Beruflich Dokumente
Kultur Dokumente
Post Term Guideline
Hochgeladen von
Eko PambudiCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Post Term Guideline
Hochgeladen von
Eko PambudiCopyright:
Verfügbare Formate
British Columbia Reproductive Care Program
Obstetric Guideline 7
POSTTERM PREGNANCY
I. INTRODUCTION
Postterm pregnancy is defined as pregnancy beyond 42 weeks or 294 days gestation from the
LMP.1 Traditionally, it is from 42 weeks gestational age that risk of adverse fetal and neonatal
outcomes, and particularly risk of perinatal death, are increased.1 However, it is known that the
risk of adverse perinatal outcomes may increase as early as 41 completed weeks and is
associated with placental insufficiency.1,2
Data obtained from the B.C. Perinatal Database Registry (BCPDR) and depicted in the graph
below shows the percentage of pregnancies in BC that went to 41 completed weeks (41-416/7),
42 completed weeks (42-426/7), and beyond 42 completed week’s gestation for the periods of
2000/2001 (total deliveries 40,051), 2001/2002 (total deliveries 39,862), and 2002/2003 (total
deliveries 39,791). The trend over the three-year period shows a decreasing percentage of
pregnancies in each of the gestational age categories.
POSTTERM DELIVERIES
14.00
12.00
10.00
Percentage
8.00
6.00
4.00
2.00
0.00
2000/01 2001/02 2002/03
41 weeks 13.64 13.46 12.59
42 weeks 2.09 1.68 1.53
>42 weeks 0.13 0.09 0.08
Source: BC Perinatal Database Registry
Historically, postterm pregnancy has been managed in two ways: either inducing labour at 41to
42 weeks gestation, or awaiting the onset of spontaneous labour while monitoring fetal well
being with ultrasound, electronic fetal monitoring, and daily fetal movement counts. Up until
1992 it was unclear which was the better approach for management. In 1992 the results of an
international randomized control trial3 suggested that induction of labour results in a lower rate
of cesarean section than serial antenatal monitoring, while the rates of perinatal mortality and
neonatal morbidity are similar.
March 2005 Page 1 of 8
Postterm Pregnancy
The recommendations in this guideline are based predominantly on the results of a review
completed by Crowley4 and published in the Cochrane Library. The main results in this review
are:
• Routine early pregnancy ultrasound reduces the number of women who require induction of
labour for apparent postterm pregnancy
• Inducing labour at > 41 weeks results in a lower rate of non-reassuring fetal heart tracings, a
lower rate of meconium stained amniotic fluid, and a lower rate of fetal macrosomia
(> 4,000 gms)
• Routine induction of labour at > 41 weeks reduces perinatal mortality, predominantly
because of the decreased stillbirth rate (OR 0.20, CI (95%) 0.06 – 0.70)
• Nipple stimulation in third trimester does not appear to affect the incidence of postterm
pregnancy
• Routine induction does not increase the caesarean section rate for both nulliparous and
parous women in postterm pregnancies compared to serial antenatal monitoring in postterm
pregnancy
Also published in the Cochrane Library is Boulain’s recent review of sweeping the membranes at
term. When performed as a general policy in women at term, this intervention appears to be
associated with reduced duration of pregnancy and reduced frequency of pregnancy continuing
beyond 41 weeks (RR 0.59, 95% CI 0.46 to 0.74) and 42 weeks (RR 0.28, 95% CI 0.15 to 0.50).5
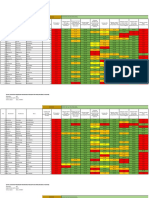
1.1 BC RATES OF CAESAREAN SECTION FOR SPONTANEOUS AND INDUCED LABOUR
AT 41, 42, AND >42 WEEKS GESTATIONAL AGE (NULLIPAROUS & MULTIPAROUS)
Data tables provided by the BCPDR are included on page 3and 4 to depict provincial rates of
caesarean section for both spontaneous and induced labour at 41, 42, and >42 weeks gestational
age (nulliparous p.3 and multiparous p.4) for the time periods of 2000/2001, 2001/2002, and
2002/2003.
