Beruflich Dokumente
Kultur Dokumente
Kushimoto Et Al-2016-Acute Medicine & Surgery
Hochgeladen von
Nisa UcilCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Kushimoto Et Al-2016-Acute Medicine & Surgery
Hochgeladen von
Nisa UcilCopyright:
Verfügbare Formate
Acute Medicine & Surgery 2016; 3: 293–297 doi: 10.1002/ams2.
207
Mini Review Article
Lactate, a useful marker for disease mortality and severity
but an unreliable marker of tissue hypoxia/hypoperfusion
in critically ill patients
Shigeki Kushimoto,1 Satoshi Akaishi,2 Takeaki Sato,2 Ryosuke Nomura,2 Motoo Fujita,2
Daisuke Kudo,1 Yu Kawazoe,2 Yoshitaro Yoshida2 and Noriko Miyagawa2
1
Division of Emergency and Critical Care Medicine, Tohoku University Graduate School of Medicine, and
2
Department of Emergency and Critical Care Medicine, Tohoku University Hospital, Aoba-ku, Sendai, Miyagi,
Japan
Early aggressive hemodynamic resuscitation using elevated plasma lactate as a marker is an essential component of managing criti-
cally ill patients. Therefore, measurement of blood lactate is recommended to stratify patients based on the need for fluid resuscita-
tion and the risks of multiple organ dysfunction syndrome and death. Hyperlactatemia is common among critically ill patients, and
lactate levels and their trend may be reliable markers of illness severity and mortality. Although hyperlactatemia has been widely rec-
ognized as a marker of tissue hypoxia/hypoperfusion, it can also result from increased or accelerated aerobic glycolysis during the
stress response. Additionally, lactate may represent an important energy source for patients in critical condition. Despite its inherent
complexity, the current simplified view of hyperlactatemia is that it reflects the presence of global tissue hypoxia/hypoperfusion with
anaerobic glycolysis. This review of hyperlactatemia in critically ill patients focuses on its pathophysiological aspects and recent clini-
cal approaches. Hyperlactatemia in critically ill patients must be considered to be related to tissue hypoxia/hypoperfusion. Therefore,
appropriate hemodynamic resuscitation is required to correct the pathological condition immediately. However, hyperlactatemia can
also result from aerobic glycolysis, unrelated to tissue dysoxia, which is unlikely to respond to increases in systemic oxygen delivery.
Because hyperlactatemia may be simultaneously related to, and unrelated to, tissue hypoxia, physicians should recognize that resus-
citation to normalize plasma lactate levels could be over-resuscitation and may worsen the physiological status. Lactate is a reliable
indicator of sepsis severity and a marker of resuscitation; however, it is an unreliable marker of tissue hypoxia/hypoperfusion.
Key words: Beta-2 adrenergic receptor, gluconeogenesis, hypoperfusion, lactate, resuscitation
Elevated plasma lactate levels have been recommended as
INTRODUCTION
a parameter for hemodynamic resuscitation. In the manage-
E ARLY AGGRESSIVE HEMODYNAMIC resuscita-
tion is recommended for managing critically ill patients,
especially those with severe trauma and sepsis. Resuscita-
ment of patients with trauma, it has been suggested that up
to 85% of severely injured patients continue to exhibit inad-
equate tissue oxygenation after normalization of the conven-
tion is a critical component of management that is required tional markers of resuscitation, including restoration of
beyond the identification of the origin of major hemorrhage normal blood pressure, heart rate, and urine output.4 There-
and its control1 and identification of the septic focus and its fore, measurement of blood lactate is recommended to strat-
treatment with appropriate antibiotics.2,3 ify patients based on the need for ongoing fluid
resuscitation, the risk of multiple organ dysfunction syn-
drome and death,4 as a marker for identifying patients
Corresponding: Shigeki Kushimoto, MD, PhD, Division of requiring early aggressive resuscitation.5
Emergency and Critical Care Medicine, Tohoku University Hyperlactatemia is common among patients requiring
Graduate School of Medicine, Department of Emergency and critical care, and lactate levels and their trend may be reli-
Critical Care Medicine, Tohoku University Hospital, 1-1 Seiryo- able markers of illness severity and mortality.6,7 Lactate
machi, Aoba-ku, Sendai 980-8574, Japan. E-mail:
kussie@emergency-medicine.med.tohoku.ac.jp.
was recently included in a multibiomarker-based outcome
Received 8 Feb, 2016; accepted 19 Mar, 2016; online publication risk model for patients with septic shock.8 Although hyper-
16 May, 2016 lactatemia has been widely recognized as a marker of
© 2016 Japanese Association for Acute Medicine 293
294 S. Kushimoto et al. Acute Medicine & Surgery 2016; 3: 293–297
tissue hypoxia/hypoperfusion, the source, biochemistry, pyruvate generation will increase lactate generation
and metabolic functions of lactate remain unclear. (Fig. 1).
