Beruflich Dokumente
Kultur Dokumente
Pedia Stickers
Hochgeladen von
mkct111Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pedia Stickers
Hochgeladen von
mkct111Copyright:
Verfügbare Formate
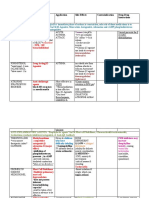
Amino acid
Empiric dose: 2-3g/day
Epinephrine Preparation: 8%/100ml
Neonate *
Asystole and Bradycardia Calcium
0.01 – 0.03 mkdose 1:10,000 Empiric dose: 200-400/day
0.1 – 0.3 ml/kg/dose IV/ET Preparation: 100mg/ml
Infants and Children * Wt x ED = mg/d x prep 1ml/100mg
1st dose: 0.01 mg/kg 1:10,000
Sodium
0.1 ml/kg max dose: 1 mg (10ml)
Empiric dose:
ET
Preparation: 2.5 meqs/mL
Uncuffed in patients ≤ 8 y/o
* Wt x ED
Age in years + 4 (uncuffed) 2.5
4 + 3 (cuffed) Potassium
16 + age/4 Empiric dose:
Depth: 3x FT size Preparation: 2 meqs/mL
* Wt x ED
Dopamine 2
IVRF x (dopa) x 60
800 or 400 TPR of Newborns
800 – 1 cc dopa + 49cc D5W BW 1-2 days 3-4 days 7-30 days
400 – 0.5 cc dopa + 49 cc D5W <750 g 100-250 150-300 120-180
750-1000g 80-150 100-150 120-180
Blood component Replacement 1000-1500g 60-100 80-150 120-180
Volume of PRBC’s = EBV (ml) x DHCT – Actual
>1500g 60-80 100-150 120-180
HCT of PRBC’s
(0.55)
CPAP
Estimated Blood Volume
CA = 100 – F102 x CPAP
Age Total Blood Volume (ml/kg) 79
Preterm 90-105 O2 = CPAP – CA
Term 78-86
1-12 mos 73-78
1-3 years 74-82 WHO Treatment Plan for Dehydration
4-6 years 80-86 Plan A ORS
7-18 year 83-90 <24 months 50-100ml 500ml/day
2-10 years 100-200ml 1000ml/day
TPN 10 years or more As tolerated 2000ml/day
Plan B Moderate or Some Dehydration
Compute for electrolytes first (Na, K, Ca, AA)
ORS to be given in the 1st 4 hours
AA of milk – 10.48 x volume of feeding
* 75ml/kg BW
1000
Plan C Severe Dehydration: IV
AA of milk – AA required = AA TPN
100ml/kg PLRS or PNSS
<12 mos older
30ml/kg 1 hr 30 mins
Feeding
Breastmilk: 20 cal/30ml or 1 oz. 70ml/kg 5 hours 2 1/2hours
Formula: 24 cal/3oml or 1 oz. Anion Gap
[Na] – ([HCO3] + [Cl])
Total Caloric Input Normal: 12 meqs/L (range: 8-16meqs/L)
Increased Anion Gap
Amount of feeding x Frequency x Cal
30cc = DKA
Present weight Renal Failure
Lactic acidosis
Hyperglycemic Nonketotic Coma
Dextrosity Disorders of AA metabolism
Large amount of Penicillin
K = Desired Dx – Actual Dx or Total of electrolytes x
Salicylate poisoning
Dx/45
D50 – Actual Ethylene glycol/methanol ingestion
K x TFR x weight = Amount of D5050 Decreased Anion Gap
Nephrotic syndrome
Lithium ingestion
GIR Multiple myeloma
Dextrosity x desired rate x K (0.167)
Weight PEFR in 6-7 y/o
Normal: 4-8 mg/kg/min
MALES ( Height in cm – 100 ) 5+ 175
FEMALES ( Height In cm – 100 ) 5+ 170
Total Fluid Requirement Peak flow variability
Amount of feeding x frequency = Highest Reading - Lowest reading x 100
Present weight Highest reading
IMMUNIZATIONS
VITAL SIGNS AT VARIOUS AGE
BCG
Intradermal HR BP RR
< 12 months: 0.05 ml AGE
> 12 months: 0.1 ml
Premature 120-170 55-75/ 35-45 40-70
HBV
Intramuscular 0-3 mos 100-150 65-85/ 45-55 35-55
1st dose: at birth (within 24 hours): 0.5ml 3-6 mos 90-120 70-90/ 50-65 30-45
2nd dose: 1 month 6-12 mos 80-120 80-100/ 55-65 25-40
3rd dose: 6 months
1-3 yr 70-110 90-105/ 55-70 20-30
4th dose: 3rd dose given < 6 months; No birth dose given;
Preterms, < 2 kg 3-6 yr 65-110 95-110/ 60-75 20-25
Measles Vaccine 6-12 yr 60-95 100-120/ 60-75 14-22
Subcutaneous
12 (*) yr 55-85 110-135/ 65-85 12-18
9 months but can be given as early as 6 months
MMR
12 months
MNEMONICS FOR WEIGHT
Booster: 4-6 years old
Given earlier: 4 weeks apart Infants < 6 months old Wt. in grams= (age in mos x 600) + BW
MMR + Varicella
Subcutaneous Infants 6-12 months old Wt. in grams= (age in mos x 500) + BW
12-15 months
Booster: 4-6 years old ≥ 2 years old Wt. in Kg= (age in year x 2) + 8
Provided that last dose is 3 months apart from last dose 6 to 12 years old Wt. in Kg= ((age in year x 7) – 5) / 2
Influenza
Intramuscular or Subcutaneous MNEMONICS FOR HEIGHT
February – June Height in 1st year = 1.5 x birth length
2 doses separated by 4 weeks Height in 2nd year= 30 inches or ½ of mature height (boys)
HAV Height in 3rd year = 36 inches (3 ft)
Intramuscular Height in 4th year = 40 inches or 2 x birth length
Recommended at 12 months Height in 13th year = 3 x birth length
2nd dose: 6-12 months from 1st dose Height in cm = (age in years x 5) + 80
Rotavirus
Monovalent: oral, 2 doses, 3 weeks – 14 weeks
(<15weeks), minimum interval: 4 week, not later than 24 RECOMMENDED ENERGY and NUTRIENT INTAKE PER DAY
weeks (RENI) From 0-18 years old
Pentavalent: oral 3 doses Population Group Weight (kg) Energy (kcal) Protein (g)
Typhoid Infants, mos
Intramuscular Birth - <6 6 560 9
History of travel 6- <12 9 720 14
Exposure to Salmonella typhi Children, y
2 years old, repeat every 2-3 years 1-3 13 1070 28
4-6 19 1410 38
7-9 24 1600 43
PRIMITIVE REFLEXES Males, y
10-12 34 2140 54
REFLEX APPEARS AT DISAPPEARS AT
13-15 50 2800 71
Suck Birth 3 mos 16-18 58 2840 73
Root Birth 3 mos 19-29 59 2490 67
Moro Birth 4-6 mos 30-49 59 2420 67
Tonic Neck Birth 6-7 mos 50-64 59 2170 67
Babinski Birth 2 years 65+ 59 1890 67
Landau 3 mos 12 mos Females, y
Persists 10-12 35 1920 49
Parachute 7-9 mos 13-15 49 2250 63
throughout life
1618 50 2050 59
Walking/
Birth 6 weeks
Stepping
Palmar grasp Birth 5-6 mos
CLASSIFICATION of SEX MATURITY STATES in GIRLS
Galant Birth 4-6 mos
SMR STAGE PUBIC HAIR BREASTS
Swimming Birth 4-6 mos
Babkin Birth
1 Preadolescent Preadolescent
Present in various
neurologic conditions 2 Sparse, lightly pigmented, Breast and papilla elevated as small
Palmomental straight, medial border of mound; diameter of areola increased
such as Down’s
labia
syndrome
3 Darker, beginning to curl, Breast and areola enlarged, no contour