The rates of caesarean section are generally consistently higher in the induced group versus those
who had spontaneous labour with expectant management, with the greatest difference in rates
apparent in the nulliparous group. It is apparent from the higher rate of caesarean section in the
induced groups that the provincial data do not replicate research findings reported in the
literature. The reasons for this may include stringent research controls utilized during
randomized clinical trials, strictly defined inclusion and exclusion criteria, and consistent
methods of induction. Primary care providers should be selective regarding who is induced, and
cognizant of the need for cervical ripening prior to initiating labour induction.
March 2005 Page 2 of 8
Postterm Pregnancy
Deliveries of Nulliparous Mothers @ 41, 42, >42 Weeks
April 1, 2000 to March 31, 2003
British Columbia Perinatal Database Registry
APRIL 1, 2000 TO MARCH 31, 2001
Gestational Age Spontaneous Labour Induced Labour
(Completed Vaginal C/Section Total Vaginal C/Section Total
Weeks) # % # % Deliveries # % # % Deliveries
41 1178 75.76 377 24.24 1,555 825 60.62 536 39.38 1,361
42 151 72.95 56 27.05 207 153 55.84 121 44.16 274
>42 16 76.19 5 23.81 21 2 25.00 6 75.00 8
APRIL 1, 2001 TO MARCH 31, 2002
Gestational Age Spontaneous Labour Induced Labour
(Completed Vaginal C/Section Total Vaginal C/Section Total
Weeks) # % # % Deliveries # % # % Deliveries
41 953 71.65 377 25.86 1,330 861 59.13 595 40.87 1,456
42 114 72.15 44 27.85 158 120 59.70 81 40.30 201
>42 7 77.78 2 25.00 9 1 33.33 2 66.67 3
APRIL 1, 2002 TO MARCH 31, 2003
Gestational Age Spontaneous Labour Induced Labour
(Completed Vaginal C/Section Total Vaginal C/Section Total
Weeks) # % # % Deliveries # % # % Deliveries
41 1,007 72.87 375 27.13 1,382 801 58.17 576 41.83 1,377
42 117 70.91 48 29.10 165 97 53.89 83 46.11 180
>42 9 90.00 1 10.00 10 5 50.00 5 50.00 10
DELIVERIES INCLUDE STILLBIRTHS AND LIVE BIRTHS
March 2005 Page 3 of 8
Postterm Pregnancy
Deliveries of Multiparous Mothers @ 41, 42, >42 Weeks
April 1, 2000 to March 31, 2003
British Columbia Perinatal Database Registry
APRIL 1, 2000 TO MARCH 31, 2001
Spontaneous Labour Induced Labour
Gestational Age Vaginal C/Section Total Vaginal C/Section Total
(Completed Weeks) # % # % Deliveries # % # % Deliveries
41 1,297 91.02 128 8.99 1,425 891 88.31 118 11.69 1,009
42 184 93.88 12 6.12 196 120 92.31 10 7.69 130
>42 13 86.67 2 13.33 15 6 85.71 1 14.29 7
APRIL 1, 2001 TO MARCH 31, 2002
Spontaneous Labour Induced Labour
Gestational Age Vaginal C/Section Total Vaginal C/Section Total
(Completed Weeks) # % # % Deliveries # % # % Deliveries
41 1,232 93.05 92 6.95 1,324 1,007 90.8 102 9.2 1,109
42 132 86.27 21 13.73 153 113 91.13 11 8.87 124
>42 11 84.62 2 15.38 13 6 100.00 0 0.00 6
APRIL 1, 2002 TO MARCH 31, 2003
Spontaneous Labour Induced Labour
Gestational Age Vaginal C/Section Total Vaginal C/Section Total
(Completed Weeks) # % # % Deliveries # % # % Deliveries
41 1,114 91.01 110 8.99 1,224 825 89.87 93 10.13 918
42 124 91.18 12 8.82 136 81 83.51 16 16.49 97
>42 10 100.00 0 0.00 10 3 100.00 0 0.00 3
DELIVERIES INCLUDE STILLBIRTHS AND LIVE BIRTHS
2000/2001 - Full Provincial Participation
(Births Under 300 - 55 facilities; Births 300 to 499 (Includes Home Births) - 3 facilities; Births 500+ - 22 facilities)
2001/2002 - Full Provincial Participation
(Births Under 300 - 51 facilities; Births 300 to 499 (Includes Home Births) - 6 facilities; Births 500+ - 21 facilities)
2002/2003 - Full Provincial Participation
(Births Under 300 - 48 facilities; Births 300 to 499 (Includes Home Births) - 8 facilities; Births 500+ - 20 facilities)
March 2005 Page 4 of 8
Postterm Pregnancy
