Beruflich Dokumente
Kultur Dokumente
Moran Jslpa 1989
Hochgeladen von
mitaCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Moran Jslpa 1989
Hochgeladen von
mitaCopyright:
Verfügbare Formate
Brainstem Electric Response Audiometry (BERA)in the Evaluation of
Hearing Loss in Infants with Cleft Palate
Linda M. Moran
Andree Durieux-Smith
Kathy Malizia
Children's Hospital of Eastern Ontario
It has been estimated that one child in 500 to 750 live births is (1980), and Feagans, Blood, and Tubman (1988). These re-
born with a cleft palate (Rood & Stool, 1981). A high incidence views have shown that, although there is a great deal of data
of middle ear pathology is known to be associated with this which suggests the detrimental effects of early hearing loss or
problem (Bluestone, 1971). It is generally accepted that this otitis media, many of the studies have been flawed by poor
population suffers from Eustachian tube dysfunction which validity. Nevertheless, it is difficult for the professional to
leads in turn to the development of middle ear effusions and ignore the possibility of a link between the deficits in speech
conductive hearing loss. The various underlying causes that and language development which the cleft palate child is know
have been postulated are related either to an anatomic malfor- to exhibit (Bzoch, 1965; Mustain, 1979; Pannbacker, 1971)
mation of the palate and tube or a functional deficiency of their and the auditory status in infancy.
musculature (Bluestone, 1971; Rood & Stool, 1981).
The purpose of this study was to review the results of
Bluestone (1971) reviewed the literature and found esti- testing of a group of infants who presented in our clinic with
mates ranging from 40% to 80% of cleft palate adults and cleft palate and to document the auditory brainstem response
children with abnormal middle ears. Paradise, Bluestone, and (ABR) thresholds of these patients. This would allow us to
Felder (1969) and Stool and Randall (1968) used otoscopy and evaluate the need for routine audiological follow-up.
tympanometry, and both groups found evidence of middle ear
effusions in virtually all of the cleft palate infants they exam-
ined. Gerber and Mencher (1978) recommended that infants Method
with cleft palate be placed at risk for middle ear effusions with Children who are born with a cleft palate in the Ottawa area
an estimated incidence of 70-100% of cases. are systematically referred to the Children's Hospital of East-
ern Ontario and followed by a multidisciplinary team that
Bluestone's review of the literature also examined the includes ENT, plastic surgery, dentistry, nursing, social work,
prevalence of hearing loss associated with this problem in speech-language pathology and audiology. They undergo
older children or adult patients. The estimates ranged from 0 BERA initially at three months of age as part of a larger
to 90 %, and B luestone concluded that one should expect some screening program at this centre, which has been described by
degree of hearing loss in at least 50% of cases. Durieux-Smith, Picton, Edwards, MacMurray, and Goodman
(1987). For this study, we reviewed the charts and results of
The use of Brainstem Electric Response Audiometry BERA for all children with cleft palate referred between
(BERA) now allows us to investigate the auditory function of January, 1984 and December, 1987.
infants with cleft palate. Gould (1980) found that 8 of 10
infants with cleft palate showed evidence of peripheral hearing Each baby was tested in a sound attenuated chamber while
loss through the use of evoked potentia!s. More recently sleeping naturally or very quietly awake. Disc electrodes were
HeIias, Chobaut, Mourot, and Lafon (1988) published results attached to the forehead at the midline and to the mastoids.
showing that 19 of 23 patients, or 83%, had electrophysiologic Figure I lists some aspects of the test protocol. Interelectrode
responses consistent with conductive hearing loss when tested impedance was maintained at 5K ohms or less. Activity be-
before palate repair and before 12 months of age. tween the forehead and mastoid ipsilateral to stimulation was
amplified, filtered between 25 and 3000 Hz, and averaged over
The implications of such early auditory deprivation for a time base of 15 msec.
language learning have been debated at length in the literature.