Shout/ pouting Infancy 1 year increased amount separation
4 Coarse, curly, abundant, but Areola and papilla form secondary mound
less than in adult
Z-SCORES 5 Adult feminine triangle, Mature, nipple projects, areola part of
spread to medial surface of general breast contour
Weight
Length/ thigh
Weight for for BMI for
Height CLASSIFICATION of SEX MATURITY STATES in BOYS
AGE Length/ Age
for AGE
Height SMR STAGE PUBIC HAIR BREASTS
Above 3 Very tall Use weight OBESE
Above 2 for length, OVERWEIGHT 1 None Preadolescent
NORMAL BMI for age POSSIBLE RISK OF 2 Scanty, long, slightly Enlarge scrotum, pink, texture altered
Above 1 chart pigmented
OVERWEIGHT
Median 3 Darker, starting to curl, small Larger
NORMAL amount
Below -1
Below -2 STUNTED Underweight WASTED 4 Resembles adult type, but Larger, scrotum dark
Severely less quantity, coarse, curly
Severely 5 Adult distribution, spread to Adult size
Below -3 Underweigh SEVERELY WASTED
Stunted medical surface of thigh
t
Assessment of Dehydration According to the World Health
MODIFIED GLASGOW COMA SCALE FOR INTANTS AND CHILDREN
Organization*
Area Two of the following signs:
Infants Children Score -Lethargic or unconscious
Assessed
Severe Dehydration -Sunken eyes
Eye
Open spontaneously Open spontaneously 4 -Not able to drink or drinking poorly
Opening
-Skin pinch goes back very slowly
Open in response to Open in response to
3
verbal stimuli verbal stimuli Two of the following signs:
Open in response to Open in response to -Restless, irritable
2 Some Dehydration -Sunken eyes
pain only pain only
No response No response 1 -Thirsty, drinks eagerly
-Skin pinch goes back slowly
Verbal
Coos and babbles Oriented, appropriate 5 Not enough of the above signs to classify as some or
Response No Dehydration
Irritable cries Confused 4 severe dehydration
Cries in response to
Inappropriate words 3
pain
Incomprehensible DEHYDRATION
Moans in response in
words or nonspecific 2 SYMPTOMS MINIMAL OR MILD NTO SEVERE
pain NONE MODERATE (>9% BW)
sound
No response No response 1 (<3% Loss of (3-9% Loss of BW)
BW)
Motor Moves spontaneously
Obeys commands Mental Status Well; alert Normal, fatigued or Apathetic, lethargic,
Response and purposefully 6
restless, irritable unconscious
Localizes painful
Withdraws to touch 5
stimuli Thirst Drinks normally, Thirsty; eager to drink Drinks poorly;
Withdraws in Withdraws in response might refuse unable to drink
4
response to pain to pain liquids
Responds to pain
with decorticate Responds to pain with Heart Rate Normal Normal to increased Tachycardia with
3 bradycardia in most
posturing (abnormal flexion
flexion) severe cases
Responds to pain Quality of Pulse Normal Normal to decreased Weak, thread, or
with decerebrate Responds to pain with impalpable
2 Breathing Normal Normal; fast Deep
posturing (abnormal extension
extension) Eyes Normal Slightly sunken Deeply sunken
No response No response 1 Tears Present Decreased Absent
Mouth and Moist Dry Parched
Tongue
Skinfold Instant recoil < 2 secs >2 secs
GLASGOW COMA SCALE FOR <5 years old
Capillary refill Normal Prolonged Prolonged, minimal
BEST MOTOR RESPONSE (6)
Spontaneous 6
Localizes 5 Extremities Warm Cool Cool; mottled,
Normal Flexion 4 cyanotic
Abnormal Flexion 3 Urine Output Normal to Decreased Minimal
Abnormal Extension 2 decreased
Flaccid 1
VERBALIZATION (5)
Appropriate for age, fixes and follows, 5 CLINICAL CORRELATES OF DEHYDRATION
social smile
Cries but consolable 4 Severity Fluid Deficit in ml/kg SIGNS
Persistently irritable 3 Infants Adolescents
Restless/Lethargic 2
None 1 Typically minimal findings but
EYE OPENING (4) may have slightly dry, buccal
MILD 50 (5%) 30 (3%)
Spontaneous 4 mucus membranes, increased
To voice 3 thirst, slightly decreased UO
To pain 2
Not at all 1
Dry buccal mucus membranes,
MILD 14-15
tachycardia, little or no UO,
MODERATE 9-13 MODERATE 100 (10%) 50-60 (5-6%)
lethargy, sunken eyes and
SEVERE 3-8 fontanelles, loss of skin turgor
KRAMER JAUNDICE SCALE Same as moderate plus a rapid
thread pulse, no tears,
Face TSB ~ 5 mg/dl cyanosis, rapid breathing,
SEVERE 150 (15%) 70-60 (7-6%)
Mid-abdomen TSB ~ 15 mg/dl delayed capillary refill,
Feet excluding soles and palms TSB ~ 20 mg/dl hypotension, mottled skin,
Including soles and palms TSB ~ 25 mg/dl coma
Grade 0 None
Grade 1 Face and neck only
Grade 2 Chest and back HOLIDAY SEGAR METHOD
Grade 3 Abdomen below umbilicus to 0-10 kg 100ml/kg
knees
Grade 4 Arms and legs below knees 10-20 kg 50ml/kg
Grade 5 Hands and feet >20kg 20ml/kg
** total ml/kg divided by 24 hours
WHO TREATMENT PLAN for DEHYDRATION < 10y/o or < 40kg: D5IMB
PLAN A ORS > 10y/o or >40kg: D5NM
<24 months 50-100 ml 500 ml/day
2-10 years 100-200 ml 10000 ml/day
10 years or more As tolerated 2000 ml/day DEFICIT THERAPY (DT)
PLAN B Moderate or Some Dehydration MILD MODERATE SEVERE
ORS to be given in the 1 st
24 hours <2 y/o or <15kg 5% 10% 15%
Wt x 50 Wt x 100 Wt x 150
*75 ml/kg BW
Plan C Severe Dehydration: IV >2 y/o or > 3% 6% 9%
100 ml/kg PLRS or PNSS 15kg Wt x 30 Wt x 60 Wt x 90
<12 mos older X1 X1.3 X1.5
30 ml/kg 1 hr 30 mins
** Run DT for 6 hours then re –assess
70 ml/kg 5 hours 2 ½ hours
KAWASAKI DISEASE TREATMENT of TYPHOID FEVER in CHILDREN
Diagnostic criteria: OPTIMAL THERAPY ALTERNATIVE EFFECTIVE DRUGS
1. Remittent fever (41C) persisting for more than 5 days SUSCEPTI ANTIBIOTIC Daily Days Antibiotic Daily Days
2. Bilateral conjunctival infection without exudates BILITY Dose Dose
3. Strawberry tongue, erythema and cracking of the lips mk/day mk/day
4. Erythema and edema od the hands and feet
UNCOMPLICATED TYPHOID FEVER
5. Polymorphous exanthems
Fully Chloramphe 50-75 14- Fluoroquino 15 5-7
6. Unilateral CLAD > 1.5 CM
Sensitive nicol 21 lone, eg.