Recently, it was clearly suggested that hyperlactatemia Lactate can be metabolized by the liver and the kidneys
could result not only from tissue hypoxia or anaerobic gly- either through direct oxidation or as a source of glucose,9,11
colysis but also from increased or accelerated aerobic gly- and the liver accounts for up to 70% of whole body lactate
colysis during the stress response.9–11 Additionally, lactate clearance.16 Under normal conditions, the generation and
may represent an important energy source for patients in consumption of lactate are equivalent, which results in a
critical condition.9,11,12 Despite its complexity, hyperlac- stable concentration of lactate in the blood.17
tatemia interpretation has been simplified as representing
the presence of global tissue hypoxia/hypoperfusion with
Gluconeogenesis and oxidation as major
anaerobic glycolysis.10,13
mechanisms of lactate metabolism
Herein, we review the pathophysiological aspects and
recent clinical approaches for hyperlactatemia in critically ill Lactate is reconverted to pyruvate and metabolized in the
patients. liver, kidney, and other tissues through the Cori cycle, which
generates glucose and consumes adenosine triphosphate
(ATP) (gluconeogenesis).12 Lactate is also metabolized
LACTATE PRODUCTION AND REMOVAL
through the tricarboxylic acid cycle and oxidative phospho-
rylation in the liver, kidney, muscle, heart, brain, and other
Production and removal of lactate from
tissues, generating ATP when pyruvate is oxidized to carbon
blood
dioxide and water.
T HE DAILY LACTATE production in resting humans is
estimated as 20 mmol/kg,14 primarily from highly gly-
colytic tissues such as skeletal muscles.15 The reaction for
Half of lactate is metabolized through oxidation at rest,
and 75–80% during exercise.18 In contrast, lactate produc-
tion by muscle and other tissues is coupled with its conver-
generating or consuming lactate is shown below: sion to glucose (gluconeogenesis).19 Thus, lactate is an
Pyruvate + NADH + H+ ⇌ lactate + NAD+. important precursor of gluconeogenesis and a key source of
Pyruvate is generated largely by anaerobic glycolysis. glucose.20
The redox-coupled interconversion of pyruvate and lactate Under stress conditions, lactate has been suggested to act
occurs in the cytosol and is catalyzed by lactate dehydro- as a biofuel that eliminates blood glucose use and provides
genase. The blood lactate : pyruvate ratio is maintained at additional glucose.12 Therefore, hyperlactatemia may indi-
approximately 10:1; therefore, any condition that increases cate a protective response to stress under critical conditions.
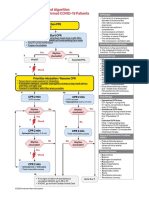
Fig. 1. Epinephrine-induced lactate production. Epinephrine increases cyclic AMP (cAMP) production through b2-adrenergic receptor
activation, glycogenolysis/glycolysis stimulation, and Na+/K+-ATPase pump activation, which converts adenosine triphosphate (ATP) to
adenosine diphosphate (ADP). ADP reactivates glycolysis and generates pyruvate through a cAMP-dependent mechanism. These
combined mechanisms result in lactate production. AMP, adenosine monophosphate; TCA, tricarboxylic acid cycle.