Reviews of the various aspects of this complicated question One hundred Ilsec rarefaction clicks were presented mon-
have been done by Ventry (1980), Menyuk (1986), Brooks aurally through a TDH-49 earphone mounted in a MX41/AR
JSLPAIROA (HCC) Vol. 13. No. 3. September 1989 43
BERA
Figure 1. Details of the test protocol (Edwards & Durieux- a rate of It/second. and replicate averages of 2000 responses
Smith, 1985). were recorded in order to assess Wave I and the Wave I-V
interval. A complete set of results could not be obtained in all
Recording electrodes cases because some of the babies awoke during testing. Figure
2 shows typical ABR recordings obtained with this population.
I nterelectrode
Impedance <5 k n
Average sweep 15 ms Those children with elevated thresholds on the initial
Filters 25-3000 Hz BERA returned for a retest and repeat otoscopic examination
Click nHL 40 dB peak SPL three months later. If an elevated threshold persisted at this first
Click Polarity rarefaction and subsequent visits. myringotomy and tube insertion were
Replications 1 recommended by the otolaryngologist.
I ntensity and
For some of the children, results of behavioural
Presentation Rate 30 dB nHL at 61/ sec audiometry were available. Attempts at visual reinforcement
(increase in 10 dB or conditioned orienting response audiometry were usually
steps if no response) started when the child was at least twelve months of age.
70 dB nHL at 11/sec Generally, results of conditioned play audiometry under ear-
Sum 4000 at 61/sec phones were not reported for children under thirty months.
2000 at 11/sec Tympanometry was carried out only after six months of age.
Paradise. Smith. and Bluestone (1976) and Schwartz and
Sch wartz (1978) reported poor reliability for this measure with
younger infants. Otomicroscopy was used by the otolaryn-
cushion. The clicks were presented initially at 30 dBnHL at a gologist on the team for the first evaluation at three months of
presentation rate of 6t/second, and two replicate averages of age and at all later test sessions. It should be noted that due to
4000 responses each were obtained. A response at 30 dBnHL the retrospective nature of this work, a strict protocol was not
was considered to demonstrate normal peripheral auditory followed in all cases.
sensitivity. If no response was recorded at 30 dBnHL. the
intensity was increased in 10 dB steps up to a maximum of 95
dBnHL until threshold was reached. Clicks also were Results
presented at 70 dBnHL (or higher in cases of hearing loss) at Fifty children, including 25 male and 25 female patients, with
cleft palate or cleft lip and palate were tested with BERA. For
Figure 2. Examples of a normal ABR tracing, a conductive hearing loss ABR, and
a sensorineural loss ABR in infant patients. (Picton & Durieux-Smith, 1988).
Posltivlty at the vertex is indicated by a downward deflection.
NORMAL CONDUCTIVE SENSORINEURAL
70dB Ills
~ ~ ~
60dB 61/5 ~ ~
.
SOdB .v~
40 dB
~ .
---=----
30dB ~
---- rlo)JV
ISms
44 JSLPAIROA (HCC) Vol. 13. No. 3. Sep/emher 1989
Moran, Durieux-Smlth & Malizla
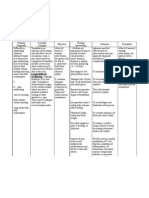
Figure 3. Flow chart of the test protocol and results.
8ERA #1
~"'---
normal,. "=50 --... abnormal
n=11 n=39
(22%) (78% )
I
SERA #2, #3
leave study ~
~
~
,
normal abnormal
n=O n=29
(7 cases still to be assessed
3 cases direct to tubes)
myringotomy and tubes
n=21
,t
post-tubes SERA
n=19
abnormal
n=8
to be assessed
n=2
/ '\
,
normal
otoscopy
n=6
amplification,
aural habilitation
abnormal
otoscopy
n=2
~
medical
treatment
and audiological and
follow-up follow-up
some of the children, infonmation was available on two, three, Six cases without otorrhea failed to resolve for the first
and as many as four tests. A total of 109 tests were examined. BERA following tube insertion. Three of these six cases have
since been found to be sensorineural in nature on the basis of
Figure 3 shows that of the 50 babies tested, 39 (78%) were air and bone conduction audiometry and impedance audiom-
found initially to have ABR thresholds of greater than 30 etry. One of these is a unilateral hearing loss. The other two
dBnHL in at least one ear, Of these, 35 showed a bilateral are bilateral and have been fitted with hearing aids and have
elevation in threshold. Of the 39 babies with abnonmal results, entered into a program of aural habilitation.