Treatment: Ofloxacin or
IVIG-treatment of choice
ciprofloxaci
-2 g/kg/day
n
Aspirin 80-100 mg/kg/day
Amoxicillin 75-100 14
Diagnosis: serial 2d echo aneurysm seen
Multidrug Fluoroquino 15 5-7 Azithromyci 8-10 7
ACUTE STAGE resistant lone or n
• cefixime
Intravenous immunoglobulin 2 g/kg over 10-12 hr
15-20 7-14 Cefixime 15-20 7-14
Quinolone Azithromyci 8-10 7 Cefixime 20 7-14
AND resistant n or
ceftriaxone
• Aspirin 80-100 mg/kg/day divided every 6 hr orally until patient is afebrile 75 10-
for at least 48 hr 14
CONVALESCENT STAGE SEVERE TYPHOID FEVER
• Aspirin 3-5 mg/kg once daily orally until 6-8 wk after illness onset Fully Ampicillin 100 14 Fluoroquino 15 10-
Sensitive or lone, eg. 14
LONG-TERM THERAPY FOR PATIENTS WITH CORONARY ABNORMALITIES Ceftriaxone Ofloxacin or
• ciprofloxaci
Aspirin 3-5 mg/kg once daily orally n
60-75 10-
• 14
Clopidogrel 1 mg/kg/day (max 75 mg/day)
Multidrug Fluoroquino 15 10- Cefrtiaxone 60 10-
• Most experts add warfarin or low-molecular-weight heparin for those resistant lone 14 or 14
patients at particularly high risk of thrombosis cefotaxime
ACUTE CORONARY THROMBOSIS 80
Quinolone Ceftriaxone 60-75 10- Fluoroquino 20-30 14
• Prompt fibrinolytic therapy with tissue plasminogen activator or other
resistant 14 lone
thrombolytic agent under supervision of a pediatric cardiologist
RECOMMENDED ERADICATION THERAPIES for H. pylori
RHD
Medications Dose Duration of
Revised jones criteria Treatment
Major Criteria Amoxicillin 50 mg/kg/day in 2 divided 14 days
1. Arthritis most common doses
2. Carditis Clarithromycin 15 mg/kg/day in 2 divided 14 days
3. Erythema Marginatum doses
4. Sydenham’s Chorea PPI 1 mg/kg/day in 2 divided 1 month
5. Subcutaneous nodules doses
Minor Criteria or
1. Arthralgia Amoxicillin 50 mg/kg/day in 2 divided 14 days
2. Fever < 39C doses
3. Elevated acute phase reactants ESR, C-reactive Metronidazole 20 mg/kg/day in 2 divided 14 days
CHON doses
4. Prolonged PR interval PPI 1 mg/kg/day in 2 divided 1 month
Diagnosis via 2 major or 1 major + 2 minor doses
Previous grp A streptococcal infection or
RHD Clarithromycin 15 mg/kg/day in 2 divided 14 days
1. Mitral regurgitation/ mitral stenosis on PE doses
2. Left ventricular/ Right ventricular hypertrophy on Metronidazole 20 mg/kg/day in 2 divided 14 days
ECG doses
3. Irregular cardiac borders on X-ray PPI 1 mg/kg/day in 2 divided 1 month
doses
INFECTIVE ENDOCARDITIS ANTIBIOTICS USED for TREATMENT of BACTERIAL MENINGITIS
Infective Endocarditis NEONATES INFANTS and CHILDREN
1. Strep Viridians – most common, use Pen G and DRUG 0-7 days 8-28 days
gentamycin Amikacin 15-20 days 20-30 divided q8h 20-30 divided
2. Staph Aureus – 2nd most common, use Methicillin and q8h
gentamycin Ampicillin 200-300 divided 300 divided q4h 300 divided q4-
q8h or q6h 6h
Cefotaxime 100 divided q12h 150-200 divided 200-300 divided
ACTIVE RF q8h or q6h q8h or q6h
1.Joint symptoms Ceftriaxone 100 divided
2. Murmurs q12h or q24h
3. Inc. heart size Ceftazidine 150 divided q12h 150 divided q8h 150 divided q8h
4. CHF Gentamicin 5 divided q12h 7.5 divided q8h 7.5 divided q8 h
5. Subcutaneous Nodules Meropenem 120 divided q8h
6. Sleeping pulse rate of > 100/min Nafcillin 100-150 divided 150-200 divided 150-200 divided
7. + C-reactive protein q8h or q12h q8h or q6h q4h or q6h
8. Consecutive fever for 3 days Penicillin G 250,000-450,000 450,000 divided 450,000 divided
Treatment for RF divided q8h q6h q4h or q6h
1. Pen G/ Benzathine given once (ED: 100K-400K) Rifampicin 20 divided q12h
2. Penicillin V/Phenoxy methyl Penicillin 2-3 times per day given for Tobramycin 5 divided q12h 7.5 divided q8h 7.5 divided q8h
10 days Vancomycin 30 divided q12h 30-45 divided q8h 60 divided q6h
3. Erythromycin 2-4 times per day given for 10 days
Diagnosis via 2 major or 1 major + 2 minor
FINDINGS: BACTERIAL MENINGITIS
Previous grp A streptococcal infection
1. See Nigrovic Clinical Decision Rule
2. CSF Color: Cloudy CSF
3. CSF Glucose much less that 50
4. CSF Protein much greater that 45
5. CSF Leukocytes: Markedly increased Neutrophils
6. CSF Opening Pressure: increased >200
Albumin
Premature 1 day 1.8-3.0 g/dl
Full term <6 days 2.5-3.4 g/dl
FINDINGS: FUNGAL MENINGITIS
<5 years old 3.9-5.0 g/dl
1. CSF Color: Clear to Cloudy Fluid 5-19 years 4.0-5.3 g/dl
2. CSF Glucose <50
Sodium
3. CSF Protein >45 Newborn 134-146 mmol/L
4. CSF Leukocytes: Monocytes increased Infant 139-146 mmol/L
5. CSF Opening Pressure: increased Child 138-145 mmol/L
Thereafter 136-146 mmol/L
Potassium
<2 months 3.0-7.0 mmol/L
FINDINGS: VIRAL MENINGITIS 2-12 months 3.5-6.0 mmol/L
1. CSF Color: Clear to Cloudy Fluid >12 months 3.5-5.0 mmol/L
2. CSF Glucose: Normal Chloride
3. CSF Protein >45 Cord blood 96-105 mmol/L
4. CSF Leukocytes: Increased CSF Lymphocytes Newborn 97-110 mmol/L
5. CSF Opening Pressure: Normal or increased Thereafter 98-106 mmol/L
Bicarbonate (HCO3)
Arterial 21-28 mmol/L
Venous 22-29 mmol/L
FINDINGS: TUBERCULOSIS MENINGITIS Carbon Dioxide Partial Pressure
1. CSF Color: Cloudy Fluid (PCO2) 27-40 mmHg
2. CSF Glucose <50 Newborn 27-41 mmHg
3. CSF Protein >45 Infant 35-48 mmHg
4. CSF Leukocytes Thereafter M 32-45 mmHg
a. Early: Neutrophils increased Thereafter F
b. Later: Lymphocytes increased Glucose
Cord blood 45-96 mg/dl
Premature 20-60 mg/dl
Neonate 30-60 mg/dl
FINDINGS: GUILLAIN-BARRE Newborn
1. CSF Color: Clear to Cloudy Fluid 1 day 40-60 mg/dl
>1 day 50-90 mg/dl
2. CSF Glucose: Normal
Child 60-100 mg/dl
3. CSF Protein much greater than 45 Adult 70-105 mg/dl
4. CSF Leukocytes: Lymphocytes normal or Creatinine
increased Cord blood 0.6-1.2 mg/dl
5. CSF Opening Pressure: Normal Newborn 0.3-1.0 mg/dl
Infant 0.2-0.4 mg/dl
Child 0.3-0.7 mg/dl
Adolescent 0.5-1.0 mg/dl
FINDINGS: NEOPLASM Adult M 0.6-1.2 mg/dl
1. CSF Color: Clear to xanthochromic Adult F 0.5-1.1 mg/dl