2. FETAL RISKS
• Fetal macrosomia
• Meconium aspiration
• Cerebral palsy
• Neonatal encephalopathy
• IPPV (with intubation)
• Perinatal death
3. CLINICAL MANAGEMENT (See Appendix A: Postterm Clinical Management Algorithm)
3.1 GESTATIONAL AGE CALCULATION
Gestational age must be assessed carefully to avoid delivery of a premature infant. Because
actual dates of conception are rarely known, the LMP is used as the reference point. This,
however, can make the accuracy of gestational age determination unreliable because of:
• Irregular menses
• A cycle length other than 28 days
• Recent cessation of the birth control pill
• Inconsistent ovulation times
Reviews compiled in the Cochrane Library4,6 found that routine early pregnancy ultrasound
reduces the number of women who require induction of labour for apparent post-term pregnancy.
Based on this evidence, it is recommended is that all pregnant patients, and certainly those who
do not have regular menses, have an ultrasound examination for gestational age assessment, prior
to 20 weeks; preferably between 18 – 19 weeks. If there is more than a one week discrepancy
between the LMP and the ultrasound findings, then the ultrasound findings should be used to
determine the EDD.
Management options will depend on gestational age, absence/presence of maternal risk
factors and/or evidence of fetal compromise, and maternal preferences/informed consent.
3.2 MANAGEMENT TO 406/7 WEEKS GESTATION
A. Healthy, uncomplicated pregnancy and fetal growth/amniotic fluid normal
For the healthy, uncomplicated pregnancy, there is no evidence to support elective induction of
labour and there is no evidence to support commencement of serial antenatal monitoring - non
stress test (NST) or Amniotic Fluid Index (AFI). (See Appendix B: Amniotic Fluid Index
Interpretation).
B. Presence of maternal risk factors or evidence of fetal compromise
Recommend cervical ripening as necessary and induction (See BCRCP Obstetric Guideline 1:
Induction of Labour) if there is evidence of maternal risk factors or evidence of fetal compromise
such as:
• Intrauterine growth restriction:
• symphysis-fundal height small for gestational age
• IUGR and/or oligohydramnios diagnosed by ultrasound
• maternal weight loss or inadequate weight gain
• Non-reassuring or non-reactive NST
March 2005 Page 5 of 8
Postterm Pregnancy
3.3 MANAGEMENT AT 41 WEEKS GESTATION7
A. Healthy, uncomplicated pregnancy
Inform the woman of the options and risks/benefits of labour induction versus expectant
management, and offer her labour induction. Establish the Bishop Score and ensure a ripening
agent is used as necessary, prior to induction.
B. If mother declines induction, then provide expectant management:
• Daily fetal movement counts
• NST twice/week to 42 weeks
• Ultrasound to assess AFI twice weekly to 42 weeks
• If either the NST or AFI is abnormal, then initiate induction immediately
• If AFI assessment is not available, then induce
• Induce at 42 weeks if NST and AFI normal
3.4 MANAGEMENT DURING LABOUR AND DELIVERY
Consider amniotomy to diagnose thick meconium. If meconium stained amniotic liquor is
present then consider risk of meconium aspiration; continuous fetal assessment with electronic
fetal monitoring (EFM) is recommended. If meconium and variable decelerations are present,
then consider amnioinfusion. If the woman has meconium stained liquor and a non-reassuring
EFM tracing and is in a facility without operating room (OR) capability, then transfer to a
facility with OR capability should be considered. Be prepared for shoulder dystocia and
neonatal resuscitation at delivery (See Newborn Guideline 7: Newborn Resuscitation, Resources
and Education).