29 went on to be retested, 3 underwent myringotomy and tubes
without further verification, and 7 have yet be re-assessed. Three other children who were found to have a persistent
hearing loss following tube insertion were fitted with aids and
Twenty-one children underwent tube insertion after a began therapy. Behavioural evaluations showed that these
second or third BERA evaluation, Of these, only 11 were found children eventually resolved to nonmal hearing some months
to have a nonmal threshold within two months post-opera- later. In two of the cases, improvement was noted only after
tively. Two cases were found to have otorrhea, and further the palate repair. The time taken before nonmal hearing was
medical management was required. Two cases have yet to be documented in these children was seven to eleven months.
assessed. No child who began with an elevated threshold
resolved to nonmal levels spontaneously or before medical Previous research in our department had indicated that
intervention at least during the first year of life. One child BERA testing was best carried out at three months corrected
eventually showed nonmal ABR thresholds, but only at fifteen age (Durieux-Smith et al., 1987). We questioned whether this
months of age. recommended age also was the ideal for the cleft palate chil-
,1SLPAiROA (HCc) {lot. 13, No. 3, September 1989 45
Figure 4. Difference in percentages of normal ears when Figure 5. Comparison of mean thresholds for children
testing took place at less than three months of age or later. tested at various ages.
<3 months ~months Mean Threshold
at BERA #1 at BERA #1 Age at test N=ears
(dB nHL)
normal =3 months 49.79
30.3% 26.7%
ears 48
=6 months 46.67
abnormal
69.7% 73.3%
ears
=6 months 50.00
X2 is not significant 7
=9 months 42.87
No significant difference when test results for each child
dren. An earlier review of a subset of this group done by compared at different ages
Tropper, Moran, OdeIl, and Durieux-Smith (1988) indicated
that the percentage of normal ABR thresholds obtained when
the children were less than four months of age was higher than
for the group who were tested at a later age. Our concern was We might have expected an even higher failure rate given
that children who passed the electrophysiologic screening at the reports of almost universal occurrence of middle ear effu-
three months of age might later develop a significant hearing sions in infants with cleft palate (Paradise et aI., 1969; Stool
loss which would go undetected. & Randall. 1968). It should be noted that the click stimulus
that was used in this study best correlates with audiometric
It was found through examination of the results of the thresholds at 2000 Hz and 4000 Hz (Coats & Martin, 1977;
larger group of children that this concern was not warranted. Gorga, Worthington, Reiland, Beauchaine, & Goldgar. 1985).
Figure 4 shows the percentage of ears of children who passed The children in whom the middle ear pathology had caused
or failed at the criterion level of 30 dBnHL. The proportion of only a low frequency hearing loss would not have been de-
ears with normal thresholds when tested at less than three tected. The results, therefore. may represent an underestimate
of auditory dysfunction for this popUlation.
months was 30.3%. The proportion of ears with normal thresh-
olds tested at a later age was 26.7%. The difference in these
two groups did not reach statistical significance at the 0.05 The incidence of bilateral sensorineural hearing loss was
level (X 2 0.017). 2 out of 50 or 4%. This yield is slightly higher than that found
through the screening of all NICU graduates at our centre,
Figure 5 shows the mean thresholds for two separate where 1.5% had a significant loss (Durieux-Smith et aI., 1987).
groups, those whose members had been tested twice, once at It has been suggested that the use of a risk factor is justifiable
three months and again at six, and those whose members had when it increases the detectability of a condition by at least ten
had tests at six and nine months of age. With this second times that found in the general population. (Joint Committee
method of analysis, no significant difference was found be- on Infant Hearing, 1982; Richards & Roberts, 1967). Our
tween the results for the younger and older age group in either results indicate that the presence of cleft palate meets this
case (3,6 months: F=1.31. df=47,1; 6,9 months: F=O.91, requirement given an incidence of congenital hearing loss in
df=6, I). We were not able to compare results for children the general population of one in 750 (Feinmesser & Tell
1982). '
across several ages as so few of the patients had been tested
more than twice.