© 2016 Japanese Association for Acute Medicine
Acute Medicine & Surgery 2016; 3: 293–297 Lactate, a useful but unreliable marker in critical care 295
glycolysis from hypoperfusion. Continued resuscitation
ANOTHER PATHWAY OF LACTATE
attempts targeting lactate levels may thus lead to unnecessary
PRODUCTION AND HYPERLACTATEMIA
blood transfusion and use of inotropic agents.27 It was also
I N TISSUE HYPOXIA, lactate is overproduced and
underutilized because of impaired mitochondrial oxida-
tion,17 largely through anaerobic glycolysis.9,11 However,
suggested that resuscitation efforts to normalize lactate for
hyperlactatemia in the later phase of sepsis could be flawed
and potentially harmful.10 However, the data supporting the
hyperlactatemia can also result from aerobic glycolysis, clinical utility of lactate as a marker of early sepsis recovery
independent of tissue hypoxia.11 Under stress conditions, are robust. In a recently revised sepsis definition, serum lac-
aerobic glycolysis is an important mechanism for rapid ATP tate level >2 mmol/L (18 mg/dL) has been used as a marker
generation. In the hyperdynamic stage of sepsis, epinephr- of circulatory and cellular/metabolic abnormalities to define
ine-dependent stimulation of the b2-adrenoceptor augments septic shock, enough to substantially increase mortality.29 In
glycolytic flux both directly and through enhancement of critical illness-related stress conditions, elevated lactate level
sarcolemmal Na+/K+-ATPase.21 Other conditions associated is also an independent predictor of mortality.30,31
with elevated epinephrine levels, such as severe trauma and The 2008 Surviving Sepsis Campaign guidelines recom-
cardiogenic shock, can cause hyperlactatemia through this mended measurement of lactate at initial presentation, with
mechanism. In inflammatory states, aerobic glycolysis can an elevated value signifying tissue hypoperfusion and neces-
also be driven by cytokine-dependent stimulation of cellular sitating resuscitation.32 Although they suggested measuring
glucose uptake.22 lactate only at the time of presentation, serial evaluation,
During high-intensity exercise and shivering, hyperlac- including lactate clearance, may have greater value, as sug-
tatemia is frequently observed. However, oxygen saturation gested in the Surviving Sepsis Campaign guidelines 2012.2
of myoglobin was found to remain stable at high exercise Although presence of hyperlactatemia can be a marker of
intensity and correlate poorly with circulating lactate con- tissue hypoxia/hypoperfusion complicated with cellular/
centration.23 Several studies have shown significant correla- metabolic abnormalities,29 lactate clearance has been sug-
tion between plasma lactate concentrations and epinephrine gested as a parameter to evaluate the effectiveness of resus-
levels.23,24 Based on these findings, hyperlactatemia during citation. The clinical relevance of lactate and its clearance
exercise may reflect increased aerobic glycolysis stimulated have been repetitively evaluated. Lactate clearance greater
by epinephrine rather than anaerobic glycolysis due to tissue than 10% from the initial value is predictive of survival from
hypoxia. septic shock, and targeting 10% clearance provided similar
The role of Na+/K+-ATPase pump stimulation was evalu- survival rates to targeting central venous oxygen satura-
ated in skeletal muscle of patients with septic shock and tion.33,34 In patients with sepsis, lactate clearance greater
shown to be a leading source of lactate formation through than 20% during the initial 8 h showed a 22% decline in
aerobic glycolysis.25 Recently, long-term b-blocker therapy mortality risk relative to clearances less than 20%.5 Further-
was shown to decrease the blood lactate concentration of more, early lactate normalization was a survival predictor in
patients with severe sepsis at presentation.26 The use of patients with severe sepsis.35 A meta-analysis of randomized
blood lactate measurement as a triage tool in the initial controlled trials evaluating the effect of early lactate clear-
assessment of septic patients undergoing b-blocker therapy ance-guided therapy in patients with sepsis36 showed that
may therefore underestimate the severity of the condition. lactate clearance-guided therapy was associated with reduc-
Although other mechanisms have been suggested,9 aero- tion in mortality. In another meta-analysis, Zhang et al.37
bic glycolysis and tissue hypoxia appear to be the key fac- found that the pooled relative risk for all-cause mortality in
tors in hyperlactatemia. Notably, the two are not mutually critically ill patients was 0.38 (95% confidence interval [CI],
exclusive and can simultaneously contribute to hyperlac- 0.29–0.50). They concluded that lactate clearance was pre-
tatemia (Fig. 1). dictive of a lower mortality rate.
The clinical significance of lactate monitoring was also
evaluated. Jansen and colleagues prospectively assessed the
LACTATE AND ITS CLEARANCE ARE USEFUL
effect of lactate monitoring and resuscitation directed at
PROGNOSTIC MARKERS
decreasing lactate levels in intensive care unit (ICU)
patients admitted with lactate levels ≥ 3.0 mEq/L.5 Treat-
T HE MECHANISM OF hyperlactatemia in critical ill-
ness is multifactorial and associated with factors beyond
tissue hypoxia/hypoperfusion.27,28 Lactic acidosis refractory
ment was targeted at decreasing lactate levels by ≥ 20%
every 2 h for the initial 8 h. Hospital mortality was lower
to standard resuscitation is frequently caused by increased and organ failures improved significantly with lactate
aerobic glycolysis in skeletal muscle instead of anaerobic monitoring.