REFERENCES
1. Society of Obstetricians and Gynecologists of Canada. (2002). Fetal Health Surveillance in
Labour. SOGC Clinical Practice Guidelines. SOGC, Ottawa.
http://www.sogc.org/sogcnet/sogc_docs/common/guide/pdfs/ps112.pdf
2. Feldman, G. (1992). Prospective risk of stillbirth. Obstetrics and Gynecology, 79: p.547-53.
3. Hannah, M., et al. (1992). Induction of labour as compared with serial antenatal monitoring
in post-term pregnancy. The New England Journal of Medicine, 326(24), p.1587-92.
4. Crowley, P. (2003). Interventions for preventing or improving the outcome of delivery at or
beyond term (Cochrane Review). In: The Cochrane Library, Issue 4, 2003. Chichester, UK,
John Wiley & Sons, Ltd.
5. Bouvain, M., Stan, C., & Irion, O. (2005). Membrane Sweeping for Induction of Labour. In:
The Cochrane Library, Issue I, 2005. Chichester, UK: John Wiley & Sons, Ltd.
http://www.update-software.com/abstracts/ab000451.htm (Abstract)
6. Neilson, P. (2004). Ultrasound for fetal assessment in early pregnancy (Cochrane Review).
In: The Cochrane Library, Issue I, 2004. Chichester, UK: John Wiley & Sons, Ltd.
7. Society of Obstetricians and Gynecologists of Canada. (1997). Post-term Pregnancy. SOGC
Clinical Practice Guidelines. SOGC, Ottawa.
8. Moore TR, & Cayle JE. (1990). The amniotic fluid index in normal human pregnancy.
American Journal of Obstetrics and Gynecology, 162(5), p. 1168-73.
March 2005 Page 6 of 8
Postterm Pregnancy
APPENDIX A
POSTTERM PREGNANCY
CLINICAL MANAGEMENT ALGORITHM
Gestational Age
17-20 weeks
(Preferably 18-19 weeks)
• Perform ultrasound.
If >1 week discrepancy with
dates, use U/S to determine G.A.
Healthy Pregnancy To 406/7 weeks Maternal risk factors
or evidence of fetal
Elective induction Not compromise
NST Recommended
AFI Recommend cervical
ripening as necessary
and Induction
At 41 weeks
Inform woman of risks and
benefits of elective induction vs.
expectant management, and
offer her labour induction.
Elective Induction Expectant Management
at 41 weeks
▪ Explain procedure &
book induction Daily fetal movement
▪ Establish Bishop Score counts
and ensure ripening NST’s twice weekly
agent is used prior to U/s for fetal size and AFI
induction, as necessary twice weekly
If AFI not available or
if NST or AFI abnormal
At 42 weeks Induce Immediately
Induce
March 2005 Page 7 of 8
Postterm Pregnancy
APPENDIX B
AMNIOTIC FLUID INDEX (AFI) INTERPRETATION8
The amount of amniotic fluid has a range of normal values, and is expressed as a score derived
by adding up the centimeters of depth of four pockets of fluid seen on ultrasound. Some
researchers feel one good pocket of 3 centimeters depth is enough to assume that there is an
adequate amount of amniotic fluid around the rest of the baby, but traditionally the AFI is
calculated as the sum of four pockets.