In addition, a much greater proportion of the children were
affected bilaterally than unilaterally. The reSUlting auditory
Discussion deprivation raises concerns about the potential for delay in
The review of these cases has highlighted several points. First, speech and language development and underlines the need for
78% ofthe 50 children with cleft palate who were tested before early assessment and vigilant follow-up.
medical intervention showed an abnormal threshold. This
figure is consistent with estimates of middle ear pathology and Tube insertion did result in improvement in threshold in
hearing loss in older cleft palate patients (Bluestone, 1971). the majority of cases. However, we noted three children in
The rate of detection of elevated response remained high whom there was an unexpected lag between treatment and the
whether the children were tested at three months of age or at a time when hearing was documented to be within normal limits.
later time during the first year of life. The reason for this delay is not evident. The tympanostomy
46 JSLPAIROA (HCC) Vol. 13, No. 3, September 1989
Moran, Durieux-Smith & Malizia
tubes seemed insufficient to clear the middle ear effusions in Feinmesser. M., Tell, L., & Levi, H. (1982). Follow-up of 40,000
these cases. The restoration of normal middle ear function may infants screened for hearing defect. Audiology, 21, 197.
be seen only after more normal Eustachian tube function is Gerber, S .E., & Mencher G.T. (Eds). (1978). Early Diagnosis of
achieved through cleft palate repair. The clinical audiologist Hearing Loss. New York: Grune and Stratton.
must be aware of the possibility of delayed improvement in
Gorga, M.P., Worthington, D.W., Reiland. J.K., Beauchaine. K.A .•
threshold in this population and plan counselling and manage- & Goldgar, D.E. (1985). Some comparisons between auditory brain
ment strategies accordingly. stem response thresholds, latencies and the pure-tone audiogram. Ear
and Hearing, 6,105-112.
Summary Gould, HJ. (1980). Early auditory evoked potentials in infants with
craniofacial malformations. Journal Auditory Research. 20, 244-248.
The results of this study should alert the audiologist to the high
Helias, J., Chobaut, I.c', Mourot. M., & Lafon, lc' (1988). Early
incidence of elevated ABR thresholds in infants with cleft detection of hearing loss in children with cleft palate by brainstem
palate. This high incidence of auditory dysfunction was noted auditory response. Archives of Otolaryngology, Head and Neck Sur-
when the children were tested at three months of age or at some gery.114,154-156.
time later, but still before their palate repair. Given the fluctu-
Joint Committee on Infant Hearing Position Statement (1982). ASHA,
ating or recurrent nature of middle ear effusions we feel that
24,1017-1018.
structured audiological follow-up and careful parent education
are recommended in order to ensure prompt management of Menyuk, P. (1986). Predicting speech and language problems with
hearing loss throughout the first years oflife in this population. persistant otitis media. In IF. Kavanagh (Ed.), Otitis Media and Child
Development (pp. 83-96). Parkton, Maryland: York Press.
Mustain, W. (1979). Linguistic and educational implications of recur-
Address all correspondence to: rent otitis media. Ear Nose alld Throat Journal. 58, 62-67.
Ms. Linda M. Moran, M.CI.Sc. Pannbacker, M. (1971). Language skills of cleft palate children: a
Children's Hospital Of Eastern Ontario review. British Journal of Disorders of Communication. 6, 37-41:
40) Smyth Rd. Paradise, J.L., Bluestone, c'D., & Felder, H. (1969). The universality
Ottawa, Ontario KIH 8Ll of otitis media in 50 infants with cleft palate. Pediatrics. 44.35-42.
Paradise, J.L.. Smith C.G., & Bluestone, c'D. (1976). Tympanomet-
References ric detection of middle ear effusion in infants and young children.
Pediatrics,58, 198-209.
