other LBP treatment in the past 6 months,
and reduced risk of invasive procedures when compared clinical signs of nerve root compression (eg, hyporeflexia) or
with delayed referral,9,13 suggesting that some patients may any red flag finding suggesting nonmusculoskeletal back
benefit from early physical therapy. Prior research has pain (eg, infection or neoplasm).
described a decision rule identifying a subgroup of patients
who have excellent results from physical therapy involving Outcome Assessments
manipulation and exercise.14,15 The subgroup defined by this A baseline assessment was conducted before randomization 567
rule includes patients with acute LBP (<16 days duration) and included all primary and secondary outcomes and demo-
without symptoms extending below the knee(s). This sub- graphic information. Patients self-reported race/ethnicity using
group may be particularly likely to benefit from early physi- categories predefined for federally sponsored research. Four-
cal therapy using a protocol of exercise and manipulation. week assessment was conducted in-person by an assessor
This study compared the efficacy of early physical therapy who was blinded to randomization. Additional assessments
of 4 sessions of manipulation and exercise with usual care for were conducted through a study website. The primary out-
patients with LBP seen in primary care fitting the decision rule come was the ODI score, a validated 10-item measure of func-
criteria. Our primary aim was to evaluate change in disability tion for individuals with LBP.16 Items assessed limitations
from baseline to 3 months. Secondary outcomes included due to LBP in activities including standing, sitting, walking,
evaluating changes in disability after 4 weeks and 1 year, and pain intensity, lifting, sleeping, social life, employment/
examining change in pain intensity, pain catastrophizing, fear- homemaking, personal care, and traveling. Scores range
avoidance beliefs, patient-reported health state and success, from 0 to 100 with higher scores indicating greater disability.17
and health care utilization. The minimum clinically important difference for the ODI was
estimated at 6 points for acute LBP.17
Secondary outcomes assessed at 4-week, 3-month, and
1-year follow-up included a numeric pain rating of LBP sever-
Methods ity (range, 0-10), 18 Pain Catastrophizing Scale (PCS), 19
Study Design and Participants Fear-Avoidance Beliefs Questionnaire (FABQ) for physical
Study protocol was approved by the University of Utah and In- activity, FABQ for work,20 and a 15-point global rating of
termountain Healthc are institutional review boards change21 dichotomized to define patient-reported success as
(Supplement 1). A data and safety monitoring board met an- occurring when 1 of the top 2 ratings were selected (a great
nually to review the study. This study was a parallel-group ran- deal better or a very great deal better). The 5-Dimensional
domized clinical trial. Outcomes were assessed in a blinded EuroQol (EQ-5D) tool assessed quality of life based on 5
manner at 4 weeks, 3 months, and 1 year following enroll- domains (mobility, self-c are, usual activities, pain/
ment. The primary outcome was disability assessed with the discomfort, and anxiety/depression), each rated on a scale of
Oswestry Disability Index (ODI) score at 3-month follow-up. 1-3, then combined to generate a comprehensive score rang-
Secondary outcomes included change in the ODI score mea- ing from 0 (extremely poor quality of life) to 1 (optimal qual-
sured after 4 weeks and 1 year, and change in other patient- ity of life).22 Patients self-rated their overall health using the
reported outcomes (described below) measured after 4 weeks, EQ-5D visual analog scale ranging from 0 (worst) to 100 (best
3 months, and 1 year. imaginable) health. We used monthly online diaries to collect
Individuals with LBP visiting a primary care physician health care utilization for LBP23 including advanced imaging
in Salt Lake City, Utah, from March 2011 through November (computed tomography or magnetic resonance imaging),
2013 were recruited. Potential participants were informed of emergency department or urgent care visit, spine specialist
the study by clinic staff or by mail using electronic medical visit (surgeon or physiatrist), spinal injection, or surgery.
1460 JAMA October 13, 2015 Volume 314, Number 14 (Reprinted) jama.com
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by a Azienda Ospedaliero- Universitaria User on 01/11/2016
Early Physical Therapy vs Usual Care for Recent-Onset Low Back Pain Original Investigation Research
Adverse effects of early physical therapy were assessed after conducted by intention-to-treat with participants analyzed 9
4 weeks with a questionnaire asking Did you experience any according to a randomly assigned treatment group irrespec-
discomfort or unpleasant reaction after any of your physical tive of compliance. Multiple imputation was used for missing
therapy treatment sessions? For those responding yes, observations. Fully sequential imputation30 was used to gen-
adverse effect categories (eg, increased pain or stiffness) erate 10 imputed data sets using available primary and sec-
were offered. Severity of each adverse effect was rated as ondary outcome scores, treatment group, employment sta-
light, mild, moderate, or severe.24 tus, sex, age, marital status, education, prior history of LBP,
and smoking. To provide distinct evaluations of treatment
Randomization effects at different follow-up times, separate analyses of
2
Following baseline evaluation participants were randomized covariance were used to compare mean change in each con-
to early physical therapy or usual care following a computer- tinuous outcome from baseline with each follow-up between
generated randomization list with randomly varying block sizes groups controlling for baseline level of outcome. The 2 or
of 4 and 8 prepared by the study statisticians prior to begin- Fisher exact tests were used to compare proportions of par-
3
ning enrollment. Sealed envelopes containing the assign- ticipants self-reporting health care utilization outcomes.
ment were used to conceal allocation. Relative risk was used to compare patient-reported success
between groups.31 We conducted a secondary, per-protocol
Interventions analysis including only participants in the usual care group
Following baseline examination but before randomization, who did not receive physical therapy during the first 4
all participants were educated about the favorable prognosis weeks, and those in the early physical therapy group who
of LBP and advised to remain as active as possible. Partici- received a protocol-compliant episode defined as attending
pants were given a copy of The Back Book,25 and the contents at least 3 treatment sessions in the first 4 weeks and receiving
were reviewed with the researcher. The Back Book provides spinal manipulation at each of the first 2 sessions. Analyses
messages consistent with LBP guidelines.8,12,26 All partici- used a 2-sided of 0.05 without adjustment for multiple
pants were advised to follow-up with their primary care phy- comparisons using SAS (SAS Institute), version 9.4.
sician as needed. The usual care group received no further
intervention.