© 2016 Japanese Association for Acute Medicine
296 S. Kushimoto et al. Acute Medicine & Surgery 2016; 3: 293–297
aerobic glycolysis unrelated to tissue dysoxia is unlikely to
PATIENTS WITH SEVERE HYPERLACTATEMIA
respond to increases in systemic oxygen delivery.
MAY COMPRISE A HETEROGENEOUS
Because hyperlactatemia can be simultaneously related to,
POPULATION
and unrelated to, tissue hypoxia, physicians should recog-
I N CRITICALLY ILL patients, severe hyperlactatemia is
not a rare condition. Recently, Haas and colleagues retro-
spectively analyzed patients with plasma lactate levels
nize that resuscitation to normalize plasma lactate levels
could be over-resuscitation and worsen the physiological
status. Thus, lactate is a reliable indicator of sepsis severity
≥10 mmol/L.38 Although the overall mortality among ICU and a marker of resuscitation, but is not a reliable marker of
patients was 9.8%, that of patients with severe hyperlac- tissue hypoxia/hypoperfusion.
tatemia was 78.2%. Thus, hyperlactatemia was associated
with death in the ICU (odds ratio, 1.35 [95% CI, 1.23–1.49;
CONFLICT OF INTEREST
P < 0.001]). The main etiology for severe hyperlactatemia
was sepsis (34.0%), cardiogenic shock (19.3%), and car-
diopulmonary resuscitation (13.8%). Patients developing
severe hyperlactatemia after >24 h of ICU treatment had
N ONE.
ACKNOWLEDGEMENTS
significantly higher mortality (89.1%) than patients devel-
oping severe hyperlactatemia within 24 h of ICU admit-
tance (69.9%, P < 0.0001). Lactate clearance after 12 h
showed a receiver–operating characteristic area under the
T HIS STUDY WAS supported by the fund of Tohoku
Kyuikai and departmental fund of the Division of
Emergency and Critical Care Medicine, Tohoku University
curve value of 0.91 for predicting ICU mortality (cut-off Graduate School of Medicine.
yielding highest sensitivity and specificity, 12-h lactate
clearance of 32.8%). In patients with 12-h lactate clear-
ance <32.8%, ICU mortality was 96.6%. Severe hyperlac-
REFERENCES
tatemia is thus associated with extremely high ICU
mortality, especially when there is no marked lactate clear- 1 ATLS Subcommittee; American College of Surgeons’ Com-
ance within 12 h. mittee on Trauma; International ATLS working group.
However, patients with severe hyperlactatemia may com- Advanced trauma life support (ATLSâ): the ninth edition. J.
prise heterogeneous etiologies. Intensive care unit mortal- Trauma Acute. Care Surg. 2013;74:1363–6.
ity, peak lactate concentration, and 12-h clearance were 2 Dellinger RP, Levy MM, Rhodes A et al. Surviving Sepsis
evaluated in etiological subgroups. The respective ICU Campaign: international guidelines for management of severe
mortality and 12-h lactate clearance (95% CI) for each sepsis and septic shock, 2012. Intensive Care Med. 2013; 39:
subgroup are as follows: sepsis, 90.4% and 3.3% ( 29.7 165–228.
to 34.9%); cardiogenic shock, 0.5% and 2.7% ( 28.9 to 3 Jones AE, Brown MD, Trzeciak S et al. The effect of a quan-
titative resuscitation strategy on mortality in patients with
39.6%); postoperative cardiosurgical patients, 3.8% and
sepsis: a meta-analysis. Crit. Care Med. 2008; 36: 2734–9.
73.8% (45.4 to 81.3%); cardiopulmonary resuscitation,
4 Tisherman SA, Barie P, Bokhari F et al. Clinical practice
8.2% and 4.1% ( 13.0 to 64.8%); hemorrhagic shock,
guideline: endpoints of resuscitation. J. Trauma 2004; 57:
70.0% and 25.8% ( 6.3 to 74.9%); liver failure, 84.6%
898–912.
and 1.5% ( 21.9 to 26.2%); mesenteric ischemia, 100.0% 5 Jansen TC, van Bommel J, Schoonderbeek FJ et al. Early lac-
and 18.9% ( 54.8 to 21.8%); and seizure, 0% and tate-guided therapy in intensive care unit patients: a multicen-
89.7% (81.3 to 91.7%). ter, open-label, randomized controlled trial. Am. J. Respir.