2. CSF Glucose: Normal or decreased Creatinine clearance: newborn 40-65 ml/min/1.73 m2 | <40 yr, M: 97-137, F:
3. CSF Protein: Normal or increased 88-128
4. CSF Leukocytes: Normal or increased lymphocytes Calcium Total
5. CSF Opening Pressure: increased >200 Cord blood 9.0-11.5 mg/dl
Newborn (3-24 hours) 9.0-10.6 mg/dl
24-48 hours 7.0- 12.0 mg/dl
4-7 days 9.0-10.9 mg/dl
FINDINGS: NEUROSYPHILIS Child 8.8-10.8 mg/dl
1. CSF Color: Clear to Cloudy Fluid Thereafter 8.4-10.2 mg/dl
2. CSF Glucose: Normal Calcium Ionized
3. CSF Protein >45 Cord blood 5.0-6.0 mg/dl
4. CSF Leukocytes: Monocytes increased Newborn (3-24 hours) 4.3-5.1 mg/dl
5. CSF Opening Pressure: Normal or increased 24-48 hours 4.0-4.7 mg/dl
Thereafter 4.8-4.92 mg/dl
Blood Urea Nitrogen
Cord blood 21-40 mg/dl
FINDINGS: INTRACRANIAL HEMORRHAGE Premature (1 wk) 3-25 mg/dl
1. CSF Color: Bloody CSF with xanthocromia Newborn 3-12 mg/dl
2. CSF Glucose: Normal or decreased Infant or child 5-18 mg/dl
Thereafter 7-18 mg/dl
3. CSF Protein >45
4. CSF Leukocytes: Increased
5. CSF Opening Pressure: increased >200 RABIES EXPOSURE
CATEGORY EXPOSURE MANAGEMENT
CATEGORY Feeding or touching an animal Wash exposed skin
Blood Component Replacement 1 Licking of intact skin immediately with soap
Volume of PRBC’s= EBV (ml) x DHCT – Actual Exposure to patients with s/sx of and water
HCT of PRBC’s (0.55) rabies by sharing or eating or NO VACCINES OR RIG
drinking utensils NEEDED
Casual contact to patients with s/sx May opt to give pre-
of rabies exposure prophylaxis
Estimated Blood Volume CATEGORY Nibbling or nipping of uncovered skin COMPLETE
Age Total Blood Volume (ml/kg) 2 with bruising VACCINATION UNTIL
Preterm 90-105 Minor scratches or abrasions without DAY 30
bleeding (If animal is rabid, died,
Term 78-86 Licks on broken skin killes, or unavailable for
1-12 mos 73-78 14 day observation or
1-3 years 74-82 died during period of
observation within 14
4-6 years 80-86 days)
7-18 years 83-90 CATEGORY Transdermal bites or scratches START VACCIONE AND
3 Mucous membranes contamination RIG IMMEDIATELY
with saliva
Handling of infected carcass or
ingestion of raw infected meat
Category II on head and neck area
Exposure to rabies patient
contamination of mucous membranes
with saliva or fluid through platerring
GINA CLASSIFICATION OF ASTHMA SEVERITY
Symptoms/D Symptoms/ PEF/ PEF
ay Nights FEV1 Variability Hematocrit (Hct)
1 day 48-69%
<1 times a
week
2 days 48-75%
3 days 44-72%
STEP 1 </= 2 times a >/= 2 months 28-42%
Asymptomatic <20%
Intermittent month 80%
and normal 6-12 months 35-45%
PEF between 12-18 months M 37-49%
attacks 12-18 months F 36-46%
>1 times a 18-49 years M 41-53%
week but <1
time a day
18-49 years F 36-46%
STEP 2
>2 times a >/= Hemoglobin (hgb)
Mild 20-30%
Attacks may month 80% 1-3 days 14.5-22.5 g/dl
Persistent
affect activity 2 months 9.0-14.0 g/dl
6-12 years 11.5-15.5 g/dl
Daily 12-18 years M 13.0-16.0 g/dl
STEP 3 12-18 years F 12.0-16.0 g/dl
>1 times a
Moderate Attacks affects 60-80% >30% 18-49 years M 13.5-17.5 g/dl
week
Persistent activity
18-49 years F 12.0-16.0 g/dl
Continouos WBC
Birth 9.0-30.0 x 1,000/mm3
STEP 4
Severe
Limited
Frequent
</=
>30%
12 hours 9.4-34.0 x 1,000/mm3
physical 60% 1 month 5.0-19.5 x 1,000/mm3
Persistent
activity 1-3 years 6.0-17.5 x 1,000/mm3
4-7 years 5.5-15.5 x 1,000/mm3
8-13 years 4.5-13.5 x 1,000/mm3
Adult 4.5-11.0 x 1,000/mm3
LEVELS OF ASTHMA CONTROL Myelocytes 0%
Characteristics Controlled (All Partly Controlled Uncontrolled Neutrophils-bands 3-5%
of the (Any measure Neutrophils-segmenters 54-62%
Following) present in any
week)
Lymphocytes 25-33%
Daytime None (≤ >twice/ week Three or
Monocytes 3-7%
symptoms twice/week) more features Eosinophils 1-3%
Limitations of None Any of partly Basophils 0-0.75%
activities controlled
asthma Plt ct NEWBORN: 84-478 x 10^6 Plt ct ADULT: 150-400x10^6
Nocturnal None Any
symptoms/ present in (after 1 wk, same as adult)
awakening any week
Need for None (≤ >twice/ week
reliever/ rescue twice/week)
treatment HEMODYNAMIC ASSESSMENT
Lung function* Normal <80% predicted or PARAMETERS Stable Compensated Hypotensive Shock
(PEF or FEV1 personal best condition Shock
Exacerbation None One or more/year One in any Clear and Clear and lucid Change of mental
week Sensorium lucid status (restless and
combative)
Capillary Brisk < 2 Prolonged > 2 sec Very prolonged,
Classification of asthma severity (0-4 years refill time sec mottled skin
Components of of age) Warm and Cool peripheries Cold and clammy
severity Extremities
Intermi Persistent pink
ttent Mild Moderat Sever Peripheral Good Weak and thread Feeble or absent
e e pulses volume
Symptoms <2 >2 Daily Throu Normal for Tachycardia Severe tachycardia
Heart Rate age with bradycardia in
days/w days/week ghout
the late shock
eek but not the
Normal for Normal systolic Narrowed PP < 20
daily day
age pressure but
Nighttime 0 1- 3- >1x/w BP
rising diastolic
awakenings 2x/month 4x/mont eek pressure
Impa h Normal Tachypnea Hyperpnea,
irme RR
Short-acting <2 >2 Daily Severa Kussmaul breathing
nt beta2- days/w days/week l times
agonist use eek but not per
for symptom daily day CRITERIA FOR DISCHARGE
control (not All of the following must be met:
prevention
1. No fever for at least 24-48 hours
of EIB
2. Improvement in clinical status (general well-being, appetite,
Interference None Minor Some
Extre hemodynamic status, urine output, no respiratory distress)
with normal limitation limitation
mely 3. Stable hematocrit
activity limite
4. Increasing trend of platelet count (usually preceded by rising
d
WBC)
Risk 0- >2 exacerbations in 6 months
1/year requiring oral systemic
Exacerbatio corticosteroids, or >4 wheezing
ns requiring episodes/1 year lasting >1 day
oral AND risk factors for persistent
systemic asthma
corticosteroi Consider severity and interval since
ds last exacerbation, frequency and severity
may fluctuate over time.