The early physical therapy group began treatment within
72 hours of enrollment with a physical therapist trained in
Results
study procedures. Four treatment sessions were scheduled From March 2011 to November 2013, 1220 potentially eligible
over 3 weeks (2 sessions in week 1, followed by 2 weekly ses- individuals were identified from which 220 participants en-
sions). Each session began with an assessment. In session 1, rolled (Figure). Randomization assigned 112 participants to
the assessment was followed by spinal manipulation using usual care and 108 participants to early physical therapy. One
the technique specified in the development of the decision participant randomized to early physical therapy was errone-
rule.15 The technique begins with the patient in a supine ously assigned to usual care. This participant was analyzed with
position. Then the physical therapist side bends and rotates the early physical therapy group for primary analyses. Eight
the patients spine and then provides a high-velocity, low- participants (3.6% of the total participants; 7 in the usual care 8
amplitude thrust to the pelvis. After spinal manipulation, the group and 1 in the early physical therapy group) dropped out
physical therapist provided instruction in spinal range-of- of the study; 7 participants gave no reason, 1 participant cited
motion exercises. Participants were instructed to perform 10 family responsibilities. One-year follow-up was completed by
exercise repetitions 3 to 4 times throughout the day. Session 207 participants (94.1%).
2 was scheduled 2 to 3 days after the first session and began The mean age was 37.4 years (SD, 10.3), 115 participants
with the manipulation followed by a review of range-of- (52.3%) were women, the mean body mass index (BMI; calcu-
motion exercises and instruction in trunk-strengthening lated as weight in kilograms divided by height in meters
exercises designed to strengthen the primary stabilizing squared) was 29.1 (SD, 7.9), and 16 participants (7.3%) were cur-
muscle of the lumbar spine, with some evidence of reducing rent smokers (Table 1). Table 1 shows characteristics of the 2
risk of LBP recurrence.27 The third and fourth sessions were groups at baseline.
scheduled at 1-week intervals and involved exercise review
and progression (eAppendix 1 in the Supplement 2). Intervention Adherence
The early physical therapy group attended 97.2% of the sched-
Power and Statistical Analysis uled treatment sessions. Ninety-nine participants (92.5%) at-
Sample size for the primary outcome, change in ODI score from tended all 4 sessions, and 8 participants attended 2 or 3 ses-
baseline to 3 months after randomization, was based on de- sions. One participant did not receive the manipulation portion
tecting a 7-point difference (assumed SD, 16)14,28,29 or an ef- of the protocol and another participant received manipula-
fect size of 0.44. Enrollment of 110 participants per group tion at the fourth session in contradiction to the protocol; oth-
(N = 220) provided at least 86% power to detect this effect with erwise sessions were consistent with the protocol. Two par-
2-sided of 0.05 assuming at least a 90% follow-up rate. ticipants in the early physical therapy group received massage
Baseline characteristics were summarized by treatment therapy during the first 4 weeks of the study in contradiction
group. Analyses of primary and secondary outcomes were to the protocol. Sixteen participants (14.3%) in the usual care
jama.com (Reprinted) JAMA October 13, 2015 Volume 314, Number 14 1461
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by a Azienda Ospedaliero- Universitaria User on 01/11/2016
Research Original Investigation Early Physical Therapy vs Usual Care for Recent-Onset Low Back Pain
Figure. Participant Recruitment and Retention
1220 Patients screened for eligibility
999 Excluded
735 Symptom duration >15 d
97 Care in past 6 mo
59 Symptoms distal to knee
38 Prior lumbar surgery
21 ODI disability score <20%
19 Had signs of nerve root
compression
18 Possible red flag finding
12 Current pregnancy
221 Eligible to participate
1 Excluded (refused participation)
220 Randomized
108 Randomized to receive early 112 Randomized to receive usual care
physical therapy 112 Received care as randomized
107 Received physical therapy
as randomized
1 Erroneously received
usual care
107 Completed 4-week follow-up 108 Completed 4-week follow-up
1 Missed follow-up 2 Missed follow-up
7 Off-protocol events 2 Dropped out
2 Massage therapy visit 16 Off-protocol events
4 Attended 2 or fewer study 7 Massage therapy visit
physical therapy visits 3 Spine specialist physician visit
1 Did not receive manipulation 3 Physical therapy visit
during study physical therapy 3 Chiropractic visit
106 Completed 3-month follow-up 108 Completed 3-month follow-up
8 1 Missed follow-up 2 Missed follow-up
1 Dropped out 2 Dropped out (cumulative)
104 Completed 1-year follow-up 103 Completed 1-year follow-up
3 Missed follow-up 2 Missed follow-up
1 Dropped out (cumulative) 7 Dropped out (cumulative)
108 Included in primary analysis 112 Included in primary analysis
(3-month outcome) (3-month outcome)
ODI indicates Oswestry Disability
Index.
group deviated from the protocol during the first 4 weeks; 7 score) at 3 months (mean difference, 3.2 [95% CI, 5.9 to
participants received massage therapy, 3 participants re- 0.47], P = .02). The ODI score also showed significantly
ceived physical therapy, 3 participants received chiropractic greater improvement for early physical therapy after 4
care, and 3 participants received a spine specialist physician weeks but not after 1 year (Table 2). Some secondary out-
visit (2 participants visited a physiatrist and 1 participant vis- comes showed statistically significant differences favoring
ited an orthopedic surgeon). greater improvement in the early physical therapy group
particularly at 3 months. These included PCS score, fear-
Early Physical Therapy Adverse Effects avoidance beliefs for work, and patients self-rating of suc-
Thirteen participants receiving early physical therapy (12.0%) cess and self-rating of their overall health (Table 2 and
reported a total of 20 adverse effects from treatment including Table 3). However, many secondary outcomes showed no
increased pain (1 mild, 4 moderate, 2 severe, and 1 no severity statistically significant benefit for early physical therapy at 3
given), stiffness (2 mild, 3 moderate, 1 severe, and 1 no severity months and/or other follow-up time points (Table 2 and
given), spasm (1 severe and 1 no severity given), shooting pain Table 3). For example, there were no significant differences
(1 moderate and 1 no severity given), and fatigue (1 mild). in pain intensity or the FABQ for physical activity at any
time point. There was no difference in the FABQ for work
Primary and Secondary Outcomes score at the 4-week or 1-year follow-up and there was no dif-
Early physical therapy showed significant improvement ference in the EQ-5D quality-of-life score at the 4-week or
compared with usual care for the primary outcome (ODI 3-month follow-up. There were no statistically significant
1462 JAMA October 13, 2015 Volume 314, Number 14 (Reprinted) jama.com
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by a Azienda Ospedaliero- Universitaria User on 01/11/2016
Early Physical Therapy vs Usual Care for Recent-Onset Low Back Pain Original Investigation Research
differences between groups for health care utilization out-
comes at any follow-up (Table 3).