Although severe hyperlactatemia in critically ill patients Crit. Care Med. 2010; 182: 752–61.
is strongly associated with high ICU mortality, the etiology 6 Cerovic O, Golubovic V, Spec-Marn A, Kremzar B, Vidmar
and clearance rates show heterogeneity. G. Relationship between injury severity and lactate levels in
severely injured patients. Intensive Care Med. 2003; 29:
1300–5.
CONCLUSIONS
7 Nichol A, Bailey M, Egi M et al. Dynamic lactate indices as
H YPERLACTATEMIA IN CRITICALLY ill patients
must be considered to be related to tissue hypoxia/hy-
poperfusion. Therefore, appropriate hemodynamic resuscita-
predictors of outcome in critically ill patients. Crit. Care
2011; 15: R242.
8 Wong HR, Lindsell CJ, Pettila V et al. A multibiomarker-
tion is required to correct the pathological condition based outcome risk stratification model for adult septic shock.
immediately. However, hyperlactatemia resulting from Crit. Care Med. 2014; 42: 781–9.
© 2016 Japanese Association for Acute Medicine
Acute Medicine & Surgery 2016; 3: 293–297 Lactate, a useful but unreliable marker in critical care 297
9 Garcia-Alvarez M, Marik P, Bellomo R. Sepsis-associated 26 Contenti J, Occelli C, Corraze H, Lemoel F, Levraut J. Long-
hyperlactatemia. Crit. Care 2014; 18: 503. Term beta-Blocker Therapy Decreases Blood Lactate Con-
10 Garcia-Alvarez M, Marik P, Bellomo R. Stress hyperlac- centration in Severely Septic Patients. Crit. Care Med. 2015;
tataemia: present understanding and controversy. Lancet Dia- 43: 2616–22.
betes Endocrinol. 2014; 2: 339–47. 27 James JH, Luchette FA, McCarter FD, Fischer JE. Lactate is
11 Kraut JA, Madias NE. Lactic acidosis. N. Engl. J. Med. 2014; an unreliable indicator of tissue hypoxia in injury or sepsis.
371: 2309–19. Lancet 1999; 354: 505–8.
12 Miller BF, Fattor JA, Jacobs KA et al. Lactate and glucose 28 Levraut J, Ciebiera JP, Chave S et al. Mild hyperlactatemia
interactions during rest and exercise in men: effect of exoge- in stable septic patients is due to impaired lactate clearance
nous lactate infusion. J. Physiol. 2002; 544: 963–75. rather than overproduction. Am. J. Respir. Crit. Care Med.
13 Mizock BA, Falk JL. Lactic acidosis in critical illness. Crit. 1998; 157: 1021–6.
Care Med. 1992; 20: 80–93. 29 Singer M, Deutschman CS, Seymour CW et al. The Third
14 Connor H, Woods HF. Quantitative aspects of L(+)-lactate International Consensus Definitions for Sepsis and Septic
metabolism in human beings. Ciba Found. Symp. 1982; 87: Shock (Sepsis-3). JAMA 2016; 315: 801–10.
214–34. 30 Mikkelsen ME, Miltiades AN, Gaieski DF et al. Serum lac-
15 Doherty JR, Cleveland JL. Targeting lactate metabolism for tate is associated with mortality in severe sepsis independent
cancer therapeutics. J. Clin. Invest. 2013; 123: 3685–92. of organ failure and shock. Crit. Care Med. 2009; 37: 1670–
16 Jeppesen JB, Mortensen C, Bendtsen F, Moller S. Lactate 7.
metabolism in chronic liver disease. Scand J Clin Lab Invest. 31 Nichol AD, Egi M, Pettila V et al. Relative hyperlactatemia
2013; 73: 293–9. and hospital mortality in critically ill patients: a retrospective