Exacerbation of any severity may occur in
patients in any severity category.
Step 1 Step 2 Step 3 and
consider short
Recommended step course of oral
for initiating systemic
therapy corticosteroids
In 2-6 weeks, depending on severity, evaluate
level of asthma control that is achieved. If no
clear benefit is observed in 4-6 weeks, consider
adjusting therapy or alternating diagnoses
pCAP C pCAP D
pCAP A or B
PEDIATRIC COMMUNITY ACQUIRED
PNEUMONIA CLASSIFICATION Pneumonia I Pneumonia II
Non-Severe
SEVERE VERY SEVERE
VARIABLES
CLINICAL
1. Dehydration NONE MILD MODERATE SEVERE
2. Malnutrition NONE MODERATE SEVERE
3. Pallor NONE PRESENT PRESENT
4. Respiratory rate
3 to 12 mos ≥50/min to ≤60/min >60/min to ≤ 70 >70/min
1 to 5 y/0 ≥40/min or ≤ 50/min >50/min >50/min
> 5 y/o ≥30/min or ≤ 35/min >35/min >35/min
5. Signs of respiratory failure
a) Retraction NONE IC/ Subcostal Supraclavicular/IC/SC
b) Head bobbing NONE PRESENT PRESENT
c) Cyanosis NONE PRESENT PRESENT
d) Grunting NONE NONE PRESENT
e) Apnea NONE NONE PRESENT
f) Sensorium NONE IRRITABLE Lethargic/ Stuporous/Comastose
Diagnostic aid at site-of-care
1. Chest X-ray findings of any of the
ff: effusion, abscess, air leak, or NONE PRESENT PRESENT
lobar consolidation
2. Oxygen saturation at room air 95% <95% <95%
using pulse oximetry
ACTION PLAN
1. Site-of-care Outpatient Admit to Ward Admit to a critical care facility
2. Follow-up End of treatment
GENERIC BRAND PREPARATION EMPIRIC DOSE FREQUENCY KEFOX 750mg/vial Neonates: 50-
250mg/vial 100mkd Q12
MAALOX <6mos=o.5ml QID Cefuroxime
Aluminum
>6mos: 1ml Children: 75-
hydroxide +
150mkd Q8
magnesium
hydroxide ALNIX 5mg/5ml <6y/o: 2.5mkd OD
Cetirizine diHcl >6y/o: 5-10mkd
Aluminum MAALOX <6mos:o.5ml QID
hydroxide + PLUS >6mos: 1ml ALNIX PLUS 5mg/5ml <6y/o: 2.5mkd OD
Cetirizine +
magnesium phenylephrine >6y/o: 5-10mkd
hydroxide +
simethicone CHLOROCAI 125mg/5ml </= 2kg: 25mkd OD
Chloramphenicol
RE >2kg: 50mkd
AMBROLE 30mg/5ml Wt x 0.2 TID palpitate
Q12
Ambroxol Hcl X 15mg/5ml
7.5mg/1ml Chlorphenamine + DISUDRIN WT X 0.2
phenylephrine
HIMOX 250mg/ 5ml 30-50 mkd TID at lowest DYNATUSSI WT X 0.2
GLOBAPEN 100mg/1ml dose Chlorphenamine + N
BID at high Dexamethasone +
Amoxicillin Guiafenasin +
dose
Paracetamol +
Phenylpropanolamine
PEDIAZITH 200mg/5ml 10mkd OD Cloxacillin RITE MED 125mg/5ml 25-50mkd QID
Azithromycin 100mg/1ml NATRAVOX 250mg/625mg/ <3mos: 30mkd BID
Brompheniramine PEDIATAP Wt x 0.2 TID Co-amoxiclav AUGMENTI 5ml >3mos: 20-
+ P (Amoxicillin + N 625mg/tab 40mkd
phenylpropanolam ZEDITAPP Clavulanic Acid) 25-45mkd TID
ine BID
ERCEFLOR 1-2 plastic tube BID Diphenhydramine BENADRYL 12.5mg/5ml 5mkd Q6
Bacillus clausii A
VOMETA 5mg/5ml Wt x 0.2
TRIDERM BID for 2 Domperidone
5mg/1ml
Betamethasone + weeks Ferlin drops 15ml Premature: 2- OD-BID
Gentamycin Ferrous sulfate + Folic
Ferlin syrup 120ml 4mkd
+Clotrimazole Acid + B complex
Child: 3-6mkd OD-TID
Gentamycin + COMDIDER BID for 2
BISOLVON 2mg/ 1ml Wt x 0.2 Betamethasone + M weeks
Bromhexin 4mg capsule Clotrimazole
Gentiane Radix SINUPRET Wt x 0.2
RITE MED 250mg/ 5ml 20-40mkd Q8
125mg/5 ml
Cefaclor 50mg/1ml
CEFALIN 250mg/ 5ml 25-100mkd Q6
125mg/5ml
Cefalexin 100mg/1ml
TERGECEF 100mg/5ml Infant: 8mkd Q12
20mg/1ml
Acute UTI:
16mkd Q12 for 1st
Cefixime day
8mkd
Q24 for 13
days
XTENDA 1gm + 10ml vial 1-5mos: 100- Q6
200mkd
Ceftriaxone
>/=6mos-child: Q6
150-200mkd
Ibuprofen DOLAN 200mg/5ml 5-10mkd Q6
100mg/5ml
forte DRUGS EMPIRIC DOSE FREQUENCY PREPARATION
KEPPRA 100mg/5ml 10-30mkd BID Amikacin IV / IM: 15-22.5 mkd Q8
Leviteracetam
500mg/tab 30-50 mkd TID 50/1
FUSKINA TID for 7 40-80 mkd 100mg/ml - drops
Mupirocin Amoxicillin
days 40: for virgin PN cases 125/5
Ointment
250/5 - suspension
Mupirocin + FUSKINA-B BID for 2 100-200 mkd Q6 125/5
Ampicillin
Betamethasone weeks 250/5
MONTAIR 4mg 6mos-5yrs: OD 20-40 mkd BID-TID 125/5 187/5
Cefaclor
5mg 4mg /Q8 250/5 375/5
Monmtelukast
10mg 6-14yrs: 5mg 25-100 mkd Q6 125/5
>14yrs: 10mg Cefalexin
250/5
Mometasone ELICA OD 6-8 mkd BID 100/5
furoate Cefixime
20/1
Ceftazidime IV: 90-150 Q8
HIDRASEC 10mg/sachet 1.5mkd TID Ceftriaxone IM/IV: 50-75 mkd BID
Racecadotril 30mg/sachet O: 20-40 BID/Q12 125/5
100mg/cap Cefuroxime I: 75-150 Q8 (750mg/vial)
2.25% 0.5ml via <4yrs: 0.05mkd Q1-2 250/5
nebulizer + 3ml NSS over <6y: 0.25 OD 2.5/ml
15 min PRN Cetirizine
>6y: 5-10 5/5
Racemic
Chloramphenicol O: 50-75 QID 125/5
Epinephrine >4yrs:
0.5ml/dose O: 15 mkd BID 125/5
Clarithromycin
+3ml NSS over Q3-4 250/5
15 mins PRN 6-8 BID 400/80/5
Cotrimoxazole
Rifampicin KIDZKIT 3 (1st 200mg/5ml 10mkd OD 200/40/5
Isoniazid + 2 mos) 200mg/5ml 10mkd O: 50-100 QID 125/5
Cloxacillin
Pyrazinamide 250mg/5ml 15mkd IV:100-200 Q4/Q6
Rifampicin KIDZKIT2 200mg/5ml 10mkd 30-50 mkd Q12 156.25/5
Isoniazid 200mg/5ml 10mkd 20-40 mkd BID 228/5ml
Salbutamol + PECOF WT X 0.2 25-40 mkd TID 312.5/5 – 250mg
Co-amoxiclav
Guiafenasin+ BID Amox
Bromhexin 457/5 – 400mg
Amox
Zinc Oxide + Calmoseptine TID for 3-
Calamine 5 days IV: 0.04-0.2 Q2-4 1/1
Diazepam PO: 0.12-0.8 mkd Q6-8 5/1
E-Zinc 55mg/5ml
Zinc Sulfate Rectal: 0.5
27.5mg/1ml
1mkd Stat 6.25/5
PEDZINC <6mos: 10 Diphenhydramine
5 mkd Q6 12.5/5
Zinc Sulfate + elemental zinc