Table 1. Baseline Participant Characteristics 4
No. (%)
Early
Per-Protocol Analysis Usual Care Physical Therapy
Per-protocol analysis excluded 3 participants from the usual (n = 112) (n = 108)
care group who received physical therapy in the first 4 weeks Age, mean (SD), y 36.5 (10.2) 38.3 (10.4)
and 5 participants in the early physical therapy group who Women 53 (47.3) 62 (57.4)
did not receive a compliant physical therapy episode. The Race/ethnicity
participant randomized to early physical therapy who erro- White 89 (79.5) 89 (82.4)
neously received usual care was included in the usual care Hispanic 13 (11.6) 5 (4.6)
group. Results were similar to primary analyses with a signifi- African American 2 (1.8) 3 (2.8)
cant difference in the primary outcome ODI score at 3 Other/multiracial 8 (7.1) 11 (10.2)
months favoring greater improvement for early physical BMI, mean (SD) 29.2 (8.5) 28.9 (7.3)
therapy (mean difference, 3.7 [95% CI, 0.93 to 6.4], Married/live with significant other 69 (61.6) 69 (63.9)
P = .01). Per-protocol analyses found significantly greater lev-
Education
els of patient-reported success at 4 weeks and 3 months and
Completed high school 110 (98.2) 106 (98.1)
significantly greater improvement in pain ratings favoring
Completed degree after high school 49 (43.8) 59 (54.6)
early physical therapy after 4 weeks and 3 months (eAppen-
Employment status 92 (82.1) 92 (85.2)
dix 2 in the Supplement 2). However, many secondary out- (employed outside the home)
comes showed no statistically significant benefit for early Comorbid health conditions
physical therapy at 1 year and/or other follow-up time points. Diabetes 6 (5.4) 3 (2.8)
There were no statistically significant differences between Hypertension 10 (8.9) 8 (7.4)
groups after 1 year for the ODI score, numeric pain rating, Anxiety/depression 31 (27.7) 28 (25.9)
FABQ score for work, PCS score, or patient self-rating of suc- Upper back/neck pain 37 (33.0) 43 (39.8)
cess outcomes. The FABQ score for physical activity and Current medications for back pain
health care utilization outcomes did not differ between
Nonsteroidal anti-inflammatory 74 (66.1) 73 (67.6)
groups at any time point.
Opioids 30 (26.8) 29 (26.9)
Muscle relaxers 61 (54.5) 62 (57.4)
Steroid anti-inflammatory 16 (14.3) 10 (9.3)
Discussion Other 8 (7.1) 4 (3.7)
Current smoker 7 (6.3) 9 (8.3)
This randomized clinical trial enrolled adults with recent-
History of treated low back pain 72 (64.3) 74 (68.5)
onset LBP following a primary care visit and compared early
ODI score, mean (SD) 40.9 (12.1) 41.3 (14.1)
physical therapy with usual care (no additional intervention
beyond education) during the first 4 weeks. The primary out- Numeric pain rating, mean (SD)a 5.1 (1.9) 5.3 (1.8)
come was change in disability, measured by the ODI score, FABQ score, mean (SD)
after 3 months. Early physical therapy resulted in statistically Physical activity 15.4 (4.9) 14.8 (4.9)
significant improvement in disability relative to usual care Work 12.1 (8.9 11.3 (9.0)
but the magnitude of the difference was modest and did not PCS score, mean (SD)b 13.8 (10.1) 13.9 (11.0)
achieve the minimum difference considered clinically impor- EQ-5D score, mean (SD)
tant at the individual patient level. There was no difference Quality of life 0.67 (0.2) 0.65 (0.2)
between groups in the ODI score at 1-year follow-up. Results Overall health self-ratingc 66.3 (19.4) 68.3 (16.5)
for other secondary outcomes were mixed. Results favored Abbreviations: BMI, body mass index (calculated as weight in kilograms divided
early physical therapy at 3-month follow-up for outcomes of by height in meters squared); EQ-5D, 5-Dimensional EuroQol; FABQ,
patient-reported success and overall health, PCS score, and Fear-Avoidance Beliefs Questionnaire; ODI, Oswestry Disability Index;
PCS, Pain Catastrophizing Scale.
fear-avoidance beliefs for work. Most differences between
a
Three missing scores (1 early physical therapy, 2 usual care), means reflect
groups were modest. There were no improvements in pain
multiple imputation for missing scores.
intensity or the FABQ for physical activity outcome at any b
One missing score (1 usual care), mean reflects multiple imputation
time point. There was no benefit for the EQ-5D quality-of-life for missing score.
outcome at 4-week or 3-month follow-up and many other c
One missing score (1 early physical therapy), mean reflects multiple imputation
secondary outcomes also showed no benefit. Health care uti- for missing score.
lization at each follow-up did not differ between groups.