Normal AFI 6 cm - 18 cm (5th percentile to 95th percentile)
Mean approximately 12 cm
Oligohydramnios: AFI < 5 cm (<5th percentile)
Polyhydramnios: AFI > 18 cm (95th percentile)
AMNIOTIC FLUID INDEX (AFI) INTERPRETATION8
The amount of amniotic fluid has a range of normal values, and is expressed as a score derived
by adding up the centimeters of depth of four pockets of fluid seen on ultrasound. Some
researchers feel one good pocket of 3 centimeters depth is enough to assume that there is an
adequate amount of amniotic fluid around the rest of the baby, but traditionally the AFI is
calculated as the sum of four pockets.
Normal AFI 6 cm - 18 cm (5th percentile to 95th percentile)
Mean approximately 12 cm
Oligohydramnios: AFI < 5 cm (<5th percentile)
Polyhydramnios: AFI > 18 cm (95th percentile)
March 2005 Page 8 of 8
Das könnte Ihnen auch gefallen
- Sheldon Raccoona - The Screwfly SolutionDokument17 SeitenSheldon Raccoona - The Screwfly Solutionscribdcarlota100% (2)
- Bovans Brown Management Guide 071021Dokument48 SeitenBovans Brown Management Guide 071021Kiggundu RonaldNoch keine Bewertungen
- Megalourethra - Clinical Review and ManagementDokument4 SeitenMegalourethra - Clinical Review and ManagementNugroho HarsonoNoch keine Bewertungen
- Contribution of EclampsiaDokument25 SeitenContribution of EclampsiaUsha AnengaNoch keine Bewertungen
- EPI BangladeshDokument4 SeitenEPI BangladeshToufiq Rahman100% (1)
- Alert: ATTENTION: Perinatal Care ProvidersDokument30 SeitenAlert: ATTENTION: Perinatal Care Providersrevathidadam55555Noch keine Bewertungen
- 4&5project Birth AsphyxiaDokument16 Seiten4&5project Birth AsphyxiaJanice ScatesNoch keine Bewertungen
- Childbirth and The Female Pelvic Floor: Christopher Maher Wesley UrogynaecologyDokument54 SeitenChildbirth and The Female Pelvic Floor: Christopher Maher Wesley UrogynaecologyVeronica MendozaNoch keine Bewertungen
- Ramón y Cajal Hospital, Madrid, SpainDokument2 SeitenRamón y Cajal Hospital, Madrid, SpainMarkoNoch keine Bewertungen
- No Kode Diagnosa Utama Jumlah %Dokument3 SeitenNo Kode Diagnosa Utama Jumlah %Ryan AkbarNoch keine Bewertungen
- A Prospective Study On The Maternal Outcome in Cases of Previous One Cesarean SectionDokument6 SeitenA Prospective Study On The Maternal Outcome in Cases of Previous One Cesarean SectionIJAR JOURNALNoch keine Bewertungen
- (Fitriani) Tugas BiosDokument7 Seiten(Fitriani) Tugas BiosereNoch keine Bewertungen
- Rekapitulasi Indeks Keluarga Sehat Per RW Di Tanjungmulya Per Maret 2019Dokument9 SeitenRekapitulasi Indeks Keluarga Sehat Per RW Di Tanjungmulya Per Maret 2019ilham nasrullohNoch keine Bewertungen
- Cervical Ripening & Induction of Labour: Obstetric Guideline 1Dokument10 SeitenCervical Ripening & Induction of Labour: Obstetric Guideline 1Maizura Syahirah MohtadaNoch keine Bewertungen
- Intraoperative Surgical Complication During Cesarean SectionDokument14 SeitenIntraoperative Surgical Complication During Cesarean Sectioncarbolico100% (1)
- Frequencies - 108Dokument12 SeitenFrequencies - 108D3Noch keine Bewertungen