17 Madias NE. Lactic acidosis. Kidney Int. 1986; 29: 752–74. multi-centre study. Crit. Care 2010; 14: R25.
18 Mazzeo RS, Brooks GA, Schoeller DA, Budinger TF. Dis- 32 Dellinger RP, Levy MM, Carlet JM et al. Surviving Sepsis
posal of blood [1-13C]lactate in humans during rest and exer- Campaign: international guidelines for management of severe
cise. J. Appl. Physiol. 1985; 1986(60): 232–41. sepsis and septic shock: 2008. Crit. Care Med. 2008; 36:
19 Consoli A, Nurjhan N, Reilly JJ Jr, Bier DM, Gerich JE. Con- 296–327.
tribution of liver and skeletal muscle to alanine and lactate 33 Jones AE, Shapiro NI, Trzeciak S et al. Lactate clearance
metabolism in humans. Am. J. Physiol. 1990; 259: E677–84. vs central venous oxygen saturation as goals of early sepsis
20 Kreisberg RA, Pennington LF, Boshell BR. Lactate turnover therapy: a randomized clinical trial. JAMA 2010; 303: 739–
and gluconeogenesis in normal and obese humans. Effect of 46.
starvation. Diabetes 1970; 19: 53–63. 34 Nguyen HB, Rivers EP, Knoblich BP et al. Early lactate
21 Levy B, Desebbe O, Montemont C, Gibot S. Increased aero- clearance is associated with improved outcome in severe sep-
bic glycolysis through beta2 stimulation is a common mecha- sis and septic shock. Crit. Care Med. 2004; 32: 1637–42.
nism involved in lactate formation during shock states. Shock 35 Puskarich MA, Trzeciak S, Shapiro NI et al. Whole blood
2008; 30: 417–21. lactate kinetics in patients undergoing quantitative resuscita-
22 Taylor DJ, Faragher EB, Evanson JM. Inflammatory cytoki- tion for severe sepsis and septic shock. Chest 2013; 143:
nes stimulate glucose uptake and glycolysis but reduce glu- 1548–53.
cose oxidation in human dermal fibroblasts in vitro. Circ. 36 Gu WJ, Zhang Z, Bakker J. Early lactate clearance-guided
Shock 1992; 37: 105–10. therapy in patients with sepsis: a meta-analysis with trial
23 Richardson RS, Noyszewski EA, Leigh JS, Wagner PD. Lac- sequential analysis of randomized controlled trials. Intensive
tate efflux from exercising human skeletal muscle: role of Care Med. 2015; 41: 1862–3.
intracellular PO2. J. Appl. Physiol. 1985; 1998(85): 627–34. 37 Zhang Z, Xu X. Lactate clearance is a useful biomarker for
24 Hughson RL, Green HJ, Sharratt MT. Gas exchange, blood the prediction of all-cause mortality in critically ill patients: a
lactate, and plasma catecholamines during incremental exer- systematic review and meta-analysis. Crit. Care Med. 2014;
cise in hypoxia and normoxia. J. Appl. Physiol. 1985; 1995 42: 2118–25.
(79): 1134–41. 38 Haas SA, Lange T, Saugel B et al. Severe hyperlactatemia,
25 Levy B, Gibot S, Franck P, Cravoisy A, Bollaert PE. Relation lactate clearance and mortality in unselected critically ill
between muscle Na+K+ ATPase activity and raised lactate patients. Intensive Care Med. 2016; 42: 202–10.
concentrations in septic shock: a prospective study. Lancet
2005; 365: 871–5.