Primary care physicians are typically the first-contact pro-
vider for patients with LBP in the United States. Guideline- lines with the rationale that a majority of patients recover
discordant decisions at initial contact are associated with rapidly regardless.12,32 Observational studies involving large
inc reased risk for prolonged disability and invasive Medicare33 and privately insured9 samples report higher
procedures.10,11,13 Referral to physical therapy is not advised costs and greater risk for invasive procedure when physical
in the first few weeks following initial contact in many guide- therapy is delayed beyond 2 to 4 weeks, suggesting referral at
jama.com (Reprinted) JAMA October 13, 2015 Volume 314, Number 14 1463
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by a Azienda Ospedaliero- Universitaria User on 01/11/2016
Research Original Investigation Early Physical Therapy vs Usual Care for Recent-Onset Low Back Pain
Table 2. Primary and Secondary Outcomes for Early Physical Therapy vs Usual Care for Recent-Onset Low Back Pain
Usual Care Early Intervention
Mean Difference
Between Groups in
10,11
Mean Change Mean Change From Change from
Outcome Visit Mean Score From Baseline Mean Score Baseline Baselinea P Value
Primary Outcome
ODI score (0-100 scale; Baseline 40.9 41.3
higher scores indicate worse (38.6 to 43.1) (38.7 to 44.0)
function)b 4 wk 14.5 26.6 11.1 30.0 3.5 .045
(12.1 to 17.0) (29.0 to 24.1) (8.7 to 13.4) (32.4 to 27.7) (6.8 to 0.08)
3 mo 9.8 31.3 6.6 34.5 3.2 .02
(7.9 to 11.7) (33.2 to 29.4) (4.7 to 8.5) (36.4 to 32.6) (5.9 to 0.47)
1y 9.0 32.1 7.0 34.1 2.0 .19
(6.8 to 11.1) (34.3 to 30.0) (4.8 to 9.1) (36.3 to 32.0) (5.0 to 1.0)
Secondary Outcomes
Numeric pain rating Baseline 5.1 5.3
(0-10 scale; higher scores (4.7 to 5.4) (4.9 to 5.6)
indicate greater pain 4 wk 2.1 3.0 1.7 3.4 0.42 .09
intensity)c (1.8 to 2.5) (3.4 to 2.7) (1.4 to 2.1) (3.8 to 3.1) (0.90 to 0.02)
3 mo 1.8 3.4 1.4 3.8 0.38 .11
(1.4 to 2.1) (3.7 to 3.1) (1.1 to 1.7) (4.1 to 3.5) (0.84 to 0.09)
1y 1.4 3.7 1.3 3.9 0.17 .44
(1.1 to 1.8) (4.0 to 3.4) (0.94 to 1.6) (4.2 to 3.6) (0.62 to 0.27)
PCS score Baseline 13.8 13.9
(0-52 scale; higher scores (12.0 to 15.7) (11.8 to 15.9)
indicate greater 4 wk 7.6 6.2 4.9 8.9 2.7 .004
pain-catastrophizing (6.3 to 9.0) (7.6 to 4.9) (3.6 to 6.2) (10.2 to 7.6) (4.6 to 0.85)
beliefs)d
3 mo 5.2 8.6 3.0 10.9 2.2 .01
(4.0 to 6.4) (9.9 to 7.4) (1.8 to 4.2) (12.1 to 9.6) (3.9 to 0.49)
1y 4.3 9.6 3.3 10.5 0.92 .31
(3.0 to 5.5) (10.8 to 8.3) (2.1 to 4.6) (11.8 to 9.3) (2.7 to 0.61)
FABQ score for physical Baseline 15.4 14.8
activity (14.5 to 16.3) (13.8 to 15.7)
(0-24 scale; higher scores 4 wk 7.9 7.2 7.2 7.8 0.67 .37
indicate greater (6.9 to 8.9) (8.2 to 6.1) (6.2 to 8.3) (8.9 to 6.8) (2.2 to 0.81)
fear-avoidance beliefs)e
3 mo 5.7 9.3 5.2 9.9 0.54 .46
(4.7 to 6.7) (10.3 to 8.3) (4.2 to 6.2) (10.9 to 8.9) (2.0 to 0.90)
1y 5.7 9.4 5.7 9.4 0.02 .98
(4.4 to 6.9) (10.6 to 8.2) (4.5 to 6.9) (10.6 to 8.2) (1.70 to 1.74)
FABQ score for work Baseline 12.1 11.3
(0-42 scale; higher scores (10.2 to 14.0) (9.6 to 13.0)
indicate greater 4 wk 9.1 2.7 8.0 3.7 1.0 .28
fear-avoidance beliefs)f (7.8 to 10.3) (4.0 to 1.4) (6.8 to 9.3) (5.0 to 2.4) (2.8 to 0.82)
3 mo 7.5 4.3 5.2 6.5 2.3 .02
(6.2 to 8.8) (5.5 to 3.0) (3.9 to 6.5) (7.9 to 5.2) (4.1 to 0.4)
1y 6.2 5.5 5.2 6.5 1.0 .31
(4.8 to 7.5) (6.9 to 4.2) (3.9 to 6.5) (7.8 to 5.2) (2.8 to 0.90)
EQ-5D score for quality Baseline 0.67 0.65
of life (0.64 to 0.80) (0.62 to 0.69)
(0-1 scale; higher scores 4 wk 0.84 0.18 0.87 0.21 0.03 .05
indicate greater quality (0.82 to 0.86) (0.15 to 0.20) (0.85 to 0.89) (0.19 to 0.23) (0.0 to 0.07)
of life)g
3 mo 0.88 0.22 0.91 0.24 0.03 .10
(0.86 to 0.90) (0.20 to 0.24) (0.88 to 0.93) (0.22 to 0.27) (0.01 to 0.06)
1y 0.88 0.22 0.92 0.26 0.04 .02
(0.86 to 0.90) (0.20 to 0.24) (0.90 to 0.94) (0.24 to 0.28) (0.01 to 0.07)
EQ-5D score for overall Baseline 66.3 68.3
health self-rating (62.7 to 69.9) (65.2 to 71.4)
(0-100 scale; higher 4 wk 72.5 5.2 77.6 10.4 5.2 .03
scores indicate greater (69.3 to 75.7) (2.0 to 8.4) (74.5 to 80.8) (7.2 to 13.5) (0.64 to 9.7)
self-rated health)c
3 mo 73.3 6.0 79.2 11.9 5.9 .02
(69.7 to 76.8) (2.5 to 9.6) (75.6 to 82.8) (8.3 to 15.5) (0.91 to 10.9)
1y 75.3 8.0 80.9 13.6 5.6 .02
(71.9 to 78.7) (4.6 to 11.4) (77.5 to 84.3) (10.3 to 17.0) (0.77 to 10.4)
d
Abbreviations: EQ-5D, 5-Dimensional EuroQol; FABQ, Fear-Avoidance Beliefs Missing scores: 1 at baseline, 6 at 4 weeks, 6 at 3 months, and 13 at 1 year;
Questionnaire; ODI, Oswestry Disability Index; PCS, Pain Catastrophizing Scale. imputed using multiple imputation procedure.