- Chapter Four ShalomDokument9 SeitenChapter Four ShalomtewodrosbayisaNoch keine Bewertungen
- Lampiran Hasil Analisis Lampiran 1. Karakteristik Sampel: Usia Ibu Saat HamilDokument5 SeitenLampiran Hasil Analisis Lampiran 1. Karakteristik Sampel: Usia Ibu Saat HamildeoNoch keine Bewertungen
- Iajt 00 I 4 P 156Dokument5 SeitenIajt 00 I 4 P 156api-3702148Noch keine Bewertungen
- Chapter Four Results The Study Sample: Frequency Percent Valid Percent Cumulative Percent 1Dokument4 SeitenChapter Four Results The Study Sample: Frequency Percent Valid Percent Cumulative Percent 1Azhi BrownNoch keine Bewertungen
- Study of Prolonged Pregnancy Between 40-42 WeeksDokument3 SeitenStudy of Prolonged Pregnancy Between 40-42 WeeksInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Beta Estimation - Additional ReadingsDokument87 SeitenBeta Estimation - Additional ReadingsReever RiverNoch keine Bewertungen
- Anemia en RNDokument21 SeitenAnemia en RNDaniel Martinez DiazNoch keine Bewertungen
- Rata FertilitatiiDokument7 SeitenRata FertilitatiiBaidac Valentin AlexandruNoch keine Bewertungen
- Rekapitulasi Indeks Keluarga Sehat Per Kelurahan Di Seberida Tahun 2019Dokument11 SeitenRekapitulasi Indeks Keluarga Sehat Per Kelurahan Di Seberida Tahun 2019Pitriana JayantiNoch keine Bewertungen
- PROM PPT UpdatedDokument26 SeitenPROM PPT Updatedsaurabh chauhanNoch keine Bewertungen
- Sheiko - 4-Day Class I Lifter ProgramDokument20 SeitenSheiko - 4-Day Class I Lifter Programclaymore7072049100% (1)
- Sheiko 4 Day ProgramDokument22 SeitenSheiko 4 Day ProgramJohn VatistasNoch keine Bewertungen
- Obesity in Pregnancy and It's OutcomeDokument14 SeitenObesity in Pregnancy and It's Outcomepavani pNoch keine Bewertungen
- Week/Date Comments Weight BMI Before Enrolling Week 1 Week 2 Week 3 Week 4 Week 5 Week 6 Week 7Dokument7 SeitenWeek/Date Comments Weight BMI Before Enrolling Week 1 Week 2 Week 3 Week 4 Week 5 Week 6 Week 7Mohnish Alka ThakkarNoch keine Bewertungen
- Xternal Ephalic Ersion: E Z W ' H P C P GDokument4 SeitenXternal Ephalic Ersion: E Z W ' H P C P GJuan SetiajiNoch keine Bewertungen
- Mothe UpdateDokument3 SeitenMothe UpdateNellyVenus85Noch keine Bewertungen
- A Comparative StudyDokument8 SeitenA Comparative StudyNatalija StamenkovicNoch keine Bewertungen
- SpssDokument5 SeitenSpssHaikal AlpinNoch keine Bewertungen
- Newborn Hypoglycemia Prevention and Care Learning Session IIDokument43 SeitenNewborn Hypoglycemia Prevention and Care Learning Session IIkcochranNoch keine Bewertungen
- Report COVID Clinical ManagmentDokument70 SeitenReport COVID Clinical ManagmentJeevan Emmanual JoyNoch keine Bewertungen
- Protein ElectrophoresisDokument5 SeitenProtein ElectrophoresisElissiaNoch keine Bewertungen
- Pediatric MedicalsDokument20 SeitenPediatric Medicalsalexandra stanescuNoch keine Bewertungen
- Process1 - Pemetaan Prevalensi Stunting Dan Cakupan Program - revNTT (3) .Dokument126 SeitenProcess1 - Pemetaan Prevalensi Stunting Dan Cakupan Program - revNTT (3) .Promkez SikkaNoch keine Bewertungen
- Ujian Metris II - HerikaDokument14 SeitenUjian Metris II - HerikaErie MoetzNoch keine Bewertungen