Vitamin C >6mos: 10 Diloxanide 20-40 mkd TID
elemental zinc Erythromycin 30-50 mkd Q6-8
Furosemide 1-2 mkd
7.5 mkd Q8 10/1
Gentamicin
IV: 5-8 40/1
5-10 Q6 100/5
Ibuprofen
200/5
INH (Isoniazid) 10-15 QID 50/5
Meropenem 60
35-50 TID 125/5
Metronidazole
STRICT 1. Throw cans or tires to avoid 15-20 Giardia
breeding grounds for mosquitoes 50-100 mkd Q6 250/5
DENGUE 2. Cover water containers
Oxacillin
IV: 100-200
10-20
Q4/Q6
Q4 100/1 -drops
3. Use insecticides to kill the vector
Paracetamol 120/5
PRECAUTIONS 4. Use mosquito repellants and 250/5
mosquito nets 100,000-400,000 ukd Q4-6
STRICT 1. Avoid exposure to cold air, smoke, Pen G Na 300,000-400,000 ukd –
and pollens meningitic dose
ALLERGIC 2. Avoid hair sprays, gel, strong Piperacillin- <6y: 150-300 mkd IV
perfume, fabric softener, powders, tazobactam >6y: 300-400 mkd IV
cosmetic, and chalk dust PPA (Phenyl- 12 BID-TID 12.5/5
PRECAUTIONS propanolamine) 250/5
3. Wear warm clothing
Pyrazinamide 15
4. Use hypoalleregenic sheets and
O: 2-4
pillows Ranitidine
IV: 2-6
5. Do not use wool blankets and furry
Rifampicin 10-20
stuffed toys SMX-TMP 6-8 mkd BID 200/40/5
6. Keep child away from dogs, cats, 10: < 6 months old OD 55/5
hamsters, mice and other pets Zinc
20: > 6 months old
7. Wash curtains and shampoo rugs
8. Clean child’s room regularly
STRICT 1. Proper hand washing before eating
and after using the toilet
ENTERIC 2. Proper hand washing before
PRECAUTIONS handling and preparing food and
cleaning utensils used for
preparation and cooking of food
3. Boil drinking water for 15 minutes
or more
4. Cook food thoroughly
5. Wash all fruits and vegetables to be
eaten raw
6. Keep fingernails clean and short
Das könnte Ihnen auch gefallen
- Vitamin B2Dokument5 SeitenVitamin B2daccciNoch keine Bewertungen
- Quinine 1Dokument3 SeitenQuinine 1Vhan BetizNoch keine Bewertungen
- Nootropil: Qualitative and Quantitative CompositionDokument12 SeitenNootropil: Qualitative and Quantitative CompositionMuhammad TalhaNoch keine Bewertungen
- C C C Vertigo,: Electrolyte and Water Balance AgentDokument12 SeitenC C C Vertigo,: Electrolyte and Water Balance AgentEarl Tony TrinidadNoch keine Bewertungen
- Drug StudyDokument15 SeitenDrug StudyMarc AnchetaNoch keine Bewertungen
- Gastrointestinal Pharmacology: Shan NanjiDokument24 SeitenGastrointestinal Pharmacology: Shan NanjijenniferluzonNoch keine Bewertungen
- Pharmacologic Management: BleomycinDokument1 SeitePharmacologic Management: BleomycinKim ApuradoNoch keine Bewertungen
- Drug Name Mechanism Application Side Effects Contraindication Drug-Drug InteractionsDokument3 SeitenDrug Name Mechanism Application Side Effects Contraindication Drug-Drug Interactionsazhar hussinNoch keine Bewertungen
- Nsaids 190204194047Dokument40 SeitenNsaids 190204194047Harini Bala100% (1)
- Naproxen PDFDokument3 SeitenNaproxen PDFMichelle EgeraNoch keine Bewertungen
- CVD HypertensionDokument15 SeitenCVD HypertensionAbigail BascoNoch keine Bewertungen
- Idiopathic Thrombocytopenic Purpura: Overview With Report of A CaseDokument4 SeitenIdiopathic Thrombocytopenic Purpura: Overview With Report of A CaseHernan GonzalezNoch keine Bewertungen
- Drug 25Dokument17 SeitenDrug 25carol_gigliotti24100% (1)
- Nitrates Comparison ChartDokument7 SeitenNitrates Comparison ChartModi Evana PutriNoch keine Bewertungen
- 28099453C Case Study 3Dokument27 Seiten28099453C Case Study 3Alice HuiiNoch keine Bewertungen
- RABIES Health Teaching BSN1DDokument24 SeitenRABIES Health Teaching BSN1DTheother OneNoch keine Bewertungen
- Availability: Classifications: Antihistamine Antipruritic Pregnancy Category: CDokument4 SeitenAvailability: Classifications: Antihistamine Antipruritic Pregnancy Category: CCay SevillaNoch keine Bewertungen
- MCN Introduction :physiologic Changes in Pregnancy..Dokument14 SeitenMCN Introduction :physiologic Changes in Pregnancy..janet_alexisNoch keine Bewertungen
- Newest Research Paper The Challenges of Student Nurses in Their Clinical Skills Development Using Digital Technology. UwuDokument50 SeitenNewest Research Paper The Challenges of Student Nurses in Their Clinical Skills Development Using Digital Technology. UwuMaryan SubaldoNoch keine Bewertungen
- Renal Guide and Charts: AlbuminDokument16 SeitenRenal Guide and Charts: AlbuminYaima JimenezNoch keine Bewertungen
- Newborn Screening Policy Catarman Doctors Hospital, Inc.: University of Eastern PhilippinesDokument7 SeitenNewborn Screening Policy Catarman Doctors Hospital, Inc.: University of Eastern PhilippinesGenn Medrano GirayNoch keine Bewertungen
- Generic Menu - Tgp3Dokument16 SeitenGeneric Menu - Tgp3Jan Clarise Geronimo MacalaladNoch keine Bewertungen
- Voxelotor Prescribing InfoDokument15 SeitenVoxelotor Prescribing InfoLamech SiguNoch keine Bewertungen
- Antihyperglycemic Agents Comparison ChartDokument9 SeitenAntihyperglycemic Agents Comparison ChartBonnieNoch keine Bewertungen
- Antihyperglycemic Agents Comparison Chart PDFDokument9 SeitenAntihyperglycemic Agents Comparison Chart PDFconcoz100% (1)
- Types of AnemiaDokument11 SeitenTypes of AnemiaCHRISTIE MONTANO50% (2)