a e
Mean differences are adjusted for baseline scores of outcome variable. Missing scores: 0 at baseline, 5 at 4 weeks, 5 at 3 months, and 13 at 1 year;
b
Missing scores: 0 at baseline, 7 at 4 weeks, 5 at 3 months, and 14 at 1 year; imputed using multiple imputation procedure.
f
imputed using multiple imputation procedure. Missing scores: 0 at baseline, 7 at 4 weeks, 6 at 3 months, and 13 at 1 year;
c
Missing scores: 3 at baseline, 6 at 4 weeks, 5 at 3 months, and 12 at 1 year; imputed using multiple imputation procedure.
g
imputed using multiple imputation procedure. Missing scores: 1 at baseline, 6 at 4 weeks, 8 at 3 months, and 13 at 1 year;
imputed using multiple imputation procedure.
1464 JAMA October 13, 2015 Volume 314, Number 14 (Reprinted) jama.com
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by a Azienda Ospedaliero- Universitaria User on 01/11/2016
Early Physical Therapy vs Usual Care for Recent-Onset Low Back Pain Original Investigation Research
Table 3. Dichotomous Secondary Outcomes for Early Physical Therapy vs Usual Care for Recent-Onset
Low Back Pain
Participants, No. (%)
Early Physical Therapy Usual Care Relative Risk (95% CI) P Valuea
Patient-reported successb
4 wk 60 (55.6) 50 (44.6) 1.24 (0.95-1.63) .12
3 mo 64 (59.3) 49 (44.0) 1.35 (1.03-1.75) .03
1y 65 (59.7) 60 (53.7) 1.11 (0.88-1.42) .38
Health Care Utilization Outcomesd
Emergency department
or urgent care visitc
4 wk 0 1 (0.9) >.99
3 mo 2 (1.9) 2 (1.8) .97
Total at 1 y 9 (8.4) 9 (8.1) .94
Advanced imaging
4 wk 0 1 (0.9) >.99
3 mo 2 (1.9) 1 (0.9) .62 a
Relative risks calculated using the
Total at 1 y 3 (2.8) 4 (3.6) .74 Zou method.31
b
Spine specialist physician visit Missing scores: 6 at 4 weeks, 5 at 3
4 wk 0 3 (2.8) >.99 months, and 12 at 1 year; imputed
using multiple imputation
3 mo 3 (2.8) 7 (6.3) .23
procedure (15-point Likert scale;
Total at 1 y 8 (7.5) 11 (9.9) .53 self-ratings of a great deal better
Spine injection or a very great deal better defined
4 wk 0 0 as success).
c
3 mo 1 (0.9) 1 (0.9) .98 P values from Fisher exact tests.
d
Total at 1 y 2 (1.9) 3 (2.8) .68 One hundred fifty six participants
(70.9%) completed 12 monthly
Spine surgery online diaries reporting utilization
4 wk 0 0 outcomes, 196 participants (89.1%)
3 mo 0 1 (0.9) >.99 completed 10 or more, 206
participants (93.6%) completed 8
Total at 1 y 2 (1.9) 1 (0.9) .62
or more.
initial contact may be preferable, at least for some patients. benefit from early physical therapy, but further research
To our knowledge, no previous studies have tested this should investigate this question.
hypothesis of early physical therapy vs usual care following Other strategies to identify patient subgroups who
initial primary care contact. Effect sizes were small and did are likely to benefit from physical therapy have been
not achieve the minimum clinically important difference for described. A promising approach stratifies patients based on
the primary outcome. For secondary outcomes, early physi- the presence of physical and psychosocial factors using the
cal therapy showed benefit across some, but not across all, StarT Back screening tool. 35 Physical therapy is recom-
domains. The potential benefits of early physical therapy mended for patients with predominantly physical prognostic
should be considered in light of the time and effort required factors, whereas therapy augmented with efforts to over-
to participate in physical therapy. come psychosocial obstacles is recommended for patients
Because of the volume of LBP patients and recognition with both physical and psychosocial factors.36 Although our
that many improve quickly, efforts have been made to iden- physical therapy protocol did not include explicit interven-
tify patient subgroups most likely to benefit from early tions to address psychosocial factors (eg, cognitive behav-
physical therapy. This study examined a subgroup described ioral therapy), we found greater improvement in important
in previous research as responsive to the specific physical psychosocial constructs including PCS score and fear-
therapy protocol used.34 The subgroup is characterized by avoidance beliefs in this group. This may result from inter-
at least moderate disability (ODI score 20), acute onset vening early for acute LBP when adverse psychosocial beliefs
(<16 days duration), no symptoms distal to the knee(s) or may be more amenable to change without specific psycho-
clinical findings suggesting nerve root compression. We logical interventions.37 However, further study is needed to
selected this subgroup because it is linked to a specific confirm this theory.
physical therapy protocol of spinal manipulation and exer- We found that patients in both groups improved rapidly.
cise, which are evidence-based LBP treatments.12 The major- Rapid and substantial improvement by most patients with
ity of exclusions resulted from the acuity criterion (<16 days acute LBP limits treatment effects in early intervention
duration). This criterion maximized likelihood of success studies.38 We detected a modest difference favoring early
with this physical therapy protocol in prior research. 34 physical therapy that was better than the natural history of
Patients with somewhat longer symptom durations may acute LBP for the primary outcome at 3-month follow-up. How-
jama.com (Reprinted) JAMA October 13, 2015 Volume 314, Number 14 1465
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by a Azienda Ospedaliero- Universitaria User on 01/11/2016
Research Original Investigation Early Physical Therapy vs Usual Care for Recent-Onset Low Back Pain
ever, the between-group difference did not achieve the thresh- a component of primary care practice,40 our approach was
old for minimum clinically important difference. Further- likely beyond what typically occurs.
more, differences were mostly undetectable by 1 year. Our study has limitations. First, although more than 90%
We designed our physical therapy protocol for effi- of participants provided data after 1 year, there were more pa-
ciency, focusing on evidence-based treatments (education, tients who dropped out from the usual care group than from
exercise, and manipulation).12 We did not include passive the early physical therapy group. Second, results of our sec-
modalities (eg, ultrasound) that are frequently used but are ondary outcomes should be interpreted cautiously as we did
not evidence-based 12 and may prolong physical therapy not adjust for multiple comparisons. Third, we did not in-
episodes.39 Our physical therapy protocol used 4 treatment clude an attention control group. Fourth, we did not assess ad-
sessions compared with national averages of more than 7 verse events in the usual care group.
sessions for acute LBP.9 We believe this 4-session protocol is
practical for routine clinical use. Additional research is
needed to evaluate its effectiveness under more pragmatic
circumstances.