Bluestone, C.D.( 1971). Eustachian tube obstruction in the infant with
Picton, T.W., & Durieux-Smith, A. (1988). Auditory evoked poten-
cleft palate. Annals of Otology, Rhinology and Laryngology. 80.
tials in the assessment of hearing. Neurologic Clinics. 6, 791-808.
Supplement 2, 1-30.
Richards, I.D.G .. & Roberts, c.J. (1967). The at-risk infant. Lancet.
Brooks, D.N. (1980). Otitis media in infancy. In G.T. Mencher & S.E.
293,711-714.
Gerber (Eds.). Early Management of Hearing Loss (pp. 121-130).
New York: Grune and Stratton. Rood, S.R., & Stool, S.E. (1981). Current concepts of the etiology.
diagnosis and management of cleft palate related otopathologic dis-
Bzoch, K.R. (1965). Articulation proficiency and error patterns of ease. Otolaryngology Clinics of North America, 14, 865-884.
preschool cleft palate and normal children. Cleft Palate Journal. 2,
340-349. Schwartz, D.M., & Schwartz, R.H. (1978). A comparison of
tympanometry and acoustic reflex measurements for detecting middle
Coats, A.C., & Martin, 1.L. (1985). Human auditory nerve action ear effusions in infants below seven months of age. In E.R. Harford,
potentials and brainstem evoked responses. Effects of audiogram F.H. Bess, C.D. Bluestone, & J .0. Klein (Eds.), Impedance Screening
shape and lesion location. Archives Otolaryngology, 103,605-622. for Middle Ear Disease in Children (pp. 91-96). New York: Grune
Durieux-Smith, A., Picton, T., Edwards, C., MacMurray, B., & Good- and Stratton.
man, J.T. (1987). Brainstem Electric Response Audiometry in infants Stool, S.E., & Randall, P. (1968). Unexpected ear disease in infants
of a Neonatal Intensive Care Unit. Audiology. 26, 284-297. with cleft palate. Cleft Palate Journal,4, 99-103.
Edwards, c'G., & Durieux-Smith, A. (1985). Auditory brainstem Tropper, G., Moran, L., Odell, P., & Durieux-Smith, A. (1988). The
responses from neonates: Special considerations. Human Communi- contribution of Brainstem Electric Response Audiometry to the eval-
cation Canada. 9, 5-14. uation and management of children with cleft palate. Journal of
Otolaryngology, 17, 103-110.
Feagans, L., Blood, I., & Tubman, J.G. (1988). In F.H. Bess (Ed.).
Hearing Impairment in Children (pp. 347-374). Parkton, Maryland: Ventry, LM. (1980). Effects of conduclive hearing loss: Fact or
York Press. fiction. Journal of Speech and Hearing Disorders, 45, 143-156.
JSLPAIROA (HCC) Vo!. 13. No. 3. September 1989 47
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- PSM Images Based QuestionsDokument27 SeitenPSM Images Based QuestionsKannan KannanNoch keine Bewertungen
- ACE Personal Trainer Manual Chapter 13Dokument59 SeitenACE Personal Trainer Manual Chapter 13Đạt NguyễnNoch keine Bewertungen
- ThesisDokument30 SeitenThesisSimran JosanNoch keine Bewertungen
- Psilocybin in Neuropsychiatry A Review of Its PharDokument11 SeitenPsilocybin in Neuropsychiatry A Review of Its PharalexandrosNoch keine Bewertungen
- Penting CI Zenner2016 PDFDokument13 SeitenPenting CI Zenner2016 PDFmitaNoch keine Bewertungen
- Patfis Atik2011Dokument5 SeitenPatfis Atik2011mitaNoch keine Bewertungen
- Tumor PDFDokument9 SeitenTumor PDFmitaNoch keine Bewertungen