- Rekap Indikator Mutu Ukm 2021Dokument4 SeitenRekap Indikator Mutu Ukm 2021Erna SawitriNoch keine Bewertungen
- Pedometer Data in Middle-Aged Romanian Women: A Pilot StudyDokument6 SeitenPedometer Data in Middle-Aged Romanian Women: A Pilot Studydonca_deliaNoch keine Bewertungen
- Queuing StudyDokument20 SeitenQueuing StudyOmer Autida El AwadNoch keine Bewertungen
- Weight For Height As A Measure of Nutritional Status in Filipino Pregnant WomenDokument9 SeitenWeight For Height As A Measure of Nutritional Status in Filipino Pregnant WomenCecilia AcuinNoch keine Bewertungen
- Unlock OBGuidelinesPainManagement4Dokument30 SeitenUnlock OBGuidelinesPainManagement4herry2swNoch keine Bewertungen
- Risk Factors For Pelvic Surgery: Y.E. Erata B. Kilic S. Güçlü U. Saygili T. UsluDokument5 SeitenRisk Factors For Pelvic Surgery: Y.E. Erata B. Kilic S. Güçlü U. Saygili T. UsluGleiciane AguiarNoch keine Bewertungen
- OUTPUTSasaran DESADokument65 SeitenOUTPUTSasaran DESANursyifa SofiantiNoch keine Bewertungen
- Bmi Tobornhs JHS 2022 2023Dokument108 SeitenBmi Tobornhs JHS 2022 2023Janus SalinasNoch keine Bewertungen
- Physical Assess ReportDokument16 SeitenPhysical Assess ReportNur Izzah AnisNoch keine Bewertungen
- Hydrological Study of Handi Khola Bridge Site, Taplejung 1 GeneralDokument14 SeitenHydrological Study of Handi Khola Bridge Site, Taplejung 1 GeneralriteshreplyNoch keine Bewertungen
- Breastfeeding and Asthma Outcomes at The Age of 6 Years. The Generation R StudyDokument15 SeitenBreastfeeding and Asthma Outcomes at The Age of 6 Years. The Generation R StudyGifanichan MvpshawolandromedaNoch keine Bewertungen
- Lampiran Hasil Analisa DataDokument30 SeitenLampiran Hasil Analisa DataDwi Wulan Novia EdyaniNoch keine Bewertungen
- Vacunas 20210609Dokument4 SeitenVacunas 20210609raulchcrNoch keine Bewertungen
- Operatia Cezariana Vejnovic2019-10-06 - 212137Dokument1 SeiteOperatia Cezariana Vejnovic2019-10-06 - 212137Laurențiu LucaNoch keine Bewertungen
- ASN.2013091003 ASN2013091003SupplementaryDataDokument20 SeitenASN.2013091003 ASN2013091003SupplementaryDataWihel PaulaNoch keine Bewertungen
- DystociaDokument8 SeitenDystociaCylin Dadural100% (1)
- 08 Chapter 08Dokument28 Seiten08 Chapter 08Miguel Antonio Barretto GarcíaNoch keine Bewertungen
- Concepts of Neonatal Care: Reported By: Genevieve Manrique R.NDokument18 SeitenConcepts of Neonatal Care: Reported By: Genevieve Manrique R.NLoggerz ArckNoch keine Bewertungen
- Provinsi: Kalimantan BaratDokument4 SeitenProvinsi: Kalimantan BaratDika Dika FaithNoch keine Bewertungen
- Terms and DefinitionsDokument31 SeitenTerms and DefinitionskauluzavanessaNoch keine Bewertungen
- OUTPUTDokument5 SeitenOUTPUTRavalandry EcvadyAnafeverNoch keine Bewertungen
- Telegram Cloud Document 5 6274073709007339605Dokument6 SeitenTelegram Cloud Document 5 6274073709007339605IlhamNoch keine Bewertungen
- G-Spots: The Clitoris, A-Spot, G-Spot and U-SpotDokument4 SeitenG-Spots: The Clitoris, A-Spot, G-Spot and U-SpotraviikumarNoch keine Bewertungen
- Vaginal Exam Learning GuideDokument2 SeitenVaginal Exam Learning GuideAprilian Ayu SitaNoch keine Bewertungen