Conclusions
We provided education to both groups. Our education in- Among adults with recent-onset LBP, early physical therapy
volved written materials and dialogue focused on encourag- resulted in statistically significant improvement in disability,
ing activity and assuaging concerns that imaging should be per- but the improvement was modest and did not achieve the mini-
formed. Although education is recommended by guidelines as mum clinically important difference compared with usual care.
ARTICLE INFORMATION Physical Therapy), and Lucy Savitz, PhD clinical guidelines for the management of
Author Contributions: Dr Fritz and Ms McFadden (Intermountain Healthcare). nonspecific low back pain in primary care.
had full access to all of the data in the study and Additional Contributions: We thank the following Eur Spine J. 2010;19(12):2075-2094.
take responsibility for the integrity of the data and research assistants for their roles in delivering the 9. Fritz JM, Childs JD, Wainner RS, Flynn TW.
the accuracy of the data analysis. physical therapy intervention: Kate Thayn, DPT Primary care referral of patients with low back pain
Study concept and design: Fritz, Asche, Brennan. (Intermountain Healthcare); Dershung Yang, PhD, to physical therapy: impact on future health care
Acquisition, analysis, or interpretation of data: Fritz, and Niina Haas, MA (both from BrightOutcome), utilization and costs. Spine (Phila Pa 1976). 2012;37
Magel, McFadden, Asche, Thackeray, Meier, developed the electronic data collection platform (25):2114-2121.
Brennan. and database, contributed to the data 10. Graves JM, Fulton-Kehoe D, Jarvik JG, Franklin
Drafting of the manuscript: Fritz, McFadden, Asche. management, and oversaw the web maintenance. GM. Health care utilization and costs associated
Critical revision of the manuscript for important Tom Greene, PhD, provided oversight for the with adherence to clinical practice guidelines for
intellectual content: Fritz, Magel, McFadden, Asche, statistical planning and data analysis of this trial. All early magnetic resonance imaging among workers
Thackeray, Meier, Brennan. of the people acknowledged above were with acute occupational low back pain. Health Serv
Statistical analysis: McFadden, Asche. compensated for their work (including the data and Res. 2014;49(2):645-665.
Obtained funding: Fritz, Asche. safety monitoring board) in this study.
Administrative, technical, or material support: Fritz, 11. Webster BS, Choi Y, Bauer AZ, Cifuentes M,
Magel, McFadden, Thackeray, Meier, Brennan. REFERENCES Pransky G. The cascade of medical services and
Study supervision: Fritz, Thackeray, Brennan. associated longitudinal costs due to nonadherent
1. Deyo RA, Mirza SK, Martin BI. Back pain magnetic resonance imaging for low back pain.
Conflict of Interest Disclosures: All authors have prevalence and visit rates: estimates from Spine (Phila Pa 1976). 2014;39(17):1433-1440.
completed and submitted the ICMJE Form for US national surveys, 2002. Spine (Phila Pa 1976).
Disclosure of Potential Conflicts of Interest. Dr Fritz 2006;31(23):2724-2727. 12. Chou R, Huffman LH; American Pain Society;
reports receiving personal fees from Focus On American College of Physicians. Nonpharmacologic
2. Licciardone JC. The epidemiology and medical therapies for acute and chronic low back pain:
Therapeutic Outcomes. No other disclosures were management of low back pain during ambulatory
reported. a review of the evidence for an American Pain
medical care visits in the United States. Osteopath Society/American College of Physicians clinical
Funding/Support: This study was funded by grant Med Prim Care. 2008;2:11. practice guideline. Ann Intern Med. 2007;147(7):
1R18HS018672 from the Agency for Healthcare 3. Martin BI, Deyo RA, Mirza SK, et al. Expenditures 492-504.
Research and Quality. The study was supported by and health status among adults with back and neck
the University of Utah Study Design and 13. Fritz JM, Brennan GP, Hunter SJ, Magel JS.
problems. JAMA. 2008;299(6):656-664. Initial management decisions after a new
Biostatistics Center, with funding in part through
grant 5UL1TR001067-02 (formerly 8UL1TR000105 4. Davis MA, Onega T, Weeks WB, Lurie JD. Where consultation for low back pain: implications of the
and UL1RR025764) from the National Center for the United States spends its spine dollars: usage of physical therapy for subsequent health
Research Resources and the National Center for expenditures on different ambulatory services for care costs and utilization. Arch Phys Med Rehabil.
Advancing Translational Sciences of the National the management of back and neck conditions. 2013;94(5):808-816.
Institutes of Health. Spine (Phila Pa 1976). 2012;37(19):1693-1701. 14. Childs JD, Fritz JM, Flynn TW, et al. A clinical
Role of the Funder/Sponsor: The Agency for 5. Freburger JK, Holmes GM, Agans RP, et al. The prediction rule to identify patients with low back
Healthcare Research and Quality had no role in the rising prevalence of chronic low back pain. Arch pain most likely to benefit from spinal
design and conduct of the study; collection, Intern Med. 2009;169(3):251-258. manipulation: a validation study. Ann Intern Med.
management, analysis, and interpretation of the 6. Mafi JN, McCarthy EP, Davis RB, Landon BE. 2004;141(12):920-928.
data; preparation, review, or approval of the Worsening trends in the management and 15. Cleland JA, Fritz JM, Kulig K, et al. Comparison
manuscript; and decision to submit the manuscript treatment of back pain. JAMA Intern Med. 2013;173 of the effectiveness of 3 manual physical therapy
for publication. (17):1573-1581. techniques in a subgroup of patients with low back
Data and Safety Monitoring Board: Roger Chou, 7. Kosloff TM, Elton D, Shulman SA, Clarke JL, pain who satisfy a clinical prediction rule:
MD (Oregon Health and Science University), Skoufalos A, Solis A. Conservative spine care: a randomized clinical trial. Spine (Phila Pa 1976).