© 2016 Japanese Association for Acute Medicine
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Airway Management Complications in Children With Difficult Tracheal Intubation From The Pediatric Difficult Intubation PeDI Registry A Prospective Cohort AnalysisDokument10 SeitenAirway Management Complications in Children With Difficult Tracheal Intubation From The Pediatric Difficult Intubation PeDI Registry A Prospective Cohort AnalysisNisa UcilNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Perinatology Journal Reading by AhimsaDokument31 SeitenPerinatology Journal Reading by AhimsaNisa UcilNoch keine Bewertungen
- HSR - USCOM FinalDokument49 SeitenHSR - USCOM FinalNisa UcilNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Bundle 6hour Step2a CVPDokument6 SeitenBundle 6hour Step2a CVPIbrahim DharmawanNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- NeurologicDokument7 SeitenNeurologicFarrah ErmanNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Abstrak Anu Lampung Revisi FinalDokument1 SeiteAbstrak Anu Lampung Revisi FinalNisa UcilNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Infantile Pityriasis Alba and Comorbid DisordersDokument5 SeitenInfantile Pityriasis Alba and Comorbid DisordersNisa UcilNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Algo Pals Pediatric BradycardiaDokument1 SeiteAlgo Pals Pediatric BradycardiaNisa UcilNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Algo Pals BLS Pediatric Cardiac ArrestDokument1 SeiteAlgo Pals BLS Pediatric Cardiac ArrestSiti NabilaNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- AlgorithmPALS CACOVID 200406 PDFDokument1 SeiteAlgorithmPALS CACOVID 200406 PDFEka RahmanizarNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Resep Baking Class 13.12.2020Dokument4 SeitenResep Baking Class 13.12.2020Nisa UcilNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Isk AafpDokument7 SeitenIsk Aafpbebekdd22Noch keine Bewertungen
- Airway Management Complications in Children With Difficult Tracheal Intubation From The Pediatric Difficult Intubation PeDI Registry A Prospective Cohort AnalysisDokument10 SeitenAirway Management Complications in Children With Difficult Tracheal Intubation From The Pediatric Difficult Intubation PeDI Registry A Prospective Cohort AnalysisNisa UcilNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Exercise During Pregnancy A Practical ApproachDokument7 SeitenExercise During Pregnancy A Practical ApproachNisa UcilNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Early Identification of Autism by The CHecklist For Autism in Toddlers CHATDokument44 SeitenEarly Identification of Autism by The CHecklist For Autism in Toddlers CHATNisa UcilNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Prevalence of Interatrial Septal Openings in Newborns and Predictive Factors For Spontaneous ClosureDokument5 SeitenThe Prevalence of Interatrial Septal Openings in Newborns and Predictive Factors For Spontaneous ClosureNisa UcilNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Exercise During Pregnancy A Practical ApproachDokument7 SeitenExercise During Pregnancy A Practical ApproachNisa UcilNoch keine Bewertungen
- Adverson, J. 2013. Feeding Children With CP Swallowing Difficulties PDFDokument4 SeitenAdverson, J. 2013. Feeding Children With CP Swallowing Difficulties PDFNicoleOrtegaAguileraNoch keine Bewertungen
- Faktor Risiko Ibu Dan Bayi Terhadap Kejadian Asfiksia Neonatorum Di Bali Penelitian Case Control PDFDokument6 SeitenFaktor Risiko Ibu Dan Bayi Terhadap Kejadian Asfiksia Neonatorum Di Bali Penelitian Case Control PDFNisa UcilNoch keine Bewertungen
- Nihms 701642Dokument10 SeitenNihms 701642Nisa UcilNoch keine Bewertungen
- Karagol 2010Dokument4 SeitenKaragol 2010Nisa UcilNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Weight-For-Length GIRLS: Birth To 2 Years (Z-Scores)Dokument1 SeiteWeight-For-Length GIRLS: Birth To 2 Years (Z-Scores)Malisa LukmanNoch keine Bewertungen
- Isk AafpDokument7 SeitenIsk Aafpbebekdd22Noch keine Bewertungen
- Algo Pals Pediatric Cardiac ArrestDokument1 SeiteAlgo Pals Pediatric Cardiac ArrestDevi ChrestellaNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- 66b3 PDFDokument6 Seiten66b3 PDFNisa UcilNoch keine Bewertungen
- Cerebrospinal Fluid Lactate and PyruvateDokument8 SeitenCerebrospinal Fluid Lactate and PyruvateNisa UcilNoch keine Bewertungen