- Bailey CH 161 Tinnitus and Hyperacusis-1-10Dokument10 SeitenBailey CH 161 Tinnitus and Hyperacusis-1-10mitaNoch keine Bewertungen
- Patfis Atik2011Dokument5 SeitenPatfis Atik2011mitaNoch keine Bewertungen
- Jco 18 01921Dokument24 SeitenJco 18 01921mitaNoch keine Bewertungen
- Main Article PDFDokument17 SeitenMain Article PDFmitaNoch keine Bewertungen
- Moran Jslpa 1989Dokument5 SeitenMoran Jslpa 1989mitaNoch keine Bewertungen
- Oma La Copil PDFDokument11 SeitenOma La Copil PDFmitaNoch keine Bewertungen
- Management of Gradenigo Syndrome in A ChildDokument4 SeitenManagement of Gradenigo Syndrome in A ChildmitaNoch keine Bewertungen
- BeraDokument7 SeitenBeramitaNoch keine Bewertungen
- Prasad 2007Dokument5 SeitenPrasad 2007mitaNoch keine Bewertungen
- Gradenigo Syndrome From Acute Sphenoiditis: A Case: OtolaryngologyDokument4 SeitenGradenigo Syndrome From Acute Sphenoiditis: A Case: OtolaryngologymitaNoch keine Bewertungen
- Adult LaryngomlaciaDokument3 SeitenAdult LaryngomlaciamitaNoch keine Bewertungen
- Pa 1Dokument48 SeitenPa 1mitaNoch keine Bewertungen
- Arch Dis Child 2016 Hilland 443 8Dokument7 SeitenArch Dis Child 2016 Hilland 443 8mitaNoch keine Bewertungen
- (Romanian Journal of Rhinology) Epistaxis Management - Our Point of View and Literature ReviewDokument7 Seiten(Romanian Journal of Rhinology) Epistaxis Management - Our Point of View and Literature ReviewRizki AuditaNoch keine Bewertungen
- Otomycosis: Case Report Dr. Ima Dewi RDokument24 SeitenOtomycosis: Case Report Dr. Ima Dewi RmitaNoch keine Bewertungen
- A Case of Giant Pleomorphic Adenoma of The Parotid GlandDokument3 SeitenA Case of Giant Pleomorphic Adenoma of The Parotid GlandmitaNoch keine Bewertungen
- Congenital Laryngeal WebsDokument3 SeitenCongenital Laryngeal WebsmitaNoch keine Bewertungen
- Adult Sinusitis Physicianresource Diagnostic Criteria RhinosinusitisDokument2 SeitenAdult Sinusitis Physicianresource Diagnostic Criteria RhinosinusitismitaNoch keine Bewertungen
- CR Pa 2 PDFDokument4 SeitenCR Pa 2 PDFmitaNoch keine Bewertungen
- Endoscopic Supraglottoplasty in Children With Severe Laryngomalacia With and Without Neurological ImpairmentDokument5 SeitenEndoscopic Supraglottoplasty in Children With Severe Laryngomalacia With and Without Neurological ImpairmentmitaNoch keine Bewertungen
- Pa 3Dokument87 SeitenPa 3mitaNoch keine Bewertungen
- Sinusitis: Prof. Sameer Ali Bafaqeeh, MD. Otolaryngology Department KSUDokument15 SeitenSinusitis: Prof. Sameer Ali Bafaqeeh, MD. Otolaryngology Department KSUmitaNoch keine Bewertungen
- Pe Rich On DR It Is of The Auricle and Its ManagementDokument6 SeitenPe Rich On DR It Is of The Auricle and Its ManagementmitaNoch keine Bewertungen
- Case Report LMDokument2 SeitenCase Report LMmitaNoch keine Bewertungen
- S 1879729612000725Dokument7 SeitenS 1879729612000725zzooooeeeeeeNoch keine Bewertungen
- Epistaxis Anterior FinalDokument7 SeitenEpistaxis Anterior FinalmitaNoch keine Bewertungen
- My Trip To The Hospital - A Coloring BookDokument0 SeitenMy Trip To The Hospital - A Coloring Bookili_thNoch keine Bewertungen
- Why Your Muscles Get SoreDokument11 SeitenWhy Your Muscles Get SoreanaluieNoch keine Bewertungen