Anthony Delitto, PhD, PT, FAPTA (University of opportunities to improve the quality and value of 2009;34(25):2720-2729.
Pittsburgh), Richard Holubkov, PhD (University of care. Popul Health Manag. 2013;16(6):390-396. 16. Fairbank JC, Pynsent PB. The Oswestry
Utah), John Childs, PhD, PT, MBA, FAPTA 8. Koes BW, van Tulder M, Lin CW, Macedo LG, Disability Index. Spine (Phila Pa 1976). 2000;25(22):
(US Army-Baylor University Doctoral Program in McAuley J, Maher C. An updated overview of 2940-2952.
1466 JAMA October 13, 2015 Volume 314, Number 14 (Reprinted) jama.com
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by a Azienda Ospedaliero- Universitaria User on 01/11/2016
Early Physical Therapy vs Usual Care for Recent-Onset Low Back Pain Original Investigation Research
17. Fritz JM, Irrgang JJ. A comparison of a modified 25. Martin R, Waddell G, Klaber Moffett J, Burton role of physical therapy. Spine (Phila Pa 1976). 2012;
Oswestry Low Back Pain Disability Questionnaire K, Main C. The Back Book. London, UK: The Stationary 37(9):775-782.
and the Quebec Back Pain Disability Scale. Phys Ther. Office; 1996. 34. Flynn T, Fritz J, Whitman J, et al. A clinical
2001;81(2):776-788. 26. van Tulder M, Becker A, Bekkering T, et al; prediction rule for classifying patients with low back
18. Childs JD, Piva SR, Fritz JM. Responsiveness of COST B13 Working Group on Guidelines for the pain who demonstrate short-term improvement
the numeric pain rating scale in patients with low Management of Acute Low Back Pain in Primary with spinal manipulation. Spine (Phila Pa 1976).
back pain. Spine (Phila Pa 1976). 2005;30(11):1331- Care. Chapter 3: European guidelines for the 2002;27(24):2835-2843.
1334. management of acute nonspecific low back pain in 35. Hill JC, Dunn KM, Lewis M, et al. A primary care
19. Sullivan MJL, Bishop SR, Pivik J. The Pain primary care. Eur Spine J. 2006;15(suppl 2):S169-S191. back pain screening tool: identifying patient
Catastrophizing Scale: development and validation. 27. Macedo LG, Maher CG, Latimer J, McAuley JH. subgroups for initial treatment. Arthritis Rheum.
Psychol Assess. 1995;7(4):524-532. doi:10.1037 Motor control exercise for persistent, nonspecific 2008;59(5):632-641.
/1040-3590.7.4.524. low back pain: a systematic review. Phys Ther. 36. Hill JC, Whitehurst DG, Lewis M, et al.
20. Waddell G, Newton M, Henderson I, Somerville 2009;89(1):9-25. Comparison of stratified primary care management
D, Main CJ. A Fear-Avoidance Beliefs Questionnaire 28. Brennan GP, Fritz JM, Hunter SJ, Thackeray A, for low back pain with current best practice
(FABQ) and the role of fear-avoidance beliefs in Delitto A, Erhard RE. Identifying subgroups of (STarT Back): a randomised controlled trial. Lancet.
chronic low back pain and disability. Pain. 1993;52 patients with acute/subacute nonspecific low 2011;378(9802):1560-1571.
(2):157-168. back pain: results of a randomized clinical trial. 37. Newcomer KL, Shelerud RA, Vickers Douglas
21. Jaeschke R, Singer J, Guyatt GH. Measurement Spine (Phila Pa 1976). 2006;31(6):623-631. KS, Larson DR, Crawford BJ. Anxiety levels,
of health status: ascertaining the minimal clinically 29. Fritz JM, Delitto A, Erhard RE. Comparison of fear-avoidance beliefs, and disability levels at
important difference. Control Clin Trials. 1989;10(4): classification-based physical therapy with therapy baseline and at 1 year among subjects with acute
407-415. based on clinical practice guidelines for patients and chronic low back pain. PM R. 2010;2(6):514-520.
22. Shaw JW, Johnson JA, Coons SJ. US valuation with acute low back pain: a randomized clinical trial. 38. Foster NE. Barriers and progress in the
of the EQ-5D health states: development and Spine (Phila Pa 1976). 2003;28(13):1363-1371. treatment of low back pain. BMC Med. 2011;9:108.
testing of the D1 valuation model. Med Care. 2005; 30. Schafer JL. Multiple imputation: a primer. Stat 39. Fritz JM, Cleland JA, Brennan GP. Does
43(3):203-220. Methods Med Res. 1999;8(1):3-15. adherence to the guideline recommendation for
23. Goossens ME, Rutten-van Mlken MP, Vlaeyen 31. Zou G. A modified Poisson regression approach active treatments improve the quality of care for
JW, van der Linden SM. The cost diary: a method to to prospective studies with binary data. Am J patients with acute low back pain delivered by
measure direct and indirect costs in Epidemiol. 2004;159(7):702-706. physical therapists? Med Care. 2007;45(10):973-980.
cost-effectiveness research. J Clin Epidemiol. 2000; 32. Fullen BM, Maher T, Bury G, Tynan A, Daly LE, 40. Dagenais S, Tricco AC, Haldeman S. Synthesis
53(7):688-695. Hurley DA. Adherence of Irish general practitioners of recommendations for the assessment and
24. Hurwitz EL, Morgenstern H, Vassilaki M, Chiang to European guidelines for acute low back pain: management of low back pain from recent clinical
LM. Frequency and clinical predictors of adverse a prospective pilot study. Eur J Pain. 2007;11(6): practice guidelines. Spine J. 2010;10(6):514-529.
reactions to chiropractic care in the UCLA neck pain 614-623.
study. Spine (Phila Pa 1976). 2005;30(13):1477-1484. 33. Gellhorn AC, Chan L, Martin B, Friedly J.