- Review Article: Autoimmune/Inflammatory Arthritis Associated Lymphomas: Who Is at Risk?Dokument12 SeitenReview Article: Autoimmune/Inflammatory Arthritis Associated Lymphomas: Who Is at Risk?Nisa UcilNoch keine Bewertungen
- PCH 32 s1 039 PDFDokument4 SeitenPCH 32 s1 039 PDF79lalalaNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- Correlation of Procalcitonin Level With NLR in Patient With SIRSDokument1 SeiteCorrelation of Procalcitonin Level With NLR in Patient With SIRSNisa UcilNoch keine Bewertungen
- Validity and ReliabilityDokument6 SeitenValidity and ReliabilityfarlynzNoch keine Bewertungen
- Safety Guidelines and Procedures in The Operating RoomDokument19 SeitenSafety Guidelines and Procedures in The Operating RoomCyndy Lopez100% (7)
- Moringa Oleifera - Cancer, Lupus, Arthritis, Gout, Diabetes PDFDokument5 SeitenMoringa Oleifera - Cancer, Lupus, Arthritis, Gout, Diabetes PDFzultrsb689100% (1)
- IOL's and TASSDokument2 SeitenIOL's and TASSOscar Padilla NavarroNoch keine Bewertungen
- Intraoperative CareDokument3 SeitenIntraoperative CareMargi PatelNoch keine Bewertungen
- Sulbutiamine ComprehensiveDokument5 SeitenSulbutiamine ComprehensiveŚС٣ΩTЏМЦṢ TξSTΪСḸЄჴNoch keine Bewertungen
- Nagor Product Catalogue 2013Dokument23 SeitenNagor Product Catalogue 2013Hossam ElkafrawiNoch keine Bewertungen
- Sample Discharge SummaryDokument4 SeitenSample Discharge SummaryPatient Safety My100% (2)
- Duties and Responsibilities of The Nursing PersonnelDokument54 SeitenDuties and Responsibilities of The Nursing PersonnelMercyNoch keine Bewertungen
- Compartment SyndromeDokument24 SeitenCompartment SyndromeDexter BluesNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Patient Positioning in Operating TheatreDokument52 SeitenPatient Positioning in Operating TheatreFatkhul AdhiatmadjaNoch keine Bewertungen
- CAseDokument3 SeitenCAseabdihakemNoch keine Bewertungen
- Congenital Cystic Adenomatoid Malformation (CCAM)Dokument7 SeitenCongenital Cystic Adenomatoid Malformation (CCAM)sarguss14Noch keine Bewertungen
- ANSYS Fluent - CFD Software PDFDokument3 SeitenANSYS Fluent - CFD Software PDFSafi AhmedNoch keine Bewertungen
- General Hospital Prog.Dokument6 SeitenGeneral Hospital Prog.AlamiN RayMan ArNobNoch keine Bewertungen
- Reflection On Nursing FundamentalsDokument7 SeitenReflection On Nursing FundamentalsFred Ashira AuraNoch keine Bewertungen
- Higher Cortical FunctionDokument4 SeitenHigher Cortical FunctionSiti Fairuz NadyaNoch keine Bewertungen
- Neonatal JaundiceDokument12 SeitenNeonatal JaundiceGiska T PutriNoch keine Bewertungen
- Hepatic EncephalopatyDokument15 SeitenHepatic EncephalopatyJariza Daryl Tamang MejiaNoch keine Bewertungen
- Foot Orthotics Claiming Checklist BLUE CROSSDokument1 SeiteFoot Orthotics Claiming Checklist BLUE CROSSBradley ChristmasNoch keine Bewertungen
- RE6210 66b2ef9052fullabstract PDFDokument110 SeitenRE6210 66b2ef9052fullabstract PDFmariamonaNoch keine Bewertungen
- Basic (Level IV) Trauma Facility CriteriaDokument6 SeitenBasic (Level IV) Trauma Facility CriteriaPiet Pogen PoelNoch keine Bewertungen
- To Explain What Is Meant by "Playing God" in This Case.)Dokument3 SeitenTo Explain What Is Meant by "Playing God" in This Case.)Hieu NguyenNoch keine Bewertungen
- 113(英文版English)List of Standard Medical Consumables普通医用耗材表Dokument34 Seiten113(英文版English)List of Standard Medical Consumables普通医用耗材表Peccamb SurgicalNoch keine Bewertungen
- Conditions For Work Effectiveness Questionnaire Iandii: User ManualDokument13 SeitenConditions For Work Effectiveness Questionnaire Iandii: User ManualGersonMercadoRamirez100% (1)
- Cellulitis NCPDokument2 SeitenCellulitis NCPKelly Riedinger85% (13)
- Nursing Care of The Patient With Neurological DisordersDokument89 SeitenNursing Care of The Patient With Neurological DisordersShara Mae More BarriosNoch keine Bewertungen
- Cataract Discharge PlanDokument2 SeitenCataract Discharge PlanLeah GordoncilloNoch keine Bewertungen
- Holistic Nursing A Way of BeingDokument6 SeitenHolistic Nursing A Way of Beingashley larsonNoch keine Bewertungen
- Check List For AmbulanceDokument2 SeitenCheck List For AmbulanceEka B100% (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBewertung: 2 von 5 Sternen2/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisVon EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (42)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (24)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 4 von 5 Sternen4/5 (3)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 5 von 5 Sternen5/5 (80)