- Nursing Process Focus Clients Receiving Ferrous Sulfate (Feosol, Others)Dokument1 SeiteNursing Process Focus Clients Receiving Ferrous Sulfate (Feosol, Others)TracyNoch keine Bewertungen
- FoscarnetDokument2 SeitenFoscarnetTandri JuliantoNoch keine Bewertungen
- DigoxinDokument18 SeitenDigoxinApril Mergelle LapuzNoch keine Bewertungen
- Drug Study: Name Mechanism of Action Indication/Contraindication Side Effects Nursing ResponsibilityDokument2 SeitenDrug Study: Name Mechanism of Action Indication/Contraindication Side Effects Nursing ResponsibilityJoshua DavantesNoch keine Bewertungen
- Math RNDokument10 SeitenMath RNMs. Jia Mae CasimoNoch keine Bewertungen
- Drug CardsDokument3 SeitenDrug CardsDave HillNoch keine Bewertungen
- Pediatric Community-Acquired Pneumonia Clinical Guideline PDFDokument1 SeitePediatric Community-Acquired Pneumonia Clinical Guideline PDFJohn Vincent Dy OcampoNoch keine Bewertungen
- Betahistine Dihydrochloride (Serc) 1aDokument3 SeitenBetahistine Dihydrochloride (Serc) 1aGirlie Jane Sevillano RNNoch keine Bewertungen
- Indomethacin 392Dokument17 SeitenIndomethacin 392Mahadie Hasan JahadNoch keine Bewertungen
- Gastric UlcerDokument4 SeitenGastric UlcerensooooooooooNoch keine Bewertungen
- StrokeDokument1 SeiteStrokeMariel Febreo MerlanNoch keine Bewertungen
- Dengue FeverDokument5 SeitenDengue FeverMae AzoresNoch keine Bewertungen
- C191W003 Control Bleeding and Hypovolemic ShockDokument51 SeitenC191W003 Control Bleeding and Hypovolemic ShockEmad Hussien Haj-AbdullaNoch keine Bewertungen
- Coreg (Carvedilol)Dokument1 SeiteCoreg (Carvedilol)Adrianne BazoNoch keine Bewertungen
- Vancomycin Protocol RQHRDokument15 SeitenVancomycin Protocol RQHRl1o2stNoch keine Bewertungen
- Dulcolax Stool Softener Supp (Docusate Sodium)Dokument2 SeitenDulcolax Stool Softener Supp (Docusate Sodium)ENoch keine Bewertungen
- Gastrointestinal DrugsDokument2 SeitenGastrointestinal DrugsJannah Mikhaela Alibay VillarinNoch keine Bewertungen
- Pharmacology - Section 23 - Antibiotics 2Dokument5 SeitenPharmacology - Section 23 - Antibiotics 2Pathalee ThalpavilaNoch keine Bewertungen
- Pharma CompilationDokument32 SeitenPharma CompilationJustin Kaye DariaNoch keine Bewertungen
- Treatment of Diabetes MellitusDokument31 SeitenTreatment of Diabetes MellitusIrfan IdealistNoch keine Bewertungen
- Paracetamol Dosage For ChildrenDokument14 SeitenParacetamol Dosage For Childrenkevinhabakuk_88Noch keine Bewertungen
- Atropine: Drug Study: NCM 106 PharmacologyDokument6 SeitenAtropine: Drug Study: NCM 106 PharmacologyKevin RosalesNoch keine Bewertungen
- Anes Drugs TableDokument20 SeitenAnes Drugs TableKathleen Grace ManiagoNoch keine Bewertungen
- Ultimate Pharmacoogy Guide PDFDokument18 SeitenUltimate Pharmacoogy Guide PDFElizabella Henrietta TanaquilNoch keine Bewertungen
- Nifedipine Uses, Dosage & Side EffectsDokument6 SeitenNifedipine Uses, Dosage & Side EffectsXICMENNoch keine Bewertungen
- Pharma MnemonicsDokument10 SeitenPharma MnemonicsMuhammad Ali Aziz100% (4)
- Clopidogrel Bisulfate - PlavixDokument2 SeitenClopidogrel Bisulfate - PlavixKristi WrayNoch keine Bewertungen
- Vitamin B & BDokument14 SeitenVitamin B & BRemedios BandongNoch keine Bewertungen
- PurpuraDokument7 SeitenPurpuraMarie Joe AbainzaNoch keine Bewertungen
- Flucloxacillin AFTcapssolnDokument6 SeitenFlucloxacillin AFTcapssolnEliza ArmanNoch keine Bewertungen
- Drugclasses Pharmacologypart 1 PDFDokument25 SeitenDrugclasses Pharmacologypart 1 PDFSutanya100% (2)
- Pedia Stickers PDFDokument8 SeitenPedia Stickers PDFAshNoch keine Bewertungen
- Neonate: TPR of Newborns BW 1500gDokument9 SeitenNeonate: TPR of Newborns BW 1500gAnne Lorraine BringasNoch keine Bewertungen
- Acute Bacterial RhinosinusitisDokument8 SeitenAcute Bacterial RhinosinusitisKathrinna Feliz AlertaNoch keine Bewertungen
- Mandibular Fracture Supplements For InternsDokument13 SeitenMandibular Fracture Supplements For Internsmkct111Noch keine Bewertungen
- CPG On OmeDokument6 SeitenCPG On OmeKita kitaNoch keine Bewertungen
- CPG On Allergic Rhinitis 2Dokument8 SeitenCPG On Allergic Rhinitis 2mkct111Noch keine Bewertungen
- Mandibular Fracture Supplements For InternsDokument13 SeitenMandibular Fracture Supplements For Internsmkct111Noch keine Bewertungen
- Supplementry Notes For Interns - TonsilsDokument11 SeitenSupplementry Notes For Interns - Tonsilsmkct111Noch keine Bewertungen
- Physiology of The Salivary GlandsDokument54 SeitenPhysiology of The Salivary Glandsmkct111Noch keine Bewertungen
- Physiology of The Auditory SystemDokument47 SeitenPhysiology of The Auditory Systemmkct111Noch keine Bewertungen
- 92 - Benign Tumors and Tumor-Like Lesions of The Oral CavityDokument1 Seite92 - Benign Tumors and Tumor-Like Lesions of The Oral Cavitymkct111Noch keine Bewertungen
- 105 - Diagnostic Imaging of The LarynxDokument1 Seite105 - Diagnostic Imaging of The Larynxmkct111Noch keine Bewertungen
- Eponymous Signs in EntDokument10 SeitenEponymous Signs in Entmkct111Noch keine Bewertungen
- CHAP12 Nasal Manifestations of Systemic Disease PGMI VERIN, MaryneilDokument57 SeitenCHAP12 Nasal Manifestations of Systemic Disease PGMI VERIN, Maryneilmkct111Noch keine Bewertungen