- Animal 3Dokument48 SeitenAnimal 3Khairy IestNoch keine Bewertungen
- Superovulasi PDFDokument68 SeitenSuperovulasi PDFHayatul IlmiNoch keine Bewertungen
- Zulu Birth Project BrochureDokument3 SeitenZulu Birth Project BrochureTanya ParkerNoch keine Bewertungen
- Certificate of Death 1Dokument2 SeitenCertificate of Death 1Charley Labicani BurigsayNoch keine Bewertungen
- Imaging PadaDokument77 SeitenImaging PadaNaja HasnandaNoch keine Bewertungen
- Wildlife Fact File - Primitive Animals - Pgs. 11-20Dokument20 SeitenWildlife Fact File - Primitive Animals - Pgs. 11-20ClearMind84100% (1)
- 40 Reasons You Should Quit Watching Porn TodayDokument12 Seiten40 Reasons You Should Quit Watching Porn TodayThavam RatnaNoch keine Bewertungen
- 696 2545 1 PBDokument7 Seiten696 2545 1 PBAnggun SasmitaNoch keine Bewertungen
- Cystic Fibrosis EssayDokument4 SeitenCystic Fibrosis EssayKitanaNoch keine Bewertungen
- Klinefelter SyndromeDokument12 SeitenKlinefelter SyndromeJustine Mae BatadlanNoch keine Bewertungen
- The Ultimate Sex Guide - Squirting Cunnilingus G-Spot Anal Vagina Clitoris Games Love Tecniques Tips Tricks Positions Kamasutra Secrets For Dummies XXXDokument43 SeitenThe Ultimate Sex Guide - Squirting Cunnilingus G-Spot Anal Vagina Clitoris Games Love Tecniques Tips Tricks Positions Kamasutra Secrets For Dummies XXXhoz1430% (4)
- DR FdarDokument2 SeitenDR FdarHenry Philip Sabado Presto0% (1)
- Jennifer B. Cagandahan CaseDokument10 SeitenJennifer B. Cagandahan CaseFrank Gernale GolpoNoch keine Bewertungen
- Provision of ATSMs in WoS September 2009Dokument2 SeitenProvision of ATSMs in WoS September 2009WAGS CommitteeNoch keine Bewertungen
- Chinese Birth Calendar - Predict Your Babies GenderDokument6 SeitenChinese Birth Calendar - Predict Your Babies GenderFemi AdesinaNoch keine Bewertungen
- Virginity Test and Corruption Kelompok 5Dokument8 SeitenVirginity Test and Corruption Kelompok 5Novita AinunNoch keine Bewertungen
- Ectopic and Abortion NCPDokument6 SeitenEctopic and Abortion NCPElizabeth Quiñones100% (1)
- Endometriosis PresentationDokument58 SeitenEndometriosis PresentationBRI KUNoch keine Bewertungen
- Postpartum QuestionsDokument2 SeitenPostpartum QuestionsRayMendez100% (4)
- Chapter14 Ob Physical and Physiological Changes During PregnancyDokument57 SeitenChapter14 Ob Physical and Physiological Changes During Pregnancyth233Noch keine Bewertungen
- The Origins of Cerebral Palsy: John M. Keogh and Nadia BadawiDokument6 SeitenThe Origins of Cerebral Palsy: John M. Keogh and Nadia BadawiC_DanteNoch keine Bewertungen
- List of Semen StationsDokument6 SeitenList of Semen StationsYogesh NNoch keine Bewertungen
- B. General Measure, Mgso4 Antihipertensi, C SectionDokument4 SeitenB. General Measure, Mgso4 Antihipertensi, C SectionValensia VivianNoch keine Bewertungen
- GB1 - W4 Module 2 1st QTR 1Dokument145 SeitenGB1 - W4 Module 2 1st QTR 1AyaNoch keine Bewertungen
- Requirement Curriculum DevelopmentDokument32 SeitenRequirement Curriculum DevelopmentArvi CalaguiNoch keine Bewertungen