- Case Scenario 1Dokument45 SeitenCase Scenario 1Payas JoshiNoch keine Bewertungen
- Pediatric Diabetes InsipidusDokument11 SeitenPediatric Diabetes InsipidusVictor Matias BarriosNoch keine Bewertungen
- Programmed Postoperative Physiotherapy May Improve Functional Outcomes in Pneumonectomy Patients of Rare Causes Case SeriesDokument7 SeitenProgrammed Postoperative Physiotherapy May Improve Functional Outcomes in Pneumonectomy Patients of Rare Causes Case SeriesAtu KaushalNoch keine Bewertungen
- Jurnal 3Dokument4 SeitenJurnal 3Arum RaniNoch keine Bewertungen
- Grade 5 Ut4 Revision UploadDokument10 SeitenGrade 5 Ut4 Revision UploadFasi HaiderNoch keine Bewertungen
- Ilovepdf MergedDokument34 SeitenIlovepdf MergedSheen LegsNoch keine Bewertungen
- Sample Health Teaching PlanDokument1 SeiteSample Health Teaching PlanGia Espinosa OcbeñaNoch keine Bewertungen
- Vibrio CholeraeDokument20 SeitenVibrio CholeraeChockalingam MeenakshisundaramNoch keine Bewertungen
- 2021 06 Reference Texts Textes de ReferenceDokument14 Seiten2021 06 Reference Texts Textes de Referenceaishwarya desaiNoch keine Bewertungen
- Health - Very Very Important Tips: WaterDokument8 SeitenHealth - Very Very Important Tips: WaterLohidas PailaNoch keine Bewertungen
- Procedure Study - Oxygen TherapyDokument4 SeitenProcedure Study - Oxygen TherapyFaye AseoNoch keine Bewertungen
- My 5senserelativ (App) : Pedro Pérez Juan Gómez Luis Mejía Group 0 English IIIDokument4 SeitenMy 5senserelativ (App) : Pedro Pérez Juan Gómez Luis Mejía Group 0 English IIIjarles mauricio hernandez parraNoch keine Bewertungen
- وسيلة منصوريDokument126 Seitenوسيلة منصوريhouda houdaNoch keine Bewertungen
- Cipla - Sheet1Dokument14 SeitenCipla - Sheet1Conflict YTNoch keine Bewertungen
- Difficulty in SwallowingDokument1 SeiteDifficulty in SwallowingmawelNoch keine Bewertungen
- Orthopaedic SlidesDokument163 SeitenOrthopaedic SlidesVivian ChepkemeiNoch keine Bewertungen
- Name: Insong, Osannah Irish B. Section: BSMT 3CDokument1 SeiteName: Insong, Osannah Irish B. Section: BSMT 3COsannah Irish InsongNoch keine Bewertungen
- Diseases of The Skeletal SystemDokument20 SeitenDiseases of The Skeletal Systemlateef ramonNoch keine Bewertungen
- Diabetes and Hearing Loss (Pamela Parker MD)Dokument2 SeitenDiabetes and Hearing Loss (Pamela Parker MD)Sartika Rizky HapsariNoch keine Bewertungen
- Autism Spectrum Disorders: A Booklet For Parents and CarersDokument40 SeitenAutism Spectrum Disorders: A Booklet For Parents and CarersAndreea SanduNoch keine Bewertungen
- Chromium Picolinate Side Effects What Are The Side Effects of Chromium Picolinate?Dokument5 SeitenChromium Picolinate Side Effects What Are The Side Effects of Chromium Picolinate?Jun JoniNoch keine Bewertungen
- Notes: Generally, What Are They?Dokument10 SeitenNotes: Generally, What Are They?Yusril MarhaenNoch keine Bewertungen
- Assesment and Summary of FindingsDokument3 SeitenAssesment and Summary of Findingscami bihagNoch keine Bewertungen
- Manual of Contact Lens Prescribing and Fitting, 3rd Edition: The Ocular Fundus Offers The Clinician AnDokument2 SeitenManual of Contact Lens Prescribing and Fitting, 3rd Edition: The Ocular Fundus Offers The Clinician AnphenixousNoch keine Bewertungen