- Mandibular Fracture Supplements For InternsDokument13 SeitenMandibular Fracture Supplements For Internsmkct111Noch keine Bewertungen
- Antithyroid MedicationsDokument4 SeitenAntithyroid Medicationsmkct111Noch keine Bewertungen
- Cowe Orals Physio 2Dokument12 SeitenCowe Orals Physio 2mkct111Noch keine Bewertungen
- ReviewerDokument12 SeitenReviewermkct111Noch keine Bewertungen
- Benign Lesions of The Ovary NotesDokument5 SeitenBenign Lesions of The Ovary Notesmkct111Noch keine Bewertungen
- Histology Lecture Notes - EarDokument3 SeitenHistology Lecture Notes - Earmkct111Noch keine Bewertungen
- Resto BrochureDokument2 SeitenResto BrochureGaanan RochelleNoch keine Bewertungen
- CPM16TH Essential Newborn CareDokument11 SeitenCPM16TH Essential Newborn CareKevin AgbonesNoch keine Bewertungen
- Cowe Orals Physio 2Dokument12 SeitenCowe Orals Physio 2mkct111Noch keine Bewertungen
- Must Knows - Second Half v2 (Orals1) PDFDokument34 SeitenMust Knows - Second Half v2 (Orals1) PDFmkct111Noch keine Bewertungen
- Must Knows - Second Half v2 (Orals1) PDFDokument34 SeitenMust Knows - Second Half v2 (Orals1) PDFmkct111Noch keine Bewertungen
- CPM16TH Essential Newborn CareDokument11 SeitenCPM16TH Essential Newborn CareKevin AgbonesNoch keine Bewertungen
- Preventive Pediatrics Part 3Dokument5 SeitenPreventive Pediatrics Part 3mkct111Noch keine Bewertungen
- MIMS Summary Table-G6PDDokument1 SeiteMIMS Summary Table-G6PDenchanteresse100% (3)
- Must Knows UpdatedDokument30 SeitenMust Knows Updatedmkct111Noch keine Bewertungen
- Emailing CPG-E PDFDokument206 SeitenEmailing CPG-E PDFCarlos H. AcuñaNoch keine Bewertungen
- Preventive Pediatrics Part 2Dokument5 SeitenPreventive Pediatrics Part 2mkct111Noch keine Bewertungen
- Preventive Pediatrics Part 1Dokument6 SeitenPreventive Pediatrics Part 1mkct111Noch keine Bewertungen
- Disha Publication Previous Years Problems On Current Electricity For NEET. CB1198675309 PDFDokument24 SeitenDisha Publication Previous Years Problems On Current Electricity For NEET. CB1198675309 PDFHarsh AgarwalNoch keine Bewertungen
- Ansys Flu - BatDokument30 SeitenAnsys Flu - BatNikola BoskovicNoch keine Bewertungen
- HotsDokument74 SeitenHotsgecko195Noch keine Bewertungen
- Worcester Vs Ocampo - DigestDokument1 SeiteWorcester Vs Ocampo - DigestMaria Raisa Helga YsaacNoch keine Bewertungen
- How To Access Proquest: Off-CampusDokument9 SeitenHow To Access Proquest: Off-CampusZav D. NiroNoch keine Bewertungen
- Elc650 Ws Guidelines (250219)Dokument3 SeitenElc650 Ws Guidelines (250219)panda_yien100% (1)
- MNT-Notes Pt. 2Dokument58 SeitenMNT-Notes Pt. 2leemon.mary.alipao8695Noch keine Bewertungen
- Experiment No 5 ZenerDokument3 SeitenExperiment No 5 ZenerEugene Christina EuniceNoch keine Bewertungen
- EchoDokument11 SeitenEchoapi-394733232100% (3)
- 2.2 Push and Pull Sources of InnovationDokument16 Seiten2.2 Push and Pull Sources of Innovationbclarke113Noch keine Bewertungen
- Physiotherapy For ChildrenDokument2 SeitenPhysiotherapy For ChildrenCatalina LucaNoch keine Bewertungen
- Geoland InProcessingCenterDokument50 SeitenGeoland InProcessingCenterjrtnNoch keine Bewertungen
- Lecture 7Dokument28 SeitenLecture 7Nkugwa Mark WilliamNoch keine Bewertungen
- What Is ForexDokument8 SeitenWhat Is ForexnurzuriatyNoch keine Bewertungen
- Mactor Report - Taller de Prospectiva D 2Dokument39 SeitenMactor Report - Taller de Prospectiva D 2Giovani Alexis Saez VegaNoch keine Bewertungen
- How To Effectively CommunicateDokument44 SeitenHow To Effectively CommunicatetaapNoch keine Bewertungen
- Admission English Test 10thDokument4 SeitenAdmission English Test 10thEduardo100% (1)
- Laser 1Dokument22 SeitenLaser 1Mantu KumarNoch keine Bewertungen
- Ahimsa From MahabharataDokument70 SeitenAhimsa From MahabharataGerman BurgosNoch keine Bewertungen
- Deborah Schiffrin .Tense Variation in NarrativeDokument19 SeitenDeborah Schiffrin .Tense Variation in Narrativealwan61Noch keine Bewertungen
- 8 ActivityDokument3 Seiten8 ActivityNICOOR YOWWNoch keine Bewertungen
- A Re Ection On The Dominant Learning Theories: Behaviourism, Cognitivism and ConstructivismDokument13 SeitenA Re Ection On The Dominant Learning Theories: Behaviourism, Cognitivism and Constructivismchill protocolNoch keine Bewertungen
- Fever and RashDokument14 SeitenFever and RashwirdahajaNoch keine Bewertungen
- Book - IMO Model Course 7.04 - IMO - 2012Dokument228 SeitenBook - IMO Model Course 7.04 - IMO - 2012Singgih Satrio Wibowo100% (4)
- Last Speech of Shri Raghavendra SwamyDokument5 SeitenLast Speech of Shri Raghavendra SwamyRavindran RaghavanNoch keine Bewertungen
- GrandEsta - Double Eyelid Surgery PDFDokument2 SeitenGrandEsta - Double Eyelid Surgery PDFaniyaNoch keine Bewertungen
- Chapter-British Parliamentary Debate FormatDokument8 SeitenChapter-British Parliamentary Debate FormatNoelle HarrisonNoch keine Bewertungen
- SSP ReviwerDokument40 SeitenSSP ReviwerRick MabutiNoch keine Bewertungen
- IJONE Jan-March 2017-3 PDFDokument140 SeitenIJONE Jan-March 2017-3 PDFmoahammad bilal AkramNoch keine Bewertungen
- Types of Sutures and Their IndicationsDokument6 SeitenTypes of Sutures and Their IndicationsAdina BurciuNoch keine Bewertungen