Management patterns in acute low back pain: the
jama.com (Reprinted) JAMA October 13, 2015 Volume 314, Number 14 1467
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by a Azienda Ospedaliero- Universitaria User on 01/11/2016
Das könnte Ihnen auch gefallen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Effectiveness of A Neck and Shoulder Stretching Exercise Program Among Office Workers With Neck Pain: A Randomized Controlled TrialDokument10 SeitenThe Effectiveness of A Neck and Shoulder Stretching Exercise Program Among Office Workers With Neck Pain: A Randomized Controlled TrialGiovanniNoch keine Bewertungen
- Prevention of LowBack PainDokument10 SeitenPrevention of LowBack PainGiovanniNoch keine Bewertungen
- Pilates Improves Pain, Function and Quality of Life in Patients With Chronic Low Back Pain: A Randomized Controlled TrialDokument11 SeitenPilates Improves Pain, Function and Quality of Life in Patients With Chronic Low Back Pain: A Randomized Controlled TrialGiovanniNoch keine Bewertungen
- Reliability and Diagnostic Accuracy of 5 Physical Examination Tests and Combination of Tests For Subacromial ImpingementDokument6 SeitenReliability and Diagnostic Accuracy of 5 Physical Examination Tests and Combination of Tests For Subacromial ImpingementGiovanniNoch keine Bewertungen
- J. Perry - Gait AnalysisDokument18 SeitenJ. Perry - Gait AnalysisGiovanniNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Pressure Vessels SHO ProgrammeDokument42 SeitenPressure Vessels SHO Programmehew ka yeeNoch keine Bewertungen
- Metallurgical Test Report: NAS Mexico SA de CV Privada Andres Guajardo No. 360 Apodaca, N.L., C.P. 66600 MexicoDokument1 SeiteMetallurgical Test Report: NAS Mexico SA de CV Privada Andres Guajardo No. 360 Apodaca, N.L., C.P. 66600 MexicoEmigdio MartinezNoch keine Bewertungen
- User Manual: 3603807 CONTACT US - 09501447202,8070690001Dokument1 SeiteUser Manual: 3603807 CONTACT US - 09501447202,8070690001Arokiaraj RajNoch keine Bewertungen
- Week5 6 2Dokument2 SeitenWeek5 6 2SAMANIEGO BERMEO DAVID SEBASTIANNoch keine Bewertungen
- EF4e Beg Quicktest 05Dokument3 SeitenEF4e Beg Quicktest 05terrenoruralcamboriuNoch keine Bewertungen
- Chapter One - FiveDokument118 SeitenChapter One - FivePrecious AnthonyNoch keine Bewertungen
- Metabolism of Carbohydrates and LipidsDokument7 SeitenMetabolism of Carbohydrates and LipidsKhazel CasimiroNoch keine Bewertungen
- Me N Mine Science X Ist TermDokument101 SeitenMe N Mine Science X Ist Termneelanshujain68% (19)
- PulpectomyDokument3 SeitenPulpectomyWafa Nabilah Kamal100% (1)
- Lesson Plan PPEDokument3 SeitenLesson Plan PPEErika Jean Moyo ManzanillaNoch keine Bewertungen
- Thorley Amended Complaint (Signed)Dokument13 SeitenThorley Amended Complaint (Signed)Heather ClemenceauNoch keine Bewertungen
- Emission Estimation Technique Manual: For Mining and Processing of Non-Metallic MineralsDokument84 SeitenEmission Estimation Technique Manual: For Mining and Processing of Non-Metallic MineralsAbdelaziem mahmoud abdelaalNoch keine Bewertungen
- Variance AnalysisDokument22 SeitenVariance AnalysisFrederick GbliNoch keine Bewertungen
- Nfpa 502 Critical Velocity Vs Fffs EffectsDokument5 SeitenNfpa 502 Critical Velocity Vs Fffs Effectsamir shokrNoch keine Bewertungen
- Resume Massage Therapist NtewDokument2 SeitenResume Massage Therapist NtewPartheebanNoch keine Bewertungen
- 220hp Caterpillar 3306 Gardner Denver SSP Screw Compressor DrawingsDokument34 Seiten220hp Caterpillar 3306 Gardner Denver SSP Screw Compressor DrawingsJVMNoch keine Bewertungen
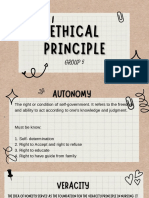
- Group 5 - Ethical PrinciplesDokument11 SeitenGroup 5 - Ethical Principlesvirgo paigeNoch keine Bewertungen
- Adult Module 1 - Five Healthy Habits Handout (English) PDFDokument2 SeitenAdult Module 1 - Five Healthy Habits Handout (English) PDFKennedy FadriquelanNoch keine Bewertungen
- TM - 1 1520 237 10 - CHG 10Dokument841 SeitenTM - 1 1520 237 10 - CHG 10johnharmuNoch keine Bewertungen
- WeaknessesDokument4 SeitenWeaknessesshyamiliNoch keine Bewertungen
- English PoemDokument4 SeitenEnglish Poemapi-276985258Noch keine Bewertungen
- Liebherr 2956 Manual de UsuarioDokument27 SeitenLiebherr 2956 Manual de UsuarioCarona FeisNoch keine Bewertungen
- Essay Type ExaminationDokument11 SeitenEssay Type ExaminationValarmathi83% (6)
- ClistDokument14 SeitenClistGuerraNoch keine Bewertungen
- Marketing Study of Mango JuiceDokument18 SeitenMarketing Study of Mango JuiceVijay ArapathNoch keine Bewertungen
- Bitumen BasicsDokument25 SeitenBitumen BasicsMILON KUMAR HORENoch keine Bewertungen
- Campus Sexual Violence - Statistics - RAINNDokument6 SeitenCampus Sexual Violence - Statistics - RAINNJulisa FernandezNoch keine Bewertungen
- Wilo Water PumpDokument16 SeitenWilo Water PumpThit SarNoch keine Bewertungen
- Complaint: Employment Sexual Harassment Discrimination Against Omnicom & DDB NYDokument38 SeitenComplaint: Employment Sexual Harassment Discrimination Against Omnicom & DDB NYscl1116953Noch keine Bewertungen
- Iso 9227Dokument13 SeitenIso 9227Raj Kumar100% (6)